Abstract
Background:
Obturator nerve (ON) stimulation during transurethral resection of lateral and posterolateral bladder wall tumor under spinal anesthesia may lead to obturator reflex, adductor contraction, and leg jerking with complications such as bleeding, bladder perforation, or incomplete tumor resection. Our study was carried out to obtain successful block of ON using ultrasound (US)-guided technique with or without nerve stimulation in patients undergoing transurethral resection of bladder tumor (TURBT) under spinal anesthesia.
Aims:
The aim of the study was to compare the effectiveness of two different techniques in blocking ON and adductor spasm during TURBT.
Settings and Design:
Prospective, randomized, double-blind study.
Subjects and Methods:
Sixty patients with American Society of Anesthesiologists Status II and III scheduled to undergo TURBT for lateral and posterolateral bladder wall tumor were enrolled. Group I (US group, n = 30) patients received 5 ml of bupivacaine 0.5% each at anterior, and posterior division of ON under real-time US visualization and Group II (US-NS group, n = 30) received the same amount of bupivacaine 0.5% for each division using US-guidance with nerve stimulation-assisted technique. Motor block onset time, block success and performance time, ease of performance of block, and complications were measured besides assessing patient and surgeon satisfaction into two groups.
Statistical Methods Used:
SPSS using two sample independent t-test and Pearson's Chi-square/Fisher's exact test.
Results:
Motor block onset was significantly faster in Group II (6.67 ± 2.40) than in Group I (12.39 ± 2.55). A success rate of 90% was achieved in Group II as compared to 76.7% in Group I with increased block performance time in Group II (4.47 ± 0.73 min) versus (2.10 ± 0.51 min) in Group I. A better patient and surgeon satisfaction were seen in Group II with combination of US and nerve stimulation technique. No complications were encountered.
Conclusion:
We conclude that both techniques are safe and easy to perform; however, nerve stimulation as an adjunct to US results in a faster onset of block with a higher success rate.
Keywords: Nerve stimulation, obturator nerve block, obturator reflex, ultrasound
INTRODUCTION
Peripheral nerve blocks remain a well-accepted component of comprehensive anesthetic care. Benefits of peripheral nerve block are improved analgesia, less need for narcotics and other pain medications, decreased recovery room and/or hospital stay, improved mobility and functional recovery after surgery, and improved patient satisfaction.[1]
Selective obturator nerve block (ONB) was first described by Labat in 1922.[2] Various techniques of ONB have been described since then.[3,4,5] ONB is used to provide pain relief in obturator neuralgia, in relief of adductor muscle spasm, associated with hemi or paraplegia among patients suffering from cerebrovascular pathologies, medullary injuries, multiple sclerosis, etc., treatment of painful hip joint conditions and in urological surgery to suppress the obturator reflex during transurethral resection of the lateral bladder wall tumor.[6] Obturator nerve (ON) passes in proximity to the inferolateral bladder wall, bladder neck, and prostatic urethra. As a result, transurethral resection of bladder tumor (TURBT) in the lateral bladder wall, when performed under spinal anesthesia, may provoke obturator reflex, adductor contraction, and leg jerking.[7]
TURBT is often performed with spinal anesthesia, but this does not block the obturator jerk reflex. However, ONB in TURBT can prevent obturator reflex to avoid complications such as bleeding, bladder perforation, or incomplete tumor resection.[7,8,9,10,11]
In our tertiary care center, a large number of patients are operated for bladder malignancies. Most of these patients are elderly with various comorbidities. Spinal anesthesia is preferred over general anesthesia in these patients. However, the ON stimulation during the procedure with subsequent obturator jerk makes spinal anesthesia less popular among our surgeons for this procedure. To overcome the obturator reflex and associated complications, we compared two different techniques of ONB for TURBT to make this procedure safer and improve patient and surgeon satisfaction.
