Abstract
Sepsis and septic shock are the leading causes of death in critically ill patients. Acute intestinal ischemia/reperfusion (AII/R) is an adaptive response to shock. The high mortality rate from AII/R is due to the severity of the disease and, more importantly, the failure of timely diagnosis. The objective of this investigation is to use nuclear magnetic resonance (NMR) analysis to characterize urine metabolomic profile of AII/R injury in a mouse model. Animals were exposed to sham, early (30 min) or late (60 min) acute intestinal ischemia by complete occlusion of the superior mesenteric artery, followed by 2 hrs of reperfusion. Urine was collected and analyzed by NMR spectroscopy. Urinary metabolite concentrations demonstrated that different profiles could be delineated based on the duration of the intestinal ischemia. Metabolites such as allantoin, creatinine, proline, and methylamine could be predictive of AII/R injury. Lactate, currently used for clinical diagnosis, was found not to significantly contribute to the classification model for either early or late ischemia. This study demonstrates that patterns of changes in urinary metabolites are effective at distinguishing AII/R progression in an animal model. This is a proof-of-concept study to further support examination of metabolites in the clinical diagnosis of intestinal ischemia reperfusion injury in patients. The discovery of a fingerprint metabolite profile of AII/R will be a major advancement in the diagnosis, treatment, and prevention of systemic injury in critically ill patients.
Introduction
Sepsis and septic shock are the leading causes of death in critically ill patients [1]. The gastrointestinal tract serves as an important defence barrier for the body. In critically ill patients, the gastrointestinal tract can become a major pathogenic source of bacteria and inflammatory mediators that can lead to a septic shock [2–5]. Acute intestinal ischemia/reperfusion (AII/R) is an adaptive response to shock. Mortality from shock due to AII/R are 60–90% and have not changed since the 1940s [6–8]. The high mortality rate for AII/R is due to the severity of the disease and, more importantly, the failure of a timely diagnosis. Rapid diagnosis of intestinal ischemia would allow for earlier intervention which would result in: 1) avoidance of surgery by earlier aggressive fluid resuscitation, 2) if surgery was needed, it would occur earlier, resulting in lower postoperative morbidity and mortality.
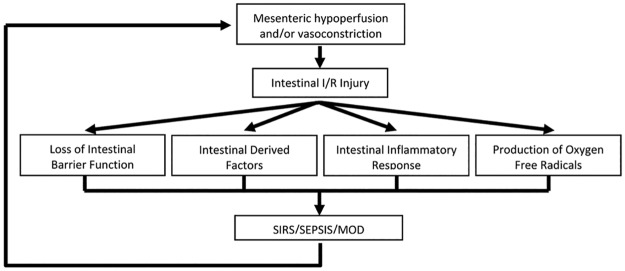
Patients may experience shock as a consequence of the body’s adaptive response to injury. This results in the vasoconstriction and hypoperfusion of mesenteric arteries. This hypoxic condition damages the intestines, which is further exacerbated by subsequent reperfusion leading to AII/R. AII/R induced intestinal mucosal barrier damage and the following inflammation results in the translocation of micro-organisms and endotoxins from the gut lumen into the systemic circulation [9–12], in combination with the production of oxygen-derived free radicals [13, 14], proinflammatory cytokines [15], and other undefined intestinally derived factors [16, 17]. In a murine model of AII/R, we demonstrated local and systemic cytokine increase [18]. The triggered signaling cascade has the potential to escalate into a vicious cycle of continuously increasing intestinal permeability (Fig 1), resulting in local small bowel and distant organ lung injuries [18]. All of these factors ultimately contribute to the onset of sepsis, septic shock and multiple organ dysfunction (MOD).
Fig 1. Cycle of mesenteric hypoperfusion resulting in sepsis, septic shock and MOD.
Following systemic shock there is a decrease intestinal mesenteric perfusion resulting in gastrointestinal injury. This can result in loss of intestinal barrier function, release of intestinal derived factors, production and release of cytokines and free radicals. The culmination of these events can lead to sepsis, septic shock and multiple organ dysfunction (MOD) which contributes to a vicious cycle of local and distant organ injury.
Several treatment modalities have shown the importance of intestinal mucosal integrity in preventing infection. A meta-analysis comparing enteral with parenteral nutrition found a significant reduction in infectious complications and a trend towards decreased mortality [19]. Glutamine, a central amino acid required for intestinal integrity, improves the prognosis in critically ill burn and trauma patients, presumably by maintaining the intestinal barrier and reducing the frequency of infections [19, 20]. It is possible to decrease the bacterial load of the gut through selective digestive tract decontamination consisting of intravenous and topical application of antibiotics in the oropharynx and stomach. In critically ill septic patients, selective digestive tract decontamination resulted in a significant reduction of 28-day mortality [21]. Additionally, we have shown that pretreatment with probiotics in an animal model reduced small bowel tissue injury in AII/R [18]. These studies provide corroborating evidence of the involvement of intestinal microflora in the pathogenesis of sepsis. The knowledge that the microbiota plays an essential role in systemic inflammation caused by AII/R supports the utility of creating a metabolomic profile.
While genomics and proteomics have become useful tools to examine gene and protein expression, metabolomics provides data on an organism’s cellular metabolism (i.e. production of amino acids, peptides, lipids, carbohydrates). The metabolite profile of an organism can vary as a result of environment or disease state. In addition, metabolomics can be used to examine alterations in the intestinal microbiota which may result from infection or metabolic syndromes [22–24]. Studies have proposed the use of metabolomics to diagnosis myocardial infarction [25] and kidney ischemia/reperfusion (I/R) injury following transplantation [26, 27]. One animal study examined late intestinal ischemia without a reperfusion phase [28]. However to date, there have been no studies applying metabolomics profiling to study AII/R.
The purpose of this investigation was to find correlations between the urinary metabolite profile and the development of AII/R injury which will aid in the diagnosis and understanding the metabolite fingerprint associated with early and late AII/R injury. This animal investigation will provide proof-of-concept that can be applied to future studies examining the role of metabolomics in the patient population.
