Abstract
Introduction:
Atypia of undetermined significance (AUS) or follicular lesion of undetermined significance (FLUS) of Bethesda system for reporting thyroid cytopathology has emerged as most controversial category due to its heterogeneity and inconsistent usage. Initially associated risk of malignancy was estimated to be about 5–15%, but eventually different results have been obtained across institutions due to variable follow-ups and interpretation. The present study was conducted to evaluate the rate of malignancy along with appropriate management in this category.
Materials and Methods:
The study included AUS/FLUS cases diagnosed over period of 4 years on thyroid fine needle aspiration cytology (FNAC). Detailed clinical history and radiological examination were recorded along with follow-ups and management of all cases. Histopathology was available for cases which underwent surgery due to high clinical suspicion, worrisome radiological features or two consecutive AUS/FLUS reports.
Results:
The incidence of AUS/FLUS was 6.4% with repeat FNAC done in 39.6%, immediate surgery in 49.2% and follow-up without intervention in 11.1% cases. The overall malignancy rate was 28.5% with most common malignancy being follicular variant of papillary carcinoma (FVPC). Malignancy rate was more in cases (24.1%) which morphologically showed atypical nuclear features in comparison to architectural atypia.
Conclusion:
AUS/FLUS is associated with higher risk of malignancy than previously anticipated. Surgical intervention may have greater implication than repeat FNAC in appropriate management of this category. Substratification of this category according to nuclear features and architecture may be more useful in predicting malignancy risk and reducing the variability in the group.
Key words: Atypia of undetermined significance, Bethesda system of reporting thyroid cytology, follicular lesion of undetermined significance, malignancy rate
Introduction
Fine needle aspiration of cytology (FNAC) is considered to be an important diagnostic tool for workup of thyroid nodules. Its rational use to triage patients for surgery or conservative management has increased immensely. However, the variation in terminology of thyroid FNA, difference in interpretation of reports and management across the globe provided an impetus to the Bethesda System for Reporting Thyroid Cytopathology (BSRTC). This system was first published in 2008 in an attempt to standardize the reporting and management of FNAC thyroid and to facilitate an effective communication between cytopathologists, endocrinologists, and surgeons.[1,2] It is a six-tier system which provides the risk of malignancy and appropriate management for each category. Out of all the categories, category III or atypia of undetermined significance\follicular lesion of undetermined significance (AUS\FLUS) which is heterogeneous category is considered to be the most controversial category. Although Bethesda consensus publication estimates the risk of malignancy in this category to be 5–15%, but different studies have reported variable risk of malignancy ranging from 25% to 50% in different clinical settings.[3,4] In addition, although BSRTC recommends repeat FNA as usual management in this category, a debate is ongoing regarding its suitable management. Therefore, the present study was conducted to evaluate the rate of malignancy in AUS\FLUS category in light of clinical and radiological features. It was also intended to study the appropriate management of cases in this category.
Materials and Methods
This study included all the cases of AUS\FLUS category of BSRTC on thyroid FNAC which were diagnosed over period of 4 years from January 2012 to January 2016 in the institute. Detailed clinical history, biochemical, and radiological investigations were recorded for each case. FNAC was performed using 26–28-gauge needle with 2–4 aspirates depending on the size of the swelling. Rapid on site evaluation (ROSE) was performed to check the adequacy of smears, wherever possible. Conventional air dried and alcohol fixed smears were prepared and subjected to May Grunwald Giemsa, Hematoxylin-eosin, and Papanicolaou stain respectively. The smears were reported according to the criteria laid down by BCRTC.[1] The category III or AUS\FLUS diagnosis was rendered when there was predominance of micro follicles and\or oncocytes in paucicellular smear or in the presence of air drying or clotting artefact and thus not otherwise fulfilling the criteria of “follicular neoplasm\suspicious of follicular neoplasm” [Figure 1]. In addition, the category III was also diagnosed when there were same nuclei showing features suspicious of papillary carcinoma in otherwise hyperplastic or colloid nodule [Figure 2] or there were presence of atypical lymphoid cells. The risk factors for surgical intervention were worrisome radiological and clinical features including age, size, margins, and ultrasonography features of hypoechogenicity, hypervascularity, and calcification. The cases with two consecutive AUS/FLUS reports on FNA were also considered suitable for surgical intervention. Incidental carcinomas which were present away from the target nodule were excluded from the study. The histopathology was noted for cases which underwent surgery (either lobectomy or thyroidectomy). The cases which did not undergo surgery were followed up for at least 6 months.
Figure 1.