SUBJECTS AND METHODS
This prospective randomized, double-blind study was conducted in the Department of Anaesthesiology and Critical Care, Sher-I-Kashmir Institute of Medical Sciences (SKIMS), Soura, Srinagar, Kashmir, during 2014–2016. SKIMS is a 700-bedded tertiary care hospital in the Northern State of Jammu and Kashmir (http://www.skims.ac.in/). The study was conducted according to the Declaration of Helsinki (1996) and was approved by the Institute Ethical Committee (SKIMS). After written informed consent, sixty patients having echographic evidence of an endovesical tumor located on lateral and posterolateral wall and undergoing TURBT were enrolled for this study. Most of the patients belonged to the American Society of Anesthesiologists Status II and III category. Patients with Inguinal lymphadenopathy, preexisting ON injury, coagulation disorder, infection or hematoma at injection site, and known allergy to local anesthetic (LA) agents were excluded from the study.
During the preoperative visit, all patients were evaluated and procedure explained. No sedation or premedication was administered. Spinal block with 25-gauge Quincke needle at the L3–L4 or L4–L5 interspace, in sitting position, using 3 ml of 0.5% hyperbaric bupivacaine, was performed to attain anesthesia to T10 level in all patients. Patients were then placed in the supine position with leg slightly abducted (30°) and externally rotated. The inguinal region was prepared with a chlorhexidine 2% solution and the ultrasound (US) probe (5–10 MHz, 50 mm linear transducer, Aloka Prosound SSD-3500SX), under sterile conditions, was used to visualize the anterior and posterior divisions of the ON between the three muscle layers (adductor longus, adductor brevis, and adductor magnus), 2–3 cm below the inguinal crease. Patients were randomized using sealed envelope method into two groups.
Group I (US group): in Group I, 22-gauge, 80 mm stimulating insulated needle was advanced under US-guidance, laterally to medially, to reach the anterior division of ON located between adductor longus and brevis. After negative aspiration, 5 ml of bupivacaine 0.5% was injected. The needle was then withdrawn and redirected toward the posterior division of the ON between adductor brevis and magnus and another volume of 5 ml of bupivacaine 0.5% was injected while the spread of the LA solution was monitored under real-time visualization. Group II (US-NS group): patients received ONB under US-guidance with nerve stimulation-assisted technique. The nerve stimulator that we used in our study was Microcontroller-based nerve stimulator (LCD-GEMI-Model: DSL-007). The needle tip (22-gauge, 80 mm) was first directed toward the anterior division of ON. Nerve stimulator was turned on and stimulation current beginning at 1–2 mA (2 Hz) was delivered to elicit muscle contraction, which was then gradually reduced to 0.5 mA. If muscle contractions were still observed in both the medial aspect of thigh and the sonogram, 5 ml of 0.5% bupivacaine was injected. The current was reduced to zero, and needle was redirected toward the posterior division. Stimulation current was again applied, as before, and when muscle contractions were observed both in the posterior aspect of thigh and the sonogram, another 5 ml of 0.5% bupivacaine was injected. Any needle redirection to reach the end-point for injection was recorded as an additional needle pass. Five minutes after the end of injection, the surgeon who was masked to group assignment entered the operating room to start TURBT and evaluate the motor blockade, which was graded as follows:
0 = Adductor spasm
1 = Reduced adductor spasm (50% reduction)
2 = No adductor spasm.
The strength of thigh adduction was measured at 5, 10, 15 min (min) after injection, and a score of 2 was considered as a successful block. If spasm persisted after 15 min, the block was classified as failed. The following data was recorded intraoperatively:
Motor block onset time: Time elapsed from the end of injection (time 0) until a motor block score of 2 was reached. Onset time was not recorded in failed blocks (when spasm persisted at 15 min)
Motor block success: The number of patients who had a score of 2 within 15 min after block placement
Block performance time: The time elapsed between the start of sonography and needle removal at the end of block
-
The ease of approach: Classified according to the number of needle redirections required to accomplish the block as follows:
- Number of needle passes ≤2 – Easy
- Number of needle passes >2 – Difficult
- Number of needle passes >10 – Failed.