Materials and methods
Animal model
This study was reviewed and approved by the University of Alberta Animal Care and Use Committee and carried out in accordance with guidelines from the Canadian Council on Animal Care (Protocol number: 643/06/11/D). Adult 129/SvEv mice were anesthetised with an intraperitoneal injection of ketamine (120 mg/kg) and xylazine (16 mg/kg) and a laparotomy was performed to expose the superior mesenteric artery. Internal body temperature was maintained at 37°C with overhead heat lamps and/or a heating pad. Animals were subjected to intestinal ischemia as described before [29]. Briefly, occlusion of the superior mesenteric artery was applied with a vascular microclamp (10g pressure). Time points representative of early (30 min, n = 4) and late (60 min, n = 4) intestinal ischemic injury were performed followed by reperfusion via removal of microclamp for 2 hrs. Sham animals were also subjected to laparotomy for 3 hrs however, no microclamp was applied to the mesenteric artery (0 min ischemia, n = 3). Mice were euthanized at the end of the 2 hrs of reperfusion. Organs were harvested for assessment and urine samples were collected directly from the bladder using a 26½G needle. Collected urine were supplemented with 1/10 vol of 0.5% (w/v) sodium azide (NaN3) to prevent bacterial contamination. Samples were given a unique identifiers and then frozen at -80°C until further analysis. The NMR operator (VT) was blinded to the samples prior to processing and analysis.
Myeloperoxidase (MPO) assay
Intestinal tissues were rinsed in PBS and homogenized in 800 μL ice-cold potassium phosphate buffer (50 mM KH2PO4 [pH 6.0] containing 50 mM hexadecyltrimethylammonium bromide (HTAB)) with a hand-held homogenizer for 15 seconds. Samples were sonicated for 15 seconds, frozen in liquid nitrogen and thawed. Following centrifugation (21,000g, 20 mins, 4°C), the supernatants were collected and the pellets were sonicated again in 400 μL of potassium phosphate buffer (pH 6.0) containing 50 mM HTAB, frozen in liquid nitrogen, thawed and centrifuged. Centrifugation, sonication, freezing and thawing was repeated an additional time (3 in total) and all the supernatents were pooled together. The pooled supernatents were frozen at -80°C until MPO activity was analyzed. The protein content of the samples was determined using the Pierce Coomassie BSA Protein Assay (Pierce, Rockford, IL). MPO activity was assessed by addition of 10 μL sample to 290 μL assay buffer (50 mM KH2PO4, pH 6.0 with 0.167 mg/mL o-dianisidine dihydrochloride and 0.0005% H2O2). The reaction kinetics (Vmax) were analyzed every minute over 30 minutes at 460 nM on a microplate reader. The Vmax value was divided by the protein concentration in order to compare MPO activity across different samples.
Nuclear magnetic resonance (NMR) analysis
Urine samples were centrifuged (4.7k x g) through rehydrated Nanosep Omega 3Kspin filters (Pall Corporation, Port Washington, NY) to remove debris/protein. Collected urine were diluted to 635 μL and 65 μL of internal standard (5 mM sodium 2, 2-dimethyl-2-silapentane-5-sulfonate-d6; DSS-d6) plus 0.2% sodium azide in 100% D2O (Chenomx internal standard, Chenomx Inc., Edmonton, Canada). The pH of each urine sample was adjusted to 6.8 ± 0.1 with HCl or NaOH. A 700 μL aliquot was placed in a 5 mm NMR tube (Wilmad, Buena, NJ) and NMR analysis was performed on the same day. One-dimensional NMR spectra of urine samples were acquired using the first increment of the standard ‘Nuclear OverHauser Enhancement Spectroscopy’ (NOESY) pulse sequence on a four-channel Varian INOVA 600 MHz NMR spectrometer equipped with a triax-gradient 5 mm HCN probe as previously described [30, 31]. Quantification of metabolites was achieved using Chenomx NMR Suite 7.0 (Chenomx Inc.). The Chenomx compound library contains 297 compounds. The NMR variables (metabolites) derived from spectral analysis were log10 transformed, mean centered, and unit variance scaling was applied. Principal component analysis (PCA) and orthogonal partial least squares-discriminant analysis (OPLS-DA) was conducted using SIMCA P11.0 (Umetrics, Umeå, Sweden). Individual metabolites (sham vs. AII/R) were analyzed by Mann-Whitney U test over the time course of ischemia. The univariate test was conducted using the Prism 4.0c (GraphPad Software Inc., San Diego, CA).
Results
Intestinal myeloperoxidase (MPO) as an index of inflammation/injury
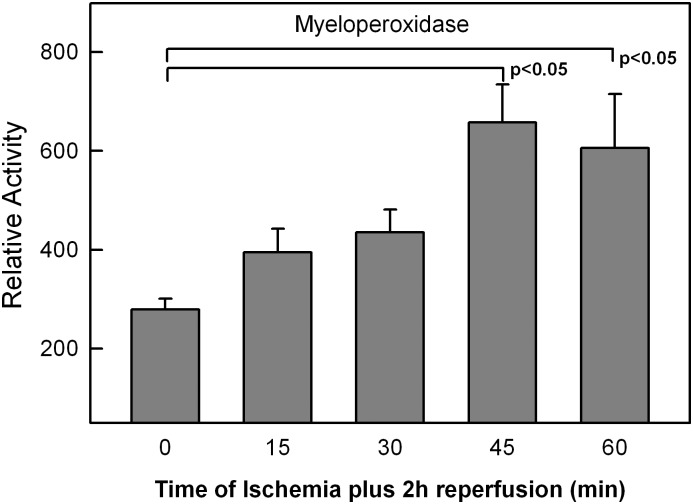
A time course for intestinal ischemia was performed at 0, 15, 30, 45, 60 minutes followed by 2 hours of reperfusion. There was an increase in MPO levels with increasing ischemia times (Fig 2). Significance in MPO activity was reached at 45 min and 60 min of ischemia compared to shame. Three time points were subsequently chosen to perform NMR analysis, sham (no ischemia), early (30 min) and late (60 min) of acute intestinal ischemia followed by 2 hours of reperfusion.
Fig 2. Small bowel myeloperoxidase (MPO) levels following acute intestinal ischemia/reperfusion (AII/R) injury.
Ischemia times were set up to represent a time course of intestinal ischemia from 0–60 min all followed by 2 hrs of reperfusion. Myeloperoxidase activity, used a surrogate marker of tissue injury, demonstrates increased intestinal injury with increasing ischemia time. MPO activity is expressed as the maximum rate of OD460 change (Vmax) normalized to the protein concentration ([protein]) of each tissue sample. Data for each animal group is expressed as the mean MPO activity with the standard error of the mean. Statistical significance was determined at p<0.05 via one-way ANOVA (nonparametric) test.
