Abstract
Educational needs assessments for nephrology fellowship training are limited. This study assessed fellows’ perceptions of current educational needs and interest in novel modalities that may improve their educational experience and quantified educational resources used by programs and fellows. We distributed a seven-question electronic survey to all United States–based fellows receiving complimentary American Society of Nephrology (ASN) membership at the end of the 2015–2016 academic year in conjunction with the ASN Nephrology Fellows Survey. One third (320 of 863; 37%) of fellows in Accreditation Council for Graduate Medical Education–accredited positions responded. Most respondents rated overall quality of teaching in fellowship as either “good” (37%) or “excellent” (44%), and most (55%) second-year fellows felt “fully prepared” for independent practice. Common educational resources used by fellows included UpToDate, Journal of the American Society of Nephrology/Clinical Journal of the American Society of Nephrology, and Nephrology Self-Assessment Program; others—including ASN’s online curricula—were used less often. Fellows indicated interest in additional instruction in several core topics, including home dialysis modalities, ultrasonography, and pathology. Respondents strongly supported interventions to improve pathology instruction and increase time for physiology and clinical review. In conclusion, current nephrology fellows perceive several gaps in training. Innovation in education and training is needed to better prepare future nephrologists for the growing challenges of kidney care.
Keywords: education, fellowship, needs-assessment
Although the prevalence of CKD may be plateauing, there is growing demand for nephrology care. Simultaneously, decreasing interest in nephrology among medical students and residents indicates that the future workforce may not be adequate to meet the needs of patients with kidney disease.1–4 Evaluating and strengthening fellowship training and its appeal to students are keys to preparing future nephrologists to face these challenges.
Few educational needs assessments of nephrology fellowships have been conducted, but the limited literature points to several areas in need of improvement.5–8 The most recent assessment, a survey of nephrologists generally in practice for <5 years, identified several areas in which participants felt less than well prepared, including peritoneal dialysis (PD) and home hemodialysis (HHD) modalities; performing and interpreting renal ultrasounds; end of life care; and the care of patients with pediatric kidney diseases.6 Nephrologists felt well trained in other core areas, including in-center hemodialysis, glomerular disease, hypertension, and general CKD management.
A more recent survey of Australian and New Zealand nephrologists within 10 years of completing fellowship echoed these findings, noting persistent concerns regarding a lack of preparedness in PD, HHD, and conservative care.7 Notably, this survey showed no improvement in training between cohorts from 2003 to 2009 and 2010 to 2014. Both studies identified practice management and research training as additional areas for improvement.
Although informative, these studies describe perceptions of physicians who have already completed fellowship rather than current fellows. To date, studies of current fellows have focused on specific educational topics in nephrology, such as procedures or end of life care, rather than a global assessment.9–12 This study, an educational needs assessment performed in conjunction with the annual American Society of Nephrology (ASN) Nephrology Fellows Survey, sought to determine current fellows’ educational needs and evaluate their interest in potential educational interventions. The results can help inform training programs to better prepare nephrologists for independent careers and potentially attract more candidates to the specialty.
Methods
The educational needs assessment survey was created by the lead author (R.W.R.) with guidance from an educational researcher (S.B.M.) followed by an iterative review process with ASN Workforce Committee members, including the other coauthors. The final survey consisted of seven questions on the following topics: the overall quality of teaching in fellowship, educational modalities used in fellowship, educational topics requiring additional emphasis, and likelihood to participate in novel educational interventions. The complete survey is included in Supplemental Material.
The content assessed generally aligned with that from the 2010 survey by Berns6 as well as the Accreditation Council for Graduate Medical Education (ACGME) nephrology program guidelines and the ACGME/American Board of Internal Medicine Milestones Project.13,14 One qualitative question asked respondents to “[d]escribe two changes that could improve [their] fellowship’s educational environment.” The survey was piloted with nephrology faculty within the lead author’s institution, and cognitive interviews were performed with medical students to evaluate the clarity of the survey. This survey development process generated confidence in the content validity of the survey.15
We distributed the survey by email in conjunction with the ASN Nephrology Fellows Survey at the end of the academic year (May and June of 2016) via the secure REDCap survey platform. Further details regarding distribution methods and strategies to increase response rates are presented in Supplemental Material. Contingency table (chi-squared) testing was used to evaluate differences in demographic characteristics between respondents and fellows nationally as well as differences in perceived preparedness for independent practice between respondents of different years. Responses for “not prepared” and “minimally prepared” were combined given reduced numbers. We analyzed the quantitative data using descriptive statistics for central tendency (mean and SD), overall counts and percentages, and frequency distributions. Analyses were conducted using GraphPad Prism software. Qualitative data were analyzed via an inductive thematic approach. The ASN Nephrology Fellows Survey was reviewed and exempted by George Washington University’s Institutional Review Board (IRB). The educational needs assessment survey questions were also exempted from review by Stanford University’s IRB.
