Abstract
Introduction
Medical cannabis is increasingly being used for a variety of health conditions as more states implement legislation permitting medical use of cannabis. Little is known about medical cannabis use patterns and motives among adults across the lifespan.
Methods
The present study examined data collected at a medical cannabis dispensary in San Francisco, California. Participants included 217 medical cannabis patients who were grouped into age-defined cohorts (younger: 18–30, middle-aged: 31–50, and older: 51–72). The age groups were compared on several measures of cannabis use, motives and medical conditions using one-way ANOVAs, chi-square tests and linear regression analyses.
Results
All three age groups had similar frequency of cannabis use over the past month; however, the quantity of cannabis used and rates of problematic cannabis use were higher among younger users relative to middle-aged and older adults. The association between age and problematic cannabis use was moderated by age of regular use initiation such that earlier age of regular cannabis use onset was associated with more problematic use in the younger users, but not among older users. Middle-aged adults were more likely to report using medical cannabis for insomnia, while older adults were more likely to use medical cannabis for chronic medical problems such as cancer, glaucoma and HIV/AIDS. Younger participants reported cannabis use when bored at a greater rate than middle-aged and older adults.
Conclusions
Findings suggest that there is an age-related risk for problematic cannabis use among medical cannabis users, such that younger users should be monitored for cannabis use patterns that may lead to deleterious consequences.
Keywords: age, cannabis, marijuana, motives, medical
1. Introduction
Twenty-eight states and the District of Columbia have implemented laws allowing the use of cannabis and its derivatives for a variety of medical conditions (National Conference of State Legislatures, 2017. With the advent of “legal” cannabis markets in more than half the United States, there is a risk of increased cannabis use by adolescents and young adults, who may access it through dispensaries and home cultivation allowances. Indeed, adolescents and adults in states with laws providing legal protection to medical cannabis dispensaries exhibit higher rates of cannabis use compared with states that do not allow medical use of cannabis, or do not allow for cannabis dispensaries (Hasin et al., 2015; Pacula et al., 2015). Furthermore, adolescents age 14–18 years in states with medical cannabis laws exhibit lower educational attainment than those in states without medical cannabis laws (Plunk et al., 2016). Greater perceived availability of cannabis and an increase in prevalence of cannabis use was observed among adults age 26 years and older in states with medical cannabis laws, but not among younger adults or adolescents (Martins et al., 2016), suggesting the impact of cannabis laws are variable. Higher rates of cannabis use among states with medical cannabis laws are also associated with a higher prevalence of cannabis use disorders (Cerda, Wall, Keyes, Galea, & Hasin, 2012), and an increase in the frequency of binge drinking among young adults age 21 or above (Wen, Hockenberry, & Cummings, 2015).
Although previous studies found relatively no differences between medical and non-medical cannabis users (Ogborne et al., 2000; Furler et al., 2004), emerging research indicates that medical cannabis users display higher medical and psychological problems, whereas non-medical cannabis users exhibit more problematic alcohol use (Compton et al., 2017; Roy-Byrne et al., 2015; Woodruff & Shillington 2016). These researchers conclude that medical cannabis users may be legitimately using cannabis to treat medical illness, pain and mental health concerns. To date, however, little research has been conducted to evaluate use characteristics, motives, and specific problems associated with medicinal cannabis use, particularly among different age cohorts.
Researchers have identified several motives for cannabis use among younger users, including altered perception, alleviation of boredom, perceived low health risk (compared to alcohol and other drugs), and sleep-aide, all of which were associated with higher frequency of cannabis use (Lee, Neighbors, Hendershot, & Grossbard, 2009). In terms of associated risk, young adults’ motives for using cannabis have been shown to have an impact on their frequency and quantity of use and the development of problematic patterns of use and misuse (Bonn-Miller & Zvolensky, 2009), which is of particular concern given that adolescence and early adulthood is a critical time for brain development (Gruber, Silveri, Dahlgren, & Yurgelun-Todd, 2011; Lopez-Larson et al., 2011). For example, adolescents who use cannabis to cope with negative affect are significantly more likely to exhibit a greater number of cannabis dependence symptoms (Fox, Towe, Stephens, Walker, & Roffman, 2011). Individuals who use cannabis to cope in this manner may be predisposed to experience more frequent and intense negative affect and may rely on cannabis as a means of regulating their mood (Mitchell, Zvolensky, Marshall, Bonn-Miller, & Vujanovic, 2007). It is unclear whether the association between cannabis use motives and use consequences (i.e., dependence symptoms), observed among young adult populations extends to older adults or individuals using cannabis for medical purposes.
Most cannabis users initiate use in late adolescence, though they typically demonstrate a pattern of maturation in which they dramatically reduce or cease use after age 29 (Chen & Kandel, 1995; Price, Risk, & Spitznagel, 2001). Accordingly, adults who continue cannabis use into middle-age represent an overlooked demographic subset that may have significant unmet needs for addiction treatment. Differences between individuals who experiment and become regular cannabis users from those who eventually moderate or stop their use may be associated with their underlying motivation for use. In a study by Banes and colleagues (2014), middle-aged (mean age 37.7, SD = 12.08) adults seeking treatment for cannabis use disorders had better clinical outcomes (i.e., decreased cannabis use frequency, dependence symptoms, and problems) if they reported less coping-oriented use of cannabis.
