Abstract
As pumping has become more prevalent among American women, pumped human milk (HM) is on the rise in their infants' diets in place of some or all feeding at the breast. We aimed to fill a gap in knowledge about mothers' motivations, practices and perceptions related to pumping, and about mothers' and other caregivers' motivations, practices, and perceptions related to feeding pumped HM. Results related to providing pumped HM are reported here, and results related to pumping are reported elsewhere. We conducted in‐depth, semi‐structured interviews among a diverse sample of mothers whose infants were fed pumped HM (n = 20), following each up to 1 year postpartum. Data were analyzed using thematic analysis with Atlas.ti. Nearly all mothers felt bottles were necessary to meet infant HM‐feeding goals. Nearly all pumped HM was fed by other caregivers because mothers typically preferred and prioritized feeding at the breast for convenience and maintaining their milk supply. Infants were bottle‐fed HM for several reasons that changed over time, such as mother's absence, latch difficulty, or desire to share the burden and bonding of feeding. Feeding practices differed between feeds from bottles versus at the breast; some infants were bottle‐fed on schedules but fed at the breast on demand. Mothers' methods for storing, transporting, and preparing HM varied substantially and included practices associated with loss of nutrients and microbial contamination. Mothers' reasons for bottle‐feeding HM may affect how much their infants are bottle‐fed. Consumption of pumped HM may not provide the same benefits to infants as feeding at the breast. These findings highlight important avenues for future research into the relationships between bottle‐feeding HM and infant health, growth, and developmental outcomes.
1. INTRODUCTION
Until recently, women have fed nearly all human milk (HM) by feeding infants at the breast. In the United States now, however, HM is increasingly pumped and fed to infants from bottles or cups in place of some or all feeds at the breast, practices that are nationally endorsed as equivalent to feeding at the breast (Eidelman et al., 2012; U.S. Department of Health and Human Services, Health Resources and Services Administration, HRSA, Maternal and Child Health Bureau, 2008; U.S. Department of Health and Human Services, 2011). This shift resulted from the congruence of women's need to work outside the home (Kimbro, 2006; Rojjanasrirat & Sousa, 2010; Ryan, Zhou, & Arensberg, 2006; Thulier & Mercer, 2009) and the recent development of high‐efficiency commercial pumps (Rasmussen & Geraghty, 2011).
Recent data about bottle‐feeding HM come from a national longitudinal survey cohort, the Infant Feeding Practices Study II (IFPS II; Fein et al., 2008). However, the IFPS II surveys did not clearly distinguish feeds at the breast from feeding pumped HM or distinguish mothers' reasons for feeding pumped HM from their reasons for pumping (Labiner‐Wolfe, Fein, Shealy, & Wang, 2008). Further, IFPS II data describe how frequently, but not how, pumped HM is fed. IFPS II surveys also did not include questions about how mothers understand or feel about feeding pumped HM, which may relate to their intended future practices for bottle‐feeding HM or infant formula and for feeding their infants at the breast. Recent qualitative data describe U.K. mothers' experiences pumping their milk, but feeding pumped milk, in their first month postpartum (Johnson, Leeming, Williamson, & Lyttle, 2013; Johnson, Williamson, Lyttle, & Leeming, 2009).
Little is known about potential consequences of bottle‐feeding HM compared to feeding at the breast, yet early data signal potential cause for concern (Felice & Rasmussen, 2015). IFPS II infants who were bottle‐fed HM exhibited more bottle‐emptying (Li, Fein, & Grummer‐Strawn, 2010) and more rapid weight gain (Li, Magadia, Fein, & Grummer‐Strawn, 2012) than those fed at the breast. Qualitative data suggest that the timing and length of feeds at the breast are more infant‐controlled than bottle‐feeds of formula (Wright, Fawcett, & Crow, 1980). In experimental data, infants fed at the breast regulated their intake to match their needs (Kent, 2007), and infants bottle‐fed formula consumed more volume and energy in a feed than those fed at the breast (Heinig, Nommsen, Peerson, Lonnerdal, & Dewey, 1993). Thus, a link between bottle‐feeding HM and increased bottle emptying and weight gain compared to feeding at the breast may be explained by differences in feeding practices. Temperature and container changes to HM from storage and preparation may also impact its nutritional, pathogenic, and immunological content (Boo, Nordiah, Alfizah, Nor‐Rohaini, & Lim, 2001; García‐Lara et al., 2012; Keim et al., 2013). Thus, mothers' practices for preparing and bottle‐feeding HM must be characterized.
We aimed to fill these gaps in knowledge by collecting in‐depth, longitudinal qualitative data on how and why mothers pump and their infants are fed pumped HM. We report the results of this work that were related to providing pumped HM here, and results related to pumping HM elsewhere (Felice et al., 2016). The distinction between these two contributions reflects an important consequence of the rise in these practices: that the provision of HM can no longer be considered an exclusively dyadic behavior (Figure 1; Felice & Rasmussen, 2015). While feeding an infant at the breast, HM is removed from the breast and provided to the infant simultaneously. In contrast, when HM is pumped and then bottle‐ or cup‐fed, the removal of HM from the breast and the provision of that HM to an infant are distinct practices that raise distinct questions. For example, the rise in pumped HM‐feeding raises questions about how different practices for storing, preparing, and feeding pumped HM relate to the safety of pumped HM as fed. The reliance of working mothers on pumping raises questions about how workplace factors may relate to their success in meeting their goals for providing their HM (Felice et al., 2016). As a result, it is now essential to distinguish among practices for feeding at the breast, pumping, and feeding pumped HM (Figure 1; Felice & Rasmussen, 2015).
Figure 1.
