Abstract
Stable, homotypic mutants of Chlamydia trachomatis for which MICs of rifampin and rifalazil are elevated were isolated by serial passage at sub-MIC concentrations of these compounds. An alternative approach, in which Chlamydia cells were incubated and subsequently passaged three times, all in the presence of the selective agent at concentrations above the MIC, appeared to be a more effective means of selecting for mutants. In every instance where an elevation in the MIC occurred, one or more mutations in the rpoB gene, encoding the rifampin binding site, were detected. With one exception, all rpoB mutants that contained a single mutation conferred lower levels of resistance than mutants containing multiple mutations. Some rpoB mutations conferred very high levels of resistance to rifampin, up to 512 μg/ml. In all cases, mutants remained susceptible to concentrations of rifalazil at or below 0.064 μg/ml. Thus, rifalazil, a compound that is extremely potent against Chlamydia wild-type cells (MIC of 0.00025 μg/ml), may also protect against the selection of mutants at physiologically achievable concentrations.
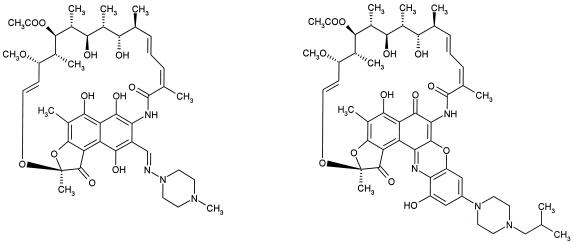
Rifalazil [3′-hydroxy-5′-(4-isobutyl-1-piperazinyl) benzoxazinorifamycin] is one of the newest generation of ansamycins (Fig. 1), compounds that inhibit bacterial RNA polymerases isolated from a wide variety of microorganisms. The ansamycins rifampin, rifabutin, and rifapentine have been utilized clinically predominantly as components of multiple-drug therapy, most commonly to treat tuberculosis (TB) patients (12). Rifalazil, otherwise known in the literature as KRM-1648 and, more recently, as ABI-1648, was originally developed by Kaneka Corporation, Osaka, Japan, through phase II clinical trials as an improved antimycobacterial agent to replace rifampin in the multidrug regimen for the treatment of TB (3, 12).
FIG. 1.
Chemical structures of ansamycins. The structure of rifampin is shown on the left; the structure of rifalazil is shown on the right.
However, rifalazil also has extraordinary potency against both Chlamydia pneumoniae (6, 11) and Chlamydia trachomatis (11, 14). MICs have been reported in the range between 0.0025 and 0.00025 μg/ml, depending on some variation in methodology. All of the studies were in agreement that rifalazil was considerably more potent in cell culture than any compound that has advanced to human clinical trials. The MICs of rifalazil were reported to be 50 to 500 times lower than azithromycin, the standard of care for urogenital infections caused by C. trachomatis or respiratory infections caused by C. pneumoniae. Studies in an acute respiratory mouse model suggest potent activity in vivo (6). In addition, experiments in which susceptibility is tested by exposing Chlamydia to a compound, followed by three compound-free passages, suggest that rifalazil uniquely eradicates Chlamydia in cell culture (14).
Taken together with the possibility that Chlamydia may have the capability of persisting after standard treatment (2), these results suggest that rifalazil could be a very promising agent to treat chlamydial infections. However, one factor that could play a decisive role in its success or failure is the development of resistance. Rifampin has been generally limited to combination therapy in the treatment of TB and gram-positive infections due to the emergence of resistance caused by mutations in the rpoB gene, which are selected for during monotherapy. The RpoB protein is one of the large subunits of the core bacterial RNA polymerase and contains the rifampin binding site, recently described by X-ray diffraction studies (1). Evaluation of clinical isolates indicates that rifalazil shares with rifampin the loss of activity against some strains that are highly resistant to rifampin, including both Mycobacterium tuberculosis (7, 10, 18, 19) and Staphylococcus aureus (16, 17). Furthermore, the recent report of the selection of stable homotypic mutants of C. trachomatis that are resistant to high concentrations of rifampin following multiple passages of C. trachomatis serovar K in cell culture in the presence of the drug indicate that RNA polymerase mutants may arise in the clinical setting (4). Given the propensity of rifampin to select for mutants, clinicians have been reluctant to utilize rifampin in therapy to treat C. trachomatis, despite its activity in cell culture (13). Therefore, we initiated a study to determine the potential for resistance to develop when Chlamydia is exposed to rifalazil and rifampin in cell culture. Our goals were to compare the frequency of mutant selection of the two compounds and to determine the MICs of rifalazil and rifampin for resistant mutants.
