Abstract
Purpose:
The purpose of this study is to evaluate the safety and benefits of immediate sequential bilateral cataract surgery.
Patients and Methods:
Retrospective data analysis of patients who underwent immediate sequential bilateral phacoemulsification with foldable intraocular lens (IOL) implantation under topical anesthesia from January 2011 to September 2016 was performed. Patients with visually significant bilateral cataract within the axial length range of 21.0–26.5 mm were included in the study. Intraoperative and postoperative complications were evaluated.
Results:
Two thousand four hundred and seventy eyes from 1235 patients with a mean age of 68.34 years (range: 4–90 years) were analyzed. Best-corrected visual acuity improved from 0.40 ± 0.17 to 0.08 ± 0.10 (logarithm of the minimum angle of resolution). Nearly 92.05% eyes achieved a target postoperative refraction of ± 0.5 D spherical equivalent. Main complications observed were prolonged postoperative inflammation in 25% (n = 31), posterior capsular tears in 0.45% (n = 11), and unilateral cystoid macular edema in 0.08% (n = 2) eyes. No sight-threatening complications such as endophthalmitis, retinal detachment, corneal decompensation and intraocular hemorrhage occurred in any of the eyes. Out of the 288 (23.2%) patients who underwent bilateral multifocal IOL implantation, 23 patients (46 eyes) had femtolaser-assisted cataract surgery procedure. Two pediatric and one Downs syndrome patient underwent bilateral cataract surgery under general anesthesia and intravenous sedation, respectively.
Conclusion:
IBSCS may be considered as a preferred practice in eligible cases considering significant patient benefits such as early visual rehabilitation, time and cost-effectiveness, and better compliance with postoperative medications. In debilitated patients and special situations, such as pediatric cataract and Downs syndrome requiring general anesthesia it may be the ideal procedure.
Keywords: Bilateral cataract surgery, retrospective, South India
Cataract surgery is the most common surgical procedure performed worldwide.[1] Various innovations in cataract surgery such as a decrease in incision size from 8 mm to sub 1 mm, clear corneal, self-sealing incisions, and invention of foldable intraocular lenses (IOLs) have accelerated the visual rehabilitation of patients to the extent of few minutes. In addition, refinement in the IOL power calculation formulae and advanced biometry techniques have significantly improved the precision of IOL power calculation with 90%–95% eyes achieving postoperative spherical equivalent (SE) within ±1.0 diopter (D).[2,3]
However, in spite of these technological advancements, the date back teaching “do not operate both the eyes simultaneously” remains unchanged due to the fear of visually-threating complications such as endophthalmitis and postoperative refractive surprises.[4,5,6,7]
In this era of evidence-based clinical practice, numerous studies have provided enough supporting data in favor of immediate sequential bilateral cataract surgery (ISBCS) being a safe and economic procedure.[4,5,6,7] In addition, the benefits of a sequential second eye surgery regarding good visual outcome and patient satisfaction have already been proven.[8,9,10,11,12,13,14]
Through this retrospective study, we hereby report the outcomes of a large series of 2470 eyes that underwent ISBCS within a span of 5 years at our center. A comparison was also performed regarding the visual and refractive outcomes, safety, risks, and benefits associated with ISBCS with the previously published reports. To the best of our knowledge, this is the largest data from India and second largest in the world on ISBCS being reported from a single NABH accredited tertiary eye hospital of South India.
Patients and Methods
Data were collected retrospectively from electronic medical records for all the patients who underwent ISBCS in Nethradhama Superspeciality Eye Hospital, Bengaluru, from January 2011 to September 2016. The study was approved by the Ethics Committee of the hospital and was conducted in accordance with the tenets of the Declaration of Helsinki.
ISBCS was considered in patients with visually significant bilateral cataract (best-corrected visual acuity worse than 6/12) with both eyes within the axial length range of 21.0–26.5 mm, patients opting for multifocal implants, and those undergoing surgery under general anesthesia.
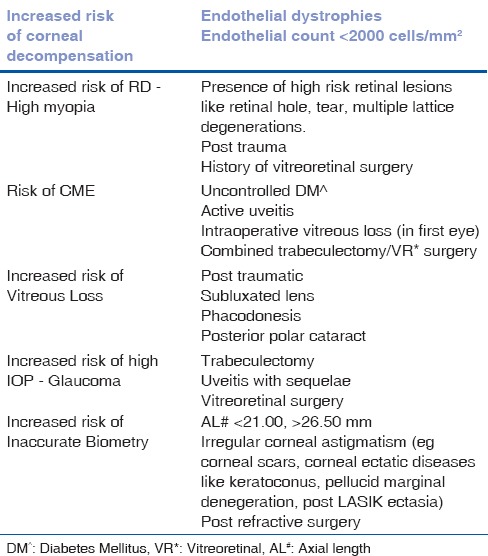
The exclusion criteria were - conditions predisposing to increased intraoperative complications such as posterior capsule rent and vitreous loss, postoperative complications such as infections, corneal decompensation, retinal detachment (RD), cystoid macular edema (CME), and inaccurate IOL power calculation. Ocular comorbidities that required a combined surgery (trabeculectomy or vitreoretinal surgery) were also excluded from the study [Table 1].