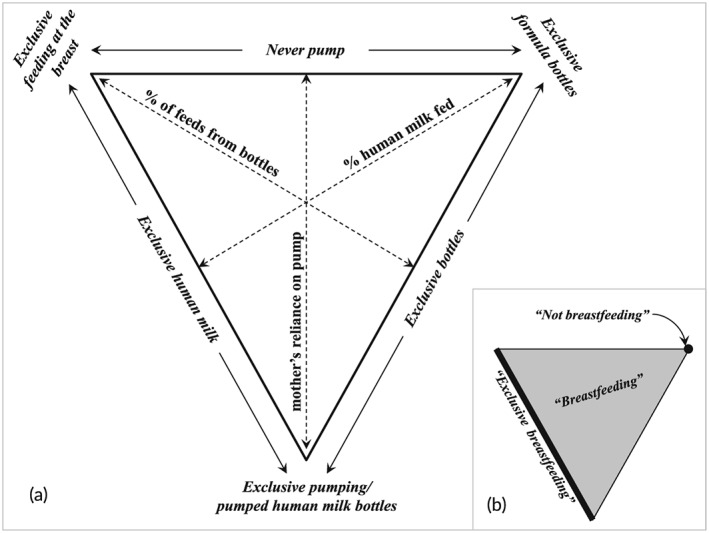
A new framework to characterize the current American mother–infant dyad. This figure illustrates the importance of distinguishing among feeding at the breast, pumping, and providing pumped human milk (Felice & Rasmussen, 2015). (a) How mothers and infants currently may be categorized when nothing is fed aside from human milk and/or infant formula (i.e., before the introduction of solids or other milks) and without considering pumped milk that is mixed with solids or cases where infants are fed human milk that was not provided by their biological mother. (b) How current terminology fits within this triangular framework of current practices for producing and feeding human milk. This figure is reprinted with permission from Breastfeeding Medicine
Here, we describe results related to the infants' perspective—that is, how pumped HM provided to infants in our sample was stored, prepared, and fed—as described by their mothers. More specifically, we describe mothers' motivations for providing pumped HM to their infants, their attitudes and perceptions of feeding pumped HM, the strategies that mothers and other caregivers used to feed pumped HM to infants, and how those motivations, perceptions, attitudes, and practices changed over time. Results related to the mothers' perspective—that is, pumping HM—are reported elsewhere (Felice et al., 2016).
Key messages
This qualitative study addresses an important gap in knowledge about the preparation and feeding of pumped milk, which have taken an increasingly prominent role in U.S. infant‐feeding practices.
This study uses a unique in‐depth longitudinal design to describe mothers' and other caregivers' practices for and perceptions of feeding pumped HM to infants in a diverse, longitudinal sample.
The findings of this study underscore available evidence suggest that feeding pumped HM to infants may not provide the same benefits as feeding them at the breast.
2. METHOD
We used longitudinal, qualitative methods among a diverse sample of HM‐feeding women in upstate New York (n = 20). These methods are described in more details elsewhere (Felice et al., 2016), where we have reported mothers' attitudes, perceptions, and practices for pumping HM. Briefly, we conducted semi‐structured, in‐depth interviews and observations between September 2011 and November 2013, following mothers from late in their pregnancies through up to 1 year postpartum.
2.1. Participants and recruitment
Participants were recruited from three counties in New York State, and gave written consent before the first interview. Mothers were considered for inclusion if they intended to feed their HM to their infants for any length of time and had heard about pumping. However, the intention to pump or feed pumped HM was not an inclusion criterion. Mothers were purposively recruited for heterogeneity on factors associated with producing HM, such as marital, employment, and socioeconomic statuses, age, ethnicity, and parity.
2.2. Data collection
For all mothers, the first interview was conducted in the third trimester, and the second was conducted at approximately 2 weeks postpartum. Afterward, mothers were contacted every 3 to 4 weeks to identify major changes in the practices with which their infants were fed (e.g., the introduction of bottles), and interviews were scheduled as soon as possible after each change (for more details, see Felice et al., 2016). Each semi‐structured, open‐ended interview focused on mothers' attitudes, perceptions, and practices for providing pumped HM to their infants and for having other caregivers feed pumped HM to their infants. Multiple interview guides were used to reflect different major changes in pumping or feeding practices and employment status, and each contained questions about main themes plus questions relevant to the most recent major changes. Because we purposively recruited a sample with diverse home, work, and family contexts, interview guides included questions that were only posed to some mothers, and interview guides were sometimes combined or omitted. For example, mothers who did not work outside the home were not interviewed using the employment‐specific interview guide.
2.3. Data analysis
Interviews were recorded and transcribed, and transcripts were checked twice for accuracy with interview recordings. Some predetermined themes were identified from existing literature (Fein et al., 2008; Li et al., 2010; Li et al., 2012). Predetermined and emerging themes were examined with a combination of iterative and deductive thematic analysis using iterative open‐ and close‐coding in Atlas.ti (Berlin, Germany). At each interview, JPF clarified with mothers the transition that necessitated the interview and mother's experiences with that transition. All quotes are reported with pseudonyms and by the infant's age at the time of quote collection. This work was approved by Cornell University's Institutional Review Board.
3. RESULTS
All infants in the study sample were born at term, and 108 interviews were conducted (range 2–7 per participant mother). Mothers varied in age, ethnicity, parity, employment and marital status, and prior experience with feeding at the breast and bottle‐feeding HM (Felice et al., 2016). All but one participant remained until one y postpartum (n = 12) or HM‐feeding cessation prior to 1 year (n = 7). Although intention to feed pumped HM was not an inclusion criterion, all infants were bottle‐fed HM at some point.
