Abstract
Background
Women’s childbirth experience can have immediate as well as long-term positive or negative effects on their life, well-being and health. When evaluating and drawing conclusions from research results, women’s experiences of childbirth should be one aspect to consider. Researchers and clinicians need help in finding and selecting the most suitable instrument for their purpose. The aim of this study was therefore to systematically identify and present validated instruments measuring women’s childbirth experience.
Methods
A systematic review was conducted in January 2016 with a comprehensive search in the bibliographic databases PubMed, CINAHL, Scopus, The Cochrane Library and PsycINFO. Included instruments measured women’s childbirth experiences. Papers were assessed independently by two reviewers for inclusion, and quality assessment of included instruments was made by two reviewers independently and in pairs using Terwee et al’s criteria for evaluation of psychometric properties.
Results
In total 5189 citations were screened, of which 5106 were excluded by title and abstract. Eighty-three full-text papers were reviewed, and 37 papers were excluded, resulting in 46 included papers representing 36 instruments. These instruments demonstrated a wide range in purpose and content as well as in the quality of psychometric properties.
Conclusions
This systematic review provides an overview of existing instruments measuring women’s childbirth experiences and can support researchers to identify appropriate instruments to be used, and maybe adapted, in their specific contexts and research purpose.
Electronic supplementary material
The online version of this article (doi:10.1186/s12884-017-1356-y) contains supplementary material, which is available to authorized users.
Keywords: Systematic review, Validated questionnaires, Measurement instruments, Psychometric properties, Childbirth experiences, Childbirth satisfaction
Background
Childbirth experiences can have immediate as well as long-term positive or negative effects on life, well-being and health [1]. A positive experience can be remembered as an empowering life event [1–3] connected to personal growth and self-knowledge affecting the transition to motherhood [4]. A negative birth experience increases the risk of negative health outcomes, such as postpartum depression [5] and future fear of giving birth [6], that can lead to a request for caesarean birth in future pregnancies [7, 8], and have an impact on future reproduction [9, 10]. The memory of a birth can vary over time for the woman, with either more positive or negative memories being recalled at a later period after birth compared to directly after [3, 11]. Furthermore childbirth, as experienced by the woman giving birth, can vary considerably from how a caregiver or relative may experience the same event. The person beside the woman may focus on more tangible, observable aspects and underestimate psychological aspects. It is therefore important that women are asked for their experiences [12]. Women have the right to a dignified, respectful, and humane health care during childbirth. Mistreatment of women in childbirth is a violation of women’s fundamental human rights [13]. Such mistreatment can occur both in the interaction between the woman and health care provider as through systematic failures in health facilities and health system levels. Therefor there is need of reliable and validated instruments to highlight women’s experiences and promote respectful and supportive care [14].
Studies on women’s childbirth experiences have been using different surrogate terms and related concepts such as ‘childbirth satisfaction’, ‘satisfaction with care’, ‘experiences of control’ or ‘of support’, ‘experience of relationship with caregivers’ and ‘experience of pain’ [15]. Women’s satisfaction with childbirth is multidimensional and affects the childbirth experience [16]. When evaluating and drawing conclusions from care in labour and birth, women’s experiences of childbirth should be one outcome of considerable importance to measure. This requires the use of reliable and valid instruments adapted to the purpose. As researchers might select and use different terms related to each other when studying women’s childbirth experiences, we have chosen to include instruments that use surrogate terms and related concepts in this review.
For an instrument to receive good levels of reliability and validity, extensive development and testing of psychometric properties is needed [17]. Without valid psychometric properties, conclusions drawn may be false and lead to invalid conclusions on the concept [18].
No review specifically focusing on instruments measuring women’s childbirth experiences has been found, but there are two reviews evaluating instruments measuring ‘maternal childbirth satisfaction’ [19, 20]. Perriman and Davis identified and reviewed 4 instruments measuring maternal satisfaction with continuity of maternity care models in before, during and after labour and birth. The papers describing the instruments primarily compared outcomes rather than describing the development of the tool [19]. Sawyer et al. identified and reviewed 9 multi-item instruments specifically studying maternal satisfaction with care given during labour and birth [20]. In an attempt to give researchers and clinicians an overview, we performed a systematic review to identify and present validated instruments measuring women’s childbirth experience.
Methods
A systematic review is a rigorous method of research that follows a systematic procedure to enable a summary of all findings from multiple studies on a specific topic. The start point is a rigorous search process for capturing the entire body of scientific studies [21]. As researchers might select and use different terms related to each other when studying women’s childbirth experience [15], we have chosen to use a broad definition and use surrogate terms and related concepts in this review, e.g. childbirth satisfaction, control, support, fear. The Cochrane guideline was used as guidance [21].
Eligibility criteria
First a review protocol was developed (see Additional file1). Inclusion and exclusion criteria were established in advance and documented in the review protocol. Criteria for inclusion in this review were as follows:
Papers representing instruments measuring women’s childbirth experience.
Papers should describe the development or test psychometric properties of an instrument.
Instruments assessing both pregnancy, childbirth and the postpartum period are included if one or more dimensions are related to women’s childbirth experiences, and this could be assessed as a separate scale.
Papers reporting original research, published in peer-reviewed journal.
Reviews were included to enable us to find original papers.
Papers published in English or French were included as the researchers could understand these languages.
Dissertations, non-original research, or conference papers were excluded.
Search strategy
The search strategy was designed and developed following consultation with a healthcare librarian. Before the final search all authors commented and agreed on the search string that was adapted for the individual databases (see Additional file 2). The final search took place in January 2016 in the electronic databases of PubMed, Scopus, CINAHL, Cochrane Library and PsycINFO. No restriction in the dates of publishing was made.
In total 8074 citations were identified (PubMed n = 2785, CINAHL n = 1140, PsycINFO n = 558, Scopus n = 3426 and Cochrane n = 165). For the initial screening all the search results were imported into reference management software (EndNote) and duplicates were removed, leaving 5106 titles and abstract to be screened for inclusion. First, papers clearly irrelevant to our topic, such as papers assessing childhood development, contraceptives etc., were removed by one of us (HN). The remaining 809 titles and abstract were assessed independently by two researchers (HN and an assistant, JC). This identified 266 residual papers which were assessed independently by two of the reviewers (HN and MB) to include papers for more in-depth full text assessment. Sixty-nine papers were retrieved in full text and assessed for eligibility criteria by two reviewers independently (HN and CB, or MB and CB, or HN and MB). Any potential conflicts were solved by the third reviewer. Fourteen additional studies were found through search of reference lists of included papers and were assessed in full-text by two independent reviewers for eligibility criteria (HN and MB). Three of these papers were included after assessment in full text. In total 83 papers were thus assessed in full text of which 37 did not fulfil the inclusion criteria and were excluded with reason (see Table 1). The names of each instrument were then searched in PubMed and CINAHL to retrieve further potential papers related to the specific instrument. No further papers on the development or testing of psychometric properties of the identified instruments were found. The flow of selection for studies are shown in Fig. 1.
Table 1.
Excluded papers with reason
| Instrument | Reason for exclusion |
|---|---|
| Bowers BB: Development of an instrument to measure mothers’ perceptions of professional labor support. Texas Woman’s University; 2001. | Dissertation |
| Callahan JL, Hynan MT: Identifying mothers at risk for postnatal emotional distress: further evidence for the validity of the perinatal posttraumatic stress disorder questionnaire. J Perinatol 2002; 22(6):448–454. | Focus on postnatal medical complications of infant in relation to mothers health rather than on childbirth experiences |
| Chen CH, Wang SY: Women’s perceptions of caesarean delivery. Gaoxiong Yi Xue Ke Xue Za Zhi 1992; 8(5):241–246. | In Chinese |
| Claudia Uribe T, Aixa Contreras M, Luis Villarroel D: Adaptation and validation of the Maternal Welfare Scale in childbirth situations: Second version for integral assistance scenarios. Revista Chilena de Obstetricia y Ginecologia 2014; 79(3): 154–160. | In Spanish |
| Claudia Uribe T, Aixa Contreras M, Luis Villarroel D, Soledad Hivera M, Paulina Bravo V, Marieta Cornejo A: Maternal wellbeing during childbirth: Development and application of a measurement scale. Revista Chilena de Obstetricia y Ginecologia 2008; 73(1):4–10. | In Spanish |
| Declercq ER, Sakala C, Corry MP, Applebaum S: Listening to Mothers II: Report of the Second National U.S. Survey of Women’s Childbearing Experiences: Conducted January-February 2006 for Childbirth Connection by Harris Interactive(R) in partnership with Lamaze International. J Perinat Educ 2007; 16(4):9–14. | Not able to distinguish childbirth experience as separate scale from rest of questionnaire. |
| De Holanda CSM, Alchieri JC, Morais FRR, De Oliveira Maranhão TM: Strategies for development, follow-up, and assessment of care provided to women in the pregnancy-postnatal cycle. Revista Panamericana de Salud Publica/Pan American Journal of Public Health 2015; 37(6):388–394. | In Portuguese |
| Drummond J, Rickwood D: Childbirth confidence: validating the Childbirth Self-Efficacy Inventory (CBSEI) in an Australian sample. J Adv Nurs 1997; 26(3):613–622 | Measures expectancies of labour |
| Denis A, Séjourné N, Callahan S: Étude de validation française de la version courte du Maternal Self-report Inventory. L’Encéphale: Revue de psychiatrie clinique biologique et thérapeutique 2013; 39(3):183–188. | Not able to separate childbirth experience from the rest of the questionnaire. |
| Garthus-Niegel S, Storksen HT, Torgersen L, Von Soest T, Eberhard-Gran M: The Wijma Delivery Expectancy/Experience Questionnaire: a factor analytic study. J Psychosom Obstet Gynaecol 2011; 32(3):160–163. | To assess fear of childbirth during pregnancy |
| Harvey S, Rach D, Stainton MC, Jarrell J, Brant R: Evaluation of satisfaction with midwifery care. Midwifery 2002; 18(4):260–267. | Not specifically on the childbirth experience |
| Hung CH, Hsu YY, Lee SF: Couples’ satisfaction with health care service during labor and delivery. Kaohsiung J Med Sci 1997; 13(4):255–262. | Assess couples’ experience, not able to distinguish women’s experiences. |
| Ip WY, Chan D, Chien WT: Chinese version of the Childbirth Self-efficacy Inventory. J Adv Nurs 2005, 51(6):625–633. | Measures expectancies of labour |
| Ip WY, Chung TK, Tang CS: The Chinese Childbirth Self-Efficacy Inventory: the development of a short form. J Clin Nurs 2008; 17(3):333–340. | Measures expectancies of labour |
