Abstract
Objective:
The objective of the following study was to assess the outcome of continuous renal replacement therapy (CRRT) and acute peritoneal dialysis (PD) in dialysis-requiring renal failure in patients with hemodynamic instability.
Materials and Methods:
A retrospective analysis of all the patients who received CRRT and acute PD over a period of 1 year at our institute, a tertiary care center, was done for diagnosis, type of renal replacement therapy (RRT), and survival outcome. The indications for administering either of the therapy were usual indications of doing hemodialysis with the presence of hemodynamic instability (systolic blood pressure <90 mm of Hg even with inotropes).
Results:
Forty patients, 22 in CRRT and 18 in acute PD group were studied. All these patients required inotropes to maintain desired blood pressure. Twenty-five (62.5%) patients had acute kidney injury (AKI), and 15 (37.5%) had chronic kidney disease (CKD) superimposed over other primary diagnosis. A total of 8 (20%) patients (4 in CRRT, 4 in acute PD) survived at the time of discharge from hospital. The mean age of survivors was approximately a decade less than nonsurvivors (P = 0.15). Overall, there were no survivors in CKD group and all the patients who survived at the time of discharge from hospital had underlying AKI (P = 0.016).
Conclusion:
This study showing comparable survival outcome in acute PD and CRRT gives evidence that either of the modalities can be adopted in hemodynamically unstable patients requiring RRT depending on the resources available.
Keywords: Acute peritoneal dialysis, continuous renal replacement therapy, hemodynamic instability, renal replacement therapy
INTRODUCTION
Renal replacement therapy (RRT) is commonly requisitioned in critically ill patients either having chronic kidney disease (CKD) or acute kidney injury (AKI) superimposed over any other primary diagnosis. Most of these patients have multiple organ dysfunction, hemodynamic instability, and/or sepsis. RRT acts as a bridge to survival until the underlying comorbidity improves. The various modes of RRT that can be offered to these patients are intermittent hemodialysis (IHD), slow low-efficiency dialysis (SLED), acute peritoneal dialysis (PD), and continuous RRT (CRRT) each with its own pros and cons. Acute PD is simple, cheap, can be done bedside, lack the risks associated with vascular access and anticoagulation with disadvantages of inability to do in patients with recent abdominal surgery, slow solute clearance, and technical failure of the procedure. CRRT is slow continuous therapy with multiple options of treatment but has disadvantage of anticoagulation, vascular access, high cost, and being labor intensive. Both CRRT and PD are slow continuous therapies with advantage of convective clearance. CRRT, PD, and SLED are less likely to aggravate hemodynamic instability. IHD carries the risks of anticoagulation, complications of vascular access, and worsening of hemodynamic status. In critically ill patients with hemodynamic instability, one can choose from either CRRT or acute PD in patients who need RRT and have hemodynamic instability because of their inherent virtue of causing least hemodynamic compromise. All blood-based therapies are associated with risks of vascular access and anticoagulation. The optimal mode of RRT in critically sick and hemodynamic unstable patients is not known. Most of the studies comparing CRRT, IHD, and very few with acute PD have shown comparable outcomes in between the modalities.[1,2,3] There is a paucity of adequately powered randomized controlled trials (RCTs) in this population for optimal mode of RRT, due to the presence of multiple confounding factors, ethical issues, economic constraints, and suitability of a patient for a particular procedure. We did a retrospective analysis of survival outcome in patient who received CRRT or PD at our center in the last 1 year.