Table 1.
List of ocular conditions excluded from the study
All patients underwent a thorough preoperative eye examination and necessary investigations according to the hospital protocol. All the patients had preoperative dilated 360° fundus examination with indentation to rule out any possible high-risk lesion, the presence of which excluded the patient for ISBCS. Biometry was performed using IOL Master 500 (Carl Zeiss Meditec AG, Jena, Germany) or A-scan device (Pac Scan Plus, Sonomed, New Hyde Park, NY, USA) in cases of dense cataracts. SRK-T formula was used for IOL power calculation to achieve the planned refraction.
Operative protocol for immediate sequential bilateral cataract surgery
The surgery protocol was derived from the previously published guidelines of the International Society of Bilateral Cataract Surgeons.[15] All the patients who underwent bilateral cataract surgeries had both eyes operated by a single experienced surgeon (Sri Ganesh) under topical anesthesia of 4% lidocaine (LOX 4%, Neon Laboratories Ltd., Andheri, Mumbai, Maharashtra, India) and intracameral anesthesia of 1% lidocaine with 1 in 20,000 adrenalin (AstraZeneca Hebbal, Bengaluru, India). Utmost care was taken to maintain strict asepsis intraoperatively. Each eye was treated as a separate procedure with complete segregation of the two procedures. Preoperatively, 5% povidone-iodine was used to coat the conjunctival sac, lid, nose, forehead, and cheek on both sides at the same time [Supplementary File 1 (359.2KB, pdf) and Video 1]. The eye with advanced cataract was operated first. A sterile plastic drape was placed over the eye, covering the lashes, and orifices of meibomian glands and a speculum was applied. All the eyes underwent a standard phacoemulsification procedure using a temporal 2.8 mm clear corneal incision with a diamond blade, followed by implantation of foldable IOLs in the capsular bag. Leak-proof sealing of the wounds was ensured at the end of the surgery.
Before operating the second eye, both the surgeon and the assistant changed their gowns and gloves. The second eye was cleaned and prepared again in a similar manner as the first eye. A new trolley with separate full cycle autoclaved instruments, viscoelastic, irrigation line, and balanced salt solution was used. Intracameral vancomycin (1 mg/0.1 ml) was injected in all cases at the end of the procedure.
In the event of posterior capsule rupture or any other visually threatening intraoperative complication in the first eye, the second eye surgery was abandoned and deferred for a later date.
All the patients were provided dark goggles after surgery and were discharged on the same day after starting the postoperative medications in the hospital. The postoperative medications included ofloxacin-Dx eyedrop (ofloxacin [0.3% w/v], dexamethasone [0.1% w/v%] Micro Labs, Bengaluru, India) and nevanac (nepafenac 0.1%, Alcon industries, Fort Worth, Texas, USA) eyedrops. Separate postoperative medication kits were provided for each eye. Patients were explained about eye hygiene and were instructed to report back immediately if ominous signs and symptoms of decreasing vision, eye pain, or redness were experienced.
Postoperative follow-up examinations were conducted at day 1, 2 weeks, 3 months, and annually. At 2 weeks, visual acuity, refraction, and dilated fundus examination were performed. Glasses were also prescribed at 2 weeks postoperative checkup. All patients completed at least 2 weeks follow-up, and hence, visual and refractive data at 2 weeks postoperative visit was used for analysis. The visual acuity was measured using snellen visual acuity chart at 6 m, which was later converted to logarithm of the minimum angle of resolution (logMAR) values for statistical analysis.
Statistical analysis
Statistical analysis was performed using SPSS software, version 23 (Statistical Package for the Social Sciences, IBM Corporation, Armonk, New York, United States) and Microsoft Excel. The mean age, visual acuity, and axial length were calculated using Microsoft Excel. Since the data were not normally distributed, Wilcoxon signed-ranks test (nonparametric test) was used for statistical analysis for assessing the differences between the preoperative and postoperative SE. Paired t-test was applied to demonstrate differences between preoperative and postoperative visual acuity.
Results
A total of 2470 eyes from 1235 patients with a mean age of 68.34 years (range: 4–90 years) were included in the study, out of which 28.9% (n = 714) were women, and 71.1% (n = 1756) were men. The mean axial length was 23.4 ± 1.76 (21.23–26.1 mm) [Table 2].
Table 2.
