Abstract
Background:
Unplanned readmissions have become an important quality indicator, particularly for reimbursement; thus, accurate assessment of readmission frequency and risk factors for readmission is critical. The purpose of this study was to determine (1) the frequency of and (2) risk factors for readmissions for all causes or procedure-specific complications within 30 days after total knee arthroplasty (TKA) as well as (3) the association between hospital volume and readmission rate.
Methods:
The Statewide Planning and Research Cooperative System (SPARCS) database from the New York State Department of Health was used to identify 377,705 patients who had undergone primary TKA in the period from 1997 to 2014. Preoperative diagnoses, comorbidities, and postoperative complications were determined using International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes. Readmission was defined as all-cause, due to complications considered by the Centers for Medicare & Medicaid Services (CMS) to be TKA-specific, or due to an expanded list of TKA-specific complications based on expert opinion. Multivariable logistic regression analysis was utilized to determine the independent predictors of readmission within 30 days after surgery.
Results:
There were 22,076 all-cause readmissions—a rate of 5.8%, with a median rate of 3.9% (interquartile range [Q1, Q3] = 1.1%, 7.2%]) among the hospitals—within 30 days after discharge. Of these, only 11% (0.7% of all TKAs) were due to complications considered to be TKA-related by the CMS whereas 31% (1.8% of all TKAs) were due to TKA-specific complications on the expanded list based on expert opinion. Risk factors for TKA-specific readmissions based on the expanded list of criteria included an age of >85 years (odds ratio [OR] = 1.32, 95% confidence interval [CI] = 1.15 to 1.52), male sex (OR = 1.41, 95% CI = 1.34 to 1.49), black race (OR = 1.24, 95% CI = 1.14 to 1.34), Medicaid coverage (OR = 1.40, 95% CI = 1.26 to 1.57), and comorbidities. Several comorbid conditions contributed to the all-cause but not the TKA-specific readmission risk. Very low hospital volume (<90 cases per year) was associated with a higher readmission risk.
Conclusions:
The frequency of readmissions for TKA-specific complications was low relative to the frequency of all-cause readmissions. Reasons for hospital readmission are multifactorial and may not be amenable to simple interventions. Health-care-quality measurement of readmission rates should be calculated and risk-adjusted on the basis of procedure-specific criteria.
Level of Evidence:
Therapeutic Level IV. See Instructions for Authors for a complete description of levels of evidence.
In 2012, the Affordable Care Act established the Hospital Readmissions Reduction Program, which requires the Centers for Medicare & Medicaid Services (CMS) to reduce payments to hospitals with excess readmissions within 30 days after discharge1. Approximately 75% of all hospitals in the program will be subject to a payment reduction of 0.01% to 3%, with the fines expected to amount to approximately $420 million in 2016, according to Medicare estimates2,3.
Penalizing hospitals for readmissions to achieve cost containment is not ideal. Penalizing them for all-cause readmissions without discriminating between those related and those unrelated to the index procedure is particularly problematic, but there is no consensus regarding which particular diagnoses should be considered procedure-specific. A lack of reliability of the collected data3 as well as medicolegal and financial incentives to admit patients especially when surgery was performed in a different hospital are also limitations of this measure4. Furthermore, it remains uncertain whether readmission risk factors can be addressed in a manner that benefits patients5.
Limitations of previous studies on readmission after total knee arthroplasty (TKA) within 30 days include the use of a single hospital database, a lack of information about the reasons for readmission, and the lack of stratification of readmissions according to comorbidities6-16. These limitations are important when studying readmission rates because an estimated 18% of patients are readmitted to a hospital other than the one at which they had the surgery17 and patients have different risks based on their comorbidity profile13,18-20.
The purpose of this study was to use a large, statewide database to determine (1) the frequency and (2) the risk factors for readmissions for all causes or for procedure-specific complications within 30 days after TKA as well as (3) the association between hospital volumes and readmission rates.
Materials and Methods
Study Design and Setting
The Statewide Planning and Research Cooperative System (SPARCS) database from the New York State (NY State) Department of Health was used to identify our patient cohort. Established in 1979, SPARCS collects hospital discharge information, including patient demographics, diagnoses and treatments, services, and charges for every non-federal-hospital discharge, ambulatory surgery case, and emergency department visit in NY State. State regulations require that inpatient data be submitted according to a designated format and schedule by all facilities certified for inpatient care.
Study Subjects
International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) procedure codes were used to identify 382,603 residents of NY State who underwent elective primary TKA (ICD-9-CM code 81.51) between January 1, 1997, and November 30, 2014, for the diagnosis of osteoarthritis, inflammatory arthritis, or osteonecrosis. Patients were excluded if the indication for the original surgery was considered nonelective (neoplasm, fracture, congenital condition, infectious condition, or other); the admission included a concurrent total hip arthroplasty, revision total hip arthroplasty or TKA, or hip resurfacing procedure; >2 TKA procedures were coded during the index hospitalization; hospital discharge was against medical advice; or there was a lack of complete information. This left 377,705 patients eligible for study.
Variables, Outcome Measures, Data Sources, and Bias
We evaluated the frequency of readmissions, within 30 days after the primary TKA, that were due to any diagnosis (all-cause readmissions), due to any of the 8 diagnoses that the CMS considers to be TKA-specific complications2 (see Appendix), and due to a complication on an expanded list that included 22 additional diagnoses considered to be TKA-specific complications in a recent publication21 (see Appendix). The potential risk factors for readmission that we evaluated included demographic characteristics, comorbidities, complications during the index procedure, length of the hospital stay, and discharge disposition. Diagnosis codes in all of the secondary diagnosis fields were used to identify comorbidities based on the Elixhauser Comorbidity Index22. We considered a risk factor to differ between readmission categories if the upper bound of the 95% confidence interval (CI) for the risk factor using one definition of readmission did not overlap with the lower bound of the 95% CI for that same risk factor using a different definition of readmission.
Hospital Volume
Hospitals that performed no TKAs were excluded. To determine the association between hospital volume and the risk of readmission after TKA, we divided hospitals into 4 volume strata that we had previously identified to be associated with distinct risk levels for post-TKA complications and mortality in NY State hospitals23. The thresholds, calculated by applying stratum-specific likelihood ratio (SSLR) analysis to receiver operating characteristic curves, were ≤89, 90 to 235, 236 to 644, and ≥645 TKAs per year23.
Statistical Analysis
Descriptive statistics were calculated for all variables. Independent samples t tests and Pearson chi-square analysis were used for bivariate comparisons. Multivariable analysis was conducted using logistic regression in order to examine the risk-adjusted association between the tested variables and readmission to the hospital. The C-statistic was calculated to estimate the predictive value of our regression model. Odds ratios (ORs) were calculated with their respective 95% CIs, and significance was assigned at the p < 0.05 level. All statistical analyses were performed using SAS 9.3 for Windows software.
Results
Of 377,705 patients who had undergone TKA and were eligible for 30-day follow-up, 22,076 (5.8%) had been readmitted to the hospital for any cause (Table I). From 1997 to 2014, the annual all-cause readmission rates among the hospitals ranged from 0% to 100% (interquartile range [Q1, Q3] = 1.1%, 7.2%), with a median of 3.9%. The all-cause readmissions were due to 918 diagnoses not included in either the CMS or expanded list of TKA-specific complications as well as to the TKA-specific diagnoses on those lists (see Appendix).
TABLE I.
