Abstract
Objectives
We used the National Joint Registry for England, Wales, Northern Ireland and the Isle of Man (NJR) to investigate the risk of revision due to prosthetic joint infection (PJI) for patients undergoing primary and revision hip arthroplasty, the changes in risk over time, and the overall burden created by PJI.
Methods
We analysed revision total hip arthroplasties (THAs) performed due to a diagnosis of PJI and the linked index procedures recorded in the NJR between 2003 and 2014. The cohort analysed consisted of 623 253 index primary hip arthroplasties, 63 222 index revision hip arthroplasties and 7585 revision THAs performed due to a diagnosis of PJI. The prevalence, cumulative incidence functions and the burden of PJI (total procedures) were calculated. Overall linear trends were investigated with log-linear regression.
Results
We demonstrated a prevalence of revision THA due to prosthetic joint infection of 0.4/100 procedures following primary and 1.6/100 procedures following revision hip arthroplasty. The prevalence of revision due to PJI in the three months following primary hip arthroplasty has risen 2.3-fold (95% confidence interval (CI) 1.3 to 4.1) between 2005 and 2013, and 3.0-fold (95% CI 1.1 to 8.5) following revision hip arthroplasty. Over 1000 procedures are performed annually as a consequence of hip PJI, an increase of 2.6-fold between 2005 and 2013.
Conclusions
Although the risk of revision due to PJI following hip arthroplasty is low, it is rising and, coupled with the established and further predicted increased incidence of both primary and revision hip arthroplasty, this represents a growing and substantial treatment burden.
Cite this article: E. Lenguerrand, M. R. Whitehouse, A. D. Beswick, S. A. Jones, M. L. Porter, A. W. Blom. Revision for prosthetic joint infection following hip arthroplasty: Evidence from the National Joint Registry. Bone Joint Res 2017;6:391–398. DOI: 10.1302/2046-3758.66.BJR-2017-0003.R1.
Keywords: Prosthetic joint infection, Hip arthroplasty, Time trend, Registry
Article focus
Hip prosthetic joint infection (PJI) is an uncommon, but serious, complication of hip arthroplasty.
Epidemiological evidence from the United Kingdom on revision for PJI is out of date and the majority of available studies are single-centre retrospective cohorts.
We identified no contemporary studies reporting the frequency or changes in use over time of single- and two-stage revision procedures.
Key messages
The overall risk of revision for PJI was 0.4% after primary total hip arthroplasty (THA) and 1.6% after aseptic revision THA.
Between 2005 and 2013, there was an increase in the risk of revision due to PJI in the three months following index THA, with no increase after three months.
The annual volume of revision hip procedures for treatment of PJI increased 2.6-fold between 2005 and 2013, with an increase in the use of single-stage revision from 18% in 2005 to 39% in 2014.
Strengths and limitations
The dataset on which this analysis was performed is one of the largest joint arthroplasty registers.
The recording of PJI as an indication for surgery is according to the opinion of the treating surgeon at the time of surgery. As such, the diagnosis has not necessarily been referenced against a benchmark set of criteria.
While the National Joint Registry now represents a mature dataset with long-term follow-up, there is still a substantial number of patients undergoing revision THA where there is no record of a linked primary THA.
Introduction
Hip prosthetic joint infection (PJI) is an uncommon, but serious, complication of hip arthroplasty,1 with an incidence of 0.6% to 2.2%.2-4 Analysis of national registry data from four Nordic countries between 1995 and 2009 demonstrated an increase in the proportion of primary hip arthroplasties revised for PJI.2 Evidence available from the United Kingdom is out of date and primarily derived from single-centre retrospective cohort studies.3,5
Surgical site infections can have a devastating effect on patients and these infections are sometimes fatal.6 PJI may be managed with surgical debridement, antibiotic treatment and implant retention with exchange of modular components (DAIR).7 This is commonly used for treatment of acute PJI with pathogens susceptible to antibiotics and in patients unfit for major surgery. However, lifelong suppressive antibiotic treatment may be required and 45% to 52% of patients receiving DAIR may subsequently need revision of their implants.8 Rates of revision of implants following treatment with DAIR may be lower with strict selection criteria,9 but larger single-centre cohort studies suggest that the rate of revision of implants is around 20% by two years.7 About half of patients who are diagnosed with PJI subsequently undergo major revision surgery.3,10 Single-stage or two-stage revision surgery may be undertaken. For many surgeons, the revision of hip arthroplasties for PJI by a two-stage approach is considered the benchmark11 but there is increasing support for a single-stage approach.12 Both interventions achieve eradication of infection in about 90% of cases in the two years following revision12 and are associated with significant morbidity and cost.13 We identified no contemporary studies reporting the frequency of use or changes in use over time of the different revision strategies.
We analysed the National Joint Registry for England, Wales, Northern Ireland and the Isle of Man (NJR), a large arthroplasty database established in April 2003,14 to obtain representative and contemporary evidence on the burden of revision surgery for hip PJI in England and Wales.
