Abstract
Opt-out HIV testing is recommended for correctional settings but may occur without inmates’ knowledge or against their wishes. Through surveying inmates receiving opt-out testing in a large prison system, we estimated the proportion unaware of being tested or not wanting a test, and associations (prevalence ratios [PRs]) with inmate characteristics. Of 871 tested, 11.8% were unknowingly tested and 10.8% had unwanted tests. Not attending an educational HIV course (PR=2.34, 95% CI 1.47–3.74), lower HIV knowledge (PR=0.95, 95% CI 0.91–0.98), and thinking testing is not mandatory (PR=9.84, 95% CI 4.93–19.67) were associated with unawareness of testing. No prior incarcerations (PR=1.59, 95% CI 1.03–2.46) and not using crack/cocaine recently (PR=2.37, 95% CI 1.21–4.64) were associated with unwanted testing. Residence at specific facilities was associated with both outcomes. Increased assessment of inmate understanding and enhanced implementation are needed to ensure inmates receive full benefits of opt-out testing: being informed and tested according to their wishes.
Keywords: HIV testing, opt-out testing, informed consent, prison, prisoners
INTRODUCTION
Incarcerated individuals are disproportionately infected with HIV, with an estimated 1 in 7 HIV-infected persons passing through the criminal justice system annually (1). Due to the high prevalence of HIV among incarcerated individuals, jails and prisons have been identified as important venues for HIV screening and treatment (2–5). An additional benefit of widespread screening of the general inmate population is that it often identifies those who do not perceive themselves to be at high risk for HIV or identify as engaging in high risk behaviors, such as having sex with a partner at risk or using non-injection drugs during sex (5). Accordingly, several states have implemented mandatory HIV testing policies. A report from the U.S. Bureau of Justice Statistics found that in 2008, 24 states tested all inmates for HIV infection at some point during their incarceration (6). However, mandatory HIV testing of inmates can be viewed as unethical when it requires testing of individuals who may wish to remain untested. Particularly in correctional settings, some individuals may be concerned about consequences of testing positive such as loss of privacy, stigmatization, and segregation (3, 7). Furthermore, mandatory testing can be viewed as compromising an individual’s autonomy and freedom to choose whether or not to be tested for HIV, which some contend should not be lost when incarcerated (8, 9).
Opt-out testing policies have been promoted as effective alternatives to mandatory testing as a means of reaching the greatest number of inmates while preserving their right to refuse the test (2, 10), and have been recommended by the Centers for Disease Control (CDC) as a component of the standard prison medical evaluation (11). A 2012 survey of all state departments of correction found that 17 reported mandatory testing; 11 provided opt-out testing; and 10 had opt-in testing, with the remaining states either not reporting, not testing, or using some other practice for testing (12). However, the ethical provision of HIV testing in correctional settings may be met with challenges even with the use of opt-out policies. For example, Seal and colleagues provide a strong ethical argument that institutional factors inherent to the criminal justice system, such as a hierarchical chain of command, may result in individuals feeling coerced to get tested for HIV even when it is technically voluntary (3, 13). Furthermore, the situational pressure of being overwhelmed and having other inmates standing in close proximity during processing can diminish prisoners’ sense of autonomy in deciding to be tested or not, even in opt-out settings (14).
Our research team recently conducted a study examining inmate awareness of HIV testing in the North Carolina (NC) prison system, which offers opt-out HIV testing, and found that although 95% of 936 prisoners surveyed were tested for HIV, not all inmates fully understood that the HIV testing was optional or knew that they had been tested (15). Over half of surveyed NC prison inmates incorrectly perceived that testing was mandatory. Moreover, 15% had been tested despite not wanting to be tested, and 16% were not able to report correctly whether they had been tested (15). This confusion could be due in part to the unclear language of the consent form, which combined voluntary HIV testing verbiage with mandatory tuberculosis and syphilis testing procedures (15). These findings suggest that potential problems may exist in the implementation of opt-out HIV testing in correctional settings.
As there has been little research investigating potential gaps in opt-out policy implementation, particularly among incarcerated persons, we conducted an exploratory study among those prison entrants who we had previously identified to have suboptimal and variable awareness of testing procedures. Specifically, we sought to identify factors associated with prisoners: 1) being unaware of having been tested; and 2) not wanting to be tested. We conclude with a discussion of the implications of our findings for opt-out testing in correctional settings.
METHODS
Study Setting and Population
To examine prison inmates’ understanding of prison testing policy, between April 2010 and March 2011 we surveyed inmates undergoing processing and medical screening at the NC state prison system’s seven intake centers that predominantly house adults. Medical screening included the opportunity to be tested for HIV. We approached inmates shortly after their entry into prison and initiation of medical screening, which included the opportunity to test for HIV. The HIV opt-out testing policy in place at the time included the reading aloud a statement of general consent by an intake prison nurse and the opportunity for the inmate to sign a general consent form. At three facilities, inmates also attended an HIV education class, but sometimes this did not occur until after they had been offered HIV testing. Further details about the HIV screening process are reported elsewhere (15).
Potential study participants were randomly selected from a roster of inmates at each of the seven adult intake prisons. The distribution of intake prisons among the study population was designed to reflect the distribution among all inmates admitted to the prison system (15). Inmates were eligible for inclusion in the study if they were: 1) age 18 years or older; 2) English-speaking; 3) not housed in solitary confinement or disciplinary segregation; 4) completed all prison health processing activities; 5) recruited within two weeks after having been offered the opportunity to test for HIV; and 6) able to provide informed consent to participate. The study protocol was approved by the North Carolina Department of Public Safety, the Institutional Review Board of the University of North Carolina at Chapel Hill, and the Office for Human Research Protection at the U.S. Department of Health and Human Services.
After inmates provided informed consent, they completed the study survey in a private room at the prison. To minimize social desirability bias in inmates’ responses, we administered the surveys using audio computer-assisted self-interviews (ACASI) with touch screen computers, whereby inmates could navigate the survey on their own unless they required assistance by a research assistant. The survey contained questions about demographics, incarceration and HIV testing history, substance use, mental health, sexual risk behaviors, attendance at the HIV course, levels of HIV knowledge and stigma, and experiences with and perceptions of HIV testing in the prison.
