Abstract
Most American mothers who produce human milk (HM) now pump in place of some or all feeding at the breast, and most American infants are now fed pumped HM. We aimed to investigate mothers' perceptions of, attitudes toward, and practices for pumping and providing pumped HM. Results related to pumping are reported here. We conducted in‐depth, semi‐structured interviews among a diverse sample of 20 mothers who pumped, following each from pregnancy through infant HM‐feeding cessation up to 1 year postpartum. Data were analyzed using thematic analysis with Atlas.ti. Mothers' reasons for pumping changed over time and reflected their needs and desires (e.g., latch difficulty, return to work, and increasing their milk supply). Mothers reported that pump type and quality were important to pumping success and that pumping was time‐consuming, costly, and unpleasant compared to feeding at the breast. Regardless of how often mothers pumped, most felt pumping was necessary to meet their infant HM‐feeding goals and was a welcome means of sharing with other caregivers the bonding opportunity and tasks they associated with feeding infants. Mothers interpreted output from pumping sessions to understand their ability to provide enough milk to meet their infants' needs. Mothers' reasons for pumping may signal constraints to infant HM feeding that may be addressed with policy changes. Mothers' attitudes and perceptions toward pumping indicate that, although pumping fills important and welcome roles for many mothers, the reality of its practice may make it an unacceptable or infeasible substitute for some.
Keywords: breastfeeding confidence, breastfeeding support, ethnographic methods, human lactation, human milk, milk expression
1. INTRODUCTION
Women have been expressing human milk (HM) from their breasts for hundreds of years by hand or with the aid of devices. However, a new era has emerged: most U.S. mothers who produce HM now use breast pumps and provide pumped HM to their infants in place of some or all feeds at the breast (Geraghty, Davidson, Tabangin, & Morrow, 2012b). National recommendations and policies endorse and promote HM expression, or pumping (Eidelman et al., 2012; Patient Protection and Affordable Care Act of 2010; U.S. Department of Health and Human Services, 2011; U.S. Department of Health and Human Services, Health Resources and Services Administration, HRSA, Maternal and Child Health Bureau, 2008), but are informed only by literature that compares feeding at the breast to bottle‐feeding formula (Eidelman et al., 2012; Rasmussen & Geraghty, 2011) and generally treats the method of feeding HM as immaterial.
Research on pumping to date is limited (Felice & Rasmussen, 2015) but indicates that pumping is now common among mothers in the United States (Fein, Labiner‐Wolfe, et al., 2008a), the United Kingdom (Johnson, Leeming, Williamson, & Lyttle, 2013; Johnson, Williamson, Lyttle, & Leeming, 2009), and Australia (Clemons & Amir, 2010; Win, Binns, Zhao, Scott, & Oddy, 2006). A recent national longitudinal cohort study, the Infant Feeding Practices Study II (IFPS II), provides early data on why and how often U.S. mothers pumped at 2, 5, and 7 months postpartum (Fein, Labiner‐Wolfe, et al., 2008a). Most IFPS II mothers who fed HM also pumped, some often or exclusively (Labiner‐Wolfe, Fein, Shealy, & Wang, 2008). Qualitative data from the United Kingdom (Johnson et al., 2009, Johnson et al., 2013) and Australia (Clemons & Amir, 2010; Win et al., 2006) describe mothers' experiences pumping their milk and the meanings that they attach to pumping. Other recent data describe the impact of a workplace lactation support program on pumping practices (Geraghty, Sucharew & Rasmussen, 2012a) or compare pump output between pumping methods (Kent et al., 2008, Morton et al., 2009; Prime, Geddes, Hepworth, Trengove, & Hartmann, 2011). Thus, very little is known about how American mothers understand, feel about, or practice pumping across their first postpartum year (Geraghty & Rasmussen, 2010; Ortiz, McGilligan, & Kelly, 2004; Rasmussen & Geraghty, 2011).
Because employment outside the home hinders feeding at the breast (Kimbro, 2006; Rojjanasrirat & Sousa, 2010; Ryan, Zhou, & Arensberg, 2006; Thulier & Mercer, 2009), it is also an important predictor of mothers' use of pumping (Labiner‐Wolfe et al., 2008). The authors of a recent review (Johns, Forster, Amir, & McLachlan, 2013) found that pumping is only associated with a longer infant HM‐feeding duration for some mothers. For working IFPS II mothers, pumping was inferior to feeding infants at the breast in the workplace to maintain infant HM feeding (Fein, Labiner‐Wolfe, et al., 2008a). The difference between pumping and feeding at the breast for maintaining HM feeding may be wider nationally, as IFPS II mothers were older and had higher income than the national average and, thus, may have more support for pumping at work. Thus, it is essential to characterize how and how much mothers pump and store HM at home and at work, and factors that may impact these practices.
The gap in knowledge about the psychosocial determinants and consequences of pumping must be filled, as psychosocial factors may have an important role in mothers' success with pumping HM. Mothers often cite perceived low‐milk supply, pain, and body ownership as reasons they stopped feeding their infants at the breast (Flower, Willoughby, Cadigan, Perrin, & Randolph, 2008; Li, Fein, Chen, & Grummer‐Strawn, 2008). These attitudes and perceptions may occur with pumping and, thus, may relate to mothers' influences for stopping pumping. This could explain, in part, inconsistent findings regarding the links between pumping and longer infant HM‐feeding duration (Fein, Mandal, & Roe, 2008b; Geraghty, Sucharew, & Rasmussen, 2012a; Win et al., 2006). Moreover, substituting feeds at the breast with pumping may disrupt bonding or emotional benefits that are commonly cited as reasons for feeding HM (Sloan, Sneddon, Stewart, & Iwaniec, 2006).
We aimed to fill these gaps with a longitudinal series of in‐depth interviews. We report the results of this work related to pumping HM here, and results related to providing pumped HM elsewhere (Felice et al., 2016a). The distinction between these two contributions reflects an important consequence of the rise in these practices: that the provision of HM can no longer be considered an exclusively dyadic behavior (Figure 1; Felice & Rasmussen, 2015). While feeding an infant at the breast, HM is removed from the breast and provided to the infant simultaneously. In contrast, when HM is pumped and then bottle‐ or cup‐fed, the removal of HM from the breast and the provision of that HM to an infant are distinct practices that raise distinct questions. For example, the reliance of working mothers on pumping raises questions about how workplace factors may relate to their success in meeting their goals for providing their HM. The rise in pumped HM feeding raises questions about how different practices for storing, preparing, and feeding pumped HM relate to the safety of pumped HM as fed (Felice et al., 2016a). As a result, it is now essential to distinguish among practices for feeding at the breast, pumping, and feeding pumped HM (Figure 1; Felice & Rasmussen, 2015).
Figure 1.