The baby boomer generation (currently age 50+) has historically demonstrated higher rates of substance use than previous generations before them, including cannabis use (SAMHSA, 2011). Given the higher rates of lifetime cannabis use among this cohort of older adults, coupled with increased prevalence of chronic medical conditions that arise in later life (Schneider, O’Donnell & Dean, 2009), examination of factors that may contribute to greater problematic cannabis use in this population is important. An observational study found that older adult patients with alcohol and substance use disorders (aged 55 years and older) exhibited similar substance use patterns and levels of functioning in terms of psychological distress, family conflicts, and legal problems compared to a demographically matched sample of young adult patients with substance use disorders (aged 22–54 years). Importantly though, at 12-month follow-up, older adult patients with substance use disorders demonstrated significantly better substance use and functioning outcomes compared with younger patients, despite having had greater medical problems (Brennan, Nichol & Moos, 2003). Although this study did not specifically examine cannabis, one reason that older adults may fare better following substance use treatment is a difference in motives for use. For example, older adults may be more likely to use substances, such as cannabis, to cope with medical problems.
Though recent research has been conducted to characterize medical cannabis patients (e.g., Ilgen et al., 2013; Reinarman et al., 2011), there is little data on how cannabis use patterns and motives for use differ across the adult lifespan in this population. Given the paucity of research on medical cannabis use among age cohorts that encompass the full developmental lifespan, the current study aimed to: (1) to characterize and compare cannabis use patterns (i.e., frequency, quantity) and problematic use of cannabis and alcohol by age defined groups; and (2) to identify differential motives and medical/psychiatric conditions for which cannabis is used, as a function of age group. Such information can better inform the practices of consumers, clinical providers, and policy-makers.
2. Methods
2.1 Participants
Study participants (N = 217) were adult patients, age 18 years and older, using medical cannabis for a physical or mental health condition obtained from a licensed medical cannabis dispensary in San Francisco, California in 2012–2013. At the time of data collection, the dispensary was one of 20 medical dispensaries in San Francisco, located in an urban, commercial neighborhood. The mean age of the sample was 41.2 years (SD = 14.9), and 24% were female. Self-reported ethnicities were 69% White/Caucasian, 7% Black/Non-Hispanic, 3% Black/Hispanic, 8% Hispanic, 3% Asian, and 10% Other. A comprehensive description of the sample, including other substance use, psychological symptoms and pain severity, was previously reported (see Bonn-Miller et al., 2014).
2.2 Procedures
Patients presenting to the medical cannabis dispensary were provided with the opportunity to participate in the study by research staff. After obtaining written informed consent to participate, interested individuals completed a battery of questionnaires. Following a debriefing by research staff, participants were entered into 1 of 4 drawings to receive a $100 prize. Study procedures were approved by the VA Palo Alto and Stanford University IRB and conducted in accordance with the ethical principles of the Declaration of Helsinki.
2.3. Measures
2.3.1. Cannabis use frequency and quantity
The Marijuana Smoking History Questionnaire (MSHQ; Bonn-Miller & Zvolensky, 2009) was used to determine past 30-day cannabis use. Primary outcome questions include “How often do you currently use cannabis?” and “On average, how much cannabis do you use per occasion?” Responses range from less than 1 gram to more than 12 grams. Although a majority of users reported smoking as their primary route of cannabis administration, the quantity and frequency of use also included vaporization, edibles and other methods of cannabis delivery. The questionnaire also assesses age of regular cannabis use onset and years of regular cannabis use. The MSHQ has performed well in previous research, with convergent validity for the items (Bonn-Miller & Zvolensky, 2009).
2.3.2. Cannabis and alcohol use problems
The Cannabis Use Disorders Identification Test- Revised (CUDIT-R) is an 8-item self-report measure of problematic or harmful cannabis use within the past 6 months (Adamson et al., 2010). A total score is calculated to produce a global measure of problematic cannabis use (possible range = 0–32)., In community samples, CUDIT-R totals of 9, 11 and 13 are suggested cut-offs for identifying mild, moderate and severe cases of DSM-5 Cannabis Use Disorder, respectively (Bruno, Marshall, & Adamson, 2013). Similarly, the Alcohol Use Disorders Identification Test (AUDIT; Saunders et al., 1993) is a 10-item self-report measure of hazardous and harmful alcohol consumption within the past year. AUDIT scores range from 0–40, with 8 as a cut-off for harmful consumption. Within the current sample, Cronbach’s alpha = 0.72 for the CUDIT-R and 0.83 for the AUDIT.
2.3.3. Cannabis use motives
The Comprehensive Cannabis Motives Questionnaire (CMMQ; Lee et al., 2009) was used to index motives for cannabis use. Participants rate how often they use cannabis for each of 36 reasons on a 5-point Likert-type scale (1= “Almost Never/Never” to 5= “Almost Always/Always”). These 36 items comprise 12 different domains (3 reasons per domain) of motives for use including: enjoyment, conformity, coping, experimentation, boredom (Cronbach’s alpha = .81), alcohol, celebration, altered perception, social anxiety, low risk, sleep and availability. Average internal consistency across the subscales was .75 (SD = .13), with a range of .53 to .90).
2.3.4. Medical Cannabis Use
The Medical Marijuana Patient Use Questionnaire (MMPUQ); Cohen et al., 2016) was used to determine the medical/psychiatric conditions for which participants used medical cannabis (i.e., “What condition(s) have led you to seek out medical cannabis (i.e., what is it prescribed for)?” followed by a number of listed conditions from which they could choose), and the length of time they used for medical purposes. This measure also assessed the preferred method of cannabis intake (i.e., oral, smoking, vaporization).
