Abstract
Background:
Pain in the dental operatory can have a profound effect on the behavior of children.
Aim:
The aim of this study is to evaluate the pain perception while administering local infiltration, in children undergoing dental extractions, using a new auto-controlled injection system.
Materials and Methods:
Children in the age range of 6–10 years with teeth indicated for extraction were recruited and allocated to either Group I, computer-controlled injection system (auto system with special cartridge and compatible disposable 30-gauge, 10 mm needles), or Group II, traditional system (30-gauge, 10 mm needle and disposable traditional syringe). Local infiltration was administered and extraction performed after 3 min. The time of administration (TOA) of infiltrate was noted whereas anxiety and pain in both groups were assessed using the Modified Child Dental Anxiety Faces Scale simplified (MCDAS(f)), pulse rate, Faces Pain Scale-Revised (FPS-R), and Face, Legs, Activity, Cry, Consolability (FLACC) Scale.
Results:
The TOA was high in computer group, compared to the traditional system (P < 0.001***); however, anxiety and pain were significantly less in computer group as reported in MCDAS(f), pulse rate, FPS-R, and FLACC (P < 0.001***).
Conclusions:
Computer system created a positive and comfortable experience for the child, as well as the practitioner. The possibility of using buccal infiltration instead of inferior alveolar nerve block in children below 10 years was also demonstrated.
Keywords: Child, injection, pain
INTRODUCTION
Pain during dental procedures is one of the major factors that have a lasting and profound impact on the behavior of the child.[1,2] Pain in the dental operatory leads to the development of negative attitude toward dentistry, which is projected as dental anxiety and fear in the future visits of a child; hence, pediatric dentists should focus on minimizing the same.[3,4] Nevertheless, most of the routine dental procedures pose some sort of discomfort or pain and can be alleviated by administering local anesthetic (LA) injections, which itself is a pain-provoking procedure. Thus, there was a need to explore strategies for painless injection techniques during LA administration, and to fulfill this, many forms of topical anesthetics, vibrotactile devices, jet injectors, and new electromagnetic and computer-controlled LA delivery systems were introduced in practice.[5,6,7] A constant search for methods to avoid the invasive and often painful nature of the injection led to the invention of comfortable and pleasant means of achieving LA, which has become a research continuum.
The key to the development of computer systems was based on the fact that delivering the anesthetic solution at a continual rate, pressure, and volume can reduce the pain of injection. However, these cannot be controlled manually; hence, many systems that allow the LA solution to be administered comfortably to the patient in different areas of the oral cavity at a continuous pressure and flow, irrespective of the tissue resistance were introduced into the clinical practice.[8] Studies showed the reduction in pain and increased comfort during injection with these systems,[9,10,11] and the clinical benefit ascribed the success of the computer systems to low pressure and slow delivery of the solution.[9] On the other hand, the reported disadvantages with these systems are the cost, extra time taken for LA administration, space occupied by the equipment, and complexity of the equipment.[12,13] Although these systems provide an array of options for the practitioners to manage the pain associated with dental procedures effectively, the dental community is slow in adopting this technology and is satisfied with the traditional methods due to the demerits of the system. However, the most important and challenging aspect for pediatric dentistry, the pain control, i.e., minimizing during dental treatment, is being ignored.
Over the years, computer systems such as Wand® (subsequent versions named as Wand Plus® and CompuDent®), Quick sleeper™, Sleeper One™, and Comfort Control Syringe™ were studied frequently and compared with traditional methods.[7,9,11,12,13,14,15,16,17,18] Gauge of the needle is reported to influence the pain of an injection;[11,13] however, dissimilar needle gauges were selected in some of the studies reported till date,[7,12,19] which can bias the results. Studies on various types of injections such as local infiltrations (including palatal pricks), nerve blocks, periodontal ligament (PDL), and intraosseous injections are available.[10,11,15,16] Pertaining to the mandible, inferior alveolar nerve block (IANB) was considered in majority of these studies;[12,19] however, in children below 10 years, it was proposed that the anesthetic solution can spread quickly and smoothly in infiltration techniques as mandible is less compact and the cortex is crossed by many canals.[20] Moreover, IANB is associated with complications such as nerve, vascular or muscle injuries, and myofascial pain. Therefore, the present study was undertaken to evaluate and compare the pain perception in children during mandibular infiltrations using a new auto-controlled injection system (EJOA painless dental anesthetic injection) and the traditional syringe (TS), with 30-gauge, 10 mm needles during dental extractions.
MATERIALS AND METHODS
Trial design
This was a superiority, open trial with parallel design and allocation ratio of 1:1.
Setting
Ethical clearance was obtained from the Institutional Ethical Committee, and the study was conducted at the department from March 2014 to September 2014.