Baseline demographic, preoperative and systemic characteristics of the patients included in the present study
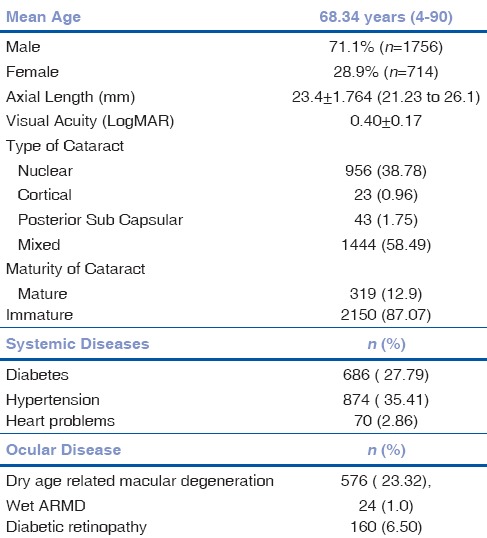
The various systemic and ocular comorbidities of the participant patients are listed in Table 3. The systemic morbidities included diabetes mellitus 27.79% (n = 686), hypertension 35.41% (n = 874), cardiac problems 2.86% (n = 70), parkinsonism 0.08% (n = 2), and arthritis 0.85% (n = 21), whereas, the noteworthy ocular comorbidities were dry age-related macular degeneration (ARMD) 23.32% (n = 576), diabetic retinopathy 6.5% (n = 160), wet ARMD 1.0% (n = 24), pseudoexfoliation 0.41% (n = 10), and epiretinal membrane 0.25% (n = 6).
Table 3.
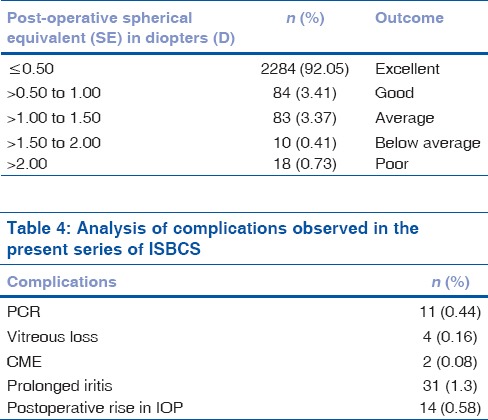
Postoperative refractive outcome achieved in terms of residual spherical equivalent (SE) at 2 weeks postoperative visit
Multifocal IOLs (MFIOLs) were implanted in 576 eyes (23.2%) of 288 patients. About 76 eyes (3%) underwent ISBCS with femtosecond laser-assisted cataract surgery (FLACS). About 46 eyes (1.86%) underwent FLACS with MFIOL implantation, while the remaining 98% underwent routine phacoemulsification surgery. Four eyes (0.16%) of two pediatric patients (age <10 years), and one patient with Downs syndrome (age 24 years) underwent bilateral cataract surgery under general anesthesia.
Visual and refractive outcomes
The mean preoperative best-corrected visual acuity was 0.40 ± 0.16 logMAR which improved significantly to 0.08 ± 0.1 logMAR at the end of 2 weeks postoperative follow-up, (P = 0.000).
A statistically significant reduction in the SE was observed as the SE reduced from a preopertive value of −1.35 ± 4.4 D to 0.15 ± 0.57 D at 2 weeks postoperatively (P = 0.001). About 92.05% patients achieved targeted postoperative SE refraction within ±0.5 D while all eyes were within ±1.5 D at the end of 2 weeks [Table 4]. Postoperative SE was within ±1.00 D in 98.7% eyes in our study when compared to 43% and 83.2%, as reported by Johansson and Sarrikkola et al., respectively [Table 5].
Table 4.
Analysis of complications observed in the present series of ISBCS
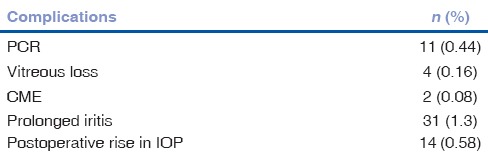
Table 5.