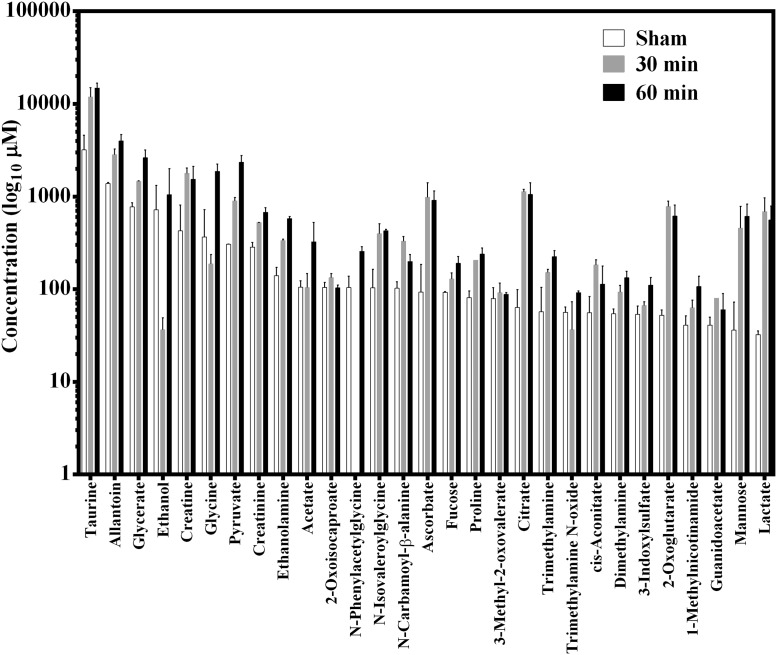
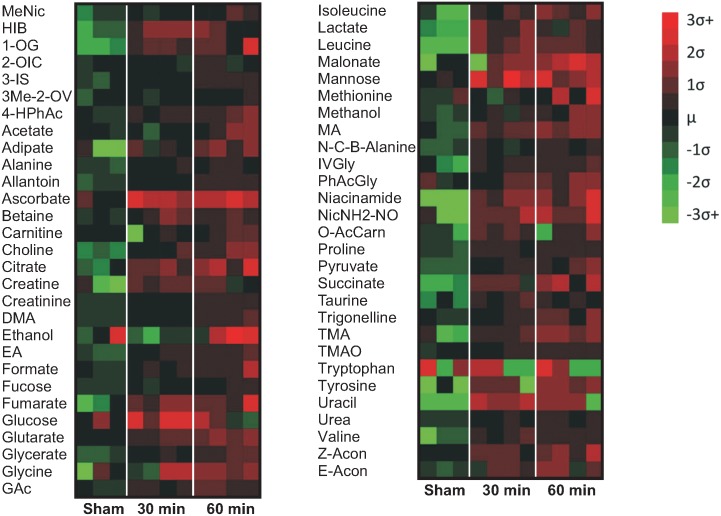
Metabolites identified in urine
Metabolite concentrations in the urine samples (sham and AII/R injury) were derived from NMR spectra analysis using a library of 297 compounds. Altogether, 57 compounds were identified in the spectra ranging from alcohols, amino acids, fatty acids, and lipids. The top 29 metabolites at baseline were illustrated from highest to lowest with lactate being the lowest (Fig 3). The concentrations of most of the metabolites were higher in the 30 min and 60 min ischemia groups compared to the sham controls (see S1 Table in the supporting data). To better visualise changes in metabolites concentration, we illustrated the results using a heat map (Fig 4). The heat map was created with the standard scores for the 57 metabolites from sham versus 30 min and 60 min of AII/R injury. The ‘standard score’ shows how the concentration of each metabolite changes relative to the mean value of the entire pooled group. Red color indicates that there was a greater abundance of that specific metabolite compared to the mean of the group; while green is indicative of lower metabolite levels. AII/R had a direct effect on the concentrations of metabolites as there was a clear visual difference between the sham animals (Fig 4, column 1–3) and the 30 min (column 4–7) and 60 min of AII/R (column 8–11). Compared to the AII/R treated mice, the concentrations of metabolites in the sham group were relatively lower than the 30 min and 60 min ischemia groups.
Fig 3. Metabolite concentrations from sham and acute intestinal ischemia/reperfusion (AII/R).
Urine from animals in sham, 30 min and 60 min ischemia (all followed by 2 hrs of reperfusion) were analyzed by NMR spectroscopy. The raw concentrations of the top 29 metabolites are illustrated. These were selected to illustrate the concentration of lactate, a common blood marker for tissue injury. Data is expressed as mean ± standard error. None of the metabolite concentrations were found to be statistically significant from the sham-treated animals.
Fig 4. Heat map profile of metabolites from sham and acute intestinal ischemia/reperfusion (AII/R) animals.
There were 57 compounds that were identified in the urine of mice in the sham and AII/R-treated groups. These metabolites belong to a variety of biochemical sub-groups. Metabolite concentrations across all animals were averaged and the resulting difference (± standard deviation; σ) displayed as a color index of red (>mean) or green (<mean). Sham (#1–3), 30 min (#4–7) and 60 min (#8–11) intestinal ischemia animals.
Principal component analysis (PCA) of varying times of intestinal ischemia
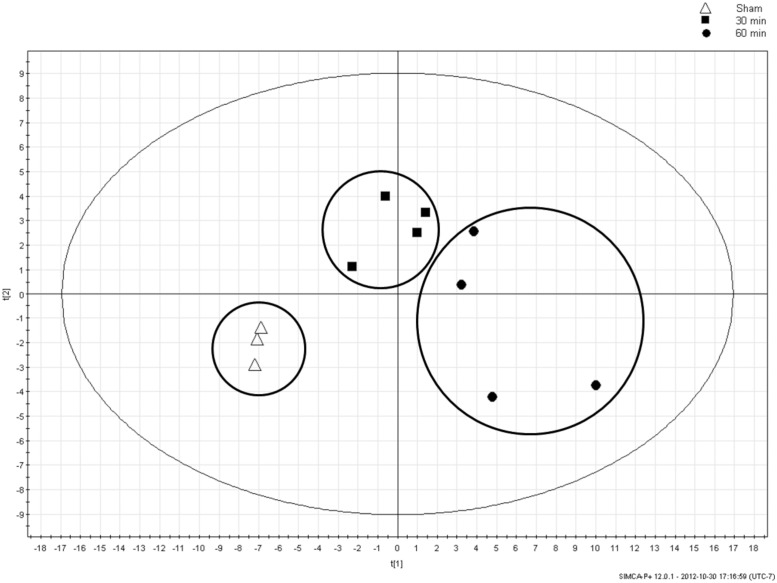
PCA is an unsupervised multivariate statistical analysis method that strives to reduce the dimensionality of multidimensional datasets [32]. PCA was used here to identify the interrelatedness within the groups. In other words, if left unsupervised, do the 3 groups—sham, early and late AII/R—group together based on their metabolite measurements? The PCA plot showed clustering of the AII/R treatment groups which separated from the sham animals (Fig 5). This finding corroborated our heat map data where a visual difference between the AII/R treatment groups and sham was observed.
