Abstract
Background and Purpose:
Fusariosis is a fungal infection often involving the skin. Various species can cause local, focally invasive, or disseminated infections. The routes of entry for Fusarium species include the respiratory tract, gastrointestinal tract, toe nails, trauma to the skin, and indwelling central venous catheter.
Case Report:
Herein, we present the case of a 35-year-old woman presenting with interdigital intertrigo. The patient had no predisposing factors and she did not take any antifungal agents. Fusiform macroconidia were observed on the slide culture of the fungus. The etiological agent of the infection was identified as Fusarium oxysporum through sequencing of the translation elongation factor-1 alpha (TEF-1α) gene using the primers EF1 and EF2.
Conclusion:
Fusariosis commonly presents as a severe fungal infection in immunocompromised patients. However, this infection may also occur in immunocompetent patients. Although treatment with amphotericin B is a routine antifungal therapy for fusariosis, many azoles such as cloterimazole can be used topically with fewer side-effects
Key Words: Fusarium oxysporum, Immunocompetent, Interdigital intertrigo infection
Introduction
Fusarium species with a worldwide distribution may be found in plants, air, and soil. Infections caused by Fusarium species often involve the skin. Various species can cause local, focally invasive, or disseminated infections [1]. Localized infections include septic arthritis, osteomyelitis, cystitis, endophthalmitis, and brain abscess. According to the literature, these infections are associated with high morbidity and mortality rates in immunosuppressed patients [2].
Today, Fusarium species represent the second most frequent mold-causing invasive fungal infections in severely immunocompromised patients. The restricted diagnostic tools usually delay the diagnosis and treatment of Fusarium infections. Also, therapy is further complicated by the variable susceptibility of pathogens to antifungal drugs.
The routes of entry for Fusarium species include the respiratory tract, gastrointestinal tract, toe nails (especially among people walking barefoot), trauma to the skin, and indwelling central venous catheter [3-5]. Herein, we present the case of a primary localized cutaneous infection in the interdigital space in a 35-year-old woman. The fungus was identified as Fusarium oxysporum through sequence analysis.
Case report
A 35-year-old woman referred to the Rehnan laboratory for the sampling of an itchy and smelly lesion, located between the web space of the third and fourth toes (Figure 1). The patient had no predisposing factors and she did not take any antifungal agents. The lesion remained localized and no invasion to the adjacent areas or toenails was observed. The patient mentioned a one-month history of the infection.
Figure 1.
An itchy and smelly lesion between the third and fourth toes
Potassium hydroxide (KOH 20%) preparation was applied for skin scrapings, and hyaline septate hyphae were seen on the direct microscopic examination (Figure 2). Subculture was performed on Sabouraud dextrose agar (SDA), SDA supplemented with chloramphenicol and cycloheximide (SCC), and urea agar medium. Growth on SCC was not detected, whereas the urease test was positive (Figure 3).
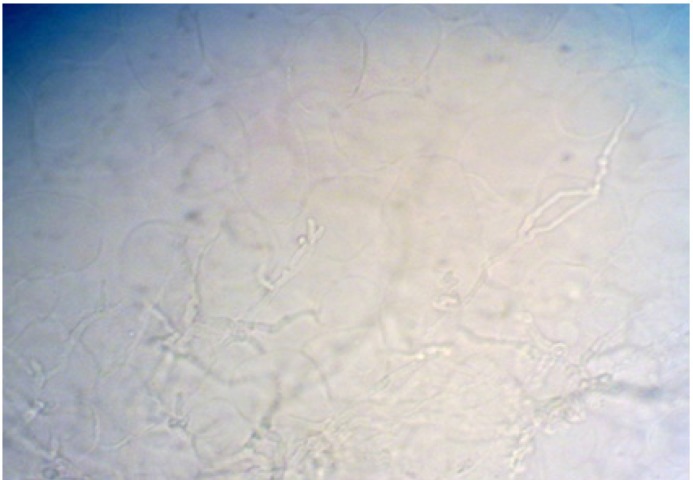
Figure 2.
Hyaline septate hyphae detected via direct microscopic examination
Figure 3.
Growth on Sabouraud dextrose agar (SDA) (left) and positive urease test (right
Fusiform macroconidia were observed on the slide culture of the fungus (Figure 4). Re-sampling was performed after one month, and the findings were similar to the primary analysis. Genomic DNA of the isolate was extracted, and the translation elongation factor-1 alpha (TEF-1α) gene was amplified, using the primers EF1 (5’-ATGGGTAAGGA(A/G)GACAAGAC-3) and EF2 (5’-GGA(G/A)GTACCAGT(G/C)ATCATGTT-3) (Figure 5) [6, 7].
