Abstract
Objectives
For patients undergoing inpatient otolaryngologic surgery, determine patient and hospital-level risk factors associated with 30-day readmission.
Study Design
Retrospective cohort study
Methods
We analyzed the State Inpatient Database (SID) from California for patients who underwent otolaryngologic surgery between 2008 and 2010. Readmission rates, readmission diagnoses, and patient- and hospital-level risk factors for 30-day readmission were determined. Hierarchical logistic regression modeling was performed to identify procedure-, patient-, and hospital-level risk factors for 30-day readmission.
Results
The 30-day readmission rate following an inpatient otolaryngology procedure was 8.1%. The most common readmission diagnoses were nutrition, metabolic or electrolyte problems (44% of readmissions) and surgical complications (10% of readmissions). New complications after discharge were the major drivers of readmission. Variables associated with 30-day readmission in hierarchical logistic regression modeling were: type of otolaryngologic procedure, Medicare or Medicaid health insurance, chronic anemia, chronic lung disease, chronic renal failure, index admission via the emergency department, in-hospital complication during the index admission, and discharge destination other than home.
Conclusions
Approximately one out of twelve patients undergoing otolaryngologic surgery had a 30-day readmission. Readmissions occur across a variety of types of procedures and hospitals. Most of the variability was driven by patient-specific factors, not structural hospital characteristics.
Keywords: readmissions, quality, health policy, complications, State Inpatient Database
Introduction
Because hospital readmissions are a metric of quality care and a source of financial penalties, there has been a burgeoning research effort to analyze readmissions for surgical patients1–7. Studies outside of otolaryngology have demonstrated that readmission rates following a variety of surgical procedures vary widely between hospitals4,5. It is unclear whether this variation is due to differences in clinical risk factors or differences related to hospital characteristics and provision of care.
There have been few publications on readmission following inpatient otolaryngologic surgery8–12. The existing otolaryngology readmissions research has suffered limitations relating to lack of generalizability (e.g. single institution, only academic hospitals, or only cancer patients), small sample size, and inability to track readmissions outside of the surgical institution. In the non-otolaryngology surgical literature, readmissions outside of the institution where the surgery occurred are common13, even for tertiary care centers14.
There are thus significant knowledge gaps about readmission following otolaryngologic surgery. It is unknown whether 30-day readmission rates for otolaryngology surgical patients vary between hospitals. The reasons for readmission following otolaryngologic surgery, and their relationship to complications have not been elucidated. The relative contribution of patient-level risk factors versus structural hospital characteristics is in explaining readmission rate variability following otolaryngologic surgery has not been analyzed.
To present a more comprehensive analysis of hospital readmission following inpatient otolaryngologic surgery, we used the State Inpatient Database (SID) from California. The California SID, available through the Healthcare Cost and Utilization Project (HCUP), is a database that captures all inpatient discharge records from acute care community hospitals in California for a given year, regardless of payer15. It provides over 100 patient-level variables and allows patients to be tracked longitudinally, permitting identification of hospital readmissions. Using the California SID, we attempted to answer the following questions in a heterogeneous group of patients undergoing hospital admission following an otolaryngologic procedure: 1) What are the reasons for readmission? 2) Do hospital readmission rates vary between hospitals? 3) Which patient- and hospital-level variables are risk factors for readmission? 4) What is the relative contribution of patient level versus hospital-level risk factors in explaining variability in readmission rates between hospitals?
Materials and Methods
Data Source and Study Population
The study was granted exempt status by the Washington University School of Medicine Institutional Review Board and Human Research Protections Office. Data was obtained from the SID for California from 2008–2010. At the time data collection for this study commenced, California SID data were available through 2011. The study end-date was chosen as December 2010 to allow for tracking of readmissions following surgery in December 2010 that would occur in January 2011. A start date of 2008 was chosen for the study to capture three years worth of data, which provided a sufficient population size.
The SID is part of a family of databases maintained by the Healthcare Cost and Utilization Project sponsored by the Agency for Healthcare Research and Quality (AHRQ)15. California SID was chosen for the study because it contains encrypted personal identifiers that allow longitudinal follow-up. In addition, information on hospitals is publically available for California, which allowed analysis of hospital characteristics. Data about structural hospital characteristics were obtained from the Hospital Annual Utilization Data available through the California Office of Statewide Health Planning and Development and linked to the SID data by hospital identifier.16
International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) procedure codes were used to identify hospital discharges for patients ≥ 18 years of age undergoing an otolaryngology procedure in California between 2008 and 2010. Procedures were chosen to capture the breadth of otolaryngology procedures without capturing patients who are not truly otolaryngology inpatients but undergo an “otolaryngology” procedure during the hospitalization (e.g. control of epistaxis in a patient admitted for a bone marrow transplant). If a patient underwent more than one type of otolaryngology surgery during the index hospitalization, the sub-specialty was assigned based on clinical relevance. The ICD-9-CM codes and classification of procedures by otolaryngology subspecialty are listed in Table 1. “General” otolaryngology procedures consisted of operations on the salivary glands, drainage of abscesses, and operations of the pharynx (for non-malignant disease, such as tonsillectomy) (ICD-9-CM codes ‘26′, ‘27′, 28′, and ‘29′). Hospitalizations were excluded if the patient died during the index admission or if data on age, gender, personal identifier, or length of stay (LOS) were missing. Inpatient admissions of persons with out-of-state residence were excluded due to potential loss of follow up. Hospitalizations coded for motor vehicle accident (E800-849.8) were excluded if the admission began in the Emergency Department (ED) to prevent inclusion of non-representative poly-trauma patients.
Table 1.
