Abstract
This study sought to investigate the clinical efficacy of arthroscopic refreshing treatment of anterior cruciate ligament (ACL) injury combined with stable medial meniscus ramp injury. Sixty-eight patients treated between January 2010 and January 2014 were included, and their clinical data were retrospectively analyzed. All patients, after being treated using ACL reconstruction, were divided into 2 groups according to meniscus injury treatment method. The observation group (31 cases) was treated by arthroscopic refreshing, which removed the tissue on both sides of the tear edge using a cutting knife, while the control group (37 cases) was treated using Fast-fix sutures. All patients were followed up for at least 24 months. Surgical duration, postoperative function recovery time, and hospital stay for patients in the observation group were significantly shorter than for those of the control group (P<0.05). Both groups showed significant post-operative improvement for Lysholm scores, IKDC scores, and average knee range of motion at 12 and 24 months post-operation (P<0.05), but no significant differences between groups were observed (P>0.05). Regarding the difference in movement range between the healthy and injured sides, both groups showed significant decrease post-operation (P<0.05). Ultimately, there was no significant difference in the recovery of ramp damage and objective symptoms between the two groups (P>0.05). Arthroscopic refreshing treatment of patients with anterior cruciate ligament injury combined with stable ramp lesion can achieve similar clinical curative effects as the Fast-fix suture, thereby providing a simple alternative for patient treatment worth popularizing.
Keywords: Anterior Cruciate Ligament Injury, Stable Medial Meniscus Ramp Injury, Arthroscopy, Refreshing, Fast-Fix Suture
Introduction
The anterior cruciate ligament (ACL) is a key structure involved in knee movement and maintenance of joint stabilization. Severe ACL injury not only leads to acute knee instability, but also may cause permanent lower limb paralysis[1]. Medial meniscus tears are common with ACL secondary injuries and a ramp injury is a common form of medial meniscus tear, caused mainly due to increased stress at the back edge of the medial meniscus. Ramp injuries, when severe, can lead to irreversible damage to the intra-articular cartilage[2]. Previous studies have shown that all-inside suture repair is excellent for unstable ramp injury[3-4]. However, stable ramp injuries are also present in patients when knee stability is restored and when there is relatively no significant activity at the edge of the medial meniscus tear. For patients with stable ramp injuries, refreshing the wound surface is most likely to heal the injury site and may obtain similar healing outcomes as all-inside suture repair. The aim of this study was to study the efficacy of arthroscopic refreshing treatment of ACL injuries where stable medial meniscus ramp injuries were present, and compare the efficacy to that of the fast-fix suture method.
Materials and methods
General patient information
Sixty-eight patients with ACL injury and arthroscopy-confirmed presence of medial meniscus ramp injury treated at the Hospital of Hebei University between January 2010 and January 2014 were analyzed retrospectively. Inclusion criteria were as follows: 1) unilateral injury; 2) maximal ramp tear of 1-2 cm; no movement of the meniscus tear free edge to the intercondylar fossa, as determined by intraoperative exploration probe hook, and stable ramp injury; 3) complete medical records and no separation within 2 years of follow-up. Exclusion criteria were as follows: 1) a bucket-handle tear of the medial meniscus within the ramp area; 2) ACL injury combined with multiple ligament injuries beyond medial collateral ligament injury; 3) knee joint bone abnormalities.
All patients underwent ACL reconstruction and were divided into two groups in accordance with the meniscal injury treatment received. The observation group were treated with arthroscopic refreshing of the surface of ramp injury, and was comprised of 31 patients (23 males and 8 females; 13 left knee injuries and 18 right knee) aged between 22 to 59 years (average age 34.8±8.1 years). Time from injury to surgery ranged from 3 to 133 d (mean 42.8±25.4 d). The control group were treated with arthroscopic fast-fix suture, and was comprised of 37 patients (28 males and 9 females; 15 left knee injuries and 22 right knee) aged between 20 to 56 years (average age 35.7±8.5 years). Time from injury to surgery ranged from 5 to 138 d (mean 45.2±28.1 d). There were no significant differences in sex, age, injury location, and time from injury to surgery between the two groups (P>0.05).
