Abstract
We report a case of cerebral venous thrombosis related to the ingestion of tadalafil. A 45-year-old man presented with posterior headache and was diagnosed with tension headache. Five days later, he was transported to our hospital via ambulance due to a tonic-clonic seizure. Head MRI showed cerebral venous thrombosis (CVT). He confessed to having recently taken a large doses of tadalafil. His anti-cardiolipin antibody and anti-caldiolipin-β2-glycoprotein-I complex antibody levels were elevated. Our case suggests the possibility that tadalafil is related to both cardiovascular complications and CVT in patients with hypercoagulability. Patients with conditions associated with hypercoagulability, including antiphospholipid syndrome may be better advised to avoid the use of tadalafil.
Keywords: antiphospholipid antibody syndrome, headache, cerebral venous thrombosis, tadalafil
Introduction
Thrombosis of the cerebral veins is a relatively uncommon disorder but it has the potential to cause fatal complications. It often affects young adults and children. The usual causes include thrombophilia, pregnancy or the use of the contraceptive pill (1,2). We herein describe the development of cerebral venous thrombosis after the ingestion of tadalafil, a phosphodiesterase inhibitor, by a patient with antiphospholipid syndrome (APS).
Case Report
A 45-year-old man presented to a walk-in clinic in our hospital with a 3-day history of severe sudden-onset posterior headache, which was exacerbated in the upright position. A tentative diagnosis of tension headache or cerebrospinal fluid hypovolemia was made and he was sent home. Three days later, he was transported to another hospital after experiencing a generalized tonic-clonic seizure and wasreferred back to our hospital. On examination, he had mild consciousness disturbance and increased deep tendon reflexes.
A blood test showed an elevated D-dimer level of 2.7 μg/mL. Contrast-enhanced head CT revealed a low density lesion of the parietal lobe (Fig. 1) and brain MRI indicated brain edema and thrombosis of the cortical veins (Fig. 2, 3). A diagnosis of cerebral venous thrombosis was made and treatment with heparin and fosphenytoin was initiated. The day after admission, his consciousness improved and he claimed that he had personally imported tadalafil and that he had occasionally taken it at a larger dose (40 mg per day) than the recommend daily dose (20 mg per day) in the 6 months prior to the onset of his symptoms. He had been using tadalafil to treat erectile dysfunction. The patient reported that he did not have sexual contact on the day prior to the onset of his headache.
Figure 1.

Contrast-enhanced head CT revealed a low-density lesion of the parietal lobe; a high-density area can be seen at the right cortical veins.
Figure 2.
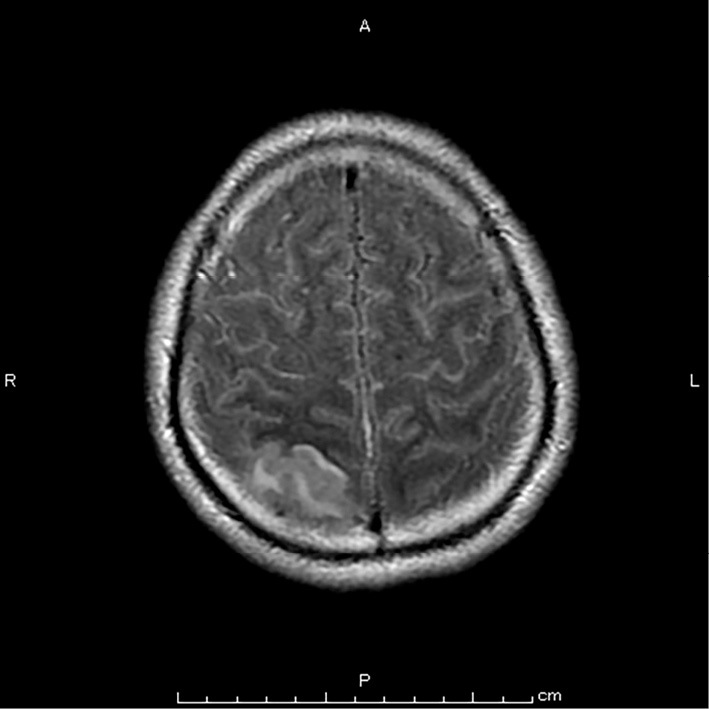
Fluid-attenuated inversion-recovery magnetic resonance imaging revealed a lesion of high signal intensity in the right parietal area, indicating brain edema.
Figure 3.