We assessed inmates’ desire to be tested by asking “During processing, did you want to have an HIV test?”, and their perception of being tested by querying “Since you’ve been at this processing center, have you been tested for HIV?”; inmates could answer “yes” or “no” to each question. We coded our study outcomes by linking these variables via a unique identification number with electronic laboratory records indicating whether inmates had actually been tested for HIV by the prison during processing. This linkage allowed us to examine the concordance between inmate testing (tested or not) with their perception of being tested and desire to be tested. As described below, these measures of concordance were the basis for our two primary outcomes. All identifiers were removed before analysis.
Analysis of survey data
In the current study, we excluded inmates who reported an HIV-diagnosis prior to their incarceration (n=11) and focused our analyses on inmates who had received an HIV test, due to the small proportion of inmates who were not tested (5.4%, n=50). Among this population, we estimated the percentage (and 95% Confidence Interval [95%CI]) of survey respondents endorsing each survey item. We then assessed factors associated with discordance in: 1) an inmate’s stated wishes (i.e., wanted to be tested or not) and 2) inmate’s awareness of being tested for HIV (i.e., thought he/she was tested or not).
To assess factors associated with discordance between receiving an HIV test and awareness of being tested/desire for a test, we estimated the proportion of respondents tested for HIV who were unaware of being tested and the proportion who did not want to be tested, for each independent variable of a priori interest. These variables included the following: 1) demographics, including race/ethnicity, age, gender, sexual identity, and education; 2) history of incarceration, including whether they were ever incarcerated and the total length of time they had spent in prison or jail; 3) history of HIV testing prior to this incarceration; 4) substance use, including binge alcohol use and use of other substances in the three months prior to incarceration including marijuana, crack and/or powder cocaine, methamphetamines, and heroin; 5) prior sexually transmitted infection (STI) diagnosis; 6) history of depression and/or anxiety, based on analyses of national data showing that depressive symptoms were associated with discrepancies between planned and actual HIV testing (16); 7) sexual risk behaviors, including having unprotected vaginal or anal intercourse, trading sex, and/or having multiple partners in the three months prior to incarceration; 8) attendance at an educational HIV course during their current incarceration; 9) level of HIV knowledge, calculated as a sum score of 21 true-false items adapted from the Brief HIV Knowledge Questionnaire (17); 10) level of perceived HIV stigma, including their level of cognitive distancing, a process whereby individuals consider themselves fundamentally different from those with HIV (18) (score of four scale items), and also their support for mandatory disclosure of an inmate’s HIV status to correctional officers and to other inmates (each indicated on a four-point scale ranging from “agree a lot” to “disagree a lot”) (19); and 11) whether they perceived the prison had a mandatory HIV testing policy.
We estimated bivariate associations between the independent variables and each outcome. (In ancillary analyses, we examined the statistical power for each of our bivariate contrasts). We then separately analyzed variables with a statistically significant bivariate association (p<0.05) for each outcome using a multivariate model to estimate their association while controlling for other covariates in the model. For the outcome of being unaware of being tested, we coded our outcome variables so that the prevalence ratio (PR) estimates greater than 1 represented an increase in the relative probability of thinking of oneself as not tested; similarly, for unwanted testing we coded our outcome so that PR estimates greater than 1 represented an increase in the relative probability of receiving an unwanted test.
In estimating PRs, we observed several variables for which the subgroup traditionally considered to be the “unexposed” (e.g., non-drug users), and thus designated as the referent, was more likely to experience our main outcomes than traditional “exposed” (e.g., drug users) groups. (We note that this phenomenon occurs regardless of whether the outcome level of interest is framed positively or negatively (e.g., framed as aware of testing or unaware of testing). In response, we selected reference groups, regardless of traditional “exposure” status, to ensure that PR estimates were available for those subgroups most likely to experience the outcome.
To avoid problems with model convergence that may arise with binomial regression, we used the modified Poisson approach with robust standard errors to estimate PRs and corresponding 95% CIs for our dichotomous outcomes (20). All analyses were conducted using SAS version 9.2 (Cary, North Carolina).
RESULTS
Description of Study Sample
Approximately 24,500 inmates were admitted to the NC prison system during the study period. Of 1,785 approached to participate in the study, 56% (1,000/1,785) consented to participate, 921/1,000 had non-missing data for both of our main outcomes and reported not testing HIV-positive before this incarceration, and 871/921 (95%) were tested for HIV. Participants were demographically similar to the general prison population, as described elsewhere (15).
Of the participants tested for HIV, most were male (86.6%) and self-identified as black (46.8%) or white (43.1%). Nearly 25% were 18–24 years of age, 51% were aged 25–40, and 25% were aged 41–64. The vast majority of respondents had been previously incarcerated (83.1%) and 45% had previously spent at least 1 year in prison (Table 1). Most inmates had been previously tested for HIV at some point in their lives (81.5%). More than half (63.8%) received the informational HIV education course prior to the time of the survey.
Table 1.