Frequency of All-Cause and TKA-Specific Readmissions 30 Days After TKA in NY State Between January 1, 1997, and November 30, 2014
| 30-Day Readmission Rate |
|||
| Type of Readmission* | No. of Readmissions | % of All-Cause Readmissions | % (95% CI) of all TKAs ( N = 377,705) |
| CMS TKA-specific† | 2,449 | 11.1 | 0.65 (0.62, 0.67) |
| Expanded TKA-specific‡ | 6,784 | 30.7 | 1.80 (1.75, 1.84) |
| All-cause§ | 22,076 | 100.0 | 5.84 (5.77, 5.92) |
Readmission categories are not mutually exclusive.
Readmissions due to any of 8 diagnoses designated by the CMS as TKA-specific complications (see Appendix).
Readmissions due to a diagnosis on an expanded list of TKA-specific complications, including 22 additional TKA-specific complications selected by a group of experts (see Appendix).
Readmissions due to all causes, including 918 conditions not included in the CMS-defined or expanded list of TKA-specific complications (see Appendix).
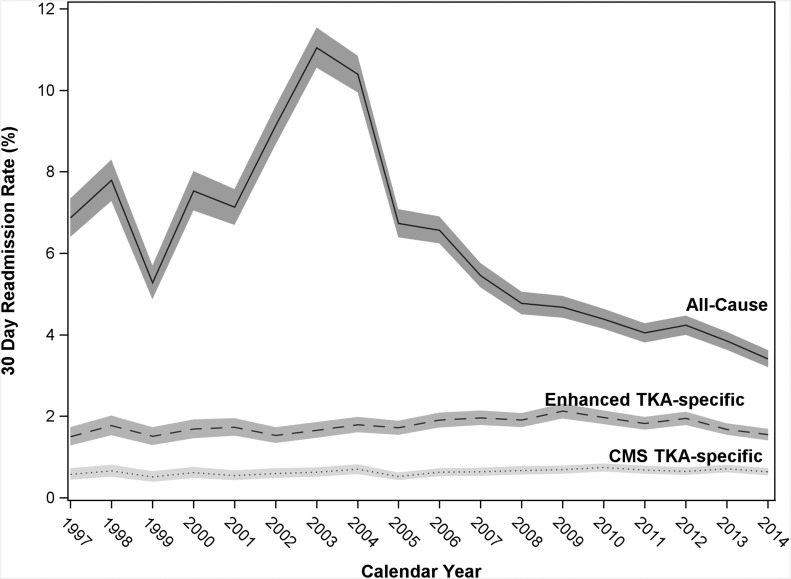
Readmissions due to CMS TKA-specific criteria accounted for only 11% (2,449) of all readmissions at 30 days, whereas readmissions due to the TKA-specific criteria on the expanded list comprised 31% (6,784) of all readmissions at 30 days (Table I). Whereas all-cause readmission rates declined significantly during the study period, those for TKA-specific complications were relatively unchanged and the rates of readmission differed significantly according to the criteria used to define them, with no overlap in CIs (Fig. 1). We also considered readmissions within 90 days but found that 71% of readmissions due to CMS-defined TKA-specific complications and 66% of those due to complications on the expanded list occurred within 30 days.
Fig. 1.
Readmission rates after TKA for all causes (solid line), for TKA-specific causes on the expanded list (dashed line [Enhanced]), and for CMS-defined TKA-specific causes (dotted line) were plotted against the year of readmission from 1997 to 2014 using the SPARCS NY State database as described in the Materials and Methods section. The shaded areas indicate the 95% CIs. The diagnoses defined as TKA-specific by the CMS and the expanded list of diagnoses defined as TKA-specific by an expert panel are shown in the Appendix.
Revision TKA, which is included on the expanded list of TKA-specific criteria for readmission, but is not a CMS criterion, was the reason for readmission of 635 (0.2%) of the patients.
Our initial analysis revealed several differences between the baseline characteristics of patients who were readmitted for any cause and those who were not readmitted (Tables II and III). Our multivariable regression model was able to predict 69% of all-cause readmissions (Tables IV and V). Older patients (>75 years of age) and male patients had a higher risk of readmission independent of other risk factors. Other factors associated with an increased risk of readmission for any cause were Medicare insurance (compared with private insurance), any complication during the index procedure, a longer hospital stay, discharge to another facility instead of home, bilateral TKA, and many comorbidities. Whether patients had undergone the TKA for osteoarthritis, inflammatory arthritis, or osteonecrosis did not affect the readmission risk.
TABLE II.
Characteristics of Patients with All-Cause or TKA-Specific Readmission 30 Days After TKA
| 30-Day Readmissions* |
||||
| Patient Characteristics | CMS TKA-Specific† (N = 2,449) | Expanded TKA-Specific‡ (N = 6,784) | All-Cause§ (N = 22,076) | No Readmission (N = 355,629) |
| Age (yr) | ||||
| Mean ± stand. dev. | 67.6 ± 11.0 | 67.4 ± 11.1 | 69.2 ± 10.5 | 66.8 ± 10.3 |
| Median | 68 | 68 | 70 | 67 |
| Q1, Q3 | 60, 76 | 60, 76 | 62, 77 | 60, 74 |
| Sex (no. [%]) | ||||
| Male | 965 (39.4%) | 2,748 (40.5%) | 8,154 (36.9%) | 120,026 (33.8%) |
| Female | 1,484 (60.6%) | 4,036 (59.5%) | 13,922 (63.1%) | 235,603 (66.2%) |
| Race/ethnicity (no. [%]) | ||||
| White | 1,814 (74.1%) | 4,965 (73.2%) | 16,619 (75.3%) | 267,516 (75.2%) |
| Black | 265 (10.8%) | 736 (10.8%) | 1,983 (9.0%) | 32,226 (9.1%) |
| Hispanic | 139 (5.7%) | 456 (6.7%) | 1,122 (5.1%) | 20,644 (5.8%) |
| Asian | 20 (0.8%) | 72 (1.1%) | 197 (0.9%) | 4,930 (1.4%) |
| Other | 129 (5.3%) | 348 (5.1%) | 876 (4.0%) | 18,123 (5.1%) |
| Missing | 82 (3.3%) | 207 (3.1%) | 1,279 (5.8%) | 12,190 (3.4%) |
| Insurance status (no. [%]) | ||||
| Medicare | 1,472 (60.1%) | 4,022 (59.3%) | 14,233 (64.5%) | 195,339 (54.9%) |
| Medicaid | 147 (6.0%) | 429 (6.3%) | 856 (3.9%) | 16,468 (4.6%) |
| Private | 685 (28.0%) | 1,920 (28.3%) | 5,975 (27.1%) | 121,482 (34.2%) |
| Workers’ Compensation | 91 (3.7%) | 272 (4.0%) | 651 (2.9%) | 14,316 (4.0%) |
| Other | 54 (2.2%) | 141 (2.1%) | 361 (1.6%) | 8,024 (2.3%) |
| Surgical indication (no. [%]) | ||||
| Osteoarthritis | 2,282 (93.2%) | 6,364 (93.8%) | 20,705 (93.8%) | 336,094 (94.5%) |
| Inflammatory arthritis | 146 (6.0%) | 370 (5.5%) | 1,205 (5.5%) | 17,333 (4.9%) |
| Osteonecrosis | 21 (0.9%) | 50 (0.7%) | 166 (0.8%) | 2,202 (0.6%) |
| Bilateral TKA (no. [%]) | 144 (5.9%) | 269 (4.0%) | 2,291 (10.4%) | 18,751 (5.3%) |
| In-hospital complications (no. [%]) | ||||
| Medical | 226 (9.2%) | 470 (6.9%) | 1,413 (6.4%) | 9,404 (2.6%) |
| Surgical | 164 (6.7%) | 336 (5.0%) | 798 (3.6%) | 6,456 (1.8%) |
| Length of hospital stay (days) | ||||
| Mean ± stand. dev. | 4.9 ± 4.3 | 4.7 ± 3.9 | 4.8 ± 3.3 | 4.1 ± 2.4 |
| Median | 4 | 4 | 4 | 3 |
| Q1, Q3 | 3, 5 | 3, 5 | 3, 5 | 3, 5 |
| Discharge disposition (no. [%]) | ||||
| Home | 948 (38.7%) | 2,795 (41.2%) | 5,388 (24.4%) | 153,069 (43.0%) |
| Short-term hospital | 197 (8.0%) | 376 (5.5%) | 1,037 (4.7%) | 5,285 (1.5%) |
| Skilled nursing facility | 900 (36.7%) | 2,726 (40.2%) | 6,219 (28.2%) | 110,916 (31.2%) |
| Rehabilitation facility | 212 (8.7%) | 437 (6.4%) | 4,426 (20.0%) | 50,852 (14.3%) |
| Other facility | 192 (7.8%) | 450 (6.6%) | 5,006 (22.7%) | 35,507 (10.0%) |
Readmission categories are not mutually exclusive.