ICD-9-CM Procedure Codes for Included Otolaryngology Procedure
| Type of Procedure | ICD-9 CM Procedure Code | # (%) |
|---|---|---|
| General | 26.0, 26.12, 26.19, 26.21, 26.30, 26.31, 26.32, 26.42, 27.0, 28.0, 28.11, 28.3, 28.6, 28.7, 28.92, 29.11, 29.12, 29.31, 29.32, 29.52, 29.53, 29.54, 29.91, 31.43, 31.45 | 9573 (16.4) |
| Otology | 18.31, 18.39, 18.6, 19.0, 19.11, 19.19, 19.21, 19.29, 19.3, 19.4, 19.52–19.55, 19.6, 19.9, 20.21–20.23, 20.41, 20.42, 20.49, 20.51, 20.59, 20.61, 20.62, 20.71, 20.79, 20.91–20.93, 20.95–20.99 | 1073 (1.8) |
| Rhinology | 21.04–21.07, 21.1, 21.22, 21.31, 21.32, 21.4, 21.5, 21.61, 21.62, 21.69, 22.11, 22.2, 22.31, 22.39, 22.41, 22.42, 22.50, 22.51, 22.52, 22.53, 22.60–22.64, 22.71, 22.79 | 3729 (6.4) |
| Head and Neck Cancer | 21.83, 25.1–25.4, 25.59, 27.55–27.57, 27.31, 27.32, 27.42, 27.43, 27.49, 27.72, 28.2, 28.5, 29.33, 29.39, 30.09, 30.1, 30.21, 30.22, 30.29, 30.3, 30.4, 40.21, 40.40, 40.41, 40.42, 76.31, 76.39, 76.41–76.43, 86.70–86.75 | 11493 (19.7) |
| Laryngology | 30.01, 31.0, 31.61–31.64, 31.69, 31.72, 31.91–31.95 | 555 (1.0) |
| Facial Plastic Surgery/Trauma | 4.71, 4.72, 4.73, 18.71, 18.72, 18.79, 21.83–21.88, 86.81, 86.82, 21.71, 21.72, 76.71–76.79 | 8372 (14.4) |
| Endocrine | 6.02, 6.09, 6.2, 6.31, 6.39, 6.4, 6.50, 6.51, 6.52, 6.6, 6.7, 6.81, 6.89 | 23436 (40.2) |
Abbreviations: ICD-9-CM = International Classification of Disease, 9th edition, Clinical Modification
There were 58,748 hospital discharges that met inclusion criteria. Hospitalizations with LOS greater than 90 days were excluded because of their presumed clinical complexity (n=155 discharges). Discharges from hospitals with less than ten otolaryngology admissions were excluded due to the small sample size (n=362 discharges). The final cohort was comprised of 56,014 unique patients who accounted for 58,231 discharges from 277 different hospitals. Of these patients, 2,007 (3.5%) had an additional otolaryngology surgery more than 30 days after the index discharge date and were categorized as having a new index surgery hospitalization.
We created a surgical admission specific identifier (ID) that was combined with variables from SID for the patient’s unique identifier (VisitLink) and a time to event (DaysToEvent). These three variables allowed us to identify hospital readmissions within 30 days of discharge from the index surgery and new surgical admissions more than 30 days after discharge from the index surgery. For each discharge, the number and timing of all readmissions within 30 days of discharge from the index surgery was determined. Only the first readmission within 30 days of discharge was analyzed.
Study Variables
Patient-level variables included demographics, median household income for patient zip code (a proxy for socioeconomic status), primary payer, comorbidities, admission source, LOS, discharge destination, and in-hospital complications. Comorbidity data was gathered using the AHRQ comorbidity software (version 3.7) and the Elixhauser Comorbidity measures for administrative data17. Postoperative complications were defined by ICD-9-CM diagnosis codes assigned at discharge (Supplemental Table 1). Fever, pain, and nutritional/electrolyte/digestive deficiencies were analyzed only as postoperative complication variables to explain the reason for readmission.
Hospital-level variables were chosen based on prior research1,4,5 and included hospital size, teaching status, ownership, and hospital disproportionate share (DSH) index. Hospital ownership was classified as public, nonprofit, for profit/investor, or University of California. Hospital size was categorized as small (<150 beds), medium, (150–400 beds), or large (>400 beds)18. Hospitals that qualified as DSH were identified based on the Medicare disproportionate share index as previously described.19
The reason for readmission was determined by searching the primary diagnosis code for the surgical and medical complications of interest (supplemental table 1). The primary diagnosis code is the reason for the hospital admission assigned at the time of discharge.
Outcome Measures
The primary outcome measure was 30-day readmission rate. Secondary outcome measures included reasons for readmission, differences in readmission rates between hospitals, and patient-level and hospital-level risk factors for readmission.
Statistical Analysis
Bivariate analyses were performed for hospital readmission. Univariable logistic regression analysis was performed on three sets of independent variables: type of otolaryngology procedure, patient factors (e.g. sociodemographics, comorbidities, hospital course), and hospital characteristics to find variables associated with readmission. To assess the relative contribution of each of the variables to the overall risk of readmission, variables associated with readmission on univariable analysis (p <0.01) with perceived clinical relevance were entered into a hierarchical logistic regression model. This model accounted for nesting of surgical admissions (level 1) within patient (level 2), and nesting of patients within hospitals (level 3). Failure to account for clustering will result in overly conservative standard errors for the higher-level variables (e.g., hospital variables), and increase the likelihood of type 1 errors. The hierarchical model was constructed using the GLIMMIX procedure in SAS Enterprise Guide 5.1 (SAS Institute, Cary, NC). Statistical tests were 2-sided. Statistical significance was indicated by p-values < 0.01. Odds ratios are presented with 99% confidence intervals given the large population size. Statistical analyses were performed in SAS Enterprise Guide 5.1
Results
Readmission Details
Of the 58,231 discharges for otolaryngologic surgery in California between 2008–2010, 4,709 (8.1%) resulted in a hospital readmission within 30 days of discharge. For individual otolaryngology subspecialties, the readmission rates ranged from 5.1% for facial plastics/trauma to 19% for laryngology (Table 2).
Table 2.