Participants
Children attending the department who fulfilled the following criteria were included:
Age range of 6–10 years
Existence of untreatable carious or over retained mandibular primary teeth, indicated for extraction
Complete physical and mental health without any confounding medical history
Whose parents gave their written informed consent.
Children who were indicated for extraction of teeth as a part of emergency/immediate phase treatment and those with negative behavior according to the Wright's modification of Frankl behavior rating scale (FBRS) during initial examination were excluded.
About auto-controlled injection system
This is a painless anesthetic computer-controlled injection system (CCIS) with compact, portable design that injects the LA solution with constant speed and pressure control. The manufacturers claim that this system is more convenient, provides psychological comfort for children, and reduces anxiety and fear [Figures 1 and 2].
Figure 1.
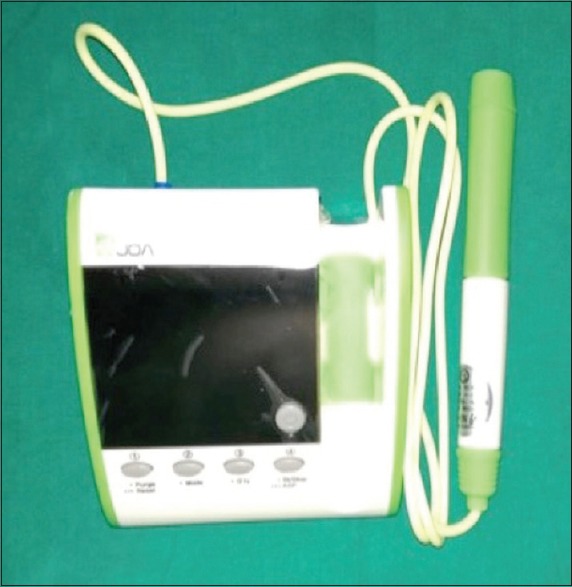
Auto-controlled injection system
Figure 2.

Cartridge containing lidocaine and Septoject disposable sterile needles
Randomization
The recruited children were allocated to one of the following two groups:
Group I (CCIS): Local infiltration of lidocaine hydrochloride 2% with adrenaline 1:80,000, marketed in special cartridge, using compatible disposable 30-gauge, 10 mm needles and auto-controlled injection system.
Group II (Traditional system): Local infiltration of lidocaine hydrochloride 2% with adrenaline 1:80,000, using 30-gauge, 10 mm needle and disposable TS.
The children were randomized to the groups using restricted, permuted block randomization with block sizes of 4 and 6. To prevent selection bias, centralized or third party assignment was used as an allocation concealment mechanism.
Interventions
For all the children, topical anesthetic gel (lignox gel 2% w/v, Warren, India) was applied to the area of injection site and after a waiting period or 1 min, 1 ml of anesthetic solution (lignox 2% A, Warren, India) (2% lignocaine hydrochloride with 1:80,000 adrenaline) was injected (with auto-controlled injection system for Group I children and TS for Group II) by a single investigator (DV) as local infiltrate following routine behavior guidance techniques. After 3 min, extraction of the mandibular primary tooth was performed using standard protocol.[1]
Outcomes
Primary outcome measures considered were as follows:
Face, Legs, Activity, Cry, Consolability (FLACC) Scale: As an observational measure of pain during LA administration, FLACC readings were noted during LA administration
Faces pain scale-Revised (FPS-R): As a self-report measure of pain, FPS-R was recorded after completion of LA administration
Modified Child Dental Anxiety Faces Scale simplified (MCDAS(f)):[2] As a self-report measure of anxiety, MCDAS(f) was noted before starting the procedure and while leaving the dental operatory.
Secondary outcome measures considered were as follows:
Time for administration: The total time taken for administration of the LA solution was noted
FBRS: The behavior of the child during oral examination, intraoral radiography, topical anesthetic application, LA administration, and extraction and departure from dental chair was rated using Wright's modification of FBRS. The ratings during examination, radiography, and topical anesthetic application were summed as “before” values, LA administration as “during” value, and the ratings during extraction and departure from dental chair as “after” values
Pulse rate: The readings of pulse rate were noted from the pulse oximeter device (Gibson Pulse Oximeter, Beijing, China) attached to the left index finger over a period of 15 min before the LA administration. All the variations during that period were recorded, and the mean was calculated. The pulse rate readings during injection of LA and 1 min postinjection period were recorded, and the mean was calculated separately and considered as during and after values.
All the above readings were noted by a trained person not involved in the treatment procedure (RK).
Sample size
Based on the findings of a pilot study (with ten children, five in each group; a sample, not included in the main study and final analysis), with the level of significance set at 0.05, power of 80%, considering the effect size of pilot study and FLACC, FPS-R, and MCDAS(f) scores as primary outcomes, a minimum sample of 49 in each group was calculated.