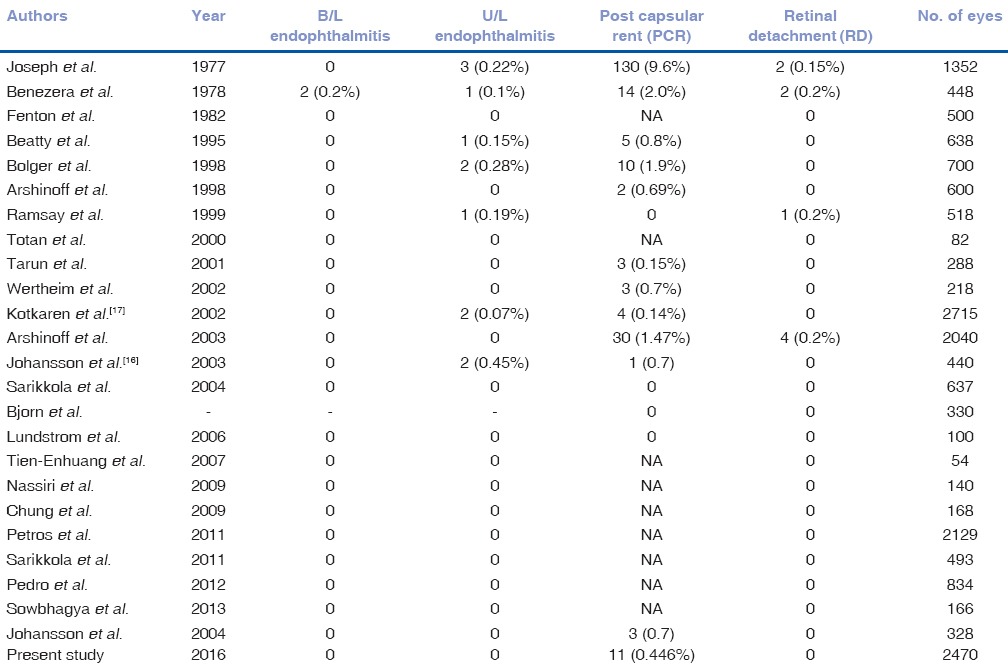
Comparative analysis of complications of ISBCS between the previously published and the present study
The 288 patients who underwent ISBCS with MFIOL implantation in this series, achieved excellent outcomes which were defined as bilateral uncorrected visual acuity of 6/9 or better, bilateral uncorrected visual acuity of N.8 or better and patient satisfaction regarding spectacle independence.
Intra- and post-operative complications
The chief intraoperative complication encountered in the series was posterior capsular tears, which occurred in 11 (0.45%) eyes. It is noteworthy to mention that this complication occurred in the second eyes of these patients, whose first eye surgery was uneventful. Of these 11 eyes, 4 eyes required anterior vitrectomy with placement of 3 piece foldable IOL in the sulcus. Among the four vitrectomized eyes, three eyes achieved a best-corrected visual acuity of 6/6 and one eye with myopic degeneration achieved a best-corrected vision of 6/12.
Postoperative complications in the decreasing order of frequency were prolonged postoperative inflammation, elevated intraocular pressure (IOP), and CME. Prolonged postoperative iritis (inflammation extending beyond 6 weeks) was seen in 1.3% (n = 31) of the patients, out of which 0.68% (n = 17) were diabetic individuals. The intermediate rise in IOP (21–30 mmHg) requiring antiglaucoma medications was seen in 0.57% (n = 14) eyes, which subsided with treatment. CME was seen in 0.08% (n = 2) eyes, both being unilateral in nondiabetic patients. No sight-threatening complications such as endophthalmitis, RD, corneal decompensation, and intraocular hemorrhages were observed in any of the eyes operated in the series [Table 4].
Discussion
Previously, some studies have reported that the major concerns in performing an ISBCS are the risks of certain vision-threatening complications such as endophthalmitis, RD, CME, irreversible corneal edema, and refractive surprises.[16,17]
However, our literature review revealed that the actual incidence of these dreaded bilateral complications was not higher, but comparable to the unilateral scenario. Regarding bilateral endophthalmitis so far four cases have been reported since 1952.[5,19,20] However, it was not specified, if these cases had any intraoperative complication such as posterior capsule rent associated with vitreous loss, which could potentially increase the risk of endophthalmitis. In addition, it was reported that these cases occurred before the advent of intracameral antibiotics for prophylaxis of postoperative endophthalmitis, which was also highlighted by the European Society of Cataract and Refractive Surgeons study.[21]
This may indicate that the chances of endophthalmitis may be significantly reduced, provided the guidelines laid by the International Society of Bilateral Cataract Surgeons[15] and the United Kingdom Royal College of Ophthalmologists[22] are strictly followed.