| Janssen PA, Dennis C, Reime B: Development and psychometric testing of the Care in Obstetrics: Measure For Testing Satisfaction (COMFORTS) scale. Research in Nursing & Health 2006, 29(1):51–60 10p. | Not able to distinguish childbirth experience so that it can qualify as a scale of its own |
| Khalatbari J, Ghasemabadi E, Ghorbanshirodi S: Effect of early Skin-to-skin contact of mother and newborn on mother’s satisfaction. Life Science Journal 2013; 10(SUPPL.3):423–425. | No psychometric analyses |
| Kishi R, McElmurry B, Vonderheid S, Altfeld S, McFarlin B, Tashiro J: Japanese Translation and Cultural Adaptation of the Listening to Mothers II Questionnaire. J Perinat Educ 2011; 20(1):14–27. | Not able to distinguish childbirth experience from the rest of the questionnaire. |
| Lee ML, Cho JH: [Development of a scale to measure the self concept of cesarean section mothers]. Kanho Hakhoe Chi 1990; 20(2):131–141. | In Korean |
| Lowe NK: Maternal confidence for labor: development of the Childbirth Self-Efficacy Inventory. Res Nurs Health 1993; 16(2):141–149. | Measures expectancies of childbirth |
| Mas-Pons R, Barona-Vilar C, Carregui-Vilar S, Ibanez-Gil N, Margaix-Fontestad L, Escriba-Aguir V: [Women’s satisfaction with the experience of childbirth: validation of the Mackey Childbirth Satisfaction Rating Scale]. Gac Sanit 2012; 26(3):236–242. | In Spanish |
| Padawer JA, Fagan C, Janoff-Bulman R, Strickland BR, Chorowski M: Women’s psychological adjustment following emergency cesarean versus vaginal delivery. Psychology of Women Quarterly 1988; 12(1):25–34. | Limited testing and description of psychometric properties. The childbirth Perception Questionnaire is further validated by Bertucci et al. (2012) which is included in the review |
| Perriman N, Davis D: Measuring maternal satisfaction with maternity care: A systematic integrative review: What is the most appropriate, reliable and valid tool that can be used to measure maternal satisfaction with continuity of maternity care? Women Birth 2016. | Review |
| Redshaw M, Martin C, Rowe R, Hockley C: The Oxford Worries about Labour Scale: women’s experience and measurement characteristics of a measure of maternal concern about labour and birth. Psychol Health Med 2009;14(3): 354–366 | Not experiences of childbirth but on worries about childbirth |
| Rini EV: The Development and Psychometric Analysis of an Instrument to Measure a Woman’s Experience of Childbirth. West Virginia University; 2014. | Dissertation |
| Ross-Davie MC, Cheyne H, Niven C: Measuring the quality and quantity of professional intrapartum support: testing a computerised systematic observation tool in the clinical setting. BMC Pregnancy Childbirth 2013; 13:163. | Not the woman’s perspective |
| Rudman A, El-Khouri B, Waldenstrom U: Women’s satisfaction with intrapartum care - a pattern approach. J Adv Nurs 2007, 59(5):474–487. | Compare different dimensions of the childbirth experience to see how they form different patterns of satisfaction |
| Salmon P, Miller R, Drew NC: Women’s anticipation and experience of childbirth: the independence of fulfillment, unpleasantness and pain. Br J Med Psychol 1990; 63 (Pt 3):255–259. | Compares antenatal anticipations of childbirth to postnatal experiences of childbirth |
| Sapountzi-Krepia D, Raftopoulos V, Tzavelas G, Psychogiou M, Callister LC, Vehvilainen-Julkunen K: Mothers’ experiences of maternity services: internal consistency and test-retest reliability of the Greek translation of the Kuopio Instrument for Mothers. Midwifery 2009; 25(6):691–700. | Focus on expectations on childbirth not on experiences |
| Sawyer A, Ayers S, Abbott J, Gyte G, Rabe H, Duley L: Measures of satisfaction with care during labour and birth: a comparative review. BMC Pregnancy Childbirth 2013; 13:108. | Review |
| Sinclair M, O’Boyle C: The Childbirth Self-Efficacy Inventory: a replication study. J Adv Nurs 1999; 30(6):1416–1423. | Measures expectancies of childbirth |
| Stahl K: [Revalidation of a questionnaire assessing women’s satisfaction with maternity care in hospital]. Psychother Psychosom Med Psychol 2010; 60(9–10): 358–367. | In German |
| Stevens NR, Hamilton NA, Wallston KA: Validation of the multidimensional health locus of control scales for labor and delivery. Res Nurs Health 2011; 34(4):282–296 | Pregnant women’s expectations |
| Sweetser L: Satisfaction with childbirth: measurement and causes. Other titles: 1976; 45(4):163–180. | No psychometric analyses |
| Takegata M, Haruna M, Matsuzaki M, Shiraishi M, Murayama R, Okano T, Severinsson E: Translation and validation of the Japanese version of the Wijma Delivery Expectancy/Experience Questionnaire version A. Nurs Health Sci 2013; 15(3):326–332. | Assesses pregnant women’s expectations |
| Tanglakmankhong K, Perrin NA, Lowe NK: Childbirth Self-Efficacy Inventory and Childbirth Attitudes Questionnaire: psychometric properties of Thai language versions. J Adv Nurs 2011; 67(1):193–203. | For pregnant women measuring expectations of childbirth |
| Tokiwa Y, Kunikiyo K: Literature review on self evaluation of childbirth experience. Kitakanto Medical Journal 2006; 56(4):295–302. | In Japanese |
| Zweig S, Kruse J, LeFevre M: Patient satisfaction with obstetric care. J Fam Pract 1986; 23(2):131–136. | No psychometric analyses |
Fig. 1.
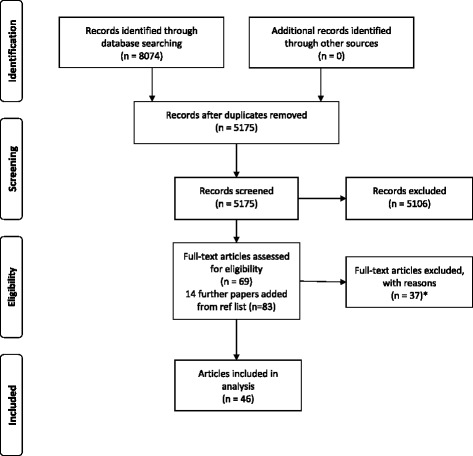
Flow chart of study selection
Quality assessment of included instruments
As the aim of this review was to identify and assess instruments measuring women’s childbirth experiences, the focus was not on the quality of the studies of the included articles but to identify psychometric properties of identified instruments. This was done using criteria specified by Terwee et al. [17] which refer to the following properties; Content validity, Internal consistency, Criterion validity, Construct validity, Reproducibility agreement, Reproducibility reliability, Responsiveness, Floor and ceiling effects, and Interpretability. The properties were evaluated as; + = positive rating, ? = indeterminate rating, − = negative rating, and 0 = no information available. Terwee et al. emphasise the importance of a clear design and method, and that the sample size needs to be greater than 50 subjects in every subgroup of the analysis [17]. In addition to quality assessment of these properties we added another two criteria. The first one considers the need for the instrument and, for a positive rating, a search for existing instruments had to have been done, demonstrating the need to develop and test a new instrument. The second rating item added is related to face validity. For a positive rating, members of the target population should have been asked about the appropriateness of the questionnaire and of each question.
This rating of the measurement properties was performed independently by two review authors (HN and MB, or HN and CB, or MB and CB). When ratings differed between the pairs, it was discussed and, when conflict remained, the third reviewer was included in the discussion to reach consensus. An overview of the results of the quality rating of psychometric properties of included instruments is displayed in Table 2. The last column in the table gives the total figure awarded to each tool, based on a mark of 1 for each ‘+’, and 0.5 for one or more ‘?’ grades. This is only a rough guide to the overall quality of the instrument and must be interpreted with caution. For example, two tools that both received a mark of 6 may be of very different quality, depending on the criteria that were awarded the points.
Table 2.
Quality rating of psychometric properties with Terwee et al.’s criteria
| Instrument | Psycometric properties | Total score | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Need for the instrument | Face validity | Content validity | Internal consist-ency | Criterion validity | Construct validity | Reprod-ucibility (Agree-ment) | Reproc-ucibility (Reliabi-lity) | Respon-sivness | Floor & ceiling effects | Inter-pretata-bility | ||
| The Childbirth Trauma Index [22] | + | 0 | + | - | 0 | ? | 0 | 0 | 0 | 0 | 0 | 2.5 |
| The Childbirth Experience Perception Questionnaire [26] | + | + | + | - | + | 0 | 0 | ? | 0 | 0 | 0 | 4.5 |
| The Childbirth Experience Questionnaire [34] | + | + | + | + | 0 | + | 0 | + | 0 | + | 0 | 7 |
| The Survey of Bangladeshi women’s experiences of maternity services [41] | + | + | + | + | 0 | + | + | 0 | 0 | 0 | 0 | 6 |
| The Birth Companion Support Questionnaire [42] | + | + | + | + | 0 | + | + | 0 | 0 | 0 | 0 | 6 |
| The Perception of Birth Scale [23, 24] | + | 0 | + | + | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 3 |
| The Birth Memories and Recall Questionnaire [30] | + | + | + | + | 0 | 0 | 0 | + | 0 | 0 | 0 | 5 |
| The Support and Control in Birth questionnaire [25] | + | + | + | + | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 4 |
| A self-administered questionnaire to assess women’s satisfaction with maternity care [43] | + | 0 | + | + | 0 | 0 | + | + | 0 | 0 | + | 6 |
| The Scale for Measuring Maternal Satisfaction- normal birth [44] | + | + | + | + | + | + | 0 | 0 | 0 | 0 | 0 | 6 |
| The Scale for Measuring Maternal Satisfaction -caesarean birth [44] | + | + | + | + | + | + | 0 | 0 | 0 | 0 | 0 | 6 |
| The Labor and Delivery Index [45] | + | + | + | 0 | 0 | + | + | + | 0 | 0 | 0 | 6 |
| The Labour Agentry Scale [46] | + | 0 | + | + | 0 | 0 | + | + | + | 0 | 0 | 6 |
| The Birth Satisfaction Scale-Revised [27–29] | + | + | + | + | 0 | ? | 0 | 0 | 0 | 0 | 0 | 4.5 |
| The Early Labour Experience Questionnaire [47] | ? | 0 | + | + | + | + | 0 | + | 0 | 0 | + | 6.5 |
| The Labor and Delivery Satisfaction Index [31] | + | + | + | - | 0 | + | + | - | 0 | 0 | 0 | 5 |
| Women’s delivery experience measures [32] | + | ? | + | + | 0 | + | 0 | 0 | 0 | 0 | ? | 5 |
| The maternal satisfaction scale for caesarean section [35] | + | + | + | + | 0 | + | 0 | + | 0 | 0 | + | 7 |
| The Satisfaction with childbirth experience questionnaire [48] | + | + | + | + | 0 | + | 0 | 0 | 0 | 0 | + | 6 |
| Women’s Perception of Control during Childbirth [48] | + | + | + | + | 0 | + | 0 | 0 | 0 | 0 | + | 6 |
| The Childbirth Schema Scale [33] | 0 | 0 | + | + | 0 | + | + | 0 | 0 | 0 | + | 5 |
| Satisfaction with obstetrical care [49] | + | + | ? | + | 0 | + | 0 | 0 | 0 | + | + | 6.5 |
| The Preterm Birth Experience and Satisfaction Scale [50] | + | + | + | + | 0 | + | 0 | ? | ? | 0 | + | 6.5 |
| The Responsivness in Perinatal and Obstetric Health Care Questionnaire [36, 37] | + | + | + | + | 0 | + | 0 | 0 | + | + | + | 8 |
| Women’s Satisfaction With Hospital-Based Intrapartum Care Scale [51] | + | + | + | + | 0 | + | 0 | 0 | 0 | 0 | + | 6 |
| Patient Perception Score [52] | + | + | + | + | + | + | 0 | 0 | 0 | 0 | + | 7 |
| Pregnancy and maternity care patients experiences questionnaire [38] | + | + | + | + | 0 | + | + | + | + | 0 | + | 9 |
| Women’s view of brith labour satisfaction questionnaire [53] | + | + | + | + | ? | + | 0 | 0 | 0 | 0 | + | 6.5 |
| The Perceived Control in Childbirth Scale [54] | + | 0 | + | + | + | + | 0 | 0 | 0 | 0 | + | 6 |
| The Satisfaction with Childbirth Scale [54] | + | 0 | + | + | + | + | 0 | 0 | 0 | 0 | + | 6 |
| The Pregnancy and Childbirth Questionnaire [55] | + | + | + | + | ? | ? | 0 | + | 0 | 0 | + | 6.5 |
| The Childbirth Perception Scale [39] | + | + | + | + | 0 | + | 0 | + | 0 | 0 | + | 7 |
| The Scale of Women’s Perception for Supportive Care Given During Labor [56] | + | + | + | + | 0 | + | 0 | 0 | 0 | 0 | + | 6 |
| The Delivery Fear Scale [57] | + | + | + | + | 0 | + | ? | 0 | 0 | 0 | + | 6.5 |
| The Wijma Delivery Expectancy/Experience Questionnaire [40] | + | + | + | + | + | + | 0 | + | + | 0 | + | 9 |
| The Parental Satisfaction and Quality Indicators of Perinatal Care Instrument [58, 59] | + | + | + | + | 0 | + | 0 | 0 | 0 | 0 | + | 6 |
Rating: + = positive, ? = intermediate, − = negative, 0 = no information available, N/A not assessable
In conducting this review, our focus and aim was on identifying measures and conducting a broad assessment of their psychometric properties. Given the large number of instruments found, and their very different foci, it was not possible to make clear recommendations as to one particular instrument that would suit all purposes. Instead, some general suggestions are made as to the instruments that appear to be emerging as the top ranking tools in terms of the quality measurement performed, and the overall mark given.