2.3.5. Psychological Symptoms
The Inventory of Depression and Anxiety Scale (IDAS; Watson et al., 2007) is a 64-item self-report questionnaire with 11 subscales: dysphoria, well-being, panic, suicidality, lassitude, insomnia, social anxiety, ill temper, traumatic intrusions, appetite loss and appetite gain (Cronbach’s alpha = .82). Respondents responded to items using a 5-point scale (1 = “not at all” to 5= “extremely”).
2.3.5. Pain
The pain Numeric Rating Scale (NRS; Jensen et al., 1999) was used to measure average pain severity during the prior week. Participants responded to a single question (i.e. “How would you rate your usual level of pain during the last week”) on an 11-point scale rated from 0 (no pain) to 10 (worst imaginable pain).
3. Data Analysis
Based on previous literature suggesting differential patterns of cannabis use among age groups (DiNitto & Choi, 2011; Delforterie et al., 2014) the sample was divided into three age cohorts. Consistent with prior work on age cohorts (e.g., Substance Abuse and Mental Health Services Administration, 2009) and the data distribution, sixty-eight participants fell between 18 and 30 years of age and were classified as “younger users.” Eighty-seven fell between 31 and 50 years of age and were classified as “middle-aged users.” Finally, sixty-two participants fell between 51 and 74 years of age and were classified as “older users.”
A series of one-way ANOVAs and chi-square tests of independence were conducted to determine whether younger, middle aged, and older users differed on relevant demographic characteristics (i.e., gender, ethnicity) and cannabis use patterns (i.e., quantity, frequency, age onset, years regular use). Next, one-way ANOVAs were used to determine the extent of problematic cannabis and alcohol use (i.e., CUDIT-R, AUDIT) between the age groups. Linear regression analysis was used to test age of regular cannabis use as a potential moderator of problematic cannabis use. Finally, one-way ANOVAs, chi-square tests of independence and Fisher’s exact tests were performed to assess the extent to which cannabis use motives (i.e., CMMQ subscales), psychological symptoms and the health condition for which cannabis was being used, respectively, differed among the age cohorts. A subsidiary linear regression analysis examined age cohort as a moderating variable of coping motives on problematic cannabis use.
4. Results
4.1. Characterizing Use as a Function of Age Group
Table 1 presents demographics and cannabis use characteristics as a function of age cohort. No differences were found among the age groups with respect to gender or race/ethnicity. A significant difference was found among the age cohorts for marital status and education, likely due to the association of age with these demographic variables. Specifically, younger adults were more likely to never have been married and less likely to have been divorced than middle-aged or older adults, X2(8, 212) = 36.60; p =.001). In addition, younger adults had less education than middle-aged and older adults, X2(2, 216) = 6.89; p =.032).
Table 1.
Participant Demographics, Cannabis Use and Psychological Symptoms by Age Group
| Young (18–30) | Middle-aged (31–50) | Older (51–74) | |
|---|---|---|---|
| Sex (Male) | 75% | 78% | 75% |
|
| |||
| Ethnicity (Caucasian) |
69% | 64% | 75% |
|
| |||
| Marital Status*** (Married or partnered) |
22% | 35% | 43% |
|
| |||
| Education* (College degree or higher) |
40% | 60% | 57% |
|
| |||
| Cannabis use frequency (times smoked in past month) |
62.4 (52.5) | 53.6 (75.7) | 52.1 (45.5) |
|
| |||
| Cannabis use quantity (number of grams smoked in past week)*** |
5.0 (1.9) (indicates 6 to 8 grams) |
4.2 (2.1) (indicates 3 to 5 grams) |
3.0 (2.2) (indicates 2 grams) |
|
| |||
| Age of first cannabis use* | 15.9 (3.6) | 16.7 (6.8) | 18.9 (5.7) |
|
| |||
| Age at onset of regular cannabis use*** | 19.0 (3.7) | 23.7 (9.4) | 30.5 (15.8) |
|
| |||
| Years of regular cannabis use*** | 6.3 (4.3) | 16.1 (10.1) | 26.8 (15.4) |
|
| |||
| Years of medical cannabis use*** | 6.4 (4.8) | 11.2 (9.1) | 15.3 (14.4) |
|
| |||
| CUDIT- R total score** | 13.8 (5.3) | 11.5 (5.0) | 9.9 (4.3) |
|
| |||
| CUDIT- R (% above cut-off)*** | 54% | 31% | 20% |
|
| |||
| AUDIT total score** | 8.52 | 9.19 | 5.36 |
|
| |||
| AUDIT (% above cut-off)* | 48% | 41% | 22% |
|
| |||
| IDAS-General Depression | 37.9 (10.6) | 40.8 (12.6) | 39.0 (13.1) |