MATERIALS AND METHODS
Organisms.
The laboratory reference strain C. trachomatis serovar L2 (L2/434/BU) was used.
Antimicrobial susceptibility testing.
MICs were tested by inoculating Chlamydia strains onto monolayers of the McCoy cell line on 96-well microtiter plates as described previously (15). Cells were maintained in antimicrobial-free growth medium consisting of minimal essential medium with 10% fetal bovine serum and 220 mg of l-glutamine/liter added. The inoculum size of infectious chlamydial forms was 10,000 to 50,000 inclusion-forming units (IFU) per well. Within 30 min of addition of Chlamydia cells, the monolayer was centrifuged by using a Beckman model J-6 M centrifuge at 1,200 × g for 1 h at 37°C, a procedure which can increase the efficiency of infection for particular serovars of C. trachomatis. Following the removal of supernatant, the same growth medium containing 1 μg of cycloheximide/ml and the appropriate concentration of rifampin or rifalazil was applied in a volume of 100 μl. Cells were incubated at 37°C in 4% CO2 for 48 h and fixed with methanol. Chlamydial inclusions were detected by fluorescence with a genus-specific monoclonal antibody CF-2 (Washington Research Foundation, Seattle). Rifampin (Sigma) and rifalazil (provided by ActivBiotics, Inc.) were prepared by solubilization in dimethyl sulfoxide to 10 mg/ml and then appropriate dilution in growth medium.
Strain purification.
The wild-type C. trachomatis L2 and mutant derivatives were purified by making twofold dilutions in cell culture to the limit of detection of Chlamydia particles. The lowest dilution that resulted in the appearance of inclusions was assumed to originate from a single bacterium or a limited number of bacteria that were genetically identical.
Making wild-type preparations.
Four independent wild-type preparations, 1 to 4, were made by purifying our wild-type stock by limiting dilution as described above and growing out 4 wild-type clones. This procedure assures that independent mutants are isolated from each preparation.
Selection for resistance. (i) Selection for resistance of Chlamydia by serial passages with methods 1 and 2.
Four isolates of C. trachomatis serovar L2/432 cloned by limiting dilution were individually passed in 75-cm2 flasks onto monolayers of McCoy cells without centrifugation. After 2 h at 37°C, with agitation every 20 min, the infected monolayer was overlaid with growth medium containing one-half the MIC of either rifampin or rifalazil. After 48 h of incubation, the monolayer was lysed, debris was removed by slow-speed centrifugation, half of the supernatant was reinoculated on a fresh McCoy monolayer in 75-cm2 flasks, and the process was repeated at one-half the MIC. In the initial infection, a total of 3 × 107 mammalian cells in the monolayer was infected with a total of 3 × 108 IFU of C. trachomatis at a multiplicity of infection of 10. The number of viable IFU transferred at each subsequent passage was dependent on the number of surviving and/or resistant Chlamydia cells resulting from the inhibitory effect of the selective agent at each passage. Survival and/or resistance was monitored at each passage by testing for MICs in parallel cultures with monolayers in 48-well microtiter plates. To maintain a concentration of one-half the MIC, the concentration of the selective agent at the initiation of each passage was suitably elevated as resistant Chlamydia cells emerged by using the MIC determined on the 48-well monitoring plate. Passages were discontinued once maximum resistance was observed (i.e., MIC of rifampin of 512 μg/ml).
As resistance emerged, mutants were either cloned by limiting dilution (method 1) or left as a mixed population (method 2) and inoculated onto monolayers in 75-cm2 flasks and overlaid with one-half the resistant MIC of appropriate drug. These passages were repeated until the highest attainable level of resistance was reached (i.e., resistance to 512 μg of rifampin/ml). Azithromycin was passed at one-half the MIC as a control for one cloned L2 isolate.
(ii) Method 3.
To select more effectively for resistance with rifalazil as the selective agent, the vial passage method, similar to the MCC3 method described previously (15), was employed. Cloned L2 isolates were inoculated onto monolayers of McCoy cells in 12-mm2 shell vials at an approximate multiplicity of infection of 25 (a total of 107 IFU of C. trachomatis). Serial twofold dilutions of either rifampin or rifalazil in growth medium were overlaid onto inoculated monolayers. The highest concentrations for rifampin and rifalazil were 0.064 μg/ml. MICs were monitored on corresponding wells of a 96-well plate to observe emerging resistance. Plates were stained and read at 48 h, and vials were passed onto new shell vial monolayers and overlaid with previous corresponding drug concentrations. After three passages under the influence of appropriate serial twofold drug concentrations, vials positive for C. trachomatis growth were cloned by limiting dilutions and MICs were determined.
