Abstract
Aims and Objectives:
The aim of this study is to compare the effects of intrathecal levobupivacaine with levobupivacaine and fentanyl in patients undergoing cesarean section.
Methods:
Patients with American Society of Anesthesiologists Physical Status I and II scheduled for cesarean section under spinal anesthesia were randomly allocated with thirty patients each. Group L: levobupivacaine group – thirty patients (10 mg). Group F: levobupivacaine plus fentanyl group – thirty patients (7.5 mg + 12.5 μg). Hemodynamic monitoring, sensory and motor levels, and neonatal Apgar score were noted intraoperatively. The total duration of motor and sensory block, time for rescue analgesia was noted postoperatively.
Results:
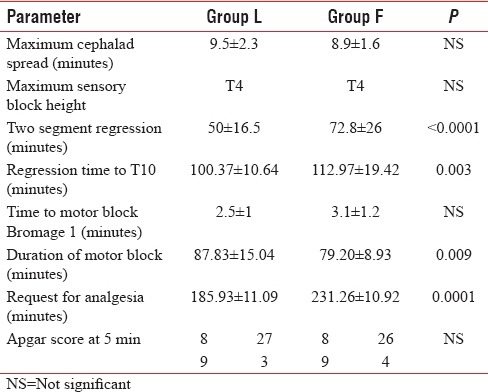
Prolonged duration of postoperative sensory and rescue analgesia was found in Group F – 112.97 ± 19.42, 231.26 ± 10.92 min as compared to Group L – 100.37 ± 10.64, 185.93 ± 11.09 min and duration of motor blockade was prolonged in Group L – 87.83 ± 15.04 min than Group F – 79.20 ± 8.93 min and P < 0.05 was found statistically significant. Apgar scores in both groups were comparable.
Conclusion:
Intrathecal levobupivacaine plus fentanyl prolonged duration of sensory block and rescue analgesia without prolonging motor block which could help in early ambulation.
Keywords: Apgar scores, bupivacaine, fentanyl, levobupivacaine
INTRODUCTION
Hyperbaric bupivacaine is the most common local anesthetic used for spinal anesthesia in parturients undergoing elective cesarean delivery.[1,2] However, compared to other local anesthetics, it has considerable adverse effects on the cardiovascular and central nervous system.[3] Enantiomers may have the same desired pharmacological properties, but fewer side effects. Levobupivacaine, the S(-)-enantiomer of bupivacaine, recently introduced for obstetric spinal and epidural anesthesia[4,5] has been shown to provide a more selective neuraxial blockade than racemic bupivacaine.[6] Often, intrathecal opioids, such as fentanyl or sufentanil, are combined with local anesthetics, thereby markedly enhancing the quality and duration of postoperative analgesia after cesarean delivery as well as providing better parturient comfort without affecting neonatal outcome significantly.[7]
In the postoperative period, prolonging the analgesia is the best way to encourage for early ambulation of patients, but associated prolonged motor blockade caused by neuraxial blockade with long-acting local anesthetic discourages the patients from early ambulation in spite of having adequate analgesia. Hence, many additives such as fentanyl, sufentanil have been administered along with local anesthetic to prolong the sensory blockade without intensifying motor block.
Hence, the above study has been formulated to assess and compare sensory and motor characteristic following spinal anesthesia with a combination of reduced of levobupivacaine (7.5 mg) and fentanyl (12.5 μg) and standard dose of levobupivacaine (10 mg) alone. Thus, to assess the ability of low-dose combination of levobupivacaine and fentanyl to provide prolonged sensory blockade and with a decreased duration of the motor blockade which may help in early ambulation of patients.
METHODS
After the Institutional Review Board approval and written informed consent, sixty parturients fitting the American Society of Anesthesiologists (ASA) Physical Status I and II presenting for elective and emergency cesarean delivery were included in this prospective, randomized, double-blinded study between age group 19 and 40 years, gestational age 37–40 weeks, and height 150–170 cm. Exclusion criteria were as follows: known allergy to local anesthetics or opioids, contraindications to spinal anesthesia, and fetal indications for cesarean delivery and multiple gestations.