|
| |||
| IDAS-Dysphoria | 18.2 (6.3) | 19.6 (7.3) | 18.1 (6.5) |
|
| |||
| IDAS-Lassitude | 12.3 (3.9) | 11.8 (4.2) | 11.5 (5.1) |
|
| |||
| IDAS-Insomnia | 11.1 (4.4) | 13.3 (6.6) | 11.5 (5.5) |
|
| |||
| IDAS-Suicidality** | 6.6 (1.3) | 7.3 (2.1) | 8.0 (2.6) |
|
| |||
| IDAS-Loss of Appetite | 5.5 (2.8) | 5.1 (2.7) | 5.5 (3.3) |
|
| |||
| IDAS- Appetite Gain** | 6.8 (2.8) | 5.3 (2.5) | 5.2 (2.0) |
|
| |||
| IDAS-Ill Temper | 7.9 (2.9) | 8.6 (4.0) | 8.4 (4.0) |
|
| |||
| IDAS-Well Being | 21.5 (6.4) | 22.8 (7.0) | 24.3 (7.6) |
|
| |||
| IDAS-Social Anxiety | 9.2 (3.8) | 8.7 (4.5) | 7.9 (3.9) |
|
| |||
| IDAS-Panic | 11.6 (3.2) | 11.5 (4.9) | 11.5 (4.0) |
|
| |||
| IDAS-Traumatic Intrusions | 6.2 (3.1) | 7.4 (4.2) | 6.6 (3.3) |
|
| |||
| NRS-Past Week Pain | 3.5 (2.7) | 3.8 (2.9) | 3.9 (2.9) |
p < .05,
p < .01,
p < .001
Results of a one-way ANOVA revealed that younger, middle-aged and older users had similar cannabis use frequency reported over the previous 30 days. However, the quantity of cannabis used over the past week differed (F = 12.76, p < 0.001, η2 = .12), with post-hoc analysis indicating older users reported using a lower quantity of cannabis than younger (p < .001) or middle-aged users (p = .003). Younger, middle-aged and older groups differed on the age at which they first used cannabis (F = 4.40, p = .013, η2 = .04), the age at which they started using cannabis regularly (F = 18.35, p < .001, η2 = .15), as well as how many years of regular use (F = 57.54, p < .001, η2 = .36). The age groups also differed on number of years of regular medical cannabis use (F = 11.30, p < .001, η2 = .11), and their preferred route of cannabis administration, X2(4, 189) = 11.57; p =.021, Cramer’s V = .18), with older adults (25%) preferring oral methods (e.g., edibles, tinctures) more than younger (7%) and middle-aged (9%) adults, while younger (30%) and middle-aged (31%) adults preferred vaping more than older adults (18%).
A one-way ANOVA showed that the problematic use of cannabis, as indexed by the CUDIT-R, significantly differed between the age cohorts and was highest among younger users, and decreased with older age (F = 8.92, p < .001, η2 = .09). Tukey HSD Post-hoc analysis indicated younger users had significantly higher CUDIT-R scores relative to middle-aged (p =.026) and older users (p <.001); there was no difference between middle-aged and older users. Chi-square analysis showed that a higher proportion of younger users were above the CUDIT-R cut-off for severe use (i.e., 13; see Bruno et al. 2013), compared to the other age groups, X2 (2, 191) = 15.91, p < .001, Cramer’s V = .29. Similarly, a one-way ANOVA showed that problematic alcohol use on the AUDIT differed by age group (F = 6.66, p <.01, η2 = .06). Tukey HSD post-hoc analysis indicated that older users (M = 5.3, SD = 5.5) had significantly fewer problems than younger (M = 8.5, SD = 4.9; p = .019) and middle-aged users (M = 9.2, SD = 7.7; p < .001) on the AUDIT; there was no difference between younger and middle-aged users.
Given the significant difference between groups on age of regular cannabis use onset, we tested this variable as a potential moderator of problematic cannabis use. A linear regression analysis revealed that the association between age groups and CUDIT-R Total Score was moderated by age of regular use onset (F = 7.62, p < 0.001; t = −3.15, p < .01; see Figure 1), such that earlier age of regular use onset was associated with higher CUDIT-R Total score in the younger users, and middle-aged users, but not in older users.
Figure 1.
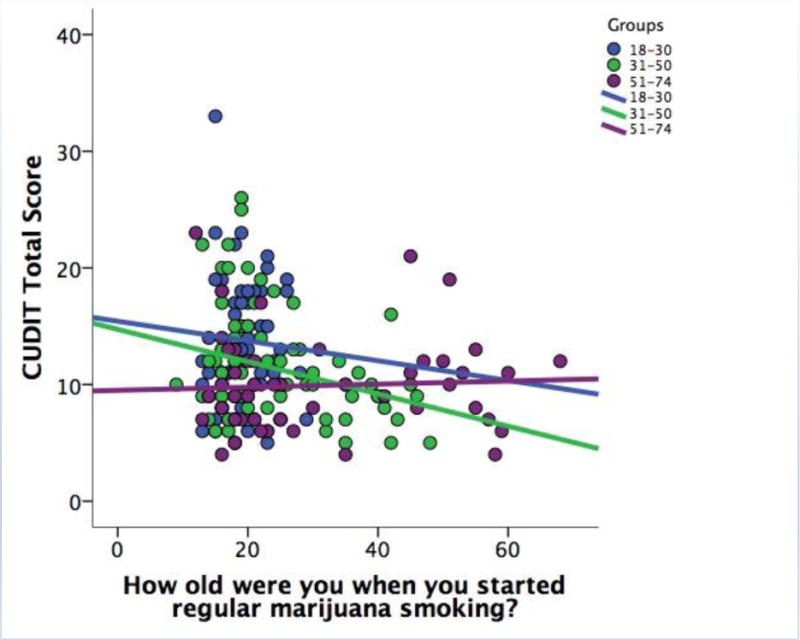
Age of Regular Cannabis Use Onset Moderates the Relationship Between Age Cohort and Problematic Cannabis Use on the CUDIT
4.2 Cannabis Motives, Psychological Symptoms and Conditions as a Function of Age Group
When examining motivations for use, younger users reported more frequent use of cannabis to relieve boredom (F = 3.06, p <.05, η2 = .03) compared with middle-aged and older users (M = 6.03, SD = 2.84 vs. M = 5.18, SD = 3.04 vs. M = 4.81, SD = 2.35, respectively). Use motives did not differ among the age cohorts for the other 11 domains which included: enjoyment, celebration, to alleviate anxiety, because it was available, to sleep, conformity, coping, experimentation, with alcohol, to alter perception, or due to perceived low risk.