MATERIALS AND METHODS
A retrospective analysis of all the patients who received CRRT and acute PD at our institute, a tertiary care center, from October 1st, 2015 to September 30th, 2016 was done. All the patients who received CRRT or acute PD and aged above 12 years were included in the study. AKI was diagnosed on the basis of rise in serum creatinine by 0.3 mg/dl in 48 h period or urine output <0.5 ml/kg/h for 6 h, and CKD was diagnosed by estimated glomerular filtration rate <60 ml/min/1.73 m2 lasting more than 3 months or previously diagnosed patient of CKD. Sepsis was diagnosed on the basis of fulfillment of systemic inflammatory response syndrome criteria with confirmed or presumed infection. All the patients in CRRT group received continuous venovenous hemodiafiltration on Fresenius multifiltrate machine with pre filter administration of substitute and unfractionated heparin as anticoagulant. Dialysate and substitute used were prepackaged. The blood flow rate was kept at 150 ml/min, and effluent volume was targeted at about 25 ml/kg/h. All the PD were done bedside by person trained in nephrology. Stiff PD catheters were inserted under aseptic precautions percutaneously. A total of 40–60 exchanges were planned with prepackaged 1.5% dextrose PD fluid, with dwell time of ½ h over 48–72 h period, and subsequently, PD catheters were removed. The indications for administering either of the therapy were usual indications of doing hemodialysis, namely, hyperkalemia, volume overload, severe metabolic acidosis, and uremic encephalopathy refractory to medical therapy, with the presence of hemodynamic instability (systolic blood pressure <90 mm of Hg even with inotropes). The data were analyzed for diagnosis, type of RRT, and survival outcome in patients at the time of discharge from hospital. Descriptive statistics including means, standard deviation, and percentages were used to describe the demographic and clinical data. Comparison between groups was performed by Chi-square or Fisher's exact test for categorical data and Student's t-test for continuous data. P < 0.05 was considered statistically significant. All statistics were carried out using SPSS, version 15 (SPSS, Chicago, IL, USA).
RESULTS
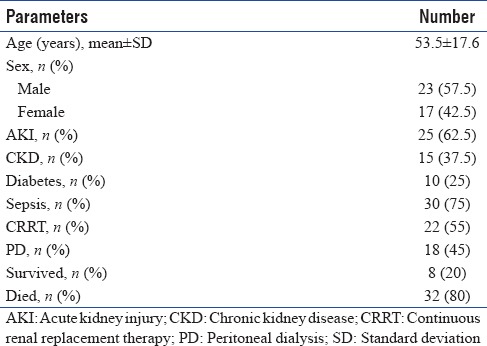
A total of 49 patients received either form of therapy (CRRT or acute PD) over the last 1 year from October 1st, 2015 to September 30th, 2016. Twenty-two patients received CRRT, and 27 patients received PD. Nine out of 27 patients in PD group received this therapy because of logistics, so they were excluded from the analysis. Hence, final analysis was done with 22 patients in CRRT and 18 patients in PD group. The mean age of study population was 53.5 ± 17.6 years with minimum of 14 and maximum of 86 years [Table 1]. All these patients required inotropes to maintain desired blood pressure. As a policy, RRT requiring patients who can maintain their systolic blood pressure ≥90 mm of Hg are taken up for IHD or SLED at our center. There were 23 (57.5%) male and 17 (42.5%) female patient. Nineteen (47.5%) patients were on ventilator and 4 (10%) were postsurgery. Thirty (75%) of patients had sepsis, and 6 (5.71%) had coronary artery disease with cardiogenic shock. The majority of the patients with sepsis (16–53.3%) had undifferentiated sepsis, followed by postsurgery – 3, 2 each had scrub typhus, pregnancy related, pancreatitis, urinary tract infection, and one each had pneumonia, burns, and tuberculosis.
Table 1.
Demographic and clinical characteristics of study patients (n=40)
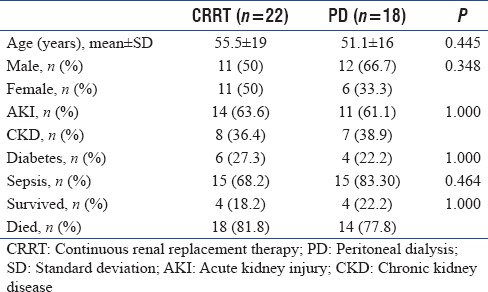
Out of 22 patients on CRRT, 14 (63.6%) had AKI, and 8 (36.4%) had CKD. Six (27.3%) out of 22 patients in CRRT group could not complete desired course of CRRT therapy, and all of them succumbed to their underlying illness. The average CRRT filter life was 19.3 h. A total of 18 patients received acute PD. Nine (50%) out of 18 patients in PD group could not complete desired course of acute PD therapy, and all of them succumbed to their underlying illness. There was no catheter-related complications or clinical evident peritonitis (cloudy effluent). Out of 18 patients in PD group, 11 (61.1%) had AKI, and 7 (38.9%) had CKD [Table 2].