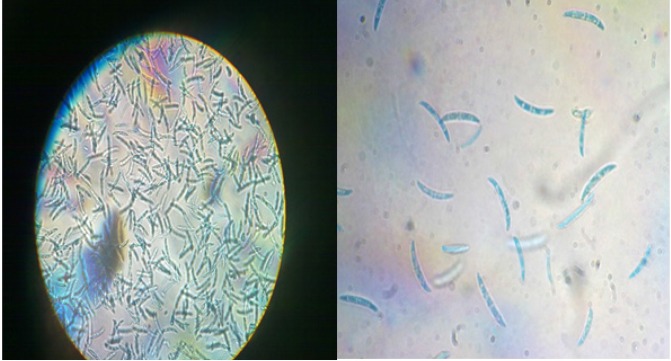
Figure 4.
Fusiform macroconidia
Figure 5.
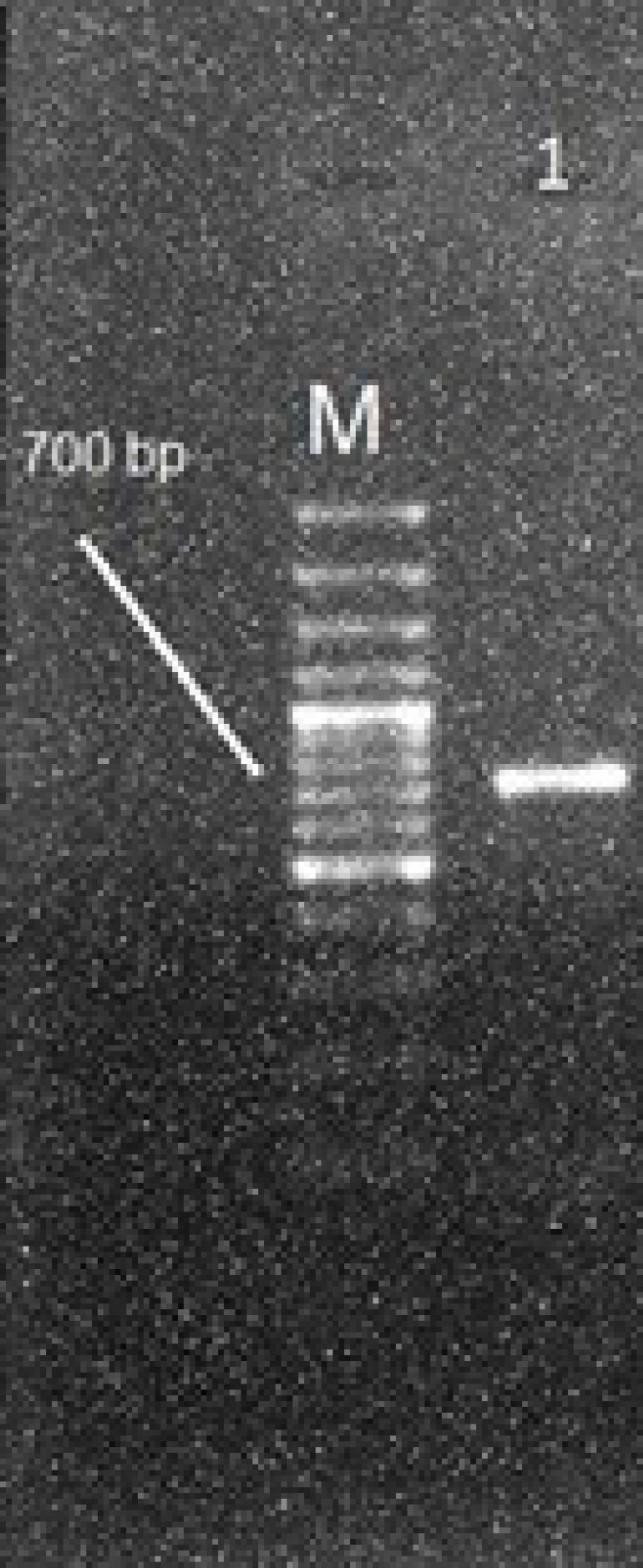
Agarose gel electrophoresis of TEF-1α PCR product of F. oxysporum (lane 1) and a 100 bp DNA size marker (lane M
The PCR product was purified using the ethanol purification method, and cycle-sequencing reactions were performed in the forward direction (Bioneer, Korea). The sequencing product was analyzed with Chromas 2.3 (http://chromas.software.informer.com/2.4/). The results were evaluated, using NCBI Basic Local Alignment Search Tool (BLAST) against fungal sequences available in the DNA database (http://blast.ncbi.nlm.nih.gov/Blast.cgi). Based on the findings, Fusarium oxysporum was identified as the etiological agent of the infection. The patient was treated with clotrimazole 1% twice a day for a period of 20 days (Figure 6).