Patient and surgeon satisfaction
Complications: The incidence of vascular puncture, hematoma, nerve injury, visceral injury, if any, was recorded.
The quantitative variables thus obtained were analyzed using two-sample independent t-test, and the categorical variables by using Pearson's Chi-square/Fisher's exact test. SPSS version 20 (IBM- SPSS Chicago, Illinois) was used for data analysis. P < 0.05 was considered to be statistically significant.
RESULTS
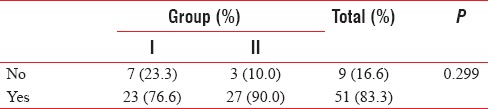
With reference to age, sex and body weight both groups were almost similar [Table 1]. Motor block onset was significantly faster in Group II (6.67 ± 2.40) than in Group I (12.39 ± 2.55, P < 0.01) [Table 2]. A success rate of 90% was achieved in Group II as compared to 76.7% in Group I [Table 3] with increased block performance time in Group II (4.47 ± 0.73 min) versus (2.10 ± 0.51 min) in Group I (P < 0.01) [Table 4]. The ease of approach between the two groups was not different [Tables 5 and 6]. A better patient and surgeon satisfaction were seen in Group II with a combination of US and nerve stimulation technique [Tables 7 and 8]. No complications were seen using two different techniques of ONB.
Table 1.
Demographic data of the groups
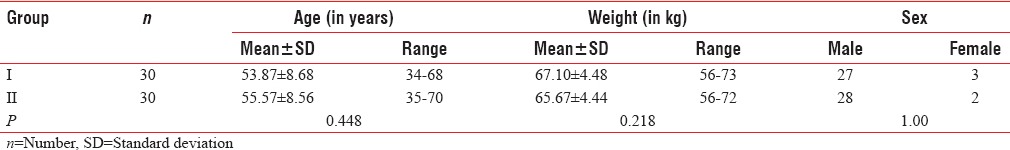
Table 2.
Motor block onset time (min)
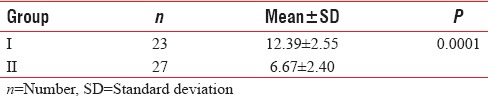
Table 3.
Motor block success percent
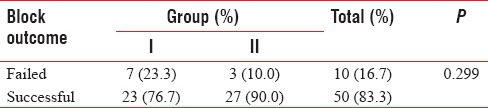
Table 4.
Block performance time (min)
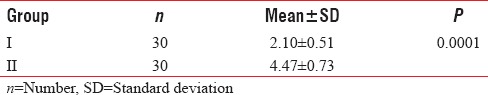
Table 5.
Ease of approach to perform block
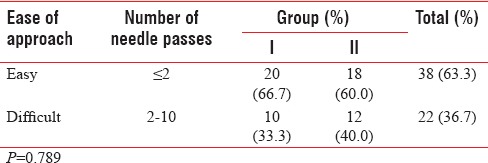
Table 6.
Number of needle passes
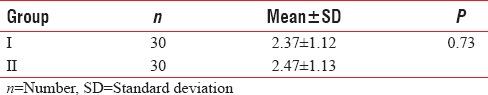
Table 7.
Patient satisfaction
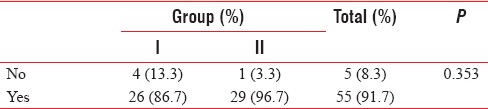
Table 8.