Otolaryngology Procedure
| Otolaryngology Procedure | Total Patients (n=58231) | Patients Without Readmission (n=53522) | Patients with Readmission (n=4709) | Readmission Rate | |||
|---|---|---|---|---|---|---|---|
|
| |||||||
| # | (%) | # | (%) | # | (%) | % | |
| General | 9573 | 16.4 | 8483 | 15.8 | 1090 | 23.1 | 12.8 |
| Otology | 1073 | 1.8 | 990 | 1.8 | 83 | 1.8 | 8.4 |
| Rhinology | 3729 | 6.4 | 3268 | 6.1 | 461 | 9.8 | 14.1 |
| Head and Neck Cancer | 11493 | 19.7 | 10334 | 19.3 | 1159 | 24.6 | 11.2 |
| Laryngology | 555 | 1.0 | 464 | 0.9 | 91 | 1.9 | 19.6 |
| Facial Plastics/Trauma | 8372 | 14.4 | 7961 | 14.8 | 411 | 8.7 | 5.2 |
| Endocrine | 23436 | 40.2 | 22022 | 41.1 | 1414 | 30.0 | 6.4 |
The reasons for readmission based on the principal diagnosis code are shown in Figure 1. Of the readmissions, 472 (10.1%) were due to surgical complications: postoperative bleeding (3.7% of readmissions), surgical site infections (4.9%), and wound dehiscence or fistula (1.5%). For patients undergoing a general pharyngeal procedure such as tonsillectomy, the most common reason for readmission was bleeding (34% of readmissions following a general pharyngeal surgery). Complications related to nutritional, metabolic, or electrolyte disturbances were common, accounting for 44% of total readmissions. For the nutritional, metabolic, electrolyte group, 211 patients (15% of readmission following endocrine surgery) were readmitted for calcium disorders. The most common reason for readmission following endocrine surgery, however, was thyroid cancer (35% of readmissions following endocrine surgery). These represent “planned” readmission for completion thyroidectomy. Of the medical complications, pulmonary complications and infections other than surgical site infections were the most common (6% of readmissions each). Most (95%) of the complications causing readmission were new diagnoses not present during the index hospitalization. The reason for readmission was not classified by the complication codes we used for the remaining 29% of patients.
Figure 1.
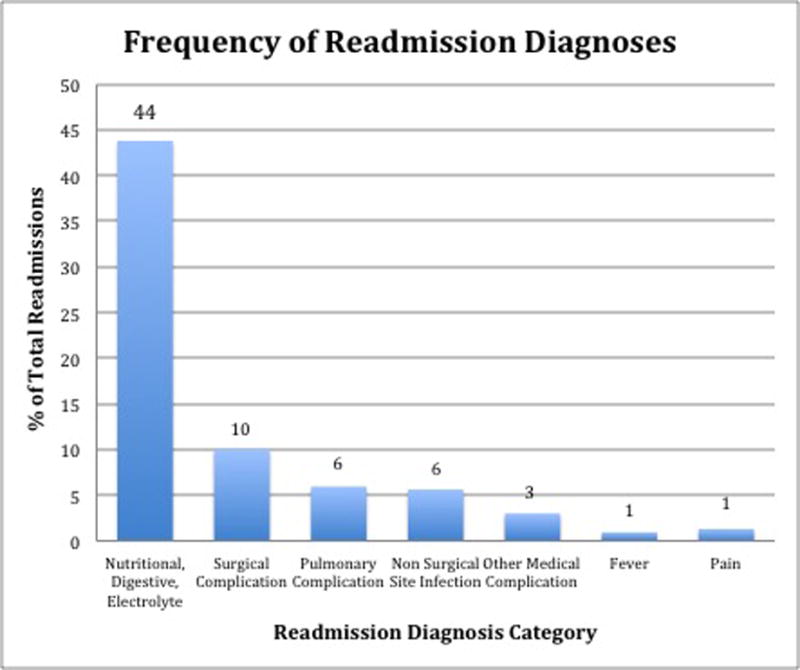
Most common readmission diagnosis categories as percent of total readmissions (n=3315). The total % of readmission diagnoses (71%) does not add up to 100% because some readmissions were not associated with one of the complication codes used in this study as the primary readmission diagnosis.
The median time to readmission was 11 days (interquartile range [IQR], 5–19 days). Seventy-five percent of patients were readmitted to the same hospital as the index discharge. The most common route of readmission was via the ED (57% of readmissions). The median LOS for the readmission hospitalization was three days (IQR, 2–7 days).
Patient-level Risk Factors for Readmission
Patient-level data for demographics, comorbidity, inpatient hospital course and complications are presented in Tables 3, 4, and 5. On univariable analysis, increased age, male gender, and race/ethnicity of black or Hispanic were associated with increased risk of readmission. Insurance status of Medicare (OR 1.99, 99% CI 1.81–2.17) and Medicaid (OR 2.10, 99% CI 1.85–2.36) were associated with an increased risk of readmission relative to private insurance. The comorbidities most strongly associated with readmission were anemia, congestive heart failure, chronic renal failure, chronic lung disease, and diabetes mellitus. A variety of inpatient medical and surgical complications during the index hospitalization increased the risk of readmission. Increasing number of index hospitalization complications was associated with greater risk of readmission. The median length of stay during the index hospitalization varied between patients with and without index hospitalization complications: one day (IQR 1–3) in patients with no index hospitalization complications versus five days (IQR 2–13) in patients with a complication. Discharge destination to home with home care (OR 3.73, 99% CI 3.42–4.07) or nursing facility (OR 4.37, 99% CI 3.96–4.82) was associated with a higher likelihood of readmission on univariable analysis.
Table 3.