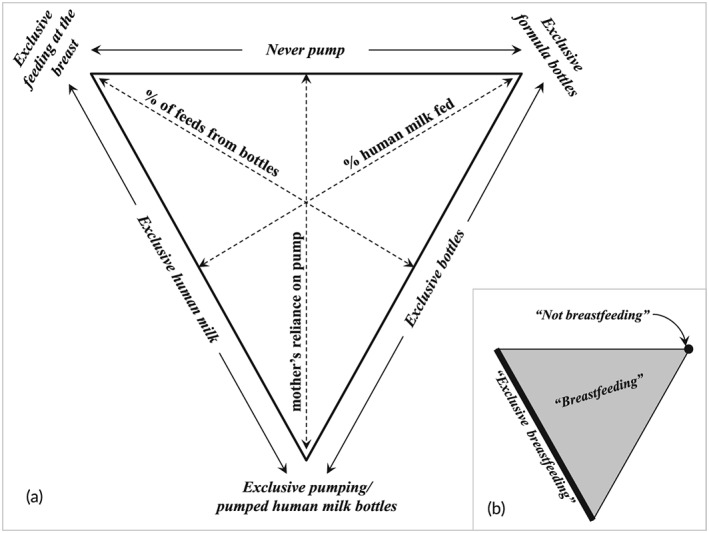
A new framework to characterize the current American mother–infant dyad. This figure illustrates the importance of distinguishing among feeding at the breast, pumping, and providing pumped HM (Felice & Rasmussen, 2015). (a) How mothers and infants currently may be categorized when nothing is fed aside from human milk and/or infant formula (i.e., before the introduction of solids or other milks) and without considering pumped milk that is mixed with solids or cases where infants are fed human milk that was not provided by their biological mother. (b) How current terminology fits within this triangular framework of current practices for producing and feeding human milk. This figure is reprinted with permission from Breastfeeding Medicine
Here, we describe results related to the mothers' perspective: their attitudes and perceptions of, strategies for, and experiences with pumping, including their motivations to pump, how they incorporated pumping into infant feeding practices and other obligations, and how their attitudes, perceptions, practices, and experiences changed over time. Results related to the infants' perspective—that is, the storage, preparation, and provision of pumped HM—are reported elsewhere (Felice et al., 2016a).
Key messages.
Pumping HM is now common among American mothers, particularly those who work outside the home, but little is known about how mothers pump at work and at home or their motivations for those practices.
Available evidence suggests that pumping may not be an equitable trade for feeding at the breast to maintain infant HM feeding in the long‐term.
This qualitative study uses a unique in‐depth longitudinal design to describe lactating mothers' practices for, experiences with, and perceptions of pumping their milk in a diverse sample.
2. METHOD
We used qualitative methods among women producing HM across three counties in upstate New York (n = 20). Specifically, we conducted longitudinal, in‐depth interviews and observations between September 2011 and November 2013 among a diverse sample to explore a range of attitudes toward, perceptions of, and practices for pumping.
2.1. Participants and recruitment
Women ≥21 years old experiencing healthy pregnancies with singleton infants were recruited from three counties in New York State. Participants were recruited in person and using cards and posters at OB‐GYN offices, Supplemental Program in Nutrition for Women, Infants, and Children (WIC) clinics, infant goods stores, and in public, and with emails sent to parenting email lists. Mothers were considered for inclusion if they intended to feed their HM to their infants and had heard about pumping; intention to pump was not an inclusion criterion. Mothers were purposively recruited for heterogeneity on factors associated with producing HM, such as marital, employment, and socioeconomic statuses, age, ethnicity, and parity. Participants gave written consent before the first interview, with separate consent for photo and video recording.
2.2. Data collection
The first interview was conducted late in mothers' pregnancies. The first postpartum interview occurred at 2 weeks postpartum to allow time for mothers to establish feeding at the breast while minimizing recall bias. Afterward, mothers were contacted every 2 to 3 weeks via email or text for the first 2 months and every 4 weeks thereafter to identify whether major shifts in their practices for providing HM had occurred, such as the start of pumping, feeding HM or formula from bottles, or feeding solids, or mothers' return to work. These regular contacts included a short list of yes‐or‐no questions about mothers' practices. If a major shift was indicated, interviews were scheduled and conducted as soon as possible. In general, we did not face problems scheduling timely interviews.
Interviews, which were between 45 min to 2.5 hr in length, were semi‐structured and open‐ended, and explored mothers' knowledge and perceptions of, attitudes toward, and intentions and practices for feeding at the breast‐ and bottle‐feeding pumped HM and formula. Multiple interview guides were created to reflect each anticipated transition. Each guide contained the relevant recurring themes in addition to questions specific to the recent transition. Interview guides were designed to reflect and document both the diversity of our sample and the incorporation of emerging themes. Namely, because we purposively recruited a sample with diverse home, work, and family contexts, interview guides included questions that were only posed to some mothers, and interview guides were sometimes combined or omitted. For example, the interview guides for the start of pumping and a mother's return to work were commonly combined, and mothers who did not work outside the home were not interviewed about a return to work. In addition, we incorporated questions about emerging themes into interview guides for subsequent data collection. These emerging themes are indicated in the results reported below and in the discussion.
2.3. Data analysis
Interviews were audio‐recorded, and recordings were transcribed and checked twice. Some predetermined themes were identified from the literature (Labiner‐Wolfe et al., 2008) to facilitate interpretation of our findings alongside available quantitative data. For example, questions on IFPS II surveys influenced the creation of themes related to mothers' motivations for pumping, their contexts and constraints for pumping at home and at work, and their experiences using different types of pumps. Predetermined and emerging themes were examined with a combination of inductive and deductive thematic analysis (Fereday & Muir‐Cochrane, 2006; Guest, MacQueen, & Namey, 2011) using open‐ and closed‐coding in Atlas.ti (Berlin, Germany). Coding was shared by four coauthors (JPF, CWQ, RY, and AJW) who trained together, peer‐checked codes, and met weekly to discuss findings. At each interview, JPF discussed with mothers her interpretations of their practices and influences from the previous interview and of the change that had necessitated the current interview. Mothers then corrected or affirmed these interpretations, which guided the rest of the interview. Quotes are presented with pseudonyms and infants' ages when the quote was collected. This work was approved by the Cornell University Institutional Review Board.
3. RESULTS
All study participants (Table 1) carried their pregnancies to term. In total, 108 interviews were conducted (range 2–7 interviews per participant): 102 in mothers' homes, three in workplaces at two mothers' invitations, and three in public for comfort or convenience (Figure 2). Except for one mother who left the study because of an unplanned out‐of‐state move, all mothers remained until 1 year postpartum (n = 12) or infant HM‐feeding cessation prior to 1 year (n = 7). All participants pumped at some point. Findings related to mothers' practices, attitudes, perceptions, and experiences related to the provision of their pumped milk to their infants are described elsewhere (Felice et al., 2016a).
Table 1.