Data extraction and analysis
The following data were extracted for each instrument: Name of instrument/acronym, authors (year), country of origin, aim/motive of instrument, number of items, dimensions/subscales, response scale, timeframe to answer the questionnaire, whether or not the questionnaire was available and a short narrative summary of included instruments. The data extraction was made by the first author (HN) and then checked by the other authors for accuracy.
One of the individual papers was conducted by one of the authors (MB). To avoid conflict of interest this paper was assessed for eligibility criteria, and quality assessment was made, by the two other authors (HN and CB).
Results
Forty-six articles presenting 36 instruments [22–59] measuring women’s childbirth experiences were included for quality assessment. Different surrogate terms and related concepts used in identified instruments were described by authors as: childbirth experience (27.8%), satisfaction with care/birth/childbirth (36.1%), perception of birth/care (13.9%), control (11.1%), support (8.3%), fear of childbirth (5.6%), childbirth trauma (2.8%), birth memories (2.8%) and childbirth schema (2.8%). In five of the identified instruments we found cultural validation/translation of the instrument had been done. Most of the instruments were developed and tested in the United States (6) and in the United Kingdom (6). Further countries represented were: Canada (4), the Netherlands (4), Turkey (3), Sweden (3), Jordan (3), France (2), Italy (2), Australia (1), Senegal (1), and Norway (1). Number of items in the instruments varied from three to 145. Nine of the instruments were uni-dimensional, and 27 consisted of several dimensions/subscales. Quality ratings of psychometric properties are presented in Table 2. Descriptive data of included instruments are presented in Table 3, and characteristics in Table 4. Instruments are reported in alphabetical order by first author.
Table 3.
Descriptive data of the included instruments
| Name of Instrument/Acronym | Authors (year) | Country | Aim/motive of instrument | Comments |
|---|---|---|---|---|
| The Childbirth Trauma Index for adolescents/CTI [22] | Anderson (2011) | USA | To determine specific indicators perceived by adolescents as influencing birth trauma. | Developed to aid nurses to assess and direct care to reduce the possibility of a trauma stress response or post-traumatic stress disorder among adolescents postpartum [22]. Further development, adaptation and evaluation of the psychometric properties of this tool would be valuable. |
| The Childbirth Experience Perception Scale/CEPS [26] | Bertucci et al. (2012) | Italy | To assess women’s perception of their childbirth experience. | A further development of ‘The childbirth perception questionnaire’ [73]. The original questionnaire was excluded from our review as the original paper does not present testing of psychometric properties. Bertucci et al. [26] are aware of this, but they consider the strengths of the questionnaire outweigh the limitations as it takes a broad view of various aspects into consideration when evaluating the childbirth perceptions. The psychometric properties need to to be further evaluated. The validity of the Childbirth experience perception scale was challenged in a letter to Midwifery journal, and the authors replied defending their position [83, 84]. |
| The Childbirth experience questionnaire/CEQ [34] | Dencker et al. (2010). | Sweden | To assess different aspects of first-time women’s perception of their childbirth experience. | Developed to assess different aspects of mothers’ childbirth experiences in order to explore them comprehensively. Suggested \to be used to identify women with negative childbirth experiences and for evaluating quality of care. The development of the instrument is clearly described and primary results of several psychometric properties are presented [34]. The instrument has been validated in the UK [77] and used in research [85]. |
| The survey of Bangladeshi women’s experiences of maternity services/SBWEMS [41] | Duff et al. (2001) | UK | To evaluate satisfaction with maternity care in Sylheti-speaking Bangladeshi women. | This cross-cultural instrument was made by cultural adaptation and translation of an existing measure. This paper can be used as a model and inspiration when developing instruments for use in minority ethnic communities [41]. |
| The Birth Companion Support Questionnaire/BCSQ [42] | Dunne (2014) | Australia | To measure women’s perceptions of social support provided during labour by at least one lay birth companion. | Presents a first rigorous study of this instrument developed to be used in midwifery research [42]. |
| The Perception of Birth Scale/POBS [23, 24] | Fawcett & Knauth (1996) Marut & Mercer (1979) |
USA | To measure women’s perceptions of their childbirth experiences. | This questionnaire was originally developed and adapted to measure the perception of women who had vaginal or unplanned caesarean births in 1975 [86] and further adapted by Marut and Marcer [24] in 1979. Attempts have been made to adapt and test psychometric properties [87, 88] before Fawcett and Knauth [23] in 1995 adapted the scale further and made an exploratory factor analysis. The scale needs further tests of its psychometric properties. |
| The Birth Memories and Recall Questionnaire/BirthMARQ [30] | Foley et al. (2014) | UK | To examine the relationship between memories of birth and postnatal mood and psychopathology. | Developed to measure characteristics of memories of childbirth and to examine the relationship between memories for birth and mental health including emotional and traumatic memories. With further testing of reliability and validity this questionnaire could become a useful tool both in research as well as in clinical practice [30]. |
| The Support and Control in Birth Questionnaire/SCIB [25] | Ford et al. (2009) | UK | To measure support and control in birth. | Focuses on different dimensions of control during childbirth. With further testing of tis psychometric properties it can provide a valid and reliable measure to examine the relationships among support, control, and birth outcomes [25]. It has been culturally validated and translated into Turkish [78]. |
| Women’s satisfaction with maternity care/WSMC [43] | Gerbaud et al. (2003) | France | To measure women’s satisfaction concerning maternity care. | This questionnaire is in French and measure women’s satisfaction with care during pregnancy, hospitalisation for birth, and homecoming. It is tested and developed to be used clinically and evaluated care [43]. |
| The Scale for Measuring Maternal Satisfaction-normal birth/SMMS-normal birth [44] | Gungor & Beji (2012) | Turkey | To measure maternal satisfaction with birth in order to evaluate women’s experiences in labour and the early postpartum period before hospital discharge. | This is a scale developed in two versions, one for normal birth and one for caesarean birth. The scales are constructed to evaluate both the experience of care and the emotional experience of childbirth as a measure of satisfaction. The evaluation of initial psychometric properties are good and with further testing these scales can become a useful tool [44]. |
| The Scale for Measuring Maternal Satisfaction- Caesarean birth/SMMS-caesarean birth [44] | Gungor & Beji (2012) | Turkey | To measure maternal satisfaction with birth in order to evaluate women’s experiences in labour and the early postpartum period before hospital discharge. | See above. |
| The Labor and Delivery Index/LADY-X [45] | Gärtner et al. (2015) | The Netherlands | A utility measure for economic evaluations in perinatal studies. | Developed to measure cost effectiveness of perinatal care interventions for use in research and is able to discriminate between groups [45]. The only instrument identified that measures economic evaluations in perinatal studies. |
| The Labour Agentry Scale/LAS [46] | Hodnett & Simmons-Tropea (1987) | Canada | An instrument measuring expectancies and experiences of personal control during childbirth. | Since this scale was developed in 1987 [46] it has been used in studies from a broad range of countries as well as in different types of studies [89–96]. Although widely used, further studies of the psychometric properties are recommended to ensure its validity and reliability. |
| The Birth Satisfaction Scale - Revised/BSS-R [27–29] | Hollins Martin & Fleming (2011) Hollins Martin et al. (2012) Hollins Martin & Martin (2014) |
UK | To measure postnatal women’s birth satisfaction. | The birth satisfaction scale – revised [28] is a further development of the Birth satisfaction scale [27, 29, 97]. The revised version of the scale is a more robust version. They have been used in research [97–99] and further cultural translation and validation has been made in Greece and the US [79, 80, 100]. |
| The Early Labour Experience Questionnaire/ELEQ [47] | Janssen & Desmarais (2013) | USA | To measure women’s experiences with their early labour care. | Developed to measure women’s experience and evaluate care given in the latent and early phase of labour [47, 101]. Additional testing of psychometric properties would strengthen the questionnaire further. |
| The Labor and Delivery Satisfaction Index/LADSI [31] | Lomas et al. (1987) | Canada | To assess the caring aspects of childbirth care. | Developed for use in clinical trials [31] and has been used in several studies evaluating care given [102–104]. It was developed and evaluated in 1987. Therefore it would be appropriate to perform further testing and updating of its psychometric properties. |
| Women’s delivery experience measures/MFRM [32] | Mannarini et al. (2013) | Italy | To assess birth experiences after both spontaneous and medically assisted conception. | The statistical analysis was made by using the Rash model with the purpose of defining and validating a latent dimension for birth perception [32]. |
| The maternal satisfaction scale for caesarean section/MSS-caesarean section [35] | Morgan et al. (1999) | Canada | To measure maternal satisfaction in women undergoing elective or non-emergent caesarean section under regional anaesthesia. | Developed by anaesthesiologists and two of the dimensions are measuring satisfaction with anaesthetics and side-effects. It has been properly tested for validity and reliability [35]. |
| The Satisfaction with childbirth experience questionnaire/SWCBE [48] | Oweis (2009) | Jordan | No aim/purpose of the instrument documented. | Oweis [48] developed two scales in the same study to assess women’s childbirth experiences including expectations, satisfaction and self-control. These two scales need further evaluation of their psychometric properties. |
| Women’s Perception of Control during Childbirth/PCCB [48] | Oweis (2009) | Jordan | No aim/purpose of the instrument documented. | See above. |
| The Childbirth Schema Scale/CSS [33] | Peirce (1994) | US | To obtain an understanding of schema formation and revision with the known stressor of childbirth. | Developed to gain understanding of the underlying structure of known stressors of childbirth, by comparing the schemas before and after birth [33]. Further development and adaptation of the instrument would strengthen the psychometric properties. |
| Satisfaction with obstetrical care/SSO [49] | Ramanah (2014) | France Canada Senegal |
To measure satisfaction in obstetrical care during labor, delivery and two hours postpartum relevant to the French-speaking context. | This instrument is tested in a French speaking context in Senegal, France and Canada [49]. Further development and evaluation of this instrument would strengthen the validity. |
| The Preterm Birth Experience and Satisfaction Scale/P-BESS [50] | Sawyer (2014) | UK | To assess parents (women and their partners) experiences and satisfaction with care during very preterm birth (<32 gestational weeks). | Further testing of psychometric properties in larger sample groups would be recommended as well as assessment of when the most suitable time after birth to administer the questionnaire would be [50]. |
| The Responsivness in Perinatal and Obstetric Health Care Questionnaire/ReproQ [36, 37] | Scheerhagen et al. (2015) van der Kooy et al. (2014). |