Readmissions due to any of 8 diagnoses designated by the CMS as TKA-specific complications (see Appendix).
Readmissions due to a diagnosis on an expanded list of TKA-specific complications, including 22 additional TKA-specific complications selected by a group of experts (see Appendix).
Readmissions due to all causes, including 918 conditions not included in the CMS-defined or expanded list of TKA-specific complications (see Appendix).
TABLE III.
Comorbidities of Patients with All-Cause or TKA-Specific Readmission 30 Days After TKA
| 30-Day Readmissions*
(no. [%]) |
||||
| Elixhauser Comorbidity Measure | CMS TKA-Specific† (N = 2,449) | Expanded TKA-Specific‡ (N = 6,784) | All-Cause§ (N = 22,076) | No Readmission (N = 355,629) |
| Congestive heart failure | 94 (3.8%) | 259 (3.8%) | 776 (3.5%) | 5,928 (1.7%) |
| Valvular disease | 131 (5.3%) | 331 (4.9%) | 1,395 (6.3%) | 15,570 (4.4%) |
| Pulmonary circulation disorder | 37 (1.5%) | 69 (1.0%) | 205 (0.9%) | 2,016 (0.6%) |
| Peripheral vascular disorder | 58 (2.4%) | 163 (2.4%) | 510 (2.3%) | 5,773 (1.6%) |
| Paralysis | 7 (0.3%) | 15 (0.2%) | 47 (0.2%) | 511 (0.1%) |
| Other neurological disorder | 73 (3.0%) | 218 (3.2%) | 610 (2.8%) | 7,914 (2.2%) |
| Chronic pulmonary disease | 418 (17.1%) | 1,257 (18.5%) | 3,568 (16.2%) | 48,380 (13.6%) |
| Diabetes | 558 (22.8%) | 1,505 (22.2%) | 4,560 (20.7%) | 66,810 (18.8%) |
| Hypothyroidism | 333 (13.6%) | 893 (13.2%) | 2,872 (13.0%) | 47,296 (13.3%) |
| Renal failure | 108 (4.4%) | 258 (3.8%) | 716 (3.2%) | 7,121 (2.0%) |
| Liver disease | 23 (0.9%) | 88 (1.3%) | 205 (0.9%) | 2,627 (0.7%) |
| Peptic ulcer disease excluding bleeding | 9 (0.4%) | 28 (0.4%) | 120 (0.5%) | 1,370 (0.4%) |
| Lymphoma | 5 (0.2%) | 13 (0.2%) | 41 (0.2%) | 304 (0.1%) |
| Metastatic cancer | 0 (0.0%) | 0 (0.0%) | 10 (0.0%) | 93 (0.0%) |
| Solid tumor without metastasis | 50 (2.0%) | 126 (1.9%) | 694 (3.1%) | 6,549 (1.8%) |
| Rheumatoid arthritis/collagen vascular disease | 137 (5.6%) | 353 (5.2%) | 1,130 (5.1%) | 16,454 (4.6%) |
| Coagulopathy | 42 (1.7%) | 110 (1.6%) | 279 (1.3%) | 3,181 (0.9%) |
| Obesity | 492 (20.1%) | 1,251 (18.4%) | 3,388 (15.3%) | 59,300 (16.7%) |
| Weight loss | 5 (0.2%) | 10 (0.1%) | 21 (0.1%) | 305 (0.1%) |
| Fluid and electrolyte disorders | 70 (2.9%) | 187 (2.8%) | 579 (2.6%) | 7,556 (2.1%) |
| Chronic blood loss anemia | 9 (0.4%) | 23 (0.3%) | 73 (0.3%) | 854 (0.2%) |
| Deficiency anemia | 181 (7.4%) | 499 (7.4%) | 1,628 (7.4%) | 21,774 (6.1%) |
| Alcohol abuse | 20 (0.8%) | 63 (0.9%) | 160 (0.7%) | 2,204 (0.6%) |
| Drug abuse | 17 (0.7%) | 50 (0.7%) | 93 (0.4%) | 1,296 (0.4%) |
| Psychoses | 36 (1.5%) | 119 (1.8%) | 316 (1.4%) | 3,975 (1.1%) |
| Depression | 303 (12.4%) | 788 (11.6%) | 2,057 (9.3%) | 33,386 (9.4%) |
| Hypertension (uncomplicated and complicated combined) | 1,633 (66.7%) | 4,442 (65.5%) | 14,185 (64.3%) | 222,516 (62.6%) |
Readmission categories are not mutually exclusive.
Readmissions due to any of 8 diagnoses designated by the CMS as TKA-specific complications (see Appendix).
Readmissions due to a diagnosis on an expanded list of TKA-specific complications, including 22 additional TKA-specific complications selected by a group of experts (see Appendix).
Readmissions due to all causes, including 918 conditions not included in the CMS-defined or expanded list of TKA-specific complications (see Appendix).
TABLE IV.