Socio‐demographic characteristics of all ethnography participants
| Characteristic | Participants (n) |
|---|---|
| Age (mean, sd) | 29.8 (4.22) |
| Ethnicity | |
| American | 12 |
| African‐American | 4 |
| Hispanic | 2 |
| Asian | 2 |
| Marital status | |
| Married | 14 |
| Partnered, cohabitating | 4 |
| Single | 2 |
| Return to work | |
| None | 5 |
| ≤3 mo | 12 |
| 3–6 mo | 3 |
| Parity | |
| Primiparous | 8 |
| Multiparous | 12 |
| Prior experience feeding at the breast | |
| Yes | 10 |
| No | 10 |
| Prior experience pumping | |
| Yes | 8 |
| No | 12 |
| Prior experience feeding formula | |
| Yes | 11 |
| No | 9 |
| Prior experience bottle‐feeding HM | |
| Yes | 10 |
| No | 10 |
| Education | |
| ≤High school | 1 |
| Some college | 6 |
| College | 8 |
| >College | 5 |
Figure 2.
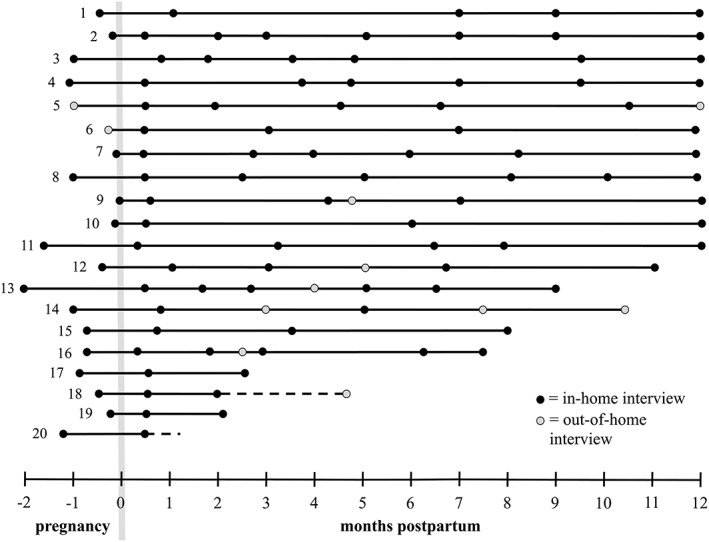
Frequency and distribution of semistructured interviews with study participants from pregnancy through up to 1 year postpartum. This figure shows the duration of participation (in months) and the distribution and frequency of interviews for each participant. Each line represents a participant, listed top to bottom roughly by duration of human milk–feeding. Each circle represents a participant interview. Dotted lines indicate that participants left the study and initiated contact afterward—one to report a new pregnancy and discuss her future intentions for pumping and one to report a sudden move that necessitated study exit
3.1. Types of pumps used
Mothers used all milk expression methods, including single manual, single electric, and double electric pumps, hospital‐grade pumps rented from hospitals or WIC, and hand expression (Table 2). Eleven mothers used multiple pumps: some replaced or supplemented defective or inefficient pumps, and some mothers bought second pumps to ease the transportation burdens of pumping both at work and at home. Frequently, nonhospital grade pumps—both electric and manual—were obtained second hand from family members, friends, acquaintances, garage sales, and unknown online sellers.
Table 2.
The type, number, and prior use of human milk expression methods and pumps used by ethnography participants
| PARTICIPANT | Method of expression | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Type of pump | Hand expression | |||||||||||||
| Double electric | Single electric | Manual | ||||||||||||
| Hospital‐grade | New | Rented | Used, known | Used, stranger | New | Rented | Used, known | Used, stranger | New | Rented | Used, known | Used, stranger | ||
| 1 | ♦ | ♦ | ♦ | ♦ | ||||||||||
| 2 | ♦ | ♦ | ♦ | |||||||||||
| 3 | ♦ | |||||||||||||
| 4 | ♦ | ♦ | ||||||||||||
| 5 | ♦ | |||||||||||||
| 6 | ♦ | |||||||||||||
| 7 | ♦ | ♦ | ||||||||||||
| 8 | ♦♦ | ♦ | ||||||||||||
| 9 | ♦ | ♦ | ♦ | |||||||||||
| 10 | ♦ | ♦ | ||||||||||||
| 11 | ♦ | ♦ | ||||||||||||
| 12 | ♦ | ♦ | ♦ | |||||||||||
| 13 | ♦ | ♦ | ||||||||||||
| 14 | ♦ | ♦♦ | ||||||||||||
| 15 | ♦ | ♦ | ||||||||||||
| 16 | ♦ | |||||||||||||
| 17 | ♦ | |||||||||||||
| 18 | ♦ | |||||||||||||
| 19 | ♦ | ♦ | ||||||||||||
| 20 | ♦ | ♦ | ♦ | |||||||||||
3.2. Mothers' motivations for pumping
3.2.1. Motivations for pumping
Mothers' motivations for pumping changed across their infants' first year (Figure 3). They reported some motivations throughout lactation, such as pumping to provide HM to be fed by another caregiver, but only reported other motivations in some stages of lactation. For example, mothers only reported pumping to establish their supply in the first postpartum month and only reported pumping so that pumped HM could be mixed with solids after solids had already been introduced.
Figure 3.
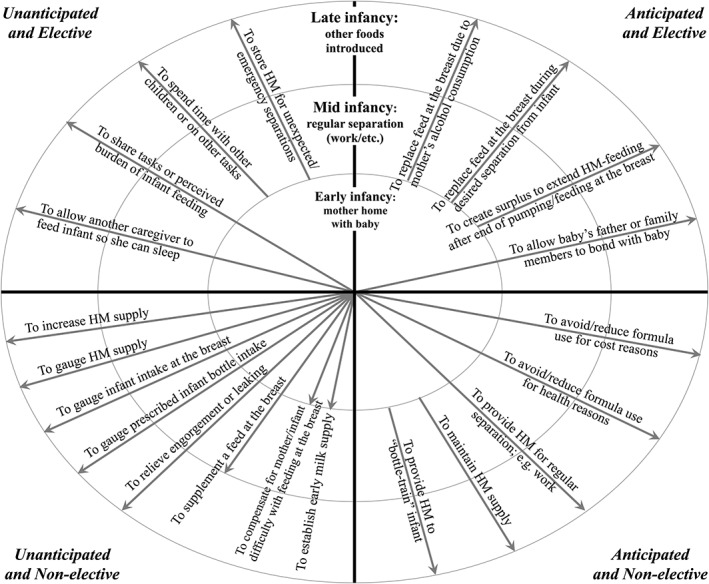
Characterizing mothers' reasons for pumping their human milk in three descriptive intervals across the first year by whether they were anticipated or unanticipated and elective or nonelective. Mothers' reasons for pumping could be were characterized by three factors: the infant's age at the time mothers pumped, whether mothers anticipated pumping for this reason or whether that reason for pumping was unanticipated, and whether mothers' reasons for pumping were elective or nonelective from mothers' perspectives. The three circles in this figure represent three dyadic stages chosen descriptively, as they occurred at different times between dyads. The first stage may be described as when mother and infant are mainly together, the second as when more regular separation occurs, and the third as when solids are also fed
On the basis of mothers' descriptions, we characterized their motivations for pumping as anticipated or unanticipated and as elective or nonelective (Figure 3). Although these binary characterizations cannot fully capture the complexity in mothers' reported motivations for pumping, they illustrate two important themes that emerged in mothers' descriptions: the roles of planning and choice in mothers' motivations for pumping. In general, a motivation was considered anticipated (vs. unanticipated) if mothers had predicted having to pump for that reason. For example, pumping to empty breasts before consuming alcohol was considered anticipated, while pumping as a result of infant latch failure was considered unanticipated. In general, an elective motivation for pumping was distinguished from a nonelective motivation by gauging whether mothers had a feasible alternative to pumping at that time (e.g., feeding at the breast or doing nothing). For example, pumping to provide milk for another family member to bond with the baby was characterized as elective, even if mothers described that bonding as important, because mothers were typically available and able to feed at the breast at the same time. However, inasmuch as all mothers who pump do so by choice, per se, mothers' needs, perceptions, and attitudes also guided the characterization of motivations as elective or nonelective. For example, for mothers who worked outside the home and wished to avoid feeding formula, pumping in the workplace was characterized as nonelective because no other choice allowed them to provide their milk.