The Netherlands | To evaluating maternal experiences of perinatal care services, using the eight-domain WHO concept. | This questionnaire is based on the eight-domain World Health Organization’s Responsiveness model. The questionnaire has an antepartum version assessing the experience during pregnancy and a postpartum version assessing women’s experiences during childbirth and postpartum care. It has been properly tested for a broad variety of psychometric properties [36, 37, 105]. It has been used to evaluate and compare care [106]. |
| Women’s Satisfaction With Hospital-Based Intrapartum Care Scale [51] | Shaban (2014) | Jordan | To measure women’s satisfaction with intrapartum care in Jordan, especially to examine how low-risk, healthy laboring women experienced are during labor and birth. | Developed to provide information on women’s experiences with the aim of helping caregivers change practices. Further studies evaluating the psychometric properties would be the next step [51]. |
| Patient Perception Score/PPS [52] | Siassakos et al. (2009) | UK | A simple tool to measure maternal satisfaction of operative abdominal and vaginal birth. | This is a short tool adapted from a Patient perception score used in simulation training of obstetric emergency situations and is easy to complete [107]. It aims to capture patient’s perception of operative birth with a focus on perceived communication, respect and safety. This is an easy tool that is suggested by the authors to be used on a regular basis in clinical settings to focus on women’s perceptions and improve care [52]. |
| Pregnancy- and maternity-care patients’ experiences questionnaire./PreMaPEQ [38] | Sjetne (2015) | Norway | To measure women’s experiences of pregnancy and maternity care in Norway and other sites having similar health system. | Developed to collect women’s experiences of the maternity health care system in Norway. It has been well tested for a broad variety of psychometric properties and is an acceptable instrument for collecting women’s experiences of maternity care [38]. |
| Women’s View of Birth Labour Satisfaction Questionnaire/WOMBLSQ [53] | Smith (2001) | UK | To measure maternal satisfaction with care quality of different models of labour care in the UK. | This questionnaire can be used to compare models or systems of labour and care during birth, giving an overall picture of care received. It would strengthen the reliability and validity if the instrument was further evaluated and adapted [53]. It has been culturally translated and adapted in several countries [108, 109] and used in studies [110]. |
| The perceived Control in Childbirth Scale/PCCh [54] | Stevens (2012) | USA | To assess patient perceptions of control of the childbirth environment. | Development of two separate scales in the same paper. A goal of the study was to clarify the theoretical distinctions among similar constructs [54]. |
| The Satisfaction with Childbirth Scale/SWCh [54] | Stevens (2012) | USA | To assess global satisfaction with the childbirth experience. | See above. |
| The Pregnancy and Childbirth Questionnaire/PCQ [55] | Truijens (2014a) | The Netherlands | To assess quality of care during pregnancy and delivery as perceived by women who recently gave birth. | Two scales, one referring to pregnancy and one referring to birth. Further research and evaluation of the psychometric properties would strengthen the validity and reliability [55]. It has been used in studies [111, 112]. |
| The Childbirth Perception Scale/CPS [39] | Truijens (2014b) | The Netherlands | To assesses the perception of delivery and the first postpartum week. | Developed to compare women’s perception of home and hospital birth [39]. Psychometric properties have been adequate tested but further testing would strengthen validity and reliability. |
| The Scale of Women’s Perception for Supportive Care Given During Labor [56] | Uludag & Mete (2015). | Turkey | To determine women’s perception of supportive care given during labor. | Developed to see how women perceive care received from nurses to evaluate quality of care [56]. Further evaluation and adaptation of the psychometric properties would strengthen validity and reliability. |
| Delivery Fear Scale/DFS [57] | Wijma et al. (2002) | Sweden | To measure fear during the process of labor. | This is the only scale that we have identified that has been tested and evaluated for psychometric properties that are meant to be used during labour [80]. The scale has been used in research [113, 114]. |
| The Wijma Delivery Expectancy/Experience Questionnaire/W-DEQ [40] | Wijma et al. (1998) | Sweden | To measure fear of childbirth during pregnancy and after childbirth. | Consists of two versions; one to be used during pregnancy (version A) and one to be used after childbirth (version B) [40]. It has been used extensively [60–66] and cultural validation and translations have been made in several countries [67–69]. It is commonly used for measuring fear of childbirth, and it is properly developed with good psychometric properties. |
| The Parental Satisfaction and Quality Indicators of Perinatal Care Instrument/PPC [58, 59] | Wool, C. (2015a). Wool, C. (2015b). |
US | To measure parental satisfaction and quality indicators in parents electing to continue a pregnancy after learning of a life-limiting fetal diagnosis. | This is the only instrument we identified concerning this subject [58, 59]. Further evaluation of the psychometric properties would strengthen the validity and reliability. |
Table 4.
Characteristics of included instruments
| Name of Instrument/Acronym | Items | Dimensions/subscales | Response | Timeframe to answer the questionnaire | Quest-ionnaire available |
|---|---|---|---|---|---|
| The Childbirth Trauma Index for Adolescents/CTI [22] | 14-items | No | 4- point Likert scale and rating of birth experience between 0 and 10 | 1–3 days postpartum | No |
| The Childbirth Experience Perception Scale/CEPS [26] | 24-items | 3 subscales; Labour and Delivery Perception, Control Perception, and Change Perception. | 6-point Likert scale | 24–48 h postpartum | No |
| The Childbirth experience questionnaire/CEQ [34] | 22-items | 4 dimensions; Own capacity, Professional support, Perceived safety, and Participant | 4- point Likert scale and VAS | 1 month postpartum | Yes |
| The survey of Bangladeshi women’s experiences of maternity services/SBWEMS [41] | 72- items | 3 subscales; Ante- (33 items), Peri- (15 items), Post-natal (24 items) | Yes/No, Likert scales and Multiple choice options | 2 month postpartum | Yes |
| the Birth Companion Support Questionnaire/BCSQ [42] | 17-items | 2 subscales; Emotional support, tangible support | 4-point Likert scale | On postnatal ward before discharge | No |
| The Perception of Birth Scale/POBS [23, 24] | 25-items | 5 subscales; Labor Experience, Delivery Experience, Delivery Outcome, Partner Participation, and Awareness | 5-point Likert scale | 1–2 days after birth | No |
| The Birth Memories and Recall Questionnaire/BirthMARQ [30] | 23-itmes | 6 dimensions; Emotional memory, centrality of memory to identity, Coherence, Reliving, Involuntary recall, and Sensory memory | 7-point Likert scale | Within 1 year after giving birth | Yes |
| The Support and Control in Birth Questionnaire/SCIB [25] | 33-items | 3 subscales; Internal control (10 items), external control (11 items), Support (12 items) | 5-point Likert scale | On average, 1 year after birth | Yes |
| Women’s satisfaction with maternity care/WSMC [43] | 44-items | 11 dimensions | Likert scales and Multiple choice options | 2 month postpartum | Yes |
| The Scale for Measuring Maternal Satisfaction-normal birth/SMMS-normal birth [44] | 43-items | 10 subscales; perception of health professionals, nursing/midwifery care in labour, comforting, information and involvement in decision making, meeting baby, postpartum care, hospital room, hospital facilities, respect for privacy, meeting expectations | 5-point Likert scale | Within 24 h | No |
| The Scale for Measuring Maternal Satisfaction- Caesarean birth/SMMS-caesarean birth [44] | 42-items | 10 subscales; perception of health professionals, preparation for caesarean, comforting, information and involvement in decision making, meeting baby, postpartum care, hospital room, hospital facilities, respect for privacy, meeting expectations | 5-point Likert scale | Within 72 h | No |
| The Labor and Delivery Index/LADY-X [45] | 7-items | 7 domains; Availability, Information, Needs, Emotional support, Worries, Safety, time to first contact with baby | 3-point Likert scale | 6–8 weeks postpartum | Yes |
| The Labour Agentry Scale/LAS [46] | 29-items | No | 7-point Likert scale | Within 72 h postpartum | No |
| The Birth Satisfaction Scale - Revised/BSS-R [27–29] | 10-items | 3 subscales: Quality of care provision (4 items), women’s personal attributes (2 items), stress experienced during labour (4 items). | 5-point Likert scale | Within 10 days postpartum | Yes |
| The Early Labour Experience Questionnaire/ELEQ [47] | 22-items | 3 subscales: Emotional Well-Being (8), Emotional Distress (8), Perception of Nursing Care (6) | 5-point Likert scale | During postpartum stay at hospital | Yes |
| The Labor and Delivery Satisfaction Index/LADSI [31] | 38-items | No | 6-point Likert scale | 2 days postpartum and 4.6 weeks postpartum | Yes |
| Women’s delivery experience measures/MFRM [32] | 31-items | 7 dimensions | 4-point Likert scale | 24–48 h postpartum | No |
| The maternal satisfaction scale for caesarean section/MSS-caesarean section [35] | 22-items | 3 subscales: Anaesthetic (6 items), Side-effects (6 items), Atmosphere (10 items) | 7-point Likert scale | Not reported | Yes |
| The Satisfaction with childbirth experience questionnaire/SWCBE [48] | 32-items | No | 5-point Likert scale | Not reported | Yes |
| Women’s Perception of Control during Childbirth/PCCB [48] | 23-items | No | 5-point Likert scale | Not reported | Yes |
| The Childbirth Schema Scale/CSS [33] | 16-item pairs | 3 factors: Emotions of outcome (6 items), Sensation of the work of childbirth (4 items), Time (3 items), Preparation for control (3 items) | 7-point Likert scale | 1 month before and 2 weeks after birth | No |
| Satisfaction with obstetrical care/SSO [49] | 49- items | 5 dimensions: Nurse (14), doctor (14), anaesthetist (5), environment (9), global satisfaction (7) | 10-point Likert scale | 48 h postpartum | Yes |
| The Preterm Birth Experience and Satisfaction Scale/P-BESS [50] | 17-items | 3 dimensions: Staff professionalism and empathy, Information and explanations, Confidence in staff | 5-point Likert scale | Up to 12 months postpartum | No |
| The Responsivness in Perinatal and Obstetric Health Care Questionnaire/ReproQ [36] | 40-items | 8 domains: Dignity, Autonomy, Confidentiality, Communication, Prompt attention, Social consideration, Basic amenities, Choice and continuity. | Not reported | 6 weeks postpartum | Yes |
| Women’s Satisfaction With Hospital-Based Intrapartum Care Scale [51] | 14-items | 3 dimensions: Interpersonal care (5 items), Information and decision making (4 items), Physical birth environment (5 items) | Not reported | 2 months postpartum | No |
| Patient Perception Score/PPS [52] | 3-items | 3 items; communication, respect and safety | 5-point Likert scale | Within 24 h of birth | yes |
| Pregnancy- and maternity-care patients’ experiences questionnaire./PreMaPEQ [38] | 145-items in total | 4 parts in the questionnaire. One of these is Birth and have 3 subscales: Personal relationships in the delivery ward, Resources and organisation in the delivery ward, Attention to partner in the delivery ward. | 5 point Likert scal for single items and index scores were transformed linearly to a scale of 0–100. | From 17 weeks after birth | Yes |
| Women’s View of Birth Labour Satisfaction Questionnaire/WOMBLSQ [53] | Not reported | 10 dimensions in addition to general satisfaction | Not reported | Within 10 days of birth | No |
| The perceived Control in Childbirth Scale/PCCh [54] | 12- items | No | 6-point Likert scale | Prior to discharge | Yes |
| The Satisfaction with Childbirth Scale/SWCh [54] | 7-items | No | 7-point Likert scale | Prior to discharge | Yes |
| The Pregnancy and Childbirth Questionnaire/PCQ [55] | 25-items | Two scales: 18-items referring to pregnancy, 7-items referring to personal treatment during delivery. | 5-point Likert scale | Within 6 weeks of birth | No |
| The Childbirth Perception Scale/CPS [39] | 12-items | 2 dimensions; Perception of delivery (6-items), perception of first postpartum week (6-items) | 4-point Likert scale | 7 days postpartum | Yes |
