Abstract
We hereby report a novel technical approach for the treatment of acute stroke with underlying tandem occlusion. The so-called retriever wire supported carotid artery revascularization (ReWiSed CARe) technique, utilizing the wire of a stent-retriever as a guiding wire for carotid artery stenting, is technically feasible in tandem occlusions caused by an internal carotid artery (ICA) dissection or high grade ICA stenosis. This technique eliminates the need to use a long microwire in order to maintain the position inside the true lumen of a dissection. Additionally, it leads to anterograde perfusion through the released stent-retriever during the time of ICA stenting, which is favorable in all tandem occlusion cases.
Keywords: Carotid artery dissection, carotid artery stenting, stroke
Introduction
Recently, multiple randomized trials have demonstrated the superiority of endovascular therapy (EVT) in acute ischemic stroke (AIS) with underlying large artery occlusion (LAO). A subset of patients thereby presents with a so-called tandem occlusion, i.e. a simultaneous occlusion of the cervical internal carotid artery (ICA) in combination with an intracranial LAO. These patients do also benefit from EVT,1,2 but current guidelines do not provide a distinct treatment strategy.3 The majority of tandem occlusion cases are caused by atherosclerotic lesions of the ICA, whereas data about tandem occlusions based on a dissection of the ICA remains sparse.4,5 Recently, Kurre et al. published a retrospective study covering 73 patients,6 including 44 patients with tandem occlusions caused by a dissection of the ICA who were treated by endovascular means, yielding a 55% favorable outcome (mRS ≤ 2 at day 90). Regarding the technical approach, tandem occlusions are usually treated in an antegrade manner with stenting of the ICA prior to intracranial thrombectomy or in a retrograde manner in which stenting is performed after intracranial thrombectomy.2,6 We hereby report the first case of a simultaneous approach in which stenting of the ICA dissection was done utilizing the 0.014 inch wire of a pREset LITE (Phenox, Bochum, Germany) stent-retriever in order to maintain the true lumen of the ICA.
Case report
A 52-year-old male patient was referred to our hospital with a tandem occlusion of the left ICA and carotid-T (Figure 1(a)). At admission to the regional stroke center he presented with a hemiparesis, aphasia, and loss of consciousness (NIHSS 24). After intracranial hemorrhage (ICH) was ruled out (ASPECTS 7) the patient received intravenous (iv) tissue plasminogen activator (tPA) and was shipped to our interventional stroke center where he was admitted 5h 30 minutes after the onset of symptoms. The patient was referred to our angio suite directly and the treatment began within 6 h (groin puncture at 5h 50 minutes after of symptom onset).
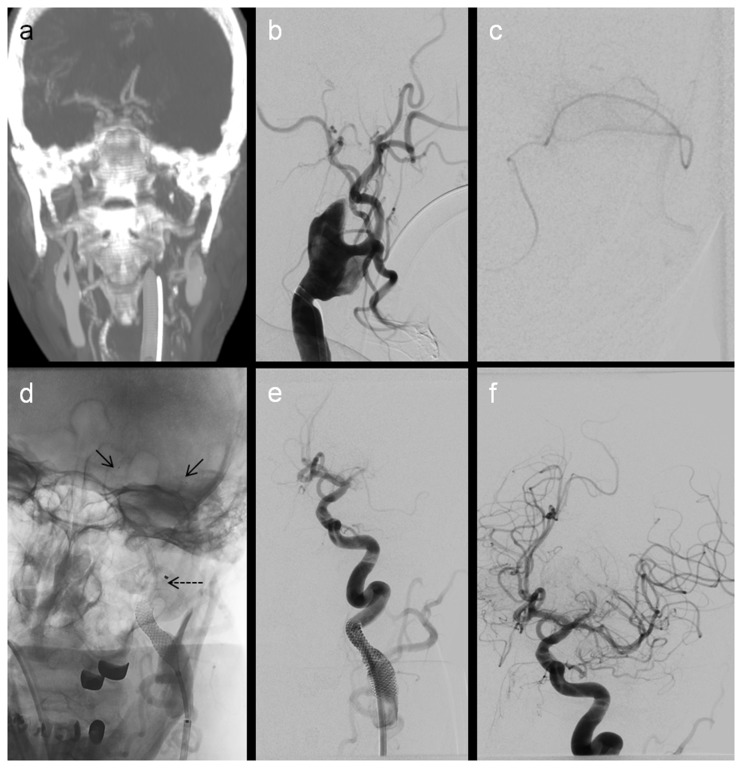
Figure 1.