Our specific aims were to:
- describe the prevalence rates of revision surgery for the treatment of hip PJI and their time trends broken down by time from index surgery to revision for infection;
- describe the cumulative incidence functions;
- estimate the national burden of hip PJI at health service level by accounting for all of the revisions and re-revision surgeries performed for hip PJI registered in the NJR.
The above aims are reported by type of index surgery, i.e. primary or revision surgery for aseptic indications.
Materials and Methods
Data source
In this observational study, we report analyses of data from the NJR. The registry was established in 2003 and includes details of primary and revision hip arthroplasties performed in England and Wales. Data entry for Northern Ireland commenced in February 2013 and for the Isle of Man in 2015, and this data is therefore excluded from these analyses.
We grouped procedures as index surgeries and subsequent revision surgeries for the treatment of hip PJI. All index surgeries performed between 01 April 2003 and 31 December 2013 were included (to give a minimum 12-month follow-up). All revision surgeries performed as a consequence of PJI between 01 January 2003 and 31 December 2014 were considered.
Ethics approval and patient consent
Patient consent was obtained for data collection by the NJR. According to the specifications of the NHS Health Research Authority, separate informed consent and ethical approval were not required for the present study.
Index surgeries
Index surgeries included all primary procedures and all revision procedures performed for indications other than PJI. The index revision procedures have been labelled ‘aseptic revision’ procedures to indicate that they were not performed due to PJI as indicated on the NJR data collection forms. Revisions not performed for PJI but that were performed on a hip previously operated on due to PJI were excluded from the index surgery cases. Any procedure with infection as one of the reported indications for surgery on the data collection form was considered as a revision for PJI. Revision procedures were classified as a single-stage, a stage one of a two-stage revision, a stage two of a two-stage revision procedure, or a hip excision. DAIR procedures with modular exchange are recorded in the NJR dataset as single-stage revision procedures. To identify which procedures recorded as single-stage revisions were DAIRs with modular exchange, as opposed to complete single-stage revisions where implants fixed to bone are also revised, the component level data were examined for both the index and revision procedures where available. Procedures recorded as single-stage revisions where only modular components were added (‘liner’, ‘femoral head’ and/or ‘proximal stem component’) were defined as DAIRs with modular exchange. Those where implants fixed to bone were implanted (‘cup’, non-modular or non-proximal ‘stem component’) were defined as single-stage revisions. Debridements where the surgeon either elects not to exchange modular components when they are present or where modular exchange is not possible (e.g. with resurfacing or non-modular implants) are not captured in the NJR.
Statistical analysis
This was performed with Stata SE 14.2 (StataCorp LP, College Station, Texas).
Prevalence rates of index surgeries performed between 2003 and 2013, and subsequently revised for an indication of infection between 2003 and 2014, were derived by year and type of index surgery, i.e. primary or ‘aseptic revision’ surgeries: number of index surgeries revised for PJI/total of index surgeries x 1000. This provides a ‘surgeon perspective’ of revision for PJI by describing the proportion of hip arthroplasties which required revision surgery for the management of infection. The prevalence rates were then derived and plotted by time from index surgery to revision for infection (within three months, between three and six months, six months to one year, one to two years, two to three years, three to four years, and five to six years). This allowed the investigation of time trends in the revision for hip PJI in the short-, mid-, and long-term following index primary or aseptic revision hip arthroplasty. The time elapsed between the index and the revision surgery was derived as the difference in months or years between the recorded procedure dates. For two-stage surgeries, the recorded date of the stage one of a two-stage revision was selected to indicate the date of revision for PJI. Log-linear regression, using the year of index or revision surgery as a continuous independent factor, was used to investigate overall linear trends between 2005 and 2013. This period was selected as over 85% (proportion of procedure records submitted to the NJR compared with the levy returns for the number of implants sold) of hip arthroplasties performed in 2005, and over 99% of those performed from 2007 onwards, had been recorded in the NJR; prior to 2005, the data capture of the NJR was < 75%.15 When evidence of a time trend was identified (year of surgery, p ⩽ 0.05), the year of surgery was re-considered as a categorical variable using 2005 as the reference period. Estimated relative risk and related 95% confidence intervals (CI) quantified the relative increase in rates between the period of interest and 2005.
To move from a surgical perspective to a patient perspective, cumulative incidence functions were derived by type of index surgery (primary or aseptic revision).16-18 They provide the probability of being revised as a consequence of PJI within a specific time period following the index surgery, while accounting for the time patients were at risk of being revised for a PJI and the competing risks of death and revision for an aseptic indication.