The most commonly reported nonelective motivations for pumping changed across lactation. In their first postpartum month, mothers' nonelective reasons for pumping primarily related to difficulties with feeding their infants at the breast. After the first postpartum month, mothers most commonly reported nonelective motivations for pumping that related to their return to work outside the home or their preparations in advance of that return.
3.3. Mother's practices for pumping
In all stages of lactation, mothers with nonelective motivations pumped more often than mothers who had only elective motivations for pumping, and those with multiple nonelective motivations pumped most often. Although most mothers pumped at home at some point, those who worked outside the home primarily or always pumped at work. Many mothers reported that support and flexibility in their schedules and obligations at work were important to their success with pumping. Mothers pumped in a variety of locations and appreciated spaces that were private (such as private offices of their own or those of others, lactation rooms, and lockable common spaces) with which to pump HM and wash their supplies. Other mothers were visible to others although they pumped in shared offices, bathrooms, a lunchroom, and a supply storage room and reported feeling embarrassment or isolation from coworkers. For some, washing supplies in common sinks was a source of discomfort.
I run into some of the administrators in the bathroom sometimes. And I think people know that I'm pumping, like it's not a shameful thing, but it's also just a little bit embarrassing. … I just don't want people to see me, like washing it. I'm sure people know, I just don't want to make it so obvious. Probably just part of it is like my professional, you know, like I want people to see me in like a professional way, and I just feel like that's a little weird.
–Maureen, 4 months
In addition, mothers who pumped in bathrooms or washed supplies in common kitchen or bathroom sinks reported concerns about potential contamination of pump supplies. In response to both privacy and hygienic concerns, some mothers replaced washing sessions at work with the use of wipes or stored pump parts with ice packs between pumping sessions at work.
Mothers had a variety of strategies for transporting and storing their pumped HM. Mothers who pumped at work stored pumped HM in private refrigerators, common refrigerators or freezers, or personal coolers. Pumped HM was carried home in coolers to be refrigerated, combined with pumped HM from later pumping sessions, or frozen until it was fed there or transported further to other caregivers. Mothers froze and prepared pumped HM in various ways, but individual mothers typically did not change their practices over time. The amount of pumped HM stored in a bag ranged from about 2 to 8 ounces. Some mothers stored pumped HM in consistent amounts determined by their perceptions of their infants' meal size, the size of freezer bags, or easily divisible numbers. Others stored pumped HM in varying amounts, either determined by their pump output or to account for changing infant meal‐size needs within and across days.
When mothers pumped at home, they typically prioritized feeding their infants at the breast, and, as a result, used infants' hunger cues and sleep to determine the timing of pumping sessions relative to feeds at the breast. A few mothers pumped one breast while the infant fed on the other to facilitate their letdown and had difficulty managing or focusing on both tasks.
I mean the thing that kinda sucks about it, it's hard to do this like with the baby in one hand and work the pump. So [my husband] helps me a lot of the time. … But when it's just me, I kinda have to use the Boppy so that [my baby] can just lay here and I have a free hand to mess with the pump and stuff. And one time we were sitting here and [husband] was messing with [the pump] and I was trying to fix it on my breast … [my baby] like almost rolled off, and dad like caught him and it was, it was scary.
–Theresa, 2.5 months
Some working mothers regularly pumped at home to supplement HM they pumped at work so as to meet their infants' needs. Some mothers who had not returned to work pumped regularly at home to compensate for difficulty feeding at the breast, a perception that feeding at the breast was inadequate or that their supply was low, or a desire to store pumped HM for later feeding.
3.4. Mothers' attitudes toward and perceptions of pumping
Mothers held a wide variety of perceptions and attitudes toward pumping. Strikingly, most mothers believed that, because some separation of mother and infant was inevitable, exclusive HM feeding was impossible without some pumping. Consequently, mothers commonly valued the availability of pumps as a potential solution to a range of obstacles to feeding their infants at the breast. Many appreciated the opportunities offered by pumping but not by feeding at the breast, such as allowing them to share the bonding and burden of feeding infants without using formula, to create stocks of pumped HM for future feeding, or to take occasional time away from their infants.
But the pumping also makes you feel a lot more liberated. Like the breastfeeding, I love it, but you also do feel so tied down, you know? And like I could never go anywhere without her. I could never be gone more than an hour on the off chance that she cried. With pumping it does kind of give you that freedom of, you know, that you can do things and you can leave.
–Dora, 12 months
However, some mothers also reported simultaneous, negative attitudes related to pumping for unanticipated or nonelective reasons—for example, sadness or frustration in response to difficulty feeding at the breast or a need to return to work earlier than desired.
Ideally I would like it if the pump was just a backup, for those times I need some time alone away. I wish it wasn't one of the primary feeding methods. … But I'm okay with having it play a bigger role, especially because it's allowing me to have a career and everything.
– Dora, 3 months
Mothers' perceptions and attitudes toward the acts of pumping and its related tasks were widely negative. Many mothers reported that pumping felt like a tedious, time‐consuming, or inconvenient chore.
And I could not—like for me, I basically had to take time out, sit down, and hold the things in place. I couldn't do anything else. At least that's how I felt when I was doing it. It was just very inconvenient.
– Sarah, 2 months
In contrast, mothers commonly described the time spent feeding their infants at the breast as well spent and enjoyable bonding time. Mothers who continued or increased pumping despite negative attitudes about or constraints to pumping were those who believed that their obstacles to pumping were surmountable and that their infants' current nutritional needs were high. Some of these mothers replaced pumps with higher quality models if they thought new pumps would be helpful and affordable.
Mothers' attitudes and perceptions toward the act of pumping were strongly influenced by which pumps they used. Most thought infants were more efficient at emptying breasts than pumps. Some said even the best pumps were inferior to infants.
No. No. No. Uh uh. It's totally different. When she's, when, when I pump, it's like I'm not getting all the milk out. But when, when she, when I'm nursing her and she's on me, she's emptying them out. And, like, it feels so much better because they're not as heavy and they're not as, like, how can I… like [clogged] milk ducts, I don't have the [clogged] milk ducts over here under my armpit, like.