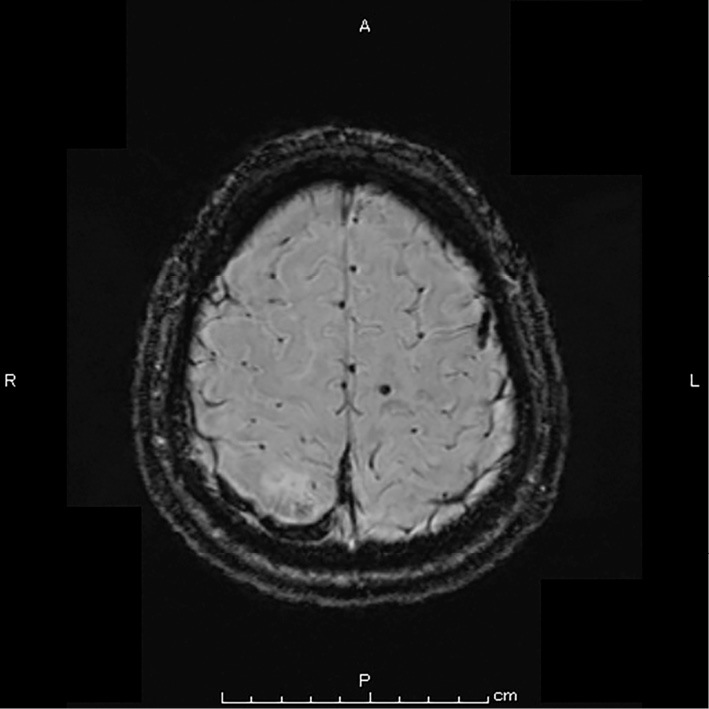
Susceptibility weighted imaging (SWI) revealed a lesion with a low signal intensity in the right cerebral cortical veins, and enlargement indicating cerebral venous thrombosis.
His anti-cardiolipin (aCL) antibody (14 U/mL; normal range <10 U/mL) and anti-caldiolipin-β2-glycoprotein-I (aCL ・ β2GPI) complex antibody (11 U/mL; normal range <3.5 U/mL) levels were elevated. He was discharged on day 15 after a full recovery from his symptoms. At the 3-month follow-up clinic visit, his aCL antibody and aCL ・ β2GPI complex antibody levels remained elevated at 7.8 U/mL and 15 U/mL, respectively. Warfarin treatment was initiated. At the time of his most recent follow-up visit, there had been no recurrence of thrombosis and he had not experienced any complications.
Discussion
Our case may suggest that tadalafil has the potential to cause cerebral venous thrombosis in patients with APS. APS can be drug-induced or idiopathic and can develop secondarily to autoimmune disorders (e.g., systemic lupus erythematosus). Our case did not have any symptoms or signs suggestive of autoimmune disorders that could lead to APS. Drug-induced APS is rarely reported (3). However, the aCL antibody and aCL β2GPI complex antibody levels of our patient remained elevated, even after the discontinuation of tadalafil. Thus, the APS in our patient might have been idiopathic.
To our knowledge, there had been no reported cases in which cerebral venous thrombosis was possibly caused by tadalafil. However, tadalafil and sildenafil have been prescribed worldwide as treatments for erectile dysfunction. These medications have been suggested to be associated with rare but serious adverse events, such as ischemic stroke (4). One previous report described a case of pulmonary embolism after taking tadalafil in a patient with protein C deficiency (5). The exact mechanism underlying the development of cerebral venous thrombosis following tadalafil is unclear. However, tadalafil, a phosphodiesterease-5 inhibitor, can cause temporary hypotension via transient vasodilatation and thus may induce low intracranial venous pressure and a subsequent low flow state, which may lead to an increased risk of venous thrombosis. Additional studies may be needed to investigate the effects of this drug. We suggest that patients with hypercoagulability may need to avoid the use of tadalafil.
The authors state that they have no Conflict of Interest (COI).
References
- 1.Stam J. Thrombosis of the cerebral veins and sinuses. N Engl J Med 352: 1791-1798, 2005. [DOI] [PubMed] [Google Scholar]
- 2.Piazza G. Cerebral venous thrombosis. Circulation 125: 1704-1709, 2012. [DOI] [PubMed] [Google Scholar]
- 3.Krischock L, Horsfield C, D'Cruz D, Rigden SPA. Drug-induced lupus and antiphospholipid syndrome associated with cysteamine therapy. Nephrol Dial Transplant 24: 1997-1999, 2009. [DOI] [PubMed] [Google Scholar]
- 4.Stefanović-Budimkić M, Jovanović DR, Beslać-Bumbaširević L, Ercegovac MD. Recurrent ischemic stroke associated with sildenafil and tadalafil use in a young adult. Clin Neurol Neurosurg 114: 405-407, 2012. [DOI] [PubMed] [Google Scholar]
- 5.Chen HC, Wang CS, Chuang SH, Wang CY. Pulmonary embolism after tadalafil ingestion. Pharm World Sci 30: 610-612, 2008. [DOI] [PubMed] [Google Scholar]