Treatment procedures
ACL reconstruction
The affected knee was placed at 90° flexion. A longitudinal 4 cm incision was made in the anterior tibia until the pes anserine (or goose foot) was exposed layer by layer in order to identify and excise 20 cm sections of the semitendinosus and gracilis tendons. The tendons were folded to form 4 strands, braided with No. 2 non-absorbable line, and attached to a loop on a steel plate waiting to be used as an autograft. A tibial tunnel was made at the ACL stump and an anatomical femoral tunnel was made extending to the center of the femoral trajectory center, followed by pulling the transplanted tendon from the tibial tunnel into the femoral tunnel. After completing the implantation, the femoral end was fixed with EndoButton and the tibial end was fixed with absorbable compression screws or portal nails in cases where meniscus injury had been treated first.
Fast-Fix meniscus suture
First, a routine observation of meniscus injury was performed to determine the necessity of suturing. The affected knee was placed at 60° flexion and the arthroscopic scope was inserted through the space between the posterior cruciate ligament and femoral medial condyle. The synovial membrane around the arthroscope was cleaned with a planer and the correct alignment of the fusion site was ensured. The knee was adjusted to a flexion of 10-20°, correcting the joint valgus and keeping the medial compartment open. A meniscus depth probe was used to determine the depth of puncture in order to select the appropriate length of the cutting puncture depth limiter. Then the needle was inserted, initially with a protection sheath, which was withdrawn after reaching the suturing position. Then the suture needle was placed perpendicular to the tearing edge of the meniscus in order to puncture the medial portion of the meniscus tearing edge and further the lateral part of the puncture tear until the depth limiter reached the meniscus surface. The suture needle was withdrawn and the first suture anchor was placed in a predetermined position. Stitching with a second needle was then initiated with the second stapling anchor in the ready position, and stiches were administered at a distance of 4 to 5 mm from the first stitch. After the second suture anchor had been placed, the delivery needle was removed, the knot was pushed with the knot pusher, the thread end was managed with a suture cutter, and finally the suture was cut.
Wound refreshing treatment
In accordance with Fast-fix technology protocols, the arthroscope was placed through the transcondylar space and the two sides of the tear were refreshed with a planing knife based on a criteria where a rough wound was formed at both sides of the tear.
Postoperative treatment
A postoperative routine was performed to prevent infection and control thrombosis. The affected knee was dressed with elastic bandage under pressure and ice treatment was applied immediately. A focus was placed on muscle strength training, activity training, anti-adhesion training, and anti-thrombotic exercise from 0-4 weeks after surgery. Patients began partial weight-bearing at around the 8th week, and full weight-bearing training was initiated at 12 weeks when knee flexion began to reach 100°. Squatting was strictly prohibited after surgery and normal exercise was restored six months after surgery.
Follow-up assessments
Surgery efficacy was assessed by comparing operation time, functional activity recovery time, and length of hospital stay between the two groups. All the patients were followed up for at least 24 months, and knee function was assessed using the Lysholm and IKDC scales at 12 and 24 months after surgery. The Lysholm scale evaluates eight topics, all of which are associated with the meniscus, ligaments, and articular cartilage, making it a simple and comprehensive evaluator of knee function. Higher scores indicate better function of the knee with a 100-point score suggesting no limitation with daily activities and the absence of symptoms. The IKDC score is aggregated using 10 questions, and is used to assess anterior cruciate ligament injuries with high sensitivity and reliability. With 100 points as the maximal score, a higher IKDC score represents better knee function. Patient knee flexion and the difference between affected and contralateral knees were recorded at the last follow-up. The difference between the contralateral and healthy sides were calculated using the Lachman test. During the follow-up period, MRI was used to evaluate meniscus ramp injury healing and to evaluate knee joint interlocking, swelling, joint space tenderness, and McMurray test results.
Statistical methods
Data were analyzed by SPSS19.0 and measurement data were expressed as (±s). Multi-point comparison was performed using repeated measures analysis of variance. Paired t-test was used to compare pre- and post-treatment measurements within one group. Independent Samples t-test was used for comparing two independent groups. For calculating composition ratios of count data, rank sum test and chi-square test was utilized. P value <0.05 was considered as statistically significant.
Results
Comparison of surgical results between the two groups
The surgical duration, functional activity recovery time, and hospital stay were significantly shorter in the observation group than in the control group (p<0.05, Table I).