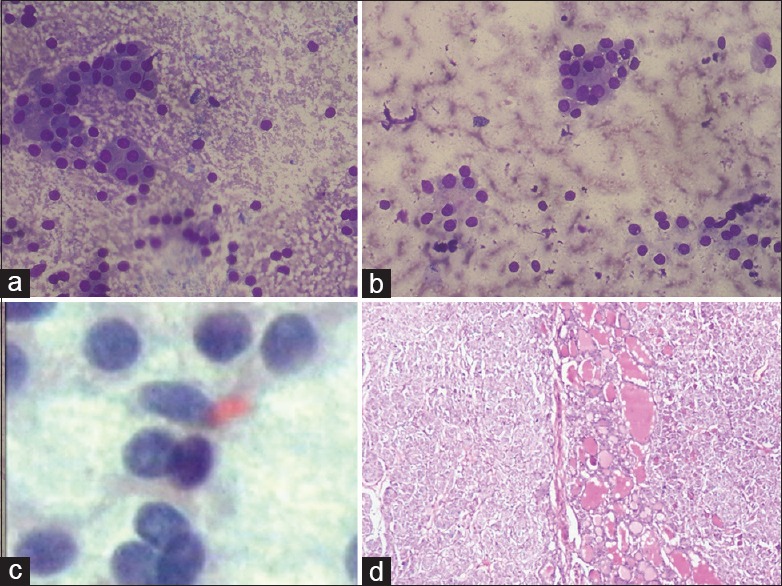
(a and b) FNAC thyroid shows mostly Hurthle cell change with few small follicles and abundant colloid in background (a: May–Grunwald–Giemsa; ×100, b: May-Grünwald-Giemsa; ×200); (c) Smears show few nuclei showing intra nuclear inclusions. Case was diagnosed as category AUS/FLUS of BSRTC (Pap stain x1000); (d) On histopathological examination, the case was diagnosed as follicular variant of papillary carcinoma (H and E stain x100)
Figure 2.
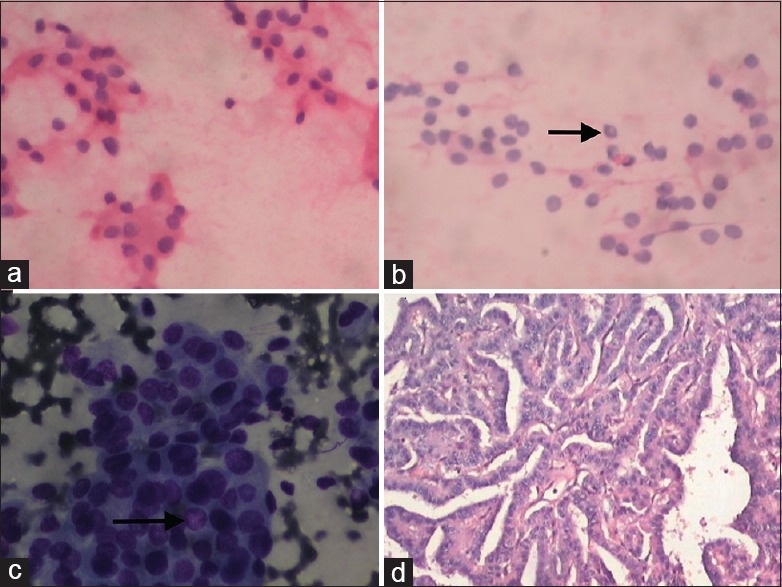
(a) FNAC thyroid showing follicular cells arranged in sheets with few showing Hurthle cell and degenerative change (H and E stain x200); (b and c) Smears show few nuclei showing intra nuclear inclusions (black arrow) but features not sufficient enough to be diagnosed as papillary carcinoma. Case was diagnosed as category AUS/FLUS of BSRTC (b: H and E stain ×200, c: May–Grunwald–Giemsa; ×400); (d) Histopathological examination of same case showed papillary carcinoma (H and E stain x200)
Results
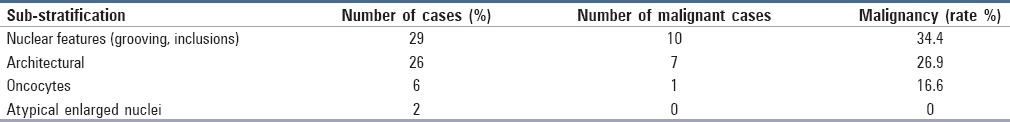
A total of 971 cases underwent thyroid FNA over period of 4 years with male female ratio of 0.23:1. Table 1 shows the distribution of various thyroid lesions according to BSRTC. It shows that AUS/FLUS or category III constituted 6.4% of total cases (63/971). The mean age of patients in this category was 44.7 years with age range of 18–90 years and showing female preponderance (female to male ratio of 4.2:1). The mean nodular size observed was 2.2 cm and 57.1% of total AUS/FLUS cases (36/63) showed worrisome radiological features including hypervascularity, microcalcifications, and complex hypoechoic nodules. Table 2 shows the management of the cases after diagnosis of AUS/FLUS in the study. It shows that maximum number of cases (49.2%) were subjected to immediate surgery in light of radiological and clinical features. Repeat FNAC which was done within period of 3 months observed 67.6% cases to be benign (17/25), malignant 20% (5/25), and three cases were again categorized as AUS/FLUS. These three cases were then subjected to surgery and turned out to be malignant and thus total malignancy rate after repeat FNAC was 32% (8/25). Out of the 31 cases which underwent immediate surgery 22 cases (72%) were benign and nine cases (27.9%) were malignant. Out of the total seven cases which were followed up without any immediate intervention, one case showed sudden increase in nodular size and was subjected to immediate surgery and histopathologically diagnosed as papillary carcinoma. Thus, out of total 63 cases of AUS/FLUS 18 cases turned out to be malignant with an overall malignancy rate of 28.5%. Table 3 shows that follicular variant of papillary carcinoma (FVPC) was the most common malignancy diagnosed on histopathology in AUS/FLUS category subjected to surgery. Table 4 shows that malignancy rate was highest in cases (24.1%) which morphologically showed nuclear features with grooving or inclusions, but not sufficient enough to be labelled as papillary carcinoma followed by cases showing architectural atypia.