The overall ‘burden of PJI’ was analysed using all documented revision procedures performed between 2003 and 2014 for an indication of PJI (rather than just those with a linked index procedure reported in the NJR), as well as any subsequent re-revision procedures in the cases, whether they were performed for PJI or another indication. This provides a ‘healthcare service perspective’ of revision for PJI. A total of 3634 patients had hip revision procedures performed between 2003 and 2014 for PJI when there was no index procedure recorded in the NJR. The overall burden was reported by the year and type of revision surgery. The stage one of a two-stage revision and stage two of a two-stage revision were considered to be one procedure to avoid double counting. The same strategy was also used to account for more than one first-stage revision of a two-stage revision procedure (i.e. more than one stage prior to the final stage of re-implantation).
Results
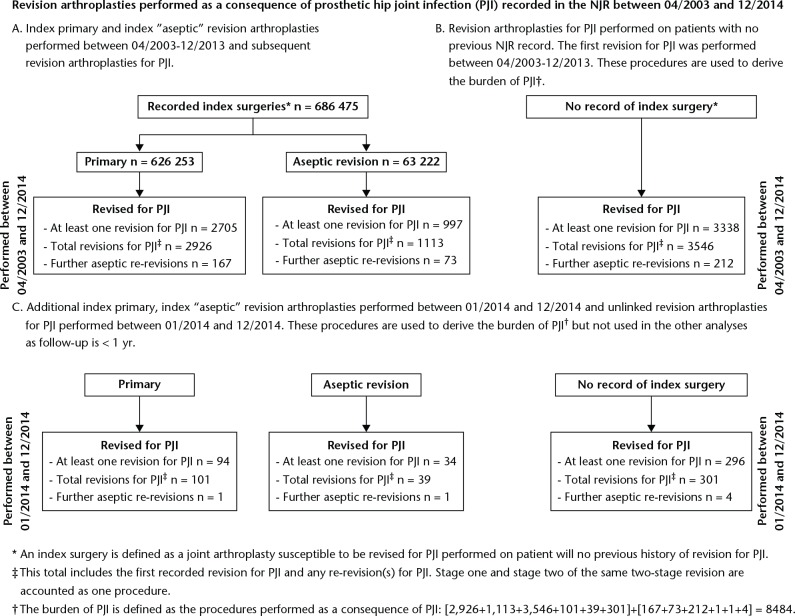
There were 623 253 primary and 63 222 aseptic revision hip arthroplasties (n = 686 475) recorded in the NJR between April 2003 and December 2013 (Table I). A total of 7040 patients required at least one revision surgery (7585 procedures) due to hip PJI between 2003 and 2014 (primary hip arthroplasty revised for PJI, n = 2705 (2926 procedures), aseptic revision re-revised for PJI, n = 997 (1113 procedures), revision for PJI but no index surgery recorded in the NJR, n = 3338 (3546 procedures)) (Fig. 1).
Table I.
Primary and aseptic revision arthroplasty procedures revised for a prosthetic hip joint infection (PJI)
| Primary | Aseptic revision | |||||
|---|---|---|---|---|---|---|
| Revised for PJI | Prevalence rate | Revised for PJI | Prevalence rate | |||
| N | n | Per 1000 procedures, 95% CI | N | n | Per 1000 procedures, 95% CI | |
| 2003 | 14 462 | 79 | 5.46 (4.26 to 6.66) | 1278 | 24 | 18.78 (11.34 to 26.22) |
| 2004 | 27 992 | 194 | 6.93 (5.96 to 7.90) | 2439 | 43 | 17.63 (12.41 to 22.85) |
| 2005 | 40 147 | 269 | 6.70 (5.90 to 7.50) | 3513 | 61 | 17.36 (13.04 to 21.68) |
| 2006 | 47 530 | 267 | 5.62 (4.95 to 6.29) | 4219 | 80 | 18.96 (14.85 to 23.08) |
| 2007 | 60 470 | 322 | 5.32 (4.74 to 5.91) | 5725 | 119 | 20.79 (17.09 to 24.48) |
| 2008 | 66 712 | 375 | 5.62 (5.05 to 6.19) | 6234 | 136 | 21.82 (18.19 to 25.44) |
| 2009 | 67 571 | 315 | 4.66 (4.15 to 5.18) | 6513 | 118 | 18.12 (14.88 to 21.36) |
| 2010 | 69 902 | 270 | 3.86 (3.40 to 4.32) | 7124 | 115 | 16.14 (13.22 to 19.07) |
| 2011 | 72 856 | 226 | 3.10 (2.70 to 3.51) | 8038 | 114 | 14.18 (11.60 to 16.77) |
| 2012 | 76 617 | 238 | 3.11 (2.71 to 3.50) | 9357 | 108 | 11.54 (9.38 to 13.71) |
| 2013 | 78 994 | 150 | 1.90 (1.60 to 2.20) | 8782 | 79 | 9.00 (7.02 to 10.97) |
| Total | 623 253 | 2705 | 4.34 (4.18 to 4.50) | 63 222 | 997 | 15.77 (14.80 to 16.74) |
CI, confidence interval.
Fig. 1.
Description of procedures recorded in the National Joint Registry (NJR).