Computed tomographic imaging to TICI2b: (a) coronal reformatted images showing a carotid-T and an ipsilateral ICA occlusion; (b) injection into the left common carotid depicts a proximal occlusion of the ICA; (c) after passage of the dissection a microcatheter injection verified the true lumen (distal M2); (d) after deployment of the stent-retriever (arrows) the carotid stent was placed over the stent-retriever wire (dotted arrows); (e) control injection after one passage with the stent-retriever showing a persistent occlusion of the M1 segment and a good reconstruction of the ICA; (f) final angiogram showing a TICI2b result.
Treatment
Treatment was performed under general anesthesia. A short 8F guide sheath was placed in the right femoral artery. Afterwards, an 8F guide catheter (Mach-1, Boston Scientific, Marlborough, MA, USA) was placed in the left common carotid artery (CCA). Injection in the left CCA revealed a dissection of the proximal ICA (Figure 1(b)) without distal filling of the ICA or the left anterior circulation. Dissection was passed with a 0.014 inch wire (Transend guide wire, Stryker, Kalamazoo, MN, USA) and a 0.021 inch microcatheter (Trevor pro 18 microcatheter, Concentric Medical/Stryker, Kalamazoo, MN, USA). The microcatheter was subsequently placed distal to the thrombus into a distal branch of the left middle cerebral artery (MCA). After removal of the microwire distal injection was performed to verify the correct position of the microcatheter (Figure 1(c)), a pREset LITE (Phenox, Bochum, Germany) stent retriever (4 mm × 20 mm) was released in the distal MCA M1 segment by withdrawal of the microcatheter. Stenting of the dissection was subsequently performed utilizing the 0.014 wire of the stent-retriever (total length: 183 cm including the stent itself) with a Wallstent (Boston Scientific, Marlborough, MA, USA) (Figure 1(d)). Prior to stent placement, 5000 IU of heparin and 500 mg of acetylsalicylic acid (ASA) were administered iv. Control injection into the left CCA showed a good reconstruction result of the ICA dissection and the 8F guide was advanced distal to the stent (Figure 1(e)). A 6F SofiaPlus aspiration catheter (Microvention, Tustin, CA, USA) was advanced to the level of the carotid terminus over the microwire of the pREset LITE and thrombectomy was performed twice using the stent-retriever assisted vacuum-locked extraction (SAVE) technique,7 resulting in a TICI2b result after a total duration of 90 min from groin to reperfusion (Figure 1(f)). Notably the stent-retriever has to be fully withdrawn into the aspiration catheter when passing the carotid stent or the stent has to be passed by the guide catheter/femoral long sheath prior to intracranial thrombectomy in order to avoid complications when the stent-retriever is retracted.
Clinical outcome
Despite a successful recanalization the patient suffered from a large MCA infarction leading to no clinical benefit after EVT; 72 h after EVT he suffered from a symptomatic hemorrhage and died five days after admission, although the acute ICA stenting was carried out without a dual antiplatelet therapy.
Discussion
EVT has emerged as standard of care for patients with AIS caused by LAO.1,3,8 Nevertheless, until today there is no distinct guideline recommendation for patients with AIS and underlying tandem occlusion.3 If EVT is carried out, high rates of favorable outcome have been reported.2,4,9 However, the majority of cases with an occlusion of the cervical ICA in combination with a proximal intracranial occlusion are caused by an atherosclerotic lesion of the ICA, whereas a tandem occlusion caused by a dissection of the ICA is a relatively rare event. In a series published by Kurre et al.,6 only 4.6% out of 1603 patients suffered from a stroke caused by a dissection of the ICA and of these only 60% presented with a tandem occlusion caused by the dissection. In an analysis of the Prognostic Factors Related to Clinical Outcome Following Thrombectomy in Ischemic Stroke (RECOST) Study that has been published recently, 22% of the patients (57/258) presented with a tandem occlusion of which 20/57 (35%) were caused by a dissection of the ICA.10 In the RECOST study, only 5/20 (25%) patients received acute stenting of the ICA, whereas Kurre et al. reported that all 44 patients with a tandem occlusion received stent assisted reconstruction of the ICA.6 The patients within the RECOST study were thereby treated with a retrograde approach allowing checking for Circle of Willis insufficiency after intracranial thrombectomy. In this series, only patients with a Circle of Willis insufficiency received a stenting of the dissected ICA. Interestingly, none of the 15 patients who were not stented despite of ICA dissection suffered from a recurrent ipsilateral stroke.10
From a technical point of view there are several options to treat a tandem occlusion with an underlying ICA dissection; the most common are described by Kurre et al.6 Regardless of the technical approach (antegrade/retrograde), treatment of a tandem occlusion is always associated with a prolonged time from groin puncture to reperfusion.2,10,11 Some authors therefore claim the retrograde approach to be superior because intracranial circulation is restored faster.11 In addition to the time issue, there is always the risk of losing the distal position within the true-lumen (in a retrograde approach) or not being able to find the true lumen again (in an anterograde approach). This risk can be minimized with the use of a long microwire, which increases the complexity of the intervention and is time-consuming. Taking all these arguments into consideration, the decision to stent a dissected ICA in cases with tandem occlusions must always to be considered carefully. Our case example demonstrates a novel technical approach in case of a dissected ICA/atherosclerotic stenosis in combination with an intracranial LAO. The ICA stenting over a stent-retriever wire helps to maintain the distal position of the wire because the stent is placed at the clot, leading to a very stable position of the wire. In particular this is an advantage in multi-segmental ICA dissection. Additionally, antegrade flow may be restored while the stent-retriever remains open within the occluded vessel, allowing for reperfusion in the occluded territory while ICA stenting is performed which is favorable independent the underlying ICA pathology. Notably, not all stent-retrievers allow use of this technique as only a few, like the pREset, Aperio (Acandis, Pforzheim, Germany) or Revive (Codman Neuro, Raynham, MA, USA) have a 0.014 inch wire.