Statistical analysis
The statistical analysis was carried out using a standard statistical package (SPSS 17.0 for Windows, SPSS Inc., Chicago, USA). The normality of data was assessed using a Shapiro–Wilk test. The distribution of participants to the two groups based on the age, gender, and accompanying person was analyzed using Chi-square test. The intergroup comparisons of metric and ordinal data were carried out using unpaired t-test and Mann–Whitney test, respectively (for both combined and segregated data). The intragroup comparisons of metric and ordinal data were carried out using paired t-test and Wilcoxon signed-rank test, respectively.
RESULTS
Table 1 shows the distribution of participants to CCIS and TS groups during LA administration based on the age, gender, and accompanying person. There was no statistically significant difference in the distribution of participants for any of the considered factors.
Table 1.
Distribution of participants to “computer-controlled injection system” and “traditional syringe” groups during local anesthesia administration based on age, gender, and accompanying person
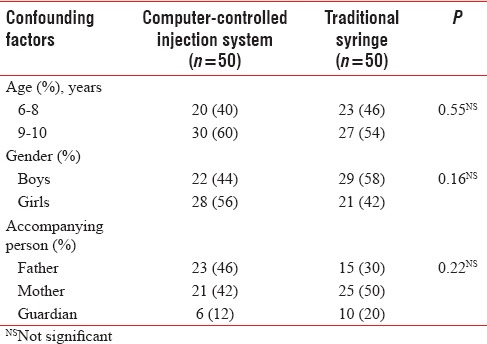
Table 2 demonstrates the comparison of metric outcome (time of administration [TOA], pulse rate, and MCDAS(f)) scores between CCIS and TS groups during LA administration. A statistically significant difference in the TOA was observed with CCIS taking longer time. No statistical difference was observed between the two groups in the pulse rate before initiating LA administration. However, the mean anxiety scores were higher among those randomized to CCIS, which were statistically significant as reported by children in MCDAS(f). The mean pulse rate values and anxiety scores were less in CCIS group, compared to TS group, which were also statistically significant, during and after LA administration.
Table 2.
Comparison of various parameters (metric data) during local anesthesia administration: “Computer-controlled injection system” versus “traditional syringe”
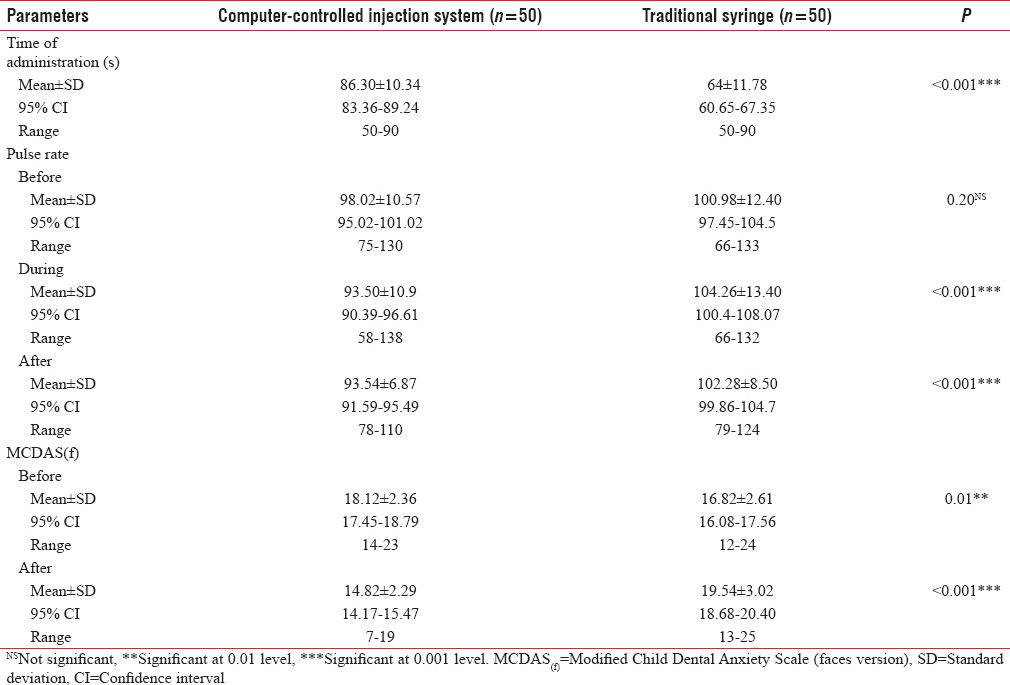
Table 3 illustrates the comparison of ordinal outcomes (scores/ratings on FBRS, FPS-R, and FLACC scores) between CCIS and TS groups during LA administration. There was no significant difference in the FBRS noted between the groups before initiating LA administration and most of the children (mode: Rating 3) were in rating 3 (positive), in both groups. During and after the treatment, most of the children randomized to CCIS were rated as positive (mode: Rating 3) and in TS group as negative (mode: Rating 2). The scores were less in children randomized to CCIS, and the differences were statistically significant in both self-report and observational measures of pain (FPS-R and FLACC).