DNA sequencing of the rpoB gene.
Standard PCR methods and sequencing were used to determine the DNA sequence of the rpoB gene in wild-type and mutant strains. Using the GenBank sequence of C. trachomatis serovar D as a guide, both strands of the entire 3,756-bp rpoB gene plus 390 bp of the promoter of the parent L2 strain were sequenced from PCR products directly without interim cloning by using the appropriate primers shown in Table 1. The parent (wild type) L2 strain contained polymorphisms compared to C. trachomatis D at codons 520 (CTG-CTA, neutral), 572 (GAT-AAT, D changed to N), and 577 (CCC-CCT, neutral). The entire rpoB gene of one mutant isolated after 20 passages in the presence of rifalazil for preparation 2 (see Table 4) was also sequenced, and only one codon change, from isoleucine to methionine at codon 517 (I 517 → M), was revealed. For all other resistant mutants, both strands of the amplification were sequenced with the primers RpoBCTD5 and RpoBCTD3. This region of the rpoB gene encodes amino acids 442 to 644, a segment that is well known to encompass the vast majority of mutations conferring resistance to rifampin.
TABLE 1.
Characteristics of primers used for PCR amplification and sequencing
| Primer | Sequence (5′-3′) | Positiona | Fragment length (bp) |
|---|---|---|---|
| Rpo1 | GTG CTA AGG CTG TTG CTA AAG | −390 | 909 |
| Rpo2 | AGC TTC TAA CCA ACT TCC TCG | +519 | |
| Rpo3 | TTT CTC AAG TCC ACC GTT CTC | +407 | 958 |
| Rpo4 | TTG AGA ACG GCT GAA GAA ATC | +1365 | |
| RpoBCTD5 | CTC CAG GAA AGA TTA TTT CTG C | +1298 | 655 |
| RpoBCTD3 | CCC TTC TAA TCC AGT TCC AAC | +1953 | |
| Rpo5 | ACA TGC AAC GGC AGG CTG TAC | +1886 | 996 |
| Rpo6 | AAA TCA ACT AGC GAC TCT CTT TC | +2882 | |
| Rpo7 | TAC ACC GTC GTT CGG CAG ATA | +2789 | 967 |
| Rpo8 | AGC ATC TAC TAC CAT AGG GCG | +3756 |
Position is given according to the initiation of the translation codon ATG.
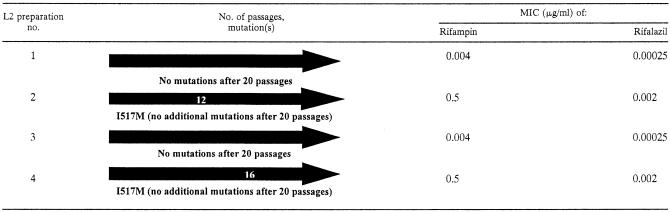
TABLE 4.
Evolution of mutant selection with rifalazil by method 2
RESULTS
Mutant selection by serial passages of Chlamydia in the presence of rifampin.
To select for mutants resistant to rifampin, C. trachomatis L2 bacterial preparations 1 to 4 were tested for resistance development by using methods 1 and 2 detailed in Materials and Methods. DNA sequencing of the rpoB gene directly from passages indicated the mutation responsible for an elevation in MIC. In all cases, mutants were also purified by limiting dilution prior to DNA sequencing, so that the predominant clone would be assessed after each observed elevation in the MIC.
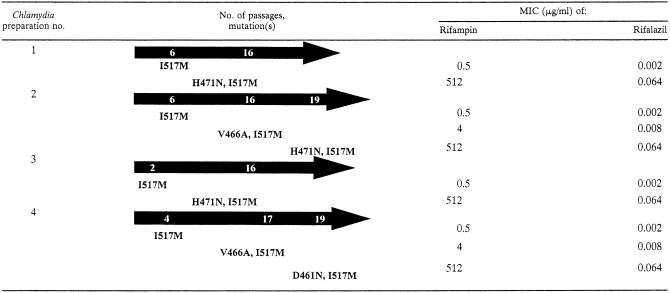
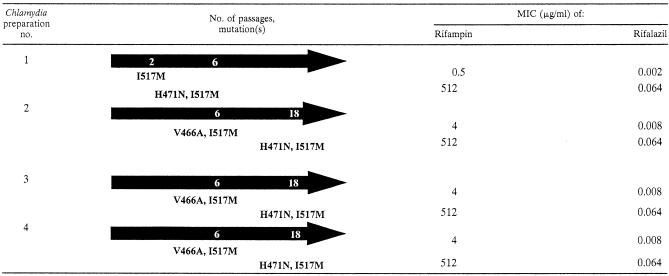
Using the methods described above, mutants for which MICs of rifampin were elevated were readily detected. Mutants were initially observed at passage 6, 6, 2, or 4 for preparations 1 to 4, respectively (Table 2), or at passage 2, 6, 6, or 6 from preparations 1 to 4, respectively (Table 3). The MIC of rifampin for the parent strain was 0.008 μg/ml. The MICs for the initial mutants were either 0.5 μg/ml (mutants with an I 517 → M change in RpoB) or 4 μg/ml (when the I 517 → M change was found in combination with a second mutation of V 466 → A).