Fig 5. Principal component analysis (PCA) of animal groups with varying times of intestinal ischemia.
Metabolites identified in the NMR spectra were condensed by PCA analysis into 2 variables (t[1] (57.3%) and t[2] (12.1%)). Analysis demonstrated a clear separation between Sham (Δ), 30 min ischemia (■) and 60 min ischemia (●) animal groups.
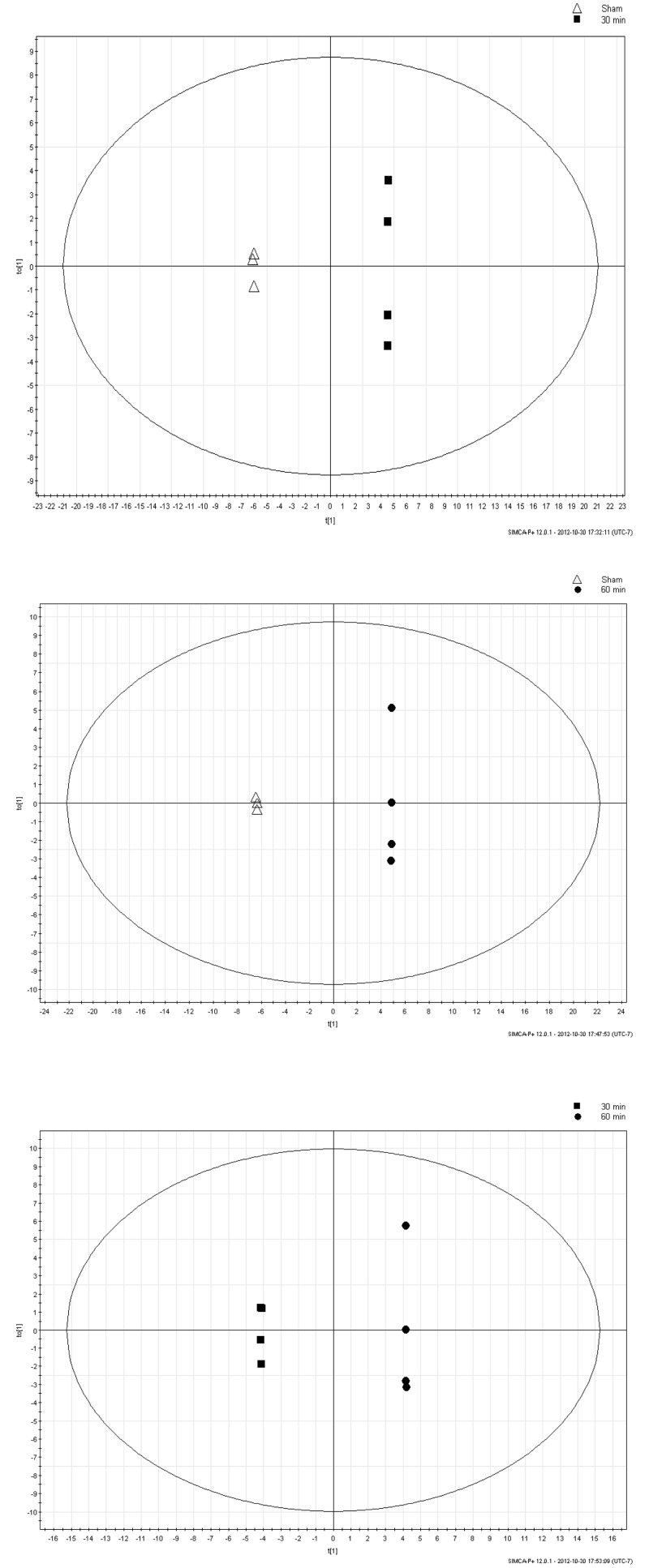
Orthogonal projection to latent structures-discriminant analysis (OPLS-DA)
OPLS-DA is a regression extension of PCA. OPLS-DA is a supervised analysis which uses class information in an attempt to maximize the separation between the groups of observations. OPLS-DA of all data derived from measured urine metabolite concentrations of sham and AII/R animals is presented in Fig 6. The groups of sham, 30, and 60 min were assigned to the program to mathematically determine the largest differences in the metabolites to separate these groups. OPLS-DA demonstrated metabolite differences with progression of early (30 min) to late (60 min) intestinal ischemia.
Fig 6. Orthogonal projection to latent structures-discriminant analysis (OPLS-DA).
The OPLS-DA of sham versus 30 min of intestinal ischemia (a), sham versus 60 min of ischemia (b), and 30 versus 60 min of ischemia (c) show a clear separation of the metabolites with sham, early and late ischemia times.
Variable Importance in the Projection (VIP) plot to identify metabolites
Following the illustration that the 3 different treatment groups (sham, 30 min and 60 min) separated and clustered together, we wanted to identify which metabolites were more likely to have an impact on predicting ischemic injury. VIP plots are used to show which metabolites have the greatest overall impact on shaping the model of AII/R injury. A Z-score was used to standardize the VIP values in terms of the number of standard deviations the mean VIP number is above a zero value. Any value above the Z-score of 1.64 was associated with having a statistically significant impact on the overall model (see Table 1 for comparisons between sham vs. 30min and sham vs. 60min). Some common metabolites such as allantoin, creatinine, proline, and methylamine were found to have an important effect in differentiating AII/R injury from sham. It is important to note that although lactate is used as a serum clinical marker for AII/R injury, urine lactate measurements did not play an important in predicting intestinal ischemia in our model. Analysis of urine lactate showed a trend towards significant difference (P = 0.057) between sham and 30 min or 60 min of AII/R (Fig 7).