Table 3.
Comparison of various parameters (ordinal data) during local anesthesia administration: “Computer-controlled injection system” versus “traditional syringe”
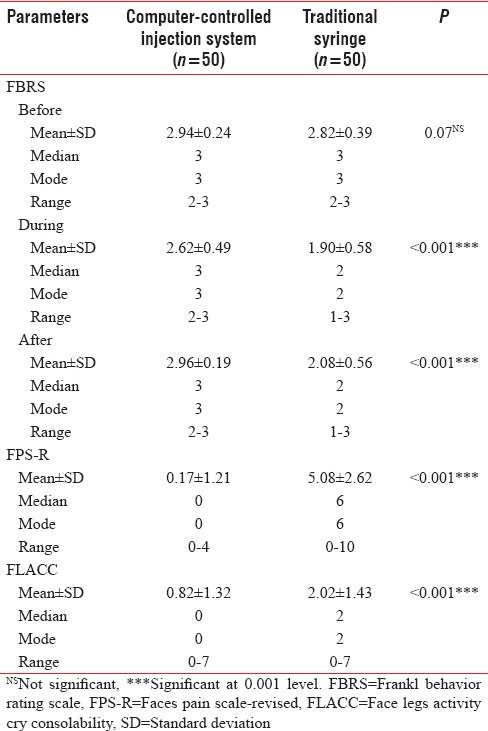
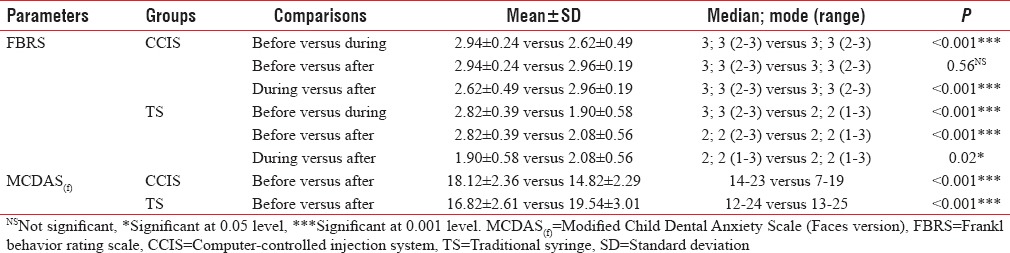
Table 4 depicts intragroup comparison of pulse rate before, during, and after LA administration in CCIS and TS groups. Statistically significant differences in pulse rates recorded were observed (before vs. during, and before vs. after LA administration) in CCIS group (after < during < before) whereas in TS group significant difference was observed only between the before and during values (during > after > before). [Table 5] shows the intragroup comparison of FBRS and MCDAS(f) scores, and significant differences in FBRS were observed (before vs during, and during vs after LA administration) in CCIS group (before, during, after - mode: rating 3, positive), whereas in TS group, differences were significant among all the three (before - mode: rating 3, positive; during and after - mode: rating 2, negative). Significant differences in MCDAS(f) scores were observed between the values reported before and after treatment, in both groups.
Table 4.
Comparison of pulse rate during local anesthesia administration: “Computer-controlled injection system” versus “traditional syringe” - Intragroup
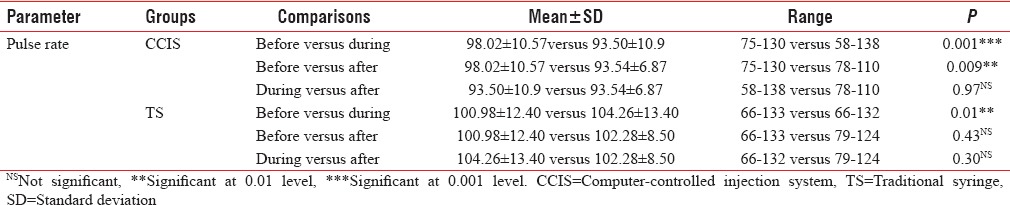
Table 5.
Comparison of various parameters during local anesthesia administration: “Computer-controlled injection system” versus “traditional syringe” - Intragroup
Interpretations based on age and gender
Based on the age (6–8 years vs. 9–10 years), a significant difference was noted only in MCDAS(f) scores in 6–8-year-old children. A significant difference was observed between the groups both before and after LA administration (CCIS group: before > after; TS group: before < after), whereas in 9–10-year-old age group, no significant difference was observed between the groups in the before values; however, there was a difference in the after values (CCIS group: before > after; TS group: before < after).