Arshinoff and Odorcic[23,24,25] calculated the risk of bilateral endophthalmitis to be 0.005% which was suggested to almost ten times rarer than the unilateral endophthalmitis [Table 5]. They also noted an obvious breach in the aseptic protocols during surgery in these cases of bilateral endophthalmitis.[23,24,25]
In our series, no eyes developed endophthalmitis (unilateral or bilateral), which could be attributed to a meticulous case selection (excluding cases with high risk of infection), thorough intraoperative asepsis protocols followed, and skillfully performed surgery. The precautions taken intraoperatively included complete segregation of the two procedures by using separate sets of drapes, gowns, gloves, and full-cycle autoclaved instruments for both eyes as described earlier. Intraoperatively, utmost care was taken to achieve a good wound architecture, minimal tissue injury, and ensure leak-proof incision closure. In addition, all eyes received intracameral antibiotics in the form of vancomycin (20 mcg/ml) at the completion of the surgery. Arshinoff and Bastianelli showed that the use of intracameral vancomycin significantly minimized the incidence of endophthalmitis to 0.001%. In addition, vancomycin was found to be equally efficacious as cephalosporin and moxifloxacin in preventing endophthalmitis.[26]
Bilateral CME is another concern regarding postoperative visual loss in the scenario of ISBCS. In our study, no patient developed bilateral CME; however, two patients presented with unilateral CME, which resolved in 3 months with treatment. Meticulous case selection by avoiding high-risk cases (uncontrolled diabetics, active uveitis, and history of arthritis), atraumatic surgery, and mandatory use of postoperative nonsteroidal anti-inflammatory drugs have been proven to prevent postoperative CME that may potentially lead to delay in the visual rehabilitation.[27]
It is known that certain conditions such as collagen vascular diseases, active rheumatism, significant dry eye, corneal thinning, and corneal exposure may increase the risk for postoperative corneal melt and uveitis and hence may be considered as contraindications for ISBCS. No eye in the series developed irreversible corneal damage or endothelial decompensation as this was well taken care of by good patient selection and meticulously performed surgery. For hard and brown cataracts and eyes with low endothelial counts (<2000 cells/mm2), a dispersive viscoelastic agent (aurocoat, sodium hyaluronate 20 mg/ml [2% w/v] chondroitin sulfate: 20 mg/ml [2% w/v], Aurolab, Madurai, India) was routinely used for endothelial protection. Most of the cases of corneal edema in our series were transient and unilateral. Wertheim and Burton reported bilateral corneal edema after ISBCS, which resolved within 3 months with medical management.[28] One case of bilateral corneal decompensation requiring penetrating keratoplasty has been reported, but there was no mention of any ocular comorbidity.[29]
There is no report of bilateral RD following ISBCS till date. In the present study also, no eye had RD in the postoperative period. The maximal axial length operated was 26.1 mm, and cases of the previous history of RD, extreme axial length, posttrauma, high-risk retinal lesions, and combined surgery were excluded from the study [Table 1]. So far, only four studies have reported postoperative RD (0.15%–0.2%),[4,5,30,31] the incidence of which is comparable to the unilateral scenario (0.1%–0.7%).[32]
Posterior capsular rent (PCR) with vitreous loss (10.7%–0.05%) was the most common intraoperative complication observed in all the previously reported case series. PCR with or without vitreous loss is known to be associated with an increased risk of more than 6-fold for acute endophthalmitis.[15] The incidence of PCR in our study was 0.44%, which was also comparable to similar studies on ISBCS by Kontkanen and Kaipiainen[33] (0.14%) and Arshinoff et al.[31] (1.47%) [Table 6].
Table 6.
Comparison of postoperative refractive outcome in terms of spherical equivalent (SE) between the previously published and the present study
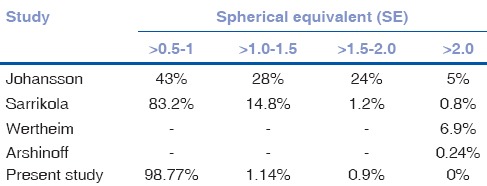
Favorable refractive outcomes were achieved with ISBCS in our series with 92.05% eyes achieving a postoperative residual SE within ±0.5 D and 98.83% within ±1.0 D [Table 3]. These refractive results were comparable to the previous studies.[28,31,34,35,36] The literature review [Table 6] revealed that refractive surprises (residual refractive error of >1.5 D SE) following ISBCS were mainly observed in high myopes or hyperopes which form the extremes of the bell-shaped distribution of postcataract surgery refractive outcome.[36] We believe our favourable outcome was possible due to strict selection criteria excluding eyes with extremes of axial lengths, irregular corneal astigmatism (e.g., corneal scars, corneal ectatic diseases such as keratoconus, pellucid marginal degeneration, post-LASIK ectasia), use of optical biometry (IOL master), appropriate IOL formulae, and optimized A-constants for IOLs.
Two hundred and eighty-eight (23.2%) patients had bilateral MFIOL implantation with excellent visual outcomes. Bilateral implantation of MFIOL has been proven to provide better contrast sensitivity, stereopsis, and faster neuro-adaptation compared to unilateral implantation.[37]
Bilateral cataract surgery may be particularly preferred in pediatric patients requiring general anesthesia owing to better safety and faster visual rehabilitation through amblyopia therapy and early recovery of stereopsis.
Our hospital maintains a Lean Six Sigma score (National Demonstration Project conducted by Quality Council of India), which aims at optimizing postoperative refractive outcomes after cataract surgery by analyzing various potential causes leading to suboptimal refractive outcomes such as errors in biometry.[38] In addition, our hospital was the first NABH accredited eye hospital of India and received the accreditation in 2008. Hence, we abide by the benchmarks prescribed by NABH for eye health standards for improvement in quality eye care services and thus qualify to practice ISBCS.[39]
The primary author of this paper holds the membership of the International Society of Bilateral Cataract Surgeons and has performed over 75,000 topical clear corneal phacoemulsifications with a complication rate of <0.5%, which demonstrates the expertise and safety record of the surgeon.