Conclusion
The retriever wire supported carotid artery revascularization (ReWiSed CARe) technique utilizing the wire of a stent-retriever as a guiding wire for carotid artery stenting is technically feasible in tandem occlusions caused by a dissected ICA or high grade ICA stenosis. This technique eliminates the need to use a long microwire in order to maintain the position inside the true-lumen of a dissection. Additionally it leads to anterograde perfusion through the released stent-retriever during the time of ICA stenting which is favorable in all tandem occlusion cases.
Declaration of conflicting interests
The authors declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: DB: travel grants from Stryker (DGNR, ESMINT); MNP: travel grants and consultancy for Siemens and Stryker, both none regarding the content of the manuscript; MK: Consultancy for Siemens.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
References
- 1.Goyal M, Menon BK, van Zwam WH, et al. Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet 2016; 387: 1723–1731. [DOI] [PubMed] [Google Scholar]
- 2.Behme D, Mpotsaris A, Zeyen P, et al. Emergency stenting of the extracranial internal carotid artery in combination with anterior circulation thrombectomy in acute ischemic stroke: a retrospective multicenter study. Am J Neuroradiol 2015; 36: 2340–2345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wahlgren N, Moreira T, Michel P, et al. Mechanical thrombectomy in acute ischemic stroke: consensus statement by ESO-Karolinska Stroke Update 2014/2015, supported by ESO, ESMINT, ESNR and EAN. Int J Stroke 2016; 11: 134–147. [DOI] [PubMed] [Google Scholar]
- 4.Sivan-Hoffmann R, Gory B, Armoiry X, et al. Stent-retriever thrombectomy for acute anterior ischemic stroke with tandem occlusion: a systematic review and meta-analysis. Eur Radiol. Epub ahead of print 16 April 2016. DOI: 10.1007/s00330-016-4338-y. [DOI] [PubMed]
- 5.Grigoryan M, Haussen DC, Hassan AE, et al. Endovascular treatment of acute ischemic stroke due to tandem occlusions: large multicenter series and systematic review. Cerebrovasc Dis 2016; 41: 306–312. [DOI] [PubMed] [Google Scholar]
- 6.Kurre W, Bansemir K, Aguilar Perez M, et al. Endovascular treatment of acute internal carotid artery dissections: technical considerations, clinical and angiographic outcome. Neuroradiology 2016; 58: 1167–1179. [DOI] [PubMed] [Google Scholar]
- 7.Jahrestagung der Deutschen Gesellschaft fur Neuroradiologie e.V. in Kooperation mit der 24. Jahrestagung der Osterreichischen Gesellschaft fur Neuroradiologie, 5–8 Oktober 2016, Gurzenich, Koln. Clin Neuroradiol 2016; 26(Suppl 1): 1–111. [DOI] [PubMed]
- 8.Berkhemer OA, Fransen PS, Beumer D, et al. A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med 2015; 372: 11–20. [DOI] [PubMed] [Google Scholar]
- 9.Mpotsaris A, Bussmeyer M, Buchner H, et al. Clinical outcome of neurointerventional emergency treatment of extra- or intracranial tandem occlusions in acute major stroke: antegrade approach with wallstent and solitaire stent retriever. Clin Neuroradiol 2013; 23: 207–215. [DOI] [PubMed] [Google Scholar]
- 10.Marnat G, Mourand I, Eker O, et al. Endovascular management of tandem occlusion stroke related to internal carotid artery dissection using a distal to proximal approach: insight from the RECOST study. Am J Neuroradiol 2016; 37: 1281–1288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lockau H, Liebig T, Henning T, et al. Mechanical thrombectomy in tandem occlusion: procedural considerations and clinical results. Neuroradiology 2015; 57: 589–598. [DOI] [PubMed] [Google Scholar]