Based on the gender (boys vs. girls), only difference observed was in anxiety and pain scores. In the MCDAS(f) scores, before starting the treatment, there was a significant difference only among girls, with those randomized to CCIS group showing higher values. In both self-report (FPS-R) and observational (FLACC) measures of pain, although significant differences were observed between the groups irrespective of gender, girls had higher values.
DISCUSSION
Imparting positive dental outlook is very important and the primary means to achieve this is the “painless anesthetic” in children dentistry. Many computer anesthetic systems are marketed, of which much of the reported studies are on Wand®, Quick Sleeper™, Sleeper One™, and Comfort Control Syringe™.[7,9,10,11,12,13,14,15,16,17,18] Wand® has gained popularity; however, clinically the major disadvantages projected with this system are the time taken for LA administration and cost and complexity of the equipment.[10,12,13,16] Hence, the EJOA painless dental anesthetic system (designated as CCIS) was selected as an alternative to Wand®, in the present study, because due to its cost-effectiveness and being user-friendly with reduced complexity. CCIS is a pen-like instrument; however, hand unit itself has the total operating control unlike Wand® that has foot control. This device resembles Comfort Control Syringe™, which has five preprogrammed speeds for different injection techniques, a digital display for time elapsed, and rate and volume of the solution.[7] In the CCIS selected for the study, there are two preprogrammed controls, and in addition, the speed and quantity of the injecting solution can be manually adjusted either in the base unit or handpiece (five levels in both speed and quantity, which can either be increased or decreased) adding a clinical advantage. As the studies with a standard protocol on these simplified versions of Wand® are meager, the present study was performed to assess the effect of this new system in reducing the pain experience of children during LA administration.
As an alternative to IANB, PDL injection with Wand® has been suggested in one study.[19] Further, it was also reported that local infiltration is sufficient for procedures such as restorations and crowns whereas insufficient for lengthy procedures such as pulpotomy in children.[6,21,22,23,24] Hence, infiltration has been suggested as an alternative to IANB, for the restoration of primary teeth in the mandibular arch.[20,24] There is insufficient literature on mandibular infiltrations as an effective alternative to IANBs during extractions. Hence, the present study is an attempt to determine the efficacy of local infiltrations when given using both CCIS and TS. No anesthetic failures or repetition of the LA procedure was observed in either group, which can be attributed to the time spent on injection that is directly proportional to the diffusion of LA solution. Thus, slow injection and short length of the procedure selected might be responsible for the high success rate of the local infiltrations in the present study, as observed by Jones and coworkers.[25]
Pain and anxiety are correlated; highly anxious children can report greater pain and display increased pain-associated behavior to LA injections.[26] To overcome this influence, the present study was restricted to children whose anxiety scores were ≤24 in the Modified Child Dental Anxiety Scale-faces version simplified (MCDAS(f)), reported by the children before starting the treatment. This scale was selected due to its proven authentic measure of dental anxiety in children, with good reliability and validity.[27,28] The simplified version, used in previous studies,[29,30] was applied to obviate some complex questions that were difficult for a child to understand, with an additional advantage of reducing the time taken to record. Before commencing the treatment, a difference in the reported anxiety values was observed between the two groups, with children in CCIS showing higher values. This difference was observed in young children (age range of 6–8 years) and among girls. Thus, girls in the age range of 6–8 years randomized to the computer group showed higher anxiety. A significant further reduction in anxiety was observed in children randomized to CCIS whereas those in TS group showed an increase in the MCDAS(f) values after the procedure. This signifies the lasting positive effect of painless anesthetic system, compared to traditional pricks. A coincidental increase in anxiety was observed, indicated by the elevated values of physiological parameter, pulse rate, in TS group children.