Characteristics of study participants receiving an HIV test in the NC prison system, 2010–2011 (n=871)
| %a | Lower 95% CI | Upper 95% CI | |
|---|---|---|---|
|
| |||
| Race/ethnicity | |||
| White | 43.1 | 39.8 | 46.3 |
| Black | 46.8 | 43.5 | 50.2 |
| Other | 10.1 | 8.1 | 12.1 |
|
| |||
| Age | |||
| 18–24b | 23.8 | 21.0 | 26.7 |
| 25–31 | 25.2 | 22.3 | 28.2 |
| 32–40 | 25.7 | 22.8 | 28.6 |
| 41–64 | 25.2 | 22.3 | 28.2 |
|
| |||
| Gender | |||
| Female | 13.4 | 11.2 | 15.7 |
| Male | 86.6 | 84.3 | 88.8 |
|
| |||
| Sexual identity | |||
| Men who have sex with women | 85.8 | 83.3 | 88.2 |
| Men who have sex with men | 0.9 | 0.2 | 1.6 |
| Men who have sex with men and women | 0.6 | 0.1 | 1.2 |
| Women who have sex with men | 11.0 | 11.0 | 13.2 |
| Women who have sex with women | 0.4 | 0.0 | 0.8 |
| Women who have sex with men and womenc | 1.3 | 0.5 | 2.1 |
|
| |||
| Education | |||
| <High school | 37.8 | 34.6 | 41.1 |
| High school or GED | 38.3 | 35.0 | 41.6 |
| >High schoolb | 23.9 | 21.0 | 26.7 |
|
| |||
| Prison facilityd | |||
| F1 | 4.9 | 3.5 | 6.4 |
| F2 | 8.5 | 6.6 | 10.3 |
| M1 | 5.9 | 4.3 | 7.4 |
| M2 | 22.8 | 20.1 | 25.6 |
| M3 | 28.2 | 25.3 | 31.2 |
| M4 | 20.2 | 17.5 | 22.9 |
| M5 | 9.4 | 7.5 | 11.4 |
|
| |||
| Previously incarceratedb | 83.1 | 80.6 | 85.6 |
|
| |||
| Time ever in prisone | |||
| <1 year | 55.3 | 51.7 | 59.0 |
| ≥1 year | 44.7 | 41.0 | 48.3 |
|
| |||
| Ever received an HIV test prior to incarcerationb | 81.5 | 78.9 | 84.1 |
|
| |||
| Binge alcohol usef | |||
| Every day | 13.0 | 10.7 | 15.2 |
| 2–6 times per week | 23.6 | 20.8 | 26.4 |
| <2–6 times per weekb | 63.4 | 60.2 | 66.6 |
|
| |||
| Substance usef | |||
| Marijuanab | 57.1 | 53.8 | 60.5 |
| Crack or cocaine | 27.8 | 24.8 | 30.8 |
| Methamphetamineb | 6.9 | 5.2 | 8.6 |
| Heroinb | 6.1 | 4.5 | 7.7 |
|
| |||
| Past STI diagnosis | 18.7 | 16.1 | 21.3 |
|
| |||
| Mental illness | |||
| Depression | 26.9 | 24.0 | 29.9 |
| Anxietyb | 24.1 | 21.3 | 27.0 |
|
| |||
| Sexual riskf | |||
| Unprotected vaginal or anal intercourseg | 71.1 | 67.9 | 74.3 |
| Received sex in exchange for money, drugs, food, or shelterb | 7.7 | 5.9 | 9.5 |
| Gave sex in exchange for money, drugs, food, or shelterb | 7.9 | 6.1 | 9.7 |
| Had multiple sexual partnersb | 35.4 | 32.2 | 38.6 |
|
| |||
| Thought HIV testing in the prison was mandatory | 55.5 | 52.2 | 58.8 |
|
| |||
| Attended the HIV course | 63.8 | 60.6 | 67.0 |
| Mean score | Lower | Upper | |
| 95% CI | 95% CI | ||
|
| |||
| HIV knowledgeh | 16.9 | 16.6 | 17.2 |
|
| |||
| Cognitive distancingi | 6.81 | 6.55 | 7.08 |
|
| |||
| Support for mandatory disclosure to correctional officersj | 1.77 | 1.69 | 1.85 |
|
| |||
| Support for mandatory disclosure to inmatesj | 2.04 | 1.96 | 2.11 |
% represents non-missing data
<3% missing
97 (11.1%) missing
Prison facilities are the NC state prison system’s seven intake centers that predominantly house adults; F1–F2 house female inmates, and M1–M5 house male inmates
157 (18%) missing
In the 3 months prior to this incarceration
92 (10.6%) missing
22-item HIV knowledge scale. Scores could range from 0–22, with higher scores indicating higher HIV knowledge (1).
5-item cognitive distancing scale. Scores could range from 0–15, with higher scores indicating higher cognitive distancing (2). 51 (5.8%) missing.
4-point support for mandatory disclosure scale. Scores could range from 0–3, with higher scores indicating stronger agreement.
HIV Testing Awareness and Desirability
More than half of participants (55.5%) inaccurately reported that HIV testing in prison was mandatory (“all inmates have to be tested for HIV—they do not have a choice”). Among the study population, which consisted of inmates tested for HIV upon entering prison, 103 (11.8%) perceived that they had not been tested, and 94 (10.8%) reported that they had not wanted an HIV test performed. Together, a total of 166 (19.1%) reported not wanting a test, thinking that they had not been tested, or both (see Figure 1).
Figure 1.
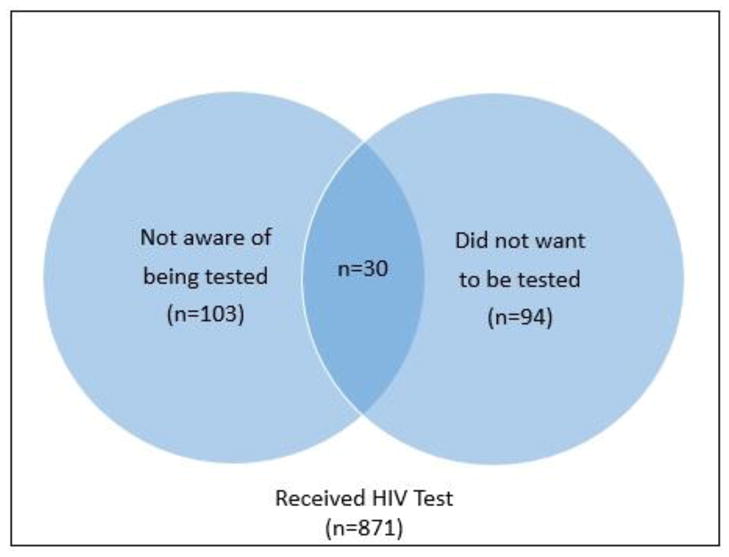
Number of NC prison inmates receiving an HIV test without being aware and/or against their wishes in an opt-out HIV testing setting, 2010–2011. Note: Diagram is not proportional. The groups in the blue circles comprise part of the 871 who received a test. 3 observations had missing data for the variable “wanted a test”.
Predictors of Being Unaware of Testing
In bivariate analyses, incorrectly reporting that one had not been HIV tested (i.e., inmate tested but believes he/she was not tested) was positively associated with being male, residing in prison facilities M1 and M5 (compared to F1), having no prior incarcerations, not attending the HIV course, thinking testing was not mandatory, and increasing cognitive distance score (Table 2). Incorrectly reporting that one had not been HIV tested was negatively associated with increasing HIV knowledge score and being aged 25–31 (compared to 18–24 years).