–Maya, 3 months
Most mothers described the importance of using the highest quality, double‐electric pump to produce enough HM in a reasonable amount of time.
I think part of [my low yield from pumping sessions] was because my pump was only a single‐boob‐at‐a‐time thing, and WIC just gave me a pump that I could do both breasts at a time. … definitely much more productive, like much quicker, and I could do both at the same time, and then just kind of get on with everything, which definitely was huge.
–Georgia, 3 months, rented hospital grade double‐electric pump
Mothers who used manual or single‐electric pumps reported delayed or weak letdown, inadequate suction and yield, and “wasted” HM leaking from the opposite breast. Many mothers felt high‐quality pumps were expensive, even prohibitively so, but some felt middle or lower quality pumps weren't worth buying at all. Thus, those who felt their pumps weren't of high enough quality either obtained a better pump or incorporated or increased formula to close the gap they perceived between their pump output and what their infants needed to eat.
Many mothers in this sample reported using data from pumping sessions—that is, the total yield of the pumping session as well as the rate of their milk flow—to guide their future practices for pumping and feeding HM. Most often, mothers interpreted pump output to represent their supply.
It is sort of a measure of my supply... It's sort of like a gauge. I know that that's not supposed to be super reliable, but that's kind of the main thing I have to go by.
–Maureen, 4 months
Some mothers also interpreted pump output to represent their infants' intake at the breast, or deliberately pumped to learn this amount.
When you're nursing and they're on your breast, you really don't know how much they're getting. But when you actually pump and you put it in the bottle you know exactly how many ounces they're getting.
–Maya, 1.5 weeks
Most mothers interpreted these data in some way to guide their future practices for pumping, bottle‐feeding, and feeding at the breast and to instruct other caregivers.
When I pump, it's usually around 3 ounces each time. ... I'm gonna have to tell daycare, if she is only drinking two ounces, she's probably still gonna be hungry. So go ahead and do another bag.
–Catherine, 7 weeks
In general, many mothers directly compared pump data to bottle data—for example, how many bottles their infants consumed with other caregivers and the size of those bottles—to infer their ability to meet their infants' needs with their pumping practices and whether they should pump more or feed formula.
Mothers' perceptions of the availability of HM compared to their infants' needs strongly influenced the end of their pumping practices. For many mothers, these perceptions were closely related to how they interpreted the data provided by pumping and bottle‐feeding HM, as described above. Mothers also compared the availability of HM to their infants' needs by considering the size of their stock of pumped HM, their infants' current need for HM (e.g., by their infants' age or health status), and their own attitudes toward HM compared to formula.
4. DISCUSSION
This longitudinal, qualitative investigation provides an in‐depth glimpse into how and why mothers pump HM. Mothers in our sample reported the importance of high‐pump quality for the success of pumping and, thus, infant HM feeding. Their reported attitudes toward and perceptions of pumping suggest that mothers who must rely on pumps more heavily to feed HM—for example, those who work outside the home or are unable or unwilling to feed their infants at the breast enough to meet their needs—may be less likely to meet recommendations for providing HM to their infants than mothers who can rely on pumps less frequently. These findings shed light on an emerging but inconsistent link between pumping practices and infant HM‐feeding outcomes (Fein, Mandal, & Roe, 2008b; Johns et al., 2013; Odom, Li, Scanlon, Perrine, & Grummer‐Strawn, 2013). Moreover, some of mothers' reported practices for pumping and storing HM raise concerns about whether pumping affects the benefits conferred to mothers and infants by feeding at the breast or introduces other risks.
In this qualitative sample, all mothers in this sample ended up pumping, whether or not they had intended to, and many viewed pumping as essential to meet their infant HM‐feeding goals because they felt some separation from their infant was inevitable. This finding is unsurprising in light of the fact that the United States is the only developed country that does not offer paid maternity leave (Heymann & McNeill, 2013) and that only 12% of the U.S. labor force has access to employer‐provided paid leave (U.S. Department of Labor, Bureau of Labor Statistics, 2013).
Our findings shed substantial light on current understanding of mothers' motivations for pumping, both related and unrelated to their employment. This progress in understanding is particularly important in light of our recent quantitative analysis of the IFPS II dataset (Felice, Cassano and Rasmussen, 2016b), in which we highlighted the importance of distinguishing and characterizing mothers' motivations for pumping to understand the impact of early pumping practices on long‐term feeding outcomes. Mothers in the qualitative sample described here reported motivations for pumping that reflected, clarified, and added to the list of motivations that have been reported by mothers in the United States (Labiner‐Wolfe et al., 2008), the United Kingdom (Johnson et al., 2009, 2013), and Australia (Clemons & Amir, 2010). For example, mothers in this sample and IFPS II mothers commonly pumped to produce HM for another caregiver to feed (Labiner‐Wolfe et al., 2008). In our qualitative sample, mothers described a wide range of motivations for having other caregivers feed pumped HM, and the HM that was fed by another caregiver had often been pumped for different, unrelated reasons. These findings suggest that, in future research into U.S. mothers' motivations for pumping, it is important to distinguish their reasons for pumping from the reasons that their infants are bottle‐fed HM. Further, mothers in the qualitative sample described here reported motivations for pumping that were not on the list of reasons available to IFPS II mothers but that may affect short‐ and long‐term infant‐feeding practices, such as pumping to establish their early milk supply or to create a surplus stock of pumped HM for long‐term feeding. In sum, our findings suggest that future epidemiologic investigations of U.S. mothers' reasons for pumping should include a list that is both more comprehensive and distinct from the reasons that infants are bottle‐fed HM.
Our characterizations of mothers' motivations as elective or nonelective and as anticipated or unanticipated also provide important insights into the drivers of the recent rise in pumping among U.S. mothers as well as potential ways to improve national practices for feeding HM. In the qualitative work reported here, the mothers who pumped most frequently described motivations for doing so that were primarily nonelective—that is, when feeding at the breast or not pumping were not available and/or feasible options. In our recent quantitative work (Felice, Cassano, & Rasmussen, 2016b), IFPS II mothers who pumped more frequently early in their first postpartum year had shorter durations of feeding exclusive HM, of feeding at the breast, and of feeding HM by any method. In addition, mothers who reported nonelective motivations for pumping fed their milk for shorter durations than those who only reported elective reasons; this association showed a dose–response relationship (Felice, Cassano, & Rasmussen, 2016b). Our qualitative findings also suggest the possibility that unanticipated pumping may relate to shorter feeding durations. For example, a mother who pumps for unanticipated motivations may not have enough time to plan and prepare accordingly—for example, by gathering funds, supplies, instructions, or support for pumping. However, no quantitative data are yet available to explore this possibility. Taken together, our quantitative (Felice, Cassano, & Rasmussen, 2016b) and qualitative findings raise the possibility that long‐term–feeding outcomes are not hindered by high‐frequency pumping, per se, but by high‐frequency pumping that results from constraints to or difficulty with feeding at the breast.