Our study did not calculate the economic benefits of ISBCS, which may be a potential limitation of the study. However, other studies have proven beyond doubts that ISBCS has a tremendous impact on cutting down health-care cost to almost half.[40,41,42,43,44,45,46,47] In our country, where there is a long waiting list for cataract surgery, and the health-care providers are mostly concentrated in the urban areas, ISBCS may be considered provided strict protocols are followed. It may provide significant patient benefits in terms of better compliance with postoperative medications, reduced hospital visits, faster visual rehabilitation, and shorter period of restrictions after surgery. However, we are absolutely against and do not recommend performing bilateral cataract surgeries in camp conditions or setups where high standards of asepsis cannot be ensured.
Conclusion
Bilateral cataract surgery may be a preferred practice in the hands of an experienced surgeon with minimal complication rate, with access to facilities such as modern biometric equipment, strict operation room sterilization protocol, and well-trained support staff.
Video Available on: www.ijo.in
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Panchapakesan J, Rochtchina E, Mitchell P. Five-year change in visual acuity following cataract surgery in an older community: The Blue Mountains Eye Study. Eye (Lond) 2004;18:278–82. doi: 10.1038/sj.eye.6700641. [DOI] [PubMed] [Google Scholar]
- 2.Narváez J, Zimmerman G, Stulting RD, Chang DH. Accuracy of intraocular lens power prediction using the Hoffer Q, Holladay 1, Holladay 2, and SRK/T formulas. J Cataract Refract Surg. 2006;32:2050–3. doi: 10.1016/j.jcrs.2006.09.009. [DOI] [PubMed] [Google Scholar]
- 3.Aristodemou P, Knox Cartwright NE, Sparrow JM, Johnston RL. Intraocular lens formula constant optimization and partial coherence interferometry biometry: Refractive outcomes in 8108 eyes after cataract surgery. J Cataract Refract Surg. 2011;37:50–62. doi: 10.1016/j.jcrs.2010.07.037. [DOI] [PubMed] [Google Scholar]
- 4.Joseph N, David R. Bilateral cataract extraction in one session: Report on five years’ experience. Br J Ophthalmol. 1977;61:619–21. doi: 10.1136/bjo.61.10.619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Benezra D, Chirambo MC. Bilateral versus unilateral cataract extraction: Advantages and complications. Br J Ophthalmol. 1978;62:770–3. doi: 10.1136/bjo.62.11.770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fenton PJ, Gardner ID. Simultaneous bilateral intraocular surgery. Trans Ophthalmol Soc U K. 1982;102(Pt 2):298–301. [PubMed] [Google Scholar]
- 7.Beatty S, Aggarwal RK, David DB, Guarro M, Jones H, Pearce JL. Simultaneous bilateral cataract extraction in the UK. Br J Ophthalmol. 1995;79:1111–4. doi: 10.1136/bjo.79.12.1111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bolger J, Steinmetz B, Claoué C. Responses to December 1997 consultation section (letters) J Cataract Refract Surg. 1998;24:430–2. [Google Scholar]
- 9.Totan Y, Bayramlar H, Cekiç O, Aydin E, Erten A, Daglioglu MC. Bilateral cataract surgery in adult and pediatric patients in a single session. J Cataract Refract Surg. 2000;26:1008–11. doi: 10.1016/s0886-3350(00)00380-1. [DOI] [PubMed] [Google Scholar]
- 10.Sharma TK, Worstmann T. Simultaneous bilateral cataract extraction. J Cataract Refract Surg. 2001;27:741–4. doi: 10.1016/s0886-3350(00)00741-0. [DOI] [PubMed] [Google Scholar]
- 11.Elliott DB, Patla A, Bullimore MA. Improvements in clinical and functional vision and perceived visual disability after first and second eye cataract surgery. Br J Ophthalmol. 1997;81:889–95. doi: 10.1136/bjo.81.10.889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Laidlaw DA, Harrad RA, Hopper CD, Whitaker A, Donovan JL, Brookes ST, et al. Randomised trial of effectiveness of second eye cataract surgery. Lancet. 1998;352:925–9. doi: 10.1016/s0140-6736(97)12536-3. [DOI] [PubMed] [Google Scholar]
- 13.Lundström M, Stenevi U, Thorburn W. Quality of life after first- and second-eye cataract surgery: Five-year data collected by the Swedish National Cataract Register. J Cataract Refract Surg. 2001;27:1553–9. doi: 10.1016/s0886-3350(01)00984-1. [DOI] [PubMed] [Google Scholar]
- 14.Javitt JC, Steinberg EP, Sharkey P, Schein OD, Tielsch JM, Diener M, et al. Cataract surgery in one eye or both. A billion dollar per year issue. Ophthalmology. 1995;102:1583–92. doi: 10.1016/s0161-6420(95)30824-x. [DOI] [PubMed] [Google Scholar]
- 15.International Society of Bilateral Cataract Surgeons. General Principles for Excellence in ISBCS. [Last accessed on 2016 Nov 01]. Available from: http://www.isbcs.org .