3.1. Mothers' motivations for providing pumped milk to their infants
Mothers reported that most of their pumped HM was fed to their infants because feeding at the breast was unavailable and reported reasons for this unavailability that changed over time. For example, in early infancy, when mothers could be with their infants most of the time, some mothers provided pumped HM to their infants because of latch problems, and four mothers relied primarily or solely on bottles to feed HM for this reason. After early infancy, when mothers and infants were separated more regularly, employment outside the home was an important constraint to feeding at the breast.
Mothers also described motivations for what their infants were fed from bottles that included preferences for providing HM versus formula for infant health and cost savings. Mothers reported supplementing with formula when they thought their infants were old and/or healthy enough that the benefit of HM was less important. Some mothers chose to feed formula to infants themselves when pumped HM was available either to avoid having to pump more, to save HM for other caregivers to feed, or to conserve stocked pumped HM and, thus, lengthen the period their infants received any HM.
Many infants in this sample were fed bottles that contained both HM and formula. Mothers and other caregivers typically added formula to pumped HM to reach what they perceived as the meal size their infants needed.
[If] I had enough, if I had pumped enough at that time—because I ended up only pumping like three or four times a day—I would just feed that, or we'd just add formula to it to get the two to three ounces. –Sarah, 2 months
However, this practice resulted in bottles that contained widely varying proportions of HM and infant formula. Some infants were fed bottles with only a nominal amount of formula added to supplement pumped HM, while others were fed a small amount of pumped HM as a nutritional and immunological supplement to formula.
3.2. Mothers' and other caregivers' practices for preparing and feeding pumped milk
Across their first year, infants were fed pumped HM to a widely varying degree, from never to as a sole source of HM or any food. Mothers typically preferred and prioritized feeding at the breast and, thus, other caregivers fed nearly all pumped HM, especially after mothers returned to work outside the home. Mothers who bottle‐fed their milk themselves described feeds at the breast as unsuccessful, uncomfortable, or inadequate.
Babies gonna lose a certain percentage [in the hospital], but he lost 2% more. I think it's our breastfeeding battle we were having. … [On day three, the pediatrician said], like, ‘Well, this, let's try [pumping],’ because I didn't really want to supplement with formula. No. And so I cried for that, too. … So I had to start pumping early, and give him whatever remaining, feed him and then pump whatever's left in my boob, and then give him that. … And I was like, it's crazy, because in the beginning, I started and there was lots of milk left, and then afterward, like with me stuffing him with the leftovers, it's like, he started just naturally eating mostly all of it by himself. … in a second.
–Linda, 3 weeks
Later in infancy, a few mothers added pumped HM to infant cereals or other solids to improve their nutrition or palatability or fed HM from cups to avoid or reduce the use of bottles.
Many strategies were used to store, transport, and prepare HM, which resulted in a variable number of storage conditions and container transfers before it was fed to infants (Figure 2). The number of pieces of equipment that HM contacted before being fed ranged from two, when HM was pumped directly into a feeding bottle from a hospital‐grade pump, to six, when HM was pumped with a commercial pump into a bottle, refrigerated in another, frozen in a bag, and fed from a bottle or cup.
Figure 2.
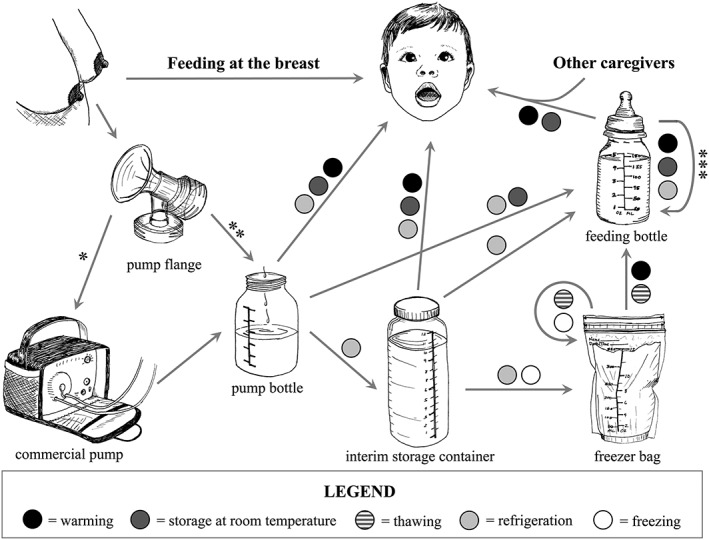
Temperature and container changes to pumped human milk (HM) before feeding to infants. *Commercially‐available pumps, designed for single users, that have open systems. **Hospital‐grade pumps that have closed systems and are safe for multiple users. ***Some mothers and other caregivers saved pumped HM from unfinished bottles and fed it to infants later. This figure represents the range of potential practices with which pumped HM was handled in this sample after it was pumped and before it was fed to infants. The figure shows potential containers with which pumped HM came in contact and potential temperature treatments done to HM between a pumping session and when that pumped HM was fed. Temperature changes include (BLACK circle) by submersion of bag in warm or hot water, by heating in a pan, or by microwaving, storage at room temperature (DARK GRAY circle), thawing (STRIPED circle) at room temperature or in the refrigerator, refrigeration or storage in cooler (LIGHT GRAY circle), and freezing (WHITE circle) in regular freezer or deep freezer. Mothers in this sample followed all potential paths of HM between breast and infant: that is, some mothers fed HM directly from pump bottle, and others used some or all container and temperature changes shown
Pumped HM to be fed within a day or two was refrigerated, and HM to be fed later was frozen in bags. Some mothers kept stocks of frozen pumped HM with daycare providers or at family members' homes to be fed there or as extra stock. Some pumped HM was fed immediately after it was pumped, but most pumped HM had undergone between 1 and 5 or more temperature changes before it was fed to infants. Frozen HM was thawed at room temperature or in hot water or a microwave, and refrigerated HM was warmed by placing bottles in hot water, a bottle warmer, or a microwave. If infants did not finish bottles, some mothers and caregivers discarded the rest to avoid contamination. Others did not want to waste HM, and kept it refrigerated or at room temperature until it was fed later.