| The Scale of Women’s Perception for Supportive Care Given During Labor [56] | 33-items | 3 subdimensions: Comfortable Behaviours (15-items), Education (8-items), Disturbing Behaviours (10 items) | 4-point Likert scale | Not reported | No |
| The Delivery Fear Scale/DFS [57] | 10-items | No | 10-point scale | During any moment of labor and delivery | Yes |
| The Wijma Delivery Expectancy/Experience Questionnaire/W-DEQ [40] | 29-items | No | 6-point Likert scale | Within 2 h of birth and 5 weeks after birth | Yes |
| The Parental Satisfaction and Quality Indicators of Perinatal Care Instrument [58, 59] | Intra-partum scale: 37 items Post-natal scale include an addit-ional 7 items |
3 scales: The Prenatal, The Intrapartum, The Postnatal Scale 8 domains: Structure and processes of care, physical aspects of care, psychological and psychiatric aspects of care, social aspects of care, spiritual, religious, and existential aspects of care, cultural aspects of care, care of the imminently dying patient, and ethical and legal aspects of care. | 7-point Likert scale | Not reported | No |
A few of the tools gained a low quality rating, which would indicate the need for further development and evaluation of their psychometric properties. These included: The Childbirth Trauma Index for adolescents [22] (overall quality mark of 2); The Perception of Birth Scale [23, 24] (overall quality marks of 3); Support and Control in Birth [25] (overall quality marks of 4); The Childbirth Experience Perception Questionnaire [26] and The Birth satisfaction scale and the Birth satisfaction scale - revised [27–29] (overall quality marks of 4.5); The Birth Memories and Recall Questionnaire [30], The labour and delivery satisfaction index [31] (an instrument developed and evaluated in 1987, and in need of further testing and updating of its psychometric properties), the Women’s delivery experience measures [32], and the Childbirth schema scale [33] (overall quality marks of 5).
In general, we would suggests that tools with marks of 2 to 4.5 are not suitable for use without further testing, especially if there is another existing tool that will serve the same purpose. Tools with a mark of 5 may be suitable if they are the only instrument developed in that topic area, but not otherwise, and further testing before use is recommended.
The majority of tools (20 out of 36, 56%) had marks of 6 or 6.5, which probably indicates a suitable tool, unless there is a higher quality one in the same area. We suggest that the seven instruments with marks of 7 to 9 (Table 2) can be considered valid and reliable although, of course, further testing is always welcome and could improve them further. These included: The Childbirth Experience Questionnaire [34], The maternal satisfaction scale for caesarean section [35], The Responsiveness in Perinatal and Obstetric Health Care Questionnaire [36, 37], Pregnancy and maternity care patients experiences questionnaire [38] and The Childbirth Perception Scale [39]. The tool with the highest quality rating, of 9, was the Wijma Delivery Expectancy/experience Questionnaire [40], an instrument measuring fear specific to labour and childbirth with one version used during pregnancy (version A) and one used after childbirth (version B). The Wijma Delivery Expectancy/experience questionnaire has been used extensively [60–66] and cultural validation and translations have been made in several countries [67–69]. As this scale is commonly used for measuring fear of childbirth, and it is properly developed with good psychometric properties, we recommend this scale for measuring women’s experience of fear in childbirth, when a detailed survey is necessary. However, a number of different cut-off points are used to define severe fear of childbirth, resulting in different prevalence rates, and these should be standardised.
Discussion
The purpose of this systematic review was to identify and analyse instruments that measure women’s childbirth experiences, and 46 papers representing 36 instruments were identified and included. By including surrogate terms and related concepts to the childbirth experiences, a broader and more holistic overview of existing instruments was achieved. Identified instruments demonstrated a wide range in purpose and content as well as in the quality of psychometric properties.
When choosing between different instruments, one needs to consider all ratings together as well as taking into account those measurement properties that are most important for a specific application, setting and population, e.g. practical aspects such as burden for women, and cost and quality aspects regarding the validity and reliability of the instrument [70]. If the researcher chooses an inappropriate or poor quality measurement instrument, this may lead to bias in the conclusion, resulting in wasted resources and unethical procedures for the women that participated [71]. Rudman [72] concluded that a multi-item instrument including different dimensions of care instead of a single global measure, gave a more diverse and richer picture of women’s childbirth experiences but also led to a more negative picture [72]. To choose the right instrument for clinicians and researchers for their specific context is a complex process. In our result we present an overview in Tables 1 and 2 of descriptive data and characteristics of instruments as well as a narrative summary of the individual instruments, which can aid in this process.
Terwee et al. [17] consider the content validity to be the single most important psychometric property of the questionnaire, and state that only if the content validity is adequate can the questionnaire be considered, and the remaining measurement properties become useful. All instruments in our review did get a positive rating of content validity. But a more thorough investigation would still be advisable to see which instruments have the strongest content validity to aid in choosing an appropriate instrument. Many of the instruments that we identified would need further testing of their psychometric properties to determine which would be best. This is consistent with the finding of Sawyer et al. [20], who evaluated nine questionnaires about women’s satisfaction during labour and birth, concluding that none of the questionnaires had optimal testing of validity and reliability. Most of the instruments in our review did report on several tests of psychometric properties, but further evaluation of validity and reliability was needed.
Among the excluded papers (Table 1) there are several questionnaires developed that were not included in this review as they did not report on psychometric properties [73] or the focus was on a study rather than development of the instrument [72, 74]. Before using a specific instrument, we suggest that a thorough investigation of the development and testing of the instrument should be done to ensure good psychometric properties. In the US Food and Drug Administration’s guidelines on developing new patient-reported outcome measures, they suggest that a new instrument can be developed by modifying an existing one [18]. As we found a large number of questionnaires and instruments, we agree with this suggestion. When conducting studies of psychometric properties of an instrument, we recommend applying standards such as the COSMIN checklist [75, 76] and Terwee et al.’s criteria [17] in order to enhance the quality of the results and to facilitate the researcher to compare and find an instrument with good psychometric properties.
Several of the papers included in our review consisted of development and validation of existing questionnaires [23, 26, 41]. As well, several of the questionnaires have been culturally translated and validated in other languages and cultures [67–69, 77–80].
Methodological considerations
The attempt with this review was to identify all studies and instruments that meet the eligibility criteria, but it is possible that we have missed relevant articles, written in other languages than English and French, or indexed in other databases than those chosen. A limitation of this search was that we did not use Terwee et al’s PubMed search filter [81] which may have generated more papers. We suggest that this review can be used as a tool for identification of existing instruments, while acknowledging that each researcher will have to assess their chosen tool themselves in the light of the lack of, in most cases, sufficient testing. Terwee et al. [82] raised in their discussion of the quality of systematic reviews of health related outcome measurement the need for reviewers to make strong recommendations. Our review consists of a large number and wide range of instruments, making it difficult to make those recommendations, particularly as a more thorough evaluation of psychometric properties and quality assessment of included studies was needed. Nevertheless, we have made some suggestions in relation to use of tools depending on their overall quality score. As we chose to include instruments that use surrogate terms and related concepts to women’s childbirth experiences this review presents for researchers and clinicians the diversity of instruments developed. For assessing methodological quality, the COSMIN checklist has newly been developed. It is a detailed and rigorous checklist [75, 76], useful in future systematic literature reviews that have a more narrowed construct of interest, so it could be manageable to do a more in-depth assessment of each instrument comprising both psychometric properties and methodological quality of the development process of each instrument.
Conclusions
This systematic review provides an overview of existing instruments measuring women’s childbirth experiences and can support researchers to identify an appropriate instrument for their research purpose. Most of the instruments require further validation and reliability testing. Given the plethora of instruments in use in the literature, and the lack of complete testing for many of them, we recommend that researchers do not develop any more new tools, but try to test thoroughly, adapt and improve those that already exist.
Researchers and clinicians need help in finding and selecting the most suitable instrument for their purpose. This makes reviews of measurement instruments important as they aid researchers in finding appropriate, established and tested instruments instead of developing new ones. When different instruments are used to measure the same construct of interest, e.g. women’s experiences of caesarean section, it can become difficult in systematic reviews to compare and statistically report the results. We trust that this review can contribute in helping clinicians and researchers to find the right instrument for their specific context.
Additional files
Review protocol. (DOCX 17 kb)
Search strategy. (DOCX 15 kb)
Acknowledgments
We thank librarian Tobias Prenler at Gothenburg university library who provided support and knowledge in develop and perform the literature search. We thank collaborator Jenny Carlsson (JC), RM, MSc, for co-screening articles for initial inclusion/exclusion.
Funding
This study was not funded.
Availability of data and materials
Not applicable.
Authors’ contributions
HN, MB and CB planned the study. HN conducted the literature search and initial screening of papers. HN and MB screened papers for full text assessment. All authors screened full text articles for inclusion and were involved with quality assessment of included instruments. HN extracted descriptive data and characteristics of included instruments. This was checked by MB and CB. HN drafted the manuscript. All authors contributed to the intellectual content, read and approved the final manuscript.
Competing interests
One of the reviewers, MB, was involved in the development and validation of the Childbirth experience questionnaire [30], one of the instruments included in the review. The inclusion and quality assessment where therefore assessed and evaluated by the other two reviewers (HN and CB).
Consent for publication
Not applicable.
Ethics approval and consent to participate
This is a systematic review of already published primary sources and as such no further ethical approval was required.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Footnotes
Electronic supplementary material
The online version of this article (doi:10.1186/s12884-017-1356-y) contains supplementary material, which is available to authorized users.