Risk of All-Cause or TKA-Specific Readmission 30 Days After TKA Based on Patient Characteristics (N = 377,705)
| 30-Day Readmissions* |
||||||
| CMS TKA-Specific† (N = 2,449; C-Statistic = 0.66) |
Expanded TKA-Specific‡ (N = 6,784; C-Statistic = 0.66) |
All-Cause§ (N = 22,076; C-Statistic = 0.69) |
||||
| OR (95% CI) | P Value | OR (95% CI) | P Value | OR (95% CI) | P Value | |
| Age group (vs. <65 yr) | ||||||
| 65-75 yr | 0.78 (0.69, 0.89) | <0.001 | 0.84 (0.78, 0.91) | <0.001 | 0.98 (0.94, 1.03) | 0.460 |
| 76-85 yr | 0.94 (0.82, 1.08) | 0.394 | 1.01 (0.93, 1.10) | 0.792 | 1.25 (1.19, 1.31) | <0.001 |
| >85 yr | 1.28 (1.02, 1.61) | 0.032 | 1.32 (1.15, 1.52) | <0.001 | 1.67 (1.54, 1.80) | <0.001 |
| Sex | ||||||
| Male vs. female | 1.34 (1.23, 1.46) | <0.001 | 1.41 (1.34, 1.49) | <0.001 | 1.26 (1.22, 1.30) | <0.001 |
| Race/ethnicity (vs. white) | ||||||
| Black | 1.20 (1.05, 1.37) | 0.009 | 1.24 (1.14, 1.34) | <0.001 | 0.99 (0.94, 1.04) | 0.583 |
| Hispanic | 1.00 (0.84, 1.20) | 0.979 | 1.18 (1.07, 1.30) | 0.001 | 0.93 (0.87, 0.99) | 0.029 |
| Asian | 0.65 (0.42, 1.02) | 0.060 | 0.86 (0.68, 1.09) | 0.216 | 0.65 (0.56, 0.75) | <0.001 |
| Other | 1.03 (0.85, 1.23) | 0.790 | 1.02 (0.91, 1.14) | 0.695 | 0.82 (0.76, 0.88) | <0.001 |
| Missing | 1.15 (0.92, 1.44) | 0.230 | 1.08 (0.93, 1.24) | 0.308 | 1.62 (1.52, 1.72) | <0.001 |
| Insurance status (vs. private) | ||||||
| Medicare | 1.31 (1.16, 1.49) | <0.001 | 1.26 (1.17, 1.36) | <0.001 | 1.10 (1.05, 1.15) | <0.001 |
| Medicaid | 1.40 (1.16, 1.69) | <0.001 | 1.40 (1.26, 1.57) | <0.001 | 0.94 (0.87, 1.02) | 0.119 |
| Workers’ Compensation | 1.07 (0.86, 1.33) | 0.551 | 1.10 (0.97, 1.25) | 0.142 | 0.90 (0.83, 0.98) | 0.015 |
| Other | 1.20 (0.90, 1.58) | 0.214 | 1.09 (0.92, 1.30) | 0.313 | 0.86 (0.77, 0.96) | 0.007 |
| Bilateral TKA | 1.22 (1.02, 1.45) | 0.028 | 0.89 (0.79, 1.01) | 0.080 | 1.63 (1.55, 1.71) | <0.001 |
| In-hospital complications | ||||||
| Medical | 2.31 (1.99, 2.68) | <0.001 | 1.85 (1.67, 2.05) | <0.001 | 1.67 (1.57, 1.78) | <0.001 |
| Surgical | 2.70 (2.28, 3.20) | <0.001 | 2.16 (1.92, 2.43) | <0.001 | 1.41 (1.30, 1.53) | <0.001 |
| Length of hospital stay# | 1.02 (1.02, 1.03) | <0.001 | 1.03 (1.02, 1.03) | <0.001 | 1.03 (1.03, 1.04) | <0.001 |
| Discharge disposition (vs. home) | ||||||
| Short-term hospital | 4.37 (3.72, 5.14) | <0.001 | 3.04 (2.71, 3.40) | <0.001 | 4.62 (4.30, 4.98) | <0.001 |
| Skilled nursing facility | 1.19 (1.08, 1.32) | <0.001 | 1.25 (1.18, 1.32) | <0.001 | 1.49 (1.44, 1.55) | <0.001 |
| Rehabilitation facility | 0.57 (0.49, 0.67) | <0.001 | 0.42 (0.38, 0.47) | <0.001 | 2.11 (2.02, 2.20) | <0.001 |
| Other facility | 0.70 (0.59, 0.82) | <0.001 | 0.56 (0.51, 0.63) | <0.001 | 3.20 (3.07, 3.34) | <0.001 |
Readmission categories are not mutually exclusive.
Readmissions due to any of 8 diagnoses designated by the CMS as TKA-specific complications (see Appendix).
Readmissions due to a diagnosis on an expanded list of TKA-specific complications, including 22 additional TKA-specific complications selected by a group of experts (see Appendix).
Readmissions due to all causes, including 918 conditions not included in the CMS-defined or expanded list of TKA-specific complications (see Appendix).
The change in risk of readmission was calculated for each additional day (unit change) that the patient stayed in the hospital.
TABLE V.
Risk of All-Cause or TKA-Specific Readmission 30 Days After TKA Based on Patient Comorbidities (N = 377,705)
| 30-Day Readmissions* |
||||||
| CMS TKA-Specific† (N = 2,449; C-Statistic = 0.66) |
Expanded TKA-Specific‡ (N = 6,784; C-Statistic = 0.66) |
All-Cause§ (N = 22,076; C-Statistic = 0.69) |
||||
| Elixhauser Comorbidity Measure (Vs. None) | OR (95% CI) | P Value | OR (95% CI) | P Value | OR (95% CI) | P Value |
| Congestive heart failure | 1.41 (1.14, 1.75) | 0.002 | 1.53 (1.34, 1.74) | <0.001 | 1.48 (1.36, 1.60) | <0.001 |
| Valvular disease | 1.07 (0.89, 1.28) | 0.466 | 1.05 (0.93, 1.17) | 0.441 | 1.21 (1.15, 1.29) | <0.001 |
| Pulmonary circulation disorder | 1.74 (1.24, 2.44) | 0.001 | 1.29 (1.01, 1.66) | 0.042 | 1.09 (0.93, 1.26) | 0.290 |
| Peripheral vascular disorder | 1.12 (0.86, 1.46) | 0.417 | 1.17 (0.99, 1.37) | 0.060 | 1.16 (1.05, 1.27) | 0.002 |
| Paralysis | 1.64 (0.77, 3.49) | 0.199 | 1.30 (0.77, 2.19) | 0.320 | 1.20 (0.89, 1.63) | 0.239 |
| Other neurological disorder | 1.17 (0.92, 1.48) | 0.198 | 1.28 (1.12, 1.47) | <0.001 | 1.22 (1.12, 1.33) | <0.001 |
| Chronic pulmonary disease | 1.16 (1.04, 1.29) | 0.008 | 1.32 (1.24, 1.41) | <0.001 | 1.24 (1.19, 1.29) | <0.001 |
| Diabetes | 1.11 (1.01, 1.23) | 0.037 | 1.08 (1.02, 1.15) | 0.012 | 1.10 (1.06, 1.14) | <0.001 |
| Renal failure | 1.47 (1.20, 1.81) | <0.001 | 1.32 (1.16, 1.50) | <0.001 | 1.35 (1.24, 1.47) | <0.001 |
| Liver disease | 0.99 (0.65, 1.50) | 0.949 | 1.40 (1.12, 1.74) | 0.003 | 1.28 (1.11, 1.49) | 0.001 |
| Peptic ulcer disease excluding bleeding | 0.92 (0.48, 1.79) | 0.813 | 1.12 (0.77, 1.63) | 0.566 | 0.89 (0.74, 1.08) | 0.238 |
| Lymphoma | 1.94 (0.80, 4.73) | 0.143 | 1.90 (1.09, 3.34) | 0.025 | 1.72 (1.23, 2.40) | 0.002 |
| Solid tumor without metastasis | 1.04 (0.78, 1.38) | 0.789 | 0.96 (0.80, 1.15) | 0.685 | 1.15 (1.06, 1.25) | <0.001 |
| Rheumatoid arthritis/collagen vascular disease | 1.11 (0.68, 1.81) | 0.684 | 1.22 (0.89, 1.67) | 0.208 | 1.09 (0.91, 1.29) | 0.352 |
| Coagulopathy | 1.56 (1.14, 2.13) | 0.006 | 1.48 (1.21, 1.80) | <0.001 | 1.19 (1.05, 1.35) | 0.008 |
| Obesity | 1.25 (1.12, 1.38) | <0.001 | 1.14 (1.07, 1.21) | <0.001 | 1.03 (0.99, 1.07) | 0.133 |
| Weight loss | 1.29 (0.53, 3.19) | 0.575 | 0.99 (0.52, 1.89) | 0.975 | 0.76 (0.48, 1.21) | 0.252 |
| Fluid and electrolyte disorders | 1.07 (0.84, 1.37) | 0.575 | 1.07 (0.92, 1.24) | 0.403 | 1.03 (0.94, 1.12) | 0.525 |
| Deficiency anemias | 1.01 (0.87, 1.19) | 0.858 | 1.06 (0.96, 1.16) | 0.259 | 1.06 (1.00, 1.12) | 0.036 |
| Alcohol abuse | 0.93 (0.59, 1.45) | 0.735 | 1.03 (0.79, 1.33) | 0.850 | 1.08 (0.91, 1.27) | 0.393 |
| Drug abuse | 1.36 (0.83, 2.23) | 0.219 | 1.34 (1.00, 1.79) | 0.054 | 1.27 (1.02, 1.58) | 0.033 |
| Psychoses | 1.09 (0.78, 1.52) | 0.630 | 1.31 (1.09, 1.58) | 0.005 | 1.32 (1.17, 1.48) | <0.001 |
| Depression | 1.35 (1.19, 1.53) | <0.001 | 1.27 (1.17, 1.37) | <0.001 | 1.13 (1.08, 1.19) | <0.001 |
| Hypertension (uncomplicated and complicated combined) | 1.09 (1.00, 1.19) | 0.065 | 1.03 (0.98, 1.09) | 0.228 | 1.06 (1.02, 1.09) | <0.001 |
Readmission categories are not mutually exclusive.
