Abstract
Obesity has been related to an increased risk of multiple diseases in which oxidative stress and inflammation play a role. Gut microbiota has emerged as a mediator in this interaction, providing new mechanistic insights at the interface between fat metabolism dysregulation and obesity development. Our aim was to analyze the interrelationship among obesity, diet, oxidative stress, inflammation and the intestinal microbiota in 68 healthy adults (29.4% normal-weight). Diet was assessed through a food frequency questionnaire and converted into nutrients and dietary compounds using food composition tables. The intestinal microbiota was assessed by quantitative PCR, fecal short chain fatty acids by gas chromatography and serum biomarkers by standard protocols. Higher levels of malondialdehyde (MDA), C reactive protein (CRP), serum leptin, glucose, fat percentage and the intestinal Lactobacillus group were found in the obese people. Cluster analysis of body mass index, fat mass, glucose, LDL/HDL ratio, leptin, MDA and CRP classified the subjects into two groups. The levels of the intestinal Bacteroides-Prevotella-Porphyromonas group were lower in the cluster and linked to a higher pro-oxidant and pro-inflammatory status, whose individuals also had lower intake of fruits, dried fruits, and fish. These results could be useful for designing strategies targeted to obesity prevention.
Keywords: oxidative stress, microbiota, obesity, antioxidant, western diet
1. Introduction
The prevalence of obesity is growing worldwide, with nearly half a billion of the world’s population considered to be overweight. Obesity, defined by the World Health Organization (WHO) as an “abnormal or excessive fat accumulation”, has been associated with an increasing risk of multiple diseases, characterized by changes in the oxidative/antioxidant balance and the presence of subclinical inflammation [1,2,3,4], including diabetes, metabolic syndrome, hypertension, dyslipidemia and cardiovascular disease among others [5]. Thanks to the great efforts made in obesity research during the last decades, several genetic, environmental and lifestyle-related factors have been identified as etiological risk elements for this condition. However, there are still factors in this equation, such as the gut microbiota, whose contribution remains to be fully elucidated. It has been proposed that the reduction of carbohydrates accessible to gut microbes from fiber-containing foodstuffs may result in a long-term reduction of microbiota diversity and in the appearance of “unhealthy” microbiomes [6,7,8]. Although it has not been possible to establish the directionality of this relationship, the gradual increase in energy intake, together with the dramatic change in the proportion of macronutrients of the Western diet, seems to be linked with the increase of the obesity prevalence [9] mediated by changes in intestinal microbial populations.
In contrast, the content in bioactive compounds of the Mediterranean Diet has been linked with the prevention of obesity and metabolic syndrome, by means of restoring the intestinal microbial balance of these patients [10,11]. An increase of the intestinal Firmicutes/Bacteroidetes ratio has been reported in several studies with obese humans [12], in obese leptin deficient ob/ob mice [13] and in wild-type animals receiving Western diets [14]. The benefits of dietary fiber in host health have been reported to be partly mediated by physiological effects linked to the formation in the colon of fecal short chain fatty acids (SCFA) produced by the microbial fermentation of complex carbohydrates. In this regard, it is known that the major SCFA synthesized by the colonic microbiota (acetic, propionic, and butyric) play a key role in regulating host energy balance in extra-intestinal organs, such as the liver and adipose tissue [15,16]. In an apparently contradictory way, high levels of fecal SCFA have been frequently found in obese subjects [17]. The specific mechanisms explaining the higher levels of fecal SCFA in obesity still remain a matter of debate and different hypotheses have been proposed, including: an increase on colonic fermentation due to the higher dietary intake; a higher capacity for energy harvest by the modification of the intestinal microbial metabolic profile linked to obesity [18,19]; and the reduction of the in vivo fluxes of SCFA from the intestinal lumen to other host organs, with accumulation in the colonic lumen [20].
The currently available evidences highlight the complex network of physiological mechanisms underlying obesity [21]. In this scenario, the intestinal microbiota may provide new mechanistic insights at the interface between fat metabolism dysregulation and obesity development. To the best of our knowledge, there are no currently available interdisciplinary studies addressing the interrelationships among obesity, diet, oxidative stress, inflammation and gut microbiota. However, a better understanding of these interactions could be useful for the development of new approaches for preventing and controlling obesity. Therefore, our aim was to determine differences in the serum concentration of malondialdehyde (MDA), glucose, lipid profile, and C reactive protein (CRP), according to the grade of obesity, to describe the gut microbial composition linked with this pathology and to analyze the role of the diet in the possible associations among these parameters.
2. Subjects and Methods
2.1. Participants
This cross-sectional study is part of a research into diet and gut microbiota in different population groups. The study sample comprised 68 adult volunteers 27 men and 41 women, aged from 19 to 67 years (mean ± SD, 52.4 ± 11.2). Participants were recruited in Asturias Region (Northern Spain) between the years 2009 and 2015 among subjects attending a program of the University of Oviedo for people older than 50 years, as well as among individuals participating in a study on nutritional habits from the Alimerka Foundation. In a personal interview, volunteers were informed of the objectives of the study and those deciding to participate gave their fully informed written consent. Then, personal appointments were made to collect the dietary information. Subjects were initially classified according to their Body Mass Index (BMI) [22]. From the initial sample four subjects were excluded from cluster analysis because no data were recorded for some of the parameters introduced as variables in our study. Moreover, three subjects had missing values for fecal microbiota and, therefore, were not included for further analyses. The following inclusion criteria were used: not being diagnosed of autoimmune diseases, inflammatory bowel disease or other conditions known to affect the intestinal function, as well as not having undergone medical treatment with oral corticoids, immunosuppressive agents, monoclonal antibodies, antibiotics or immunotherapy or not having consumed any supplement containing probiotics or prebiotics during the previous month. Volunteers diagnosed for diabetes mellitus type II were specifically excluded from the study. Ethical approval for this study was obtained from the Bioethics Committee of CSIC (Consejo Superior de Investigaciones Científicas) and from the Regional Ethics Committee for Clinical Research (“Servicio de Salud del Principado de Asturias nº13/2010”) in compliance with the Declaration of Helsinki of 1964. All experiments were carried out in accordance with approved guidelines and regulations.
2.2. Nutritional Assessment
Dietary intake was assessed in a personal interview by means of an annual semi-quantitative food frequency questionnaire (FFQ) method which details 160 items and has been widely used and validated in previous studies [23,24]. The consumption of foods was converted into energy and macronutrients using the nutrient food composition tables developed by the Centro de Enseñanza Superior de Nutrición y Dietética (CESNID) [25]; the intake of monosaccharides (glucose, galactose, fructose) sucrose, starch and digestible polysaccharides and trans fatty acids was converted using the National Nutrient Database for Standard Reference from the United States Department of Agriculture (USDA) [26]. Information about dietary soluble and insoluble fibers was completed from Marlett et al. [27] and phenolic intake was estimated from the Phenol Explorer database [28]. Data about the Oxygen Radical Absorbance Capacity (ORAC) of foods was obtained from the Database from the ORAC of Selected Foods from USDA [29]. This database reports the hydrophilic ORAC, lipophilic ORAC and total ORAC values for 275 foods as μmol of Trolox equivalents (TE)/100 g. For the estimation of these variables in the study sample we used the information contained in our database regarding the daily intake of each food in g/day for all the evaluated subjects. This information has been crossed with the data contained in the ORAC database in order to calculate the intake of ORAC hydrophilic, lipophilic and total in μmol TE for each food and subject. Once this partial information was available, the summary of all the hydrophilic ORAC, lipophilic ORAC and total ORAC obtained per subject was calculated in order to estimate the total antioxidant capacity of the diet by subject.
2.3. Anthropometric Measures
At the same time of carrying out the blood extraction, between eight and nine o’clock and after over-night fast, anthropometric measures were taken. Height was registered using a stadiometer with an accuracy of ±1 mm (Año-Sayol, Barcelona, Spain). Subjects stood barefoot, in an upright position and with the head positioned in the Frankfort horizontal plane. Weight was measured on a scale with an accuracy of ±100 g (Seca, Hamburg, Germany). BMI was calculated and stratified according to the Sociedad Española para el Estudio De la Obesidad (SEEDO) [22] criteria: lean–normal weight (≤25.0 kg/m2), over-weight (25.0–30.0 kg/m2), and obese (≥30.0 kg/m2). Body fat percentage was measured by bioelectrical impedance (BIA) with ±1% variation, with subjects in light clothes and in fasted state (Tanita Corporation of America, Inc., Arlington Heights, IL, USA). Basal Metabolic Rate (BMR) was calculated by the Harris-Benedict formula [30].