Contributor Information
Helena Nilvér, Email: helena.nilver@gmail.com.
Cecily Begley, Email: cbegley@tcd.ie.
Marie Berg, Email: marie.berg@fhs.gu.se.
References
- 1.Lundgren I. Swedish women’s experience of childbirth 2 years after birth. Midwifery. 2005;21(4):346–354. doi: 10.1016/j.midw.2005.01.001. [DOI] [PubMed] [Google Scholar]
- 2.Simkin P. Just another day in a woman’s life? Women’s long-term perceptions of their first birth experience. Part I. Birth. 1991;18(4):203–210. doi: 10.1111/j.1523-536X.1991.tb00103.x. [DOI] [PubMed] [Google Scholar]
- 3.Simkin P. Just another day in a woman’s life? Part II: Nature and consistency of women’s long-term memories of their first birth experiences. Birth. 1992;19(2):64–81. doi: 10.1111/j.1523-536X.1992.tb00382.x. [DOI] [PubMed] [Google Scholar]
- 4.Nelson AM. Transition to motherhood. J Obstet Gynecol Neonatal Nurs. 2003;32(4):465–477. doi: 10.1177/0884217503255199. [DOI] [PubMed] [Google Scholar]
- 5.Bell AF, Andersson E. The birth experience and women’s postnatal depression: A systematic review. Midwifery. 2016;39:112–123. doi: 10.1016/j.midw.2016.04.014. [DOI] [PubMed] [Google Scholar]
- 6.Nilsson C, Lundgren I, Karlstrom A, Hildingsson I. Self reported fear of childbirth and its association with women’s birth experience and mode of delivery: a longitudinal population-based study. Women Birth. 2012;25(3):114–121. doi: 10.1016/j.wombi.2011.06.001. [DOI] [PubMed] [Google Scholar]
- 7.Hildingsson I, Radestad I, Rubertsson C, Waldenstrom U. Few women wish to be delivered by caesarean section. BJOG. 2002;109(6):618–623. doi: 10.1111/j.1471-0528.2002.01393.x. [DOI] [PubMed] [Google Scholar]
- 8.Pang MW, Leung TN, Lau TK, Hang Chung TK. Impact of first childbirth on changes in women’s preference for mode of delivery: follow-up of a longitudinal observational study. Birth. 2008;35(2):121–128. doi: 10.1111/j.1523-536X.2008.00225.x. [DOI] [PubMed] [Google Scholar]
- 9.Gottvall K, Waldenstrom U. Does a traumatic birth experience have an impact on future reproduction? BJOG. 2002;109(3):254–260. doi: 10.1111/j.1471-0528.2002.01200.x. [DOI] [PubMed] [Google Scholar]
- 10.Larkin P, Begley CM, Devane D. ‘Not enough people to look after you’: an exploration of women’s experiences of childbirth in the Republic of Ireland. Midwifery. 2012;28(1):98–105. doi: 10.1016/j.midw.2010.11.007. [DOI] [PubMed] [Google Scholar]
- 11.Waldenstrom U. Women’s memory of childbirth at two months and one year after the birth. Birth. 2003;30(4):248–254. doi: 10.1046/j.1523-536X.2003.00254.x. [DOI] [PubMed] [Google Scholar]
- 12.Fayers PM, Machin D, Ebooks C. Quality of Life: the assessment, analysis and interpretation of patient-reported outcomes. Chichester: John Wiley & Sons, Ltd; 2007. [Google Scholar]
- 13.World Health Organization . WHO Statment: The prevention and elimiation of disrespect and abuse during facility-based childbirth. 2014. [Google Scholar]
- 14.Bohren MA, Vogel JP, Hunter EC, Lutsiv O, Makh SK, Souza JP, Aguiar C, Saraiva Coneglian F, Diniz AL, Tuncalp O, et al. The Mistreatment of Women during Childbirth in Health Facilities Globally: A Mixed-Methods Systematic Review. PLoS Med. 2015;12(6):e1001847. doi: 10.1371/journal.pmed.1001847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Larkin P, Begley CM, Devane D. Women’s experiences of labour and birth: an evolutionary concept analysis. Midwifery. 2009;25(2):e49–e59. doi: 10.1016/j.midw.2007.07.010. [DOI] [PubMed] [Google Scholar]
- 16.Goodman P, Mackey MC, Tavakoli AS. Factors related to childbirth satisfaction. J Adv Nurs. 2004;46(2):212–219. doi: 10.1111/j.1365-2648.2003.02981.x. [DOI] [PubMed] [Google Scholar]
- 17.Terwee CB, Bot SD, de Boer MR, van der Windt DA, Knol DL, Dekker J, Bouter LM, de Vet HC. Quality criteria were proposed for measurement properties of health status questionnaires. J Clin Epidemiol. 2007;60(1):34–42. doi: 10.1016/j.jclinepi.2006.03.012. [DOI] [PubMed] [Google Scholar]
- 18.US Department of Helath and Human Services. Food and Drug Administration . Guidance for industry: patient-reported outcome measures: use in medical product development to support labeling claims. 2009. [Google Scholar]
- 19.Perriman N, Davis D. Measuring maternal satisfaction with maternity care: A systematic integrative review: What is the most appropriate, reliable and valid tool that can be used to measure maternal satisfaction with continuity of maternity care? Women Birth. 2016;29(3):293–299. doi: 10.1016/j.wombi.2015.12.004. [DOI] [PubMed] [Google Scholar]
- 20.Sawyer A, Ayers S, Abbott J, Gyte G, Rabe H, Duley L. Measures of satisfaction with care during labour and birth: a comparative review. BMC Pregnancy Childbirth. 2013;13:108. doi: 10.1186/1471-2393-13-108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Higgins JPT & Green S. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. Cochrane Collaboration. 2011. Available from www.handbook.cochrane.org.
- 22.Anderson C. Construct validity of the childbirth trauma index for adolescents. J Perinat Educ. 2011;20(2):78–90. doi: 10.1891/1058-1243.20.2.78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fawcett J, Knauth D. The factor structure of the perception of birth scale. Nurs Res. 1996;45(2):83–86. doi: 10.1097/00006199-199603000-00005. [DOI] [PubMed] [Google Scholar]
- 24.Marut JS, Mercer RT. Comparison of primiparas’ perceptions of vaginal and cesarean births. Nurs Res. 1979;28(5):260–266. doi: 10.1097/00006199-197909000-00002. [DOI] [PubMed] [Google Scholar]
- 25.Ford E, Ayers S, Wright DB. Measurement of maternal perceptions of support and control in birth (SCIB) J Womens Health (Larchmt) 2009;18(2):245–252. doi: 10.1089/jwh.2008.0882. [DOI] [PubMed] [Google Scholar]
- 26.Bertucci V, Boffo M, Mannarini S, Serena A, Saccardi C, Cosmi E, Andrisani A, Ambrosini G. Assessing the perception of the childbirth experience in Italian women: A contribution to the adaptation of the childbirth perception questionnaire. Midwifery. 2012;28(2):265–274. doi: 10.1016/j.midw.2011.02.009. [DOI] [PubMed] [Google Scholar]
- 27.Hollins Martin C, Fleming V. The birth satisfaction scale. Int J Health Care Qual Assur. 2011;24(2):124–135. doi: 10.1108/09526861111105086. [DOI] [PubMed] [Google Scholar]
- 28.Hollins Martin CJ, Martin CR. Development and psychometric properties of the Birth Satisfaction Scale-Revised (BSS-R) Midwifery. 2014;30(6):610–619. doi: 10.1016/j.midw.2013.10.006. [DOI] [PubMed] [Google Scholar]
- 29.Hollins Martin CJ, Snowden A, Martin CR. Concurrent analysis: Validation of the domains within the Birth Satisfaction Scale. J Reprod Infant Psychol. 2012;30(3):247–260. doi: 10.1080/02646838.2012.710833. [DOI] [Google Scholar]
- 30.Foley S, Crawley R, Wilkie S, Ayers S. The Birth Memories and Recall Questionnaire (BirthMARQ): development and evaluation. BMC Pregnancy Childbirth. 2014;14:211. doi: 10.1186/1471-2393-14-211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lomas J, Dore S, Enkin M, Mitchell A. The Labor and Delivery Satisfaction Index: the development and evaluation of a soft outcome measure. Birth. 1987;14(3):125–129. doi: 10.1111/j.1523-536X.1987.tb01472.x. [DOI] [PubMed] [Google Scholar]
- 32.Mannarini S, Boffo M, Bertucci V, Andrisani A, Ambrosini G. A Rasch-based dimension of delivery experience: spontaneous vs. medically assisted conception. J Clin Nurs. 2013;22(17–18):2404–2416. doi: 10.1111/jocn.12264. [DOI] [PubMed] [Google Scholar]
- 33.Peirce AG. Cognitive appraisal of stress events: measuring the personal schema of childbirth. J Nurs Meas. 1994;2(2):117–127. [PubMed] [Google Scholar]
- 34.Dencker A, Taft C, Bergqvist L, Lilja H, Berg M. Childbirth experience questionnaire (CEQ): development and evaluation of a multidimensional instrument. BMC Pregnancy Childbirth. 2010;10:81. doi: 10.1186/1471-2393-10-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Morgan PJ, Halpern S, Lo J. The development of a maternal satisfaction scale for caesarean section. Int J Obstet Anesth. 1999;8(3):165–170. doi: 10.1016/S0959-289X(99)80132-0. [DOI] [PubMed] [Google Scholar]
- 36.Scheerhagen M, van Stel HF, Birnie E, Franx A, Bonsel GJ. Measuring client experiences in maternity care under change: development of a questionnaire based on the WHO Responsiveness model. PLoS One. 2015;10(2):e0117031. doi: 10.1371/journal.pone.0117031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.van der Kooy J, Valentine NB, Birnie E, Vujkovic M, de Graaf JP, Denktas S, Steegers EA, Bonsel GJ. Validity of a questionnaire measuring the world health organization concept of health system responsiveness with respect to perinatal services in the Dutch obstetric care system. BMC Health Serv Res. 2014;14:622. doi: 10.1186/s12913-014-0622-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sjetne IS, Iversen HH, Kjollesdal JG. A questionnaire to measure women’s experiences with pregnancy, birth and postnatal care: instrument development and assessment following a national survey in Norway. BMC Pregnancy Childbirth. 2015;15:182. doi: 10.1186/s12884-015-0611-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Truijens SE, Wijnen HA, Pommer AM, Oei SG, Pop VJ. Development of the Childbirth Perception Scale (CPS): perception of delivery and the first postpartum week. Arch Womens Ment Health. 2014;17(5):411–421. doi: 10.1007/s00737-014-0420-0. [DOI] [PubMed] [Google Scholar]
- 40.Wijma K, Wijma B, Zar M. Psychometric aspects of the W-DEQ; a new questionnaire for the measurement of fear of childbirth. J Psychosom Obstet Gynaecol. 1998;19(2):84–97. doi: 10.3109/01674829809048501. [DOI] [PubMed] [Google Scholar]