Table 1.
Distribution of thyroid lesions according to BSRTC
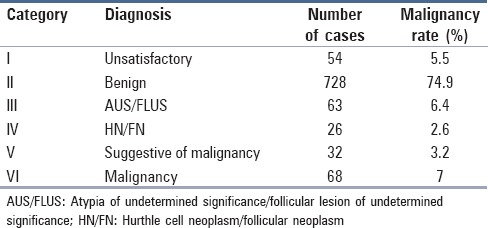
Table 2.
Management of the cases after diagnosis of AUS/FLUS
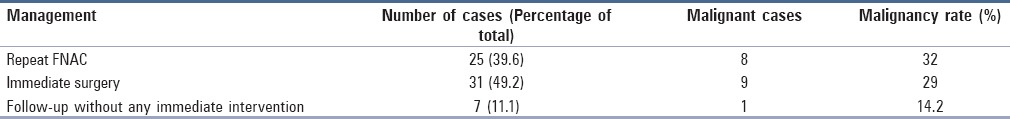
Table 3.
Type of malignancy on histopathology in AUS/FLUS category
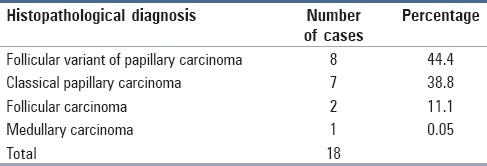
Table 4.
AUS/FLUS substratification and malignancy rate
Discussion
AUS/FLUS category of BSRTC is heterogeneous category which includes thyroid aspirates that are not sufficient enough for suggestive of malignancy or neoplasm, but have atypical nuclear and architectural features which limits their inclusion in benign category.[3,4] BSRTC defines this category as category of last resort and should not include more than 7% of total thyroid FNAs.[1] In the present study, this category III of AUS/FLUS included 6.4% of total cases and thus falling in the recommended range. However, different studies have reported variable rates of AUS/FLUS ranging from 0.8% to 29%.[5,6,7,8] It has been suggested that the AUS/FLUS to malignant ratio should be 1:3 and under diagnosis of malignancy and over diagnosis of AUS/FLUS leads to higher ratio of 3.[4] The present study observed the AUS/FLUS to malignant ratio of 1:3.3 and thus overrules the possibility of over diagnosis of AUS/FLUS or under diagnosis of malignancy in the study. It has also been suggested that the “benign category” may be extended to include those cases which “favor benign”, but need mandatory clinical follow-up. This may limit the over diagnosis of benign cases and thus limiting AUS/FLUS to only 2–8%.[9]
The BSRTC has estimated the risk of malignancy to range from 5% to15% in AUS/FLUS category and the usual recommended management is repeat FNA.[1] However, studies have observed higher malignancy rate in different clinical settings and recommend reconsideration of malignancy rate and management guidelines in this category.[10,11] The present study also observed higher malignancy rate (28.5%) than the estimated risk in this category. The various confounding factors which may be associated with increased malignancy rate are overuse of this category, inclusion of incidental carcinomas and heterogeneity of AUS/FLUS category.[4,10] Layfield et al. and Broome et al. observed the AUS/FLUS rate of 12.1% and 29% with malignant rate of 28% and 20% respectively in all resected cases thus supporting the view of high malignancy rate in studies which show increased AUS/FLUS rate than the recommended limit.[12,7] The inclusion of incidental carcinomas in the studies have also resulted in inflated rate of AUS/FLUS.[13] However, both these factors did not affect the malignancy rate in the present study as incidental carcinomas were excluded from the study and also the AUS/FLUS rate (6.4%) also lie in the recommended BSRTC rate. However, an important factor which may be associated with increased malignancy rate in the study is the referral bias as the study was done in tertiary care center where patients were referred with increased chances of malignancy.