Surgeon satisfaction
DISCUSSION
Peripheral nerve blocks are cost effective anesthetic techniques used to provide anesthesia while avoiding airway instrumentation and hemodynamic consequences of general anesthesia. Patient satisfaction, a growing demand for cost-effective anesthesia, and a favorable postoperative recovery profile have resulted in increased demand for regional techniques.[12]
A well-accepted peripheral nerve block technique involves US-guided placement of LA adjacent to anatomic structures with known perineural proximity (e.g., fascia and vasculature).[13,14,15] Nerve stimulation techniques rely on the needle tip being directed towards the nerve itself and are particularly useful when a nerve is difficult to image sonographically. The ON is one such nerve that can be both, difficult to stimulate electrically and image sonographically.[16] Stimulation of the ON by electric current during TURBT causes sudden jerk (obturator reflex) due to contraction of adductor muscles. This may lead to bladder perforation or deep cut causing profuse bleeding. This may also result in incomplete resection of the bladder tumor and dissemination.[7,8]
Use of general anesthesia with muscle relaxants, ONB, superficial resection with low current, and cutting with bipolar resectoscope are different procedures which have been reported in literature, to prevent the adductor jerk and associated complications.[17,18,19,20] Different approaches for the ONB have evolved in the last decade. Recently, US-guided interfascial injection was proposed as an alternative method for performing an ONB, before[21] or after the division of the ON.[22]
Till now, limited studies have been undertaken to compare US-guided and nerve stimulation techniques to perform ONB. The present study aimed to compare the ONB characteristics and success rates, performed under US-guidance with (Group II) and without nerve stimulator (Group I), after the division of ON, in patients undergoing TURBT. Both the groups were homogenous with reference to age, sex and body weight. Motor block was assessed at 5, 10 and 15 min, from the time of injection of LA. The onset of motor block was faster in Group II than in Group I (P < 0.05). Manassero et al.[16] conducted the first study to compare interfascial injection versus a neurostimulation-assisted ONB, under US-guidance. They found a similar motor block onset time with US group (7.2 ± 3.6 min) and USENS group (6.2 ± 2.1 min). This was in contradiction to our study. The rapid onset of action in Group II, in our study, could be attributed to precise administration of LA around the nerve. Taha.[23] in his study evaluated a proximal US-guided ONB technique using an interfascial LA injection and reported a median motor block onset time of 4 min (95% confidence interval, 3–5 min). Successful motor block defined in our study as a motor block score of 2 at 15 min of injection of LA, was achieved in 23 out of 30 patients in Group I, and 27 of 30 patients in Group II with a success rate of 76.7% and 90%, respectively. However, the difference was statistically insignificant. Out of failed block cases, four patients in Group I and one patient in Group II had a score of 0 at 15 min. General anesthesia with muscle relaxant had to be administered in these cases. Rest of the failed cases had a reduced adductor spasm (score of 1 at 15 min), and the surgical procedure was completed under regional anesthesia after decreasing the current of electrocautery. Failures encountered during the procedure may be attributed to poor US visibility of nerve (in US group), anatomical variability of the ON, and inadequate diffusion of LA (in both groups). Min et al.[24] in their study using nerve stimulator to perform ONB achieved an overall success rate of 95.4%. Bolat et al.[25] using nerve stimulator for ONB, reported a success rate of 88.6%. The observations of above studies were in congruence to our study.
The mean block performance time in our study was 2.10 ± 0.51 min in Group I and 4.47 ± 0.73 min in Group II. This difference was statistically significant (P < 0.05). Our results are in congruence with Manassero et al.,[16] who observed a longer block performance time in the USENS group than in the US group (3.0 vs. 1.6 min) while performing ONB. An almost similar time of 2 min has been reported by Sinha et al.,[22] in their study, using US-guided ONB without nerve stimulation.