Patient Demographics
| Variable | Total Patients (n=58231) | Patients Without Readmission (n=53522) | Patients with Readmission (n=4709) | Odds Ratio | 99% CI | |||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| # | (%) | # | (%) | # | (%) | |||
| Age categories | ||||||||
| <45 | 18018 | 30.9 | 16883 | 31.5 | 1135 | 24.1 | 1 (Ref) | |
| 45–54 | 12078 | 20.7 | 11183 | 20.9 | 895 | 19.0 | 1.19 | 1.06–1.34 |
| 55–64 | 12116 | 20.8 | 11130 | 20.8 | 986 | 20.9 | 1.32 | 1.17–1.48 |
| 65–74 | 8936 | 15.3 | 8139 | 15.2 | 797 | 16.9 | 1.46 | 1.29–1.65 |
| >=75 | 7083 | 12.2 | 6187 | 11.6 | 896 | 19.0 | 2.15 | 1.91–2.43 |
|
| ||||||||
| Sex | ||||||||
| Female | 32143 | 55.2 | 29812 | 55.7 | 2331 | 49.5 | 1 (Ref) | |
| Male | 26088 | 44.8 | 23710 | 44.3 | 2378 | 50.5 | 1.28 | 1.19–1.39 |
|
| ||||||||
| Race | ||||||||
| White | 33536 | 57.6 | 30833 | 57.6 | 2703 | 57.4 | 1 (Ref) | |
| Black | 4449 | 7.6 | 4001 | 7.5 | 448 | 9.5 | 1.78 | 1.11–1.47 |
| Hispanic | 10840 | 18.6 | 9866 | 18.4 | 974 | 20.7 | 1.13 | 1.02–1.25 |
| Asian | 4204 | 7.2 | 3844 | 7.2 | 360 | 7.6 | 1.07 | 0.92–1.24 |
| Other | 1064 | 1.8 | 979 | 1.8 | 85 | 1.8 | 0.99 | 0.74–1.33 |
| Missing race | 4138 | 7.1 | 3999 | 7.5 | 139 | 3.0 | 0.40 | 0.32–0.50 |
|
| ||||||||
| Median household income of ZIP (quartiles) | ||||||||
| 4 (lowest) | 12801 | 22.0 | 11642 | 21.8 | 1159 | 24.6 | 1 (Ref) | |
| 3 | 14081 | 24.2 | 12932 | 24.2 | 1149 | 24.4 | 0.89 | 0.80–1.00 |
| 2 | 14741 | 25.3 | 13559 | 25.3 | 1182 | 25.1 | 0.88 | 0.78–0.98 |
| 1 (highest) | 15603 | 26.8 | 14464 | 27.0 | 1139 | 24.2 | 0.79 | 0.71–0.89 |
| Missing | 1005 | 1.7 | 925 | 1.7 | 80 | 1.7 | 0.87 | 0.64–1.19 |
|
| ||||||||
| Insurance | ||||||||
| Private | 28499 | 48.9 | 26763 | 50.0 | 1736 | 36.9 | 1 (Ref) | NA |
| Medicaid | 5868 | 10.1 | 5167 | 9.7 | 701 | 14.9 | 1.98 | 1.81–2.17 |
| Medicare | 16866 | 29.0 | 14945 | 27.9 | 1921 | 40.8 | 2.09 | 1.85–2.36 |
| Self-pay | 2781 | 4.8 | 2657 | 5.0 | 124 | 2.6 | 0.72 | 0.56–0.92 |
| Other | 4217 | 7.2 | 3990 | 7.5 | 227 | 4.8 | 0.88 | 0.73–1.06 |
Abbreviations: CI = confidence interval; Ref = reference
Table 4.
Comorbidities
| Variable | Total Patients (n=58231) | Patients Without Readmission (n=53522) | Patients with Readmission (n=4709) | Odds Ratio | 99% CI | |||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| # | (%) | # | (%) | # | (%) | |||
| Alcohol Abuse | ||||||||
| Yes | 2193 | 3.8 | 1948 | 3.6 | 245 | 5.2 | 1.45 | 1.22–1.74 |
|
| ||||||||
| Anemia | ||||||||
| Yes | 4527 | 7.8 | 3615 | 6.8 | 912 | 19.4 | 3.32 | 2.99–3.70 |
|
| ||||||||
| CHF | ||||||||
| Yes | 1592 | 2.7 | 1267 | 2.4 | 325 | 6.9 | 3.06 | 2.59–3.61 |
|
| ||||||||
| Chronic Lung Disease | ||||||||
| Yes | 7487 | 12.9 | 6595 | 12.3 | 892 | 18.9 | 1.66 | 1.50–1.84 |
|
| ||||||||
| Depression | ||||||||
| Yes | 3320 | 5.7 | 2953 | 5.5 | 367 | 7.8 | 1.45 | 1.25–1.68 |
|
| ||||||||
| Diabetes Mellitus | ||||||||
| Yes | 8254 | 14.2 | 7262 | 13.6 | 992 | 21.1 | 1.70 | 1.54–1.87 |
|
| ||||||||
| Hypertension | ||||||||
| Yes | 21924 | 37.7 | 19711 | 36.8 | 2213 | 47.0 | 1.52 | 1.41–1.65 |
|
| ||||||||
| Metastatic cancer | ||||||||
| Yes | 5883 | 10.1 | 5170 | 9.7 | 713 | 15.1 | 1.70 | 1.49–1.87 |
|
| ||||||||
| Obesity | ||||||||
| Yes | 5892 | 10.1 | 5438 | 10.2 | 454 | 9.6 | 0.94 | 0.83–1.08 |
|
| ||||||||
| Renal failure | ||||||||
| Yes | 2807 | 4.8 | 2266 | 4.2 | 541 | 11.5 | 2.94 | 2.66–3.24 |
Abbreviations: CHF = Congestive Heart Failure
Table 5.