Like if he'll stop, sometimes he'll go back to sleep for another hour or two, and then we just pull out that same bottle and use it. Cause I do not want to waste any of the milk that takes me so long to get. –Theresa, 2.5 months
Mothers and other caregivers determined how much to put in infants' bottles in a range of ways. In general, the purpose of a feeding guided the amount of HM caregivers put in bottles. When bottles were a supplement to feeds at the breast or solids, they contained a small amount (~1–3 oz.), and infants were typically permitted to stop as they wished.
When bottles were fed as a meal in place of feeds at the breast, their contents reflected mothers' or caregivers' perceptions of their infants' needed meal size. Many infants were fed the same amount at each feeding, and this amount only changed when mothers perceived that their infants' needs had increased. The few mothers who varied bottle sizes to meet infants' episodic needs, or instructed other caregivers to do so, were those who relied on feeding at the breast for most HM feeding or were confident in their infants' ability to eat as much as they needed.
[I deliver pumped HM to the caregiver] right in the bags, because I figured it varies a lot because of how much she drinks [while I feed her at my breast], so it's going to vary how much she's going to drink during the day, too. So there'll be times when she just needs a little bit, or sometimes she needs more. Maybe she'll start off with a big one and really still be thirsty, then she could have a little one or something. So I just gave them the bags as‐is. –Flora, 3 months
When mothers' and other caregivers' bottle‐feeding practices differed, mothers often described responding to their infant's episodic needs. Some worried that caregivers did not read infant cues as well and, thus, overfed, but three adopted caregivers' practices even if they questioned them.
He wasn't really even wanting to drink [the bottle], like you had to encourage him. Well, I didn't, the babysitter had to encourage him to drink the six ounces. And my babysitter, she's funny. She likes to take charge, I guess. … She came up with a whole new schedule for him that we just started like two days ago. He's now drinking like a four‐ounce bottle here with some cereal, and then—I don't know, I have her schedule written out, I don't even know it myself. –Avery, 7 months
Practices with which infants were fed HM differed by the method of feeding and the feeding context. How HM‐feeding episodes began and ended differed by breast versus bottles, regardless of who bottle‐fed infants. Feeds at the breast were typically initiated by infants and ended when infants pulled away, fell asleep or, in mothers' perception, stopped sucking productively. In contrast, although some mothers and caregivers bottle‐fed on demand, many mothers who relied on bottles regularly or anticipated that they would be in the future reported that their infants were bottle‐fed on schedules, even if mothers continued feeding at the breast on demand. Practices for bottle‐feeding HM also differed by where infants were bottle‐fed. It was common for infants to be fed on demand at home—for example, given amounts tailored to their episodic needs or allowed to leave bottles unfinished—whether or not mothers bottle‐fed infants themselves. Some infants were bottle‐fed on demand at home but not with outside caregivers.
[The daycare providers feed a bottle] every two hours. And so we told them, ‘Oh you only need to feed her when she's fussy, that's when to feed her. She gets fussy you'll be able to tell.’ But it's every two hours. And when you go to her little information sheet, they're like, ‘[baby] likes to eat every two hours.’ So, we're like meh, it works. … I think they just like everything on a schedule. –Dora, 6 months
Further, some mothers noted that infants did not finish bottles with them, but other caregivers reported consistent bottle emptying, which was a common impetus for increasing bottle size.
Well, [the increase in meal bottle size] wasn't so much me. It was that the sitter was saying ‘He's really chugging his bottles, you know, he's really just downing them and acting like he could go for more.’ And I said, ‘Well then test it out with him!’ You know, like, ‘Instead of four, give him, give him, give him five. If he does five, you know, eventually, and he's acting hungry still, give him six.’ So we went from three 4‐ounce bottles… to four 4‐ounce, and then it was three or four 5‐ounce, and now he's doing I think three 6‐ounce bottles. –Kerry, 6 months
If mothers were unable or unwilling to pump more to meet their infants' increasing needs with pumped HM, regular bottle emptying with caregivers contributed to starting or increasing formula use.
Because the mothers in this sample only provided their own pumped HM to their infants, the end of feeding pumped HM was a direct result of the end of pumping. Our findings about mothers' motivations for stopping pumping are reported elsewhere (Felice et al., 2016). For all but one mother, the end of feeding pumped HM fell between a few days and a few weeks after mothers stopped pumping. Three mothers intended to create a large stock of frozen pumped HM; of these, two experienced work‐related constraints to accumulating a large enough stock to meet their goals.
3.3. Mothers' attitudes toward and perceptions of providing pumped milk to their infants
Mothers described a range of attitudes toward and perceptions of their infants' consumption of pumped HM that changed over time and reflected their perceptions of their infants' current need for HM, their attitudes toward pumping and formula, and their other obligations at home. These attitudes and perceptions were related to three general topics.
First, mothers described attitudes and perceptions toward the general availability of pumped HM. All mothers felt that, to avoid or reduce formula use, they would need pumped HM for when feeding at the breast was not successful, available, or desired. Most mothers appreciated that pumped HM allowed them to share the bonding and tasks of infant feeding, to avoid feeding their infants at the breast in public, and to provide extra nutrition and immunologic benefit to older infants. However, some were uncomfortable sharing feeding decision‐making with other caregivers.
