Abstract
Background
Evidence suggests obesity can have a negative influence on a child's motor development and postural control behavior. Little research has examined the impact of infant weight on gross motor behavior, particularly postural control at the onset of sitting.
Objective
The purpose of this study was to determine whether normal weight and overweight infants differed in their postural control strategies at the onset of sitting and one-month post onset of sitting.
Methods
29 infants (n=19 normal weight, n=10 overweight) were recruited to participate in this study. Infant's length and weight were measured at 3 months of age (visit 1). Infant's center of pressure (COP) was measured on an AMTI force platform at the onset of sitting (visit 2) and one-month post onset (visit 3). Data were analyzed using linear measures (range and RMS for the anterior/posterior (AP) and medial/lateral (ML) directions, sway path) and nonlinear measures (Sample Entropy in AP and ML directions).
Results
Overweight infants had significantly greater RMS values in the ML direction at visit 2 and reduced Sway Path values in comparison to normal weight infants at visits 2 and 3. Further, there was a significant difference in Sample Entropy as overweight infants increased Sample Entropy from visit 2 to 3 while normal weight infants decreased Sample Entropy values during this time period.
Conclusions
These findings suggest that overweight infants adopt a different postural control strategy. This altered strategy may limit exploration early in development. More research is needed to determine if longitudinal differences continue to emerge.
Keywords: overweight, obesity, postural control, sitting
Introduction
Worldwide, more than 40 million children under the age of 5 are overweight or obese [1]. The first year of a child's life can make a significant impact on their long-term health as rapid increases in weight during the first 6 months has been associated with increased risk for obesity at age 3 [2]. Furthermore, obese children are more likely to become obese adults [3]. Childhood obesity greatly increases one's risk of high blood pressure, high cholesterol, and type 2 diabetes and being obese as an adult is associated with a variety of chronic health problems including coronary heart disease and some cancers [4]. Another negative effect of obesity that has not received sufficient attention is altered postural control.
Research examining the effect of obesity on children's motor development and postural balance has suggested that obesity may limit motor development and postural balance [5,6]. Several research groups have identified poor gross motor development in obese children [7-9]. McGraw et al., [7] found that obese pre-pubertal boys had greater standing postural sway than non-obese boys. Infant motor skill development is also influenced by being overweight and obesity. Overweight infants presented with gross motor delays in comparison to normal weight infants [10]. In contrast, others have found that even though overweight infants are able to achieve sitting earlier, early sitting was unrelated to overall motor development [11]. However, there is limited research published about infants in relation to obesity, and more specifically in terms of how they achieve sitting postural control.
Learning how to sit without support and maintain postural control is a key developmental milestone. Once infants are able to sit without support, they have improved opportunities for visual exploration as well as the ability to improve fine motor skills through reaching nearby items [12,13]. Unfortunately, infant obesity may alter the natural patterns of movement to achieve the sitting milestone, which is key in allowing infants to better explore the world around them [14]. The attainment of this motor milestone is fundamental to the achievement of other developmental milestones, such as running that promotes physical activity, a known factor associated with maintaining a healthy weight [15]. Additionally, research has shown a positive relationship between reaching motor and speech developmental milestones and cognitive abilities later in life [16,17]. For instance, the earlier a child learned to stand was associated with a small increase in intelligence quotient (IQ) at the age of eight [18]. Additionally, a child's gross motor skills have been found to be predictive of working memory and cognitive processing speed [17]. During adulthood, a significant linear relationship has been found between the age of standing and adult executive function [16].
The early years are critical to the prevention of obesity, improved cognitive outcomes and they are related to long-term health risks [18,19].Thus, it is imperative to determine the earliest point of intervention for identifying those who may be at risk for developmental delays. Assessing sitting postural control has been used previously to determine differences between typically developing infants and infants who may be at risk for developmental delays [12,20]. Sitting posture can be examined qualitatively, by observation, or by investigating the center of pressure (COP) trajectories as an infant sits on a force platform. COP data allows researchers to objectively quantify postural sway, providing a more accurate view of postural control patterns. Patterns of infants sitting posture, through the COP can be explored with two different ways: with linear and nonlinear measures of postural sway. Linear measures provide information on the quantity of movement, or in other words the amount of postural sway. Nonlinear measures provide information on patterns of movement potentially indicating the quality of movement [12,21]. Specifically, nonlinear measures allow the evaluation of the temporal structure of postural sway time series or how a set of values in a particular distribution are organized in time or even across a range of time scales [20].The combination of these measures gives us the opportunity to unravel different patterns of organization, which could reflect the strategies used to maintain a sitting position. Previously the complimentary use of these measures was able to provide a more complete and thorough description of the development of sitting [20,22] as well as the ability and sensitivity to identify progress through development and intervention [23].