In our study, we could not find any difference in the number of needle passes between the two groups as was also noted by Manassero et al.[16] While evaluating the efficacy of US-guided ONB in transurethral surgery, Thallaj and Rabah et al.[17] found an appropriate patient and surgeon satisfaction. In our study, patient satisfaction was found to be 86.7% in Group I compared to 96.7% in Group II whereas surgeon satisfaction was found to be 76.6% in Group I and 90% in Group II. Complications resulting from poor nerve blockade and subsequent adductor jerks have been reported in many studies.[11,16] However, no complications were seen during our study as also reported by many other studies comparing blind, US-guided, and US nerve stimulator-guided ONB for transurethral surgery.[17,16,26]
CONCLUSION
The results of our study suggest that ONB along with spinal anesthesia is a safe and reliable technique for prevention of obturator jerk during TURBT resulting in good patient and surgeon satisfaction. Although both techniques are safe and easy to perform; however, nerve stimulation as an adjunct to US results in a faster onset of block with a higher success rate.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Swenson JD, Bay N, Loose E, Bankhead B, Davis J, Beals TC, et al. Outpatient management of continuous peripheral nerve catheters placed using ultrasound guidance: An experience in 620 patients. Anesth Analg. 2006;103:1436–43. doi: 10.1213/01.ane.0000243393.87912.9c. [DOI] [PubMed] [Google Scholar]
- 2.Labat G. Regional Anesthesia: Its Technic and Clinical Application. Philadelphia, PA: WB Saunders; 1922. [Google Scholar]
- 3.Choquet O, Capdevila X, Bennourine K, Feugeas JL, Bringuier-Branchereau S, Manelli JC. A new inguinal approach for the obturator nerve block: Anatomical and randomized clinical studies. Anesthesiology. 2005;103:1238–45. doi: 10.1097/00000542-200512000-00020. [DOI] [PubMed] [Google Scholar]
- 4.Baba M, Nishihara L, Tomi K. Pubic tubercle side approach to the obturator nerve block. Masui. 2007;56:1174–8. [PubMed] [Google Scholar]
- 5.Khorrami MH, Javid A, Saryazdi H, Javid M. Transvesical blockade of the obturator nerve to prevent adductor contraction in transurethral bladder surgery. J Endourol. 2010;24:1651–4. doi: 10.1089/end.2009.0659. [DOI] [PubMed] [Google Scholar]
- 6.Heywang-Köbrunner SH, Amaya B, Okoniewski M, Pickuth D, Spielmann RP. CT-guided obturator nerve block for diagnosis and treatment of painful conditions of the hip. Eur Radiol. 2001;11:1047–53. doi: 10.1007/s003300000682. [DOI] [PubMed] [Google Scholar]
- 7.Kuo JY. Prevention of obturator Jerk during transurethral resection of bladder tumor. JTUA. 2008;19:27–31. [Google Scholar]
- 8.Mydlo JH, Weinstein R, Shah S, Solliday M, Macchia RJ. Long-term consequences from bladder perforation and/or violation in the presence of transitional cell carcinoma: Results of a small series and a review of the literature. J Urol. 1999;161:1128–32. [PubMed] [Google Scholar]
- 9.Tatlisen A, Sofikerim M. Obturator nerve block and transurethral surgery for bladder cancer. Minerva Urol Nefrol. 2007;59:137–41. [PubMed] [Google Scholar]
- 10.Hradec E, Soukup F, Novák J, Bures E. The obturator nerve block. Preventing damage of the bladder wall during transurethral surgery. Int Urol Nephrol. 1983;15:149–53. doi: 10.1007/BF02085445. [DOI] [PubMed] [Google Scholar]
- 11.Akata T, Murakami J, Yoshinaga A. Life-threatening haemorrhage following obturator artery injury during transurethral bladder surgery: A sequel of an unsuccessful obturator nerve block. Acta Anaesthesiol Scand. 1999;43:784–8. doi: 10.1034/j.1399-6576.1999.430717.x. [DOI] [PubMed] [Google Scholar]
- 12.Moore DC. Traditional or supraclavicular technique. Reg Anesth. 1980;5:3–5. [Google Scholar]