TABLE 2.
Evolution of mutant selection with rifampin by method 1
TABLE 3.
Evolution of mutant selection with rifampin by method 2
We planned to carry out each serial experiment for 20 passages, but when rifampin was the selective agent, no experiment was carried out beyond 19 passages because the maximum level of resistance (512 μg/ml) had already been reached. This highest level of resistance was caused by the acquisition of a second mutation, either D 461 → N or H 471 → N, in combination with I 517 → M. In one case (Table 3), the maximum MIC was reached after just 6 passages. Clearly the selection of mutant strains occurs with relative facility with either method 1 or method 2.
The rpoB mutations appeared to be stable even in the absence of selective pressure. Both MICs and DNA sequence modifications were monitored directly from passages as well as after strain purification by limiting dilution. This purification procedure results in the propagation of mutants for a total of 1010 bacterial generations in drug-free conditions (10-ml preparations containing ∼109 IFU of C. trachomatis per ml in the absence of rifampin). We observed good agreement before and after purification by limiting dilution, in both the MIC and DNA sequence determinations, which suggests that these mutants are stable.
The MICs of rifalazil against the mutant clones were found to be unexpectedly low in all cases (Tables 2 and 3). Single lesions led to a rise in MIC from 0.00025 μg/ml to just 0.002 μg/ml, whereas the MIC for strains with multiple mutations rose to the range of 0.008 to 0.064 μg/ml, depending on the genotype.
Selecting for resistant mutants with rifalazil as the selective agent.
Because there was a marked difference in the MICs of rifampin and rifalazil for the mutants, the question as to whether rifalazil would select for mutants with equal frequency as rifampin became a more compelling issue. Indeed, when Chlamydia was exposed to rifalazil, mutant selection occurred at lower frequency (Table 4), even with method 2, which allows for any combination of multiple mutations during the 20 passages of constant selection at one-half the MIC. In two instances (preparations 1 and 3), no increase in MIC was detected after 20 passages. In the other two experiments, mutants containing a single lesion were selected at passages 12 and 16 from inocula from preparations 2 and 4, respectively. After 20 passages, the MIC of rifalazil for the survivors was 0.002 μg/ml. However, the MIC of rifampin for these same survivors had increased to 0.5 μg/ml, leaving no doubt that a mutant strain had taken over the culture. DNA sequencing showed the presence of the I 517 → M mutation in each case.
Selecting for mutants by serial passages at sub-MIC concentrations of rifalazil did not result in a high frequency of mutant selection. Therefore, we attempted to isolate mutants by serial passages in the presence of higher concentrations of rifalazil. Using method 3 (see Materials and Methods), Chlamydia was exposed to three successive passages at a fixed, higher drug concentration, regardless of the detection of inclusion bodies in the previous passage. One mutant strain was selected following exposure and passage at 0.032 μg/ml, considerably above the MIC of rifalazil (Table 5). Method 3 was indeed a more efficient process for selecting rifalazil-resistant mutants, in that an elevated MIC was detected approximately 50% of the time after three passages. It should be noted that fewer Chlamydia cells were transferred in method 3. Thus, it appears that use of rifalazil concentrations higher than the MIC enhances the chances of obtaining rifalazil-resistant mutants.
TABLE 5.