2.4. Blood Biochemical Analyses
Fasting blood samples were drawn by venepuncture after a 12 h fast and collected in separate tubes for serum and plasma. Samples were kept on ice and centrifuged (1000× g, 15 min) within 2–4 h after collection. Plasma and serum aliquots were kept at −20 °C until analyses were performed. Plasma glucose, cholesterol, and triglycerides were determined by standard methods. Serum levels of CRP were determined by using a CRP Human Instant ELISA kit (Ebioscience, San Diego, CA, USA), and those of MDA with a colorimetric assay of lipid peroxidation (Byoxytech LPO-586, Oxis International S.A., Paris, France); the within-run coefficient of variation ranged from 1.2% to 3.4%, depending on the concentration of MDA [31].
Serum leptin was measured by a sensitive ELISA test (Human Leptin ELISA Development Kit, 900-K90 PeproTech Inc., Rocky Hill, NJ, USA) according to the manufacturer’s instructions. The detectable concentration range was 63–4000 pg/mL. The intra-assay and interassay coefficients of variation were 5.21% and 5.20%, respectively.
2.5. Fecal Collection and Microbiological Analyses
Participants received detailed instructions to collect fecal samples and were provided with a sterile container. Samples were immediately frozen at −20 °C after deposition. For analyses, fecal samples were melted, weighed, diluted 1/10 in sterile PBS, and homogenized in a LabBlender 400 Stomacher (Seward Medical, London, UK) for 4 min; the DNA was extracted using the QIAamp DNA stool mini kit (Qiagen, Hilden, Germany) as previously described [32]. Quantification of different bacterial populations that covered the major bacterial groups present in the gut microbial ecosystem (Table 1) was performed in feces with a 7500 Fast Real-Time PCR System (Applied Biosystems, Foster City, CA, USA) using SYBR Green PCR Master Mix (Applied Biosystems). One microlitre of template fecal DNA (~5 ng) and 0.2 μM of each primer were added to the 25-μL reaction mixture. PCR cycling consisted of an initial cycle of 95 °C 10 min, followed by 40 cycles of 95 °C 15 s, and 1 min at the appropriate primer-pair temperature (Table 1). The number of cells was determined by comparing the Ct values obtained from a standard curve constructed using the pure cultures of appropriate strains that were grown overnight in GAM (Gifu Anaerobic Medium) medium (Nissui Pharmaceutical Co., Tokyo, Japan) under anaerobic conditions (Table 1). The Ct values were plotted as a linear function of the base-10 logarithm of the number of cells calculated by plate counting. Fecal DNA extracts were analysed and the mean quantity per gram of fecal wet weight was calculated.
Table 1.
Bacterial groups, standard cultures, primers, and annealing temperatures (Tm) used for qPCR in this study.
| Microbial Target | Strain Used for Standard Curve | Primer Sequence 5′–3′ | Tm (°C) | Reference |
|---|---|---|---|---|
| Akkermansia | Akkermansia muciniphila CIP 107961 | F: CAGCACGTGAAGGTGGGGAC | 60 | [32] |
| R: CCTTGCGGTTGGCTTCAGAT | ||||
|
Bacteroides group Bacteroides-Prevotella-Porphiromonas |
Bacteroides thetaiotaomicron DSMZ 2079 | F: GAGAGGAAGGTCCCCCAC | 60 | [32] |
| R: CGCKACTTGGCTGGTTCAG | ||||
| Bifidobacterium | Bifidobacterium longum NCIMB 8809 | F:GATTCTGGCTCAGGATGAACGC | 60 | [32] |
| R: CTGATAGGACGCGACCCCAT | ||||
| Faecalibacterium | Faecalibacterium prausnitzi DSMZ 17677 | F:GGAGGAAGAAGGTCTTCGG | 60 | [33] |
| R: AATTCCGCCTACCTCTGCACT | ||||
|
Clostridia XIVa Blautia coccoides—Eubacterium rectale group |
Blautia coccoides DSMZ 935 | F: CGGTACCTGACTAAGAAGC | 55 | [32] |
| R: AGTTTYATTCTTGCGAACG | ||||
| Lactobacillus group | Lactobacillus gasseri IPLA IF7/5 | F: AGCAGTAGGGAATCTTCCA | 60 | [32] |
| R: CATGGAGTTCCACTGTCCTC |
2.6. Short Chain Fatty Acids (SCFA) Analyses
The analysis of SCFA was performed by gas chromatography to determine the concentrations of acetate, propionate and butyrate. Supernatants from 1 mL of the homogenized feces were obtained by centrifugation and filtration as previously indicated [32,33]. A chromatograph 6890N (Agilent Technologies Inc., Palo Alto, CA, USA) connected to a mass spectrometry detector (MS) 5973N (Agilent Technologies) and a flame ionization detector (FID) was used for identification and quantification of SCFA, respectively. Chromatographic conditions and SCFA analyses were carried out essentially as described by Salazar et al. [34].
2.7. Statistical Analysis
Statistical analysis was performed using the IBM SPSS program version 22.0 (IBM SPSS, Inc., Chicago, IL, USA). Goodness of fit to the normal distribution was analyzed by means of the Kolmogorov-Smirnov test. When the distribution of variables was skewed, the natural logarithm of each value was used in the statistical test. Overall, categorical variables were summarized with counts and percentages while continuous variables were summarized using means and standard deviations. The chi-squared test and independent samples t-test were used for group comparisons where appropriate. Differences in general characteristics, anthropometric, blood parameters, major microbial target and SCFA were assessed in accordance to body mass index classification by means of uni- and multivariate analyses controlling by gender or energy, as appropriate. Also, in order to explore the association between the intestinal microbiota and SCFA with BMI, a linear regression was conducted.
Using the program R (version 3.3.1 for Windows), a cluster analysis using the Ward’s method was performed in order to classify the participants based on the similarity of the different obesity related factors evaluated (BMI, percentage of fat mass, serum glucose, leptin, MDA, CRP and LDL/HDL ratio). This is a hierarchical cluster technique done on the basis of Euclidean distances; therefore, the centers of clusters are grounded on least squares estimation. Differences in the intake of food groups, macronutrients and some dietary components, including antioxidants, were obtained by means of a multivariate analysis controlling for energy intake. The conventional probability value of 0.05 was used in the interpretation of results to indicate statistical significance.
3. Results
The general characteristics of the sample classified according to BMI are presented in Table 2.
Table 2.
General characteristics of the studied population according to BMI.
| Normal Weight BMI ≤ 25.0 n = 20 |
Over Weight BMI 25.0–30.0 n = 35 |
p | Obesity BMI ≥ 30.0 n = 13 |
p | |
|---|---|---|---|---|---|
| Age (years) a | 56.4 ± 10.1 | 51.7 ± 11.7 | 0.152 | 47.8 ± 10.2 | 0.033 |
| Female (%) | 80.0 | 51.4 | 0.036 | 53.8 | 0.110 |
| BMI (kg/m2) a | 23.0 ± 1.5 | 27.5 ± 1.4 | <0.001 | 34.1 ± 2.7 | <0.001 |
| Energy intake (Kcal/day) a | 1958 ± 537 | 1790 ± 482 | 0.261 | 2040 ± 548 | 0.681 |
| Basal Metabolic rate (Kcal/day) a | 1280 ± 167 | 1416 ± 228 | <0.001 | 1548 ± 324 | <0.001 |
| Sedentary lifestyle (%) | 20.0 | 17.1 | 0.792 | 30.8 | 0.481 |
| Current smokers (%) | 27.8 | 26.5 | 0.729 | 25.0 | 0.978 |
| Alcohol consumers (%) | 70.0 | 54.3 | 0.252 | 61.5 | 0.614 |
| Body fat (%) a | 26.2 ± 7.5 | 35.6 ± 9.3 | <0.001 | 51.7 ± 10.8 | <0.001 |
| Blood parameters | |||||
| Serum glucose (mg/dL) a | 97.1 ± 14.2 | 96.0 ± 9.1 | 0.711 | 108 ± 11.1 | 0.020 |
| Triglycerides (mg/dL) a | 100 ± 47.8 | 117 ± 56.9 | 0.288 | 147 ± 91.0 | 0.070 |
| LDL/HDL ratio a | 2.5 ± 0.8 | 2.6 ± 0.8 | 0.869 | 2.3 ± 0.6 | 0.347 |
| Leptin (ng/mL) a | 6.1 ± 4.3 | 9.2 ± 5.2 | 0.021 | 14.7 ± 6.8 | <0.001 |
| MDA (μM) a | 2.1 ± 0.6 | 2.2 ± 0.9 | 0.700 | 3.2 ± 1.6 | 0.012 |
| CRP (mg/L) a | 0.9 ± 0.8 | 3.8 ± 8.4 | 0.150 | 5.4 ± 7.4 | 0.009 |
a Results from univariate analysis were adjusted by gender and presented as mean ± standard deviation. Differences in categorical variables were examined using chi-squared analysis and presented as percentage (%). BMI, body mass index. LDL, low-density lipoprotein. HDL, high-density lipoprotein. MDA, malondialdehyde. CRP, C reactive protein. p value was calculated using normal weight volunteers as reference.