Therefore, the purpose of this study was to determine whether normal weight and overweight infants differed in their postural control strategies at the onset of sitting and one-month post onset of sitting. We hypothesized that overweight infants would achieve the motor skill milestone of sitting at the same time or later than normal weight infants and that they will exhibit increased (linear measures) and very repetitive and rigid (nonlinear measures) postural sway during sitting in comparison to the normal weight infants.
Methods
Participants
We recruited 29 infants (19 normal weight, 10 overweight to participate in this study. Infants were recruited at three months of age from local baby friendly businesses (e.g., pediatricians, WIC clinics), social media (e.g., Facebook), and word of mouth (e.g., family/friend recommendations). Exclusion criteria included having a birth defect or congenital abnormality, having been born preterm (<37 weeks), a weight-for-length z score <5th percentile (underweight), or any other diagnosed medical condition that might affect brain development, visual, auditory or motor impairment. Inclusion criteria included typically developing infants < 3 months of age. Before data collection was initiated, caregivers provided informed consent using documents approved by a university institutional review board. Infants were classified into two groups based on weight for length z-score [1]. Due to infant temperament during data collection (i.e., sitting on the force place for three 10-second trials) 23 out of the 29 infants were able to produce useable data for both visits two and three. Thus the two groups included 9 overweight infants (<90th percentile) and 14 normal weight infants (>90th percentile).
Procedures
Participation involved three visits to a university research lab. Visit 1 occurred at 3-months of age (mean age [SD], 3 months, 3 days [11.98] days), visit 2 occurred at the onset of sitting (5 months, 3 days (160 [27.15] days), and visit 3 occurred one-month post onset of sitting 6 months, 5 days (195 [26.24] days). Infants' anthropometric measurements were completed by one of three trained graduate students. Infants were undressed to their diapers by caregivers prior to the measurements. In order to classify infants into normal weight or overweight, at the first visit weight was measured to the nearest 10 g via a Detecto Pediatric scale. Length was measured to the nearest .1 cm via a SECA infantometer [5]. Head and abdominal circumference were measured to the nearest .5 and .1 cm, using a standard tape measure. Abdominal circumference was measured immediately above the belly button and head circumference was measured by wrapping the measuring tape above the infant's eyebrows and ears.
To determine postural control, at visit 2 and 3, an AccuSway AMTI force platform was used to record infants COP data. Caregivers were asked to contact research personnel once their infant was able to sit independently for 10 seconds. Research personnel then scheduled a time for caregivers and infants to come to the motor development lab. If research personnel had not heard from caregivers within one month of the initial visit a follow-up phone call was made to assess sitting status. The researcher then contacted the mothers every two weeks until it was confirmed sitting had occurred. To determine independent sitting time at each visit, component forces (Fx, Fy, Fz) and moments (Mx, My, Mz) were sampled at 200 Hz based on frequency analysis. To collect data, once an infant was calm, they were placed in the sitting position in the middle of the force plate. Research personnel held the infant at the trunk, gradually letting go until the infant was able to sit independently while the caregiver or other research personnel distracted the infant with toys. For safety purposes, the caregiver and research personnel were in front of and by the side of the infant to prevent unstable positions such as falling. Data collection began once research personnel were able to completely let go of the infant. At this time the caregiver or research personnel remained still in order to not divert the infants' attention. Data were collected continuously while the infant attempted to sit independently and continued until the infant had performed three trials of 10 seconds of sitting. A maximum of 10 minutes was allowed to obtain these trials.