Selection of mutants by method 3
| L2 preparation no. | Selective agent | Selection concn (μg/ml) | Mutation at Escherichia coli (C. trachomatis) location designation:
|
|||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 507 (R453) | 516 (D461) | Not reported (V466) | 522 (A467) | 526 (H471) | 572 (I517) | MIC (μg/ml) of:
|
||||
| Rifampin | Rifalazil | |||||||||
| 1, 2, 3, 4 | None | 0.008 | 0.00025 | |||||||
| 1 | Rifalazil | 0.00025 | I517M | 0.5 | 0.002 | |||||
| 0.0005 | I517M | 0.5 | 0.002 | |||||||
| 0.001 | I517M | 0.5 | 0.002 | |||||||
| 0.002 | I517M | 0.5 | 0.002 | |||||||
| 0.032 | H471N | I517M | 512 | 0.064 | ||||||
| 2 | Rifalazil | 0.00025 | H471L | I517M | 512 | 0.064 | ||||
| 0.0005 | R453P | 0.5 | 0.002 | |||||||
| 0.001 | I517M | 0.5 | 0.002 | |||||||
| 0.008 | H471L | 64 | 0.032 | |||||||
| 3 | Rifalazil | 0.00025 | I517M | 0.5 | 0.002 | |||||
| 0.001 | H471N | 16 | 0.016 | |||||||
| 0.002 | I517M | 0.5 | 0.002 | |||||||
| 0.004 | H471L | 64 | 0.032 | |||||||
| 4 | Rifalazil | 0.00025 | I517M | 8 | 0.008 | |||||
| 0.002 | H471Y | 64 | 0.032 | |||||||
| 2 | Rifampin | 0.064 | V466A | A467T | I517M | 64 | 0.032 | |||
| 2 | Rifampin | 0.064 | H471N | I517M | 512 | 0.064 | ||||
| 2 | Rifampin | 0.05 | V466A | I517M | 4 | 0.008 | ||||
When rifalazil was the selective agent, the acquisition of a single mutation tended to result in only low-level resistance to rifalazil, 0.002 μg/ml, with the exceptions of mutations at position 471 when method 3 was used. The H471 → N mutation resulted in an MIC of 0.016, whereas the H471 → L and H471 → Y mutations resulted in a MIC of 0.032 μg/ml (Table 5). Mutants with multiple mutations were observed with method 3 when rifalazil was the selective agent (H 471 → N with I 517 → M and H 471→ L with I 517 → M). Multiple mutations were also observed when rifampin was used to select (again H 471→ N with I 517 → M, V 466 → A with I 517 → M, and the triple mutant V 466 → A, A 467 → T, and I 517 → M) (Table 5). When multiple mutations were selected with method 3, the rifalazil MIC still did not rise above 0.064 μg/ml, whereas the MIC of rifampin was considerably higher, up to 512 μg/ml.
Correlation of mutant genotypes and phenotypes.
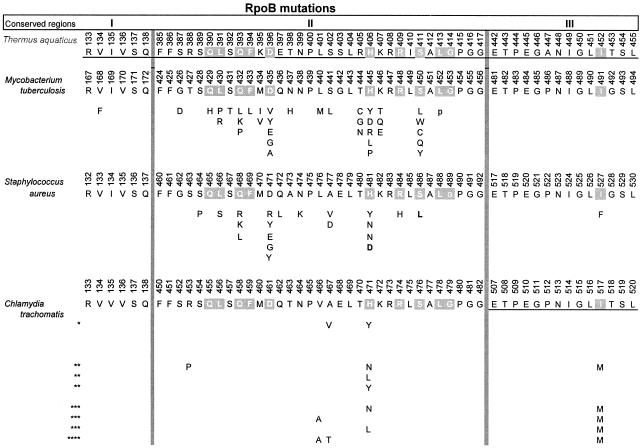
Figure 2 shows the location of all rpoB mutations described in this study, aligned with lesions identified previously in Chlamydia (4) and with homologous positions of the rpoB genes of rifampin-resistant M. tuberculosis and S. aureus clinical isolates. As anticipated, there is a strong overlap in the location of mutations in Chlamydia and in these other resistant organisms, within the well-conserved region of rpoB encoding the rifampin binding site (1).
FIG. 2.
Amino acid substitutions conferring rifampin resistance in C. trachomatis. Positions in RpoB resulting in resistance to rifampin of clinical isolates of M. tuberculosis (7, 10, 18, 19) and S. aureus (16, 17) as well as laboratory isolates of S. aureus (9) are shown within the conserved regions of RpoB known to be involved in resistance to rifampin. The C. trachomatis mutated RNA polymerases are as follows: *, single amino acid changes reported previously; **, single changes observed in this study; ***, double amino acid changes from this study; ****, triple amino acid changes from this study. The sequence of the rifampin binding site determined from the X-ray crystal structure with Thermus aquaticus RpoB is shown. The residues known to contact rifampin are shown with a grey background and are conserved in all sequences shown.