Considering the literature on coping motives among young adults as related to problematic cannabis use, we investigated whether coping motives were differentially associated with CUDIT total score as a function of age group. A linear regression analysis showed coping and age as significant predictors of problematic cannabis use (F = 19.34, p < .001) but this relationship was not moderated by age cohort (t = −.34, p = .74).
Younger adults had higher scores than middle-aged adults and older adults on the Appetite/Weight Gain subscale (M= 6.8, SD =2.8 vs 5.3 SD = 2.5) vs. 5.2 (2.0), respectively on the IDAS, a measure of depression and anxiety symptoms. There was also a difference on the Suicidality subscale such that younger adults had the lowest scores (M = 6.6, SD =1.3), followed by middle-aged adults (M = 7.3, SD =2.1) and older adults (M = 8.0, SD = 2.6). There were no differences on other IDAS scales or the pain measure.
When examining the relation between age cohort and specific conditions for medicinal cannabis use, older users had higher proportions of use for chronic medical conditions. Specifically, older individuals were more likely to report medicinal cannabis use than middle-aged and younger individuals for cancer (13% vs. 2% vs. 0%; X2 (2, 212) = 14.27, p = .001, Cramer’s V = .26) and glaucoma (13% vs. 4% vs. 0%; X2 (2, 212) = 12.21, p = .002, Cramer’s V = .24). Older and middle-aged users were more likely to report using medical cannabis for HIV/AIDS than younger users (13% vs. 10% vs. 0%; X2 (2, 212) = 13.62; p = .013, Cramer’s V = .20). However, a higher proportion of middle-aged users (58%) reported using medicinal cannabis for insomnia compared with younger (47%) and older users (32%), X2 (2, 212) = 9.94, p = 0.007, Cramer’s V = .22) with post-hoc analysis showing a significant difference between the middle-aged and older users (p =.01); no post-hoc difference was found between the younger and middle-aged users with respect to insomnia. There were no differences among the three cohorts in the proportions of individuals reporting using medicinal cannabis for chronic pain, nausea, anxiety, PTSD, stress, depression, nightmares, appetite, epilepsy, seizures, muscle spasms, or multiple sclerosis.
5. Discussion
The current study investigated how age cohort may impact cannabis use patterns, motives and severity of use among medical cannabis dispensary patients in California. Participants from all three age groups (i.e., younger, 18–30 years; middle-age, 31–50 years; and older adults, 51–74 years) reported equivalent cannabis use frequency over the past 30 days, however, older users reported a lower quantity of cannabis use than younger and middle-aged users. Interestingly, older users preferred oral ingestion of cannabis compared to the other age groups, while younger and middle-aged users reported a preference for vaping cannabis more than older adults. Given that a majority of the sample reported smoking as their primary route of cannabis administration (61%), medical cannabis patients could be educated about how to reduce health risks associated with smoking (Gieringer, 2001) and the expanding options for cannabis delivery. For example, cannabis edibles, capsules, transdermal products, and tinctures are now sold at most dispensaries, and handheld/portable vaporization devices can be purchased online or in retail stores at low cost. Cannabis vaporization is generally regarded as safer than smoking as it does not involve pulmonary delivery of the tars and harmful byproducts of combustion that occurs with smoked cannabis (Bloor et al., 2008). FDA-approved synthetic cannabinoid medications are also available in oral formulations and have the added benefit of meeting established quality control regulations for pharmaceutials.
Participants across the age cohorts initiated regular cannabis use at significantly different ages. Indeed, on average, older users delayed initiation of cannabis use longer than middle-aged and younger users. This is likely due to less cannabis availability and social acceptance, and greater legal consequences when the older users were younger. For example, the Boggs Act of 1951 imposed mandatory minimum sentencing penalties for cannabis possession of two to ten years and up to $20,000 fines until its repeal in 1970. Although cannabis became popular among counterculture movements in the 1960s leading to more lenient attitudes, President Nixon’s initiative for the “War on Drugs” increased government efforts against the sale, distribution, and consumption of illicit drugs in the United States. In contrast, the widespread accessibility, increasing social acceptability, and legalization for medical use in California beginning in 1996 likely contributed to earlier adoption of non-medical use of cannabis among the younger age group (Wen et al., 2015).
As expected, the length of the participants’ sustained cannabis use also differed significantly across all three age groups. On average, younger users reported using cannabis regularly for six years, middle-aged users reported using cannabis regularly for sixteen years, and older users reported using cannabis regularly for twenty-six years. Interestingly, participants in the younger age group reported more problematic cannabis use as measured by the CUDIT-R, and were the only group to exhibit a mean score above the clinical cut-off for harmful use (Adamson et al., 2010). Thus, though older users appeared to have more experience with frequent and sustained cannabis use than middle aged and younger users, they reported fewer difficulties and negative consequences stemming from such use.
The relations between age cohort and CUDIT-R total score was moderated by age of regular use onset. Specifically, an earlier age of regular use onset was associated with a higher CUDIT-R total score in the younger and middle-aged users, but not in the older users. The age of regular use onset may therefore be a more potent risk factor for problematic cannabis use than user age alone. Interestingly, the years of regular use of cannabis and years of medical cannabis use were nearly identical for younger users but not for middle-aged and older users, suggesting medical cannabis as a point of entry for cannabis use of younger adults. Likewise, adults with cannabis use problems may decide to obtain medical cannabis because they qualify for medical reasons, and this behavior may differ by age cohort (i.e., older adults tend to have more medical problems).