- 13.Dingemans E, Williams SR, Arcand G, Chouinard P, Harris P, Ruel M, et al. Neurostimulation in ultrasound-guided infraclavicular block: A prospective randomized trial. Anesth Analg. 2007;104:1275–80. doi: 10.1213/01.ane.0000226101.63736.20. [DOI] [PubMed] [Google Scholar]
- 14.Sites BD, Beach ML, Spence BC, Wiley CW, Shiffrin J, Hartman GS, et al. Ultrasound guidance improves the success rate of a perivascular axillary plexus block. Acta Anaesthesiol Scand. 2006;50:678–84. doi: 10.1111/j.1399-6576.2006.01042.x. [DOI] [PubMed] [Google Scholar]
- 15.Tran DQ, Dugani S, Finlayson RJ. A randomized comparison between ultrasound-guided and landmark-based superficial cervical plexus block. Reg Anesth Pain Med. 2010;35:539–43. doi: 10.1097/AAP.0b013e3181faa11c. [DOI] [PubMed] [Google Scholar]
- 16.Manassero A, Bossolasco M, Ugues S, Palmisano S, De Bonis U, Coletta G. Ultrasound-guided obturator nerve block: Interfascial injection versus a neurostimulation-assisted technique. Reg Anesth Pain Med. 2012;37:67–71. doi: 10.1097/AAP.0b013e31823e77d5. [DOI] [PubMed] [Google Scholar]
- 17.Thallaj A, Rabah D. Efficacy of ultrasound-guided obturator nerve block in transurethral surgery. Saudi J Anaesth. 2011;5:42–4. doi: 10.4103/1658-354X.76507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yoshimura R, Adachi T, Funao K, Kobayakawa H, Matsuyama M, Tsuchida K, et al. Treatment of bladder tumors and benign prostatic hyperplasia with a new TUR system using physiological saline as perfusate. World J Surg. 2006;30:473–7. doi: 10.1007/s00268-005-0258-8. [DOI] [PubMed] [Google Scholar]
- 19.Kitamura T, Mori Y, Ohno N, Suzuki Y, Yamada Y. Case of bladder perforation due to the obturator nerve reflex during transurethral resection (TUR) of bladder tumor using the TUR in saline (Turis) system under spinal anesthesia. Masui. 2010;59:386–9. [PubMed] [Google Scholar]
- 20.Gupta NP, Saini AK, Dogra PN, Seth A, Kumar R. Bipolar energy for transurethral resection of bladder tumours at low-power settings: Initial experience. BJU Int. 2011;108:553–6. doi: 10.1111/j.1464-410X.2010.09903.x. [DOI] [PubMed] [Google Scholar]
- 21.Anagnostopoulou S, Kostopanagiotou G, Paraskeuopoulos T, Chantzi C, Lolis E, Saranteas T. Anatomic variations of the obturator nerve in the inguinal region: Implications in conventional and ultrasound regional anesthesia techniques. Reg Anesth Pain Med. 2009;34:33–9. doi: 10.1097/AAP.0b013e3181933b51. [DOI] [PubMed] [Google Scholar]
- 22.Sinha SK, Abrams JH, Houle TT, Weller RS. Ultrasound-guided obturator nerve block: An interfascial injection approach without nerve stimulation. Reg Anesth Pain Med. 2009;34:261–4. doi: 10.1097/AAP.0b013e3181a32c4d. [DOI] [PubMed] [Google Scholar]
- 23.Taha AM. Brief reports: Ultrasound-guided obturator nerve block: A proximal interfascial technique. Anesth Analg. 2012;114:236–9. doi: 10.1213/ANE.0b013e318237fb40. [DOI] [PubMed] [Google Scholar]
- 24.Min HG, Cheon MY, Choi KT. Use of nerve stimulator for the obturator nerve block. Korean J Anesthesiol. 2006;50:650–4. [Google Scholar]
- 25.Bolat D, Aydogdu O, Tekgul ZT, Polat S, Yonguc T, Bozkurt IH, et al. Impact of nerve stimulator-guided obturator nerve block on the short-term outcomes and complications of transurethral resection of bladder tumour: A prospective randomized controlled study. Can Urol Assoc J. 2015;9:E780–4. doi: 10.5489/cuaj.3149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Khorrami M, Hadi M, Javid A, Izadpahani MH, Mohammadi Sichani M, Zargham M, et al. A comparison between blind and nerve stimulation guided obturator nerve block in transurethral resection of bladder tumor. J Endourol. 2012;26:1319–22. doi: 10.1089/end.2012.0037. [DOI] [PubMed] [Google Scholar]