Some nonelective motivations for pumping—for example, those related to difficulty with or unavailability of feeding at the breast, concerns about milk supply and infant intake, or mothers' employment outside the home—may be addressed with changes to policies that may impact these practices. For example, our findings (Felice, Cassano, & Rasmussen, 2016b; Felice et al., 2016a) and those from the IFPS II (Baker & Milligan, 2008) suggest that mothers' reliance on pumping could be reduced by increasing mothers' access to help with feeding their infants at the breast, by providing federally mandated paid maternity leave and by offering working mothers onsite child care, more flexible work schedules, or the option to telework.
Some of mothers' practices for pumping, preparing pumped HM for storage, and cleaning pumping supplies also raise concerns about pathogenic contamination of pumped HM as fed. The common use of second‐hand pumps is of concern because commercial pumps' open systems are only safely designed for single users. Moreover, some mothers' practices of either rinsing or wiping pump flanges instead of washing them and mixing pumped HM from multiple‐pumping sessions before storage raise additional contamination concerns. These findings are troubling in light of recent data that show pathogenic contamination of pumped HM (Boo, Nordiah, Alfizah, Nor‐Rohaini, & Lim, 2001; Keim et al., 2013) and increased risk of coughing and wheezing among infants fed pumped HM versus those fed at the breast (Soto‐Ramirez et al., 2013). Mothers do not have comprehensive evidence‐based guidelines for safe, hygienic pumping and storing HM that address all of the practices they may use. To create these guidelines, data are needed on pathogenic contamination of pumps, pump flanges and tubes, storage containers, and pumped HM that may result from practices reported here.
Mothers in this sample provided insights into factors that may impact their success in pumping and, thus, feeding HM. Most prominently, mothers in this sample made clear the importance of their access to high‐quality pumps. Mothers' beliefs that the output from pumps varied widely by pump quality reflect experimental data showing that different pump types yield a wide range of pump output (Mitoulas et al., 2002; Kent et al., 2008; Morton et al., 2009). Further, these findings and quantitative analyses reported elsewhere (Felice, Cassano, & Rasmussen, 2016b) suggest that, in addition to a potential impact of pumping on mothers' perceptions of their milk supply, pumping may adversely impact mothers' actual HM supply. Specifically, HM production in response to feeding at the breast is a supply‐and‐demand system, wherein infants' sucking behavior and, thus, demand for HM stimulates the production of a corresponding supply of HM from breasts (Kent, 2007). Thus, reducing demand on breasts by substituting feeds at the breast for pumping sessions with manual or lower‐quality pumps may adversely impact a mother's milk supply in the long‐term. These results are important because they highlight the importance of making high‐quality pumps accessible to all mothers who wish to pump. The importance of pump quality is underscored by an important theme that emerged in this work: mothers' interpretation of the output and flow rate from their pumping sessions to understand the adequacy of their milk supply to meet their infants' needs. It is well known that mothers' perceptions of low‐ or inadequate‐HM supply are key determinants of early cessation of any or exclusive HM feeding (Blyth et al., 2002; Dennis, 2002; Flower et al., 2008; Li et al., 2008; Meedya, Fahy, & Kable, 2010,). Further, mothers in this sample nearly always attributed decreases in pump output to a falling supply rather than to a fluctuation in their supply or to stress, which has been associated with impaired milk ejection (Feher, Berger, Johnson, & Wilde, 1989; Ueda, Yokoyama, Irahara, & Aono, 1994).
Finally, our findings make an important contribution to an ongoing feminist literature about breastfeeding (Johnson et al., 2009; McCarter‐Spaulding, 2008) by highlighting the importance of considering mothers' lived experiences when conducting future research into the determinants, practices, and consequences of pumping. National endorsement of and support for pumping underscores a mother's right to provide her milk to her infant but not her right to choose how to provide that milk. In our sample, it was common for mothers to describe negative experiences that related to difficulty using their pumps, the burdens associated with negotiating contextual and job‐related constraints to pumping, and the stress that resulted from monitoring pump output to gauge the adequacy of their supply, their pumps, and the food they provided to their infants. Further, our findings and those of other investigators (Johnson et al., 2013) indicate that pumps may have important roles in mothers' perceptions of whether they are—or are perceived as—“good” mothers, in influencing the division of childcare between parents, and in managing mothers' embarrassment about feeding at the breast in public. In addition to the potential impact these roles may have on mothers' long‐term pumping and feeding practices (Dykes, 2005; Johnson et al., 2009, 2013; Ryan, Team, & Alexander, 2013), these reports underscore that it is important to consider the well‐being, agency, and experiences of lactating mothers in future research, legislation, and initiatives related to producing and providing HM. Further, our findings underscore the importance of studying pumping as a practice distinct from feeding at the breast and providing pumped HM (Figure 1).
The qualitative work described here has three limitations. First, we recruited participants based on their intention to feed HM to their infants, not on their intention to pump, so that we could include mothers who did not plan to pump but did at some point. However, all potential participants had considered and anticipated pumping, and all participants pumped. Second, interview guides evolved to incorporate emerging themes. Thus, earlier participants were not explicitly asked about all themes. Third, our binary characterizations of mothers' motivations for pumping do not and cannot fully capture the complexity of those motivations between or within mothers. However, in general, each motivation for pumping could be characterized similarly across mothers in this sample—for example, a motivation that was characterized as nonelective was typically nonelective for most or all mothers that reported that motivation. Further, we did not aim to capture the full complexity of mothers' motivations by characterizing them as elective or nonelective. Instead, we aimed to make a simpler distinction: whether an acceptable and feasible alternative to pumping was available. As a result, we believe this characterization to be a valid representation of this distinction within mothers' experiences.
This work also has a number of strengths that permitted us to address existing gaps in data. The use of interviews and observations that were semi‐structured, in mothers' homes, and longitudinal provided data of great depth and detail. As a result, this study makes a substantial contribution to a small but striking emerging literature on pumping. Recent longitudinal, qualitative data on pumping from mothers the United Kingdom were limited as they were only collected until 6 weeks postpartum, came from the small subsample of HM‐feeding mothers who pumped (n = 7), and were analyzed post hoc (Johnson et al., 2013). Among the few qualitative investigations of HM‐feeding women in the United States, none has focused on pumping, and data have been limited by narrow content, small or homogenous samples, and data from short, recall‐reliant, or non‐home study designs (Cricco‐Lizza, 2005; Flower et al., 2008; Gill, 2001). Last, the diversity in our sample and exclusion of mothers who fed only infant formula added measurably to the quantity and breadth of data available from this prior work.
5. CONCLUSIONS
Although national recommendations and policies endorse pumping as equivalent to feeding infants at the breast, our findings suggest that some mothers may not find pumping to be an adequate or acceptable trade for feeding at the breast. Our findings showed mothers' pumping success may depend on their access to adequate pumps and, for those who work outside the home, workplace support. However, the potential relationships between mothers' support systems and pump quality on their practices for pumping and feeding HM are not yet measured in national data or addressed fully in national legislation. Further, we showed the range of pumping practices that result, in part, from a lack of consistent, adequate advice. Some of these practices raise concerns about whether pumping may modify the benefits conferred to mothers and infants by feeding at the breast. Taken together, these findings demonstrate the need for data to inform evidence‐based guidelines for pumping and storing HM.