To facilitate blinding, the study solutions were prepared by a pharmacist who was not otherwise involved in the study. The preservative-free study drug was diluted to a total volume of 2 ml, containing either 10 mg of levobupivacaine or levobupivacaine 7.5 mg plus fentanyl 12.5 μg. The dose of local anesthetics administered (10 mg) was chosen in accordance with a recent dose-finding study.[6] Neither the anesthesiologist nor the parturient herself was aware of the drugs or dose administered. Randomization of the parturients was performed with sealed envelope technique, in which each treatment allocation was sealed in an individual envelope, and all sixty envelopes were shuffled.
Preloading was done with Ringer's lactate at a rate of 10 ml/kg. In left lateral position using 25-gauge Quincke needle at the L2–L3 or L3–L4 interspace, spinal anesthesia was administered. Heart rate, noninvasive blood pressure, SpO2, and respiratory rate were monitored. Bradycardia and hypotension were treated when heart rate <60 beats/min and mean arterial pressure (MAP) <60 mmHg and treated with intravenous (IV) boluses atropine 0.6 mg and ephedrine 6 mg, respectively. Nausea and vomiting if any treated with injection ondansetron 4 mg IV. Intraoperatively, parameters assessed are time taken for maximal cephalad spread, maximum cephalad level of sensory block, two segment regression time to T10, time to motor block Bromage 1, duration of the motor block, time for rescue analgesia, and Apgar score at 5 min. Postoperative heart rate, noninvasive blood pressure, SpO2, respiratory rate, and side effects (nausea, vomiting, hypotension, and bradycardia) were observed and recorded for every 30 min till 3 h, hourly till 12 h, and then every 4th hourly till 24 h. Data are presented as mean ± standard deviation, median and range or number of parturients where appropriate. Calculation and data analyses were performed using SPSS version 20 (IBM Corp, Armonak, NY, USA). Chi-square test was used to compare nominal categorical data between study groups. Student's t-test has been used to find the significance of study parameters on continuous scale between two groups. Differences were considered to be statistically significant if P < 0.05.
RESULTS
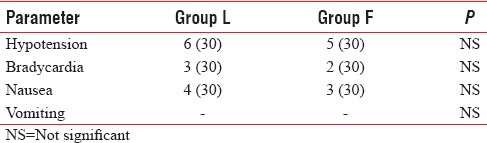
There were no significant differences between the two groups in demographic data, ASA classification, induction to incision time, and duration surgery (P > 0.05) Table 1. Hemodynamic parameters were similar in both groups (P > 0.05) [Figure 1 and Table 2].
Table 1.
Demographic profile and ASA status of patients, Surgical characteristics
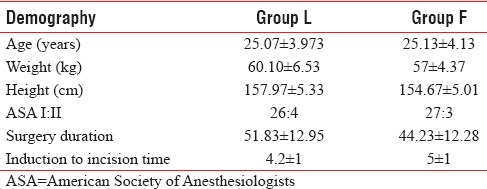
Figure 1.
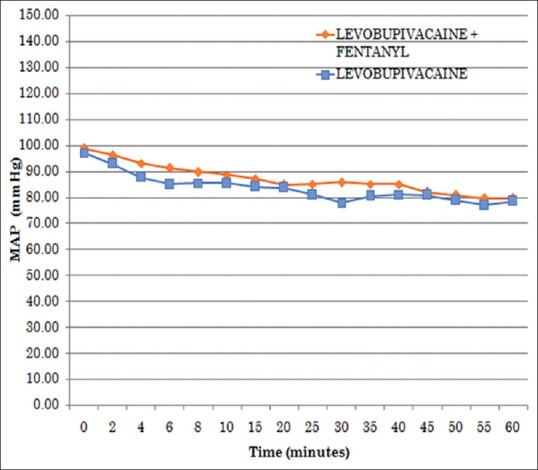
Comparison of mean arterial pressure between two groups
Table 2.