As was expected, obese subjects had significantly higher basal metabolic rate, percentage of fat mass, serum glucose, leptin, MDA and CRP than normal weight volunteers. Regarding the fecal microbial composition and the microbial metabolic activity (SCFA), the levels of Lactobacillus group and acetate concentrations were directly related with the grade of obesity (Table 3).
Table 3.
Differences in fecal short chain fatty acids (SCFA) concentration and major microbial groups according to BMI (kg/m2) and results of linear regression analyses to estimate their association with BMI.
| Normal Weight BMI ≤ 25.0 n = 20 |
Over Weight BMI 25.0–30.0 n = 31 |
Obesity BMI ≥ 30.0 n = 13 |
BMI | |||
|---|---|---|---|---|---|---|
| R2 | β | p | ||||
| Model 1. Fecal SCFA concentration (mM) | ||||||
| Acetate | 35.7 ± 14.6 | 38.0 ± 16.8 | 46.6 ± 17.0 | 0.081 | 0.282 | 0.025 |
| Propionate | 14.4 ± 6.5 | 13.7 ± 6.7 | 17.1 ± 8.2 | 0.022 | 0.136 | 0.288 |
| Butyrate | 11.6 ± 8.7 | 10.3 ± 6.4 | 12.3 ± 9.0 | 0.047 | 0.040 | 0.748 |
| Model 2. Microbial target(log nº cells/gram of faeces) | ||||||
| Akkermansia | 6.3 ± 2.2 | 5.6 ± 1.6 | 5.6 ± 2.1 | 0.026 | −0.143 | 0.264 |
| Bacteroides-Prevotella-Porphyromonas | 8.8 ± 1.3 | 8.9 ± 1.1 | 8.2 ± 1.2 | 0.067 | −0.245 | 0.052 |
| Bifidobacterium | 7.7 ± 2.0 | 8.2 ± 0.8 | 8.2 ± 0.7 | 0.090 | 0.126 | 0.305 |
| Clostridia cluster XIVa group | 7.7 ± 1.7 | 8.2 ± 1.3 | 8.4 ± 1.1 | 0.048 | 0.150 | 0.236 |
| Lactobacillus group | 5.7 ± 1.3 | 6.0 ± 1.1 | 6.7 ± 0.9 * | 0.194 | 0.256 | 0.029 |
| Faecalibacterium prausnitzii | 7.3 ± 1.0 | 7.5 ± 1.0 | 7.7 ± 0.9 | 0.024 | 0.152 | 0.233 |
Results derived from multivariate analysis are presented as mean ± standard deviation. Variables included in model 1: acetate, propionate, butyrate and energy; model 2: Akkermansia, Bacteroides-Prevotella-Porphyromonas, Bifidobacterium, Clostridia cluster XIVa, Lactobacillus group, Faecalibacterium prausnitzii and energy. Linear regression analyses are adjusted by energy; R2, coefficient of multiple determination; β, standardized regression coefficient. * p ≤ 0.05.
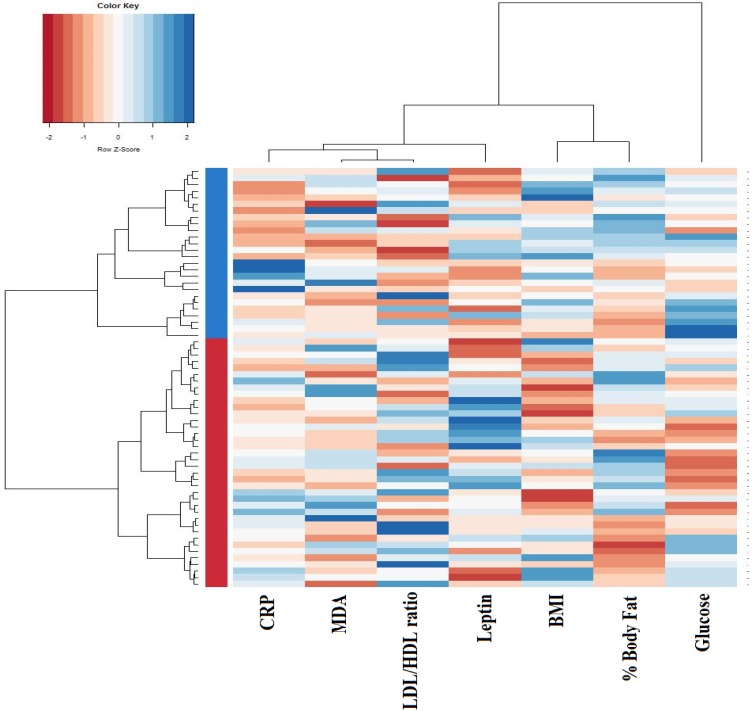
To explore whether the fecal microbiota may be related with the pro-oxidant and pro-inflammatory status frequently linked to obesity, subjects were classified into clusters performed by jointly considering values for BMI, fat mass, serum glucose, LDL/HDL ratio, serum leptin, MDA and CRP. This approach established two independent groups of individuals, thereafter referred to as cluster I (n = 38) and cluster II (n = 26) (Figure 1).
Figure 1.
Dendogram clustering based on individual body composition, serum glucose, lipid profile, and oxidative stress biomarkers. The heatmap shows the dendrogram classification for clusters, based on C reactive protein (CRP), malondialdehyde (MDA), LDL/HDL ratio, serum leptin, Body Mass Index (BMI), body fat percentage and serum glucose (columns). Colors in the vertical bar at the left of the heatmap identify Cluster I (red) and Cluster II (blue).
Cluster II was characterized by higher BMI and body fat together with higher concentration of serum glucose, MDA and CRP. The LDL/HDL ratio and serum leptin, however, did not show significant differences between both clusters (Table 4).
Table 4.
Differences in the parameters used for cluster analyses.
| Cluster I n = 38 |
Cluster II n = 26 |
p | |
|---|---|---|---|
| BMI (kg/m2) | 25.2 ± 2.7 | 30.3 ± 4.3 | <0.001 |
| Body fat (%) | 30.5 ± 8.0 | 42.3 ± 13.3 | <0.001 |
| Blood parameters | |||
| Serum glucose (mg/dL) | 92.7 ± 8.2 | 108.2 ± 10.9 | <0.001 |
| LDL/HDL ratio | 2.6 ± 0.8 | 2.5 ± 0.8 | 0.921 |
| Leptin (ng/mL) | 8.2 ± 5.1 | 10.8 ± 6.4 | 0.074 |
| MDA (μM) | 2.0 ± 0.6 | 2.8 ± 1.3 | 0.001 |
| CRP (mg/L) | 0.9 ± 0.9 | 6.7 ± 10.4 | 0.001 |
Univariate analysis was adjusted by gender and presented as mean ± standard deviation. LDL, low-density lipoprotein. HDL, high-density lipoprotein. MDA, malondialdehyde. CRP, C reactive protein.
When we compared the microbiota variables between both groups no significant differences were found for most of the microbial groups and SCFA studied, except for acetate, which displayed higher fecal concentration in cluster II, and the Bacteroides group whose levels resulted higher in cluster I (Table 5).
Table 5.
Differences in fecal SCFA and major microbial groups between clusters.
| Cluster I n = 37 |
Cluster II n = 24 |
|
|---|---|---|
| Model 1. Fecal SCFA concentration (mM) | ||
| Acetate | 35.8 ± 14.8 | 44.8 ± 17.7 * |
| Propionate | 14.0 ± 6.7 | 16.2 ± 7.3 |
| Butyrate | 11.1 ± 8.0 | 11.8 ± 7.7 |
| Model 2. Microbial target (log nº cells/gram of feces) | ||
| Akkermansia | 6.0 ± 1.8 | 5.6 ± 2.2 |
| Bacteroides-Prevotella-Porphyromonas | 9.0 ± 1.0 | 8.3 ± 1.3 * |
| Bifidobacterium | 8.1 ± 0.9 | 7.9 ± 1.8 |
| Clostridia cluster XIVa group | 7.9 ± 1.4 | 8.2 ± 1.4 |
| Lactobacillus group | 6.0 ± 1.1 | 6.1 ± 1.3 |
| Faecalibacterium prausnitzii | 7.4 ± 0.9 | 7.5 ± 0.9 |
Results derived from multivariate analysis are presented as mean ± standard deviation. Variables included in model 1: acetate, propionate, butyrate and energy; model 2: Akkermansia, Bacteroides-Prevotella-Porphyromonas, Bifidobacterium, Clostridia cluster XIVa, Lactobacillus group, Faecalibacterium prausnitzii and energy. * p ≤ 0.05.