Pain during LA administration was assessed using self-report and observational measures; FLACC scale, a proven valid observational measure in children, was considered due to its simplicity of application in clinical settings, which comprises five behavioral categories: Facial expression, Leg movement, Bodily activity, Cry or verbalization, and Consolability; each rated on a scale of 0–2 to provide a maximum overall pain score of 10.[30,31,32,33,34] To achieve self-report of pain possible on comparable 0–10 metric, FPS-R adapted from the FPS was employed,[35,36] due to ease of administration and absence of smiles and tears in the faces. A statistically significant reduction of pain perception during mandibular infiltration was observed in children randomized to CCIS as evident in both self-report and observational scales, compared to TS. The positivity of painless system was clearly evident in the self-report scale, FPS-R (the mode was 0 in CCIS whereas 6 in TS group), showing the superiority of CCIS in reducing the injection pain. No significant difference in this transcend was observed among different age groups, as well as the gender. This reduction in pain with computer anesthetic systems can be ascribed to the constant flow and slow injection of the solution with the system used. Influence of two different flow rates (slow versus fast) with computer system alone also proved that slow injection rate has significantly less pain, compared to the increased velocity.[37] The solution deposited ahead of the needle tip also might have anesthetized the access path of the needle for injection and the pen grasp of the injector increased preciseness and accuracy of injection. The superiority of computer system observed in the present study is in accordance with other studies related to maxillary buccal and palatal infiltrations, PDL injections, and inferior alveolar blocks using Wand®, which was evident in both self-report and observational scales.[7,10,11,12,16,17] However, the results are in contrast to the findings observed in other studies with no difference reported in the pain experienced on using these computer systems.[13,14,25]
The beneficial aspect of painless system was also noted in the Frankl ratings of the present study. Most of the children were rated as positive initially in both groups; however, the behavior remained positive during and after treatment only in CCIS. This can be ascribed to the physical appearance of the injector, to which children pay more attention. The handpieces of these systems are not syringe shaped and, hence, might have been readily accepted by young patients.[38] Reduction in disruptive behavior of children was also observed in other studies conducted on Wand®, but the potential drawback reported has been prolonged injection time, demanding the cooperation of children. In the present study, the TOA is almost 0.5 times higher in CCIS group than the traditional infiltrations. Although a significant difference in the TOA was observed between CCIS and TS, the mean difference is less, compared to other studies.[10,13,16]
The most convincing part of the present study is that similar gauge needles were selected for both TS and CCIS, whereas in most of the previous studies, dissimilar gauges were used or gauge was not considered, which could have influenced their results.[7,11,12,13,19] The present study also highlighted mandibular infiltration as a potent alternative to IANB. However, the major limitation of the present study is the study design; a split mouth study and comparison with Wand® might have revealed more important findings. Considering only single-needle gauge and excluding children with negative behavior are other limitations. Hence, while generalizing the finding to population, these aspects need consideration.
CONCLUSIONS
The primary objective of instilling a positive attitude in children toward dentistry had been attained with painless anesthetic system in the present study. Computer system created a positive experience not only for the child but also for the practitioner due to the comfort. It acted as a good tool for building positive dentist–child relationship. The study also eliminated the influence of needle gauge as a confounding factor influencing the pain in the studies pertaining to computer-controlled LA systems. The study also demonstrated the possibility of using buccal infiltration instead of IANB in children; however, further research is needed to understand the duration of anesthetic effect and the sufficiency of single injection for lengthier procedures.