Data Analysis
COP displacements in both the anterior-posterior (AP) and medial-lateral (ML) sway directions were calculated from the forces and moments through the Qualisys (Qualisys medical AB, Gothenburg, Sweden) software that was integrated with the AMTI (Advanced Mechanical Technology Inc, 176 Waltham St, Watertown, MA 02472-4800) force platform. Data were then exported in .txt format, which was then used for analysis. Linear and nonlinear measures were calculated and averaged from the COP paths of the three sitting trials. Customized MatLab software was utilized to calculate the linear measures from the COP data from the selected trials, using the methodology of Prieto et al. (1996) [24]. Linear measures included the RMS and the range of the COP path in both the AP and ML directions, as well as the sway path (total length of the COP trajectory). One nonlinear measure was calculated from the COP paths in both the AP and ML directions: Sample Entropy (SampEn). The SampEn was calculated using the algorithm of Richman and Moorman (2000) implemented in MATLAB (Mathworks, USA) [25]. This measure is a regularity statistic that quantifies the probability that similar patterns of observations in the COP path will not be followed temporally by additional similar observations.
Statistical Analysis
Descriptive statistics were run to describe the samples and dependent variables. An independent t-test was used to test whether the age at which overweight and normal weight infants achieved the sitting skills differed significantly between the groups. A mixed way ANOVA model (2×2) was used to assess differences in the the postural control measures between normal and overweight infants (Group, non repeating factor) at the 2nd and 3rd visits (Visit, repeating factor). The p value was set at 0.05 while we also computed the eta squared to determine the effect size when appropriate.
Results
There was no significant difference in the age of onset of sitting between overweight and normal weight infants (Table 1).
Table 1.
Infant Demographics.
| Normal Weight (n=14) | Overweight n=9 | |
|---|---|---|
| Weight (lb) | ||
| Mean (SD) | 14.27±1.68 | 16.92±2.06 |
| Length (cm) | ||
| Mean (SD) | 61.69±2.75 | 62.79±2.23 |
| Z-score | ||
| Mean (SD) | 0.13±0.93 | 1.39±0.88 |
| Head Circumference (cm) | ||
| Mean (SD) | 40.8±1.28 | 42.67±1.88 |
| Abdominal Circumference (cm) | ||
| Mean (SD) | 43.78±4.16 | 47.66±2.80 |
| Age of Onset of Sitting (months) | ||
| Mean (SD) | 5.10±26.42 | 5.12±28.25 |
Linear Parameters
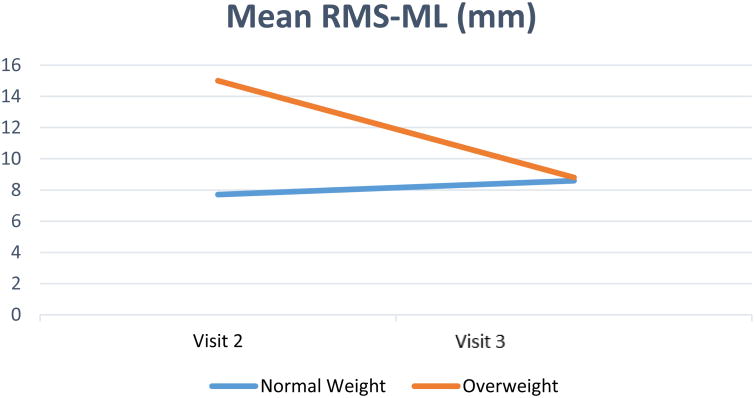
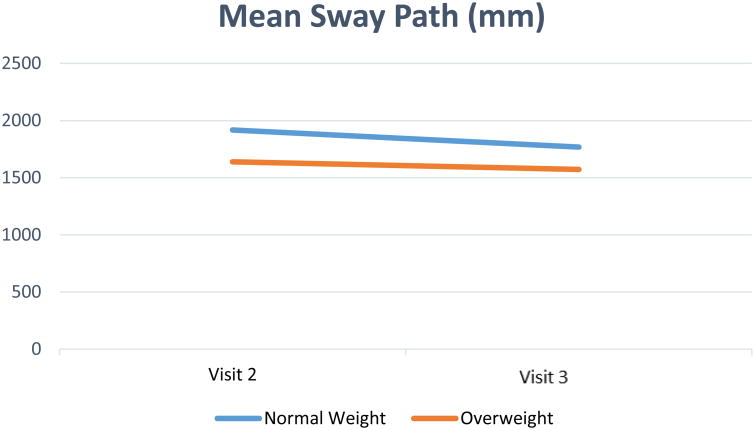
While there were no significant main effects for Group for RMS in AP, Range in AP and ML direction, as well as no significant interaction effects for all linear variables examined (see Table 2), there was a significant main effect of Group (F(1,21)=4.41, p=.048, η2=0.17) for RMS in ML direction and for Sway Path (F(1, 21)=5.428, p=.03, η2=0.20). Specifically, overweight infants presented greater RMS values in ML direction while their sway path trajectory was smaller in both visits in comparison to normal weight infants.