Table 1. Analysis of Variable Importance in Projection (VIP) metabolites at 30 and 60 min.
| Metabolites | Sham vs 30m | Sham vs 60 m | |||
|---|---|---|---|---|---|
| Z-score | P value | Z-score | P value | ||
| Amines | Methylamine | 3.49 | 0.001 | 3.54 | 0.001 |
| Ethanolamine | 2.37 | 0.01 | 2.40 | 0.01 | |
| Dimethylamine | 2.41 | 0.01 | 4.17 | 0.001 | |
| Trimethylamine | 0.92 | 0.18 | 1.91 | 0.05 | |
| Amino Acids | Valine | 1.67 | 0.05 | 3.48 | 0.001 |
| Leucine | 2.34 | 0.01 | 2.02 | 0.05 | |
| Isoleucine | 2.26 | 0.01 | 2.63 | 0.01 | |
| N-Isovaleroylglycine | 1.93 | 0.05 | 2.03 | 0.05 | |
| Proline | 2.65 | 0.01 | 3.14 | 0.001 | |
| Alanine | 2.56 | 0.01 | 1.77 | 0.05 | |
| Tyrosine | 0.76 | 0.22 | 2.29 | 0.01 | |
| Lipid Metabolism | Choline | 1.31 | 0.10 | 2.65 | 0.01 |
| Glycerate | 2.45 | 0.01 | 4.04 | 0.001 | |
| Glutarate | 1.66 | 0.01 | 2.17 | 0.05 | |
| Purines | Allantoin | 4.61 | 0.001 | 6.62 | 0.00001 |
| Urea | 2.77 | 0.01 | 2.08 | 0.05 | |
| Creatinine | 2.97 | 0.001 | 5.25 | 0.001 | |
| Creatine | 1.62 | 0.05 | 0.52 | 0.30 | |
| Others | 4-Hydroxyphenylacetate | 1.78 | 0.05 | 2.05 | 0.05 |
| Fucose | 2.57 | 0.01 | 2.33 | 0.01 | |
A Z-score was used to standardize the VIP values. Any value above the Z-score of 1.64 was associated with having a statistically significant impact on the overall model.
Fig 7. Lactate concentrations cannot differentiate early from late intestinal ischemia/reperfusion (AII/R) injury.
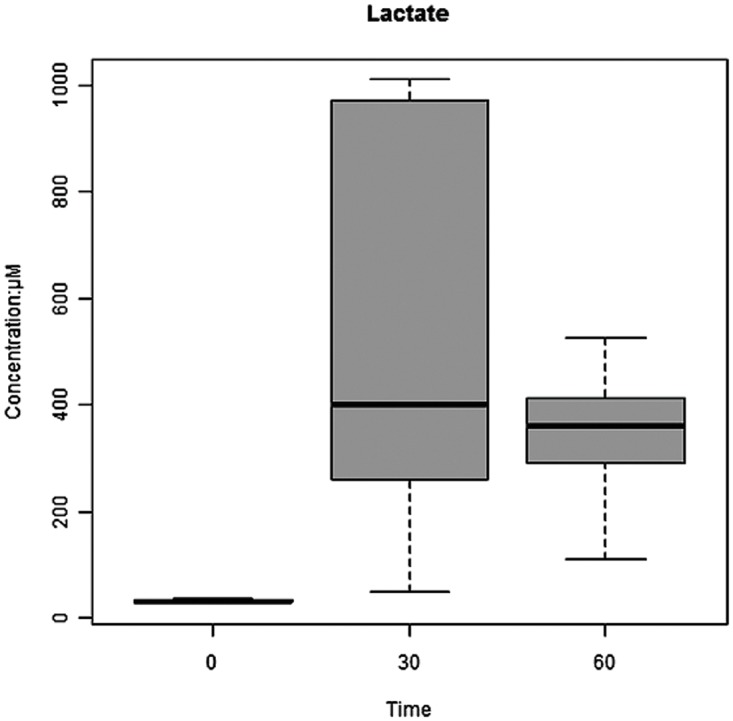
Mean lactate levels increased with AII/R injury but did not differentiate early (30 min) from late (60 min) intestinal ischemia.
Discussion
Acute intestinal ischemia/reperfusion (AII/R) broadly affects critically ill patients in the areas of trauma, transplantation, cardiac surgery, shock, and sepsis. AII/R injury is associated with high mortality rates ranging from 60–90% which has not changed in the last 70 years [6–8]. The high mortality is attributable, in part, to the lack of a predictive diagnostic test that can facilitate the early detection in those at high-risk for intestinal ischemia. This is particularly relevant in those who are critically ill where the classic symptoms of abdominal pain are obfuscated due to sedation and mechanical ventilation [33]. Earlier diagnosis can result in either earlier treatment potentially preventing the need for surgery or if surgery was indicated, it would occur earlier, reducing the morbidity and mortality. We have demonstrated in patients that conventional markers of intestinal ischemia, serum lactate and white blood cell count (WBC) both lack sensitivity and specificity [34], whereas invasive diagnostic tests, such as computer tomography (CT) or angiography, expose patients to the risk of contrast-induced nephropathy and are also not definitive [35].
The aim of this study was to evaluate the potential for diagnosing AII/R using metabolic profiling. Here we used an unsupervised PCA plot to convert a large pool of metabolites that were condensed into a 2-dimentional data set. We illustrated a clear separation between sham controls and AII/R treated mice at 30 min and 60 min, demonstrating that urinary metabolite concentrations are effective at distinguishing AII/R progression. PCA data derived from measured urinary metabolite concentration has the power to differentiate a unique metabolite fingerprint based on the duration of ischemia. Serum lactate is normally used in clinical medicine to ascertain ischemia, however in our model, urine lactate did not play a significant role as a predictive metabolite in differentiating between sham and intestinal ischemia. Previous studies conducted by us and others have shown that urine lactate is not a good predictor of intestinal ischemia [29, 34, 36]. Only one paper has examined metabolite makers in a mouse intestinal ischemia model, using gas chromatography-mass spectrometry, and they corroborate our findings that lactate was not a predictive marker of intestinal ischemia [28]. However, two important distinguishing features in this paper was that metabolomics analysis was done on serum samples, while their model only had an ischemia phase without reperfusion. Our study utilised urine samples and included the important and clinically relevant reperfusion which results in liberation of oxygen free radicals leading to local and distant organ injury [13, 14, 18, 37].