Table 6 shows the genotypic changes of all mutants and their phenotypic changes with regard to susceptibility to rifampin and rifalazil. In all cases, mutations conferred a large change in the MIC of rifampin. Even a single nucleotide change invariably led to an increase in the rifampin MIC of 64-fold or more. In contrast, the increase in MIC of rifalazil was approximately eightfold, except for the H 471 → L and H 471 → Y mutations, which led to a more substantial increase. When higher levels of resistance were obtained, multiple mutations were usually present. In the case of rifampin, multiple mutations led to MICs from 4 to 512 μg/ml, whereas the MIC of rifalazil did not increase above 0.064 μg/ml, regardless of the presence of single, double, or triple mutations in the rpoB gene.
TABLE 6.
Summary of ansamycin-resistant mutants
| Nucleotide change(s) in rpoB | Amino acid change | Selective agent | Method no. | MIC (μg/ml) of:
|
Mutant/wild type MIC ratio for:
|
Rifampin/rifalazil MIC ratio | ||
|---|---|---|---|---|---|---|---|---|
| Rifampin | Rifalazil | Rifampin | Rifalazil | |||||
| None | None | None | None | 0.008 | 0.00025 | 32 | ||
| ATT → ATG | I 517 → M | Rifampin and rifalazil | 1, 2, 3 | 0.5 | 0.002 | 64 | 8 | 256 |
| CGT → CCT | R 453 → P | Rifalazil | 3 | 0.5 | 0.002 | 64 | 8 | 256 |
| CAC → CTC | H 471 → L | Rifalazil | 3 | 64 | 0.032 | 8,192 | 128 | 2,048 |
| CAC → TAC | H 471 → Y | Rifalazil | 3 | 64 | 0.032 | 8,192 | 128 | 2,048 |
| CAC → AAC | H 471 → N | Rifalazil | 3 | 16 | 0.016 | 2,048 | 64 | 1,024 |
| CAC → AAC | H 471 → N | Rifampin and rifalazil | 1, 2, 3 | 512 | 0.064 | 65,535 | 256 | 8,192 |
| ATT → ATG | I 517 → M | |||||||
| GAT → AAT | D 461 → N | Rifampin | 1 | 512 | 0.064 | 65,535 | 256 | 8,192 |
| ATT → ATG | I 517 → M | |||||||
| GTC → GCC | V 466 → A | Rifampin | 1, 2, 3 | 4 | 0.008 | 512 | 32 | 512 |
| ATT → ATG | I 517 → M | |||||||
| CAC → CTC | H 471 → L | Rifalazil | 3 | 512 | 0.064 | 65,535 | 256 | 8,192 |
| ATT → ATG | I 517 → M | |||||||
| GTC → GCC | V 466 → A | Rifampin | 3 | 64 | 0.032 | 8,192 | 128 | 2,048 |
| GCA → ACA | A 467 → T | |||||||
| ATT → ATG | I 517 → M | |||||||
DISCUSSION
Rifalazil has potential uses in treating acute and chronic bacterial infections caused by Chlamydia (urogenital infections, pelvic inflammatory disease, prevention of tubal infertility, trachoma, and possibly atherosclerosis). These possibilities make the best use of rifalazil's attributes (12), including high potency against C. trachomatis and C. pneumoniae, high intracellular concentrations, long half-life (possibly providing a prolonged protective advantage in the single-dose treatment of sexually transmitted diseases), and lack of P450 interaction (which contrasts with rifampin, a P450 inducer) (8).
Development of resistance is also an important consideration for any chemotherapeutic agent. In S. aureus, mutations in the rpoB gene can result in high levels of resistance to rifampin, probably from a single nucleotide change, and some of these mutant clinical isolates are also highly resistant to rifalazil (16, 17). Although rifampin is one of the most potent anti-S. aureus drugs against susceptible strains, the specter of resistant subpopulations has relegated rifampin to a combination drug for the treatment of serious gram-positive infections or for prophylaxis when the bioburden is minimal, so that the existence of a resistant subpopulations would not be a major risk. To assess the potential issue of resistance development in Chlamydia, in this work, we studied the nature and appearance of mutations in the rpoB gene following selection with rifampin and rifalazil.
Chlamydia strains present formidable obstacles in genetic studies because they are not amenable to genetic engineering (cloning and transformation, etc.), and furthermore, Chlamydia organisms are obligate intracellular pathogens. Even the isolation of a single bacterium, which is accomplished by streaking free-living bacteria on agar plates, is not straightforward for Chlamydia. To assemble a collection of independently isolated resistant mutants, selections for resistant bacteria were carried out with four wild-type preparations by using the limiting dilution procedure to make sure that each wild-type preparation originated from a single wild-type bacterium or a low number of genetically identical wild-type bacteria, as described in Materials and Methods. Thus, in each of the four wild-type preparations, resistant mutants were independently generated as a result of errors in DNA replication during the growth of each preparation. Mutants were considered to be stable because MICs and DNA sequence changes in rpoB remained constant whether measured from passages or after extensive growth in drug-free medium during strain purification (data not shown).