Findings
Respondent Demographics
Overall, 377 of 1218 fellows to whom ASN offers complimentary membership completed the survey (31% response rate). Respondents in their first or second year of ACGME-accredited adult nephrology training were included in the analysis (320 fellows). Included respondents represented 37% (320 of 863) of ACGME-accredited fellows for the same academic year (2015–2016). Demographics are outlined in Table 1. With respect to age, sex, and race, respondents were similar to the overall cohort of fellows according to the most recent ACGME data. However, there were statistically significant differences between respondents and the ACGME cohort in the location of medical school of record (United States versus international medical schools) and medical degree (Doctor of Medicine versus Doctor of Osteopathic Medicine).
Table 1.
Demographics of educational survey respondents and recipients
| Demographic | Respondents | ACGME Fellows (AY 2015)a |
|---|---|---|
| Total | ||
| N | 320 | 863 |
| Sex, % (differences between respondents and ACGME fellows were not statistically significant [P=0.43]) | ||
| Women | 34 | 36 |
| Men | 66 | 63 |
| Age, yr | ||
| Mean (PGY-4) | 32.9 | 33.7 |
| Median | 32 | — |
| Range | 28–62 | — |
| Race/ethnicity, % (differences between respondents and ACGME fellows were not statistically significant [P=0.21])b | ||
| Asian/Pacific Islander | 36 | 41 |
| Black | 7 | 7 |
| White | 32 | 23 |
| Other | 14 | 12 |
| Hispanic/Latino | 9 | 8 |
| Unknown | — | 10 |
| Medical education, % (MD/DO and USMG/IMG comparisons between respondents and ACGME fellows were borderline statistically significant [P=0.05] and statistically significant [P=0.03], respectively) | ||
| Allopathic (MD) | 89 | 92 |
| Osteopathic (DO) | 11 | 8 |
| USMG | 40 | 34 |
| IMG | 60 | 65 |
| Fellowship year (%) | ||
| First year | 122 (38) | 434 (50.2) |
| Second year | 155 (48) | 429 (49.7) |
| No response | 43 (13) | — |
Percentages may not total 100% due to rounding. P values for comparison are from chi-squared tests for independence; α=0.05. AY, academic year; PGY-4, post-graduate year 4; —, not applicable; MD, Doctor of Medicine; DO, Doctor of Osteopathic Medicine; USMG, United States medical graduate; IMG, international medical graduate.
ACGME data for first- and second-year fellows AY 2015–2016.46
Comparison for differences between white, black, Asian/Pacific Islander, and other. Differing data collection methods between ASN/George Washington University and ACGME obviate the ability to determine unknown responses or perform further comparisons.
Quality and Educational Makeup of Fellowship Teaching
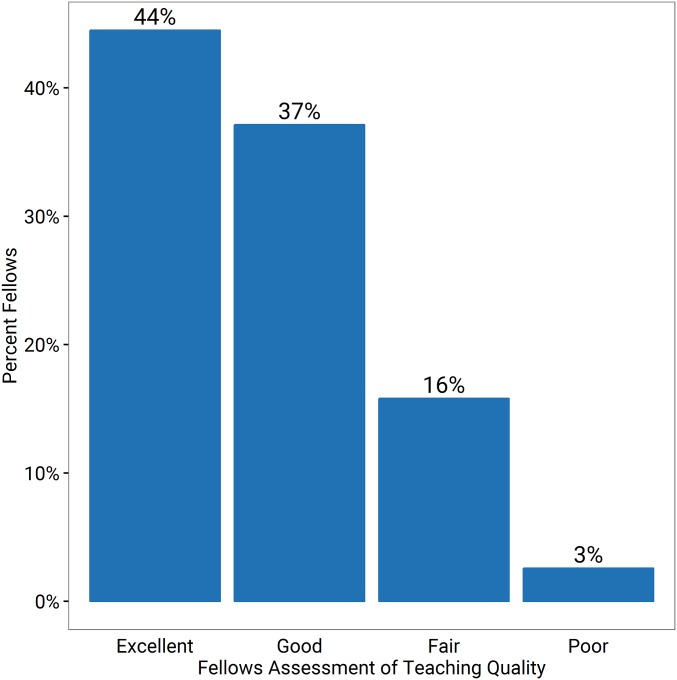
Most respondents described the overall quality of fellowship teaching as either “good” (37%) or “excellent” (44%) (Figure 1). Similarly, almost one half of second-year respondents (42%) felt “moderately prepared” for independent practice, and more than one half (55%) felt “fully prepared” (Figure 2). Second-year fellows felt more prepared than first-year fellows (P<0.01; chi-squared test for independence).