- 41.Duff LA, Lamping DL, Ahmed LB. Evaluating satisfaction with maternity care in women from minority ethnic communities: development and validation of a Sylheti questionnaire. Int J Qual Health Care. 2001;13(3):215–230. doi: 10.1093/intqhc/13.3.215. [DOI] [PubMed] [Google Scholar]
- 42.Dunne CL, Fraser J, Gardner GE. Women’s perceptions of social support during labour: development, reliability and validity of the Birth Companion Support Questionnaire. Midwifery. 2014;30(7):847–852. doi: 10.1016/j.midw.2013.10.010. [DOI] [PubMed] [Google Scholar]
- 43.Gerbaud L, Mascart M, Belgacem B, Lejeune ML, Lacombe C, Prunayre M, Mille P, Lemery D, Buisson J, Colomb A, et al. Development of a self-administered questionnaire to assess women’s satisfaction with maternity care. J Gynecol Obstet Biol Reprod (Paris) 2003;32(2):139–156. [PubMed] [Google Scholar]
- 44.Gungor I, Beji NK. Development and psychometric testing of the scales for measuring maternal satisfaction in normal and caesarean birth. Midwifery. 2012;28(3):348–357. doi: 10.1016/j.midw.2011.03.009. [DOI] [PubMed] [Google Scholar]
- 45.Gärtner FR, De Miranda E, Rijnders ME, Freeman LM, Middeldorp JM, Bloemenkamp KWM, Stiggelbout AM, Van Den Akker-Van Marle ME. Good reliability and validity for a new utility instrument measuring the birth experience, the Labor and Delivery Index. J Clin Epidemiol. 2015;68(10):1184–1194. doi: 10.1016/j.jclinepi.2015.05.020. [DOI] [PubMed] [Google Scholar]
- 46.Hodnett ED, Simmons-Tropea DA. The Labour Agentry Scale: psychometric properties of an instrument measuring control during childbirth. Res Nurs Health. 1987;10(5):301–310. doi: 10.1002/nur.4770100503. [DOI] [PubMed] [Google Scholar]
- 47.Janssen PA, Desmarais SL. Development and psychometric properties of the Early Labour Experience Questionnaire (ELEQ) Midwifery. 2013;29(3):181–189. doi: 10.1016/j.midw.2012.05.012. [DOI] [PubMed] [Google Scholar]
- 48.Oweis A. Jordanian mother’s report of their childbirth experience: findings from a questionnaire survey. Int J Nurs Pract. 2009;15(6):525–533. doi: 10.1111/j.1440-172X.2009.01774.x. [DOI] [PubMed] [Google Scholar]
- 49.Ramanah R, Dumont A, Schepens F, Traore M, Gaye A, Schaal JP, Riethmuller D, Rude N. Satisfaction with obstetrical care: development and validation of a scale on quality of care. Gynecol Obstet Fertil. 2014;42(7–8):477–482. doi: 10.1016/j.gyobfe.2014.05.002. [DOI] [PubMed] [Google Scholar]
- 50.Sawyer A, Rabe H, Abbott J, Gyte G, Duley L, Ayers S. Measuring parents’ experiences and satisfaction with care during very preterm birth: a questionnaire development study. BJOG. 2014;121(10):1294–1301. doi: 10.1111/1471-0528.12925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Shaban I, Mohammad K, Homer C. Development and Validation of Women’s Satisfaction With Hospital-Based Intrapartum Care Scale in Jordan. J Transcult Nurs. 2016;27(3):256–261. [DOI] [PubMed]
- 52.Siassakos D, Clark J, Sibanda T, Attilakos G, Jefferys A, Cullen L, Bisson D, Draycott T. A simple tool to measure patient perceptions of operative birth. BJOG. 2009;116(13):1755–1761. doi: 10.1111/j.1471-0528.2009.02363.x. [DOI] [PubMed] [Google Scholar]
- 53.Smith LF. Development of a multidimensional labour satisfaction questionnaire: dimensions, validity, and internal reliability. Qual Health Care. 2001;10(1):17–22. doi: 10.1136/qhc.10.1.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Stevens NR, Wallston KA, Hamilton NA. Perceived control and maternal satisfaction with childbirth: a measure development study. J Psychosom Obstet Gynaecol. 2012;33(1):15–24. doi: 10.3109/0167482X.2011.652996. [DOI] [PubMed] [Google Scholar]
- 55.Truijens SE, Pommer AM, van Runnard Heimel PJ, Verhoeven CJ, Oei SG, Pop VJ. Development of the Pregnancy and Childbirth Questionnaire (PCQ): evaluating quality of care as perceived by women who recently gave birth. Eur J Obstet Gynecol Reprod Biol. 2014;174:35–40. doi: 10.1016/j.ejogrb.2013.11.019. [DOI] [PubMed] [Google Scholar]
- 56.Uludag E, Mete S. Development and Testing of Women’s Perception for the Scale of Supportive Care Given During Labor. Pain Manag Nurs. 2015;16(5):751–758. doi: 10.1016/j.pmn.2015.05.001. [DOI] [PubMed] [Google Scholar]
- 57.Wijma K, Alehagen S, Wijma B. Development of the Delivery Fear Scale. J Psychosom Obstet Gynaecol. 2002;23(2):97–107. doi: 10.3109/01674820209042791. [DOI] [PubMed] [Google Scholar]
- 58.Wool C. Instrument development: Parental satisfaction and quality indicators of perinatal palliative care. J Hosp Palliat Nurs. 2015;17(4):301–308. doi: 10.1097/NJH.0000000000000163. [DOI] [PubMed] [Google Scholar]
- 59.Wool C. Instrument Psychometrics: Parental Satisfaction and Quality Indicators of Perinatal Palliative Care. J Palliat Med. 2015;18(10):872–877. doi: 10.1089/jpm.2015.0135. [DOI] [PubMed] [Google Scholar]
- 60.Carlsson IM, Ziegert K, Nissen E. The relationship between childbirth self-efficacy and aspects of well-being, birth interventions and birth outcomes. Midwifery. 2015;31(10):1000–1007. doi: 10.1016/j.midw.2015.05.005. [DOI] [PubMed] [Google Scholar]
- 61.Christiaens W, Verhaeghe M, Bracke P. Childbirth expectations and experiences in Belgian and Dutch models of maternity care. J Reprod Infant Psychol. 2008;26(4):309–322. doi: 10.1080/02646830802350872. [DOI] [Google Scholar]
- 62.Fenwick J, Gamble J, Nathan E, Bayes S, Hauck Y. Pre- and postpartum levels of childbirth fear and the relationship to birth outcomes in a cohort of Australian women. J Clin Nurs. 2009;18(5):667–677. doi: 10.1111/j.1365-2702.2008.02568.x. [DOI] [PubMed] [Google Scholar]
- 63.Larsson C, Saltvedt S, Edman G, Wiklund I, Andolf E. Factors independently related to a negative birth experience in first-time mothers. Sex Reprod Healthc. 2011;2(2):83–89. doi: 10.1016/j.srhc.2010.11.003. [DOI] [PubMed] [Google Scholar]
- 64.Rouhe H, Salmela-Aro K, Toivanen R, Tokola M, Halmesmaki E, Saisto T. Life satisfaction, general well-being and costs of treatment for severe fear of childbirth in nulliparous women by psychoeducative group or conventional care attendance. Acta Obstet Gynecol Scand. 2015;94(5):527–533. doi: 10.1111/aogs.12594. [DOI] [PubMed] [Google Scholar]
- 65.Sluijs AM, Cleiren MP, Scherjon SA, Wijma K. No relationship between fear of childbirth and pregnancy-/delivery-outcome in a low-risk Dutch pregnancy cohort delivering at home or in hospital. J Psychosom Obstet Gynaecol. 2012;33(3):99–105. doi: 10.3109/0167482X.2012.685905. [DOI] [PubMed] [Google Scholar]
- 66.Ulfsdottir H, Nissen E, Ryding EL, Lund-Egloff D, Wiberg-Itzel E. The association between labour variables and primiparous women’s experience of childbirth; a prospective cohort study. BMC Pregnancy Childbirth. 2014;14:208. doi: 10.1186/1471-2393-14-208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Fenaroli V, Saita E. Fear of childbirth: A contribution to the validation of the Italian version of the Wijma Delivery Expectancy/Experience Questionnaire (WDEQ) TPM - Testing, Psychometrics, Methodology in Applied Psychology. 2013;20(2):131–154. [Google Scholar]
- 68.Korukcu O, Bulut O, Kukulu K. Psychometric Evaluation of the Wijma Delivery Expectancy/Experience Questionnaire Version B. Health Care Women Int. 2014;37(5):1–18. doi: 10.1080/07399332.2014.943838. [DOI] [PubMed] [Google Scholar]
- 69.Korukcu O, Kukulu K, Firat MZ. The reliability and validity of the Turkish version of the Wijma Delivery Expectancy/Experience Questionnaire (W-DEQ) with pregnant women. J Psychiatr Ment Health Nurs. 2012;19(3):193–202. doi: 10.1111/j.1365-2850.2011.01694.x. [DOI] [PubMed] [Google Scholar]
- 70.Mokkink LB, Terwee CB, Patrick DL, Alonso J, Stratford PW, Knol DL, Bouter LM, de Vet HC. The COSMIN study reached international consensus on taxonomy, terminology, and definitions of measurement properties for health-related patient-reported outcomes. J Clin Epidemiol. 2010;63(7):737–745. doi: 10.1016/j.jclinepi.2010.02.006. [DOI] [PubMed] [Google Scholar]
- 71.Ioannidis JP, Greenland S, Hlatky MA, Khoury MJ, Macleod MR, Moher D, Schulz KF, Tibshirani R. Increasing value and reducing waste in research design, conduct, and analysis. Lancet. 2014;383(9912):166–175. doi: 10.1016/S0140-6736(13)62227-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Rudman A, El-Khouri B, Waldenstrom U. Women’s satisfaction with intrapartum care - a pattern approach. J Adv Nurs. 2007;59(5):474–487. doi: 10.1111/j.1365-2648.2007.04323.x. [DOI] [PubMed] [Google Scholar]
- 73.Padawer JA, Fagan C, Janoff-Bulman R, Strickland BR, Chorowski M. Women’s psychological adjustment following emergency cesarean versus vaginal delivery. Psychol Women Q. 1988;12(1):25–34. doi: 10.1111/j.1471-6402.1988.tb00925.x. [DOI] [Google Scholar]
- 74.Salmon P, Miller R, Drew NC. Women’s anticipation and experience of childbirth: the independence of fulfillment, unpleasantness and pain. Br J Med Psychol. 1990;63:255–259. doi: 10.1111/j.2044-8341.1990.tb01617.x. [DOI] [PubMed] [Google Scholar]
- 75.Mokkink LB, Prinsen CA, Bouter LM, Vet HC, Terwee CB. The COnsensus-based Standards for the selection of health Measurement INstruments (COSMIN) and how to select an outcome measurement instrument. Braz J Phys Ther. 2016;20(2):105–113. doi: 10.1590/bjpt-rbf.2014.0143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Mokkink LB, Terwee CB, Patrick DL, Alonso J, Stratford PW, Knol DL, Bouter LM, de Vet HC. The COSMIN checklist for assessing the methodological quality of studies on measurement properties of health status measurement instruments: an international Delphi study. Qual Life Res. 2010;19(4):539–549. doi: 10.1007/s11136-010-9606-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Walker KF, Wilson P, Bugg GJ, Dencker A, Thornton JG. Childbirth experience questionnaire: validating its use in the United Kingdom. BMC Pregnancy Childbirth. 2015;15:86. doi: 10.1186/s12884-015-0513-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Inci F, Gokce Isbir G, Tanhan F. The Turkish version of perceived support and control in birth scale. J Psychosom Obstet Gynaecol. 2015;36(3):103–113. doi: 10.3109/0167482X.2015.1073708. [DOI] [PubMed] [Google Scholar]