Readmissions due to any of 8 diagnoses designated by the CMS as TKA-specific complications (see Appendix).
Readmissions due to a diagnosis on an expanded list of TKA-specific complications, including 22 additional TKA-specific complications selected by a group of experts (see Appendix).
Readmissions due to all causes, including 918 conditions not included in the CMS-defined or expanded list of TKA-specific complications (see Appendix).
Our multivariable regression model was able to predict 66% of the readmissions for a TKA-specific complication as defined by the CMS or that was included on the expanded list. Several factors that increased the risk of all-cause readmissions did not affect the risk of TKA-specific readmissions and vice versa (Tables IV and V). Regardless of whether the CMS or expanded criteria for TKA-specific readmissions were used, black patients and those with Medicaid insurance had an increased risk, although those patient characteristics did not affect the all-cause readmission risk. Advanced age was a risk for TKA-specific readmission only when the patient was >85 years, whereas an age of >75 years increased the risk of all-cause readmissions. An age of 65 to 75 years conferred slight protection against TKA-specific readmissions but not against all-cause readmissions. In contrast to all-cause readmissions, the risk of TKA-specific readmissions was decreased by a discharge to a rehabilitation center or “other” facility. Bilateral surgery was a risk factor for all-cause readmissions and TKA-specific readmissions according to the CMS criteria but not according to the criteria on the expanded list. Only 8 of the 16 comorbid conditions that increased the all-cause readmission risk also increased both categories of TKA-specific readmission risk. Obesity increased the TKA-specific but not the all-cause readmission risk.
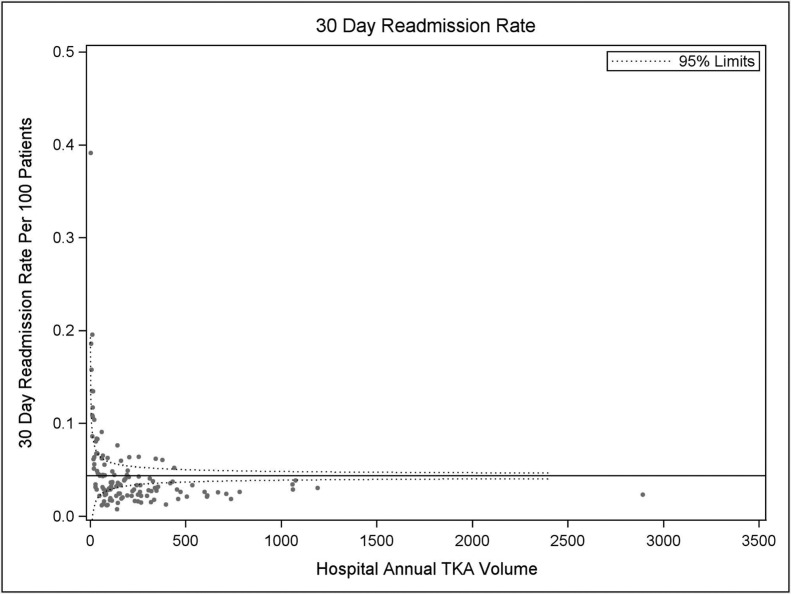
Higher hospital volume was associated with fewer readmissions (Fig. 2), with a volume of ≤89 TKAs per year increasing the risk of both all-cause and TKA-specific readmissions (Table VI) and a volume of 90 to 235 increasing the risk of all-cause readmissions and those due to criteria on the expanded list but not to readmissions due to the CMS-defined TKA-specific criteria. Volumes of 236 to 644 conferred protection against all-cause readmissions without affecting TKA-specific readmissions.
Fig. 2.
Hospital TKA volume plotted against frequency of readmission 30 days after primary TKA for 1 year from December 2013 to November 2014 with use of the SPARCS NY State database.
TABLE VI.
Risk of All-Cause or TKA-Specific Readmission 30 Days After TKA Based on Hospital Annual Volume of TKAs (N = 377,705)
| 30-Day Readmissions* |
||||||
| CMS TKA-Specific† (N = 2,449; C-Statistic = 0.66) |
Expanded TKA-Specific‡ (N = 6,784; C-Statistic = 0.66) |
All-Cause§ (N = 22,076; C-Statistic = 0.69) |
||||
| Hospital Annual Volume# | OR (95% CI) | P Value | OR (95% CI) | P Value | OR (95% CI) | P Value |
| ≤89 vs. ≥645 | 1.32 (1.16, 1.51) | <0.001 | 1.43 (1.32, 1.56) | <0.001 | 1.26 (1.20, 1.32) | <0.001 |
| 90-235 vs. ≥645 | 1.09 (0.97, 1.22) | 0.160 | 1.24 (1.15, 1.33) | <0.001 | 1.05 (1.01, 1.09) | 0.021 |
| 236-644 vs. ≥645 | 0.95 (0.84, 1.08) | 0.429 | 1.01 (0.93, 1.08) | 0.896 | 0.74 (0.71, 0.78) | <0.001 |
Readmission categories are not mutually exclusive. †Readmissions due to any of 8 diagnoses designated by the CMS as TKA-specific complications (see Appendix).
Readmissions due to a diagnosis on an expanded list of TKA-specific complications, including 22 additional TKA-specific complications selected by a group of experts (see Appendix).
Readmissions due to all causes, including 918 conditions not included in the CMS-defined or expanded list of TKA-specific complications (see Appendix).
Thresholds for hospital annual volume were determined using SSLR analysis as described in the Materials and Methods section.
Discussion
The frequency of all-cause readmission that we reported for NY State (mean 5.8%; median, 3.9%; Q1, Q3 = 1.1%, 7.2%) is consistent with the upper values of the previously reported range of 2.0% to 6.6% within 30 days after primary TKA6-8,13-15,24,25. However, we found much lower frequencies of readmissions for TKA-specific causes. Only 11% of readmissions (0.7% of primary TKAs) could be considered due to TKA-specific complications according to CMS criteria2. Even when using our expanded criteria21, which included 22 additional diagnoses, only one-third of the readmissions (1.8% of the TKAs) could be considered TKA-specific. We also showed that, whereas all-cause readmission rates changed over time, TKA-specific readmission rates were relatively stable from 1997 to 2014. The apparent decline in the all-cause readmission rate over time was not expected, given that, in 2012, Cram et al. reported increasing readmission rates over a similar time frame (1991 to 2010)26. The discrepancy may be due to differences in the populations, as Cram et al. examined Medicare patients exclusively whereas we also studied non-Medicare patients, including those younger than 65 years old. A recent review suggests that the proportion of younger patients treated with TKA has increased over time; such a trend in our NY State cohort could have resulted in a decreasing readmission rate27. Whatever the reasons, it is evident that most readmissions are not related to complications of the TKA specifically, especially in the short term, calling into question the use of all-cause readmission rates as a measure of TKA safety.