Metabolomics is increasingly being used to study the pathophysiology of gastrointestinal diseases [38]. Though very limited publications have looked at metabolite changes following acute intestinal inflammation, several studies were able to discriminate patients with chronic intestinal inflammation (those with inflammatory bowel disease) from non-inflamed controls (reviewed by De Preter and Verbeke (38)). According to our VIP plot, there were 16 metabolites that played a statistically significant role in directing changes in both 30 and 60 min time points in the AII/R mice compared to the sham controls. The vast majority of these 16 metabolites developed into several common themes with respect to metabolic processes (Table 1). In comparing sham versus 30min AII/R animals, we found allantoin (ranked #1/16 via Z score), methylamine (2/16), creatinine (3/16), and to a lesser extent, urea as the top contributing metabolites in the early acute ischemia. Allantoin is the predominant product of free radical-induced oxidation product of uric acid. Uric acid acts as an antioxidant and upon the availability of biologically relevant oxidants, it is converted into allantoin [39]. Similar to other studies that showed allantoin as a sensitive marker of oxidative stress [39–41], we also show here that AII/R injury results in high levels of allantoin at both ischemia times. Methylamine is a product of gut bacteria metabolising dietary choline and it is lowered upon alterations in gut microbiota composition [42–44]. It is therefore not surprising that after 60 min of ischemia, the levels of methyalamines drops and level of choline increases in our model. We [18] and others [45] have shown that probiotics and preservation of gut microbiota can protect the intestine against ischemia/reperfusion-induced intestinal injury. Interestingly, creatinine was a consistent driving metabolite at both 30 and 60 min; its precursor, creatine was a driving metabolite at 30 min (but not at 60 min). This may indicate an elevation of creatine might be a marker for early I/R while its breakdown product, creatinine remains elevated even during the late ischemia phase (60 min).
Several key amino acids were fundamental in driving overall metabolite changes at both 30 and 60 min. Alanine is an end product of amino acid catabolism at a multitude of metabolic loci, and it is synthesized and secreted in abundance under even the most favourable conditions [46]. Alanine typically increases from intestinal amino acid catabolism. However, here we show that with an increase in ischemia times (from 30 min to 60 min), synthesize of alanine is disrupted and its effect on the ischemic model decreases. We speculate that with prolonged intestinal ischemia might shut down vital metabolomic and catabolism processes in the intestine [47]. As such, we also observed decrease of leucine, and proline following 60 min ischemia. However, we noted an increase in valine and isoleucine at 60 min ischemia. Valine and isoleucine are part of the branched-chain amino acids (BCAA) that promote normal growth, tissue repairs and help prevent the breakdown of muscle. Increase of these BCAA supports the theory that prolonged ischemia shuts down the body’s metabolomic and catabolism processes. Other compounds such as fucose, ethanolamine, methylamine, dimethylamine and 4-hydroxyphenylacetate exhibit a consistent theme of an adverse event leading to cell and tissue degradation. While others have used false discovery rate as a mathematical model to control for false-positive discoveries [48–50], we utilised class membership or family-wise correction via OPLS-DA to better expose separation between the treatment groups. Our aim was to identify differences in metabolites between the groups, however, further studies are needed to generate cross validated predictive models.
Though metabolomics-based strategies provide a powerful tool in modern clinical research and precision medicine, precautionary steps are needed in order to avoid pitfalls. Inconsistent sample collection, storage and subsequent preparation for NMR can alter the concentrations of measured metabolites [51]. Additionally, poor quality of data obtained and subsequent data analysis can hamper the interpretation of the data. Rarely do single metabolomic changes occur in pathology but instead a pattern of changes are observed resulting in the metabolic fingerprint or metabolic profile. For this reason, multivariate statistics are required to analyze the data using individual covariate metabolites as well as interaction terms when necessary. Care must be taken to prevent chance correlations and/or of overfitting of the data.
Conclusions
This study illustrates that changes in the urinary metabolite profile detected through NMR analysis is effective at detecting AII/R injury and progression in an animal model. The difference in injury was apparent in the PCA and heat map analysis which demonstrated the utility of metabolomics as a diagnostic tool. The unique metabolic fingerprint for AII/R injury makes it an attractive non-invasive and sensitive diagnostic test for AII/R injury. Furthermore, lactate which is a traditional metabolite marker currently used in clinical medicine was not a sensitive predictor of AII/R injury. This proof-of-concept study supports the further examination of NMR technology in a patient population at risk for intestinal ischemia. The discovery of a fingerprint profile of AII/R will be a major advancement in its diagnosis and treatment in critically ill patients.
Supporting information
This illustrates the metabolites that play a role in the changes seen following acute intestinal ischemia/reperfusion injury.
(TIF)
The concentrations of the metabolites found in sham controls, 30 min and 60 min ischemia groups are presented.
(DOCX)
Acknowledgments
We gratefully thank Chenomx and Dr. David Chang for assistance on data analysis. The authors acknowledge the Canadian National High Field NMR Centre (NANUC) for use of the facilities for collection of the NMR data.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
None of the authors have any financial disclosure.