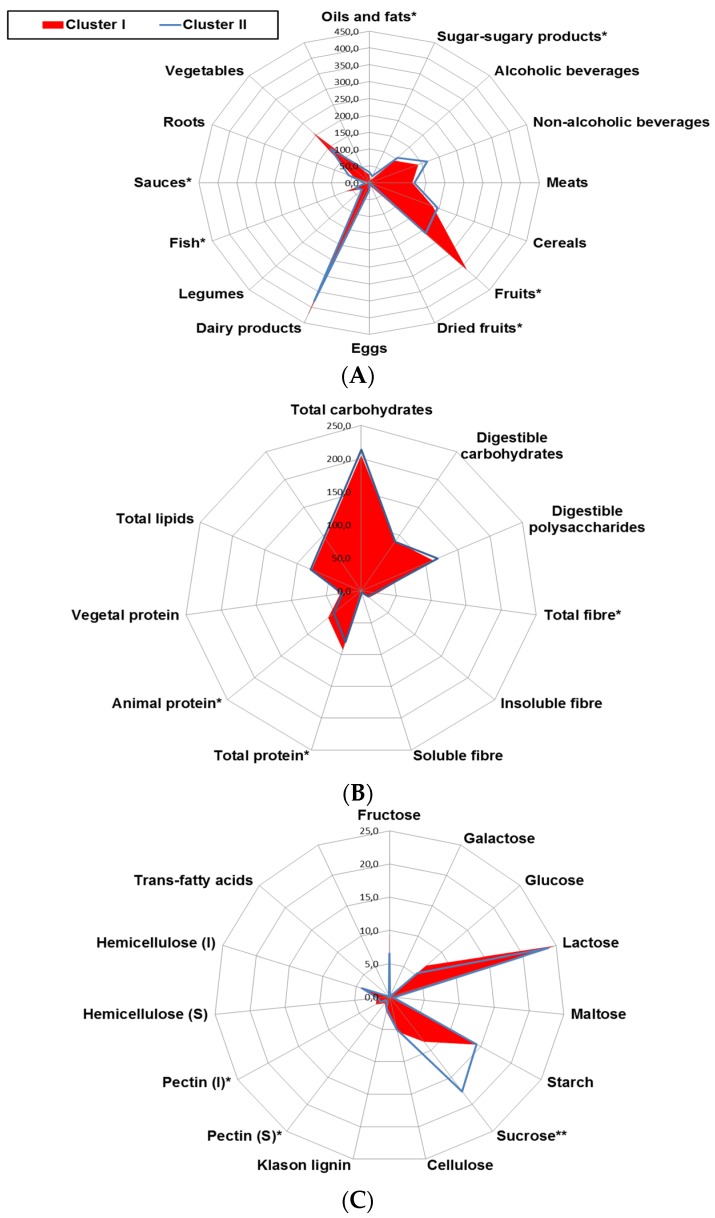
With the above information, and in order to evaluate whether differential daily consumption of foods may be related with the pro-oxidant and pro-inflammatory status linked to obesity, food groups and nutrient intake profiles were compared between clusters I and II (Figure 2). Cluster II was characterized by a profile with a higher intake of oils and fats, sweetened foods and sauces and lower intake of fruits, dried fruits, and fish, representative of a Western pattern (Figure 2A). Among nutrients, higher intake of sucrose and lower intake of fiber and total animal protein was observed in individuals from cluster II (Figure 2B,C).
Figure 2.
Radar plot representing differences in the daily intake of (A) major food groups (g/day); (B) macronutrient and fiber (g/day) and (C) detailed carbohydrate and fibers (g/day) among clusters. Cluster I (n = 38), Cluster II (n = 26). Multivariate regression analyses were adjusted by energy intake (Kcal/day). * p ≤ 0.05.
The intake of major antioxidants among clusters was also investigated (Table 6). Subjects from cluster II obtained lower total antioxidant capacity from diet, both for water soluble and fat soluble antioxidant compounds (hydrophilic and lipophilic ORAC, respectively). This group also had lower intake of total carotenoids, vitamin C, total polyphenols and flavonoids than cluster I.
Table 6.
Differences in the intake of the major dietary antioxidants between clusters.
| Cluster I n = 38 |
Cluster II n = 26 |
p | |
|---|---|---|---|
| ORAC, hydrophilic (μmol TE/day) | 10367 ± 6641 | 6089 ± 4179 | 0.004 |
| ORAC, lipophilic (μmol TE/day) | 244 ± 193 | 138 ± 103 | 0.011 |
| ORAC, Total (μmol TE/day) | 10609 ± 6790 | 6229 ± 4224 | 0.004 |
| Selenium (μg/day) | 123 ± 40.3 | 115 ± 43.6 | 0.250 |
| Total carotenoids (μg/day) | 2391 ± 1538 | 1660 ± 1001 | 0.034 |
| γ-Tocopherol (mg/day) | 2.6 ± 1.1 | 2.1 ± 2.2 | 0.249 |
| Vitamin C (mg/day) | 222 ± 196 | 131 ± 102 | 0.021 |
| Vitamin E (mg/day) | 10.1 ± 4.1 | 12.7 ± 8.2 | 0.063 |
| Total polyphenols (mg/day) | 2057 ± 1076 | 1553 ± 975 | 0.043 |
| Total flavonoids (mg/day) | 435 ± 291 | 303 ± 232 | 0.049 |
| Total phenolics (mg/day) | 198 ± 192 | 224 ± 236 | 0.626 |
| Flavanols (mg/day) | 222 ± 187 | 189 ± 194 | 0.505 |
Results adjusted by energy derived from multivariate analysis are presented as mean ± standard deviation. ORAC, Oxygen radical absorbance capacity. TE, Trolox equivalents.
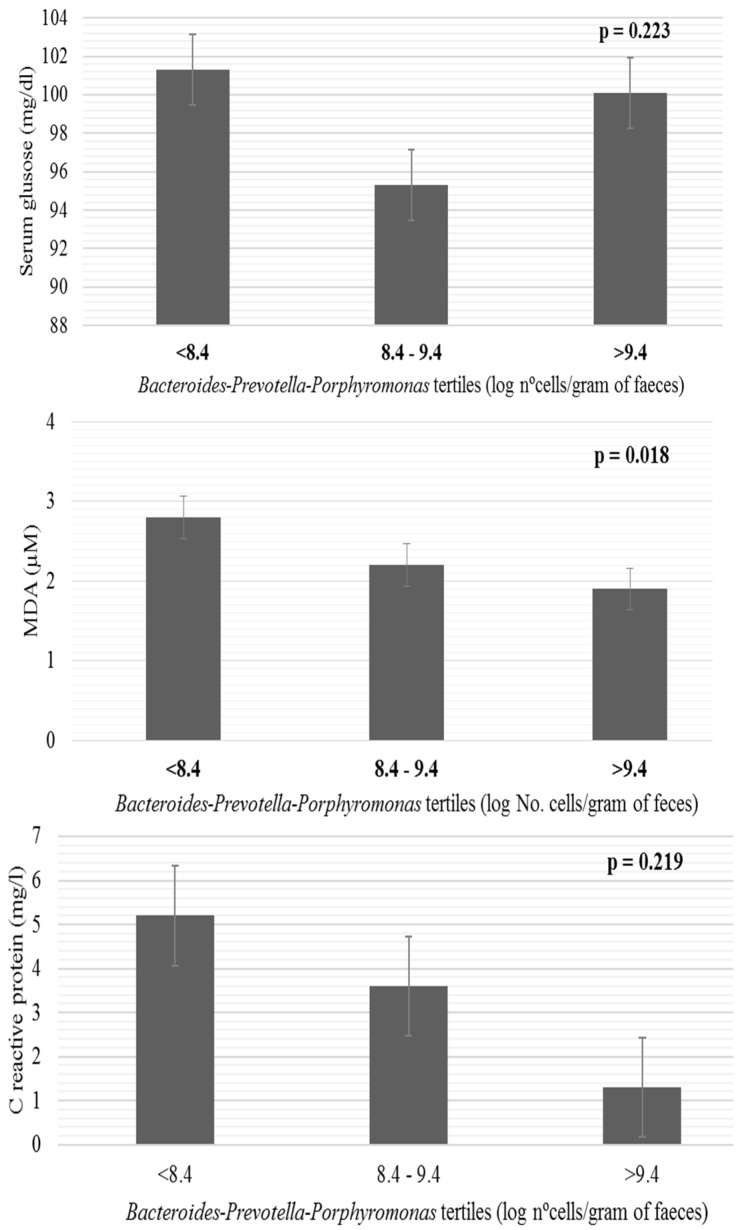
In order to elucidate the role of the fecal microbiota in the observed associations, differences in some biomarkers related to obesity according to the tertiles formed with the fecal levels of Bacteroides-Prevotella-Porphyromonas (log nº cells/gram of feces) were assessed (Figure 3). Higher serum concentrations of MDA were found across the tertiles of Bacteroides-Prevotella-Porphyromonas in relation with the decrease in abundance of this microbial group.