Table I.
Comparison of surgical results between the two groups (x̄±s).
| Group (n) | Surgical duration (min) | Functional recovery time (d) | Hospital stay (d) |
|---|---|---|---|
| Observation (31) | 50.2±8.5 | 21.7±5.2 | 4.1±1.8 |
| Control (37) | 66.5±7.3 | 25.8±6.4 | 5.6±2.1 |
| t | -7.142 | -2.385 | -2.610 |
| P | 0.000 | 0.027 | 0.012 |
Pre- and post-surgical Lysholm scores
Lysholm scores in both groups increased significantly post-surgery (p<0.05), but no significant differences was observed between the two groups at any of the time points (p>0.05, Table II).
Table II.
Lysholm scores before and after surgery in two groups (x̄±s, score).
| Group (n) | Before surgery | 12 months after surgery | 24 months after surgery |
|---|---|---|---|
| Observation (31) | 64.2±6.3 | 87.7±10.5 | 90.3±8.7 |
| Control (37) | 66.2±5.6 | 88.2±7.1 | 90.5±5.8 |
| F time point, P | 75.482, <0.001 | ||
| F time point × group, P | 2.077, 0.148 | ||
| F group, P | 0.109, 0.742 |
IKDC scores before and after surgery.
IKDC scores were increased significantly (p<0.05), but there was no interaction between time points and group (p>0.05). Moreover, there were no significant differences at different time points between the two groups (p>0.05, Table III).
Table III.
IKDC scores before and after surgery in the two groups (x̄±s, score).
| Group (n) | Before surgery | 12 months after surgery | 24 months after surgery |
|---|---|---|---|
| Observation (31) | 64.2±6.3 | 83.5±3.7 | 85.1±4.2 |
| Control (37) | 66.2±5.6 | 83.0±3.5 | 85.9±4.0 |
| F time point, P | 255.412, <0.001 | ||
| F time point × group, P | 0.057,0.848 | ||
| F group, P | 0.019,0.890 |
Knee range of motion before and after surgery and the difference between the contralateral and affected sides
Knee range of motion was significantly improved at last follow-up in both groups (p<0.05) and the difference between the contralateral and affected side were significantly decreased in both groups (p<0.05). However, no significant differences at different time points between the two groups were noted (p>0.05, Table IV).
Table IV.
Knee range of motion before and after surgery in the two groups and the difference between the contralateral and affected side (x̄ ± s)
| Group (n) | Range of motion for affected knee (°) | Difference between contralateral and affected side (mm) | ||
|---|---|---|---|---|
| Before surgery | Last follow-up | Before surgery | Last follow-up | |
| Observation (31) | 66.7±4.7 | 125.4±7.9* | 6.7±1.4 | 1.4±0.9* |
| Control (37) | 65.9±5.2 | 127.1±9.5* | 6.5±1.3 | 1.3±0.7* |
| t | 0.660 | -0.793 | 0.610 | 0.515 |
| P | 0.511 | 0.430 | 0.545 | 0.608 |
= p <0.001 compared with pre-surgery.
Recovery of objective symptoms
At the last follow-up, two patients in the observation group and three patients the control group had tenderness in the medial joint space. All of the patients recovered well after the conservative treatment. Recovery of ramp injury was excellent without the presence of knee interlocking, swelling, and tenderness in the joint space for all patients except the five mentioned above. Moreover, the McMurray test was negative for all patients. There was no significant difference in objective symptoms presentation between the two groups (p>0.05).
MRI results
All patients underwent MRI examination before operation to confirm clear ramp injury. At 12 months after surgery, all patients underwent MRI review, and 18 patients in the observation group, as well as 21 patients in the control group, were found to have healed completely. There was no statistically significant difference in healing efficacy between the two groups (p>0.05). All patients with grade III MRI signals were treated with the same secondary arthroscopic procedure as the previous treatment, showing reliable final therapeutic effects. There was no significant difference between the two groups in MRI examination results at 1 year after operation (p>0.05, Table V).
Table V.