Surgeon perspective
Around 0.43% (95% CI 0.42 to 0.45) of the primary hip arthroplasties recorded in the NJR were subsequently revised due to PJI and 1.58% (95% CI 1.48 to 1.67) of the aseptic revision hip arthroplasties were similarly revised due to PJI (Table I).
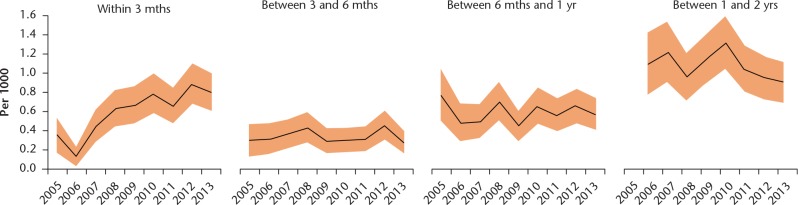
Figure 2 shows trends in primary surgeries revised for PJI within two years of the index surgery. The revision rates of a primary hip arthroplasty for PJI within three months of the index procedure increased over time, with the rate in 2013 twice that of the rate in 2005: rate ratio (RR) 2.29 (95% CI 1.28 to 4.08), time trend (likelihood ratio test, p < 0.0001). No evidence of time trends in the rates of revision within three to six months, six months to one year, and one to two years, was found between 2005 and 2013. The rates of late revision for PJI decreased over time (supplementary Fig. a): between two and three years (2011 compared with 2005), RR 0.52 (95% CI 0.32 to 0.84), time trend (likelihood ratio test, p < 0.0001); between three and four years (2010 compared with 2005), RR 0.49 (95% CI 0.31 to 0.80), time trend (likelihood ratio test, p = 0.001); and between four and five years (2009 compared with 2005), RR 0.44 (95% CI 0.27 to 0.73), time trend (likelihood ratio test, p = 0.028).
Fig. 2.
Prevalence (95% confidence intervals) of revision for prosthetic joint infection within two years of the index primary surgery.
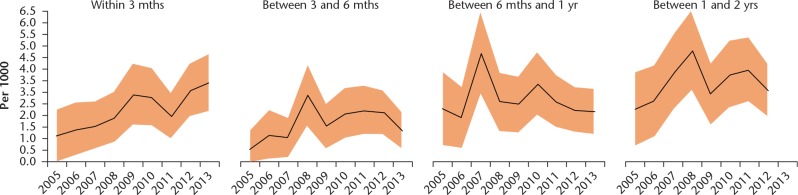
Figure 3 and supplementary Figure b show trends in aseptic revision surgeries revised for PJI. The proportion of aseptic revisions subsequently revised for PJI within three months of the procedure also increased over time, RR 3.00 (95% CI 1.06 to 8.51), time trend (likelihood ratio test, p = 0.002). No important differences were noted in the rates of revision for infection performed at any time beyond three months from the index revision surgery (all time trend, likelihood ratio test, p-values > 0.1).
Fig. 3.
Prevalence (95% confidence intervals) of revision for prosthetic joint infection within two years of the index aseptic revision surgery.
Patient perspective
Figure 4 shows the probability over time of revision for infection in patients with an index primary or aseptic revision while accounting for the time at risk of revision for infection, the risk of death and revision for any indication other than infection. The probability of revision for PJI at one year following a primary hip arthroplasty was 0.15% (95% CI 0.14 to 0.16) compared with 0.69% (95% CI 0.63 to 0.76) following an aseptic revision hip arthroplasty. At two years, the probability was 0.26% (95% CI 0.24 to 0.27) and 1.06% (95% CI 0.98 to 1.14) respectively. At five years, it was 0.44% (95% CI 0.42 to 0.46) and 1.77% (95% CI 1.66 to 1.89), respectively. The probability of revision for PJI within the first ten years following primary hip arthroplasty was 0.62% (95% CI 0.59 to 0.65). The ten-year probability following an aseptic revision was much higher, with up to 2.25% (95% CI 2.08 to 2.43) of those procedures subsequently revised for PJI.
Fig. 4.

Cumulative incidence function of revision for prosthetic joint infection following index primary and aseptic revision hip arthroplasty (CI, confidence interval).
Healthcare service perspective
Table II shows the revision surgeries performed after primary and aseptic revision hip arthroplasty index procedures by the year the revision for the management of PJI was performed. All revision surgeries are represented, including repeated procedures performed to manage PJI and any subsequent revision procedures performed thereafter for any indication. To estimate the burden of infection in 2014, revisions performed in 2014 as a consequence of PJI, which either relate to index surgeries performed in 2014 (n = 142) or cannot be linked to any index procedure (n = 305), were also included (Fig. 1). This represents an estimation of the annual burden attributable to hip PJI at the level of England and Wales, as most of those 8484 revisions could have been avoided if the infection had not occurred.
Table II.