Our regression model was able to predict about two-thirds of the all-cause, CMS-defined TKA-specific, and expanded-criteria TKA-specific readmissions at 30 days. These analyses also corroborate that many all-cause readmissions occur for reasons unrelated to TKA. Consistent with previous reports, we found male patients to be at higher risk for readmission, regardless of the criteria used to define the readmission15. However, discrepancies among the readmission categories were detected for many other risk factors.
An age of >75 years was a risk factor for all-cause readmissions, but the risk of TKA-specific readmissions increased only after the age of 85 years and an age of 65 to 75 years conferred a slight protective effect. Our results suggest that previous findings with regard to the effect of age on readmission may have been mixed because different criteria were used to define readmission7,10,15,16,28,29. Higuera et al. found no association between age and readmissions16. Avram et al.7 and Pugely et al.30 found that older age was a predictor of readmissions at 30 days after discharge whereas Zmistowski et al. found that younger patients were more likely to be readmitted15, all in large cohorts.
Black race was a risk factor for TKA-related readmission but not all-cause readmission. Previous studies have shown black patients to have higher complication and readmission rates after total joint arthroplasty19,31,32. Clearly, this is an area that continues to require study and improvement.
In agreement with previous studies11,20, our study showed that patients with more comorbid conditions were at higher risk for readmission. However, not all of the diagnoses that increased the risk of all-cause readmission affected TKA-specific readmission. Consistent with previous studies, we found that patients with coagulopathies10,33,34, renal disease3,10 heart disease13,35, obesity8,13,36 and mental health problems4,37 were at increased risk for TKA-specific readmission. Although we found depression to be a risk factor for TKA-specific readmissions, drug abuse and psychoses contributed only to all-cause readmissions in our cohort. Diabetes10,13,35 and anemia16,34 have been reported to increase the risk of readmission after TKA; in our model these were risk factors for all-cause but not TKA-specific readmission. Consistent with previous reports, our study showed that in-hospital complications and a longer stay in the hospital also increased the risk of readmission, regardless of the criteria used to define the readmission7,29,38,39. Whether addressing these risks can decrease readmission frequency remains unclear40,41.
Bilateral surgery was a risk factor for all-cause readmissions and TKA-specific readmissions according to the CMS criteria but not the criteria on the expanded list, suggesting that while bilaterality does not compromise the outcome of TKA itself, the duration or extent of surgery may be riskier for sicker patients. While Hart et al.42 did not find an increased readmission rate after bilateral surgery, they did report a slightly higher rate of major complications. Although bilateral surgery is not part of the CMS Comprehensive Care for Joint Replacement Model (CJR) or Bundled Payments for Care Improvement (BPCI) initiative for lower-extremity joint replacement, they were included in our analysis to replicate as closely as possible the CMS readmission measure methodology, in which bilateral operations are risk-adjusted but included43.
As in previous studies, we found insurance coverage and disposition to influence readmission rates4,10,14,33,39,44. However, we also found that the influence of these factors depended on whether the readmission was all-cause or due to a TKA-specific diagnosis. In our study, Medicare coverage increased the risk of all 3 categories of readmission but Medicaid coverage was a risk factor only for TKA-specific readmission, suggesting that lower socioeconomic status affected TKA outcomes specifically. This finding is in agreement with previous observations33,39,44 and underscores the need to determine how to improve TKA-specific care in this population. We also found that discharge to anywhere other than home increased the risk of all-cause readmission, which is consistent with previous reports4,13,39 and our finding that sicker patients have a higher readmission risk. However, discharge to a rehabilitation facility conferred a protective effect only against TKA-specific readmissions. This is consistent with the expectation that post-TKA aftercare at rehabilitation facilities is better than what could be provided at home.
The relationship between higher procedure volume and better procedure outcome has been reported for TKA and other surgical procedures5,45,46, although the reasons for it remain opaque. Surgeon procedure volume may be a contributing factor24,47. Our findings confirm the volume-outcome relationship in hospitals across NY State. Previously, we identified TKA volume thresholds (≤89, 90 to 235, 236 to 644, and ≥645 TKA per year) in NY State hospitals that were associated with decreasing risks of complications 90 days after surgery23. We add to our previous findings the observation that these volume strata are also associated with decreasing risk of readmission 30 days after TKA. Our findings could suggest that TKAs should be performed only in hospitals where ≥90 operations are done per year. An alternative approach might be to encourage primary care physicians (or other gatekeepers) to steer patients to higher-volume centers but ultimately leave the decision to the patient, allowing them to weigh the possibly increased risk of complications against factors that might make a smaller hospital more appealing to them, such as proximity or familiarity. Surprisingly, hospitals reporting a volume of 236 to 644 cases per year had a lower rate of all-cause readmissions than hospitals reporting ≥645 cases, despite the fact that in our previous study these 2 strata had the same 90-day complication risk and the highest-volume hospitals had the lowest mortality risk23. Considering that the rates of TKA-specific readmission were the same in the top 2 volume strata of hospitals, the higher all-cause readmission risk in the highest-volume hospitals likely arises from medical or surgical issues not related to TKA directly. Large, highly specialized hospitals reporting ≥645 TKAs per year are likely to be in urban areas and thus may serve a different population than lower-volume hospitals. For example, readmission may be more common for medicolegal reasons. Further investigation is required to understand why hospitals in the highest-volume stratum have the lowest TKA-related readmission rates but not the lowest all-cause readmission rates. Studies to elucidate the proportion of high-risk patients treated at each volume tier of hospitals would be instructive. Whatever the reasons may be, the discrepancy underscores our overall conclusion that procedure-specific and all-cause readmissions do not measure the same outcome.
The limitations of our study are related to the use of an administrative database. Inaccuracy of coding of diagnoses and procedures and a lack of detailed clinical information are concerns. However, this database is similar to the one used by Medicare to measure readmission rates and can provide a picture of all-payer health-care delivery over a large geographic region in a cohort that is much larger than those in most previous studies. Although a wide variety of communities (urban, suburban, and rural) are represented in NY State, it is possible that patients, surgeons, and hospital-related factors unique to our state are not entirely reflective of the rest of the U.S. Finally, even though we restricted our study to NY State residents, patients living near borders with other states may have been readmitted to hospitals in those states, resulting in an underestimation of readmission frequency.
In conclusion, using a statewide database, we determined that TKA-specific readmissions account for only 11% to 31% of all-cause readmissions at 30 days after discharge, indicating that all-cause readmission rates are not an accurate measure of TKA safety. Fortunately, in the final rule for the CMS total joint replacement bundle, the CJR payment model does not use all-cause readmission as a performance measure48, even though it had been considered when first proposed49. However, with regard to the Hospital Readmissions Reduction Program, our findings suggest that CMS may be unfairly penalizing hospitals using this methodology for the calculation of readmission rates following TKA. We identified several risk factors for TKA-specific readmission. The fact that some risk factors— including bilateral TKA and disposition to a rehabilitation facility—contributed to all-cause but not TKA readmission indicate that analysis of procedure-specific readmissions is necessary for accurate risk adjustment. Readmission rates are lower at higher-volume hospitals, with the risk of readmission declining in hospitals performing at least 90 TKAs per year.
Overall, our finding of an imperfect overlap of risk factors for all-cause versus TKA-specific readmission suggests that clearly defining the parameters for a relevant readmission will affect not only the apparent frequency of readmission but the definition of its risk factors. This is important when considering how readmission frequencies might be risk-adjusted to prevent excessive readmission-related penalties for hospitals serving a greater proportion of at-risk patients.