Complications during the Index Surgical Admission
| Variable | Total Patients (n=58231) | Patients Without Readmission (n=53522) | Patients with Readmission (n=4709) | Odds Ratio | 99% CI | |||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| # | (%) | # | (%) | # | (%) | |||
| Admission Route | ||||||||
| Routine | 43944 | 75.5 | 40899 | 76.4 | 3045 | 64.7 | 1 (Ref) | |
| Other hospital | 3075 | 5.3 | 2767 | 5.2 | 308 | 6.5 | 1.85 | 1.69–2.02 |
| Emergency Room | 11212 | 19.3 | 9856 | 18.4 | 1356 | 28.8 | 1.5 | 1.27–1.76 |
|
| ||||||||
| Hemorrhage/Seroma | ||||||||
| Yes | 1727 | 3.0 | 1529 | 2.9 | 198 | 4.2 | 1.49 | 1.22–1.82 |
|
| ||||||||
| Wound Dehiscence/Fistula | ||||||||
| Yes | 424 | 0.7 | 343 | 0.6 | 81 | 1.7 | 2.72 | 1.97–3.74 |
|
| ||||||||
| SSI | ||||||||
| Yes | 1968 | 3.4 | 1771 | 3.3 | 197 | 4.2 | 1.28 | 1.05–1.56 |
|
| ||||||||
| CNS Complication | ||||||||
| Yes | 307 | 0.5 | 257 | 0.5 | 50 | 1.1 | 2.23 | 1.49–3.32 |
|
| ||||||||
| Cardiac Complication | ||||||||
| Yes | 4013 | 6.9 | 3383 | 6.3 | 630 | 13.4 | 2.29 | 2.03–2.58 |
|
| ||||||||
| Pulm Complication | ||||||||
| Yes | 3450 | 5.9 | 2751 | 5.1 | 699 | 14.8 | 3.22 | 2.86–3.62 |
|
| ||||||||
| VTE | ||||||||
| Yes | 367 | 0.6 | 260 | 0.5 | 107 | 2.3 | 4.74 | 3.53–6.42 |
|
| ||||||||
| AKI | ||||||||
| Yes | 975 | 1.7 | 718 | 1.3 | 257 | 5.5 | 4.25 | 3.51–5.14 |
|
| ||||||||
| UTI | ||||||||
| Yes | 1023 | 1.8 | 784 | 1.5 | 239 | 5.1 | 3.60 | 2.96–4.37 |
|
| ||||||||
| Sepsis/Septicemia | ||||||||
| Yes | 867 | 1.5 | 645 | 1.2 | 222 | 4.7 | 4.06 | 3.30–4.98 |
|
| ||||||||
| # of Index Complications | ||||||||
| 0 | 47447 | 81.5 | 44378 | 82.9 | 3069 | 65.2 | 1 (Ref) | NA |
| 1 | 7925 | 13.6 | 6912 | 12.9 | 1013 | 21.5 | 2.12 | 1.92–2.34 |
| >=2 | 2859 | 4.9 | 2232 | 4.2 | 627 | 13.3 | 4.06 | 3.58–4.61 |
|
| ||||||||
| Type of Complication | ||||||||
| None | 47447 | 81.5 | 44378 | 82.9 | 3069 | 65.2 | 1 (Ref) | NA |
| Surgical only | 2807 | 4.8 | 2571 | 4.8 | 236 | 5.0 | 1.33 | 1.11–1.59 |
| Medical only | 6860 | 11.8 | 5656 | 10.6 | 1204 | 25.6 | 3.08 | 2.8–3.38 |
| Medical and surgical complication | 1117 | 1.9 | 917 | 1.7 | 200 | 4.2 | 3.15 | 2.57–3.88 |
|
| ||||||||
| Index LOS | ||||||||
| <=3days | 43463 | 74.6 | 41181 | 76.9 | 2282 | 48.5 | 1 (Ref) | NA |
| 4–7 days | 7805 | 13.4 | 6932 | 13.0 | 873 | 18.5 | 2.27 | 2.04–2.53 |
| 8–14 | 3849 | 6.6 | 3089 | 5.8 | 760 | 16.1 | 4.44 | 3.95–5.00 |
| 15–30 | 2068 | 3.6 | 1565 | 2.9 | 503 | 10.7 | 5.80 | 5.03–6.69 |
| >=31 | 1046 | 1.8 | 755 | 1.4 | 291 | 6.2 | 6.96 | 5.77–8.38 |
|
| ||||||||
| Discharge Destination | ||||||||
| Home | 52017 | 89.3 | 48651 | 90.9 | 3366 | 71.5 | 1 (Ref) | NA |
| Home with care | 3680 | 6.3 | 2925 | 5.5 | 755 | 16.0 | 3.73 | 3.42–4.07 |
| Nursing facility | 2534 | 4.4 | 1946 | 3.6 | 588 | 12.5 | 4.37 | 3.96–4.82 |
Abbreviations: SSI = surgical site infection; CNS = central nervous system; pulm = pulmonary; VTE = venous thromboembolism; AKI = acute kidney injury; UTI = urinary tract infection; LOS = length of stay
Hospital-level Risk Factors for Readmission
Hospital characteristics and readmission rates are presented in Table 6. Surgery at a teaching hospital was associated with a small increased risk of readmission (OR 1.25, 99% CI 1.17–1.33), as was surgery at a disproportionate share hospital (OR 1.23, 99% CI 1.16–1.31). Surgery in a hospital with ownership other than “not-for-profit” had a slightly increased risk of readmission. Hospital bed-size was not associated with risk of readmission.
Table 6.