SOURCE OF FUNDING
This study was funded by N.I.H. (T32DK007158) and U.S.D.A. (Hatch 399449).
CONFLICTS OF INTEREST
The authors declare that they have no conflicts of interest.
CONTRIBUTIONS
This study was conceived by JPF and KMR. Interviews were conducted by JPF. Interviews were transcribed by JPF, CWQ, RY, and AJW. Primary data analysis was conducted by JPF. CWQ, RY, and AJW assisted with data analysis, and KMR and SRG provided primary guidance on data interpretation. Primary manuscript writing was conducted by JPF, with additional input from KMR and SRG.
ACKNOWLEDGMENTS
The authors would like to thank study participants, their families, and the staff members at OB‐GYN offices and WIC clinics in Tompkins, Cortland, and Onondaga counties who helped recruit them, for their time and effort. The authors would also like to thank Drs. Christine Olson and Carol Devine of the Division of Nutritional Sciences at Cornell University for their insight throughout manuscript writing.
Felice JP, Geraghty SR, Quaglieri CW, Yamada R, Wong AJ, Rasmussen KM “Breastfeeding” without baby: A longitudinal, qualitative investigation of how mothers perceive, feel about, and practice human milk expression. Matern Child Nutr. 2017;13:e12426 10.1111/mcn.12426
REFERENCES
- Baker, M. , & Milligan, K. (2008). Maternal employment, breastfeeding, and health: Evidence from maternity leave mandates. Journal of Health Economics, 27, 871–887. [DOI] [PubMed] [Google Scholar]
- Blyth, R. , Creedy, D. K. , Dennis, C.‐L. , Moyle, W. , Pratt, J. , & De Vries, S. M. (2002). Effect of maternal confidence on breastfeeding duration: An application of breastfeeding self‐efficacy theory. Birth, 29, 278–284. [DOI] [PubMed] [Google Scholar]
- Boo, N. Y. , Nordiah, A. J. , Alfizah, H. , Nor‐Rohaini, A. H. , & Lim, V. K. E. (2001). Contamination of breast milk obtained by manual expression and breast pumps in mothers of very low birthweight infants. Journal of Hospital Infection, 49, 274–281. [DOI] [PubMed] [Google Scholar]
- Clemons, S. N. , & Amir, L. H. (2010). Breastfeeding women's experience of expressing: A descriptive study. Journal of Human Lactation, 26, 258–265. [DOI] [PubMed] [Google Scholar]
- Cricco‐Lizza, R. (2005). The Milk of human kindness: Environmental and human interactions in a WIC clinic that influence infant‐feeding decisions of Black women. Qualitative Health Research, 15, 525–538. [DOI] [PubMed] [Google Scholar]
- Dennis, C.‐L. (2002). Breastfeeding initiation and duration: A 1990‐2000 literature review. Journal of Obstetric, Gynecologic, and Neonatal Nursing, 31, 12–32. [DOI] [PubMed] [Google Scholar]
- Dykes, F. (2005). ‘Supply’ and ‘demand’: Breastfeeding as labour. Social Science & Medicine, 60, 2283–2293. [DOI] [PubMed] [Google Scholar]
- Eidelman, A. I. , Schanler, R. J. , Johnston, M. , Landers, S. , Noble, L. , Szucs, K. , & Viehmann, L. (2012). Breastfeeding and the use of human milk. Pediatrics, 129, e827–e841. [DOI] [PubMed] [Google Scholar]
- Feher, S. D. , Berger, L. R. , Johnson, J. D. , & Wilde, J. B. (1989). Increasing breast milk production for premature infants with a relaxation/imagery audiotape. Pediatrics, 83, 57–60. [PubMed] [Google Scholar]
- Fein, S. B. , Labiner‐Wolfe, J. , Shealy, K. R. , Li, R. , Chen, J. , & Grummer‐Strawn, L. M. (2008a). Infant feeding practices study II: Study methods. Pediatrics, 122, S28–S35. [DOI] [PubMed] [Google Scholar]
- Fein, S. B. , Mandal, B. , & Roe, B. E. (2008b). Success of strategies for combining employment and breastfeeding. Pediatrics, 122, S56–S62. [DOI] [PubMed] [Google Scholar]
- Felice, J. P. , & Rasmussen, K. M. (2015). Breasts, pumps and bottles, and unanswered questions. Breastfeeding Medicine, 10, 412–415. [DOI] [PubMed] [Google Scholar]
- Felice, J. P. , Geraghty, S. R. , Quaglieri, C. W. , Yamada, R. , Wong, A. J. , & Rasmussen, K. M. (2016a). ‘Breastfeeding’ but not at the breast: Mothers' descriptions of providing pumped human milk to their infants via other containers and caregivers. Maternal & Child Nutrition, In revision. doi: 10.1111/mcn.12425 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Felice, J. P. , Cassano, P. A. , & Rasmussen, K. M. (2016b). Pumping human milk in the early postpartum period: Its impact on long‐term practices for feeding at the breast and exclusively feeding human milk in a longitudinal survey cohort. American Journal of Clinical Nutrition, 103, 1267–1277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fereday, J. , & Muir‐Cochrane, E. (2006). Demonstrating rigor using thematic analysis: A hybrid approach of inductive and deductive coding and theme development. International Journal of Qualitative Methods, 5, 80–92. [Google Scholar]
- Flower, K. , Willoughby, M. , Cadigan, R. , Perrin, E. , & Randolph, G. (2008). Understanding breastfeeding initiation and continuation in rural communities: A combined qualitative/quantitative approach. Maternal and Child Health Journal, 12, 402–414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geraghty, S. R. , & Rasmussen, K. M. (2010). Redefining "breastfeeding" initiation and duration in the age of breastmilk pumping. Breastfeeding Medicine, 5, 135–137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geraghty, S. R. , Sucharew, H. , & Rasmussen, K. M. (2012a). Trends in breastfeeding: It is not only at the breast anymore. Maternal & Child Nutrition, 9, 180–187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geraghty, S. , Davidson, B. , Tabangin, M. , & Morrow, A. (2012b). Predictors of breastmillk feeding duration. Breastfeeding Medicine, 7, 112–117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gill, S. L. (2001). The little things: Perceptions of breastfeeding support. Journal of Obstetric, Gynecologic, and Neonatal Nursing, 30, 401–409. [DOI] [PubMed] [Google Scholar]
- Guest, G. , MacQueen, K. M. , & Namey, E. E. (2011). Applied thematic analysis. Thousand Oaks, CA: Sage. [Google Scholar]
- Heymann, J. , & McNeill, K. (2013). Children's chances: How countries can move from surviving to thriving. Cambridge: Harvard University Press. [Google Scholar]