Figure 3.
Differences in blood parameters related to obesity according to the levels of Bacteroides-Prevotella-Porphyromonas tertiles (log nº cells/gram of feces). Bars represent mean and whiskers standard error derived from univariate analysis adjusted by energy. MDA, malondialdehyde.
4. Discussion
In line with previous evidence from other authors, an association between obesity and higher serum concentrations of leptin [35], MDA [3,36], CRP [3] and glucose was corroborated in our study. However, our work also provides novel insight into the differences found in some intestinal bacterial groups related to BMI and obesity-associated oxidative stress and inflammation in the general population. Furthermore, the identification of different dietary patterns in overweight and obese people, who have a more pro-oxidant and inflammatory status than the normal-weight group, points to the potential interest of designing strategies based on the consideration of the impact of a balanced diet (with high content of antioxidants in comparison with fats and refined sugars) on the microbiota, in order to improve or prevent obesity-associated disorders.
In recent years, hyperleptinemia has also been identified as an independent risk factor for cardiovascular disease and myocardial infarction [37,38] directly linked to inflammation [39] and oxidative stress [3,35]. In the present study, we have found that leptin level increased proportionally with the degree of obesity (Table 2) and is positively correlated with adiposity (Pearson correlation with the percentage of fat mass r = 0.590, p < 0.001, data not shown), its serum concentration being similar to that previously reported by other authors [40,41]. Higher serum levels of MDA and CRP have been previously reported in obesity and metabolic syndrome [42] and have also linked obesity to alterations in the lipoprotein particles profile as well as to increased lipid peroxidation, during which the MDA is one of the most abundant products formed [43,44,45,46,47]. In this way, our results regarding levels of MDA are in-line with previous findings and the levels of CRP corroborate studies relating to the presence of obesity with chronic low-grade inflammation [48]. In our sample the mean concentrations of MDA and CRP were higher in obese than in overweight and normal-weight groups, however the range observed for MDA was far from the cutoff points associated with increased risk of mortality by different causes [49]. It should be noted in the interpretation of these results that we have excluded people with cancer, autoimmune, or digestive diseases, as these are linked to oxidative stress. Despite the fact that the mechanisms linking oxidative damage to adipose tissue dysfunction remain largely unknown, we suggest that the MDA values determined in this study could reflect the degree of adipose oxidative stress [50]. Moreover, in agreement with our results, an increasing body of evidence supports the notion that diets high in glucose and fats, as occurs in obesity, may activate inflammatory signalling pathways in cells, potentially by increasing oxidative stress [51,52,53,54].
In recent years, it has been repeatedly reported that the gut microbiota in obese humans is different to that of lean people, both in terms of diversity and in the relative abundance of the dominant phyla Bacteroidetes and Firmicutes [55,56,57,58,59,60]. The different bacterial populations assessed in this study (Akkermansia, Bacteroides-Prevotella-Porphyromonas, Bifidobacterium, Clostridia cluster XIVa group (Lactobacillus group and Faecalibacterium prausnitzzi) represent more than 95% of the overall phylogenetic types of the human intestinal microbiota [8]. Our data identify the microorganisms related to Lactobacillus as a potential risk factor related with obesity. This result, that would have been surprising a few years ago, is in good agreement with some recent studies reporting higher levels of Lactobacillus in obese children [56] and adults [61]. Despite not reaching statistical significance, our results show a trend towards reduced levels of the Bacteroides-group in obese subjects. These observations are in good agreement with the increased Firmicutes/Bacteroidetes ratio [12] and the reduced Bacteroides levels repeatedly reported in obese subjects [57,60]. In addition, we found the majority of intestinal SCFA (acetate) to be another risk factor, with its levels increasing with BMI, which is in agreement with the higher levels of SCFA observed in obese subjects by other authors [15]. At this point, and based on the ability of the intestinal microbiota to act as an endocrine organ [50,56] we wonder to what extent this microbial ecosystem could be acting as a link between diet, systemic inflammation, metabolic dysfunction and obesity [62,63].
In this scenario, the traditional statistical analysis which considers the variables independently may be unrealistic when applied to complex biological systems; such is the case with obesity, in which there is a wide range of interrelated variables and mutually supporting disturbances. Therefore, we have gone one step further by evaluating the differences in the microbiota and dietary levels in those individuals in which different obesity-related factors occur together. The analyses of these obesity-related factors separated the individuals into two clusters. One of them (Cluster II) comprised the obese/over-weight participants showing higher serum concentrations of glucose, MDA and CRP. Interestingly, the negative association between Bacteroides and obesity reported previously by other authors [57,60,64] was also identified in our study when individuals were classified in clusters, while the association of Lactobacillus with obesity (BMI ≥ 30) did not raise statistical significance when also considering oxidative stress and inflammation related parameters.
Both obesity and dietary patterns have been shown to be related to changes in gut microbiota composition [65,66]. Therefore, when analyzing the differences in diets between clusters I and II, it was not surprising that the higher intake of fat and oils and sweetened foods, suggestive of consuming a highly palatable diet, was associated with the presence of a chronic pro-inflammatory and pro-oxidant status linked to overweight and obese subjects from cluster II [67,68,69,70,71,72,73]. The mechanisms by which dietary components may produce changes at the microbiota level remain largely unknown. However, considering both our results and the evidence from experimental studies with germ free animals receiving a diet high in fats and sucrose, it is likely that the impact of these foods in obesity and related pathologies is mediated through microbiota modulation [74]. This is supported by the fact that we found an inverse association between the levels of MDA and those of the Bacteroides group.
In addition, the reduced intake of fruits, which have a known anti-obesogenic effect, could be also linked to changes in the microbiota composition. Vegetables and fruits were the major dietary sources of pectin in our cohort [23] which can be metabolized in the colon by bacteria such as Bacteroides resulting in the production of SCFA [75] that may exert different beneficial effects on the host [76]. Moreover, in our studied population, vegetables and fruits were also the main sources of vitamin C and carotenoids, compounds that have a known anti-inflammatory activity and also provide other bioactive compounds, such as polyphenols, that are involved in the regulation of some metabolic conditions linked to obesity [77,78] and inflammation [78]. Considering these preliminary results, we hypothesize that the Bacteroides group could act as a mediator in antioxidant metabolism, playing a key role in some of the health effects attributed to these compounds.
The limited sample size of this study may have somewhat hampered our ability to detect other significant associations. Moreover, although FFQ is the most suitable tool to describe long-term habits, its ability to accurately quantify the dietary intake is limited. In addition, fecal SCFA measurements comprise only the 5% to 10% that is not absorbed in the colon [75]. These facts underline the difficulty of drawing firm conclusions from the studies conducted in this area of research.
Acknowledgments
This work was funded through the Grant GRUPIN14-043 “Microbiota Humana, Alimentación y Salud” funded by “Plan Regional de Investigación del Principado de Asturias”, Spain, by grants AGL2010-14952 from Spanish “Plan Nacional I + D + I”, by Biopolis group S.L., Valencia, within the framework of the e-CENIT Project SENIFOOD from the Spanish Ministry of Science and Innovation, and by the Alimerka Foundation. NS was the recipient of a postdoctoral contract supported by a Clarín regional grant (ACB 14-08) cofinanced by the Marie Curie CoFund European Program and IG-D benefits for a grant supported by Fundación Universia. Regional and national grants received cofounding from European Union FEDER funds. We show our greatest gratitude to all the volunteers participating in the study.