The authors suggest that substratification of the category III into subgroups may be useful in reducing the heterogeneity of AUS/FLUS category and more appropriate prediction of malignancy. It was observed in the present study that cases which showed presence of nuclear features suggestive of papillary carcinoma showed the highest malignancy rate (24.1%) in comparison to smears showing architectural disturbances (19.2%) or oncocytic predominance (16.6%). In addition, the FVPC was the most common malignancy that was observed in AUS/FLUS category. The authors thus conclude that thyroid nodules in AUS/FLUS category with atypical nuclear features (cannot exclude papillary carcinoma) are at higher risk of malignancy in comparison of architectural atypia. Few recent studies have similarly concluded that nuclear atypia indicates higher risk of malignancy than the microfollicular architecture.[14,15] Studies have concluded that skillful examination of subtle features are needed on thyroid smears so that sensitivity of BSRTC is not reduced.[8] The present study also observed that 57.1% of total AUS/FLUS cases showed worrisome radiological features with mean nodular size of 2.2 cm thus suggesting that radiological and clinical assessment may play an important role in predicting increased malignancy risk. However, in contrast Park et al. have concluded that ultrasound features and nodular size does not differ in malignancy with single or repeat AUS/FLUS results.[16]
The present study also questions the utility of repeat FNA recommended by BSRTC as the observed malignancy rate after single FNAC in resected cases is comparable to malignancy rate after repeat FNAC [Table 2]. Thus waiting for repeat FNA for 3 months will unduly delay the surgery in thyroid nodules harboring the malignancy. Although no ancillary technique was performed in the study, but the authors suggest immunohistochemistry and molecular analysis may be helpful in defining the malignancy risk in AUS/FLUS and differentiating high risk and low risk cases. Furthermore, Hyeon et al. has concluded that BRAF molecular testing is useful in stratifying the malignant risk of AUS cases into high and low risk groups.[14] However, Ho et al. observed no difference in malignancy risk at similar substratification of AUS/FLUS category.[10]
The important limitations of the present study were that lesser number of cases were included with an extended follow-up and therefore cases which were considered benign may show different prognosis on prolonged follow-up. This is especially important as thyroid neoplasms show indolent nature. In addition, referral bias to tertiary care center may have also limited the observation of the study. The authors therefore suggest that further large studies may be done with extended follow-up with utilization of ancillary techniques so as to clearly assess the malignancy rate in AUS/FLUS category.
The study thus concludes that AUS/FLUS or category III of BSRTC is associated with higher risk of malignancy (28.5%) than previously anticipated by Bethesda consensus publication (5–15%). Surgical intervention may have greater implication than repeat FNAC in appropriate management of this category. In addition, substratification of this category according to nuclear features and architecture may be more useful in predicting malignancy risk and reducing the variability in the group. Further larger studies with ancillary techniques including immunohistochemistry and molecular analysis may be more useful in precisely defining the malignancy risk and appropriate management of this heterogeneous category.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Cibas ES, Ali SZ. NCI Thyroid FNA State of the Science Conference. The Bethesda system for reporting thyroid cytopathology. Am J Clin Pathol. 2009;132:658–65. doi: 10.1309/AJCPPHLWMI3JV4LA. [DOI] [PubMed] [Google Scholar]
- 2.Baloch ZW, LiVolsi VA, Asa SL, Rosai J, Merino MJ, Randolph G, et al. Diagnostic terminology and morphologic criteria for cytologic diagnosis of thyroid lesions: A synopsis of the National Cancer Institute Thyroid Fine Needle Aspiration State of the Science Conference. Diagn Cytopathol. 2008;36:425–37. doi: 10.1002/dc.20830. [DOI] [PubMed] [Google Scholar]