Appendix
Tables showing the CMS-defined and expanded lists of TKA-specific diagnoses leading to readmission as well as the diagnoses leading to 80% of the readmissions due to non-TKA-specific reasons are available with the online version of this article as a data supplement at jbjs.org (http://links.lww.com/JBJS/C967).
Acknowledgments
Note: The authors thank Kaitlyn Yin and Naaman Mehta for assistance in the preparation of this manuscript.
Footnotes
Investigation performed at the Hospital for Special Surgery, New York, NY
A commentary by Michael D. Ries, MD, is linked to the online version of this article at jbjs.org.
Disclosure: This study was funded by National Institutes of Health (NIH) Grant UL1RR024996 to the Weill Cornell Clinical Translational Science Center, National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS) Grants R03 AR05063 and RC1 AR0589280, and Agency for Healthcare Research and Quality (AHRQ) Centers for Education & Research on Therapeutics (CERTs) Grant U18 HS16075. On the Disclosure of Potential Conflicts of Interest forms, which are provided with the online version of the article, one or more of the authors checked “yes” to indicate that the author had a relevant financial relationship in the biomedical arena outside the submitted work (http://links.lww.com/JBJS/C966).
References
- 1.Centers for Medicare & Medicaid Services. Readmissions Reduction Program. https://www.cms.gov/medicare/medicare-fee-for-service-payment/acuteinpatientpps/readmissions-reduction-program.html. Accessed 2017 Jan 26.
- 2.Dorsey K, Grady JN, Suter LG, Kwon JY, Parzynski CS, DeBuhr J, Bernheim S, Krumholz HM. 2016 Procedure-specific measure updates and specifications report. Hospital-level risk-standardized complication measure. Elective primary total hip arthroplasty (THA) and/or total knee arthroplasty (TKA) – version 5.0. 2016.
- 3.Keeney JA, Adelani MA, Nunley RM, Clohisy JC, Barrack RL. Assessing readmission databases: how reliable is the information? J Arthroplasty. 2012. September;27(8)(Suppl):72-6.e1: 2. Epub 2012 May 11. [DOI] [PubMed] [Google Scholar]
- 4.Lavernia CJ, Villa JM, Iacobelli DA. Readmission rates in the state of Florida: a reflection of quality? Clin Orthop Relat Res. 2013. December;471(12):3856-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chen JC, Shaw JD, Ma Y, Rhoads KF. The role of the hospital and health care system characteristics in readmissions after major surgery in California. Surgery. 2016. February;159(2):381-8. Epub 2015 Jul 21. [DOI] [PubMed] [Google Scholar]
- 6.Adelani MA, Keeney JA, Nunley RM, Clohisy JC, Barrack RL. Readmission following total knee arthroplasty: venous thromboembolism as a “never event” is a counterproductive misnomer. J Arthroplasty. 2013. May;28(5):747-50. Epub 2013 Mar 13. [DOI] [PubMed] [Google Scholar]
- 7.Avram V, Petruccelli D, Winemaker M, de Beer J. Total joint arthroplasty readmission rates and reasons for 30-day hospital readmission. J Arthroplasty. 2014. March;29(3):465-8. Epub 2013 Aug 28. [DOI] [PubMed] [Google Scholar]
- 8.Huddleston JI, Maloney WJ, Wang Y, Verzier N, Hunt DR, Herndon JH. Adverse events after total knee arthroplasty: a national Medicare study. J Arthroplasty. 2009. September;24(6)(Suppl):95-100. Epub 2009 Jul 4. [DOI] [PubMed] [Google Scholar]
- 9.Mesko NW, Bachmann KR, Kovacevic D, LoGrasso ME, O’Rourke C, Froimson MI. Thirty-day readmission following total hip and knee arthroplasty - a preliminary single institution predictive model. J Arthroplasty. 2014. August;29(8):1532-8. Epub 2014 Mar 04. [DOI] [PubMed] [Google Scholar]
- 10.Raines BT, Ponce BA, Reed RD, Richman JS, Hawn MT. Hospital acquired conditions are the strongest predictor for early readmission: an analysis of 26,710 arthroplasties. J Arthroplasty. 2015. August;30(8):1299-307. Epub 2015 Feb 28. [DOI] [PubMed] [Google Scholar]
- 11.Ramkumar PN, Chu CT, Harris JD, Athiviraham A, Harrington MA, White DL, Berger DH, Naik AD, Li LT. Causes and rates of unplanned readmissions after elective primary total joint arthroplasty: a systematic review and meta-analysis. Am J Orthop. 2015. September;44(9):397-405. [PubMed] [Google Scholar]
- 12.Saucedo JM, Marecek GS, Wanke TR, Lee J, Stulberg SD, Puri L. Understanding readmission after primary total hip and knee arthroplasty: who’s at risk? J Arthroplasty. 2014. February;29(2):256-60. Epub 2013 Aug 17. [DOI] [PubMed] [Google Scholar]
- 13.Schaeffer JF, Scott DJ, Godin JA, Attarian DE, Wellman SS, Mather RC 3rd. The association of ASA class on total knee and total hip arthroplasty readmission rates in an academic hospital. J Arthroplasty. 2015. May;30(5):723-7. Epub 2014 Dec 16. [DOI] [PubMed] [Google Scholar]
- 14.Tayne S, Merrill CA, Smith EL, Mackey WC. Predictive risk factors for 30-day readmissions following primary total joint arthroplasty and modification of patient management. J Arthroplasty. 2014. October;29(10):1938-42. Epub 2014 Jun 2. [DOI] [PubMed] [Google Scholar]
- 15.Zmistowski B, Restrepo C, Hess J, Adibi D, Cangoz S, Parvizi J. Unplanned readmission after total joint arthroplasty: rates, reasons, and risk factors. J Bone Joint Surg Am. 2013. October 16;95(20):1869-76. [DOI] [PubMed] [Google Scholar]
- 16.Higuera CA, Elsharkawy K, Klika AK, Brocone M, Barsoum WK. 2010 Mid-America Orthopaedic Association Physician in Training Award: predictors of early adverse outcomes after knee and hip arthroplasty in geriatric patients. Clin Orthop Relat Res. 2011. May;469(5):1391-400. Epub 2011 Feb 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Staples JA, Thiruchelvam D, Redelmeier DA. Site of hospital readmission and mortality: a population-based retrospective cohort study. CMAJ Open. 2014. May 01;2(2):E77-85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Schairer WW, Vail TP, Bozic KJ. What are the rates and causes of hospital readmission after total knee arthroplasty? Clin Orthop Relat Res. 2014. January;472(1):181-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.SooHoo NF, Lieberman JR, Ko CY, Zingmond DS. Factors predicting complication rates following total knee replacement. J Bone Joint Surg Am. 2006. March;88(3):480-5. [DOI] [PubMed] [Google Scholar]
- 20.Voskuijl T, Hageman M, Ring D. Higher Charlson comorbidity index scores are associated with readmission after orthopaedic surgery. Clin Orthop Relat Res. 2014. May;472(5):1638-44. Epub 2013 Nov 26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pierce O, Allen M. How we measured surgical complications. 2015 Jul 13. https://www.propublica.org/article/surgeon-level-risk-short-methodology. Accessed 2017 Jan 26.