Author Contributions
S.G. performed most of the experimental procedures. T.F.-N., I.G.-D. and S.G. were involved in the nutritional assessments, anthropometrical measurements and collection of samples. N.S., M.G., C.G.d.l.R.-G. and S.G. provided biological samples, performed microbiological analyses and financial support. T.F.-N., I.G.-D. and S.G. drafted the manuscript. All authors participated in the study design and data interpretation, reviewed the manuscript and approved the final version.
Conflicts of Interest
The authors declared no potential competing financial interests concerning this study. Funders had no role in study conception, design, analysis of the results or decision to publish.
References
- 1.Becer E., Cirakoglu A. Association of the Ala16Val MnSOD gene polymorphism with plasma leptin levels and oxidative stress biomarkers in obese patients. Gene. 2015;568:35–39. doi: 10.1016/j.gene.2015.05.009. [DOI] [PubMed] [Google Scholar]
- 2.Furukawa S., Fujita T., Shimabukuro M., Iwaki M., Yamada Y., Nakajima Y., Nakayama O., Makishima M., Matsuda M., Shimomura I. Increased oxidative stress in obesity and its impact on metabolic syndrome. J. Clin. Investig. 2004;114:1752–1761. doi: 10.1172/JCI21625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hopps E., Noto D., Caimi G., Averna M.R. A novel component of the metabolic syndrome: The oxidative stress. Nutr. Metab. Cardiovasc. Dis. 2010;20:72–77. doi: 10.1016/j.numecd.2009.06.002. [DOI] [PubMed] [Google Scholar]
- 4.Vincent H.K., Taylor A.G. Biomarkers and potential mechanisms of obesity-induced oxidant stress in humans. Int. J. Obes. 2006;30:400–418. doi: 10.1038/sj.ijo.0803177. [DOI] [PubMed] [Google Scholar]
- 5.Pego-Fernandes P.M., Bibas B.J., Deboni M. Obesity: The greatest epidemic of the 21st century? Sao Paulo Med. J. 2011;129:283–284. doi: 10.1590/S1516-31802011000500001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sonnenburg E.D., Smits S.A., Tikhonov M., Higginbottom S.K., Wingreen N.S., Sonnenburg J.L. Diet-induced extinctions in the gut microbiota compound over generations. Nature. 2016;529:212–215. doi: 10.1038/nature16504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sonnenburg J.L., Xu J., Leip D.D., Chen C.H., Westover B.P., Weatherford J., Buhler J.D., Gordon J.I. Glycan foraging in vivo by an intestine-adapted bacterial symbiont. Science. 2005;307:1955–1959. doi: 10.1126/science.1109051. [DOI] [PubMed] [Google Scholar]
- 8.Yatsunenko T., Rey F.E., Manary M.J., Trehan I., Dominguez-Bello M.G., Contreras M., Magris M., Hidalgo G., Baldassano R.N., Anokhin A.P., et al. Human gut microbiome viewed across age and geography. Nature. 2012;486:222–227. doi: 10.1038/nature11053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Broussard J.L., Devkota S. The changing microbial landscape of Western society: Diet, dwellings and discordance. Mol. Metab. 2016;5:737–742. doi: 10.1016/j.molmet.2016.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.De Filippis F., Pellegrini N., Vannini L., Jeffery I.B., La Storia A., Laghi L., Serrazanetti D.I., Di Cagno R., Ferrocino I., Lazzi C., et al. High-level adherence to a Mediterranean diet beneficially impacts the gut microbiota and associated metabolome. Gut. 2015 doi: 10.1136/gutjnl-2015-309957. [DOI] [PubMed] [Google Scholar]
- 11.Haro C., Montes-Borrego S.M., Rangel-Zúñiga O.A., Alcalá-Díaz J.F., Gómez-Delgado F., Pérez-Martínez P., Delgado-Lista J., Quintana-Navarro G.M., Tinahones F.J., Landa B.B., et al. Two healthy diets modulate gut microbial community improving insulin sensitivity in a human obese population. J. Clin. Endocrinol. Metab. 2016;101:233–242. doi: 10.1210/jc.2015-3351. [DOI] [PubMed] [Google Scholar]
- 12.De los Reyes-Gavilán C.G., Delzenne N.M., González S., Gueimonde M., Salazar N. Development of functional foods to fight against obesity: Opportunities for probiotics and prebiotics. Agro FOOD Ind. Hi Tech. 2014;25:35–39. [Google Scholar]
- 13.Ley R.E., Backhed F., Turnbaugh P., Lozupone C.A., Knight R.D., Gordon J.I. Obesity alters gut microbial ecology. Proc. Natl. Acad. Sci. USA. 2005;102:11070–11075. doi: 10.1073/pnas.0504978102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Turnbaugh P.J., Backhed F., Fulton L., Gordon J.I. Diet-induced obesity is linked to marked but reversible alterations in the mouse distal gut microbiome. Cell Host Microbe. 2008;3:213–223. doi: 10.1016/j.chom.2008.02.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Samuel B.S., Shaito A., Motoike T., Rey F.E., Backhed F., Manchester J.K., Hammer R.E., Williams S.C., Crowley J., Yanagisawa M., et al. Effects of the gut microbiota on host adiposity are modulated by the short-chain fatty-acid binding G protein-coupled receptor, Gpr41. Proc. Natl. Acad. Sci. USA. 2008;105:16767–16772. doi: 10.1073/pnas.0808567105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Den Besten G., van Eunen K., Groen A.K., Venema K., Reijngoud D.J., Bakker B.M. The role of short-chain fatty acids in the interplay between diet, gut microbiota, and host energy metabolism. J. Lipid Res. 2013;54:2325–2340. doi: 10.1194/jlr.R036012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Schwiertz A., Taras D., Schafer K., Beijer S., Bos N.A., Donus C., Hardt P.D. Microbiota and SCFA in lean and overweight healthy subjects. Obesity. 2010;18:190–195. doi: 10.1038/oby.2009.167. [DOI] [PubMed] [Google Scholar]
- 18.Clarke G., Stilling R.M., Kennedy P.J., Stanton C., Cryan J.F., Dinan T.G. Minireview: Gut microbiota: The neglected endocrine organ. Mol. Endocrinol. 2014;28:1221–1238. doi: 10.1210/me.2014-1108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Turnbaugh P.J., Ley R.E., Mahowald M.A., Magrini V., Mardis E.R., Gordon J.I. An obesity-associated gut microbiome with increased capacity for energy harvest. Nature. 2006;444:1027–1031. doi: 10.1038/nature05414. [DOI] [PubMed] [Google Scholar]
- 20.Den Besten G., Havinga R., Bleeker A., Rao S., Gerding A., van Eunen K., Groen A.K., Reijngoud D., Bakker B.M. The short-chain fatty acid uptake fluxes by mice on a guar gum supplemented diet associate with amelioration of major biomarkers of the metabolic syndrome. PLoS ONE. 2014;9:e107392. doi: 10.1371/journal.pone.0107392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lean M.E., Malkova D. Altered gut and adipose tissue hormones in overweight and obese individuals: Cause or consequence? Int. J. Obes. 2016;40:622–632. doi: 10.1038/ijo.2015.220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Salas-Salvadó J., Rubio M.A., Barbany M., Moreno B. SEEDO 2007 Consensus for the evaluation of overweight and obesity and the establishment of therapeutic intervention criteria. Med. Clin. 2007;128:184–196. doi: 10.1016/S0025-7753(07)72531-9. [DOI] [PubMed] [Google Scholar]
- 23.Cuervo A., Valdés L., Salazar N., de los Reyes-Gavilán C.G., Ruas-Madiedo P., Gueimonde M., González S. Pilot study of diet and microbiota: Interactive associations of fibers and polyphenols with human intestinal bacteria. J. Agric. Food Chem. 2014;62:5330–5336. doi: 10.1021/jf501546a. [DOI] [PubMed] [Google Scholar]
- 24.Cuervo A., Hevia A., López P., Suárez A., Sánchez B., Margolles A., González S. Association of polyphenols from oranges and apples with specific intestinal microorganisms in systemic lupus erythematosus patients. Nutrients. 2015;7:1301–1317. doi: 10.3390/nu7021301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Centro de Enseñanza Superior de Nutrición Humana y Dietética (CESNID) Tablas de Composición de Alimentos por Medidas Caseras de Consumo Habitual en España. McGraw-Hill, Plublicaciones y Ediciones de la Universidad de Barcelona; Barcelona, Spain: 2008. [Google Scholar]
- 26.United States Department of Agriculture (USDA) Agriculture Research Service, 2016 USDA National Nutrient Database for Standard References. [(accessed on 15 March 2017)]; Available online: http://www.ars.usda.gov/services/docs.htm?docid=8964.