Table 2.
Demographic and clinical characteristics of the treatment groups
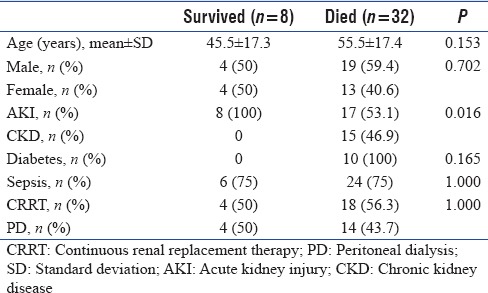
A total of 8 (20%) patients among 40 (combined CRRT and acute PD) survived at the time of discharge from hospital, four (18.2%) out of 22 patients in CRRT group, and 4 (22.2%) out of 18 in acute PD group survived at the time of discharge from hospital. The mean age of survivors was approximately a decade less than nonsurvivors (P = 0.15). Overall, there were no survivors in CKD group and all the patients who survived at the time of discharge from hospital had underlying AKI (P = 0.016) [Table 3].
Table 3.
Comparison of groups according to the outcome
DISCUSSION
There is ever increasing need of RRT in intensive care scenario where number of patients with multiple comorbidities, and hemodynamic instability is continuing to increase. Uchino et al. in a multinational, multicenter study found the prevalence of RRT in between 5% and 6% in Intensive Care Units (ICUs), and it was associated with high mortality rate.[4] The mode of RRT and overall outcome in critically ill patients differ according to regional and institutional practices. In a study by George et al., the combined mortality of entire group of CRRT, and PD was 78% in critically sick patients.[3] They also opined that the severity of underlying illness and need of ventilator support are more important determinant of outcome rather than type of RRT. Martin has also predicted mortality rate of 40%–80% in patients with septic shock applying the consensus conference definition.[5] The overall mortality in our study was also high of 80% mainly because of the presence of shock in all the patients, and 75% had sepsis as underlying comorbidity. The patients, who are critically sick but hemodynamically stable and they require RRT, are taken for either SLED or IHD at our center.
Acute PD has been used as mode of RRT, for about last seven decades and has saved number of lives. It may be the only possible therapy in neonates and infants where difficulty of appropriate vascular access and lack of miniaturization of HD instrumentation may prevent administration of HD albeit they have large peritoneal surface area making them suitable for PD. PD has also been found to be effective in hypercatabolic patients.[6,7] George et al. randomized 25 patients each to CRRT and PD group over period of 3 years and demonstrated comparable outcomes with respect to improvement in metabolic parameters.[3] Gabriel et al. also demonstrated comparable survival in PD and daily hemodialysis groups.[7] Uehlinger et al. compared outcomes among ICU patients on IHD and CRRT and found comparable outcomes with regard to survival and overall hemodynamic stability on either of therapy.[8] Extended daily dialysis of duration of more than 6 h but <24 h has shown comparable outcome versus CRRT in a meta-analysis of RCTs; however, former modality was associated with lower mortality risk in meta-analysis of observational studies.[9] CONVINT trial, a single-center trial of CRRT (continuous venovenous hemofiltration) versus IHD and Kitchlu et al. in a cohort study of CRRT versus SLED (8 h session with blood flow rate of 200 ml/min) have demonstrated no difference in outcomes mainly with respect of mortality in any of the therapies in critically ill patients.[10,11] It is difficult to draw any firm inference from the available evidence regarding choice of RRT in intensive care scenario except that the mode of RRT is not the sole determinant of outcome. The current study although retrospective but representative of practical intensive care scenario also shows comparable survival outcomes in hemodynamically unstable patients treated with CRRT or PD with the advantage of lower cost with latter form of therapy. In our study, the survival in AKI was better than CKD with either form of the therapy. Hence, underlying comorbidity is more important determinant of outcomes rather than mode of RRT.