Table 2.
Bivariate and multivariate predictors of testing awareness among study participants tested for HIV in the NC prison system, 2010–2011
| Na | Thought they were not tested | ||||||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| n | % | PR | 95% CI | p-value | aPR | 95% CI | p-value | ||
|
| |||||||||
| Race/ethnicity | -- | -- | -- | ||||||
| White (ref) | 375 | 39 | 10.4 | 1 | -- | -- | |||
| Black | 408 | 53 | 13.0 | 1.25 | 0.85–1.84 | 0.2625 | |||
| Other | 88 | 11 | 12.5 | 1.20 | 0.64–2.25 | 0.5657 | |||
|
| |||||||||
| Age | |||||||||
| 18–24 (ref) | 203 | 27 | 13.3 | 1 | -- | -- | 1 | -- | -- |
| 25–31 | 215 | 12 | 5.6 | 0.42 | 0.22–0.81 | 0.0091 | 0.86 | 0.40–1.85 | 0.6993 |
| 32–40 | 219 | 21 | 9.6 | 0.72 | 0.42–1.23 | 0.2329 | 1.67 | 0.85–3.32 | 0.1388 |
| 41–64 | 215 | 42 | 19.5 | 1.47 | 0.94–2.29 | 0.0897 | 1.84 | 0.98–3.47 | 0.0596 |
|
| |||||||||
| Gender | |||||||||
| Female (ref) | 117 | 5 | 4.3 | 1 | -- | -- | -- | -- | -- |
| Male | 754 | 98 | 13.0 | 3.04 | 1.26–7.31 | 0.0130 | |||
|
| |||||||||
| Prison facilityb | |||||||||
| F1 (ref) | 43 | 2 | 4.7 | 1 | -- | -- | 1 | -- | -- |
| F2 | 74 | 3 | 4.1 | 0.87 | 0.15–5.01 | 0.8777 | 1.04 | 0.19–5.65 | 0.9630 |
| M1 | 51 | 22 | 43.1 | 9.27 | 2.31–37.22 | 0.0017 | 8.25 | 2.15–31.65 | 0.0021 |
| M2 | 199 | 25 | 12.6 | 2.70 | 0.66–10.98 | 0.1648 | 6.46 | 1.62–25.75 | 0.0081 |
| M3 | 246 | 22 | 8.9 | 1.92 | 0.47–7.88 | 0.3638 | 3.89 | 0.96–15.77 | 0.0572 |
| M4 | 176 | 8 | 4.5 | 0.98 | 0.22–4.44 | 0.9762 | 2.46 | 0.53–11.39 | 0.2512 |
| M5 | 82 | 21 | 25.6 | 5.51 | 1.35–22.39 | 0.0171 | 4.88 | 1.12–21.34 | 0.0351 |
|
| |||||||||
| Previously incarcerated | |||||||||
| Yes (ref) | 717 | 77 | 10.7 | 1 | -- | -- | 1 | -- | -- |
| No | 146 | 24 | 16.4 | 1.53 | 1.00–2.33 | 0.0482 | 1.19 | 0.84–1.70 | 0.3253 |
|
| |||||||||
| Ever received an HIV test prior to incarceration | -- | -- | -- | ||||||
| Yes (ref) | 703 | 79 | 11.2 | 1 | -- | -- | |||
| No | 160 | 22 | 13.8 | 1.22 | 0.79–1.90 | 0.3690 | |||
|
| |||||||||
| Recent marijuana use | -- | -- | -- | ||||||
| Yes (ref) | 488 | 51 | 10.5 | 1 | -- | -- | |||
| No | 366 | 48 | 13.1 | 1.25 | 0.87–1.82 | 0.2292 | |||
|
| |||||||||
| Recent crack or cocaine use | -- | -- | -- | ||||||
| Yes (ref) | 242 | 23 | 9.5 | 1 | -- | -- | |||
| No | 629 | 80 | 12.7 | 1.34 | 0.86–2.08 | 0.1937 | |||
|
| |||||||||
| Recent methamphetamine use | --c | --c | --c | -- | -- | -- | |||
| Yes (ref) | 59 | 0 | 0 | ||||||
| No | 795 | 99 | 12.5 | ||||||
|
| |||||||||
| Recent heroin use | |||||||||
| Yes (ref) | 52 | 4 | 7.7 | 1 | -- | -- | -- | -- | -- |
| No | 802 | 95 | 11.9 | 1.54 | 0.59–4.02 | 0.3782 | |||
|
| |||||||||
| Thought HIV testing in the prison was mandatory | |||||||||
| Yes (ref) | 483 | 10 | 2.1 | 1 | -- | -- | 1 | -- | -- |
| No | 388 | 93 | 24.0 | 11.58 | 6.11–21.92 | <0.0001 | 9.84 | 4.93–19.67 | <0.0001 |
|
| |||||||||
| Attended the HIV course | |||||||||
| Yes | 556 | 40 | 7.2 | 1 | -- | -- | 1 | -- | -- |
| No | 315 | 63 | 20.0 | 2.78 | 1.92–4.03 | <0.0001 | 2.34 | 1.47–3.74 | 0.0004 |
|
| |||||||||
| HIV knowledge (mean, SD) | 16.9 (4.1) | 15.1 (4.8) | -- | 0.92 | 0.89–0.95 | 0.1996 | 0.95 | 0.91–0.98 | .0036 |
|
| |||||||||
| Cognitive distancing | 6.8 (3.9) | 8.1 (4.0) | -- | 1.08 | 1.04–1.14 | 0.0006 | 1.04 | 0.99–1.08 | 0.1006 |
N corresponds to percentages and unadjusted PR
Prison facilities are the NC state prison system’s seven intake centers that predominantly house adults; F1–F2 house female inmates, and M1–M5 house male inmates
Estimate not computed because of cell with zero observations
In the multivariable model, incorrectly reporting that one had not been HIV tested was associated with residing at prison facilities M1, M2, or M5 (M1: PR=8.25, 95% CI 2.15–31.65; M2: PR= 6.46, 95%CI: 1.62–25.75; M5: PR= 4.88, 95% CI: 1.12–21.34 compared to F1), not attending the HIV course (PR= 2.34, 95% CI: 1.47–3.74), perceiving testing as not being mandatory (PR=9.84, 95% CI 4.93–19.67), and lower HIV knowledge score (PR=0.95, 95%CI: 0.91–0.98) (Table 2).