- Johns, H. M. , Forster, D. A. , Amir, L. H. , & McLachlan, H. L. (2013). Prevalence and outcomes of breast milk expressing in women with healthy term infants: A systematic review. Pregnancy and Childbirth, 13, 212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson, S. , Leeming, D. , Williamson, I. , & Lyttle, S. (2013). Maintaining the ‘good maternal body’: Expressing milk as a way of negotiating the demands and dilemmas of early infant feeding. Journal of Advanced Nursing, 69, 590–599. [DOI] [PubMed] [Google Scholar]
- Johnson, S. , Williamson, I. , Lyttle, S. , & Leeming, D. (2009). Expressing yourself: A feminist analysis of talk around expressing breast milk. Social Science & Medicine, 69, 900–907. [DOI] [PubMed] [Google Scholar]
- Keim, S. A. , Hogan, J. S. , McNamara, K. A. , Gudimetla, V. , Dillon, C. E. , Kwiek, J. J. , & Geraghty, S. R. (2013). Microbial contamination of human milk purchased via the Internet. Pediatrics, 132, e1227–e1235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kent, J. C. , Mitoulas, L. R. , Cregan, M. D. , Geddes, D. T. , Larsson, M. , Doherty, D. A. , & Hartmann, P. E. (2008). Importance of vacuum for breastmilk expression. Breastfeeding Medicine, 3, 11–19. [DOI] [PubMed] [Google Scholar]
- Kent, J. C. (2007). How breastfeeding works. Journal of Midwifery & Women's Health, 52, 564–570. [DOI] [PubMed] [Google Scholar]
- Kimbro, R. (2006). On‐the‐job moms: Work and breastfeeding initiation and duration for a sample of low‐income women. Maternal and Child Health Journal, 10, 19–26. [DOI] [PubMed] [Google Scholar]
- Labiner‐Wolfe, J. , Fein, S. B. , Shealy, K. R. , & Wang, C. (2008). Prevalence of breast milk expression and associated factors. Pediatrics, 122, S63–S68. [DOI] [PubMed] [Google Scholar]
- Li, R. , Fein, S. B. , Chen, J. , & Grummer‐Strawn, L. M. (2008). Why mothers stop breastfeeding: Mothers' self‐reported reasons for stopping during the first year. Pediatrics, 122, S69–S76. [DOI] [PubMed] [Google Scholar]
- McCarter‐Spaulding, D. (2008). Is breastfeeding fair? Tensions in feminist perspectives on breastfeeding and the family. Journal of Human Lactation, 24, 206–212. [DOI] [PubMed] [Google Scholar]
- Meedya, S. , Fahy, K. , & Kable, A. (2010). Factors that positively influence breastfeeding duration to 6 months: A literature review. Women and Birth, 23, 135–145. [DOI] [PubMed] [Google Scholar]
- Mitoulas, L. R. , Lai, C. T. , Gurrin, L. C. , Larsson, M. , & Hartmann, P. E. (2002). Effect of vacuum profile on breast milk expression using an electric breast pump. Journal of Human Lactation, 18, 353–360. [DOI] [PubMed] [Google Scholar]
- Morton, J. , Hall, J. Y. , Wong, R. J. , Thairu, L. , Benitz, W. E. , & Rhine, W. D. (2009). Combining hand techniques with electric pumping increases milk production in mothers of preterm infants. Journal of Perinatology, 29, 757–764. [DOI] [PubMed] [Google Scholar]
- Odom, E. C. , Li, R. , Scanlon, K. S. , Perrine, C. G. , & Grummer‐Strawn, L. (2013). Reasons for earlier than desired cessation of breastfeeding. Pediatrics, 131, e726–e732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ortiz, J. , McGilligan, K. , & Kelly, P. (2004). Duration of breast milk expression among working mothers enrolled in an employer‐sponsored lactation program. Pediatric Nursing, 30, 111. [PubMed] [Google Scholar]
- Patient Protection and Affordable Care Act , H.R. 3590, 111th Congress, 2nd Sess. (2010) Retrieved from: http://www.dol.gov/whd/regs/compliance/whdfs73.htm (accessed 17 December 2016).
- Prime, D. K. , Geddes, D. T. , Hepworth, A. R. , Trengove, N. J. , & Hartmann, P. E. (2011). Comparison of the patterns of milk ejection during repeated breast expression sessions in women. Breastfeeding Medicine, 6, 183–190. [DOI] [PubMed] [Google Scholar]
- Rasmussen, K. M. , & Geraghty, S. R. (2011). The quiet revolution: Breastfeeding transformed with the use of breast pumps. American Journal of Public Health, 101, 1356–1359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rojjanasrirat, W. , & Sousa, V. D. (2010). Perceptions of breastfeeding and planned return to work or school among low‐income pregnant women in the USA. Journal of Clinical Nursing, 19, 2014–2022. [DOI] [PubMed] [Google Scholar]
- Ryan, K. , Team, V. , & Alexander, J. (2013). Expressionists of the twenty‐first century: The commodification and commercialization of expressed breast milk. Medical Anthropology, 32, 467–486. [DOI] [PubMed] [Google Scholar]
- Ryan, A. S. , Zhou, W. , & Arensberg, M. B. (2006). The effect of employment status on breastfeeding in the United States. Women's Health Issues, 16, 243–251. [DOI] [PubMed] [Google Scholar]
- Sloan, S. , Sneddon, H. , Stewart, M. , & Iwaniec, D. (2006). Breast is best? Reasons why mothers decide to breastfeed or bottlefeed their babies and factors influencing the duration of breastfeeding. Child Care in Practice, 12, 283–297. [Google Scholar]
- Soto‐Ramirez, N. , Karmaus, W. , Zhang, H. , Davis, S. , Agarwal, S. , & Albergottie, A. (2013). Modes of infant feeding and the occurrence of coughing/wheezing in the first year of life. Journal of Human Lactation, 29, 71–80. [DOI] [PubMed] [Google Scholar]
- Thulier, D. , & Mercer, J. (2009). Variables associated with breastfeeding duration. Journal of Obstetric, Gynecologic, and Neonatal Nursing, 38, 259–268. [DOI] [PubMed] [Google Scholar]
- Ueda, T. , Yokoyama, Y. , Irahara, M. , & Aono, T. (1994). Influence of psychological stress on suckling‐induced pulsatile oxytocin release. Obstetrics & Gynecology, 84, 259–262. [PubMed] [Google Scholar]
- U.S. Department of Labor, Bureau of Labor Statistics (2013) Leave benefits: Access, civilian workers: National Compensation Survey, March 2013. Washington, DC: U.S. Department of Labor.
- U.S. Department of Health and Human Services (2011). Executive Summary: The surgeon general's call to action to support breastfeeding. Breastfeeding Medicine, 6, 3–5. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services, Health Resources and Services Administration (HRSA), Maternal and Child Health Bureau . (2008) Employees' guide to breastfeeding and working. Every Mother, Inc. and Rich Winter Design and Multimedia. pp. 3–5.
- Win, N. N. , Binns, C. W. , Zhao, Y. , Scott, J. A. , & Oddy, W. H. (2006). Breastfeeding duration in mothers who express breast milk: A cohort study. International Breastfeeding Journal, 1, 28. [DOI] [PMC free article] [PubMed] [Google Scholar]