CONCLUSION
The present study and most of the literature available do not provide unequivocal evidence for superiority of one form of RRT over other in intensive care settings. However, both CRRT and PD have advantages of convective clearance and better hemodynamic tolerability. The success of any form of RRT in intensive care settings depend on expertise, technical suitability of the patient for particular therapy, and appropriate management of the underlying comorbid condition. Beside this, underlying illness is more important marker of outcome rather than type of RRT. Thus, the choice of therapy in intensive care settings should be based on expertise, experience, technical feasibility of the procedure, and available resources.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The authors would like to thank Residents, technical and nursing staff Dialysis Unit, Department of Nephrology, Indira Gandhi Medical College, Shimla.
REFERENCES
- 1.Lameire N, Van Biesen W, Vanholder R. Dialysing the patient with acute renal failure in the ICU: The emperor's clothes? Nephrol Dial Transplant. 1999;14:2570–3. doi: 10.1093/ndt/14.11.2570. [DOI] [PubMed] [Google Scholar]
- 2.Liang KV, Sileanu FE, Clermont G, Murugan R, Pike F, Palevsky PM, et al. Modality of RRT and recovery of kidney function after AKI in patients surviving to hospital discharge. Clin J Am Soc Nephrol. 2016;11:30–8. doi: 10.2215/CJN.01290215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.George J, Varma S, Kumar S, Thomas J, Gopi S, Pisharody R. Comparing continuous venovenous hemodiafiltration and peritoneal dialysis in critically ill patients with acute kidney injury: A pilot study. Perit Dial Int. 2011;31:422–9. doi: 10.3747/pdi.2009.00231. [DOI] [PubMed] [Google Scholar]
- 4.Uchino S, Kellum JA, Bellomo R, Doig GS, Morimatsu H, Morgera S, et al. Acute renal failure in critically ill patients: A multinational, multicenter study. JAMA. 2005;294:813–8. doi: 10.1001/jama.294.7.813. [DOI] [PubMed] [Google Scholar]
- 5.Martin GS. Sepsis, severe sepsis and septic shock: Changes in incidence, pathogens and outcomes. Expert Rev Anti Infect Ther. 2012;10:701–6. doi: 10.1586/eri.12.50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chitalia VC, Almeida AF, Rai H, Bapat M, Chitalia KV, Acharya VN, et al. Is peritoneal dialysis adequate for hypercatabolic acute renal failure in developing countries? Kidney Int. 2002;61:747–57. doi: 10.1046/j.1523-1755.2002.00177.x. [DOI] [PubMed] [Google Scholar]
- 7.Gabriel DP, Caramori JT, Martin LC, Barretti P, Balbi AL. Continuous peritoneal dialysis compared with daily hemodialysis in patients with acute kidney injury. Perit Dial Int. 2009;29(Suppl 2):S62–71. [PubMed] [Google Scholar]
- 8.Uehlinger DE, Jakob SM, Ferrari P, Eichelberger M, Huynh-Do U, Marti HP, et al. Comparison of continuous and intermittent renal replacement therapy for acute renal failure. Nephrol Dial Transplant. 2005;20:1630–7. doi: 10.1093/ndt/gfh880. [DOI] [PubMed] [Google Scholar]
- 9.Zhang L, Yang J, Eastwood GM, Zhu G, Tanaka A, Bellomo R. Extended daily dialysis versus continuous renal replacement therapy for acute kidney injury: A meta-analysis. Am J Kidney Dis. 2015;66:322–30. doi: 10.1053/j.ajkd.2015.02.328. [DOI] [PubMed] [Google Scholar]
- 10.Schefold JC, von Haehling S, Pschowski R, Bender T, Berkmann C, Briegel S, et al. The effect of continuous versus intermittent renal replacement therapy on the outcome of critically ill patients with acute renal failure (CONVINT): A prospective randomized controlled trial. Crit Care. 2014;18:R11. doi: 10.1186/cc13188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kitchlu A, Adhikari N, Burns KE, Friedrich JO, Garg AX, Klein D, et al. Outcomes of sustained low efficiency dialysis versus continuous renal replacement therapy in critically ill adults with acute kidney injury: A cohort study. BMC Nephrol. 2015;16:127. doi: 10.1186/s12882-015-0123-4. [DOI] [PMC free article] [PubMed] [Google Scholar]