Number of revision procedures (n, %) performed as a consequence of a prosthetic joint infection (PJI) by type and year of procedure*
| Year | n | DAIR | Single-stage | Two-stage | Excision |
|---|---|---|---|---|---|
| 2003 | 140 | 0 (0.0) | 69 (49.3) | 71 (50.7) | 0 (0.0) |
| 2004 | 270 | 1 (0.4) | 49 (18.1) | 207 (67.7) | 13 (4.8) |
| 2005 | 384 | 4 (1.0) | 60 (15.6) | 309 (80.5) | 11 (2.9) |
| 2006 | 491 | 5 (1.0) | 69 (14.1) | 399 (81.3) | 18 (3.7) |
| 2007 | 590 | 12 (2.0) | 80 (13.6) | 470 (79.7) | 28 (4.8) |
| 2008 | 748 | 19 (2.5) | 148 (19.8) | 558 (74.6) | 23 (3.1) |
| 2009 | 902 | 31 (3.4) | 168 (18.6) | 683 (75.7) | 20 (2.2) |
| 2010 | 899 | 35 (3.9) | 209 (23.3) | 629 (70.0) | 26 (2.9) |
| 2011 | 961 | 30 (3.1) | 248 (25.8) | 660 (68.7) | 23 (2.4) |
| 2012 | 1094 | 49 (4.5) | 298 (27.2) | 719 (65.7) | 28 (2.6) |
| 2013 | 1003 | 58 (5.8) | 264 (26.3) | 663 (66.1) | 18 (1.8) |
| 2014 | 1002 | 76 (7.6) | 298 (29.7) | 608 (60.7) | 20 (2.0) |
| Total | 8484 | 320 (3.8) | 1960 (23.1) | 5976 (70.4) | 228 (2.7) |
this table reports the revision procedures performed after any index surgery revised as a consequence of PJI, including subsequent re-revision procedures whether performed to manage an infection or not. It also includes the revision procedures performed between 2003 and 2014 on 3634 ‘infected’ patients with no index procedure documented in the National Joint Registry
The absolute number of procedures performed as a consequence of infection has increased from 384 in 2005 to 1002 in 2014, i.e. a relative increase of around 2.6. This is higher than the relative increase in volume of primary procedures observed over the same period (a two-old increase), but close to the increase in volume of index revision surgeries between 2005 and 2013 (8782 out of 3513, a 2.5-fold increase) (Table I). While around 70% of those revisions are two-stage, the relative weight of single-stage revisions for PJI has increased from 15.6% in 2005 to 29.7% in 2014. DAIR with modular exchange procedures represents less than 4% of the total burden for PJI reported in the NJR between 2003 and 2014, but their proportion has risen from < 1% in 2005 to nearly 4% in 2010 and 7.6% in 2014.
Overall, the median interval between stages of a two-stage revision following a primary index surgery was 105 days (25th and 75th percentiles interquartile range (IQR) 70 to 173). No evidence of significant temporal change was found, respectively 141 (IQR 111 to 203), 93 (IQR 58 to 173), and 117 (IQR 77 to 182) in 2005, 2009 and 2013. A median interval of 119 days (IQR 72 to 189) was observed for two-stage revision performed to manage PJI following an index aseptic revision surgery; no evidence of a trend over time was found, 147 (IQR 63 to 280), 120 (IQR 56 to 173), 139 (IQR 84 to 251).
Discussion
This study is the largest to date investigating the treatment of hip PJI, including 686 475 index primary and aseptic revision hip arthroplasty procedures and 7585 revision THAs performed due to a diagnosis of PJI. It has demonstrated that the probability of undergoing a revision for PJI is higher following aseptic revision hip arthroplasty than for primary hip arthroplasty, and that the risk of undergoing revision for PJI within three months of surgery has risen over time for primary and revision procedures. The majority of revisions performed for PJI are still two-stage procedures, but the use of single-stage revision is increasing. The total burden of treating PJI of the hip has risen substantially and this mirrors the rise in aseptic revision surgery recorded in the NJR rather than the increase in primary surgery over the period of observation.14
We have shown an elevated cumulative incidence rate of revision for PJI following aseptic revision hip arthroplasty (2.3% at ten years) compared with primary hip arthroplasty (0.6% at ten years). This is consistent with the findings of previous large cohort studies. In analyses of United States Medicare data, Mahomed et al19 and Zhan et al20 noted a four- to five-fold increased risk of wound infection within 90 days of surgery in patients with revision, compared with primary hip arthroplasty. Similarly, in a United States surgical registry, both Bohl et al21 and Pugely et al22 observed an approximate fourfold greater risk of deep infection in the first 30 days after revision, compared with primary hip arthroplasty.