- 27.Marlett J.A., Cheung T.F. Database and quick methods of assessing typical dietary fiber intakes using data for 228 commonly consumed foods. J. Am. Diet. Assoc. 1997;97:1139–1151. doi: 10.1016/S0002-8223(97)00275-7. [DOI] [PubMed] [Google Scholar]
- 28.Neveu V., Perez-Jiménez J., Vos F., Crespy V., Chaffaut L.D., Mennen L., Knox C., Eisner R., Cruz J., Wishart D., et al. Phenol-Explorer: An online comprehensive database on polyphenol contents in foods. Database Oxf. 2010:bap024. doi: 10.1093/database/bap024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.United States Department of Agriculture (USDA) U.S. Dep. Agric; 2017. [(accessed on 14 March 2017)]. Database for the Oxigen Radical Absorbance Capacity (ORAC) of Selected Foods. Available online: http://www.ars.usda.gov/ba/bhnrc/ndl. [Google Scholar]
- 30.Harris J.A., Benedict F.G. A biometric study of human basal metabolism. Proc. Natl. Acad. Sci. USA. 1918;4:370–373. doi: 10.1073/pnas.4.12.370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gerard-Monnier D., Erdelmeier I., Regnard K., Moze-Henry N., Yadan J.C., Chaudiere J. Reactions of 1-methyl-2-phenylindole with malondialdehyde and 4-hydroxyalkenals. Analytical applications to a colorimetric assay of lipid peroxidation. Chem. Res. Toxicol. 1998;11:1176–1183. doi: 10.1021/tx9701790. [DOI] [PubMed] [Google Scholar]
- 32.Arboleya S., Binetti A., Salazar N., Fernández N., Solis G., Hernández-Barranco A., Margolles A., de los Reyes-Gavilán C.G., Gueimonde M. Establishment and development of intestinal microbiota in preterm neonates. FEMS Microbiol. Ecol. 2012;79:763–772. doi: 10.1111/j.1574-6941.2011.01261.x. [DOI] [PubMed] [Google Scholar]
- 33.Ramirez-Farias C., Slezak K., Fuller Z., Duncan A., Holtrop G., Louis P. Effect of inulin on the human gut microbiota: Stimulation of Bifidobacterium adolescentis and Faecalibacterium prausnitzii. Br. J. Nutr. 2009;101:541–550. doi: 10.1017/S0007114508019880. [DOI] [PubMed] [Google Scholar]
- 34.Salazar N., Gueimonde M., Hernández-Barranco A.M., Ruas-Madiedo P., de los Reyes-Gavilán C.G. Exopolysaccharides produced by intestinal Bifidobacterium strains act as fermentable substrates for human intestinal bacteria. Appl. Environ. Microbiol. 2008;74:4737–4745. doi: 10.1128/AEM.00325-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pandey G., Shihabudeen M.S., David H.P., Thirumurugan E., Thirumurugan K. Association between hyperleptinemia and oxidative stress in obese diabetic subjects. J. Diabetes Metab. Disord. 2015;14:24. doi: 10.1186/s40200-015-0159-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lee S.M., Cho Y.H., Lee S.Y., Jeong D.W., Cho A.R., Jeon J.S., Park E.J., Kim Y.J., Lee J.G., Yi Y.H., et al. Urinary malondialdehyde is associated with visceral abdominal obesity in middle-aged men. Mediat. Inflamm. 2015;2015:524291. doi: 10.1155/2015/524291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gundala R., Chava V.K., Ramalingam K. Association of leptin in periodontitis and acute myocardial infarction. J. Periodontol. 2014;85:917–924. doi: 10.1902/jop.2012.110620. [DOI] [PubMed] [Google Scholar]
- 38.Karbowska J., Kochan Z. Leptin as a mediator between obesity and cardiac dysfunction. Postepy Hig. Med. Dosw. 2012;66:267–274. doi: 10.5604/17322693.997817. [DOI] [PubMed] [Google Scholar]
- 39.Paepegaey A.C., Genser L., Bouillot J.C., Oppert J.M., Clément K., Poitou C. High levels of CRP in morbid obesity: The central role of adipose tissue and lessons for clinical practice before and after bariatric surgery. Surg. Obes. Relat. Dis. 2015;11:148–154. doi: 10.1016/j.soard.2014.06.010. [DOI] [PubMed] [Google Scholar]
- 40.Havel P.J., Kasim-Karakas S., Dubuc G.R., Mueller W., Phinney S.D. Gender differences in plasma leptin concentrations. Nat. Med. 1996;2:949–950. doi: 10.1038/nm0996-949b. [DOI] [PubMed] [Google Scholar]
- 41.Saad M.F., Riad-Gabriel M.G., Khan A., Sharma A., Michael R., Jinagouda S.D., Boyadjian R., Steil G.M. Diurnal and ultradian rhythmicity of plasma leptin: Effects of gender and adiposity. J. Clin. Endocrinol. Metab. 1998;83:453–459. doi: 10.1210/jc.83.2.453. [DOI] [PubMed] [Google Scholar]
- 42.Piccoli de Melo L.G., Vargas Nunes S.O., Anderson G., Vargas H.O., Barbosa D.S., Galecki P., Carvalho A.F., Maes M. Shared metabolic and immune-inflammatory, oxidative and nitrosative stress pathways in the metabolic syndrome and mood disorders. Prog Neuro-Psychopharmacol. Biol. Psychiatry. 2017;17 doi: 10.1016/j.pnpbp.2017.04.027. [DOI] [PubMed] [Google Scholar]
- 43.Solomon C.G., Manson J.E. Obesity and mortality: A review of the epidemiologic data. Am. J. Clin. Nutr. 1997;66:1044–1050. doi: 10.1093/ajcn/66.4.1044S. [DOI] [PubMed] [Google Scholar]
- 44.World Health Organisation . Obesity: Preventing and Managing the Global Epidemic. Volume 894. World Health Organisation; Geneva, Switzerland: 2000. (Report of a WHO Consultation. WHO Technical Report Series 894, World Health Organization Technical Report Series). [PubMed] [Google Scholar]
- 45.He Q.R., Yu T., Fau-Li P., Li P. Association of oxidative stress and serum adiponectine in patients with metabolic syndrome. Sichuan Da Xue Xue Bao Yi Xue Ban. 2009;40:623–627. [PubMed] [Google Scholar]
- 46.Maes M., Ruckoanich P., Fau-Chang Y.S., Chang Y.S., Fau-Mahanonda N., Mahanonda N., Fau-Berk M., Berk M. Multiple aberrations in shared inflammatory and oxidative & nitrosative stress (IO&NS) pathways explain the co-association of depression and cardiovascular disorder (CVD), and the increased risk for CVD and due mortality in depressed patients. Prog. Neuro-Psychopharmacol. Biol. Psychiatry. 2011;35:769–783. doi: 10.1016/j.pnpbp.2010.06.008. [DOI] [PubMed] [Google Scholar]
- 47.Sankhla M., Sharma T.K., Fau-Mathur K., Mathur K., Fau-Rathor J.S., Rathor J.S., Fau-Butolia V., Butolia V., Fau-Gadhok A.K., Gadhok A.K., et al. Relationship of oxidative stress with obesity and its role in obesity induced metabolic syndrome. Clin. Lab. 2012;58:385–392. [PubMed] [Google Scholar]
- 48.Illán-Gómez F., Gonzálvez-Ortega M., Aragón-Alonso A., Orea-Soler I., Alcatraz-Tafalla M.S., Pérez-Paredes M., Lozano-Almeda M.L. Obesity, endothelial function and inflammation: The effects of weight loss after bariatric surgery. Nutr. Hosp. 2016;33:1340–1346. doi: 10.20960/nh.793. [DOI] [PubMed] [Google Scholar]
- 49.Proctor P.H., Reynolds E.S. Free radicals and disease in man. Physiol. Chem. Phys. Med. NMR. 1984;16:175–195. [PubMed] [Google Scholar]
- 50.Murdolo G., Piroddi M., Luchetti F., Tortoioli C., Canonico B., Zerbinati C., Galli F., Iuliano L. Oxidative stress and lipid peroxidation by-products at the crossroad between adipose organ dysregulation and obesity-linked insulin resistance. Biochimie. 2013;95:585–594. doi: 10.1016/j.biochi.2012.12.014. [DOI] [PubMed] [Google Scholar]
- 51.Gregor M.F., Hotamisligil G.S. Inflammatory mechanisms in obesity. Annu. Rev. Immunol. 2011;29:415–445. doi: 10.1146/annurev-immunol-031210-101322. [DOI] [PubMed] [Google Scholar]
- 52.Belza A., Toubro S., Stender S., Astrup A. Effect of diet-induced energy deficit and body fat reduction on high-sensitive CRP and other inflammatory markers in obese subjects. Int. J. Obes. 2009;33:456–464. doi: 10.1038/ijo.2009.27. [DOI] [PubMed] [Google Scholar]