Being at home now for the month and a half or so I've been home, I feel like I'm so much more in tune to him. Because then, it was like somebody else was making his schedule, and I'm asking them, ‘When does my baby eat?’ And I didn't like that, but I had no control over it. And I felt like he was eating when I didn't feel like he needed to be eating. ... So now that I've been home, I feel like I'm much more in tune to what he needs to eat, and I set the schedule now, so what I feel like is best for him and works best for us. –Avery, 9.5 months
Mothers' perceptions of the benefits to infants of pumped HM differed. Most felt that pumped HM was equivalent to HM directly from the breast for their infant's health. Comparatively, fewer mothers described perceived differences, such as a higher risk of overfeeding or overweight or suboptimal language development conferred by bottle‐feeding versus feeding at the breast.
Second, mothers also described attitudes and perceptions toward the acts of preparing and feeding pumped HM that were commonly negative and influenced their preferences among feeding at the breast, bottle‐feeding HM, and bottle‐feeding formula. Many mothers described a long list of tasks and considerations that were necessary to provide what they perceived was enough HM to meet their infants' needs (Figure 3). Most frequently, mothers found the tasks associated with feeding pumped HM to be time‐consuming, tedious, and never‐ending, but easy to understand and accomplish.
Figure 3.
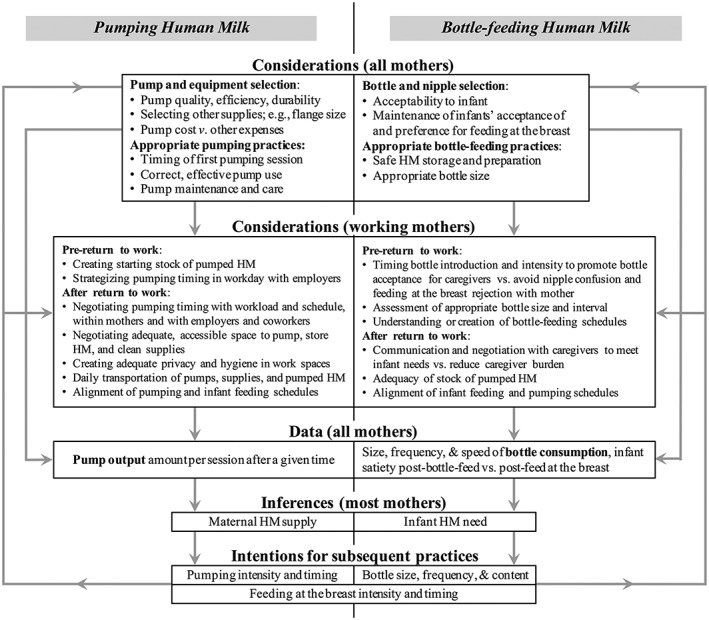
Mothers' considerations and interpretations related to pumping and bottle‐feeding human milk (HM) to their infants. This figure should be read from the top down, from practical considerations for pumping and bottle‐feeding HM for all mothers and for working mothers to data collected and consequent inferences and intentions at the bottom. Mothers' inferences and intentions manifested in subsequent practices, which perpetuate practical considerations. To reflect that pumps and bottles split feeding at the breast into two separately occurring phenomena—removing HM from mothers' breasts and feeding infants—this figure may also be read in two sides. The left side of the figure shows mothers' considerations related to pumping, and the right side shows those related to bottle‐feeding HM. Feeding at the breast is included under intentions as they were impacted by considerations and cognitive processes for pumping and bottle‐feeding HM and shown on both sides as it both removes HM from breasts and feeds it to infants
Third, mothers described perceptions about the relationships among their pump output, their milk supply, and their infants' needs. Specifically, mothers compared the size and frequency of their infants' bottles and the rate at which they consumed them—information that was typically reported by other caregivers—to the output from and length of each of their pumping sessions and the number of times they were able and willing to pump. Many mothers perceived that the availability of this information was a benefit compared to feeding at the breast. However, mothers who did not pump as much as their infants consumed reported stress or feelings of personal failure.
Well, I just feel like a little bit like my self‐worth is tied to my milk output. I feel like, ‘Oh, if I'm not making enough milk, I'm not going to provide for my baby.’ But that adds to the stress, and then that makes it harder to get the milk out.
–Maureen, 7 months
Regardless of whether mothers intentionally sought this information, nearly all recognized and interpreted it to guide their subsequent behaviors. A perceived “deficit”—for examle, when a mother's yield from a pumping session was less than what her infant was fed from a bottle—often resulted in an introduction to or increase in formula or an increase in bottle feeds.
…he's really not getting [at the breast] what he gets when he's with the sitter, because he's getting 6‐ounce bottles [of formula and HM mixed]. I know that I'm pumping at best 3 ounces, pretty much, sometimes three and a half in a sitting. …So if he's just nursing off and on every couple hours, he's not getting what he's used to volumetrically from the sitter. So this last weekend, I made a point to … give him at least one [bottle]‐feeding ... so that I knew that he was getting a good 6 ounces. –Kerry, 6 months
4. DISCUSSION
Mothers in this sample described a wide range of practices with which their pumped HM was prepared and fed to their infants. In many cases, practices for bottle‐feeding HM were less responsive than practices for feeding the same infant at the breast, and practices for preparing HM before feeding it to infants included a range of changes in temperature and container. Mothers described a wide range of reasons that they both wanted and needed to feed pumped HM to their infants instead of feeding them at the breast. Most mothers felt that feeding pumped HM was necessary to meet overall goals for feeding HM and appreciated it as an option when they could not feed their infants at the breast. Taken together, these findings permit the development of a more nuanced understanding of how and why infants are fed pumped HM.