Figure 1.
Fellows have positive perceptions of the overall quality of their training. Bars indicate the percentages of respondents for each assessment class.
Figure 2.
A majority of second-year fellows report moderate or full preparedness for independent practice.
Although the prior 2010 Berns6 survey did not assess overall preparation for independent practice, the percentage of respondents indicating that they were well trained and competent ranged from approximately 80% for in-center hemodialysis and transplant care to 15% for HHD care. Further characterizations of nephrology fellows’ overall preparation for independent practice are not present in the literature. In contrast, a 2001 survey of graduating internal medicine residents found that, although 91% felt very prepared to care for inpatients independently, only 48% felt very prepared for the ambulatory setting.16
Importantly, anchor effect bias within a Likert scale may increase the selection of moderate choices rather than extremes and underestimate the number of fully prepared fellows.17 However, although this subjective measure of preparedness for a future and as yet unknown job is flawed, it is likely that this preparedness gap is at least partially generated by educational deficiencies in fellowship. Educational innovations designed to improve global performance will likely reduce this gap.
Educational Modalities and Resources
Participants were asked to identify educational modalities and resources used in fellowship. Table 2 details educational modalities that respondents indicated were used in their fellowships. Traditional modalities (e.g., journal clubs, lectures, and grand rounds) predominated, with between 72% and 90% of respondents reporting their use. Other modalities, including protected time for physiology and clinical nephrology review, reading lists, simulation training for catheters or biopsies, communications training, and ultrasound training, were reported by <50% of respondents.
Table 2.
Educational modalities in current use (269 fellows responded)
| Which of the Following Are Used in Your Fellowship Curriculum? (Select All That Apply) | N (%) |
|---|---|
| Journal clubs—led by fellows | 243 (90) |
| Curriculum lectures—led by attendings | 240 (89) |
| Renal pathology conferences | 239 (88) |
| Grand rounds—presented by attendings | 193 (72) |
| Grand rounds—presented by fellows | 171 (64) |
| Curriculum lectures—led by fellows | 159 (59) |
| Fellow-led case reports | 142 (53) |
| Journal clubs—led by attendings | 135 (50) |
| Key articles or reading lists/collections | 121 (45) |
| Temporary dialysis catheter simulation training | 111 (41) |
| Morbidity and mortality conferences | 111 (41) |
| Kidney biopsy simulation training | 80 (30) |
| Uninterrupted protected time for renal physiology, pathophysiology, and/or clinical nephrology review (separate from core curriculum lectures) | 73 (27) |
| Communications training for end of life care and dialysis decision making | 69 (26) |
| Online audio/video recordings of presentations (e.g., grand rounds, lectures) | 68 (25) |
| Interventional nephrology training | 44 (16) |
| Formal ultrasound training | 32 (12) |
| Online collaborative learning forum where fellows can post questions, cases, resources, and presentations | 24 (9) |
These results suggest that the general educational structure, as perceived by fellows, is reasonably similar among programs given the prevalence of traditional educational modalities, such as curriculum lectures, journal clubs, and grand rounds. A recent survey of nephrology training program directors also indicated that these modalities are nearly universal.18 In this survey, simulation training was perceived as less prevalent than expected given the ACGME mandate to include simulation in curricula.13 Although respondents may not have understood the variety of simulation training that may be included in their fellowship and although the survey did not include all potential simulation curricula, this discrepancy raises concern. Fellows’ receptiveness to additional simulation training seemed mixed. Respondents reported that they were less likely to participate in simulation training for catheter placement, biopsies, or communication skills compared with other strategies. In contrast, the desire for biopsy and ultrasound training was emphasized in answers to a free response question about educational improvements (discussed below). Notably, there is at least preliminary evidence to support the use of simulation in nephrology education.11,19–22
Fellows were also asked to report extracurricular resources used within the last 3 months (Table 3). UpToDate was nearly universally used, with the Clinical Journal of the American Society of Nephrology, the Journal of the American Society of Nephrology, and the ASN Nephrology Self-Assessment Program used by a majority of respondents.23 However, several expert-led and potentially effective educational resources, such as the American Journal of Kidney Disease (AJKD) Kidney Core Curriculum, the Renal Fellow Network blog, Nephrology Journal Club, the AJKD blog, and the ASN online curricula, seem less utilized.24–28 These resources deliver content on topics requested by respondents in this survey, such as home dialysis modalities and GN, and their heightened focus on social media formats may prove useful for digital learners. Formal evaluation of their usefulness and dissemination of the content through effective avenues would be valuable for fellows and their programs.