- 22.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998. January;36(1):8-27. [DOI] [PubMed] [Google Scholar]
- 23.Wilson S, Marx RG, Pan TJ, Lyman S. Meaningful thresholds for the volume-outcomes relationship in total knee arthroplasty. J Bone Joint Surg Am. 2016;98(20):1683-90. [DOI] [PubMed] [Google Scholar]
- 24.Ravi B, Croxford R, Austin PC, Hollands S, Paterson JM, Bogoch E, Kreder H, Hawker GA. Increased surgeon experience with rheumatoid arthritis reduces the risk of complications following total joint arthroplasty. Arthritis Rheumatol. 2014. March;66(3):488-96. [DOI] [PubMed] [Google Scholar]
- 25.Singh JA, Lu X, Rosenthal GE, Ibrahim S, Cram P. Racial disparities in knee and hip total joint arthroplasty: an 18-year analysis of national Medicare data. Ann Rheum Dis. 2014. December;73(12):2107-15. Epub 2013 Sep 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cram P, Lu X, Kates SL, Singh JA, Li Y, Wolf BR. Total knee arthroplasty volume, utilization, and outcomes among Medicare beneficiaries, 1991-2010. JAMA. 2012. September 26;308(12):1227-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Singh JA. Epidemiology of knee and hip arthroplasty: a systematic review. Open Orthop J. 2011. March 16;5:80-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fang M, Noiseux N, Linson E, Cram P. The effect of advancing age on total joint replacement outcomes. Geriatr Orthop Surg Rehabil. 2015. September;6(3):173-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kheir MM, Clement RC, Derman PB, Flynn DN, Speck RM, Levin LS, Fleisher LA. Are there identifiable risk factors and causes associated with unplanned readmissions following total knee arthroplasty? J Arthroplasty. 2014. November;29(11):2192-6. Epub 2014 Jul 2. [DOI] [PubMed] [Google Scholar]
- 30.Pugely AJ, Callaghan JJ, Martin CT, Cram P, Gao Y. Incidence of and risk factors for 30-day readmission following elective primary total joint arthroplasty: analysis from the ACS-NSQIP. J Arthroplasty. 2013. October;28(9):1499-504. Epub 2013 Jul 26. [DOI] [PubMed] [Google Scholar]
- 31.Centers for Disease Control and Prevention (CDC). Racial disparities in total knee replacement among Medicare enrollees—United States, 2000-2006. MMWR Morb Mortal Wkly Rep. 2009. February 20;58(6):133-8. [PubMed] [Google Scholar]
- 32.Cai X, Cram P, Vaughan-Sarrazin M. Are African American patients more likely to receive a total knee arthroplasty in a low-quality hospital? Clin Orthop Relat Res. 2012. April;470(4):1185-93. Epub 2011 Aug 31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Browne JA, Novicoff WM, D’Apuzzo MR. Medicaid payer status is associated with in-hospital morbidity and resource utilization following primary total joint arthroplasty. J Bone Joint Surg Am. 2014. November 05;96(21):e180. [DOI] [PubMed] [Google Scholar]
- 34.Miric A, Inacio MCS, Namba RS. Can total knee arthroplasty be safely performed in patients with chronic renal disease? Acta Orthop. 2014. February;85(1):71-8. Epub 2014 Jan 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Vorhies JS, Wang Y, Herndon JH, Maloney WJ, Huddleston JI. Decreased length of stay after TKA is not associated with increased readmission rates in a national Medicare sample. Clin Orthop Relat Res. 2012. January;470(1):166-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Dowsey MM, Liew D, Choong PFM. Economic burden of obesity in primary total knee arthroplasty. Arthritis Care Res (Hoboken). 2011. October;63(10):1375-81. [DOI] [PubMed] [Google Scholar]
- 37.Browne JA, Sandberg BF, D’Apuzzo MR, Novicoff WM. Depression is associated with early postoperative outcomes following total joint arthroplasty: a nationwide database study. J Arthroplasty. 2014. March;29(3):481-3. Epub 2013 Oct 3. [DOI] [PubMed] [Google Scholar]
- 38.Bini SA, Fithian DC, Paxton LW, Khatod MX, Inacio MC, Namba RS. Does discharge disposition after primary total joint arthroplasty affect readmission rates? J Arthroplasty. 2010. January;25(1):114-7. Epub 2009 Jan 15. [DOI] [PubMed] [Google Scholar]
- 39.Keeney JA, Nam D, Johnson SR, Nunley RM, Clohisy JC, Barrack RL. Socioeconomically disadvantaged CMS beneficiaries do not benefit from the readmission reduction initiatives. J Arthroplasty. 2015. December;30(12):2082-5. Epub 2015 Jun 20. [DOI] [PubMed] [Google Scholar]
- 40.Inacio MCS, Kritz-Silverstein D, Raman R, Macera CA, Nichols JF, Shaffer RA, Fithian DC. The risk of surgical site infection and re-admission in obese patients undergoing total joint replacement who lose weight before surgery and keep it off post-operatively. Bone Joint J. 2014. May;96-B(5):629-35. [DOI] [PubMed] [Google Scholar]
- 41.Lui M, Jones CA, Westby MD. Effect of non-surgical, non-pharmacological weight loss interventions in patients who are obese prior to hip and knee arthroplasty surgery: a rapid review. Syst Rev. 2015. September 27;4:121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hart A, Antoniou J, Brin YS, Huk OL, Zukor DJ, Bergeron SG. Simultaneous bilateral versus unilateral total knee arthroplasty: a comparison of 30-day readmission rates and major complications. J Arthroplasty. 2016. January;31(1):31-5. Epub 2015 Jul 21. [DOI] [PubMed] [Google Scholar]
- 43.Dorsey K, Grady JN, Desai N, Suter LG, Bierlein M, Parzynski CS, Wang C, DeBuhr J, Bernheim S, Krumholz HM. 2016 Procedure-specific measures updates and specifications report. Hospital-level 30-day risk-standardized readmission measures. Isolated coronary artery bypass graft (CABG) surgery – version 3.0. Elective primary total hip arthroplasty (THA) and/or total knee arthroplasty (TKA) –version 5.0. 2016. [Google Scholar]
- 44.Barrack RL, Ruh EL, Chen J, Lombardi AV Jr, Berend KR, Parvizi J, Della Valle CJ, Hamilton WG, Nunley RM. Impact of socioeconomic factors on outcome of total knee arthroplasty. Clin Orthop Relat Res. 2014. January;472(1):86-97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Pamilo KJ, Peltola M, Paloneva J, Mäkelä K, Häkkinen U, Remes V. Hospital volume affects outcome after total knee arthroplasty. Acta Orthop. 2015. February;86(1):41-7. Epub 2014 Oct 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Glassou EN, Hansen TB, Mäkelä K, Havelin LI, Furnes O, Badawy M, Kärrholm J, Garellick G, Eskelinen A, Pedersen AB. Association between hospital procedure volume and risk of revision after total hip arthroplasty: a population-based study within the Nordic Arthroplasty Register Association database. Osteoarthritis Cartilage. 2016. March;24(3):419-26. Epub 2015 Oct 21. [DOI] [PubMed] [Google Scholar]
- 47.Tan SC, Chan YH, Chong HC, Chin PL, Yew A, Chia SL, Tay D, Lo NN, Yeo SJ. Association of surgeon factors with outcome scores after total knee arthroplasty. J Orthop Surg (Hong Kong). 2014. December;22(3):378-82. [DOI] [PubMed] [Google Scholar]
- 48.American Health Care Association. Comprehensive Care for Joint Replacement (CJR) final rule summary. 2015. https://www.ahcancal.org/facility_operations/medicare/Documents/AHCA%20Summary%20of%20CJR%20Final%20Rule.pdf. Accessed 2017 Jan 26.
- 49.Centers for Medicare & Medicaid Services (CMS). HHS. Medicare program; comprehensive care for joint replacement payment model for acute care hospitals furnishing lower extremity joint replacement services. Final rule. Fed Regist. 2015. November 24;80(226):73273-554. [PubMed] [Google Scholar]