Mothers' motivations for providing their pumped HM to their infants and their reports that most pumped HM was fed by other caregivers indicate important gaps in available data. Limited prior understanding of mothers' motivations for providing pumped HM comes from the IFPS II (Labiner‐Wolfe et al., 2008) and qualitative data from the U.K. (Johnson et al., 2013; Johnson et al., 2009) and Australia (Clemons & Amir, 2010). However, these studies only provided data about mothers' reasons for pumping. Our findings suggest that motivations for feeding pumped HM to infants do not always relate to mothers' motivations for pumping and that some of IFPS II mothers' reported motivations for pumping were actually reasons that their infants were fed pumped HM. Further, these findings underscore the importance of studying the provision of pumped HM as a practice distinct from feeding at the breast and pumping (Figure 1). More specifically, future research into feeding pumped HM must distinguish motivations for feeding pumped HM to infants from mothers' motivations for pumping. Moreover, our finding that most pumped HM was fed by caregivers other than mothers highlights the need to measure in national survey data both how much and how other caregivers feed HM.
Mothers' reports of how HM was handled and prepared before it was fed to infants echo concerns raised by others (Boo et al., 2001; Cooper, Barnett, Gentles, Cairns, & Simpson, 2013; García‐Lara et al., 2012; Johnson et al., 2013; Keim et al., 2013; Wojcik, Rechtman, Lee, Montoya, & Medo, 2009) about the nutritional adequacy and microbial safety of pumped HM as fed. In this sample, pumped HM was stored for durations between minutes and months and went through 0 to 5 or more temperature changes before it was fed to infants. The macronutrient composition of HM changes across a year to meet infants' changing needs (Kent, 2007), and long‐term freezing of pumped HM may lower its fat content and energy (García‐Lara et al., 2012). Thus, pumped HM that is fed to infants after weeks or months of storage may have since decreased in fat content. Moreover, our finding that pumped HM comes in contact with 2 to 6 containers before feeding is important because it may partly explain recent data showing widespread pathogenic contamination of pumped HM (Boo et al., 2001; Keim et al., 2013) and increased coughing and wheezing among infants bottle‐fed HM compared to those fed at the breast (Soto‐Ramírez et al., 2013). Data are now needed to quantify the impact of various practices for pumping, handling, and preparing pumped HM on its nutritional adequacy and immunological integrity as fed.
Mothers' descriptions of how their infants were fed their pumped HM and the perceptions that informed those feeding practices amplify concerns raised by other investigators about growth outcomes among infants who are bottle‐fed HM compared to those who are fed at the breast. In this sample, some infants were bottle‐fed on schedules and with consistent bottle sizes even when they were fed at the breast on demand. Mothers who described having different practices for feeding their infants than outside caregivers reported that they fed their infants more responsively than other caregivers. Responsive feeding is important to meet infants' needs, which vary within a day and over time (Kent, 2007). IFPS II infants who were bottle‐fed at high intensity—whether HM or formula—had impaired self‐regulation of intake (Li et al., 2010) and faster weight gain (Li et al., 2012) by the end of their first year than those fed at the breast. Thus, our findings suggest that the more rapid weight gain among infants bottle‐fed HM may be explained, in part, by less responsive feeding practices for bottle‐feeding HM versus feeding at the breast. These findings support a recent clinical practice statement (Whitaker & Wright, 2012) that raised concerns about caregiver‐controlled, amount‐oriented bottle‐feeding of HM, and its potential impacts on infant growth. As a result, it is important to investigate practices for feeding at the breast and bottle‐feeding HM to understand their potential links to infant growth outcomes.
Mothers described a range of attitudes that illustrated generally positive feelings toward the availability of feeding pumped HM as an option when desired or needed, particularly as it related to sharing the bonding experience of feeding infants with significant others (Hoddinott, Britten, McInnes, Craig, & Darwent, 2013; Leeming, Williamson, Lyttle, & Johnson, 2013). They also described simultaneous, generally negative feelings toward their experiences providing pumped milk or having other caregivers do so. These findings raise concerns about the infants of mothers who must replace feeds at the breast with pumped HM feeds more often they would prefer. These mothers may suffer greater disruption to their work and home obligations or may be more likely to feed formula. Further, our findings highlight that attitudes toward feeding at the breast and bottle‐feeding HM should be studied separately to understand how they might affect mothers' intentions and practices.
Our finding that mothers interpret information from their infants' bottle feeds to gauge their infants' needs, and compare this information to their pump output to determine their ability to meet their infants' needs, is important because these practices may have two consequences of concern. First, some mothers who regularly used bottle‐feeding and pumping information to guide their infant‐feeding practices reported that the availability and the use of that information caused or increased their concern about the adequacy of their supply. This finding is important because mothers who perceive a low‐milk supply are more likely to stop feeding HM exclusively or at all (Li, Fein, Chen, & Grummer‐Strawn, 2008; Meedya, Fahy, & Kable, 2010). Second, the use of data from pumps and bottles may fundamentally change the nature of HM‐feeding as it relates to infants' changing demands. While feeding at the breast, only an infant or his mother can determine when a feed should start and end. In contrast, in our sample, it was common for an infants' bottle size to be determined by external factors, such as the efficiency of a mother's pump or the perceptions of other caregivers. This finding is important because infants who are fed at the breast regulate their own energy intake, and their needs vary within and across days, weeks, and months (Kent, 2007). As a result, our findings are important because they suggest that current practices for bottle‐feeding pumped HM may reduce the control that infants have over their intake compared to feeding at the breast and, thus, may not meet their changing needs as effectively.