Table 3.
Educational tools in current use (271 fellows responded)
| Which of the Following Educational Tools Have You Used in the Last 3 mo? | N (%) |
|---|---|
| UpToDate | 261 (96) |
| CJASN articles | 181 (67) |
| ASN NephSAP | 171 (63) |
| JASN articles | 160 (59) |
| Textbooks | 156 (58) |
| KDIGO/KDOQI clinical practice guidelines | 128 (47) |
| AJKD articles | 126 (47) |
| Journal articles in general | 113 (42) |
| Renal fellow network blog | 93 (34) |
| ASN KSAP | 74 (27) |
| AJKD kidney core curriculum | 30 (11) |
| NephJC (Twitter-based journal club) | 19 (7) |
| AJKD Blog | 18 (7) |
| ASN online dialysis curriculum | 7 (3) |
| ASN online geriatrics curriculum | 4 (2) |
CJASN, Clinical Journal of the American Society of Nephrology; NephSAP, Nephrology Self-Assessment Program; JASN, Journal of the American Society of Nephrology; KDIGO, Kidney Disease Improving Global Outcomes; KDOQI, Kidney Disease Outcomes Quality Initiative; KSAP, Kidney Self-Assessment Program; NephJC, Nephrology Journal Club.
Educational Content Needs and Suggestions for Improving the Educational Environment
Participants were asked to identify topics that they would like additional instruction in during fellowship (Table 4). Top desired topics (>30% responding) included home dialysis modalities (PD and HHD), radiology and pathology interpretation, obstetric nephrology, GN, and toxicology, suggesting an educational need in these areas; 10% or fewer of fellows desired further instruction in topics, such as AKI management, outpatient CKD management, or diabetic nephropathy.
Table 4.
Additional instruction during fellowship (266 fellows responded)
| Which Topics Would You Most Like to Receive Additional Instruction in during Fellowship? | N (%) |
|---|---|
| HHD | 136 (51) |
| PD | 119 (45) |
| Kidney ultrasound interpretation | 118 (44) |
| Acute GN diagnosis/management | 101 (38) |
| Obstetric nephrology | 95 (36) |
| Toxicology | 89 (33) |
| Renal pathology interpretation | 85 (32) |
| Nephrolithiasis | 69 (26) |
| Hemodialysis | 67 (25) |
| Care of adults with pediatric renal disease | 62 (23) |
| Renal pharmacology | 61 (23) |
| Genetic renal diseases | 59 (22) |
| Conservative/palliative management of ESRD | 53 (20) |
| Electrolyte disorders/acid-base disorders | 53 (20) |
| Secondary hypertension diagnosis/management | 52 (19) |
| Nutrition | 45 (17) |
| Kidney biopsy | 44 (16) |
| Temporary dialysis catheter placement | 42 (16) |
| Mineral and bone disease management | 40 (15) |
| Nephrotic syndrome | 32 (12) |
| Urinalysis | 31 (12) |
| Post-transplant outpatient management | 30 (11) |
| Geriatric nephrology | 28 (11) |
| Inpatient general AKI diagnosis/management | 26 (10) |
| Post-transplant acute inpatient management | 25 (9) |
| Outpatient CKD diagnosis/management | 24 (9) |
| Diabetic nephropathy | 18 (7) |
| Anemia of renal disease management | 14 (5) |
| Others specified by respondents: interventional nephrology, renal physiology | N/A |
N/A, not applicable.
A total of 100 of 320 participants (31%) responded to the open-ended question: “Describe two changes that could improve your fellowship’s educational environment.” Responses centered on two themes: (1) structural changes and (2) desires for specific educational content. Structural changes included requests for more protected time to study independently, lectures and presentations sheltered from the competing interests of clinical care (e.g., “[a]llow ‘pager free’ time so that focus can be given to lectures”), and more faculty involvement in curricular development and implementation. Suggestions for educational content centered largely on increasing emphasis in four content areas: procedures (e.g., “[p]rovide protected time for simulations programs, i.e., reading [ultrasounds] dialysis catheter placement”), home dialysis modalities, ultrasound and other renal imaging, and renal pathology and physiology. Further representative quotes are listed in Table 5.
Table 5.