Table 2.
Dependent Variables.
| Normal Weight Infants | Overweight Infants | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Dependent Variable | Visit 2 | Visit 3 | Visit 2 | Visit 3 | ||||||||
| Mean | SD | Range | Mean | SD | Range | Mean | SD | Range | Mean | SD | Range | |
| RMS ML (mm) | 7.7 | 3.2 | 2.6-12.7 | 8.6 | 4.2 | 3.5-15.9 | 15 | 10.4 | 7.2-40.5 | 8.8 | 4.9 | 3.8-18.3 |
| RMS AP (mm) | 9.9 | 5.1 | 2.5-20.9 | 12 | 10 | 5.1-46.7 | 10.3 | 5.6 | 1.4-20.6 | 11.1 | 8.2 | 3.3-33.2 |
| Range AP (mm) | 48 | 21 | 14.1-89.5 | 53.7 | 31.8 | 21.5-135.1 | 53.2 | 18.5 | 29.4-82.9 | 54.1 | 30.6 | 22.3-123.6 |
| Range ML (mm) | 39.3 | 15.1 | 14.2-64.2 | 43 | 19.7 | 17.2-78.2 | 56.3 | 20.8 | 30.7-90.9 | 43 | 36.4 | 21.6-75.6 |
| Sway Path (mm) | 1917.6 | 383.2 | 1388.4-2523.5 | 1767.5 | 262.1 | 1415.6-2246.0 | 1638.5 | 195.3 | 1352.3-1959.8 | 1572.9 | 226.5 | 1248.9-2031.3 |
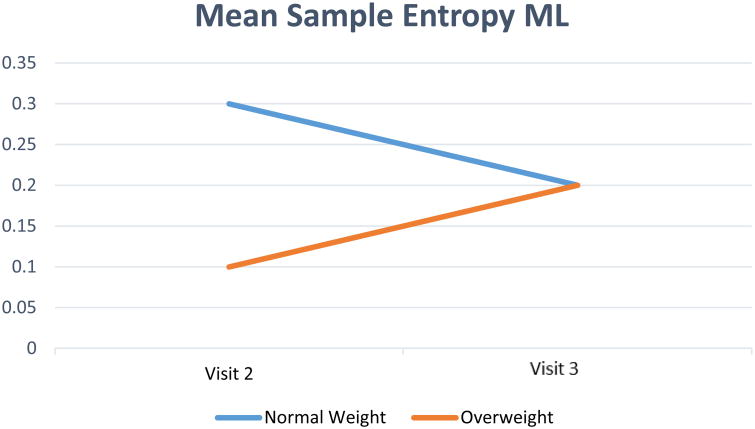
| Sample Entropy ML | 0.3 | 0.17 | .1 -.6 | 0.2 | 0.1 | .1-.4 | 0.1 | 0.4 | .1-.2 | 0.2 | 0.1 | .06-.4 |
| Sample Entropy AP | 0.3 | 0.18 | .1 -.7 | 0.3 | 0.2 | .02-.9 | 0.3 | 0.4 | .06-1.3 | 0.2 | 0.2 | .04-.7 |
Nonlinear Parameters
Regarding nonlinear parameters, there was a main effect of Group (F(1,21)=5.49, p=.029, η2=0.20) for SampEn in the ML direction but not in the AP direction, and a significant interaction effect (F(1,21)=4.651, p=0.043, η2=0.18). Specifically, overweight infants increased SampEn in ML direction values from visit 2 to visit 3 while normal weight infants decreased SampEn values from visit 2 to visit 3.
Discussion
The goal of the present study was to determine whether normal weight and overweight infants present dissimilar postural control strategies during the development of sitting. Sitting posture is an important milestone since it is the first vertical position that a child can achieve to explore their surroundings and promote the development of parallel skills, such as cognitive, language and social competencies [26-28]. We hypothesized that overweight infants would achieve the motor skill milestone of sitting at the same time or later than normal weight infants and present increased postural sway in comparison to the normal weight infants. Our findings partly verified our hypotheses. Specifically, both groups of infants started to sit around the same age; however, overweight infants adopted a reduced postural sway but an overly flexible strategy for controlling their sitting posture in comparison to the normal weight infants, especially at the onset of sitting.