Comparison of MRI reexamination results between the two groups.
| Group (n) | Normal (%) | Grade I signal (%) | Grade II signal (%) | Grade III signal (%) |
|---|---|---|---|---|
| Observation (31) | 18 (58.1) | 4 (12.9) | 5 (16.1) | 4 (12.9) |
| Control (37) | 21 (56.8) | 7 (18.9) | 5 (13.5) | 4 (10.8) |
| Z | -0.082 | |||
| P | 0.934 |
A typical case analysis
XX Jia was a 47 year old male patient. [Figure 1A] indicates the results from the preoperative MRI diagnosis, with the white arrow indicating the ramp tear signal. [Figure 1B] presentes the result of the anterolateral approach during surgery, with the white arrow indicating that the meniscus could not be pulled into the intercondylar fossa, suggesting that the stability of the posterior horn of the meniscus. [Figure 1C] presents the results of the postoperative arthroscopic review after one year, showing good meniscus wound healing.
Figure 1.
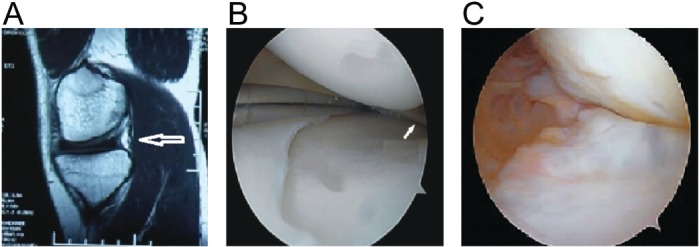
Images for a typical case: A: Preoperative MRI showed ramp tear (white arrow). B: Intraoperative exploration showed stability of the posterior horn of the meniscus and the hook could not enter the intercondylar fossa (white arrow). C: Arthroscopic review one year after surgery showed the complete healing of the ramp injury.
Discussion
ACL injury is often associated with medial meniscus ramp injury. Liu X et al[5] reported that the incidence rate of ramp injury was around 16.59% in patients with ACL injury and that incidence rate increased significantly with prolonged injury time in males, and that those under the age of 30 were more prone to ramp injury. The main reason for the meniscus ramp injury is due to damage to the complete 8-character structure of the meniscus and cruciate ligament. Therefore, even in the absence of recent meniscus injury, the loss of knee movement regularity will lead to secondary meniscus injury, which will further affect patient knee function.
Previous studies did not distinguish whether ramp injuries were stable or not, and thus often resulted in the conclusion that Fast-fix suture technology could achieve reliable clinical efficacy. Miller et al[6] reported that 15 patients undergoing Fast-fix suture treatment recovered back to pre-surgical conditions in term of mobility, such as normal knee flexion function and absence of pain while walking. Tucciarone et al[7] also showed that Fast-fix technology was more effective than meniscectomy in the treatment of patients with ACL injury combined with ramp injury. However, the results of this study showed that refreshing the tear edge by debriding and grinding the wound was able to obtain similar clinical efficacy as Fast-fix technology in the treatment of stable ramp injury. Our conclusion was supported by the following observations. First, the Lysholm and IKDC scores in the observation group were close to those of the control group at 12 and 24 months after operation. Moreover, the range of motion at last follow-up, as well as the difference between the contralateral side and the affected side, were similar between groups. These data suggested that knee joint function recovery was similar. Second, the recovery of objective symptoms at last follow-up and MRI examination results at 12 months after surgery were similar in the two groups, indicating that the objective repair of ACL injury and ramp injury were close in the two groups. Therefore, for stable ramp injury at the medial meniscus, the wound refreshing treatment is both feasible and effective. On the other hand, although the Fast-fix technique is a new meniscus suturing method and its procedure has been relatively standardized and fixed, it is still complicated to perform[8]. Under the guidance of this study, for patients with stable ramp injury of the medial meniscus, a singular treatment using arthroscopic wound refreshing helps to simplify the operation procedure and ensures better patient prognosis.
The possible underlying mechanism for excellent efficacy of the refreshing treatment may be because the tear present in ramp injury is on the edge of the meniscus, where there is sufficient blood supply. Meanwhile, relatively little movement is present around the tear of stable ramp injury after knee stability recovery, allowing the meniscus a great opportunity to heal post-treatment. Nepple JJ et al[9] reported that the refreshing treatment alone can effectively promote the healing for small-sized meniscus tears, which is consistent with the conclusion of this study. Another advantage of the sole refreshing treatment is that it can greatly simplify the operation and reduce surgical trauma. In this study, the surgical duration in the observation group was remarkably shorter than that of the control group, and hospitalization and functional activity recovery time were also significantly and consistently shorter, which could be due to the decreased additional trauma on patients as a result of a simplified surgical procedure.