- 79.Barbosa-Leiker C, Fleming S, Hollins Martin CJ, Martin CR. Psychometric properties of the Birth Satisfaction Scale-Revised (BSS-R) for US mothers. J Reprod Infant Psychol. 2015;33(5):504–511. doi: 10.1080/02646838.2015.1024211. [DOI] [Google Scholar]
- 80.Vardavaki Z, Hollins Martin CJ, Martin CR. Construct and content validity of the Greek version of the Birth Satisfaction Scale (G-BSS) J Reprod Infant Psychol. 2015;33(5):488–503. doi: 10.1080/02646838.2015.1035235. [DOI] [Google Scholar]
- 81.Terwee CB, Jansma EP, Riphagen II, de Vet HC. Development of a methodological PubMed search filter for finding studies on measurement properties of measurement instruments. Qual Life Res. 2009;18(8):1115–1123. doi: 10.1007/s11136-009-9528-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Terwee CB, Prinsen CA, Ricci Garotti MG, Suman A, de Vet HC, Mokkink LB. The quality of systematic reviews of health-related outcome measurement instruments. Qual Life Res. 2016;25(4):767–779. doi: 10.1007/s11136-015-1122-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Mannarini S, Boffo M. Reply to ‘Measurement validity of childbirth perceptions’ by H. Shepherd and L.L. Glenn. Midwifery. 2013;29(5):e28–e29. doi: 10.1016/j.midw.2012.09.007. [DOI] [PubMed] [Google Scholar]
- 84.Shepherd HL, Glenn LL. Measurement validity of childbirth perceptions. Midwifery. 2013;29(5):e27. doi: 10.1016/j.midw.2012.08.004. [DOI] [PubMed] [Google Scholar]
- 85.Toivonen E, Palomaki O, Huhtala H, Uotila J. Maternal experiences of vaginal breech delivery. Birth. 2014;41(4):316–322. doi: 10.1111/birt.12119. [DOI] [PubMed] [Google Scholar]
- 86.Samko MR, Schoenfeld LS. Hypnotic susceptibility and the Lamaze childbirth experience. Am J Obstet Gynecol. 1975;121(5):631–636. doi: 10.1016/0002-9378(75)90464-0. [DOI] [PubMed] [Google Scholar]
- 87.Cranley MS, Hedahl KJ, Pegg SH. Women’s perceptions of vaginal and cesarean deliveries. Nurs Res. 1983;32(1):10–15. doi: 10.1097/00006199-198301000-00003. [DOI] [PubMed] [Google Scholar]
- 88.Mercer RT, Hackley KC, Bostrom AG. Relationship of psychosocial and perinatal variables to perception of childbirth. Nurs Res. 1983;32(4):202–207. doi: 10.1097/00006199-198307000-00004. [DOI] [PubMed] [Google Scholar]
- 89.Calisir H, Karacam Z. Factors associated with parenting behavior of mothers in the early postpartum period in Turkey. Nurs Health Sci. 2011;13(4):488–494. doi: 10.1111/j.1442-2018.2011.00646.x. [DOI] [PubMed] [Google Scholar]
- 90.Cheung W, Ip WY, Chan D. Maternal anxiety and feelings of control during labour: a study of Chinese first-time pregnant women. Midwifery. 2007;23(2):123–130. doi: 10.1016/j.midw.2006.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Geerts CC, Klomp T, Lagro-Janssen AL, Twisk JW, van Dillen J, de Jonge A. Birth setting, transfer and maternal sense of control: results from the DELIVER study. BMC Pregnancy Childbirth. 2014;14:27. doi: 10.1186/1471-2393-14-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Goffinet F, Dreyfus M, Carbonne B, Magnin G, Cabrol D. Survey of the practice of cervical ripening and labor induction in France. J Gynecol Obstet Biol Reprod (Paris) 2003;32(7):638–646. [PubMed] [Google Scholar]
- 93.Iida M, Horiuchi S, Porter SE. The relationship between women-centred care and women’s birth experiences: a comparison between birth centres, clinics, and hospitals in Japan. Midwifery. 2012;28(4):398–405. doi: 10.1016/j.midw.2011.07.002. [DOI] [PubMed] [Google Scholar]
- 94.Janssen PA, Carty EA, Reime B. Satisfaction with planned place of birth among midwifery clients in British Columbia. J Midwifery Women’s Health. 2006;51(2):91–97. doi: 10.1016/j.jmwh.2005.10.012. [DOI] [PubMed] [Google Scholar]
- 95.Lee SL, Liu CY, Lu YY, Gau ML. Efficacy of warm showers on labor pain and birth experiences during the first labor stage. J Obstet Gynecol Neonatal Nurs. 2013;42(1):19–28. doi: 10.1111/j.1552-6909.2012.01424.x. [DOI] [PubMed] [Google Scholar]
- 96.Sapkota S, Kobayashi T, Kakehashi M, Baral G, Yoshida I. In the Nepalese context, can a husband’s attendance during childbirth help his wife feel more in control of labour? BMC Pregnancy Childbirth. 2012;12:49. doi: 10.1186/1471-2393-12-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Hollins Martin CJ, Robb Y. Women’s views about the importance of education in preparation for childbirth. Nurse Educ Pract. 2013;13(6):512–518. doi: 10.1016/j.nepr.2013.02.013. [DOI] [PubMed] [Google Scholar]
- 98.Belanger-Levesque MN, Pasquier M, Roy-Matton N, Blouin S, Pasquier JC. Maternal and paternal satisfaction in the delivery room: a cross-sectional comparative study. BMJ Open. 2014;4(2):e004013. doi: 10.1136/bmjopen-2013-004013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Hinic KA. The relationships among perceived stress, birth satisfaction, and breastfeeding self-efficacy in early postpartum women. New Jersey; Seton Hall University. vol. Ph.D. 2015.
- 100.Fleming SE, Donovan-Batson C, Burduli E, Barbosa-Leiker C, Hollins Martin CJ, Martin CR. Birth Satisfaction Scale/Birth Satisfaction Scale-Revised (BSS/BSS-R): A large scale United States planned home birth and birth centre survey. Midwifery. 2016;41:9–15. doi: 10.1016/j.midw.2016.07.008. [DOI] [PubMed] [Google Scholar]
- 101.Janssen PA, Desmarais SL. Women’s experience with early labour management at home vs. in hospital: a randomised controlled trial. Midwifery. 2013;29(3):190–194. doi: 10.1016/j.midw.2012.05.011. [DOI] [PubMed] [Google Scholar]
- 102.Bernitz S, Oian P, Sandvik L, Blix E. Evaluation of satisfaction with care in a midwifery unit and an obstetric unit: a randomized controlled trial of low-risk women. BMC Pregnancy Childbirth. 2016;16(1):143. doi: 10.1186/s12884-016-0932-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Harvey S, Rach D, Stainton MC, Jarrell J, Brant R. Evaluation of satisfaction with midwifery care. Midwifery. 2002;18(4):260–267. doi: 10.1054/midw.2002.0317. [DOI] [PubMed] [Google Scholar]
- 104.Letts PJ, Baker PRA, Ruderman J, Kennedy K. The use of hypnosis in labor and delivery: a preliminary study. J Women’s Health. 1993;2(4):335–341. doi: 10.1089/jwh.1993.2.335. [DOI] [Google Scholar]
- 105.Scheerhagen M, van Stel HF, Tholhuijsen DJ, Birnie E, Franx A, Bonsel GJ. Applicability of the ReproQ client experiences questionnaire for quality improvement in maternity care. PeerJ. 2016;4:e2092. doi: 10.7717/peerj.2092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Hitzert M, Hermus MA, Scheerhagen M, Boesveld IC, Wiegers TA, van den Akker-van Marle ME, van Dommelen P, van der Pal-de Bruin KM, de Graaf JP. Experiences of women who planned birth in a birth centre compared to alternative planned places of birth. Results of the Dutch Birth Centre Study. Midwifery. 2016;40:70–78. doi: 10.1016/j.midw.2016.06.004. [DOI] [PubMed] [Google Scholar]
- 107.Hickson GB, Clayton EW, Entman SS, Miller CS, Githens PB, Whetten-Goldstein K, Sloan FA. Obstetricians’ prior malpractice experience and patients’ satisfaction with care. JAMA. 1994;272(20):1583–1587. doi: 10.1001/jama.1994.03520200039032. [DOI] [PubMed] [Google Scholar]
- 108.Floris L, Mermillod B, Chastonay P. Translation and validation in French of a multidimensional scale to evaluate the degree of satisfaction during childbirth. Rev Epidemiol Sante Publique. 2010;58(1):13–22. doi: 10.1016/j.respe.2009.09.005. [DOI] [PubMed] [Google Scholar]
- 109.Marin-Morales D, Carmona-Monge FJ, Penacoba-Puente C, Olmos Albacete R, Toro Molina S. Factor structure, validity, and reliability of the Spanish version of the Women’s Views of Birth Labour Satisfaction Questionnaire. Midwifery. 2013;29(12):1339–1345. doi: 10.1016/j.midw.2012.12.015. [DOI] [PubMed] [Google Scholar]
- 110.Frauenfelder S, van Rijn R, Radder CM, de Vries MC, Dijksman LM, Godfried MB. Patient satisfaction between remifentanil patient-controlled analgesia and epidural analgesia for labor pain. Acta Obstet Gynecol Scand. 2015;94(9):1014–1021. doi: 10.1111/aogs.12694. [DOI] [PubMed] [Google Scholar]
- 111.Banga FR, Truijens SE, Fransen AF, Dieleman JP, van Runnard Heimel PJ, Oei GS. The impact of transmural multiprofessional simulation-based obstetric team training on perinatal outcome and quality of care in the Netherlands. BMC Med Educ. 2014;14:175. doi: 10.1186/1472-6920-14-175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Truijens SE, Banga FR, Fransen AF, Pop VJ, van Runnard Heimel PJ, Oei SG. The Effect of Multiprofessional Simulation-Based Obstetric Team Training on Patient-Reported Quality of Care: A Pilot Study. Simul Healthc. 2015;10(4):210–216. doi: 10.1097/SIH.0000000000000099. [DOI] [PubMed] [Google Scholar]
- 113.Alehagen S, Wijma K, Wijma B. Fear during labor. Acta Obstet Gynecol Scand. 2001;80(4):315–320. doi: 10.1034/j.1600-0412.2001.080004315.x. [DOI] [PubMed] [Google Scholar]
- 114.Jespersen C, Hegaard HK, Schroll AM, Rosthoj S, Kjaergaard H. Fear of childbirth and emergency caesarean section in low-risk nulliparous women: a prospective cohort study. J Psychosom Obstet Gynaecol. 2014;35(4):109–115. doi: 10.3109/0167482X.2014.952277. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Review protocol. (DOCX 17 kb)
Search strategy. (DOCX 15 kb)
Data Availability Statement
Not applicable.