The linear analysis revealed that even though overweight infants presented smaller excursions of the COP path in both visits, at the same time, they moved more in the ML direction (RMS in ML) at the onset of sitting in comparison to normal weight infants (Figure 1). The complimentary nonlinear analysis suggested that this persistence in moving mostly in the ML direction at the onset of sitting, is characterized by a more sinusoidal and periodic behavior of the trajectory of the COP, which reaches the values of the normal weight infants by visit 3. Differences between groups in the RMS and SampEn in the ML direction were mostly different by the changes at the onset of sitting, while the reduced postural sway path values were persistent in both visits for the overweight infants (Figure 2, 3). Some postural control differences between overweight and normal weight infants dissipate, others persist. It is evident that overweight infants exhibit different postural control strategies than normal weight infants as they acquire the sitting skill. Overweight infants are rather rigid and repetitive (SampEn ML) at the onset of sitting to control the additional weight and allow only ML movement (RMS ML). As they become more experienced they are able to adapt to the weight constraint and perform similarly as normal weight infants, even though they still prefer to overall move less (Sway Path) possibly to avoid falling over. More research is needed to determine if these variances result in other developmental differences.
Fig. 1.
Mean RMS-ML
Fig. 2.
Sway Path
Fig 3.
Sample Entropy ML
The present findings are not in agreement with other studies that examined postural control differences between normal and overweight children. Specifically, these studies suggested that overweight children exhibit greater sway path values during standing than normal weight children [29,30], while the overweight infants in the present study employed a reduced postural sway strategy during sitting in comparison to the normal weight infants. However, it should be noted that we examined a different postural control skill (sitting) and a much younger cohort of children (infants). The results of the present study can also be compared with others that examined infant sitting postural control. For example, Deffeyes and colleagues found that developmentally delayed infants presented less complex patterns in the ML direction similar to our overweight infants at the onset of sitting [12,31], which could be an indication of the overall gross motor delay that other studies have observed [8,9]. Moreover, Kyvelidou and colleagues [32] showed that infants with greater weight presented decreased upper body coordination during sitting development in the ML direction, which may be indicative of the rigidity and reduced complexity that overweight infants exhibit at the onset of sitting. It is possible that the additional weight, forces the infants to choose different strategies to maintain the sitting posture. The question that arises is whether these initial changes in sitting posture affect the development of other skills and domains such as cognition, play and physical activity behaviors.
Limitations
Our study as many is characterized by some limitations. Our effect sizes were moderate (eta square between 0.17-0.2); an increase in the sample size, particularly data on overweight infants, could result in greater effect sizes. Additionally, as caregivers were asked to contact research personnel at the onset of their infant's sitting (e.g., sit independently for 10 seconds), this was subjective to the caregiver's judgment and may have influenced the findings. However, there were no significant differences between the onset of sitting between normal weight and overweight infants. Further, weight-for-length may not be the best method for determining risk for differing postural control strategies as weight distribution may be an even more important indicator. More research could examine the influence of skinfold thickness at different regions of the body and the development of sitting postural control. Finally, due to infant temperament six infants were not included in the study and inclusion of all infants may altered the findings.
Conclusions
An infant's ability to achieve motor milestones allows the opportunity for greater exploration of their surroundings and improved motor and cognitive development. This study demonstrated overweight infants employ a different postural strategy including differences in RMS, sway path, and SampEn at the onset of sitting. However, the only difference that remained one-month post sitting onset was a reduced sway path. More research is needed to understand if and how these differences in postural strategies impact how infants explore their environments and if there are longitudinal impacts on behaviors as the infant continues to develop and grow. By having a better understanding of this relationship it can be determined if overweight infants are at risk of developmental delays and in need of intervention.
Highlights.
Normal weight and overweight infants learned to sit at similar ages.
Postural control strategies differed between the two groups at sitting onset.
Normal weight infants had greater postural sway at one-month post onset of sitting.
Acknowledgments
We would like to thank the students and technicians for their assistance in data collection. Additionally, we would like to thank the caregivers and their infants for participating in the study.
This work was supported by the National Institutes of Health Centers of Biomedical Research Excellence (1P20GM109090-01). Study sponsors had no involvement in the design, analysis, or reporting of this study.