With regard to motivations for cannabis use, younger users were more likely than middle-aged and older adults to use out of boredom (i.e., had nothing better to do, to relieve boredom, wanted something to do”). One possible explanation for this finding is that contemporary adolescents and young adults may have difficulty sitting with solitude and boredom, as conditioned by interactive technology (LaRose, Lin & Easton, 2003). A recent study examining the factor structure of the Marijuana Motives Measure (MMM; Simons et al. 1998) among young adults suggested that boredom and habit loaded onto a separate factor labeled as “routine” (Benschop et al., 2015). The boredom factor on the CMMQ is positively associated with cannabis use frequency (Lee et al., 2009), and boredom motives are associated with problems at a higher frequency of cannabis use among younger users (Hiles, Walsh, Crosby & Swogger, 2014). Although the study cannot determine causation, differences in motivations for cannabis use combined with the observed elevated CUDIT-R and AUDIT scores suggest that earlier use may preclude the development of intrinsic coping mechanisms. Alternatively, individuals who are motivated by boredom, or who are already exhibiting greater impulsivity and novelty seeking, may be at greater risk for initiating regular use at a younger age and subsequently becoming addicted to cannabis.
Although differences were found among the age groups for the psychological symptoms of appetite/weight gain and suicidality, we did not have specific hypotheses around these scales Thus, the findings should be interpreted with caution. The IDAS Appetite Gain scale may have limited utility in the current population as the symptoms are relatively non-specific and pervasive, and could be associated with side effects from cannabis use, such that younger users have higher appetite stimulation as a function of higher cannabis use. Regarding suicidality, it may be a spurious finding or have an inverse relationship with cannabis use severity, such that the symptom is being managed by cannabis use.
Increasing the availability and reinforcement from non-substance related pleasurable activities among youth has been associated with decreased drinking among college students (Murphy, Correia, Colby & Vuchinich et al., 2005) and could be a strategy for targeting boredom among adolescents and young adults who use cannabis. Previous reports recommend delayed onset of regular cannabis use and harm reduction strategies for young adults who regularly use cannabis (DeWit et al., 2000). By postponing initiation of cannabis use until it is medically indicated, individuals may be afforded the opportunity to learn healthier strategies and life skills for dealing with emotional uncertainty and social situations. In our sample of medical cannabis users, higher endorsement of coping motives for cannabis use was associated with problematic cannabis use across the lifespan.
Middle-aged users were more likely to use cannabis to help ease insomnia than younger or older users. This finding corresponds to the literature indicating that middle-aged adults have higher rates of insomnia than younger and older adults (Sepehrmanesh, Ahmadvand, & Ghoreishi, 2010). Since middle-age users suffer from sleep problems and are using medical cannabis to alleviate this condition, this group may benefit from first-line treatments for insomnia such as Cognitive-Behavioral Therapy for Insomnia (CBT-I; Edinger et al., 2001).
The older user cohort was more likely to report using cannabis for cancer, glaucoma, and HIV/AIDS, consistent with older adults having higher base rates of chronic medical conditions compared to middle-aged and younger adults (Ryan-Ibarra, Induni, & Ewing, 2015). Indeed, the age of onset of regular cannabis use for older adults in our sample was 31 years, suggesting many of these individuals are using cannabis primarily for medical reasons later in life. Given the increasing numbers of older cannabis users, future research should examine both the harmful and beneficial effects of medical cannabis among this population, particularly as a function of disease progression.
Limitations of the current study include that the sample was a self-selected group of cannabis dispensary patients from a single site in the United States and cross-sectional design. No information is available regarding dispensary patients from the same site who refused the study, so we cannot determine whether participation rates are independent from age. The differences seen among age groups could be explained by a birth year cohort effect, current age effect, natural attrition (e.g., death, incarceration) or “aging out” of problematic cannabis use after experiencing negative consequences (Chen & Kandel, 1995). Indeed, higher probability of use for medical conditions in older adults is also confounded by the fact that chronic medical conditions increase in prevalence with age (Schneider et al., 2009). Further research into the psychosocial effects of early onset cannabis use is necessary to elucidate whether cohort effects may be implicated in the relation between early initiation and problematic patterns of use. This research should also account for differential base rates of conditions by age, as this may explain why older and middle aged users are more likely to use for medical ailments rather than psychosocial purposes. Finally, additional research is needed to determine whether route of cannabis administration, in addition to age, is differentially associated with cannabis use consequences and other relevant outcomes.
6. Conclusion
The present study identifies similarities and differences in the characteristics of cannabis use among medical cannabis dispensary patients of varying age groups. This study contributes to our understanding of medical cannabis patients by highlighting more problematic cannabis and alcohol use, and boredom motives for cannabis use, among younger adults compared to middle-aged and older adults. The association between age and problematic cannabis use was moderated by age of regular use onset, a finding that corroborates extant literature recommending the postponement of cannabis initiation. Middle-aged adults reported using medical cannabis for insomnia, while older adults were more likely to use medical cannabis for chronic medical problems such as cancer, glaucoma and HIV/AIDS. Clinical implications for medical providers and cannabis dispensary staff include having an awareness of age-related risk for problematic cannabis use, and providing preventive screening and brief interventions, particularly for young people who may be using out of boredom or who lack healthy coping alternatives in their lives.