- 16.Henderson BA, Schneider J. Same-day cataract surgery should not be the standard of care for patients with bilateral visually significant cataract. Surv Ophthalmol. 2012;57:580–3. doi: 10.1016/j.survophthal.2012.05.001. [DOI] [PubMed] [Google Scholar]
- 17.Tatham A, Brookes JL. Bilateral same-day cataract surgery should routinely be offered to patients? No. Eye (Lond) 2012;26:1033–5. doi: 10.1038/eye.2012.92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kashkouli MB, Salimi S, Aghaee H, Naseripour M. Bilateral Pseudomonas aeruginosa endophthalmitis following bilateral simultaneous cataract surgery. Indian J Ophthalmol. 2007;55:374–5. doi: 10.4103/0301-4738.33825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ozdek SC, Onaran Z, Gürelik G, Konuk O, Tekinsen A, Hasanreisoglu B. Bilateral endophthalmitis after simultaneous bilateral cataract surgery. J Cataract Refract Surg. 2005;31:1261–2. doi: 10.1016/j.jcrs.2005.04.005. [DOI] [PubMed] [Google Scholar]
- 20.Puvanachandra N, Humphry RC. Bilateral endophthalmitis after bilateral sequential phacoemulsification. J Cataract Refract Surg. 2008;34:1036–7. doi: 10.1016/j.jcrs.2008.01.032. [DOI] [PubMed] [Google Scholar]
- 21.Endophthalmitis Study Group, European Society of Cataract and Refractive Surgeons. Prophylaxis of postoperative endophthalmitis following cataract surgery: Results of the ESCRS multicenter study and identification of risk factors. J Cataract Refract Surg. 2007;33:978–88. doi: 10.1016/j.jcrs.2007.02.032. [DOI] [PubMed] [Google Scholar]
- 22.Benjamin L, Allen D, Desai P. Cataract Surgery Guidelines. 2010. Royal College of Ophthalmologists of the United Kingdom. 2010:69–71. [Google Scholar]
- 23.Arshinoff SA, Odorcic S. Same-day sequential cataract surgery. Curr Opin Ophthalmol. 2009;20:3–12. doi: 10.1097/ICU.0b013e32831b6daf. [DOI] [PubMed] [Google Scholar]
- 24.Arshinoff S. Simultaneous bilateral cataract surgery. J Cataract Refract Surg. 1998;24:1015–6. doi: 10.1016/s0886-3350(98)80089-8. [DOI] [PubMed] [Google Scholar]
- 25.Cao H, Zhang L, Li L, Lo S. Risk factors for acute endophthalmitis following cataract surgery: A systematic review and meta-analysis. PLoS One. 2013;8:e71731. doi: 10.1371/journal.pone.0071731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Arshinoff SA, Bastianelli PA. Incidence of postoperative endophthalmitis after immediate sequential bilateral cataract surgery. J Cataract Refract Surg. 2011;37:2105–14. doi: 10.1016/j.jcrs.2011.06.036. [DOI] [PubMed] [Google Scholar]
- 27.Ursell PG, Spalton DJ, Whitcup SM, Nussenblatt RB. Cystoid macular edema after phacoemulsification: Relationship to blood-aqueous barrier damage and visual acuity. J Cataract Refract Surg. 1999;25:1492–7. doi: 10.1016/s0886-3350(99)00196-0. [DOI] [PubMed] [Google Scholar]
- 28.Wertheim M, Burton R. Immediately sequential phacoemulsification performed under topical anaesthesia as day case procedures. Br J Ophthalmol. 2002;86:1356–8. doi: 10.1136/bjo.86.12.1356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Abe T, Hayasaka S, Nagaki Y, Kadoi C, Matsumoto M, Hayasaka Y. Pseudophakic cystoid macular edema treated with high-dose intravenous methylprednisolone. J Cataract Refract Surg. 1999;25:1286–8. doi: 10.1016/s0886-3350(99)00159-5. [DOI] [PubMed] [Google Scholar]
- 30.Ramsay AL, Diaper CJ, Saba SN, Beirouty ZA, Fawzi HH. Simultaneous bilateral cataract extraction. J Cataract Refract Surg. 1999;25:753–62. doi: 10.1016/s0886-3350(99)00035-8. [DOI] [PubMed] [Google Scholar]
- 31.Arshinoff SA, Strube YN, Yagev R. Simultaneous bilateral cataract surgery. J Cataract Refract Surg. 2003;29:1281–91. doi: 10.1016/s0886-3350(03)00052-x. [DOI] [PubMed] [Google Scholar]