Hospital Characteristics and 30-day Readmission Rates
| Hospital Variable | # of Hospitals | % of Hospitals | # of Otolaryngology Surgical Cases/Hospital | Hospital Readmission Rate (%) | ||
|---|---|---|---|---|---|---|
|
| ||||||
| Median | IQR | Median | IQR | |||
| Hospital Type | ||||||
| Public | 36 | 13 | 120 | 34–260 | 8 | 5–10 |
| Investor | 63 | 23 | 41 | 17–85 | 9 | 5–17 |
| Non-profit | 172 | 62 | 151 | 59–320 | 7 | 5–10 |
| University | 6 | 2 | 1161 | 658–1514 | 10 | 9–11 |
|
| ||||||
| # of Beds | ||||||
| <=150 | 84 | 30 | 32 | 15–65 | 8 | 5–15 |
| 151–399 | 148 | 53 | 155 | 63–282 | 7 | 5–10 |
| >=400 | 45 | 16 | 434 | 204–675 | 8 | 7–10 |
|
| ||||||
| Teaching Hospital | ||||||
| No | 254 | 92 | 97 | 34–230 | 7 | 5–11 |
| Yes | 23 | 8 | 591 | 156–1304 | 9 | 8–10 |
|
| ||||||
| Disproportionate Share Hospital | ||||||
| No | 196 | 71 | 127 | 51–284 | 7 | 5–10 |
| Yes | 81 | 29 | 58 | 26–226 | 9 | 7–11 |
Abbreviations: IQR = interquartile range
Hierarchical Logistic Regression Model of Readmission
A hierarchical logistical regression model was used to determine variables independently associated with an increased risk of 30-day readmission (Table 7). These included: otolaryngologic procedure type, insurance status, chronic anemia, chronic lung disease, chronic renal failure, index admission via the ED, in-hospital complication during the index admission, and discharge destination. None of the structural hospital characteristics were associated with 30-day readmission. Three comorbidity variables (anemia, chronic lung disease, and chronic renal failure) were associated with an increased likelihood of readmission. Medical complications were associated with a higher rate of readmission than surgical complications. The presence of both a surgical and medical complication was not associated with a greater risk of readmission than only a medical complication. Patients discharged to a nursing facility or home with home health had a two-fold increased risk of readmission compared to patients discharged to home.
Table 7.
Variables Associated with 30-day Readmission in Multivariable Analysis
| Patient Variable | p value | Odds Ratio | 99% CI |
|---|---|---|---|
| Procedure Type | |||
| General | Reference | – | – |
| Otology | 0.0161 | 0.74 | 0.54–1.02 |
| Rhinology | 0.0072 | 1.18 | 1.01–1.39 |
| Head and Neck Cancer | 0.2709 | 0.95 | 0.83–1.08 |
| Laryngology | 0.4308 | 1.11 | 0.80–1.53 |
| Facial Plastics/Trauma | <0.0001 | 0.54 | 0.46–0.64 |
| Endocrine | <0.0001 | 0.77 | 0.68–0.87 |
|
| |||
| Insurance | |||
| Private | Reference | – | – |
| Medicaid | 0.0005 | 1.27 | 1.12–1.43 |
| Medicare | <0.0001 | 1.54 | 1.34–1.77 |
| Self-pay | <0.0001 | 0.75 | 0.57–0.97 |
| Other | <0.0001 | 0.83 | 0.68–1.02 |
|
| |||
| Anemia | |||
| Yes | <0.0001 | 1.61 | 1.43–1.82 |
|
| |||
| Chronic Lung Disease | |||
| Yes | <0.0001 | 1.19 | 1.06–1.33 |
|
| |||
| Renal Failure | |||
| Yes | <0.0001 | 1.70 | 1.46–1.97 |
|
| |||
| Index admission via ED | |||
| Yes | <0.0001 | 1.32 | 1.18–1.49 |
|
| |||
| Index-Hospitalization Complication | |||
| Surgical Only | 0.2084 | 0.91 | 0.75–1.10 |
| Medical Only | <0.0001 | 1.52 | 1.36–1.71 |
| Surgical and Medical | 0.006 | 1.27 | 1.02–1.59 |
|
| |||
| Discharge Destination | |||
| Home | Reference | – | – |
| Home with Home Health | <0.00001 | 2.23 | 1.96–2.55 |
| Nursing Facility | <0.00001 | 2.21 | 1.89–2.57 |
Discussion
Readmission Details
This study is the first to examine the incidence, reasons, and factors associated with 30-day readmission in a heterogeneous cohort of patients from variety of different hospitals undergoing otolaryngologic surgery. It expands upon single-institution retrospective studies examining 30-day otolaryngology readmissions. The 30-day readmission rate in this study was 8.1%, similar to other studies for otolaryngology8,9,11,12.
Of these readmissions, 25% occurred outside the index institution, concordant with numbers in the general surgery literature13,14. Readmission to a hospital other than where the surgery occurred has patient care implications, since it is associated with worse survival13,20. The effect of care fragmentation (i.e. admission to the non-index hospital) in otolaryngology is unknown, however, and future investigation into the topic is warranted. It also has implications for future study design, as a significant number of patients are likely missed in single institution studies.
Nutritional, digestive, and electrolyte abnormalities were the most common reason for readmission in this study. This finding could be explained by the fact that endocrine surgery represented nearly 40% of the surgeries. However, dysphagia and malnutrition-related readmissions due to surgery of the upper aerodigestive tract represented a sizable portion of readmissions as well.
Other analyses of otolaryngology readmissions have found that postoperative complications are the most common reasons for readmision8,10–12. In this study, surgical complications of bleeding, surgical site infection, and wound dehiscence only accounted for approximately 10% of all readmissions. That 34% of readmissions following procedures such as tonsillectomy were related to bleeding is concordant with previous studies21. The difference in the percentage of readmissions due to postoperative complications between this study and others may reflect the higher proportion of head and neck cancer patients in previous studies.
As in other studies1,7,10, new complications after discharge, not in-hospital complications, were the major drivers of readmission. An in-hospital surgical complication was not associated with increased risk of readmission; however, a medical or medical and surgical complication was. In this study, only 5% of readmissions were due to the recurrence or persistence of a complication from the index hospitalization. The rest of the readmissions were due to the development of new complications after discharge.
Variables Associated with Increased Risk of Readmission
In the multivariable analysis, most of the factors associated with readmission were patient-level factors; none of the hospital-level factors were significant. This is consistent with studies examining readmissions in general7 and cardiac surgery5. Surgical volume was not analyzed as a hospital-level factor in the study. Given its relationship to quality care in other otolaryngology studies,22 it merits investigation in future studies of otolaryngology readmission. The type of procedure was associated with differences in the rates of 30-day readmission, with facial plastics/trauma and endocrine associated with lower risk of readmission compared to general otolaryngologic surgery. Although not statistically significant in the final model, a high rate of readmissions was noted for laryngology procedures. This is likely the result of selection bias, as most laryngology procedures are office based or outpatient, and only the highest risk patients are admitted to the hospital.