Revision hip arthroplasty is performed in a population with increased host and procedure risk factors for infection or further revision,23 and involves prolonged operation time and also implantation of a greater volume of prosthetic material and adjuncts such as bone graft that may present a favourable environment for bacterial colonisation and subsequent PJI.24
We have demonstrated a substantial time trend of an increased risk of revision for PJI within the first three months of an index procedure being performed. In their analysis of the Nordic Arthroplasty Register Association dataset, Dale et al2 also noted increased revision rates due to hip PJI. Similar to our findings, the increased risk of revision was mainly in the three months after the primary index procedure. The trend for increased risk of early revision for hip PJI is likely to be multifactorial. Factors may include the increased accuracy of tests available to clinicians for the diagnosis of PJI,25 and the increased risk factors for PJI among the population undergoing hip arthroplasty such as elevated body mass index26 and increased bed occupancy.27 It may also represent a progression towards earlier recognition and/or treatment in specialist centres with a subsequent benefit in terms of reduced long-term PJI. There may be a trend towards the use of revision surgery to manage PJI rather than suppressive treatment with antibiotics but we cannot comment on this as non-surgical management of PJI is not captured in the NJR. Risk factors recorded in the Nordic registries could not account for the increase in early revision rates, suggesting that the trend could reflect an actual increase in the risk of early PJI.2
The current rate of surgical revision performed as a consequence of hip PJI is approximately 1000 cases/year across the NJR. This represents a significant healthcare burden which has more than doubled over the last decade. The cost of revision hip arthroplasty due to PJI is more than three times that of primary hip arthroplasty, and over twice that of aseptic revision.28 In the NHS, the cost is in excess of £20 000 per case, not accounting for the litigation costs.13 Single-stage revision offers an advantage over two-stage in both patient- and surgeon-derived utility values in the short and long term,29 suggesting that this increased burden could be mitigated by the increased use of single-stage revision.
We have identified an increased use of single-stage, as compared with two-stage, revision for hip PJI. Currently in the NJR, the only option to record DAIR with modular exchange procedures is to record them as single-stage revisions.30 This complicates their differentiation from single-stage surgeries where implants fixed to bone such as a acetabular component and stem (distal or non-modular) are revised. This represents a potential weakness of the data collection form as this may be subject to different interpretation by surgeons, despite the fact that recording of procedures in which any component is removed or inserted is mandatory. We have used component-level data for individual cases to identify DAIR procedures with modular exchange. A few single-stage revisions for PJI unlinked to an index procedure were considered as DAIRs in view of the components implanted (n = 43).
The importance of arthroplasty registries in identifying best clinical practice and improving health outcomes is recognised.31 The NJR is one of the largest joint arthroplasty registers, with comprehensive coverage of procedures undertaken, which is reassuring in terms of the generalisability of the data generated by the study. Issues relating to under-reporting, and thus potentially lower incidence estimates, are acknowledged.32 The data are prospectively entered into the registry and are observational which implies certain limitations. The recording of PJI as an indication for surgery is at the discretion of the treating surgeon at the time of surgery. As such, the diagnosis has not necessarily been referenced against a benchmark set of criteria and hence may be subject to misdiagnosis. Linkage to multiple other datasets, including those containing microbiology data and results, may improve the sensitivity and specificity of the diagnosis of PJI in these cases.33 While the NJR now represents a mature dataset with long-term follow-up, there is still a substantial number of patients undergoing revision hip arthroplasty with no record of a linked primary hip arthroplasty. As anonymised data were provided to us, it is difficult to determine to what extent this might be due to issues related to the patient identification and linkage to their related index procedures in the original dataset. This is reflective of the fact that some PJI revisions were performed in the early days of the registry and relate to index procedures performed prior to the start of the registry or at a time data capture was still improving but incomplete. The proportion of patients with a revision for PJI reported in the NJR but unlinked to an index surgery has indeed reduced over time: from 79% in 2005 compared with 46% in 2009 and 36% in 2014. Survivorship of hip arthroplasty is high14 and it is also likely that some PJI revision procedures occur a long time after the index procedure due to PJI secondary to haematogenous spread: around 21% (280/1345) of revision procedures for PJI have been reported at greater than two years after the index surgery,34 with 10% performed at five years or beyond. The sample we present is six times larger than previous reports and therefore it is likely that a certain volume of our unlinked procedures are late revisions of index procedures performed before 2003 or in the first years of the registry.
The number of revisions performed annually in England and Wales for infected hip arthroplasties is rising, as is the risk of revision for infection in the first three months following surgery. This has substantial implications for service delivery given the surgical burden and costs associated with performing revision hip arthroplasties for prosthetic joint infection. Single-stage revisions are still performed less frequently than two-stage revisions but are becoming more popular.
Footnotes
Author Contribution: E. Lenguerrand: Conception and design, Analysis and interpretation of the data, Drafting of the article, Critical revision of the article for important intellectual content, Final approval, Statistical expertise, Obtaining of funding.
M. R. Whitehouse: Conception and design, Analysis and interpretation of the data, Drafting of the article, Critical revision of the article for important intellectual content, Final approval.
A. D. Beswick: Conception and design, Analysis and interpretation of the data, Drafting of the article, Critical revision of the article for important intellectual content, Final approval, Obtaining of funding.