Footnotes
Conflict of interest statement: No conflicts of interest.
Ethical board review statement: The study was approved by an Institutional Review Board.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.World Health Organization, Child overweight and obesity. 2016 http://www.who.int/dietphysicalactivity/childhood/en/
- 2.Taveras EM, Rifas-Shiman SL, Belfort MB, Kleinman KP, Oken E, Gillman MW. Weight status in the first 6 months of life and obesity at 3 years of age. Pediatrics. 2009;123:1177–1183. doi: 10.1542/peds.2008-1149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Reilly JJ, Methven E, McDowell ZC, Hacking B, Alexander D, Stewart L, Kelnar C. Health consequences of obesity. Arch Dis Child. 2003;88:748–752. doi: 10.1136/adc.88.9.748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.National Heart, Lung, and Blood Institute. What Are the Health Risks of Overweight and Obesity? 2012 https://www.nhlbi.nih.gov/health/health-topics/topics/obe/risks.
- 5.Slining M, Adair LS, Goldman BD, Borja JB, Bentley M. Infant overweight is associated with delayed motor development. J Ped. 2010;157:20–25. doi: 10.1016/j.jpeds.2009.12.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wearing SC, Hennig EM, Byrne NM, Steele JR, Hills AP. The impact of childhood obesity on musculoskeletal form. Obesity Rev. 2006;7:209–218. doi: 10.1111/j.1467-789X.2006.00216.x. [DOI] [PubMed] [Google Scholar]
- 7.McGraw B, McClenaghan BA, Williams HG, Dickerson J, Ward DS. Gait and postural stability in obese and nonobese prepubertal boys. Arch Phys Med Rehab. 2000;81:484–489. doi: 10.1053/mr.2000.3782. [DOI] [PubMed] [Google Scholar]
- 8.Mond JM, Stich H, Hay PJ, Krmer A, Baune BT. Associations between obesity and developmental functioning in pre-school children: A population-based study. Int J Obes. 2007;31:1068–1073. doi: 10.1038/sj.ijo.0803644. [DOI] [PubMed] [Google Scholar]
- 9.Okely AD, Booth ML, Chey T. Relationships between body composition and fundamental movement skills among children and adolescents. Res Quar Ex Sport. 2004;75:238–247. doi: 10.1080/02701367.2004.10609157. [DOI] [PubMed] [Google Scholar]
- 10.Jaffe M, Kosakov C. The motor development of fat babies. Clin Pediatrics. 1982;21:619–621. doi: 10.1177/000992288202101011. [DOI] [PubMed] [Google Scholar]
- 11.Onis M. Relationship between physical growth and motor development in the WHO child growth standards. Acta Paediatrica. 2006;95:96–101. doi: 10.1111/j.1651-2227.2006.tb02380.x. [DOI] [PubMed] [Google Scholar]
- 12.Deffeyes JE, Harbourne RT, Kyvelidou A, Stuberg WA, Stergiou N. Nonlinear analysis of sitting postural sway indicates developmental delay in infants. Clinical Biomechanics. 2009;24:564–570. doi: 10.1016/j.clinbiomech.2009.05.004. [DOI] [PubMed] [Google Scholar]
- 13.Ryalls BO, Harbourne R, Kelly-Vance L, Wickstrom J, Stergiou N, Kyvelidou A. A perceptual motor intervention improves play behavior in children with moderate to severe cerebral palsy. Front Psych. 2016;7:643. doi: 10.3389/fpsyg.2016.00643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Neelon SEB, Oken E, Taveras EM, Rifas-Shiman SL, Gillman MW. Age of achievement of gross motor milestones in infancy and adiposity at age 3 years. Mat Child Health. 2012;16:1015–1020. doi: 10.1007/s10995-011-0828-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stodden DF, Goodway JD, Langendorfer SJ, Roberton MA, Rudisill ME, Garcia C, Garcia LE. A developmental perspective on the role of motor skill competence in physical activity: An emergent relationship. Quest. 2008;60:290–306. [Google Scholar]
- 16.Murray GK, Veijola J, Moilanen K, Miettunen J, Glahn DC, Cannon TD, Isohanni M. Infant motor development is associated with adult cognitive categorisation in a longitudinal birth cohort study. J Child Psychology Psychiatry. 2006;47:25–29. doi: 10.1111/j.1469-7610.2005.01450.x. [DOI] [PubMed] [Google Scholar]