- 32.Powe NR, Schein OD, Gieser SC, Tielsch JM, Luthra R, Javitt J, et al. Synthesis of the literature on visual acuity and complications following cataract extraction with intraocular lens implantation. Cataract Patient Outcome Research Team. Arch Ophthalmol. 1994;112:239–52. doi: 10.1001/archopht.1994.01090140115033. [DOI] [PubMed] [Google Scholar]
- 33.Kontkanen M, Kaipiainen S. Simultaneous bilateral cataract extraction: A positive view. J Cataract Refract Surg. 2002;28:2060–1. doi: 10.1016/s0886-3350(02)01787-x. [DOI] [PubMed] [Google Scholar]
- 34.Johansson B. Resulting refraction after same-day bilateral phacoemulsification. J Cataract Refract Surg. 2004;30:1326–34. doi: 10.1016/j.jcrs.2003.10.036. [DOI] [PubMed] [Google Scholar]
- 35.Sarikkola AU, Uusitalo RJ, Hellstedt T, Ess SL, Leivo T, Kivelä T. Simultaneous bilateral versus sequential bilateral cataract surgery: Helsinki Simultaneous Bilateral Cataract Surgery Study Report 1. J Cataract Refract Surg. 2011;37:992–1002. doi: 10.1016/j.jcrs.2011.01.019. [DOI] [PubMed] [Google Scholar]
- 36.Ladas JG, Stark WJ. Improving cataract surgery refractive outcomes. Ophthalmology. 2011;118:1699–700. doi: 10.1016/j.ophtha.2011.05.038. [DOI] [PubMed] [Google Scholar]
- 37.Arens B, Freudenthaler N, Quentin CD. Binocular function after bilateral implantation of monofocal and refractive multifocal intraocular lenses. J Cataract Refract Surg. 1999;25:399–404. doi: 10.1016/s0886-3350(99)80089-3. [DOI] [PubMed] [Google Scholar]
- 38.Ramaswamy SS, Ganesh S, Jain KH, Krishna DG. Improvement in the postoperative visual outcome following cataract surgeries by reducing the average residual spherical error. J Natl Accredit Board Hosp Healthc Providers. 2015;2:9–14. [Google Scholar]
- 39. [Last accessed on 2017 Jan 23]; Avialble from: http://www.nabh.co/hos-accr12.aspx . [Google Scholar]
- 40.Lundström M, Albrecht S, Nilsson M, Aström B. Benefit to patients of bilateral same-day cataract extraction: Randomized clinical study. J Cataract Refract Surg. 2006;32:826–30. doi: 10.1016/j.jcrs.2006.01.075. [DOI] [PubMed] [Google Scholar]
- 41.Huang TE, Kuo HK, Lin SA, Fang PC, Wu PC, Chen YH, et al. Simultaneous bilateral cataract surgery in general anesthesia patients. Chang Gung Med J. 2007;30:151–60. [PubMed] [Google Scholar]
- 42.Nassiri N, Nassiri N, Sadeghi Yarandi SH, Rahnavardi M. Immediate vs. delayed sequential cataract surgery: A comparative study. Eye (Lond) 2009;23:89–95. doi: 10.1038/sj.eye.6702989. [DOI] [PubMed] [Google Scholar]
- 43.Chung JK, Park SH, Lee WJ, Lee SJ. Bilateral cataract surgery: A controlled clinical trial. Jpn J Ophthalmol. 2009;53:107–13. doi: 10.1007/s10384-008-0627-6. [DOI] [PubMed] [Google Scholar]
- 44.Aristodemou P, Knox Cartwright NE, Sparrow JM, Johnston RL. First eye prediction error improves second eye refractive outcome results in 2129 patients after bilateral sequential cataract surgery. Ophthalmology. 2011;118:1701–9. doi: 10.1016/j.ophtha.2011.05.010. [DOI] [PubMed] [Google Scholar]
- 45.Serrano-Aguilar P, Ramallo-Fariña Y, Cabrera-Hernández JM, Perez-Silguero D, Perez-Silguero MA, Henríquez-de la Fe F, et al. Immediately sequential versus delayed sequential bilateral cataract surgery: Safety and effectiveness. J Cataract Refract Surg. 2012;38:1734–42. doi: 10.1016/j.jcrs.2012.05.024. [DOI] [PubMed] [Google Scholar]
- 46.Sowbhagya HN, Patil P, Himamshu NV, Kiran Kumar L, Rafi A, Raj K, et al. Safety and benefit of simultaneous bilateral cataract surgery in tertiary care centre. J Evol Med Dent Sci. 2013;12:1747–54. [Google Scholar]
- 47.Leivo T, Sarikkola AU, Uusitalo RJ, Hellstedt T, Ess SL, Kivelä T. Simultaneous bilateral cataract surgery: Economic analysis; Helsinki Simultaneous Bilateral Cataract Surgery Study Report 2. J Cataract Refract Surg. 2011;37:1003–8. doi: 10.1016/j.jcrs.2010.12.050. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