S. A. Jones: Analysis and interpretation of the data, Critical revision of the article for important intellectual content, Final approval, Obtaining of funding.
M. L. Porter: Analysis and interpretation of the data, Critical revision of the article for important intellectual content, Final approval.
A. W. Blom: Conception and design, Analysis and interpretation of the data, Drafting of the article, Critical revision of the article for important intellectual content, Final approval, Obtaining of funding.
Conflicts of Interest Statement: All authors declare no financial relationships with any organisations that might have an interest in the submitted work, and no other relationships or activities that could appear to have influenced the submitted work.
M. L. Porter is Medical Director of the National Joint Registry and also acts as Chair of the Programme Steering Committee for the National Institute for Health Research (NIHR) INFORM programme (PGfAR programme: RP-PG-1210-12005).
Supplementary material
Figures showing prevalence (95% CI) of revision for prosthetic joint infection are available alongside this article at www.bjr.boneandjoint.org.uk
Funding Statement
*Acting on behalf of the National Joint Registry for England, Wales, Northern Ireland and the Isle of Man
We thank the patients and staff of all the hospitals who have contributed data to the National Joint Registry. We are grateful to the Healthcare Quality Improvement Partnership, the National Joint Registry Steering Committee, and staff at the National Joint Registry for facilitating this work.
This work was supported by the National Institute for Health Research (NIHR) under its Programme Grants for Applied Research (RP-PG-1210-12005). The views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health. The funder had no role in study design, data collection analysis and data interpretation, decision to submit, or preparation of the manuscript.
The views expressed represent those of the authors and do not necessarily reflect those of the National Joint Registry Steering Committee or Healthcare Quality Improvement Partnership, who do not vouch for how the information is presented.
References
- 1. Kapadia BH, Berg RA, Daley JA, et al. Periprosthetic joint infection. Lancet 2016;387:386-394. [DOI] [PubMed] [Google Scholar]
- 2. Dale H, Fenstad AM, Hallan G, et al. Increasing risk of prosthetic joint infection after total hip arthroplasty. Acta Orthop 2012;83:449-458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Blom AW, Taylor AH, Pattison G, Whitehouse S, Bannister GC. Infection after total hip arthroplasty. The Avon experience. J Bone Joint Surg [Br] 2003;85-B:956-959. [DOI] [PubMed] [Google Scholar]
- 4. Ong KL, Kurtz SM, Lau E, et al. Prosthetic joint infection risk after total hip arthroplasty in the Medicare population. J Arthroplasty 2009;24(Suppl):105-109. [DOI] [PubMed] [Google Scholar]
- 5. Phillips JE, Crane TP, Noy M, Elliott TS, Grimer RJ. The incidence of deep prosthetic infections in a specialist orthopaedic hospital: a 15-year prospective survey. J Bone Joint Surg [Br] 2006;88-B:943-948. [DOI] [PubMed] [Google Scholar]
- 6. Zmistowski B, Karam JA, Durinka JB, Casper DS, Parvizi J. Periprosthetic joint infection increases the risk of one-year mortality. J Bone Joint Surg [Am] 2013;95:2177-2184. [DOI] [PubMed] [Google Scholar]
- 7. Byren I, Bejon P, Atkins BL, et al. One hundred and twelve infected arthroplasties treated with ‘DAIR’ (debridement, antibiotics and implant retention). J Antimicrob Chemother 2009;63:1264-1271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Romanò CL, Manzi G, Logoluso N, Romanò D. Value of debridement and irrigation for the treatment of peri-prosthetic infections. A systematic review. Hip Int 2012;22(Suppl 8):S19-S24. [DOI] [PubMed] [Google Scholar]
- 9. Sendi P, Lötscher PO, Kessler B, et al. Debridement and implant retention in the management of hip periprosthetic joint infection: outcomes following guided and rapid treatment at a single centre. Bone Joint J 2017;99-B:330-336. [DOI] [PubMed] [Google Scholar]
- 10. Lindgren JV, Gordon M, Wretenberg P, Kärrholm J, Garellick G. Validation of reoperations due to infection in the Swedish Hip Arthroplasty Register. BMC Musculoskelet Disord 2014;15:384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Cooper HJ, Della Valle CJ. The two-stage standard in revision total hip replacement. Bone Joint J 2013;95-B(Suppl A):84-87. [DOI] [PubMed] [Google Scholar]
- 12. Kunutsor SK, Whitehouse MR, Blom AW, Beswick AD; INFORM Team. INFORM Team. Re-infection outcomes following one- and two-stage surgical revision of infected hip prosthesis: a systematic review and meta-analysis. PLoS One 2015;10:e0139166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Vanhegan IS, Malik AK, Jayakumar P, Ul Islam S, Haddad FS. A financial analysis of revision hip arthroplasty: the economic burden in relation to the national tariff. J Bone Joint Surg [Br] 2012;94-B:619-623. [DOI] [PubMed] [Google Scholar]
- 14. No authors listed. National Joint Registry for England, Wales and Northern Ireland: 12th Annual Report. http://www.njrcentre.org.uk/njrcentre/Portals/0/Documents/England/Reports/12th%20annual%20report/NJR%20Online%20Annual%20Report%202015.pdf (date last accessed 09 June 2017).