Changes to educational environment suggested by fellows
| Theme | Sample Quotations |
|---|---|
| Structural changes desired | “Protected teaching time not interrupted by pages” |
| “Allow ‘pager free’ time so that focus can be given to lectures” | |
| “More core lecture series and board question–based conferences” | |
| “More time emphasized on education over service” | |
| “Reduce patient load/clinical responsibilities … [to] provide more dedicated time for study” | |
| “More attending involvement in planning a cohesive curriculum” | |
| “Structured curriculum with readings in textbook and/or key articles to go with lectures/cases” | |
| “Providing fellows with their own panel of patients rather than those designated to an attending” | |
| Educational content desired | “Introductory lectures during the first 3 months on basic nephrology topics” |
| “[Establish] specific … electives in second year for either US or IR” | |
| “Provide protected time for simulations programs, i.e., reading US, dialysis catheter placement” | |
| “More opportunity to do kidney [biopsies] and [for] training in performing ultrasound” | |
| “Dedicated renal physiology lectures and training” | |
| “More stress on home dialysis therapies/outpatient therapies and less in-hospital training |
Qualitative responses were reviewed by the first author (R.W.R.), who selected 14 representative quotes from 13 respondents. US, Ultrasound; IR, interventional radiology.
The content areas identified by fellows for additional educational emphasis align with those topics previously identified in the Berns6 2010 survey of recently graduated nephrologists.
The need for additional training in home dialysis modalities is especially notable given the desire to expand these patient-centered and potentially less expensive options. Without strengthening fellowship training in these key therapeutic options, the full adoption of these modalities across the specialty will be difficult.
Future Educational Innovations
Lastly, fellows were surveyed on how likely they were to participate in educational interventions reflective of the nephrology educational literature and traditional educational modalities (Table 6). Respondents viewed all potential interventions at least neutrally in aggregate. However, fellows were more likely to participate in renal pathology conferences and “dedicated time for renal physiology, pathophysiology, and/or clinical nephrology review.”
Table 6.
Educational strategies (234 fellows responded)
| How Likely Are You to Participate in the Following Educational Strategies as a Fellow? (1–5 Likert Scale, with 1 Indicating Very Unlikely, 3 Indicating Neither Unlikely nor Likely, and 5 Indicating Very Likely) | Mean (SD) Likelihood of Participation |
|---|---|
| Renal pathology conferences | 4.30 (0.86) |
| Dedicated time for renal physiology, pathophysiology, and/or clinical nephrology review | 4.03 (1.03) |
| Training in performing ultrasound | 3.75 (1.26) |
| Fellow-led in-person case-based pathophysiology/management discussions (“morning report style”) | 3.73 (1.16) |
| Formal teaching opportunities (e.g., medical school, IM residency lectures) | 3.67 (1.14) |
| Formalized “pre-tending” as a fellow (acting as an attending during consultation rotations with minimized formal attending supervision) | 3.65 (1.22) |
| Key article reading list with fellow-authored article summaries | 3.64 (1.17) |
| Computer simulation exercises of HD/PD cases where you can alter prescriptions and follow results | 3.62 (1.27) |
| Watching online recordings of lectures, grand rounds, or journal clubs | 3.50 (1.27) |
| Simulated renal biopsy training | 3.50 (1.28) |
| Communications training for end of life care and dialysis decision making | 3.49 (1.20) |
| Conferences between local fellowships (e.g., in New England) targeted at fellows | 3.45 (1.27) |
| Simulated catheter placement training | 3.44 (1.29) |
| Fellow-led online case-based pathophysiology/management discussions where fellows share and contribute to cases on a regular basis | 3.41 (1.24) |
| Interventional nephrology training | 3.41 (1.33) |
| Case-based debates between specialties (e.g., rheumatology and nephrology fellows) | 3.39 (1.26) |
| Problem sets (“homework”) on various topics | 3.37 (1.16) |
| Formal education in “how to teach” | 3.34 (1.26) |
IM, internal medicine; HD, hemodialysis.