The qualitative investigation presented here has two limitations. First, in this sample, most pumped HM was fed by caregivers other than the mothers, and mothers' knowledge of these practices ranged from none to complete. This limitation reflects an important shift in the decision‐making power of feeding HM from solely mothers to multiple caregivers. Consequently, qualitative and quantitative data on feeding pumped HM are needed from all caregivers who feed HM. Second, because we iteratively modified interview guides to incorporate emerging themes, early participants were not explicitly asked about some themes. As a result, important themes identified here must be investigated systematically using surveys of larger and more representative samples.
This work has a number of strengths that act together to fill prior gaps in qualitative data on HM‐feeding. This work is the most comprehensive qualitative investigation of HM‐feeding yet reported and the only qualitative investigation of feeding pumped HM, a behavior that has become widespread in the United States. The use of semi‐structured, in‐home interviews and observations provided us with data of great depth and detail about infant feeding. The inclusion of open‐ended questions in interviews provides novel opportunity to understand mothers' reasoning for and responses to the practices with which their infants are fed pumped HM. Our longitudinal design is unusual in qualitative investigation of HM, and the duration of our observation of these mothers was unprecedented. It minimized mothers' reliance on recall and allowed real‐time observation of the evolution of mothers' attitudes and perceptions and their short‐ and longer‐term impact on practices.
5. CONCLUSIONS
Our findings provide novel insights into practices for providing pumped HM to American infants. These findings complement emerging quantitative evidence that suggests that feeding pumped HM may not confer the same benefits to infants as feeding them at the breast and may introduce other risks. This possibility raises urgent questions about national policies that endorse bottle‐feeding pumped HM as equivalent to feeding at the breast. Further, these findings are a call to researchers and clinicians to be aware of and to investigate relationships between feeding pumped HM and infant health, growth, and developmental outcomes.
SOURCE OF FUNDING
This study was funded by N.I.H. (T32DK007158) and U.S.D.A. (Hatch 399449).
CONFLICTS OF INTEREST
The authors declare that they have no conflicts of interest.
CONTRIBUTIONS
This study was conceived by JPF and KMR. Interviews were conducted by JPF. Interviews were transcribed by JPF, CWQ, RY, and AJW. Primary data analysis was conducted by JPF. CWQ, RY, and AJW assisted with data analysis, and KMR and SRG provided primary guidance on data interpretation. Primary manuscript writing was conducted by JPF, with additional input from KMR and SRG.
ACKNOWLEDGMENTS
The authors would like to thank study participants, their families, and the staff members at OB‐GYN offices and WIC clinics in Tompkins, Cortland, and Onondaga counties who helped recruit them, for their time and effort. The authors would also like to thank Drs. Christine Olson and Carol Devine of the Division of Nutritional Sciences at Cornell University for their insight throughout manuscript writing.
Felice JP, Geraghty SR, Quaglieri CW, Yamada R, Wong AJ, Rasmussen KM. “Breastfeeding” but not at the breast: Mothers' descriptions of providing pumped human milk to their infants via other containers and caregivers. Matern Child Nutr. 2017;13:e12425 10.1111/mcn.12425
REFERENCES
- Boo, N. Y. , Nordiah, A. J. , Alfizah, H. , Nor‐Rohaini, A. H. , & Lim, V. K. E. (2001). Contamination of breast milk obtained by manual expression and breast pumps in mothers of very low birthweight infants. Journal of Hospital Infection, 49, 274–281. [DOI] [PubMed] [Google Scholar]
- Clemons, S. N. , & Amir, L. H. (2010). Breastfeeding women's experience of expressing: A descriptive study. Journal of Human Lactation, 26, 258–265. [DOI] [PubMed] [Google Scholar]
- Cooper, A. R. , Barnett, D. , Gentles, E. , Cairns, L. , & Simpson, J. H. (2013). Macronutrient content of donor human breast milk. Archives of Disease in Childhood ‐ Fetal and Neonatal Edition, 98, F539–F541. [DOI] [PubMed] [Google Scholar]
- Eidelman, A. I. , Schanler, R. J. , Johnston, M. , Landers, S. , Noble, L. , Szucs, K. , … Onyema, N . (2012). Breastfeeding and the use of human milk. Pediatrics 129, e827‐e841. [DOI] [PubMed] [Google Scholar]
- Fein, S. B. , Labiner‐Wolfe, J. , Shealy, K. R. , Li, R. , Chen, J. , & Grummer‐Strawn, L. M. (2008). Infant Feeding Practices Study II: Study methods. Pediatrics, 122, S28–S35. [DOI] [PubMed] [Google Scholar]
- Felice, J. P. , & Rasmussen, K. M. (2015). Breasts, pumps and bottles, and unanswered questions. Breastfeeding Medicine, 10, 412–415. [DOI] [PubMed] [Google Scholar]