When rifampin was the selective agent in passaging experiments, a sequence of mutational events was observed (Tables 2 and 3). The I 517 → M mutation occurred first, leading to a low level of resistance (MIC of rifampin of 0.5 μg/ml). Then a transiently observed V 466 → A mutation was found in combination with I 517 → M, resulting in an intermediate level of resistance (MIC of rifampin of 4 μg/ml). Subsequently, with the exposure to higher rifampin concentrations, mutants carrying the V 466 → A lesion were replaced by mutants carrying either the H 471 → N change or the D 461 → N change in combination with I 517 → M, conferring the high resistance (rifampin MIC of 512 μg/ml).
Using methods 1 to 3, we detected a total of eight different mutations within six codons in the rpoB gene (Fig. 2; Table 6). Mutations arose several independent times at codon 471 as well as at codon 517. In addition, a mutation altering codon 453 was observed once. Mutations in codons 461, 466, and 467 appeared only in combination with other mutations (Fig. 2). Mutations in positions 461, 466, and 467 appear to affect resistance because the MICs for combination mutants were higher than that of the isogenic strain carrying the wild-type allele at positions 461, 466, and 467. Mutations at positions 453, 461, 466, 467, 471, and 517 have been reported in other species at the corresponding codon positions (Fig. 2). In addition, Dreses-Werringloer et al. previously described the isolation of stable rifampin-resistant mutants of C. trachomatis with alterations in codons 467 and 471 (4).
Our investigation of C. trachomatis mutants in cell culture suggests a clear potential benefit of rifalazil over rifampin with regard to resistance development. Specifically, (i) the frequency of mutant selection was much reduced when rifalazil rather than rifampin was the selective agent, and (ii) mutants containing up to three lesions in rpoB and mutants that conferred total resistance to rifampin remained susceptible to rifalazil.
Rifalazil has greater potency against Chlamydia than rifampin, which is in contrast to the equivalent MICs that rifampin and rifalazil have against some gram-positive pathogens such as S. aureus (5). The results showing that rifalazil retains activity against Chlamydia strains that are resistant to rifampin was unanticipated, particularly in light of the cross-resistance of a high proportion of clinical isolates of both S. aureus (16, 17) and M. tuberculosis (7, 10, 18, 19) to both rifampin and rifalazil. It would be most interesting to isolate RNA polymerase from wild-type and mutant cells to determine whether rifalazil's special potency is related to increased affinity to its target.
Acknowledgments
We thank Marcia Osburne for critically reading the manuscript, Chris Murphy for information and assistance provided for Fig. 2, Christo Shalish for computer skills in making Tables 2 to 4, and John Van Duzer for work on Fig. 1.
REFERENCES
- 1.Campbell, E. A., N. Korzheva, A. Mustaev, K. Murakami, S. Nair, A. Goldfarb, and S. A. Darst. 2001. Structural mechanism for rifampicin inhibition of bacterial RNA polymerase. Cell 104:901-912. [DOI] [PubMed] [Google Scholar]
- 2.Dean, D., R. J. Suchland, and W. E. Stamm. 2000. Evidence for long-term cervical persistence of Chlamydia trachomatis by omp1 genotyping. J. Infect. Dis. 182:909-916. [DOI] [PubMed] [Google Scholar]
- 3.Dietze, R., L. Teixeira, L. M. Rocha, M. Palaci, J. L. Johnson, C. Wells, L. Rose, K. Eisenach, and J. J. Ellner. 2001. Safety and bactericidal activity of rifalazil in patients with pulmonary tuberculosis. Antimicrob. Agents Chemother. 45:1972-1976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dreses-Werringloer, U., I. Padubrin, L. Kohler, and A. P. Hudson. 2003. Detection of nucleotide variability in rpoB in both rifampin-sensitive and rifampin-resistant strains of Chlamydia trachomatis. Antimicrob. Agents Chemother. 47:2316-2318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fujii, K., A. Tsuji, S. Miyazaki, K. Yamaguchi, and S. Goto. 1994. In vitro and in vivo antibacterial activities of KRM-1648 and KRM-1657, new rifamycin derivatives. Antimicrob. Agents Chemother. 38:1118-1122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kuo, C.-C., J. T. Grayston, T. Hidaka, and L. M. Rose. 1997. A comparison of the in vitro sensitivity of Chlamydia pneumoniae to macrolides and a new benzoxazinorifamycin, KRM-1648, p. 317-321. In S. H. Zinner, L. S. Young, J. F. Acar, and H. C. Neu (ed.), Expanding indications for the new macrolides, azalides, and streptogramins. Infectious disease and therapy series, vol. 21. Marcel Dekker, New York, N.Y.