Although interest in simulation within this survey seems mixed, the ability of simulation curricula to increase fellows’ procedural competence should continue to be explored. A lack of procedural confidence and opportunities in fellowship, beyond representing a potential educational challenge, may be a deterrent to recruiting fellows who enjoy working with their hands or are concerned about limited revenue potential in nephrology.29
The use of novel educational tools in nephrology has vastly expanded in the last two decades.30–33 Although recent literature has emphasized the potential for educational innovations to improve nephrology training, consistent outcome data are lacking.34–37 These methods, including but not limited to social media (e.g., blogs, Twitter, and physician networks), connectivity aids (e.g., audience response systems and lecture capture), video production, clinical debates, and medical gaming, provide opportunities to create interactive and captivating education placed within a clinically relevant context at all trainee levels. Importantly, although nephrology has taken a strong place in the nascent development of social media educational tools, our understanding of their efficacy remains limited.38 Assessing and expanding innovation in nephrology education may not only improve education of trainees but also, given the connection between education and interest in nephrology, help address the growing disinterest in our field.29,39,40
Parallel with these developing educational tools, the ASN has also sponsored recent workforce activities, including (1) the Kidney Tutored Research and Education for Kidney Students Program, which provides medical students core physiology education as well as ongoing mentorship and scholarship experiences that seem to increase interest in nephrology as a career choice; (2) the Mentoring and Awareness Program for Students, a community CKD screening program; and (3) the Kidney Students and Residents Program, which provides travel grants to medical students and residents to attend ASN Kidney Week.41–44 Moving forward, the longitudinal assessment of participants in these programs is a priority for the ASN leadership.
Limitations of the Survey
This study has several limitations, most notably the limited response rate. Multiple approaches to improving participation were used and are discussed in Supplemental Material. Although the response rate may limit the generalizability of the results, this survey represents, to the best of the authors’ knowledge, the largest sampling of nephrology fellows within an educational study to date. Furthermore, respondents were representative of the ACGME fellows cohort in terms of age, sex, and race. The limited response rate may also have contributed to the variance in responses regarding future educational modalities, limiting our ability to discriminate between interventions. Unfortunately, increasing follow-up outreach beyond what was performed has not been associated with improved response rates, and direct financial incentives, which are effective, were unavailable (aside from a chance at winning complimentary ASN membership or Board Review Course and Update registration).45 Future studies may benefit from these incentives as well as consideration of inclusion within the national fellow in-training examination to improve response rates.
It also must be recognized that surveys may accentuate the concerns of a minority of vocal respondents, further limiting generalizability. As discussed earlier, fellows in training inherently lack the perspective that comes from independent practice, which may partially explain the reduced interest in some topics (e.g., end of life care/geriatric nephrology, nutrition, and outpatient CKD management). However, in limiting this survey to current fellows rather than practicing nephrologists, we could better assess what educational interventions are more likely to be supported by fellows. Future studies should endeavor to capture a greater totality of current fellows’ experience and further incorporate the evolving educational tools that we are developing.
Conclusion
As the specialty of nephrology addresses what it means to be a “nephrologist” and what future trainees will require for professional success, the ongoing evolution of training standards, competencies, and educational modalities will be critically important.4 This study represents the most current general educational needs assessment of United States nephrology fellows. It outlines areas for additional curricular emphasis, including home dialysis modalities, as well as the potential utility of emerging educational innovations in fellowship. Over time, continued improvements in fellowship curricula may not only improve the education of current trainees but also, help ensure the future of the specialty as well.
Disclosures
R.W.R. is an ongoing contributor to the Renal Fellow Network blog without financial interest. K.A.P. is an employee of the American Society of Nephrology. The remaining authors have no competing interests.
Supplementary Material
Acknowledgments
The authors thank the members of the American Society of Nephrology Workforce Committee as well as investigators from the George Washington University Health Workforce Institute research team (led by Edward Salsberg and Leah Masselink) for their assistance in developing and implementing this project. In addition, we thank the members of Stanford’s Rathmann Medical Education Fellowship team for their guidance and support.
Footnotes
Published online ahead of print. Publication date available at www.jasn.org.
This article contains supplemental material online at http://jasn.asnjournals.org/lookup/suppl/doi:10.1681/ASN.2016101061/-/DCSupplemental.