References
- 1.Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). Jama. 2016;315(8):801–10. doi: 10.1001/jama.2016.0287 ; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Swank GM, Deitch EA. Role of the gut in multiple organ failure: bacterial translocation and permeability changes. World journal of surgery. 1996;20(4):411–7. Epub 1996/05/01. . [DOI] [PubMed] [Google Scholar]
- 3.Taylor DE. Revving the motor of multiple organ dysfunction syndrome. Gut dysfunction in ARDS and multiorgan failure. Respir Care Clin N Am. 1998;4(4):611–31, vii–viii. Epub 1999/01/09. . [PubMed] [Google Scholar]
- 4.Nieuwenhuijzen GA, Goris RJ. The gut: the 'motor' of multiple organ dysfunction syndrome? Curr Opin Clin Nutr Metab Care. 1999;2(5):399–404. Epub 1999/12/10. . [DOI] [PubMed] [Google Scholar]
- 5.Rotstein OD. Pathogenesis of multiple organ dysfunction syndrome: gut origin, protection, and decontamination. Surgical infections. 2000;1(3):217–23; discussion 23–5. Epub 2003/02/22. doi: 10.1089/109629600750018141 . [DOI] [PubMed] [Google Scholar]
- 6.Klempnauer J, Grothues F, Bektas H, Pichlmayr R. Long-term results after surgery for acute mesenteric ischemia. Surgery. 1997;121(3):239–43. Epub 1997/03/01. . [DOI] [PubMed] [Google Scholar]
- 7.Wilcox MG, Howard TJ, Plaskon LA, Unthank JL, Madura JA. Current theories of pathogenesis and treatment of nonocclusive mesenteric ischemia. Dig Dis Sci. 1995;40(4):709–16. Epub 1995/04/01. . [DOI] [PubMed] [Google Scholar]
- 8.Kassahun WT, Schulz T, Richter O, Hauss J. Unchanged high mortality rates from acute occlusive intestinal ischemia: six year review. Langenbecks Arch Surg. 2008;393(2):163–71. Epub 2008/01/04. doi: 10.1007/s00423-007-0263-5 . [DOI] [PubMed] [Google Scholar]
- 9.Deitch EA. Bacterial translocation or lymphatic drainage of toxic products from the gut: what is important in human beings? Surgery. 2002;131(3):241–4. Epub 2002/03/15. . [DOI] [PubMed] [Google Scholar]
- 10.Sheng ZY, Dong YL, Wang XH. Bacterial translocation and multiple system organ failure in bowel ischemia and reperfusion. Chin Med J (Engl). 1991;104(11):897–903. Epub 1991/11/01. . [PubMed] [Google Scholar]
- 11.Marshall JC, Christou NV, Meakins JL. The gastrointestinal tract. The "undrained abscess" of multiple organ failure. Ann Surg. 1993;218(2):111–9. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pastores SM, Katz DP, Kvetan V. Splanchnic ischemia and gut mucosal injury in sepsis and the multiple organ dysfunction syndrome. Am J Gastroenterol. 1996;91(9):1697–710. . [PubMed] [Google Scholar]
- 13.Granger DN. Role of xanthine oxidase and granulocytes in ischemia-reperfusion injury. Am J Physiol. 1988;255(6 Pt 2):H1269–75. . [DOI] [PubMed] [Google Scholar]
- 14.McKelvey TG, Hollwarth ME, Granger DN, Engerson TD, Landler U, Jones HP. Mechanisms of conversion of xanthine dehydrogenase to xanthine oxidase in ischemic rat liver and kidney. Am J Physiol. 1988;254(5 Pt 1):G753–60. . [DOI] [PubMed] [Google Scholar]
- 15.Deitch EA, Xu D, Franko L, Ayala A, Chaudry IH. Evidence favoring the role of the gut as a cytokine-generating organ in rats subjected to hemorrhagic shock. Shock. 1994;1(2):141–5. Epub 1994/02/01. . [DOI] [PubMed] [Google Scholar]
- 16.Dayal SD, Hauser CJ, Feketeova E, Fekete Z, Adams JM, Lu Q, et al. Shock mesenteric lymph-induced rat polymorphonuclear neutrophil activation and endothelial cell injury is mediated by aqueous factors. The Journal of trauma. 2002;52(6):1048–55; discussion 55. Epub 2002/06/05. . [DOI] [PubMed] [Google Scholar]
- 17.Adams JM, Hauser CJ, Adams CA, Xu DZ, Livingston DH, Deitch EA. Entry of gut lymph into the circulation primes rat neutrophil respiratory burst in hemorrhagic shock. Crit Care Med. 2001;29(11):2194–8. Epub 2001/11/09. . [DOI] [PubMed] [Google Scholar]
- 18.Salim SY, Young PY, Lukowski CM, Madsen KL, Sis B, Churchill TA, et al. VSL#3 probiotics provide protection against acute intestinal ischaemia/reperfusion injury. Beneficial microbes. 2013;4(4):357–65. doi: 10.3920/BM2013.0026 . [DOI] [PubMed] [Google Scholar]
- 19.Heyland DK, Dhaliwal R, Drover JW, Gramlich L, Dodek P. Canadian clinical practice guidelines for nutrition support in mechanically ventilated, critically ill adult patients. JPEN J Parenter Enteral Nutr. 2003;27(5):355–73. Epub 2003/09/16. doi: 10.1177/0148607103027005355 . [DOI] [PubMed] [Google Scholar]
- 20.De-Souza DA, Greene LJ. Intestinal permeability and systemic infections in critically ill patients: effect of glutamine. Crit Care Med. 2005;33(5):1125–35. Epub 2005/05/14. . [DOI] [PubMed] [Google Scholar]
- 21.de Smet AM, Kluytmans JA, Cooper BS, Mascini EM, Benus RF, van der Werf TS, et al. Decontamination of the digestive tract and oropharynx in ICU patients. The New England journal of medicine. 2009;360(1):20–31. Epub 2009/01/02. doi: 10.1056/NEJMoa0800394 . [DOI] [PubMed] [Google Scholar]
- 22.Gill SR, Pop M, Deboy RT, Eckburg PB, Turnbaugh PJ, Samuel BS, et al. Metagenomic analysis of the human distal gut microbiome. Science. 2006;312(5778):1355–9. Epub 2006/06/03. doi: 10.1126/science.1124234 ; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sekirov I, Finlay BB. Human and microbe: united we stand. Nat Med. 2006;12(7):736–7. Epub 2006/07/11. doi: 10.1038/nm0706-736 . [DOI] [PubMed] [Google Scholar]
- 24.Nicholson JK, Holmes E, Wilson ID. Gut microorganisms, mammalian metabolism and personalized health care. Nat Rev Microbiol. 2005;3(5):431–8. Epub 2005/04/12. doi: 10.1038/nrmicro1152 . [DOI] [PubMed] [Google Scholar]
- 25.Sabatine MS, Liu E, Morrow DA, Heller E, McCarroll R, Wiegand R, et al. Metabolomic identification of novel biomarkers of myocardial ischemia. Circulation. 2005;112(25):3868–75. Epub 2005/12/14. doi: 10.1161/CIRCULATIONAHA.105.569137 . [DOI] [PubMed] [Google Scholar]
- 26.Wishart DS. Metabolomics in monitoring kidney transplants. Curr Opin Nephrol Hypertens. 2006;15(6):637–42. Epub 2006/10/21. doi: 10.1097/01.mnh.0000247499.64291.52 . [DOI] [PubMed] [Google Scholar]
- 27.Serkova N, Fuller TF, Klawitter J, Freise CE, Niemann CU. H-NMR-based metabolic signatures of mild and severe ischemia/reperfusion injury in rat kidney transplants. Kidney international. 2005;67(3):1142–51. Epub 2005/02/09. doi: 10.1111/j.1523-1755.2005.00181.x . [DOI] [PubMed] [Google Scholar]