- 53.Aljada A., Mohanty P., Ghanim H., Abdo T., Tripathy D., Chaudhuri A., Dandona P. Increase in intranuclear nuclear factor κB and decrease in inhibitor κB inmononuclear cells after a mixed meal: Evidence for a proinflammatory effect. Am. J. Clin. Nutr. 2004;79:682–690. doi: 10.1093/ajcn/79.4.682. [DOI] [PubMed] [Google Scholar]
- 54.Dalmas E., Rouault C., Abdennour M., Rovere C., Rizkalla S., Bar-Hen A., Nahon J.L., Bouillot J.L., Guerre-Millo M., Clément K., et al. Variations in circulating inflammatory factors are related to changes in calorie and carbohydrate intakes early in the course of surgery-induced weight reduction. Am. J. Clin. Nutr. 2011;94:450–458. doi: 10.3945/ajcn.111.013771. [DOI] [PubMed] [Google Scholar]
- 55.Abdallah I.N., Ragab S.H., Abd E.A., Shoeib A.R., Alhosary Y., Fekry D. Frequency of Firmicutes and Bacteroidetes in gut microbiota in obese and normal weight Egyptian children and adults. Arch. Med. Sci. 2011;7:501–507. doi: 10.5114/aoms.2011.23418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Bervoets L., Van H.K., Kortleven I., Van N.C., Hens N., Vael C., Goossens H., Desager K.N., Vankerckhoven V. Differences in gut microbiota composition between obese and lean children: A cross-sectional study. Gut Pathog. 2013;5:10. doi: 10.1186/1757-4749-5-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Duca F.A., Sakar Y., Lepage P., Devime F., Langelier B., Dore J., Covasa M. Replication of obesity and associated signaling pathways through transfer of microbiota from obese-prone rats. Diabetes. 2014;63:1624–1636. doi: 10.2337/db13-1526. [DOI] [PubMed] [Google Scholar]
- 58.Harris K., Kassis A., Major G., Chou C.J. Is the gut microbiota a new factor contributing to obesity and its metabolic disorders? J. Obes. 2012;2012:879151. doi: 10.1155/2012/879151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Hartstra A.V., Bouter K.E., Backhed F., Nieuwdorp M. Insights into the role of the microbiome in obesity and type 2 diabetes. Diabetes Care. 2015;38:159–165. doi: 10.2337/dc14-0769. [DOI] [PubMed] [Google Scholar]
- 60.Park J.S., Seo J.H., Youn H.S. Gut microbiota and clinical disease: Obesity and nonalcoholic fatty liver disease. Pediatr. Gastroenterol. Hepatol. Nutr. 2013;16:22–27. doi: 10.5223/pghn.2013.16.1.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Million M., Maraninchi M., Henry M., Armougom F., Richet H., Carrieri P., Valero R., Raccah D., Vialettes B., Raoult D. Obesity-associated gut microbiota is enriched in Lactobacillus reuteri and depleted in Bifidobacterium animalis and Methanobrevibacter smithii. Int. J. Obes. 2012;36:817–825. doi: 10.1038/ijo.2011.153. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 62.Escobedo G., López-Ortíz E., Torres-Castro I. Gut microbiota as a key player in triggering obesity, systemic inflammation and insulin resistance. Rev. Investig. Clin. 2014;66:450–459. [PubMed] [Google Scholar]
- 63.Sanz Y., Santacruz A., Gauffin P. Gut microbiota in obesity and metabolic disorders. Proc. Nutr. Soc. 2010;69:434–441. doi: 10.1017/S0029665110001813. [DOI] [PubMed] [Google Scholar]
- 64.Chakraborti C.K. New-found link between microbiota and obesity. World J. Gastrointest. Pathophysiol. 2015;6:110–119. doi: 10.4291/wjgp.v6.i4.110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.David L.A., Maurice C.F., Carmody R.N., Gootenberg D.B., Button J.E., Wolfe B.E., Ling A.V., Devlin A.S., Varma Y., Fischbach M.A., et al. Diet rapidly and reproducibly alters the human gut microbiome. Nature. 2014;505:559–563. doi: 10.1038/nature12820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Turnbaugh P.J., Ridaura V.K., Faith J.J., Rey F.E., Knight R., Gordon J.I. The effect of diet on the human gut microbiome: A metagenomic analysis in humanized gnotobiotic mice. Sci. Transl. Med. 2009;1:6ra14. doi: 10.1126/scitranslmed.3000322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Da R.R., Assaloni R., Ceriello A. Postprandial hyperglycemia and diabetic complications. Recenti Prog. Med. 2005;96:436–444. [PubMed] [Google Scholar]
- 68.Hennig B., Toborek M., McClain C.J. High-energy diets, fatty acids and endothelial cell function: Implications for atherosclerosis. J. Am. Coll. Nutr. 2001;20:97–105. doi: 10.1080/07315724.2001.10719021. [DOI] [PubMed] [Google Scholar]
- 69.Klop B., Proctor S.D., Mamo J.C., Botham K.M., Castro C.M. Understanding postprandial inflammation and its relationship to lifestyle behaviour and metabolic diseases. Int. J. Vasc. Med. 2012;2012:947417. doi: 10.1155/2012/947417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Nappo F., Esposito K., Cioffi M., Giugliano G., Molinari A.M., Paolisso G., Marfella R., Giugliano D. Postprandial endothelial activation in healthy subjects and in type 2 diabetic patients: Role of fat and carbohydrate meals. J. Am. Coll. Cardiol. 2002;39:1145–1150. doi: 10.1016/S0735-1097(02)01741-2. [DOI] [PubMed] [Google Scholar]
- 71.Ong P.J., Dean T.S., Hayward C.S., Della Monica P.L., Sanders T.A., Collins P. Effect of fat and carbohydrate consumption on endothelial function. Lancet. 1999;354:2134. doi: 10.1016/S0140-6736(99)03374-7. [DOI] [PubMed] [Google Scholar]
- 72.Roberts C.K., Barnard R.J., Sindhu R.K., Jurczak M., Ehdaie A., Vaziri N.D. Oxidative stress and dysregulation of NAD(P)H oxidase and antioxidant enzymes in diet-induced metabolic syndrome. Metabolism. 2006;55:928–934. doi: 10.1016/j.metabol.2006.02.022. [DOI] [PubMed] [Google Scholar]
- 73.Wallace J.P., Johnson B., Padilla J., Mather K. Postprandial lipaemia, oxidative stress and endothelial function: A review. Int. J. Clin. Pract. 2010;64:389–403. doi: 10.1111/j.1742-1241.2009.02146.x. [DOI] [PubMed] [Google Scholar]
- 74.Sonnenburg J.L., Backhed F. Diet-microbiota interactions as moderators of human metabolism. Nature. 2016;535:56–64. doi: 10.1038/nature18846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Topping D.L., Clifton P.M. Short-chain fatty acids and human colonic function: Roles of resistant starch and nonstarch polysaccharides. Physiol. Rev. 2001;81:1031–1064. doi: 10.1152/physrev.2001.81.3.1031. [DOI] [PubMed] [Google Scholar]
- 76.Ríos-Covián D., Ruas-Madiedo P., Margolles A., Gueimonde M., de los Reyes-Gavilán C.G., Salazar N. Intestinal short chain fatty acids and their link with diet and human health. Front. Microbiol. 2016;7:185. doi: 10.3389/fmicb.2016.00185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Boque N., Campion J., de la Iglesia R., de la Garza A.L., Milagro F.I., San R.B., Banuelos O., Martínez J.A. Screening of polyphenolic plant extracts for anti-obesity properties in Wistar rats. J. Sci. Food Agric. 2013;93:1226–1232. doi: 10.1002/jsfa.5884. [DOI] [PubMed] [Google Scholar]
- 78.Shen C.L., Cao J.J., Dagda R.Y., Chanjaplammootil S., Lu C., Chyu M.C., Gao W., Wang J.S., Yeh J.K. Green tea polyphenols benefits body composition and improves bone quality in long-term high-fat diet-induced obese rats. Nutr. Res. 2012;32:448–457. doi: 10.1016/j.nutres.2012.05.001. [DOI] [PubMed] [Google Scholar]