- 17.Piek JP, Dawson L, Smith LM, Gasson N. The role of early fine and gross motor development on later motor and cognitive ability. Hum Mov Sci. 2008;27:668–681. doi: 10.1016/j.humov.2007.11.002. [DOI] [PubMed] [Google Scholar]
- 18.Murray GK, Jones PB, Kuh D, Richards M. Infant developmental milestones and subsequent cognitive function. Ann Neuro. 2007;62:128–136. doi: 10.1002/ana.21120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ulrich DA, Hauck JL. Programming physical activity in young infants at-risk for early onset of obesity. Kines Rev. 2013;2:221–232. [Google Scholar]
- 20.Kyvelidou A, Harbourne RT, Shostrom VK, Stergiou N. Reliability of center of pressure measures for assessing the development of sitting postural control in infants with or at risk of cerebral palsy. Arch Phys Med Rehab. 2010;91:1593–1601. doi: 10.1016/j.apmr.2010.06.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Stergiou N, Buzzi UH, Kurz MJ, Heidel J. Nonlinear tools in human movement: Innovative analysis of human movement analytical tools for human movement research. Human Kinetics. 2004:63–90. [Google Scholar]
- 22.Harbourne RT, Deffeyes JE, Kyvelidou A, Stergiou N. Complexity of postural control in infants: linear and nonlinear features revealed by principal component analysis, Nonlinear Dynamics. Psych Life Sci. 2010;13:123–144. [PubMed] [Google Scholar]
- 23.Harbourne RT, Willett S, Kyvelidou A, Deffeyes J, Stergiou N. A comparison of interventions for children with cerebral palsy to improve sitting postural control: a clinical trial. Phys Ther. 2010;90:1881–1898. doi: 10.2522/ptj.2010132. [DOI] [PubMed] [Google Scholar]
- 24.Prieto TE, Myklebust JB, Hoffman RG, Lovett EG, Myklebust BM. Measures of postural steadiness: Differences between healthy young and elderly adults. IEEE Trans Biomed Eng. 1996;43:956–66. doi: 10.1109/10.532130. [DOI] [PubMed] [Google Scholar]
- 25.Richman JS, Moorman JR. Physiological time-series analysis using approximate entropy and sample entropy. Am J Physiol Heart Circ Physiol. 2000;278:H2039–49. doi: 10.1152/ajpheart.2000.278.6.H2039. [DOI] [PubMed] [Google Scholar]
- 26.Bornstein MH, Hahn CS, Suwalsky JT. Physically developed and exploratory young infants contribute to their own long-term academic achievement. Psych Sci. 2013:1–12. doi: 10.1177/0956797613479974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.LeBarton ES, Iverson JM. Fine motor skill predicts expressive language in infant siblings of children with autism. Dev Sci. 2013;16:815–827. doi: 10.1111/desc.12069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Libertus K, Violi DA. Sit to Talk: Relation between motor Skills and language development in infancy. Fron Psych. 2016;7:1–8. doi: 10.3389/fpsyg.2016.00475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Boucher F, Handrigan GA, Mackrous I, Hue O. Childhood obesity affects postural control and aiming performance during an upper limb movement. Gait Posture. 2015;42:116–121. doi: 10.1016/j.gaitpost.2015.04.016. [DOI] [PubMed] [Google Scholar]
- 30.D'Hondt E, Deforche B, De Bourdeaudhuij I, Gentier I, Tanghe A, Shultz S, Lenoir M. Postural balance under normal and altered sensory conditions in normal-weight and overweight children. Clin Biomech. 2011;26:84–89. doi: 10.1016/j.clinbiomech.2010.08.007. [DOI] [PubMed] [Google Scholar]
- 31.Deffeyes JE, Harbourne RT, DeJong SL, Kyvelidou A, Stuberg WA, Stergiou N. Use of information entropy measures of sitting postural sway to quantify developmental delay in infants. J Neuroengineering Rehab. 2009;6:34. doi: 10.1186/1743-0003-6-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kyvelidou, Stuberg WA, Harbourne RT, Deffeyes JE, Blanke D, Stergiou N. Development of upper body coordination during sitting in typically developing infants. Ped Res. 2009;65:553–558. doi: 10.1203/PDR.0b013e31819d9051. [DOI] [PMC free article] [PubMed] [Google Scholar]