References
- 1.Murphy D, McCulloch CE, Lin F, Banerjee T, Bragg-Gresham JL, Eberhardt MS, Morgenstern H, Pavkov ME, Saran R, Powe NR, Hsu C-Y; Centers for Disease Control and Prevention Chronic Kidney Disease Surveillance Team : Trends in prevalence of chronic kidney disease in the United States. Ann Intern Med 165: 473–481, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.United States Renal Data System : 2015 USRDS Annual Data Report: Epidemiology of Kidney Disease in the United States, Bethesda, MD, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, 2015 [Google Scholar]
- 3.Parker MG, Pivert KA, Ibrahim T, Molitoris BA: Recruiting the next generation of nephrologists. Adv Chronic Kidney Dis 20: 326–335, 2013 [DOI] [PubMed] [Google Scholar]
- 4.Berns JS, Ellison DH, Linas SL, Rosner MH: Training the next generation’s nephrology workforce. Clin J Am Soc Nephrol 9: 1639–1644, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kimmel PL, Bosch JP: Effectiveness of renal fellowship training for subsequent clinical practice. Am J Kidney Dis 18: 249–256, 1991 [DOI] [PubMed] [Google Scholar]
- 6.Berns JS: A survey-based evaluation of self-perceived competency after nephrology fellowship training. Clin J Am Soc Nephrol 5: 490–496, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Beaton TJ, Krishnasamy R, Toussaint ND, Phoon RK, Gray NA: Nephrology training in Australia and New Zealand: A survey of outcomes and adequacy. Nephrology (Carlton) 22: 35–42, 2017 [DOI] [PubMed] [Google Scholar]
- 8.Mehrotra R, Blake P, Berman N, Nolph KD: An analysis of dialysis training in the United States and Canada. Am J Kidney Dis 40: 152–160, 2002 [DOI] [PubMed] [Google Scholar]
- 9.Combs SA, Culp S, Matlock DD, Kutner JS, Holley JL, Moss AH: Update on end-of-life care training during nephrology fellowship: A cross-sectional national survey of fellows. Am J Kidney Dis 65: 233–239, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Berns JS, O’Neill WC: Performance of procedures by nephrologists and nephrology fellows at U.S. nephrology training programs. Clin J Am Soc Nephrol 3: 941–947, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Clark E, Barsuk JH, Karpinski J, McQuillan R: Achieving procedural competence during nephrology fellowship training: Current requirements and educational research. Clin J Am Soc Nephrol 11: 2244–2249, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sachdeva M, Ross DW, Shah HH: Renal ultrasound, dialysis catheter placement, and kidney biopsy experience of US nephrology fellows. Am J Kidney Dis 68: 187–192, 2016 [DOI] [PubMed] [Google Scholar]
- 13.Accreditation Council for Graduate Medical Education: ACGME Program Requirements for Graduate Medical Education in Nephrology, 2016. Available at: http://www.acgme.org/Portals/0/PFAssets/ProgramRequirements/148_nephrology_int_med_2016.pdf. Accessed October 4, 2016
- 14.Accreditation Council for Graduate Medical Education and American Board of Internal Medicine: The Internal Medicine Subspecialty Milestones Project, 2016. Available at: http://www.acgme.org/Portals/0/PDFs/Milestones/InternalMedicineSubspecialtyMilestones.pdf. Accessed October 4, 2016
- 15.Beckman TJ, Cook DA, Mandrekar JN: What is the validity evidence for assessments of clinical teaching? J Gen Intern Med 20: 1159–1164, 2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Blumenthal D, Gokhale M, Campbell EG, Weissman JS: Preparedness for clinical practice: Reports of graduating residents at academic health centers. JAMA 286: 1027–1034, 2001 [DOI] [PubMed] [Google Scholar]
- 17.Bishop PA, Herron RL: Use and misuse of the likert item responses and other ordinal measures. Int J Exerc Sci 8: 297–302, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Liebman SE, Moore CA, Monk RD, Rizvi MS: What are we doing? A survey of United States nephrology fellowship program directors [published online ahead of print December 5, 2016]. Clin J Am Soc Nephrol doi: 10.2215/CJN.06530616 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Noble VE, Murray AF, Capp R, Sylvia-Reardon MH, Steele DJ, Liteplo A: Ultrasound assessment for extravascular lung water in patients undergoing hemodialysis. Time course for resolution. Chest 135: 1433–1439, 2009 [DOI] [PubMed] [Google Scholar]
- 20.Oliver SW, Patel RK, Ali KA, Geddes CC, MacKinnon B: Teaching percutaneous renal biopsy using unfixed human cadavers. BMC Nephrol 16: 209, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Schell JO, Green JA, Tulsky JA, Arnold RM: Communication skills training for dialysis decision-making and end-of-life care in nephrology. Clin J Am Soc Nephrol 8: 675–680, 2013 [DOI] [PubMed] [Google Scholar]