Insurance status was predictive of readmission, with an increased risk of readmission for Medicare and Medicaid relative to private insurance. The association between insurance status and increased risk of readmission has been found across a variety of surgical subspecialties3,5,8,23. Patients with Medicare are may have had a higher rate of readmission because they are in general more frail and have less support for managing complications following hospital discharge24. Patients with Medicaid may have a higher rate of readmission due to fewer resources for postoperative care, less medical knowledge for identifying post-discharge problems, more challenge returning for follow-up care, and less availability of primary care for managing medical problems. Data on insurance status is absent from publications about readmissions that use National Surgical Quality Improvement Program (NSQIP)1,2,7,25, and is potentially an important risk factor not captured in these studies.
Comorbidities associated with an increased rate of readmission were chronic anemia, chronic lung disease, and chronic renal failure. Similar comorbidities have been identified as risk factors for readmission in otolaryngology patients8,11, likely because of the intimate relationship of these comorbidities to surgery on the upper aerodigestive tract.
Discharge to home with home health or a nursing facility was also associated with an increased risk of readmission. This has been seen in studies examining readmission following otolaryngologic8,11 and general surgery1,6. Possible explanations include the complexity/unfamiliarity of wound care, unmeasured patient comorbidity/frailty, loss of information surrounding transitions of care, and a lower threshold for readmission when complications are encountered by home health aides or in a nursing facility26. In addition, it may be a surrogate marker for marginal social status, limited social support, or distance from local health services. Interventions focused on improving transitions of care represent an opportunity for decreasing readmission.
The presence and timing of postoperative complications has been evaluated in other studies1,7,8,10. Concordant with these studies, in-hospital complications in this study were only minimally associated with 30-day readmissions. Furthermore, this increased risk was primarily due to in-hospital medical complications, not surgical complications. This might represent an opportunity for quality improvement for better communication and closer follow up with the primary care physician as the patient transitions care out of the acute hospital setting.
Limitations
There are limitations to this administrative data-based study. It is limited by the accuracy of the ICD-9-CM diagnosis codes, especially for minor complications27. Readmission diagnoses in administrative data do not always correlate with the true reason for readmission24,28. There is uncertainty about how these data will apply ICD-10-CM diagnosis codes. It is also unknown whether data about otolaryngology patients from California are generalizable to otolaryngology patients elsewhere. A future study using SID data from multiple states and comparing readmission rates across states (and regions) would be a worthwhile future study. Twenty-nine percent of the reasons for readmissions were not categorized by the complication codes we used in this study. Finally, we were unable to reliably distinguish between “planned” and “unplanned” readmissions.
Despite these limitations, this study has a number of methodological strengths relative to prior studies. Unlike single institution studies, it contains a large and heterogeneous number of patients, analyzes different types of hospitals, compares readmission rates across hospitals, and identified and analyzed the 25% of readmissions that occurred outside the index institution. Unlike studies based on Medicare data, this study included patients with insurance status other than Medicare (which was an independent risk factor for readmission), as well as patients under the age of 65 years, which was the overwhelming majority of otolaryngology patients in this study.
Conclusions
Thirty-day readmission following otolaryngologic surgery is not uncommon, and occurs across a variety of types of procedures and hospitals. Most of the variation was driven by patient-specific factors, not structural hospital characteristics. Variables associated with 30-day readmission in hierarchical logistic regression modeling were: type of otolaryngologic procedure, Medicare or Medicaid health insurance, chronic anemia, chronic lung disease, chronic renal failure, index admission via the emergency department, in-hospital complication during the index admission, and discharge destination other than home.
Supplementary Material
Acknowledgments
Research/Funding Support: This research was funded in part by Washington University Institute of Clinical and Translational Sciences Grant # UL1 TR000448 from the National Center for Advancing Translational Sciences (NCATS), AHRQ Grant #R24 HS19455, NCI Grant # KM1CA156708, the P30 Research Center for Auditory and Vestibular Studies and the National Institutes of Health NIDCD Grant # P30DC04665, and departmental funds (Brian Nussenbaum, MD).
Footnotes
Conflict of interest/financial disclosures: The authors have no relevant conflicts of interest or financial disclosures
This manuscript was presented at the Combined Sections Meeting in Miami, Florida, USA, January 22–24, 1016.