Predictors of Unwanted Testing
In bivariate analyses, being tested without wanting an HIV test was associated with residing in prison facility M1 (compared to F1), having no prior incarcerations, reporting no use of marijuana or crack/powder cocaine, not attending the HIV course, thinking that HIV testing was not mandatory, having lower HIV knowledge, and having a higher HIV cognitive distancing score (Table 3).
Table 3.
Bivariate and multivariate predictors of testing desire among study participants tested for HIV in the NC prison system, 2010–2011
| Na | Did not want to be HIV tested | ||||||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| n | % | PR | 95% CI | p-value | aPR | 95% CI | p-value | ||
|
| |||||||||
| Race/ethnicity | -- | -- | -- | ||||||
| White (ref) | 375 | 36 | 9.6 | 1 | -- | -- | |||
| Black | 408 | 47 | 11.5 | 1.20 | 0.80–1.81 | 0.3845 | |||
| Other | 85 | 11 | 12.9 | 1.35 | 0.72–2.54 | 0.3550 | |||
|
| |||||||||
| Age | |||||||||
| 18–24 (ref) | 203 | 22 | 10.8 | 1 | -- | -- | 1 | -- | -- |
| 25–31 | 215 | 16 | 7.4 | 0.69 | 0.37–1.27 | 0.2309 | 0.61 | 0.29–1.28 | 0.1920 |
| 32–40 | 219 | 20 | 9.1 | 0.84 | 0.47–1.50 | 0.5594 | 0.94 | 0.47–1.90 | 0.8700 |
| 41–64 | 213 | 33 | 15.5 | 1.43 | 0.86–2.37 | 0.1648 | 1.23 | 0.64–2.37 | 0.5285 |
|
| |||||||||
| Gender | |||||||||
| Female (ref) | 117 | 11 | 9.4 | 1 | -- | -- | -- | -- | -- |
| Male | 751 | 83 | 11.1 | 1.18 | 0.65–2.14 | 0.5961 | |||
|
| |||||||||
| Prison facilityb | |||||||||
| F1 (ref) | 43 | 2 | 4.7 | 1 | -- | -- | 1 | -- | -- |
| F2 | 74 | 9 | 12.2 | 2.61 | 0.59–11.55 | 0.2047 | 3.24 | 0.75–14.00 | 0.1159 |
| M1 | 51 | 14 | 27.5 | 5.90 | 1.42–24.54 | 0.0146 | 4.78 | 1.14–20.11 | 0.0326 |
| M2 | 198 | 24 | 12.1 | 2.61 | 0.64–10.61 | 0.1813 | 3.95 | 0.89–17.57 | 0.0712 |
| M3 | 245 | 20 | 8.2 | 1.76 | 0.43–7.24 | 0.4365 | 2.56 | 0.59–11.02 | 0.2080 |
| M4 | 175 | 14 | 8.0 | 1.72 | 0.41–7.29 | 0.4615 | 3.02 | 0.65–14.07 | 0.1602 |
| M5 | 82 | 11 | 13.4 | 2.88 | 0.67–12.43 | 0.1553 | 1.95 | 0.41–9.26 | 0.4014 |
|
| |||||||||
| Previously incarcerated | |||||||||
| Yes (ref) | 715 | 67 | 9.4 | 1 | -- | -- | 1 | -- | -- |
| No | 146 | 26 | 17.8 | 1.90 | 1.25–2.88 | 0.0025 | 1.59 | 1.03–2.46 | 0.0367 |
|
| |||||||||
| Ever received an HIV test prior to incarceration | -- | -- | -- | ||||||
| Yes (ref) | 701 | 69 | 9.8 | 1 | -- | -- | |||
| No | 159 | 22 | 13.8 | 1.41 | 0.90–2.20 | 0.1362 | |||
|
| |||||||||
| Recent marijuana use | |||||||||
| Yes (ref) | 488 | 42 | 8.6 | 1 | -- | -- | 1 | -- | -- |
| No | 363 | 48 | 13.2 | 1.54 | 1.04–2.27 | 0.0314 | 1.25 | 0.79–1.97 | 0.3412 |
|
| |||||||||
| Recent crack or cocaine use | |||||||||
| Yes (ref) | 240 | 14 | 5.8 | 1 | -- | -- | 1 | -- | -- |
| No | 628 | 80 | 12.7 | 2.18 | 1.26–3.78 | 0.0052 | 2.37 | 1.21–4.64 | 0.0119 |
|
| |||||||||
| Recent methamphetamine use | -- | -- | -- | ||||||
| Yes (ref) | 59 | 2 | 3.4 | 1 | -- | -- | |||
| No | 792 | 88 | 11.1 | 3.28 | 0.83–12.98 | 0.0909 | |||
|
| |||||||||
| Recent heroin use | |||||||||
| Yes (ref) | 52 | 5 | 9.6 | 1 | -- | -- | -- | -- | -- |
| No | 799 | 85 | 10.6 | 1.11 | 0.47–2.61 | 0.8172 | |||
|
| |||||||||
| Thought HIV testing in the prison was mandatory | |||||||||
| Yes (ref) | 483 | 39 | 8.1 | 1 | -- | -- | 1 | -- | -- |
| No | 385 | 55 | 14.3 | 1.77 | 1.20–2.61 | 0.0039 | 1.44 | 0.96–2.16 | 0.0802 |
|
| |||||||||
| Attended the HIV course | |||||||||
| Yes | 554 | 47 | 8.5 | 1 | -- | -- | 1 | -- | -- |
| No | 314 | 47 | 15.0 | 1.76 | 1.21–2.58 | 0.0034 | 1.79 | 0.97–3.31 | 0.0639 |
|
| |||||||||
| HIV knowledge (mean, SD) | 16.9 (4.1) | 15.9 (4.4) | -- | 0.95 | 0.91–0.99 | 0.0084 | 0.99 | 0.95–1.04 | 0.7408 |
|
| |||||||||
| Cognitive distancing (mean, SD) | 6.8 (3.9) | 8.1 (3.8) | -- | 1.09 | 1.03–1.14 | 0.0008 | 1.05 | 1.00–1.10 | 0.0706 |
N corresponds to percentages and unadjusted PR
Prison facilities are the NC state prison system’s seven intake centers that predominantly house adults; F1–F2 house female inmates, and M1–M5 house male inmates
In the multivariable model, not wanting an HIV test was associated with residing at the M1 prison facility (PR=4.78, 95% CI 1.14–20.11, compared to F1), having no prior incarcerations (PR=1.59, 95% CI 1.03–2.46), and having not used crack or powder cocaine in the three months prior to incarceration (PR=2.37, 95% CI 1.21–4.64) (Table 3).