Figure 6.
The lesion treated by antifungal therapy with clotrimazole 1% over 20 days
Discussion
Some fungi may deteriorate the status of interdigital intertrigo, including dermatophytes (Trichophyton rubrum, Trichophyton mentagrophytes, and Epidermophyton floccosum), yeasts, and molds. Candida species are the most prevalent fungi, associated with intertrigo. The inflammation may begin as a dermatophyte infection, which can damage the stratum corneum and influence the proliferation of other microorganisms, generally antibiotic-resistant bacteria [8].
Fusarium species can act as pathogens in immunosuppressed individuals. These species have been infrequently reported as a cause of disease in immunocompetent people. Fusarium may be a superinfecting fungal agent of deep skin ulcers and surgical wounds [9]. Since the skin may be often the primary source of infection, more attention should be paid to the development of skin lesions and their possible spread.
If a patient has atypical appearing nails, the etiological agent should be determined and proper treatment should be initiated [10]; similarly, topical treatment should be considered for any wound and cutaneous dermatitis. Disseminated infection occurs when two or more sites are involved. The predisposing factors for the infection include hematological malignancies, AIDS, solid tumors, Epstein-Barr infection, and burns [11].
Interdigital intertrigo, caused by Fusarium species, has been rarely reported in the literature. This infection may be a result of walking barefoot or close proximity to the soil infected with the organism [12]. The invasion of F. oxysporum to the moist skin has been reported in a study by English [13]. In addition, Singhal et al. [14] reported skin fusariosis in a 65-year-old agricultural laborer with lesions on his forehead.
Furthermore, Romano et al. [15] reported a case of primary localized cutaneous infection on the first finger of the left hand, caused by F. oxysporum in a 29-year-old woman. If Fusarium infection is confirmed, debridement may be required. Also, oral antifungal therapy with amphotericin B (conventional or lipid formulation) or itraconazole may be essential. It should be noted that the available oral antifungal agents have restricted effectiveness [16]. In this study, clotrimazole 1% was used for treatment; however, the majority of the isolates were resistant to rifampin, flucytosine, and imidazole [17]. On the other hand, significant in vitro activity has been shown for amphotericin B and miconazole [18].
Conclusion
In conclusion, fusariosis commonly presents as a severe and deep fungal infection in immunocompromised patients and is associated with a high mortality rate. However, this infection may also occur in immunocompetent patients and should not be ignored in this population. Although treatment with amphotericin B is a routine antifungal therapy for fusariosis, many azoles such as cloterimazole can be used topically with fewer side-effects.
Acknowledgments
The authors express their appreciation to the Rehnan laboratory personnel.
Author’s contribution
M.B., H.B., P.D. and R.K. performed phenotypic and molecular tests, respectively, and R.M. wrote and analyzed the data of article.
Conflicts of Interest:
The authors declare no conflicts of interest.
Financial disclosure
No financial interests related to content of this article are declared.