Side-effect profile
There was no statistical difference between the time for maximal cephalad spread and maximum sensory block height (T4). Two-segment regressions, regression time to T10, duration of motor block, and rescue analgesia showed the significant statistical difference. Prolonged duration of postoperative sensory and request for rescue analgesia was found in Group F – 112.97 ± 19.42, 231.26 ± 10.92 min as compared to Group L – 100.37 ± 10.64, 185.93 ± 11.09 min and duration of motor blockade was prolonged in Group L – 87.83 ± 15.04 min than Group F – 79.20 ± 8.93 min. Time to motor blockade (Bromage 1) and Apgar score at 5 min, on the other hand, did not show difference [Table 3].
Table 3.
Sensory and Motor characteristics
DISCUSSION
This study demonstrates that 12.5 μg fentanyl added to 7.5 mg of 0.5% levobupivacaine provides adequate anesthesia which is similar to that obtained from 10 mg of 0.5% levobupivacaine for cesarean section, and the lower dose of local anesthetic used with fentanyl may offer the advantage of shorter duration of motor block.
It has been well documented that a combination of opioids and local anesthetics administered intrathecally has a synergistic analgesic effect.[4,5] Kuusniemi et al. found that the addition of fentanyl 25 μg to 5 mg of bupivacaine for spinal anesthesia resulted in effective anesthesia with motor block of short duration[8] Ben-David et al. found that a small dose of fentanyl (10 μg) added to dilute bupivacaine (3 ml of 0.17% solution) in ambulatory patients undergoing knee arthroscopies intensified and increased the sensory block without increasing the intensity of motor block or prolonging recovery.[9]
Bremerich et al. found that, compared to 7.5 mg levobupivacaine, 10 and 12.5 mg levobupivacaine prolonged the duration of effective analgesia postoperatively (45 vs. 81 and 96 min, respectively).[6] These authors recommended 10 mg levobupivacaine for parturients undergoing elective cesarean section with spinal anesthesia. In our study, the dose used was similar. The lower dose of local anesthetics used with fentanyl may offer the advantage of shorter duration of motor block.
Goel et al. found that fentanyl 12.5 μg added to low-dose bupivacaine 5 mg intrathecally provides better surgical anesthesia and increased the reliability of block than intrathecal fentanyl 7.5 or 10 μg. Hemodynamic stability was the same for all dose combinations used.[10]
Gunusen et al. found that levobupivacaine 7.5 mg plus fentanyl 15 μg was found to be suitable due to the lower incidence of hypotension than when levobupivacaine 10 mg is used.[2]
According to a report by Van Gessel et al., the decrease in MAP was significantly more severe in the hyperbaric (30%) than in the isobaric (18%) or hypobaric (14%) solutions. We used isobaric solution and decrease in MAP was comparable between the two.[11]
Lee et al. compared the clinical efficacy, motor block, and hemodynamic effects of using 2.6 ml of 0.5% levobupivacaine and 2.3 ml of 0.5% levobupivacaine with fentanyl 15 μg during urological surgery and showed that levobupivacaine with fentanyl was as effective as levobupivacaine alone[12] Lee et al. found that the highest level of sensory block was similar between the two groups and the resolution of motor block was faster in the combination group than in the levobupivacaine group, which was similar to our study.
The clinical significance of a reduced duration of motor block resulting from lower dose levobupivacaine plus fentanyl would be early ambulation. Pharmacological profile of levobupivacaine reveals no fetal toxicity. For subarachnoid block, small quantities of levobupivacaine were used and the rate of drug absorption from the subarachnoid space is low, thereby reducing the potential fetal drug load to about 1/10 of that given epidurally. In the present study, neonatal Apgar scores (neonatal outcome) showed no evidence of neonatal depression and limitation of our study being cord blood arterial blood gas was not analyzed.
CONCLUSION
Both regimes are effective. Fentanyl added to levobupivacaine during subarachnoid block offers faster onset of sensory block, prolonged duration of sensory block, and shorter duration of motor blockade; this might help early ambulation as an added advantage over sole levobupivacaine in cesarean section.