Although the present system is cost-effective compared to the Wand®, the usage of it is possible only in commercial setup. For the clinicians, this may be an extra burden and, hence, is not being used in individual clinics. Manufacturers should try to introduce simpler and economical alternatives in the equipment so that these painless anesthetic systems are utilized in clinical setting on a larger scale.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Oosterink FM, de Jongh A, Aartman IH. What are people afraid of during dental treatment? Anxiety-provoking capacity of 67 stimuli characteristic of the dental setting. Eur J Oral Sci. 2008;116:44–51. doi: 10.1111/j.1600-0722.2007.00500.x. [DOI] [PubMed] [Google Scholar]
- 2.Splieth CH, Bünger B, Pine C. Barriers for dental treatment of primary teeth in East and West Germany. Int J Paediatr Dent. 2009;19:84–90. doi: 10.1111/j.1365-263X.2008.00949.x. [DOI] [PubMed] [Google Scholar]
- 3.Paryab M, Hosseinbor M. Dental anxiety and behavioral problems: A study of prevalence and related factors among a group of Iranian children aged 6-12. J Indian Soc Pedod Prev Dent. 2013;31:82–6. doi: 10.4103/0970-4388.115699. [DOI] [PubMed] [Google Scholar]
- 4.Hosey MT, Macpherson LM, Adair P, Tochel C, Burnside G, Pine C. Dental anxiety, distress at induction and postoperative morbidity in children undergoing tooth extraction using general anaesthesia. Br Dent J. 2006;200:39–43. doi: 10.1038/sj.bdj.4813123. [DOI] [PubMed] [Google Scholar]
- 5.Ogle OE, Mahjoubi G. Advances in local anesthesia in dentistry. Dent Clin North Am. 2011;55:481–99, viii. doi: 10.1016/j.cden.2011.02.007. [DOI] [PubMed] [Google Scholar]
- 6.Ram D, Peretz B. Administering local anaesthesia to paediatric dental patients – Current status and prospects for the future. Int J Paediatr Dent. 2002;12:80–9. doi: 10.1046/j.1365-263x.2002.00343.x. [DOI] [PubMed] [Google Scholar]
- 7.Langthasa M, Yeluri R, Jain AA, Munshi AK. Comparison of the pain perception in children using comfort control syringe and a conventional injection technique during pediatric dental procedures. J Indian Soc Pedod Prev Dent. 2012;30:323–8. doi: 10.4103/0970-4388.108931. [DOI] [PubMed] [Google Scholar]
- 8.Friedman MJ, Hochman MN. A 21st century computerized injection system for local pain control. Compend Contin Educ Dent. 1997;18:995. [PubMed] [Google Scholar]
- 9.Hochman M, Chiarello D, Hochman CB, Lopatkin R, Pergola S. Computerized local anesthetic delivery vs. traditional syringe technique. Subjective pain response N Y State Dent J. 1997;63:24–9. [PubMed] [Google Scholar]
- 10.Nusstein J, Berlin J, Reader A, Beck M, Weaver JM. Comparison of injection pain, heart rate increase and post injection pain of articaine and lidocaine in a primary intraligamentary injection administered with a computer-controlled local anesthetic delivery system. Anesth Prog. 2004;51:126–33. [PMC free article] [PubMed] [Google Scholar]
- 11.Özer S, Yaltirik M, Kirli I, Yargic I. A comparative evaluation of pain and anxiety levels in 2 different anesthesia techniques: Locoregional anesthesia using conventional syringe versus intraosseous anesthesia using a computer-controlled system (Quicksleeper) Oral Surg Oral Med Oral Pathol Oral Radiol. 2012;114(5 Suppl):S132–9. doi: 10.1016/j.oooo.2011.09.021. [DOI] [PubMed] [Google Scholar]
- 12.Palm AM, Kirkegaard U, Poulsen S. The wand versus traditional injection for mandibular nerve block in children and adolescents: Perceived pain and time of onset. Pediatr Dent. 2004;26:481–4. [PubMed] [Google Scholar]
- 13.Kandiah P, Tahmassebi JF. Comparing the onset of maxillary infiltration local anaesthesia and pain experience using the conventional technique vs. the Wand in children. Br Dent J. 2012;213:E15. doi: 10.1038/sj.bdj.2012.988. [DOI] [PubMed] [Google Scholar]
- 14.Tahmassebi JF, Nikolaou M, Duggal MS. A comparison of pain and anxiety associated with the administration of maxillary local analgesia with Wand and conventional technique. Eur Arch Paediatr Dent. 2009;10:77–82. doi: 10.1007/BF03321604. [DOI] [PubMed] [Google Scholar]
- 15.Ram D, Kassirer J. Assessment of a palatal approach-anterior superior alveolar (P-ASA) nerve block with the Wand in paediatric dental patients. Int J Paediatr Dent. 2006;16:348–51. doi: 10.1111/j.1365-263X.2006.00752.x. [DOI] [PubMed] [Google Scholar]
- 16.Saloum FS, Baumgartner JC, Marshall G, Tinkle J. A clinical comparison of pain perception to the Wand and a traditional syringe. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;89:691–5. doi: 10.1067/moe.2000.106333. [DOI] [PubMed] [Google Scholar]
- 17.Allen KD, Kotil D, Larzelere RE, Hutfless S, Beiraghi S. Comparison of a computerized anesthesia device with a traditional syringe in preschool children. Pediatr Dent. 2002;24:315–20. [PubMed] [Google Scholar]
- 18.Sixou JL, Marie-Cousin A, Huet A, Hingant B, Robert JC. Pain assessment by children and adolescents during intraosseous anaesthesia using a computerized system (QuickSleeper) Int J Paediatr Dent. 2009;19:360–6. doi: 10.1111/j.1365-263X.2009.00983.x. [DOI] [PubMed] [Google Scholar]