Analysis of statistical power. Given the observational nature of the study and the fixed sample size(s), we estimated statistical power for contrasts within each variable in our bivariate analyses (e.g. power to detect a difference in the proportion of Blacks and Whites who thought they had not been tested for HIV). We identified contrasts with a power of ≥80% (with a 2-sided test and alpha=0.05), as this is commonly used as a threshold for sufficient power. For the outcome “Thought not tested,” power was ≥ 80% for contrasts within the following variables: Gender, Thought testing was mandatory, Attended the HIV course, and Facility (contrasts between facilities M1 and M5 with F1, the referent). Comparisons of means for cognitive distance and HIV knowledge between those “thought tested” and “thought not tested” were also powered ≥ 80%. For the outcome “Did not want to be HIV tested,” contrasts with power ≥ 80% included facility M1 (compared to F1), Previous incarceration, History of Crack use, Thought testing was mandatory, and HIV course attendance; among continuous variables, the contrasts for cognitive distancing but not HIV knowledge was sufficiently powered.
DISCUSSION
HIV testing is integral to the seek-test-treat-retain model for control of the HIV epidemic. However, although HIV testing can afford considerable personal and public health benefit, it remains potentially sensitive given the stigmatization and discrimination known to occur among individuals identified to be infected with HIV (21), particularly in correctional settings. Opt-out testing policies have the potential to yield high rates of HIV testing while maintaining inmates’ right to refuse the test (4), although in practice, they have not always yielded higher rates of newly diagnosed HIV (22). The CDC’s 2006 recommendations for opt-out testing state that if the patient has given general consent for medical care, pre-test counseling and informed consent for the HIV test are not required; rather, the patient is notified that testing will be conducted unless the patient declines testing (11). However, depending on the implementation of opt-out policies, some inmates may still be at risk of being HIV tested against their wishes or without complete and informed awareness. The current research is an exploratory and novel study of risk factors for prison inmates being tested without their awareness or against their wishes in an opt-out setting.
In the broader study, which enrolled a representative sample of NC prison inmates undergoing opt-out testing, the vast majority (95%) received an HIV test, but roughly one-fifth of those receiving a test were unaware of having been tested and/or did not want a test (15). We sought in this study to examine which inmates were most vulnerable to receiving these two discordant testing outcomes. We found that inmates were more likely to be unaware that they had been tested if they resided at certain prison facilities (described below), had not attended the educational HIV course provided at some prison facilities, correctly perceived that testing was not mandatory, and had lower HIV knowledge scores. Those who were more likely to be tested without wanting a test resided at one specific prison facility, had never been incarcerated, and reported no recent pre-incarceration use of crack or powder cocaine.
Although inmates may refuse a test for any reason under opt-out testing, most inmates are tested for HIV (15, 23). The occurrence of undesired and unaware testing in our sample (n=166, 19%) and the high numbers of inmates incorrectly reporting that HIV testing was mandatory in prison (n=483, 55%) may suggest inadequate or unclear communication with inmates about their testing options (15). The scant past research that has examined patient understanding of opt-out HIV testing has found a wide range of understanding in an urban U.S. emergency department and in prenatal Sub-Saharan African settings (24–26). The current study is unique in examining potential factors associated with understanding of opt-out HIV testing policies. In light of these findings in other settings, the misperception that opt-out HIV testing is mandatory could be expected to be even more common in correctional settings where coercion and power imbalances are inherent (3, 27, 28). Furthermore, nurses in correctional settings may lack the training and time to educate inmates fully about opt-out testing during processing.
Our results suggest that inmates were more susceptible to being tested without their knowledge or receiving an unwanted test if they had less experience with and knowledge about testing in prison. Inmates who had been previously incarcerated were less likely to have a discordant testing outcome, suggesting that prior incarceration experience may have increased their understanding of their ability to decline the test; however, considering that North Carolina had opt-in testing prior to November, 2008, it is not likely that the majority of those inmates had directly experienced opt-out testing during their prior incarcerations. Rather, prior incarceration may have reduced their general confusion during the intake processing and improved their ability to understand opt-out testing when it was presented during medical consent, or those incarcerated prior to November 2008 may have believed testing was still opt-in.
Those who did not attend the HIV course were also at higher risk of being tested without their awareness, possibly due to missing important information about prison testing policy discussed in the course. Also, those who endorsed the incorrect statement that HIV testing at the prison was mandatory were much more likely to be aware of receiving an HIV test, likely due to believing that all inmates were tested without the option of refusing.
Environmental factors may also influence the likelihood that an inmate is unaware of being tested or tested against his/her wishes. Participants residing at one male prison facility (M1) were at highest likelihood of receiving both discordant outcomes, and those residing at two other male prison facilities (M2 and M5) were at increased risk of being unaware of having been tested. A number of facility-level characteristics, such as the practices and beliefs of individual staff members, staff and inmate norms and culture, and prison-specific policies and procedures, may explain the facility differences in undesired testing and unawareness of testing in our study results. For example, HIV testing is presented to women inmates as one of a series of reproductive health tests (including testing for pregnancy and other sexually transmitted infections), which may account for women’s increased awareness of being tested. Furthermore, availability of the educational HIV course can also affect awareness of being tested. At the time of this study, female prison processing facilities in North Carolina did not offer the course, meaning that female prisoners did not have that structured opportunity to learn about HIV testing policy and were more likely to perceive testing as mandatory (15). Curiously, although women were more likely to perceive the test as mandatory in our previous study (15), women were less likely than men to be tested against their wishes, possibly due to the higher likelihood of women to engage in health-promoting behaviors (29). Such differences may partially explain why the three facilities at increased risk for discordant outcomes were those housing male rather than female inmates.