Financial support and sponsorship
The study was done in Bangalore Medical College, Bangalore, Karnataka, India.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Bajwa SJ, Kaur J. Clinical profile of levobupivacaine in regional anesthesia: A systematic review. J Anaesthesiol Clin Pharmacol. 2013;29:530–9. doi: 10.4103/0970-9185.119172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gunusen I, Karaman S, Sargin A, Firat V. A randomized comparison of different doses of intrathecal levobupivacaine combined with fentanyl for elective cesarean section: Prospective, double-blinded study. J Anesth. 2011;25:205–12. doi: 10.1007/s00540-011-1097-4. [DOI] [PubMed] [Google Scholar]
- 3.Cuvas O, Basar H, Yeygel A, Turkyilmaz E, Sunay MM. Spinal anesthesia for transurethral resection operations: Levobupivacaine with or without fentanyl. Middle East J Anaesthesiol. 2010;20:547–52. [PubMed] [Google Scholar]
- 4.Bouvet L, Da-Col X, Chassard D, Daléry F, Ruynat L, Allaouchiche B, et al. ED50 and ED95 of intrathecal levobupivacaine with opioids for caesarean delivery. Br J Anaesth. 2011;106:215–20. doi: 10.1093/bja/aeq296. [DOI] [PubMed] [Google Scholar]
- 5.Bremerich DH, Fetsch N, Zwissler BC, Meininger D, Gogarten W, Byhahn C. Comparison of intrathecal bupivacaine and levobupivacaine combined with opioids for caesarean section. Curr Med Res Opin. 2007;23:3047–54. doi: 10.1185/030079907X242764. [DOI] [PubMed] [Google Scholar]
- 6.Bremerich DH, Kuschel S, Fetsch N, Zwissler B, Byhahn C, Meininger D. Levobupivacaine for parturients undergoing elective caesarean delivery. A dose-finding investigation. Anaesthesist. 2007;56:772–9. doi: 10.1007/s00101-007-1201-1. [DOI] [PubMed] [Google Scholar]
- 7.Urbanek B, Kapral S. Levobupivacaine for regional anesthesia. A systematic review. Anaesthesist. 2006;55:296–313. doi: 10.1007/s00101-005-0941-z. [DOI] [PubMed] [Google Scholar]
- 8.Kuusniemi KS, Pihlajamäki KK, Pitkänen MT, Helenius HY, Kirvelä OA. The use of bupivacaine and fentanyl for spinal anesthesia for urologic surgery. Anesth Analg. 2000;91:1452–6. doi: 10.1097/00000539-200012000-00029. [DOI] [PubMed] [Google Scholar]
- 9.Ben-David B, Solomon E, Levin H, Admoni H, Goldik Z. Intrathecal fentanyl with small-dose dilute bupivacaine: Better anesthesia without prolonging recovery. Anesth Analg. 1997;85:560–5. doi: 10.1097/00000539-199709000-00014. [DOI] [PubMed] [Google Scholar]
- 10.Goel S, Bhardwaj N, Grover VK. Intrathecal fentanyl added to intrathecal bupivacaine for day case surgery: A randomized study. Eur J Anaesthesiol. 2003;20:294–7. doi: 10.1017/s0265021503000462. [DOI] [PubMed] [Google Scholar]
- 11.Van Gessel EF, Forster A, Schweizer A, Gamulin Z. Comparison of hypobaric, hyperbaric, and isobaric solutions of bupivacaine during continuous spinal anesthesia. Anesth Analg. 1991;72:779–84. doi: 10.1213/00000539-199106000-00011. [DOI] [PubMed] [Google Scholar]
- 12.Lee YY, Muchhal K, Chan CK, Cheung AS. Levobupivacaine and fentanyl for spinal anaesthesia: A randomized trial. Eur J Anaesthesiol. 2005;22:899–903. doi: 10.1017/S0265021505001523. [DOI] [PubMed] [Google Scholar]