- 22.Prince LK, Abbott KC, Green F, Little D, Nee R, Oliver JD 3rd, Bohen EM, Yuan CM: Expanding the role of objectively structured clinical examinations in nephrology training. Am J Kidney Dis 63: 906–912, 2014 [DOI] [PubMed] [Google Scholar]
- 23.American Society of Nephrology: ASN NephSAP. Available at: http://www.asn-online.org/education/nephsap. Accessed October 4, 2016
- 24.American Journal of Kidney Disease: Core Curriculum in Nephrology, 2016. Available at: http://www.ajkd.org/content/corecurriculum. Accessed October 4, 2016
- 25.Renal Fellow Network: Renal Fellow Network Blog. Available at: http://renalfellow.blogspot.com. Accessed October 4, 2016
- 26.NephJC: Nephrology Journal Club. Available at: http://www.nephjc.com. Accessed October 4, 2016
- 27.American Journal of Kidney Disease: Blog AJKD. Available at: https://ajkdblog.org. Accessed October 4, 2016
- 28.American Society of Nephrology: ASN Online Curricula. Available at: http://www.asn-online.org/education/distancelearning/curricula. Accessed October 4, 2016
- 29.Jhaveri KD, Sparks MA, Shah HH, Khan S, Chawla A, Desai T, Iglesia E, Ferris M, Parker MG, Kohan DE: Why not nephrology? A survey of US internal medicine subspecialty fellows. Am J Kidney Dis 61: 540–546, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bayefsky SD, Shah HH, Jhaveri KD: Nephrology education for medical students: A narrative review. Ren Fail 38: 1151–1159, 2016 [DOI] [PubMed] [Google Scholar]
- 31.Jhaveri KD, Sparks MA, Shah HH: Novel educational approaches to enhance learning and interest in nephrology. Adv Chronic Kidney Dis 20: 336–346, 2013 [DOI] [PubMed] [Google Scholar]
- 32.Roberts JK, Sparks MA, Lehrich RW: Medical student attitudes toward kidney physiology and nephrology: A qualitative study. Ren Fail 38: 1683–1693, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Woods M, Rosenberg ME: Educational tools: Thinking outside the box. Clin J Am Soc Nephrol 11: 518–526, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yuan CM, Prince LK, Zwettler AJ, Nee R, Oliver JD 3rd, Abbott KC: Assessing achievement in nephrology training: Using clinic chart audits to quantitatively screen competency. Am J Kidney Dis 64: 737–743, 2014 [DOI] [PubMed] [Google Scholar]
- 35.Desai T, Stankeyeva D, Chapman A, Bailey J: Nephrology fellows show consistent use of, and improved knowledge from, a nephrologist-programmed teaching instrument. J Nephrol 24: 345–350, 2011 [DOI] [PubMed] [Google Scholar]
- 36.Topf JM, Hiremath S: Social media, medicine and the modern journal club. Int Rev Psychiatry 27: 147–154, 2015 [DOI] [PubMed] [Google Scholar]
- 37.Shah HH, Mattana J, Jhaveri KD: Evidence-based nephrology-rheumatology debates: A novel educational experience during nephrology fellowship training. Ren Fail 35: 911–913, 2013 [DOI] [PubMed] [Google Scholar]
- 38.Hamm MP, Chisholm A, Shulhan J, Milne A, Scott SD, Klassen TP, Hartling L: Social media use by health care professionals and trainees: A scoping review. Acad Med 88: 1376–1383, 2013 [DOI] [PubMed] [Google Scholar]
- 39.Pivert KA: Nephrology Match AY 2017–Preliminary Results: Data Brief. Available at: https://www.asn-online.org/education/training/workforce/ASN_Data_Brief_Nephrology_Match_AY_2017_Preliminary_Results.pdf. Accessed January 31, 2017
- 40.Shah HH, Jhaveri KD, Sparks MA, Mattana J: Career choice selection and satisfaction among US adult nephrology fellows. Clin J Am Soc Nephrol 7: 1513–1520, 2012 [DOI] [PubMed] [Google Scholar]
- 41.American Society of Nephrology: Medical Students: Kidney TREKS. Available at: http://www.asn-online.org/education/training/students/treks. Accessed January 31, 2017
- 42.Maursetter LJ, Stern LD, Sozio SM, Patel AB, Rao R, Shah HH, Leight K, Okusa MD, Zeidel ML, Parker MG: Enhancing nephrology career interest through the ASN kidney TREKS program. J Am Soc Nephrol 27: 1604–1607, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.American Society of Nephrology: Medical Students: Kidney MAPS. Available at: https://www.asn-online.org/education/training/students/maps. Accessed January 31, 2017
- 44.American Society of Nephrology: Kidney STARS (Students and Residents) Application. Available at: https://www.asn-online.org/grants/travel/details.aspx?app=MSR. Accessed January 31, 2017
- 45.Cho YI, Johnson TP, Vangeest JB: Enhancing surveys of health care professionals: A meta-analysis of techniques to improve response. Eval Health Prof 36: 382–407, 2013 [DOI] [PubMed] [Google Scholar]
- 46. ACGME: ACGME Data Resource Book: Academic Year 2015–2016, Chicago, Accreditation Council for Graduate Medical Education, 2016.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.