Inmates who used crack or powder cocaine were significantly less likely to have an undesired HIV test. Many factors may account for this result. It is possible that inmates reporting crack or cocaine use are more likely to want an HIV test because they represent a more disadvantaged population and perceive HIV testing in prison as an important and accessible health care opportunity (30). Additionally, those with a history of crack and cocaine use may have engaged in more HIV risk behaviors and therefore felt that testing was more relevant for them (31). These theories are supported by the fact that in the full sample from our study (including both inmates who received and did not receive an HIV test), a significantly higher percentage of inmates who used crack or powder cocaine reported wanting an HIV test than among those who reported no use (94.4% vs. 87.1% respectively, p=0.0016).
Finally, we found that increased cognitive distancing—whereby individuals think of themselves as dissimilar from those with HIV (18)—was related to inmates’ low testing awareness and desire in the bivariate but not multivariable models. Cognitive distancing is a key component of stigma (18), which itself has been identified as an important limiting factor to uptake of opt-out testing among inmates in Baltimore jails (13) and was described as a barrier to seeking HIV testing among inmates in the southern U.S. (32). More research is needed to understand how stigma, and its components, influence prisoners’ perceived risk and sense of personal relevance of HIV.
This study has several limitations. Most importantly, due to the cross-sectional study design, the measures included in the survey instrument were not designed with the objective of determining causation, particularly with the complex outcomes we examined in this analysis. Participants may have been influenced by social desirability bias in their survey responses, although we believe that we minimized this effect by administering the surveys via ACASI, supported by the relatively frequent reporting of traditionally stigmatized behavior in this sample such as risky sex and substance abuse. Additionally, our study did not collect data on each inmate’s communication with prison staff during medical screening, which would have increased our understanding of factors leading to discordance in testing outcome. Although our study has a large overall sample, we found that some analyses were under-powered. Additionally, while our sample is representative of the NC prison population, our findings are limited in their generalizability to other correctional systems. Finally, due in part to its novelty, this study was not theoretically based or guided, but rather conducted for exploratory purposes to understand the phenomenon of disagreements in testing, testing awareness, and testing desire in opt-out prison settings. In spite of these limitations, this study makes a worthwhile contribution in its novel exploration of discordant testing outcomes in opt-out prison settings.
Prison systems with opt-out policies should consider enhancing their implementation so that all inmates are informed and tested in accordance with their wishes. Understanding which groups are vulnerable to having discordant testing outcomes under opt-out policies may assist prisons in targeting these efforts. Our study suggests that efforts to increase awareness of opt-out policies are needed and are particularly important to those residing at certain male prison facilities, and to those who have never been previously incarcerated or did not recently use substances. Communication about opt-out testing may be most effective when paired with messages to increase inmates’ sense of personal relevance or risk for HIV. The educational HIV course already offered at many prison facilities decreased inmates’ likelihood of being tested without their awareness, and should therefore be considered an important opportunity for enhanced communication of prison testing policies, particularly if inmates attend the course prior to being offered HIV testing. Future research efforts should seek to more broadly assess the associations demonstrated in this research with the ultimate goal of improving testing outcomes for vulnerable groups in opt-out settings.
Acknowledgments
We would like to thank Rebecca Ochtera for her thoughtful input into the analysis plan for this manuscript, and to Becky White, Jeanine May, Robert DeVellis, J. Michael Bowling, and members of the UNC Criminal Justice Working Group for their work on the parent study. This work would not have been possible without NC Department of Public Safety staff and study participants who generously gave their time and energy to the study. This research was funded by National Institute of Health (NIH) grant R01 MH079720-01A1 and supported by the University of North Carolina at Chapel Hill Center for AIDS Research (CFAR), an NIH funded program P30 AI50410.
References
- 1.Spaulding AC, Seals RM, Page MJ, Brzozowski AK, Rhodes W, Hammett TM. HIV/AIDS among inmates of and releasees from US correctional facilities, 2006: declining share of epidemic but persistent public health opportunity. PLoS One. 2009;4(11):e7558. doi: 10.1371/journal.pone.0007558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Westergaard RP, Spaulding AC, Flanigan T. HIV among persons incarcerated in the USA: a review of evolving concepts in testing, treatment, and linkage to community care. Curr Opin Infect Dis. 2013 Feb;26(1):10–6. doi: 10.1097/QCO.0b013e32835c1dd0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Seal DW, Eldridge GD, Zack B, Sosman J. HIV testing and treatment with correctional populations: people, not prisoners. J Health Care Poor Underserved. 2010 Aug;21(3):977–85. doi: 10.1353/hpu.0.0351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Beckwith CG, Zaller ND, Fu JJ, Montague BT, Rich JD. Opportunities to diagnose, treat, and prevent HIV in the criminal justice system. J Acquir Immune Defic Syndr. 2010;55(Suppl 1):S49–55. doi: 10.1097/QAI.0b013e3181f9c0f7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.VanHandel M, Beltrami JF, MacGowan RJ, Borkowf CB, Margolis AD. Newly identified HIV infections in correctional facilities, United States, 2007. Am J Public Health. 2012 May;102(Suppl 2):S201. doi: 10.2105/AJPH.2011.300614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Maruschak L, Beavers R. HIV in Prisons, 2007–08: Bureau of Justice Statistics. 2009 Report No.: NCJ 228307. [Google Scholar]