Acknowledgments
We would like to thank the Substance and Anxiety Intervention Laboratory at the VA Palo Alto, cannabis dispensary patients in San Francisco who participated in this research and Omid Khalili for assistance in the development of the research questions posed in this manuscript.
References
- Adamson SJ, Kay-Lambkin FJ, Baker AL, Lewin TJ, Thornton L, Kelly BJ, Sellman JD. An improved brief measure of cannabis misuse: The Cannabis Use Disorders Identification Test-Revised (CUDIT-R) Drug and Alcohol Dependence. 2010;110(1–2):137–43. doi: 10.1016/j.drugalcdep.2010.02.017. [DOI] [PubMed] [Google Scholar]
- Banes KE, Stephens RS, Blevins CE, Walker DD, Roffman RA. Changing motives for use: Outcomes from a cognitive-behavioral intervention for cannabis-dependent adults. Drug and Alcohol Dependence. 2014;139:41–46. doi: 10.1016/j.drugalcdep.2014.02.706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benschop A, Liebregts N, van der Pol P, Schaap R, Buisman R, van Laar M, van der Birnk W, de Graaf R, Korf DJ. Reliability and validity of the Marijuana Motives Measure among young adult frequent cannabis users and associations with cannabis dependence. Addictive Behaviors. 2015;40:91–95. doi: 10.1016/j.addbeh.2014.09.003. [DOI] [PubMed] [Google Scholar]
- Bloor RN, Wang TS, Spanel P, Smith D. Ammonia release from heated ‘street’ cannabis leaf and its potential toxic effects on cannabis users. Addiction. 2008;103(10):1671–7. doi: 10.1111/j.1360-0443.2008.02281.x. [DOI] [PubMed] [Google Scholar]
- Bonn-Miller MO, Zvolensky MJ. An evaluation of the nature of cannabis use and its motives among young adult active users. The American Journal On Addictions / American Academy of Psychiatrists in Alcoholism and Addictions. 2009;18(5):409–416. doi: 10.3109/10550490903077705. [DOI] [PubMed] [Google Scholar]
- Bonn-Miller MO, Boden MT, Bucossi MM, Babson KA. Self-reported cannabis use characteristics, patterns and helpfulness among medical cannabis users. The American Journal of Drug and Alcohol Abuse. 2014;40(1):23–30. doi: 10.3109/00952990.2013.821477. [DOI] [PubMed] [Google Scholar]
- Bowles DW. Persons registered for medical cannabis in the United States. Journal of Palliative Medicine. 2012;15(1):9–11. doi: 10.1089/jpm.2011.0356. [DOI] [PubMed] [Google Scholar]
- Brennan PL, Nichol AC, Moos RH. Older and younger patients with substance use disorders: Outpatient mental health service use and functioning over a 12-month interval. Psychology of Addictive Behaviors. 2003;17(1):42–48. doi: 10.1037/0893-164X.17.1.42. [DOI] [PubMed] [Google Scholar]
- Bruno R, Marshall S, Adamson S. Screening for DSM-5 cannabis dependence using the Cannabis Use Identification Test- Revised (CUDIT-R); Poster presented at the Australasian Professional Society on Alcohol and other Drugs; Brisbane, Australia. 2013. Nov, [Google Scholar]
- Cerda M, Wall M, Keyes KM, Galea S, Hasin D. Medical marijuana laws in 50 states: Investigating the relationship between state legalization of medical marijuana and marijuana use, abuse and dependence. Drug and Alcohol Dependence. 2012;120:22–27. doi: 10.1016/j.drugalcdep.2011.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen K, Kandel DB. The natural history of drug use from adolescence to the mid-thirties in a general population sample. American Journal of Public Health. 1995;85(1):41–47. doi: 10.2105/AJPH.85.1.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Compton WM, Han B, Hughes A, Jones CM, Blanco C. Use of Marijuana for Medical Purposes Among Adults in the United States. JAMA: Journal Of The American Medical Association. 2017;317(2):209–211. doi: 10.1001/jama.2016.18900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delforterie MJ, Creemers HE, Agrawal A, Lynskey MT, Jak S, Huizink AC. The influence of age and gender on the likelihood of endorsing cannabis abuse/dependence criteria. Addictive Behaviors. 2015;42:172–175. doi: 10.1016/j.addbeh.2014.11.029. [DOI] [PubMed] [Google Scholar]
- DeWit DJ, Hance J, Offord DR, Ogborne A. The influence of early and frequent use of marijuana on the risk of desistance and of progression to marijuana-related harm. Preventive Medicine: An International Journal Devoted to Practice and Theory. 2000;31(5):455–464. doi: 10.1006/pmed.2000.0738. [DOI] [PubMed] [Google Scholar]
- DiNitto DM, Choi NG. Cannabis use among older adults in the U.S.A.: User characteristics, patterns of use, and implications for intervention. International Psychogeriatrics. 2011;23(5):732–741. doi: 10.1017/S1041610210002176. [DOI] [PubMed] [Google Scholar]
- Choi NG, DiNitto DM, Marti CN. Treatment use, perceived need, and barriers to seeking treatment for substance abuse and mental health problems among older adults compared to younger adults. Drug and Alcohol Dependence. 2014;145:113–120. doi: 10.1016/j.drugalcdep.2014.10.004. [DOI] [PubMed] [Google Scholar]