- 28.Fahrner R, Beyoglu D, Beldi G, Idle JR. Metabolomic markers for intestinal ischemia in a mouse model. J Surg Res. 2012. Epub 2012/09/06. doi: 10.1016/j.jss.2012.08.011 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Khadaroo RG, Fortis S, Salim SY, Streutker C, Churchill TA, Zhang H. I-FABP as biomarker for the early diagnosis of acute mesenteric ischemia and resultant lung injury. PloS one. 2014;9(12):e115242 doi: 10.1371/journal.pone.0115242 ; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Slupsky CM, Rankin KN, Wagner J, Fu H, Chang D, Weljie AM, et al. Investigations of the effects of gender, diurnal variation, and age in human urinary metabolomic profiles. Analytical chemistry. 2007;79(18):6995–7004. Epub 2007/08/19. doi: 10.1021/ac0708588 . [DOI] [PubMed] [Google Scholar]
- 31.Weljie AM, Newton J, Mercier P, Carlson E, Slupsky CM. Targeted profiling: quantitative analysis of 1H NMR metabolomics data. Analytical chemistry. 2006;78(13):4430–42. Epub 2006/07/01. doi: 10.1021/ac060209g . [DOI] [PubMed] [Google Scholar]
- 32.Sainani KL. Introduction to principal components analysis. PM & R: the journal of injury, function, and rehabilitation. 2014;6(3):275–8. doi: 10.1016/j.pmrj.2014.02.001 . [DOI] [PubMed] [Google Scholar]
- 33.Khadaroo RG, Marshall JC. Gastrointestinal dysfunction in the critically ill: can we measure it? Crit Care. 2008;12(5):180 Epub 2008/10/03. doi: 10.1186/cc7001 ; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Salim SY, Young PY, Churchill TA, Khadaroo RG. Urine intestinal fatty acid-binding protein predicts acute mesenteric ischemia in patients. J Surg Res. 2016. doi: 10.1016/j.jss.2016.07.017 . [DOI] [PubMed] [Google Scholar]
- 35.Glenister KM, Corke CF. Infarcted intestine: a diagnostic void. ANZ J Surg. 2004;74(4):260–5. Epub 2004/03/27. doi: 10.1111/j.1445-2197.2004.02956.x . [DOI] [PubMed] [Google Scholar]
- 36.Demir IE, Ceyhan GO, Friess H. Beyond Lactate: Is There a Role for Serum Lactate Measurement in Diagnosing Acute Mesenteric Ischemia? Digest Surg. 2012;29(3):226–35. doi: 10.1159/000338086 [DOI] [PubMed] [Google Scholar]
- 37.Nishino T. The conversion of xanthine dehydrogenase to xanthine oxidase and the role of the enzyme in reperfusion injury. J Biochem (Tokyo). 1994;116(1):1–6. . [DOI] [PubMed] [Google Scholar]
- 38.De Preter V, Verbeke K. Metabolomics as a diagnostic tool in gastroenterology. World J Gastrointest Pharmacol Ther. 2013;4(4):97–107. ; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kand'ar R, Zakova P, Muzakova V. Monitoring of antioxidant properties of uric acid in humans for a consideration measuring of levels of allantoin in plasma by liquid chromatography. Clin Chim Acta. 2006;365(1–2):249–56. doi: 10.1016/j.cca.2005.09.002 . [DOI] [PubMed] [Google Scholar]
- 40.Yardim-Akaydin S, Sepici A, Ozkan Y, Simsek B, Sepici V. Evaluation of allantoin levels as a new marker of oxidative stress in Behcet's disease. Scand J Rheumatol. 2006;35(1):61–4. doi: 10.1080/03009740510026878 . [DOI] [PubMed] [Google Scholar]
- 41.Dryland P, Love D, Walker M, Dommels Y, Butts C, Rowan D, et al. Allantoin as A Biomarker of Inflammation in an Inflammatory Bowel Disease Mouse Model: NMR Analysis of Urine. The Open Bioactive Compounds Journal 2008;1:6. [Google Scholar]
- 42.Pelantova H, Bartova S, Anyz J, Holubova M, Zelezna B, Maletinska L, et al. Metabolomic profiling of urinary changes in mice with monosodium glutamate-induced obesity. Anal Bioanal Chem. 2016;408(2):567–78. doi: 10.1007/s00216-015-9133-0 . [DOI] [PubMed] [Google Scholar]
- 43.Yap IK, Li JV, Saric J, Martin FP, Davies H, Wang Y, et al. Metabonomic and microbiological analysis of the dynamic effect of vancomycin-induced gut microbiota modification in the mouse. J Proteome Res. 2008;7(9):3718–28. doi: 10.1021/pr700864x . [DOI] [PubMed] [Google Scholar]
- 44.Goytia M, Shafer WM. Polyamines can increase resistance of Neisseria gonorrhoeae to mediators of the innate human host defense. Infection and immunity. 2010;78(7):3187–95. doi: 10.1128/IAI.01301-09 ; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Perez-Chanona E, Muhlbauer M, Jobin C. The microbiota protects against ischemia/reperfusion-induced intestinal injury through nucleotide-binding oligomerization domain-containing protein 2 (NOD2) signaling. Am J Pathol. 2014;184(11):2965–75. doi: 10.1016/j.ajpath.2014.07.014 ; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Drake KJ, Sidorov VY, McGuinness OP, Wasserman DH, Wikswo JP. Amino acids as metabolic substrates during cardiac ischemia. Exp Biol Med (Maywood). 2012;237(12):1369–78. doi: 10.1258/ebm.2012.012025 ; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kalogeris T, Baines CP, Krenz M, Korthuis RJ. Cell biology of ischemia/reperfusion injury. Int Rev Cell Mol Biol. 2012;298:229–317. doi: 10.1016/B978-0-12-394309-5.00006-7 ; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Yoav B, Yosef H. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J R Statist Soc B. 1995;57:289–300. [Google Scholar]
- 49.Kim SB, Chen VC, Park Y, Ziegler TR, Jones DP. Controlling the False Discovery Rate for Feature Selection in High-resolution NMR Spectra. Stat Anal Data Min. 2008;1(2):57–66. doi: 10.1002/sam.10005 ; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Sreekumar A, Poisson LM, Rajendiran TM, Khan AP, Cao Q, Yu J, et al. Metabolomic profiles delineate potential role for sarcosine in prostate cancer progression. Nature. 2009;457(7231):910–4. doi: 10.1038/nature07762 ; [DOI] [PMC free article] [PubMed] [Google Scholar] [Research Misconduct Found]
- 51.Kohler I, Verhoeven A, Derks RJ, Giera M. Analytical pitfalls and challenges in clinical metabolomics. Bioanalysis. 2016;8(14):1509–32. doi: 10.4155/bio-2016-0090 . [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
This illustrates the metabolites that play a role in the changes seen following acute intestinal ischemia/reperfusion injury.
(TIF)
The concentrations of the metabolites found in sham controls, 30 min and 60 min ischemia groups are presented.
(DOCX)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.