- 19.Oztas N, Ulusu T, Bodur H, Dogan C. The wand in pulp therapy: An alternative to inferior alveolar nerve block. Quintessence Int. 2005;36:559–64. [PubMed] [Google Scholar]
- 20.Salomon E, Mazzoleni S, Sivolella S, Cocilovo F, Gregori D, Giuca MR, et al. Age limit for infiltration anaesthesia for the conservative treatment of mandibular first molars. A clinical study on a paediatric population. Eur J Paediatr Dent. 2012;13(3 Suppl):259–62. [PubMed] [Google Scholar]
- 21.Khalil H. A basic review on the inferior alveolar nerve block techniques. Anesth Essays Res. 2014;8:3–8. doi: 10.4103/0259-1162.128891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Donohue D, Garcia-Godoy F, King DL, Barnwell GM. Evaluation of mandibular infiltration versus block anesthesia in pediatric dentistry. ASDC J Dent Child. 1993;60:104–6. [PubMed] [Google Scholar]
- 23.Oulis CJ, Vadiakas GP, Vasilopoulou A. The effectiveness of mandibular infiltration compared to mandibular block anesthesia in treating primary molars in children. Pediatr Dent. 1996;18:301–5. [PubMed] [Google Scholar]
- 24.Meechan JG, Kanaa MD, Corbett IP, Steen IN, Whitworth JM. Pulpal anaesthesia for mandibular permanent first molar teeth: A double-blind randomized cross-over trial comparing buccal and buccal plus lingual infiltration injections in volunteers. Int Endod J. 2006;39:764–9. doi: 10.1111/j.1365-2591.2006.01144.x. [DOI] [PubMed] [Google Scholar]
- 25.Jones CM, Heidmann J, Gerrish AC. Children's ratings of dental injection and treatment pain, and the influence of the time taken to administer the injection. Int J Paediatr Dent. 1995;5:81–5. doi: 10.1111/j.1365-263x.1995.tb00169.x. [DOI] [PubMed] [Google Scholar]
- 26.Ortiz MI, Rangel-Barragán RO, Contreras-Ayala M, Mora-Alba JD, Gómez-Bonifaz LG, Murguía-Cánovas G, et al. Procedural pain and anxiety in pediatric patients in a Mexican dental clinic. Oral Health Dent Manag. 2014;13:495–501. [PubMed] [Google Scholar]
- 27.Howard KE, Freeman R. Reliability and validity of a faces version of the Modified Child Dental Anxiety Scale. Int J Paediatr Dent. 2007;17:281–8. doi: 10.1111/j.1365-263X.2007.00830.x. [DOI] [PubMed] [Google Scholar]
- 28.Wong HM, Humphris GM, Lee GT. Preliminary validation and reliability of the Modified Child Dental Anxiety Scale. Psychol Rep. 1998;83(3 Pt 2):1179–86. doi: 10.2466/pr0.1998.83.3f.1179. [DOI] [PubMed] [Google Scholar]
- 29.Manepalli S, Nuvvula S, Kamatham R, Nirmala S. Comparative efficacy of a self-report scale and physiological measures in dental anxiety of children. J Investig Clin Dent. 2014;5:301–6. doi: 10.1111/jicd.12046. [DOI] [PubMed] [Google Scholar]
- 30.Nuvvula S, Alahari S, Kamatham R, Challa RR. Effect of audiovisual distraction with 3D video glasses on dental anxiety of children experiencing administration of local analgesia: A randomised clinical trial. Eur Arch Paediatr Dent. 2015;16:43–50. doi: 10.1007/s40368-014-0145-9. [DOI] [PubMed] [Google Scholar]
- 31.Merkel SI, Voepel-Lewis T, Shayevitz JR, Malviya S. The FLACC: A behavioral scale for scoring postoperative pain in young children. Pediatr Nurs. 1997;23:293–7. [PubMed] [Google Scholar]
- 32.Johansson M, Kokinsky E. The COMFORT behavioural scale and the modified FLACC scale in paediatric intensive care. Nurs Crit Care. 2009;14:122–30. doi: 10.1111/j.1478-5153.2009.00323.x. [DOI] [PubMed] [Google Scholar]
- 33.Voepel-Lewis T, Zanotti J, Dammeyer JA, Merkel S. Reliability and validity of the face, legs, activity, cry, consolability behavioral tool in assessing acute pain in critically ill patients. Am J Crit Care. 2010;19:55–61. doi: 10.4037/ajcc2010624. [DOI] [PubMed] [Google Scholar]
- 34.Nilsson S, Finnström B, Kokinsky E. The FLACC behavioral scale for procedural pain assessment in children aged 5-16 years. Paediatr Anaesth. 2008;18:767–74. doi: 10.1111/j.1460-9592.2008.02655.x. [DOI] [PubMed] [Google Scholar]
- 35.Hicks CL, von Baeyer CL, Spafford PA, van Korlaar I, Goodenough B. The Faces Pain Scale-Revised: Toward a common metric in pediatric pain measurement. Pain. 2001;93:173–83. doi: 10.1016/S0304-3959(01)00314-1. [DOI] [PubMed] [Google Scholar]
- 36.Bieri D, Reeve RA, Champion GD, Addicoat L, Ziegler JB. The Faces Pain Scale for the self-assessment of the severity of pain experienced by children: Development, initial validation, and preliminary investigation for ratio scale properties. Pain. 1990;41:139–50. doi: 10.1016/0304-3959(90)90018-9. [DOI] [PubMed] [Google Scholar]
- 37.Primosch RE, Brooks R. Influence of anesthetic flow rate delivered by the Wand local anesthetic system on pain response to palatal injections. Am J Dent. 2002;15:15–20. [PubMed] [Google Scholar]
- 38.Kuscu OO, Akyuz S. Children's preferences concerning the physical appearance of dental injectors. J Dent Child (Chic) 2006;73:116–21. [PubMed] [Google Scholar]