- Felice, J. P. , Geraghty, S. R. , Quaglieri, C. W. , Yamada, R. , Wong, A. J. , & Rasmussen, K. M. (2016). ‘Breastfeeding’ without baby: A longitudinal, qualitative investigation of how mothers perceive, feel about, and practice human milk expression. Maternal and Child Nutrition. doi: 10.1111/mcn.12426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- García‐Lara, N. R. , Escuder‐Vieco, D. , García‐Algar, O. , De laCruz, J. , Lora, D. , & Pallás‐Alonso, C. (2012). Effect of freezing time on macronutrients and energy content of breastmilk. Breastfeeding Medicine, 7, 295–301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heinig, M. J. , Nommsen, L. A. , Peerson, J. M. , Lonnerdal, B. , & Dewey, K. G. (1993). Energy and protein intakes of breast‐fed and formula‐fed infants during the first year of life and their association with growth velocity: The DARLING Study. The American Journal of Clinical Nutrition, 58, 152–161. [DOI] [PubMed] [Google Scholar]
- Hoddinott, P. , Britten, J. , McInnes, R. J. , Craig, L. , & Darwent, K. (2013). Significant others, situations and their influences on infant feeding. BMC Pregnancy & Childbirth, 13, 114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson, S. , Leeming, D. , Williamson, I. , & Lyttle, S. (2013). Maintaining the ‘good maternal body’: Expressing milk as a way of negotiating the demands and dilemmas of early infant feeding. Journal of Advanced Nursing, 69, 590–599. [DOI] [PubMed] [Google Scholar]
- Johnson, S. , Williamson, I. , Lyttle, S. , & Leeming, D. (2009). Expressing yourself: A feminist analysis of talk around expressing breast milk. Social Science & Medicine, 69, 900–907. [DOI] [PubMed] [Google Scholar]
- Kent, J. C. (2007). How breastfeeding works. Journal of Midwifery & Women's Health, 52, 564–570. [DOI] [PubMed] [Google Scholar]
- Keim, S. A. , Hogan, J. S. , McNamara, K. A. , Gudimetla, V. , Dillon, C. E. , Kwiek, J. J. , & Geraghty, S. R. (2013). Microbial contamination of human milk purchased via the Internet. Pediatrics, 132, e1227–e1235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimbro, R. (2006). On‐the‐job moms: Work and breastfeeding initiation and duration for a sample of low‐income women. Maternal and Child Health Journal, 10, 19–26. [DOI] [PubMed] [Google Scholar]
- Labiner‐Wolfe, J. , Fein, S. B. , Shealy, K. R. , & Wang, C. (2008). Prevalence of breast milk expression and associated factors. Pediatrics, 122, S63–S68. [DOI] [PubMed] [Google Scholar]
- Leeming, D. , Williamson, I. , Lyttle, S. , & Johnson, S. (2013). Socially sensitive lactation: Exploring the social context of breastfeeding. Psychology & Health, 28, 450–468. [DOI] [PubMed] [Google Scholar]
- Li, R. , Fein, S. B. , & Grummer‐Strawn, L. M. (2010). Do infants fed from bottles lack self‐regulation of milk intake compared with directly breastfed infants. Pediatrics, 125, e1386–e1393. [DOI] [PubMed] [Google Scholar]
- Li, R. , Magadia, J. , Fein, S. B. , & Grummer‐Strawn, L. M. (2012). Risk of bottle‐feeding for rapid weight gain during the first year of life. Archives of Pediatrics & Adolescent Medicine, 166, 431–436. [DOI] [PubMed] [Google Scholar]
- Li, R. , Fein, S. B. , Chen, J. , & Grummer‐Strawn, L. M. (2008). Why mothers stop breastfeeding: Mothers' self‐reported reasons for stopping during the first year. Pediatrics, 122, S69–S76. [DOI] [PubMed] [Google Scholar]
- Meedya, S. , Fahy, K. , & Kable, A. (2010). Factors that positively influence breastfeeding duration to 6 months: A literature review. Women and Birth, 23(4) 135–145. [DOI] [PubMed] [Google Scholar]
- Rasmussen, K. M. , & Geraghty, S. R. (2011). The quiet revolution: Breastfeeding transformed with the use of breast pumps. American Journal of Public Health, 101, 1356–1359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rojjanasrirat, W. , & Sousa, V. D. (2010). Perceptions of breastfeeding and planned return to work or school among low‐income pregnant women in the USA. Journal of Clinical Nursing, 19, 2014–2022. [DOI] [PubMed] [Google Scholar]
- Ryan, A. S. , Zhou, W. , & Arensberg, M. B. (2006). The effect of employment status on breastfeeding in the United States. Women's Health Issues, 16, 243–251. [DOI] [PubMed] [Google Scholar]
- Soto‐Ramírez, N. , Karmaus, W. , Zhang, H. , Davis, S. , Agarwal, S. , & Albergottie, A. (2013). Modes of infant feeding and the occurrence of coughing/wheezing in the first year of life. Journal of Human Lactation, 29, 71–80. [DOI] [PubMed] [Google Scholar]
- Thulier, D. , & Mercer, J. (2009). Variables associated with breastfeeding duration. Journal of Obstetric, Gynecologic, & Neonatal Nursing, 38, 259–268. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services , Health Resources and Services Administration (HRSA) , Maternal and Child Health Bureau . (2008). Employees' guide to breastfeeding and working. Every Mother, Inc. and Rich Winter Design and Multimedia. pp. 3–5.
- U.S. Department of Health and Human Services . (2011). Executive summary: The surgeon general's call to action to support breastfeeding. Breastfeeding Medicine, 6, 3–5. [DOI] [PubMed] [Google Scholar]
- Whitaker, R. C. , & Wright, J. A. (2012). Why feed breast milk from a bottle. Archives of Pediatrics & Adolescent Medicine, 166, 483–484. [DOI] [PubMed] [Google Scholar]
- Wojcik, K. Y. , Rechtman, D. J. , Lee, M. L. , Montoya, A. , & Medo, E. T. (2009). Macronutrient analysis of a nationwide sample of donor breast milk. Journal of the American Dietetic Association, 109, 137–140. [DOI] [PubMed] [Google Scholar]
- Wright, P. , Fawcett, J. , & Crow, R. (1980). The development of differences in the feeding behaviour of bottle and breast fed human infants from birth to two months. Behavioural Processes, 5, 1–20. [DOI] [PubMed] [Google Scholar]