- 7.Moghazeh, S. L., X. Pan, T. Arain, C. K. Stover, J. M. Musser, and B. N. Kreiswirth. 1996. Comparative antimycobacterial activities of rifampin, rifapentine, and KRM-1648 against a collection of rifampin-resistant Mycobacterium tuberculosis isolates with known rpoB mutations. Antimicrob. Agents Chemother. 40:2655-2657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Niemi, M., J. T. Backman, M. F. Fromm, P. J. Neuvonen, and K. T. Kivisto. 2003. Pharmacokinetic interactions with rifampicin: clinical relevance. Clin. Pharmacokinet. 42:819-850. [DOI] [PubMed] [Google Scholar]
- 9.Oliva, B., A. O'Neill, J. M. Wilson, P. J. O'Hanlon, and I. Chopra. 2001. Antimicrobial properties and mode of action of the pyrrothine holomycin. Antimicrob. Agents Chemother. 45:532-539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Park, Y. K., B. J. Kim, S. Ryu, Y. H. Kook, Y. K. Choe, G. H. Bai, and S. J. Kim. 2002. Cross-resistance between rifampicin and KRM-1648 is associated with specific rpoB alleles in Mycobacterium tuberculosis. Int. J. Tuberc. Lung Dis. 6:166-170. [PubMed] [Google Scholar]
- 11.Roblin, P. M., T. Reznik, A. Kutlin, and M. R. Hammerschlag. 2003. In vitro activities of rifamycin derivatives ABI-1648 (rifalazil, KRM-1648), ABI-1657, and ABI-1131 against Chlamydia trachomatis and recent clinical isolates of Chlamydia pneumoniae. Antimicrob. Agents Chemother. 47:1135-1136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rothstein, D. M., A. D. Hartman, M. H. Cynamon, and B. I. Eisenstein. 2003. Development potential of rifalazil. Expert Opin. Investig. Drugs 12:255-271. [DOI] [PubMed] [Google Scholar]
- 13.Schachter, J. 1983. Rifampin in chlamydial infections. Rev. Infect. Dis. 5(Suppl. 3):S562-S564. [DOI] [PubMed] [Google Scholar]
- 14.Stamm, W. E., W. M. Geisler, and R. J. Suchland. 2002. Assessment of antimicrobial resistance in Chlamydia trachomatis strains associated with treatment failure or same strain recurrence, p. 353-360. In Chlamydial infections: Proceedings of the 10th International Symposium on Human Chlamydial Infections. Basim Yeri: GRAFMAT Basim ve Reklam Sanayi Tic. Ltd. Sti., Antalya, Turkey.
- 15.Suchland, R. J., W. M. Geisler, and W. E. Stamm. 2003. Methodologies and cell lines used for antimicrobial susceptibility testing of Chlamydia spp. Antimicrob Agents Chemother. 47:636-642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wichelhaus, T. A., V. Schafer, V. Brade, and B. Boddinghaus. 1999. Molecular characterization of rpoB mutations conferring cross-resistance to rifamycins on methicillin-resistant Staphylococcus aureus. Antimicrob. Agents Chemother. 43:2813-2816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wichelhaus, T. A., V. Schafer, V. Brade, and B. Boddinghaus. 2001. Differential effect of rpoB mutations on antibacterial activities of rifampicin and KRM-1648 against Staphylococcus aureus. J. Antimicrob. Chemother. 47:153-156. [DOI] [PubMed] [Google Scholar]
- 18.Williams, D. L., L. Spring, L. Collins, L. P. Miller, L. B. Heifets, P. R. Gangadharam, and T. P. Gillis. 1998. Contribution of rpoB mutations to development of rifamycin cross-resistance in Mycobacterium tuberculosis. Antimicrob. Agents Chemother. 42:1853-1857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yang, B., H. Koga, H. Ohno, K. Ogawa, M. Fukuda, Y. Hirakata, S. Maesaki, K. Tomono, T. Tashiro, and S. Kohno. 1998. Relationship between antimycobacterial activities of rifampicin, rifabutin and KRM-1648 and rpoB mutations of Mycobacterium tuberculosis. J. Antimicrob. Chemother. 42:621-628. [DOI] [PubMed] [Google Scholar]