- 3.Bongiovanni M, Krane JF, Cibas ES, Faquin WC. The atypical thyroid fine needle aspiration: Past, present and future. Cancer Cytopathol. 2012;120:73–86. doi: 10.1002/cncy.20178. [DOI] [PubMed] [Google Scholar]
- 4.Kholova I, Ludvikova M. Thyroid atypia of undetermined significance or follicular lesion of undetermined significance: An indispensable Bethesda 2010 diagnostic category or waste garbage? Acta Cytol. 2014;58:319–29. doi: 10.1159/000366498. [DOI] [PubMed] [Google Scholar]
- 5.Bohacek L, Milas M, Nitchell J, Siperstein A, Berber E. Diagnostic accuracy of surgeon performed ultrasound guide fine needle aspiration of thyroid nodules. Ann Surg Oncol. 2012;19:45–51. doi: 10.1245/s10434-011-1807-z. [DOI] [PubMed] [Google Scholar]
- 6.Wu HH, Rose C, Elsheik TM. The Bethesda system for reporting thyroid cytopathology: An experience of 1382 cases in a community practice setting with the implication for risk of neoplasm and risk of malignancy. Diagn Cytopathol. 2012;40:399–403. doi: 10.1002/dc.21754. [DOI] [PubMed] [Google Scholar]
- 7.Broome JT, Solorzano CC. The impact of atypia/follicular lesion of undetermined significance on the rate of malignancy in thyroid fine needle aspiration: Evaluation of the Bethedsa system for reporting thyroid cytopathology. Surgery. 2011;150:1234–41. doi: 10.1016/j.surg.2011.09.006. [DOI] [PubMed] [Google Scholar]
- 8.Vanderlaan PA, Krane JF, Cibas ES. The frequency of “atypia of undetermined significance” interpretations for thyroid fine needle aspirations is negatively correlated with histologically proven malignant outcomes. Acta Cytol. 2011;55:512–7. doi: 10.1159/000333231. [DOI] [PubMed] [Google Scholar]
- 9.Renshaw AA, Krane JF. Can changing the terminology for benign aspirates reduce the atypia of undetermined significance/follicular lesion of undetermined significance rate in thyroid fine needle aspirates? Cancer Cytopathol. 2013;121:175–8. doi: 10.1002/cncy.21236. [DOI] [PubMed] [Google Scholar]
- 10.Ho AS, Sarti EE, Jain KS, Wang H, Nixon IJ, Shaha AR, et al. Malignancy rate in thyroid nodules classified as Bethesda category III (AUS/FLUS) Thyroid. 2014;24:832–9. doi: 10.1089/thy.2013.0317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Al-Abbadi MA, Shareef SQ, Ali JA, Yousef MM. Application of the Bethesda system for reporting cytopathology in the eastern province of Saudi Arabia: Phase I pilot retrospective analysis. Acta Cytol. 2013;57:481–8. doi: 10.1159/000351612. [DOI] [PubMed] [Google Scholar]
- 12.Layfield LJ, Morton MJ, Cramer HM, Hirschowitz S. Implications of the proposed thyroid fine needle aspiration category of “follicular lesion of undetermined significance”: A five year multi-institutional analysis. Diagn Cytopathol. 2009;37:710–4. doi: 10.1002/dc.21093. [DOI] [PubMed] [Google Scholar]
- 13.Jo VY, Stelow EB, Dustin SM, Hanley KZ. Malignancy risk for fine needle aspiration of thyroid lesions according to the Bethesda system for reporting thyroid cytopathology. Am J Clin Pathol. 2010;134:450–6. doi: 10.1309/AJCP5N4MTHPAFXFB. [DOI] [PubMed] [Google Scholar]
- 14.Hyeon J, Ahn S, Shin JH, Oh YL. The prediction of malignant risk in the category “atypia of undetermined significance/follicular lesion of undetermined significance” of the Bethesda system for reporting thyroid cytopathology using subcategorization and BRAF mutation results. Cancer Cytopathol. 2014;122:368–76. doi: 10.1002/cncy.21396. [DOI] [PubMed] [Google Scholar]
- 15.Shrestha RT, Hennessey JV. Cytologic subclassification of atypia of undetermined significance may predict thyroid nodules more likely to be malignant at surgery. Diagn Cytopathol. 2016;44:492–8. doi: 10.1002/dc.23472. [DOI] [PubMed] [Google Scholar]
- 16.Park VY, Kim EK, Kwak JY, Yoon JH, Moon HJ. Malignancy risk and characteristics of thyroid nodules with two consecutive results of atypia of undetermined significance or follicular lesion of undetermined significance on cytology. Eur Radiol. 2015;25:2601–7. doi: 10.1007/s00330-015-3668-5. [DOI] [PubMed] [Google Scholar]