- 15. No authors listed. National Joint Registry for England and Wales. 9th Annual Report. http://www.njrcentre.org.uk/njrcentre/Portals/0/Documents/England/Reports/9th_annual_report/NJR%209th%20Annual%20Report%202012.pdf (date last accessed 09 June 2017).
- 16. Coviello V, Boggess M. Cumulative incidence estimation in the presence of competing risks. Stata J 2004;4:103-112. [Google Scholar]
- 17. Gillam MH, Ryan P, Graves SE, et al. Competing risks survival analysis applied to data from the Australian Orthopaedic Association National Joint Replacement Registry. Acta Orthop 2010;81:548-555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Ranstam J, Robertsson O. Statistical analysis of arthroplasty register data. Acta Orthop 2010;81:10-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Mahomed NN, Barrett JA, Katz JN, et al. Rates and outcomes of primary and revision total hip replacement in the United States medicare population. J Bone Joint Surg [Am] 2003;85-A:27-32. [DOI] [PubMed] [Google Scholar]
- 20. Zhan C, Kaczmarek R, Loyo-Berrios N, Sangl J, Bright RA. Incidence and short-term outcomes of primary and revision hip replacement in the United States. J Bone Joint Surg [Am] 2007;89-A:526-533. [DOI] [PubMed] [Google Scholar]
- 21. Bohl DD, Samuel AM, Basques BA, et al. How much do adverse event rates differ between primary and revision total joint arthroplasty? J Arthroplasty 2016;31:596-602. [DOI] [PubMed] [Google Scholar]
- 22. Pugely AJ, Martin CT, Gao Y, Schweizer ML, Callaghan JJ. The incidence of and risk factors for 30-day surgical site infections following primary and revision total joint arthroplasty. J Arthroplasty 2015;30(Suppl):47-50. [DOI] [PubMed] [Google Scholar]
- 23. Prokopetz JJ, Losina E, Bliss RL, et al. Risk factors for revision of primary total hip arthroplasty: a systematic review. BMC Musculoskelet Disord 2012;13:251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Winkler H. Rationale for one stage exchange of infected hip replacement using uncemented implants and antibiotic impregnated bone graft. Int J Med Sci 2009;6:247-252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Deirmengian C, Kardos K, Kilmartin P, et al. Combined measurement of synovial fluid alpha-Defensin and C-reactive protein levels: highly accurate for diagnosing periprosthetic joint infection. J Bone Joint Surg [Am] 2014;96:1439-1445. [DOI] [PubMed] [Google Scholar]
- 26. Paxton EW, Inacio MC, Khatod M, et al. Risk calculators predict failures of knee and hip arthroplasties: findings from a large health maintenance organization. Clin Orthop Relat Res 2015;473:3965-3973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Kaier K, Mutters NT, Frank U. Bed occupancy rates and hospital-acquired infections—should beds be kept empty? Clin Microbiol Infect 2012;18:941-945. [DOI] [PubMed] [Google Scholar]
- 28. Klouche S, Sariali E, Mamoudy P. Total hip arthroplasty revision due to infection: a cost analysis approach. Orthop Traumatol Surg Res 2010;96:124-132. [DOI] [PubMed] [Google Scholar]
- 29. Wolf CF, Gu NY, Doctor JN, Manner PA, Leopold SS. Comparison of one and two-stage revision of total hip arthroplasty complicated by infection: a Markov expected-utility decision analysis. J Bone Joint Surg [Am] 2011;93-A:631-639. [DOI] [PubMed] [Google Scholar]
- 30. No authors listed. Data collection forms. http://www.njrcentre.org.uk/njrcentre/Healthcareproviders/Collectingdata/Datacollectionforms/tabid/103/Default.aspx (date last accessed 09 June 2017).
- 31. No authors listed. National disease registries for advancing health care. Lancet 2011;378-9809:2050. [DOI] [PubMed] [Google Scholar]
- 32. Gundtoft PH, Overgaard S, Schønheyder HC, et al. The “true” incidence of surgically treated deep prosthetic joint infection after 32,896 primary total hip arthroplasties: a prospective cohort study. Acta Orthop 2015;86:326-334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Gundtoft PH, Pedersen AB, Schønheyder HC, Overgaard S. Validation of the diagnosis 'prosthetic joint infection' in the Danish Hip Arthroplasty Register. Bone Joint J 2016;98-B:320-325. [DOI] [PubMed] [Google Scholar]
- 34. Huotari K, Peltola M, Jämsen E. The incidence of late prosthetic joint infections: a registry-based study of 112,708 primary hip and knee replacements. Acta Orthop 2015;86:321-325. [DOI] [PMC free article] [PubMed] [Google Scholar]