References
- 1.Zapater RC, Arrechea A. Mycotic keratitis by Fusarium A review and report of two cases. Ophthalmologica. 1975;170(1):1–12. doi: 10.1159/000307154. [DOI] [PubMed] [Google Scholar]
- 2.Walsh TJ, Hiemenz JW, Anaissie E. Recent progress and current problems in treatment of invasive fungal infections in neutropenic patients. Infect Dis Clin North Am. 1996;10(2):365–400. doi: 10.1016/s0891-5520(05)70303-2. [DOI] [PubMed] [Google Scholar]
- 3.Nakamura Y, Xu X, Saito Y, Tateishi T, Takahashi T, Kawachi Y, et al. Deep cutaneous infection by Fusarium solani in a healthy child: successful treatment with local heat therapy. J Am Acad Dermatol. 2007;56(5):873–7. doi: 10.1016/j.jaad.2006.10.960. [DOI] [PubMed] [Google Scholar]
- 4.Pereiro M Jr, Abalde MT, Zulaica A, Caeiro JL, Flórez A, Peteiro C, et al. Chronic infection due to Fusarium oxysporum mimicking lupus vulgaris: case report and review of cutaneous involvement in fusariosis. Acta Derm Venereol. 2001;81(1):51–3. doi: 10.1080/000155501750208218. [DOI] [PubMed] [Google Scholar]
- 5.Taj-Aldeen SJ, Gene J, Al Bozom I, Buzina W, Cano JF, Guarro J. Gangrenous necrosis of the diabetic foot caused by Fusarium acutatum. Med Mycol. 2006;44(6):547–52. doi: 10.1080/13693780500543246. [DOI] [PubMed] [Google Scholar]
- 6.Kristensen R, Torp M, Kosiak B, Holst-Jensen A. Phylogeny and toxigenic potential is correlated in Fusarium species as revealed by partial translation elongation factor 1 alpha gene sequences. Mycol Res. 2005;109 (Pt 2):173–86. doi: 10.1017/s0953756204002114. [DOI] [PubMed] [Google Scholar]
- 7.Silva FP, Vechiato MH, Harakava R. EF-1α gene and IGS rDNA sequencing of Fusarium oxysporum f sp vasinfectum and F oxysporum f sp phaseoli reveals polyphyletic origin of strains. Trop Plant Pathol. 2014;39(1):64–73. [Google Scholar]
- 8.Janniger CK, Schwartz RA, Szepietowski JC, Reich A. Intertrigo and common secondary skin infections. Am Famil Physician. 2005;72(5):833–8. [PubMed] [Google Scholar]
- 9.English MP. Observations on strains of Fusarium solani, F oxysporum and Candida parapsilosis from ulcerated legs. Sabouraudia. 1972;10(1):35–42. [PubMed] [Google Scholar]
- 10.Arrese JE, Piérard-Franchimont C, Piérard GE. Fatal hyalohyphomycosis following Fusarium onychomycosis in an immunocompromised patient. Am J Dermatopathol. 1996;18(2):196–8. doi: 10.1097/00000372-199604000-00014. [DOI] [PubMed] [Google Scholar]
- 11.Martino P, Gastaldi R, Raccah R, Girmenia C. Clinical patterns of Fusarium infections in immunocompromised patients. J Infect. 1994;28(Suppl 1):7–15. doi: 10.1016/s0163-4453(94)95911-0. [DOI] [PubMed] [Google Scholar]
- 12.Romano C, Miracco C, Difonzo EM. Skin and nail infections due to Fusarium oxysporum in Tuscany, Italy. Mycoses. 1998;41(9-10):433–7. doi: 10.1111/j.1439-0507.1998.tb00369.x. [DOI] [PubMed] [Google Scholar]
- 13.English MP. Invasion of the skin by filamentous non-dermatophyte fungi. Br J Dermatol. 1968;80(5):282–6. doi: 10.1111/j.1365-2133.1968.tb12300.x. [DOI] [PubMed] [Google Scholar]
- 14.Singhal KV, Saoji V, Saoji SV. Fusarium skin infection: a case report. Dermatol Online J. 2011;18(4):6. [PubMed] [Google Scholar]
- 15.Romano C, Caposciutti P, Ghilardi A, Miracco C, Fimiani M. A case of primary localized cutaneous infection due to Fusarium oxysporum. Mycopathologia. 2010;170(1):39–46. doi: 10.1007/s11046-010-9290-9. [DOI] [PubMed] [Google Scholar]
- 16.Gupta AK, Baran R, Summerbell RC. Fusarium infections of the skin. Curr Opin Infect Dis. 2000;13(2):121–8. doi: 10.1097/00001432-200004000-00005. [DOI] [PubMed] [Google Scholar]
- 17.Guarro J, Gene J. Opportunistic fusarial infections in humans. Eur J Clin Microbiol Infect Dis. 1995;14(9):741–54. doi: 10.1007/BF01690988. [DOI] [PubMed] [Google Scholar]
- 18.Sekhon A, Padhye AA, Garg AK, Ahmad H, Moledina N. In vitro sensitivity of medically significant Fusarium species to various antimycotics. Chemotherapy. 1994;40(4):239–44. doi: 10.1159/000239199. [DOI] [PubMed] [Google Scholar]