- 7.April MD. Bull World Health Organ. Switzerland: 2010. Rethinking HIV exceptionalism: the ethics of opt-out HIV testing in sub-Saharan Africa; pp. 703–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.WHO. Health in prisons: A WHO guide to the essentials in prison health. WHO Regional Office for Europe; 2007. [Google Scholar]
- 9.Rennie S, Behets F. Desperately seeking targets: the ethics of routine HIV testing in low-income countries. Bulletin of the World Health Organization. 2006;84(1):52–7. doi: 10.2471/blt.05.025536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Malek M, Bazazi AR, Cox G, Rival G, Baillargeon J, Miranda A, et al. Implementing opt-out programs at Los Angeles county jail: a gateway to novel research and interventions. J Correct Health Care. 2011;17(1):69–76. doi: 10.1177/1078345810385916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.CDC. Revised recommendations for HIV testing of adults, adolescents, and pregnant women in health-care settings. MMWR. 2006;55(RR14):1–17. [PubMed] [Google Scholar]
- 12.Maruschak L, Berzofsky M, Unangst J. Medical Problems of State and Federal Prisoners and Jail Inmates, 2011–12: Bureau of Justice Statistics. 2015 Report No.: NCJ 248491. [Google Scholar]
- 13.Beckwith CG, Nunn A, Baucom S, Getachew A, Akinwumi A, Herdman B, et al. Rapid HIV Testing in Large Urban Jails. Am J Public Health. 2012;102(S2):S184–6. doi: 10.2105/AJPH.2011.300514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Grinstead O, Seal DW, Wolitski R, Flanigan T, Fitzgerald C, Nealey-Moore J, et al. HIV and STD testing in prisons: perspectives of in-prison service providers. AIDS Educ Prev. 2003;15(6):547–60. doi: 10.1521/aeap.15.7.547.24045. [DOI] [PubMed] [Google Scholar]
- 15.Rosen DL, Golin CE, Grodensky CA, May J, Bowling JM, DeVellis RF, et al. Opt-out HIV testing in prison: informed and voluntary? AIDS Care. 2015;27(5):545–54. doi: 10.1080/09540121.2014.989486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ostermann J, Kumar V, Pence BW, Whetten K. Trends in HIV testing and differences between planned and actual testing in the United States, 2000–2005. Arch Intern Med. 2007 Oct;167(19):2128–35. doi: 10.1001/archinte.167.19.2128. [DOI] [PubMed] [Google Scholar]
- 17.Carey MP, Schroder KE. Development and psychometric evaluation of the brief HIV Knowledge Questionnaire. AIDS Educ Prev. 2002 Apr;14(2):172–82. doi: 10.1521/aeap.14.2.172.23902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Asaoka K, Shoji H, Nishizaka S, Ayabe M, Abe T, Ohori N, et al. Non-herpetic acute limbic encephalitis: Cerebrospinal fluid cytokines and magnetic resonance imaging findings. Internal Medicine. 2004;43(1):42–8. doi: 10.2169/internalmedicine.43.42. [DOI] [PubMed] [Google Scholar]
- 19.Ochtera RD. Conceptualizing HIV-associated stigma and exploring the correlates of HIV testing behaviors for incarcerated men in North Carolina. Chapel Hill: University of North Carolina at Chapel Hill; 2012. [Google Scholar]
- 20.Zou G. A modified poisson regression approach to prospective studies with binary data. American journal of epidemiology. 2004;159(7):702–6. doi: 10.1093/aje/kwh090. [DOI] [PubMed] [Google Scholar]
- 21.Parker R, Aggleton P. HIV and AIDS-related stigma and discrimination: a conceptual framework and implications for action. Social science and medicine. 2003;57:13–24. doi: 10.1016/s0277-9536(02)00304-0. [DOI] [PubMed] [Google Scholar]
- 22.Wohl DA, Golin C, Rosen DL, May JM, White BL. Detection of undiagnosed HIV among state prison entrants. JAMA. 2013;310(20):2198–9. doi: 10.1001/jama.2013.280740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.CDC. HIV Screening of Male Inmates During Prison Intake Medical Evaluation — Washington, 2006–2010. MMWR. 2011;60(24):811–3. [PubMed] [Google Scholar]
- 24.Haukoos JS, Hopkins E, Bender B, Al-Tayyib A, Long J, Harvey J, et al. Use of kiosks and patient understanding of opt-out and opt-in consent for routine rapid human immunodeficiency virus screening in the emergency department. Acad Emerg Med. 2012 Mar;19(3):287–93. doi: 10.1111/j.1553-2712.2012.01290.x. [DOI] [PubMed] [Google Scholar]
- 25.Ujiji OA, Rubenson B, Ilako F, Marrone G, Wamalwa D, Wangalwa G, et al. Is ‘Opt-Out HIV Testing’ a real option among pregnant women in rural districts in Kenya? BMC Public Health. 2011;11:151. doi: 10.1186/1471-2458-11-151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mugore L, Engelsmann B, Ndoro T, Dabis F, Perez F. An assessment of the understanding of the offer of routine HIV testing among pregnant women in rural Zimbabwe. AIDS Care. 2008;20(6):660–6. doi: 10.1080/09540120701687034. [DOI] [PubMed] [Google Scholar]
- 27.Emerson GG, Smith JR, Wilson DJ, Rosenbaum JT, Flaxel CJ. Primary treatment of acute retinal necrosis with oral antiviral therapy. Ophthalmology. 2006 Dec;113(12):2259–61. doi: 10.1016/j.ophtha.2006.05.063. [DOI] [PubMed] [Google Scholar]
- 28.Walker J, Sanchez R, Davids J, Stevens M, Whitehorn L, Greenspan J, et al. Is routine testing mandatory or voluntary? Clinical Infectious Diseases. 2005;40(2):319. doi: 10.1086/426147. [DOI] [PubMed] [Google Scholar]
- 29.Courtenay WH. Behavioral Factors Associated with Disease, Injury, and Death among Men: Evidence and Implications for Prevention. Journal of Men’s Studies. 2000;9(1):81–142. [Google Scholar]
- 30.Wenzel SL, Rhoades H, Tucker JS, Golinelli D, Kennedy DP, Zhou A, et al. HIV risk behavior and access to services: what predicts HIV testing among heterosexually active homeless men? AIDS Educ Prev. 2012 Jun;24(3):270–9. doi: 10.1521/aeap.2012.24.3.270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Al-Zarzour N, Monem F. Are human herpes viruses associated with autoimmune thyroid disease? Journal of infection in developing countries. 2011;5(12):890–2. doi: 10.3855/jidc.1757. [DOI] [PubMed] [Google Scholar]
- 32.Derlega VJ, Winstead BA, Brockington JE. AIDS stigma among inmates and staff in a USA state prison. Int J STD AIDS. 2008 Apr;19(4):259–63. doi: 10.1258/ijsa.2007.007141. [DOI] [PubMed] [Google Scholar]
- 33.Snell WE, Finney PD, Godwin LJ. Stereotypes about AIDS. Contemporary Social Psychology. 1991;15:18–38. [Google Scholar]