Level of Evidence: 2b
References
- 1.Merkow RP, Ju MH, Chung JW, et al. Underlying reasons associated with hospital readmission following surgery in the United States. JAMA. 2015;313:483–495. doi: 10.1001/jama.2014.18614. [DOI] [PubMed] [Google Scholar]
- 2.Kassin MT, Owen RM, Perez SD, et al. Risk factors for 30-day hospital readmission among general surgery patients. Journal of the American College of Surgeons. 2012;215:322–330. doi: 10.1016/j.jamcollsurg.2012.05.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dailey EA, Cizik A, Kasten J, Chapman JR, Lee MJ. Risk factors for readmission of orthopaedic surgical patients. The Journal of bone and joint surgery. 2013;95:1012–1019. doi: 10.2106/JBJS.K.01569. [DOI] [PubMed] [Google Scholar]
- 4.Tsai TC, Joynt KE, Orav EJ, Gawande AA, Jha AK. Variation in surgical-readmission rates and quality of hospital care. The New England journal of medicine. 2013;369:1134–1142. doi: 10.1056/NEJMsa1303118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Li Z, Armstrong EJ, Parker JP, Danielsen B, Romano PS. Hospital variation in readmission after coronary artery bypass surgery in California. Circulation Cardiovascular quality and outcomes. 2012;5:729–737. doi: 10.1161/CIRCOUTCOMES.112.966945. [DOI] [PubMed] [Google Scholar]
- 6.Sanford DE, Olsen MA, Bommarito KM, et al. Association of discharge home with home health care and 30-day readmission after pancreatectomy. Journal of the American College of Surgeons. 2014;219:875–886. doi: 10.1016/j.jamcollsurg.2014.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Morris MS, Deierhoi RJ, Richman JS, Altom LK, Hawn MT. The relationship between timing of surgical complications and hospital readmission. JAMA Surg. 2014;149:348–354. doi: 10.1001/jamasurg.2013.4064. [DOI] [PubMed] [Google Scholar]
- 8.Graboyes EM, Liou TN, Kallogjeri D, Nussenbaum B, Diaz JA. Risk factors for unplanned hospital readmission in otolaryngology patients. Otolaryngology–head and neck surgery. 2013;149:562–571. doi: 10.1177/0194599813500023. [DOI] [PubMed] [Google Scholar]
- 9.Jalisi S, Bearelly S, Abdillahi A, Truong MT. Outcomes in head and neck oncologic surgery at academic medical centers in the United States. The Laryngoscope. 2013;123:689–698. doi: 10.1002/lary.23835. [DOI] [PubMed] [Google Scholar]
- 10.Graboyes EM, Yang Z, Kallogjeri D, Diaz JA, Nussenbaum B. Patients undergoing total laryngectomy: an at-risk population for 30-day unplanned readmission. JAMA otolaryngology–head & neck surgery. 2014;140:1157–1165. doi: 10.1001/jamaoto.2014.1705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dziegielewski PT, Boyce B, Manning A, et al. Predictors and costs of readmissions at an academic head and neck surgery service. Head & neck. 2015 doi: 10.1002/hed.24030. [DOI] [PubMed] [Google Scholar]
- 12.Rajasekaran K, Revenaugh P, Benninger M, Burkey B, Sindwani R. Development of a Quality Care Plan to Reduce Otolaryngologic Readmissions: Early Lessons from the Cleveland Clinic. Otolaryngology–head and neck surgery. 2015 doi: 10.1177/0194599815570025. [DOI] [PubMed] [Google Scholar]
- 13.Tsai TC, Orav EJ, Jha AK. Care fragmentation in the postdischarge period: surgical readmissions, distance of travel, and postoperative mortality. JAMA Surg. 2015;150:59–64. doi: 10.1001/jamasurg.2014.2071. [DOI] [PubMed] [Google Scholar]
- 14.Tosoian JJ, Hicks CW, Cameron JL, et al. Tracking early readmission after pancreatectomy to index and nonindex institutions: a more accurate assessment of readmission. JAMA Surg. 2015;150:152–158. doi: 10.1001/jamasurg.2014.2346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.HCUP State Inpatient Databases (SID) 2014 Available at: http://www.hcup-us.ahrq.gov/sidoverview.jsp. Accessed March 10 2014.
- 16.Hospital Annual Utilization Data. 2014 Nov; Available at: http://www.oshpd.ca.gov/hid/Products/Hospitals/Utilization/Hospital_Utilization.html. Accessed March 3 2014.
- 17.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Medical care. 1998;36:8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 18.OSHPD. Available at: http://www.oshpd.ca.gov/HID/Products/Listings.html. Accessed March 12 2014.
- 19.Chatterjee P, Joynt KE, Orav EJ, Jha AK. Patient experience in safety-net hospitals: implications for improving care and value-based purchasing. Archives of internal medicine. 2012;172:1204–1210. doi: 10.1001/archinternmed.2012.3158. [DOI] [PubMed] [Google Scholar]
- 20.Brooke BS, Goodney PP, Kraiss LW, Gottlieb DJ, Samore MH, Finlayson SR. Readmission destination and risk of mortality after major surgery: an observational cohort study. Lancet. 2015;(15):S0140–6736. 60087–3. doi: 10.1016/S0140-6736(15)60087-3. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bhattacharyya N, Kepnes LJ. Revisits and postoperative hemorrhage after adult tonsillectomy. The Laryngoscope. 2014;124:1554–1556. doi: 10.1002/lary.24541. [DOI] [PubMed] [Google Scholar]
- 22.Eskander A, Merdad M, Irish JC, et al. Volume-outcome associations in head and neck cancer treatment: a systematic review and meta-analysis. Head & Neck. 2014;36:1820–1834. doi: 10.1002/hed.23498. [DOI] [PubMed] [Google Scholar]
- 23.Keeney JA, Nam D, Johnson SR, Nunley RM, Clohisy JC, Barrack RL. The Impact of Risk Reduction Initiatives on Readmission: THA and TKA Readmission Rates. J Arthroplasty. 2015;30:2057–2060. doi: 10.1016/j.arth.2015.06.007. [DOI] [PubMed] [Google Scholar]
- 24.Chiang LY, Liu J, Flood KL, et al. Geriatric assessment as predictors of hospital readmission in older adults with cancer. J Geriatr Oncol. 2015 doi: 10.1016/j.jgo.2015.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dawes AJ, Sacks GD, Russell MM, et al. Preventable readmissions to surgical services: lessons learned and targets for improvement. Journal of the American College of Surgeons. 2014;219:382–389. doi: 10.1016/j.jamcollsurg.2014.03.046. [DOI] [PubMed] [Google Scholar]
- 26.Mor V, Intrator O, Feng Z, Grabowski DC. The revolving door of rehospitalization from skilled nursing facilities. Health Aff (Millwood) 2010;29:57–64. doi: 10.1377/hlthaff.2009.0629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Awad MI, Shuman AG, Montero PH, Palmer FL, Shah JP, Patel SG. Accuracy of administrative and clinical registry data in reporting postoperative complications after surgery for oral cavity squamous cell carcinoma. Head & neck. 2014 doi: 10.1002/hed.23682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sacks GD, Dawes AJ, Russell MM, et al. Evaluation of hospital readmissions in surgical patients: do administrative data tell the real story? JAMA Surg. 2014;149:759–764. doi: 10.1001/jamasurg.2014.18. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