This study indicates that prior to repairing meniscus ramp injury, it is necessary to determine whether the injury is stable via arthroscopic exploration during ACL reconstruction. In ACL reconstruction, it is required to observe the posterior horn of the medial meniscus using a conventional anterior and anterolateral approach to the knee, and to examine meniscus stability through an arthroscopic hook[10]. A stable injury can be confirmed when no movement of the free edge of the meniscus tear to the intercondylar fossa is present.
In summary, for patients suffering from ACL combined with stable medial meniscal injuries, arthroscopic refreshing the meniscus tear during ACL injury reconstruction is able to achieve similar clinical efficacy with meniscus suture technology. This finding potentially simplifies operational procedures, and is thus worth spreading.
Footnotes
The authors have no conflict of interest. This study was supported by Science and Technology Research Development Program of Hebei Province of China (No. 072761417).
Edited by: P. Lyritis
References
- 1.Schmitt A, Batisse F, Bonnard C. Results with all-inside meniscal suture in pediatrics [J] Orthop Traumatol Surg Res. 2016;102(2):207–211. doi: 10.1016/j.otsr.2015.12.018. [DOI] [PubMed] [Google Scholar]
- 2.Hengtao T, Xuntong S. Arthroscopic repair of the meniscal injury using meniscal repair device [J] Indian J Orthop. 2015;49(5):510–515. doi: 10.4103/0019-5413.164047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Thaunat M, Fayard JM, Guimaraes TM, Jan N, Murphy CG, Sonnery-Cottet B. Classification and surgical repair of ramp lesions of the medial meniscus. Arthrosc Tech. 2016;5:e871–e875. doi: 10.1016/j.eats.2016.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Li WP, Chen Z, Song B, et al. The FasT-Fix Repair Technique for Ramp Lesion of the Medial Meniscus [J] Knee Surg Relat Res. 2015;27(1):56–60. doi: 10.5792/ksrr.2015.27.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Liu X, Feng H, Zhang H, Hong L, Wang XS, Zhang J. Arthroscopic prevalence of ramp lesion in 868 patients with anterior cruciate ligament injury. Am J Sports Med. 2011;39:832–837. doi: 10.1177/0363546510388933. [DOI] [PubMed] [Google Scholar]
- 6.Miller MD, Kline AJ, Gonzales J, Beach WR. Pitfalls associated with FasT-Fix meniscal repair. Arthroscopy. 2002;18:939–943. doi: 10.1053/jars.2002.36146. [DOI] [PubMed] [Google Scholar]
- 7.Tucciarone A, Godente L, Fabbrini R, Garro L, Salate SF, Chillemi C. Meniscal tear repaired with Fast-Fix sutures: Clinical results in stable versus ACL-deficient knees. Arch Orthop Trauma Surg. 2012;132:349–356. doi: 10.1007/s00402-011-1391-5. [DOI] [PubMed] [Google Scholar]
- 8.Liu X, Feng H, Zhang H, et al. Arthroscopic prevalence of ramp lesion in 868 patients with anterior cruciate ligament injury [J] Am J Sports Med. 2011;39(4):832–37. doi: 10.1177/0363546510388933. [DOI] [PubMed] [Google Scholar]
- 9.Nepple JJ, Dunn WR, Wright RW. Meniscal repair outcomes at greater than five years: a systematic literature review and meta-analysis [J] J Bone Surg Am. 2012;94(24):2222–2227. doi: 10.2106/JBJS.K.01584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.González-Fernendez ML, PLrez-Castrillo S, Sznchez-Lhzaro JA, et al. Assessment of regeneration in meniscal lesions by use of mesenchymal stem cells derived from equine bone marrow and adipose tissue [J] Am J Vet Res. 2016;77(7):779–788. doi: 10.2460/ajvr.77.7.779. [DOI] [PubMed] [Google Scholar]