- Cohen NL, Heinz AJ, Ilgen M, Bonn-Miller MO. Pain, cannabis species, and addiction. Journal of Studies on Alcohol and Drugs. 2016;77(3):515–520. doi: 10.15288/jsad.2016.77.515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edinger JD, Wohlgemuth WK, Radtke RA, Marsh GR, Quillian RE. Cognitive behavioral therapy for treatment of chronic primary insomnia: A randomized controlled trial. Journal of the American Medical Association. 2001;285(14):1856–1864. doi: 10.1001/jama.285.14.1856. [DOI] [PubMed] [Google Scholar]
- Fontes MA, Bolla KI, Cunha PJ, Almeida PP, Jungerman F, Laranjeira RR, Lacerda AT. Cannabis use before age 15 and subsequent executive functioning. The British Journal Of Psychiatry. 2011;198(6):442–447. doi: 10.1192/bjp.bp.110.077479. [DOI] [PubMed] [Google Scholar]
- Fox CL, Towe SL, Stephens RS, Walker DD, Roffman RA. Motives for cannabis use in high-risk adolescent users. Psychology Of Addictive Behaviors. 2011;25(3):492–500. doi: 10.1037/a0024331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Furler MD, Einarson TR, Millson M, Walmsley S, Bendayan R. Medicinal and Recreational Marijuana Use by Patients Infected with HIV. AIDS Patient Care And Stds. 2004;18(4):215–228. doi: 10.1089/108729104323038892. [DOI] [PubMed] [Google Scholar]
- Gieringer DH. Cannabis “vaporization”: A promising strategy for smoke harm reduction. Journal of Cannabis Therapeutics. 2001;1(3/4):153–170. [Google Scholar]
- Gruber SA, Silveri MM, Dahlgren MK, Yurgelun-Todd D. Why so impulsive? White matter alterations are associated with impulsivity in chronic cannabis smokers. Experimental And Clinical Psychopharmacology. 2011;19(3):231–242. doi: 10.1037/a0023034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasin DS, Wall M, Keyes KM, Cerdá M, Schulenberg J, O’Malley PM, Galea S, Pacula R, Feng T. Medical marijuana laws and adolescent marijuana use in the USA from 1991 to 2014: results from annual, repeated cross-sectional surveys. Lancet Psychiatry. 2015;2:601–608. doi: 10.1016/S2215-0366(15)00217-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hiles M, Walsh Z, Corsby K, Swogger MT. Cannabis use motives and frequency of use: Combined and distinct associations with cannabis use problems. Drug and Alcohol Dependence. 2014;140:E88–E89. [Google Scholar]
- Ilgen MA, Bohnert K, Kleinberg F, Jannausch M, Bohnert ASB, Walton M, Blow F. Characteristics of adults seeking medical marijuana certification. Drug and Alcohol Dependence. 2013;132(3):654–659. doi: 10.1016/j.drugalcdep.2013.04.019. [DOI] [PubMed] [Google Scholar]
- Jensen M, Turner J, Romano J, Fisher L. Comparative reliability and validity of chronic pain intensity measures. Pain. 1999;83:157–162. doi: 10.1016/s0304-3959(99)00101-3. [DOI] [PubMed] [Google Scholar]
- LaRose R, Lin CA, Easton MS. Unregulated internet usage: Addiction, habit or self-regulation? Media Psychology. 2003;5:225–253. [Google Scholar]
- Lee CM, Neighbors C, Hendershot CS, Grossbard JR. Development and preliminary validation of a comprehensive cannabis motives questionnaire. Journal Of Studies On Alcohol And Drugs. 2009;70(2):279–287. doi: 10.15288/jsad.2009.70.279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopez-Larson MP, Bogorodzki P, Rogowska J, McGlade E, King JB, Terry J, Yurgelun-Todd D. Altered prefrontal and insular cortical thickness in adolescent cannabis users. Behavioural Brain Research. 2011;220(1):164–172. doi: 10.1016/j.bbr.2011.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martins SS, Mauro CM, Santaella-Tenorio J, Kim JH, Cerda M, Keyes KM, Hasin DS, Galea S, Wall M. State-level medical marijuana laws, marijuana use and perceived availability of marijuana among the general U.S. population. Drug And Alcohol Dependence. 2016;169:26–32. doi: 10.1016/j.drugalcdep.2016.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meier MH, Caspi A, Ambler A, Harrington H, Houts R, Keefe RE, Moffitt TE. Persistent cannabis users show neuropsychological decline from childhood to midlife. Proceedings of The National Academy of Sciences of The United States of America. 2012;109(40):E2657–E2664. doi: 10.1073/pnas.1206820109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell H, Zvolensky MJ, Marshall EC, Bonn-Miller MO, Vujanovic AA. Incremental validity of coping-oriented cannabis use motives in the prediction of affect-based psychological vulnerability. Journal of Psychopathology And Behavioral Assessment. 2007;29(4):277–288. doi: 10.1007/s10862-007-9047-z. [DOI] [Google Scholar]
- Murphy JG, Correia CJ, Colby SM, Vuchinich RE. Using behavioral theories of choice to predict drinking outcomes following a brief intervention. Experimental and Clinical Psychopharmacology. 2005;13(2):93–101. doi: 10.1037/1064-1297.13.2.93. [DOI] [PubMed] [Google Scholar]
- National Conference of State Legislatures. State medical cannabis laws. 2017 Retrieved from: http://www.ncsl.org/research/health/state-medical-marijuana-laws.aspx.
- Ogborne AC, Smart RG, Weber T, Birchmore-Timney C. Who is using cannabis as a medicine and why: An exploratory study. Journal Of Psychoactive Drugs. 2000;32(4):435–443. doi: 10.1080/02791072.2000.10400245. [DOI] [PubMed] [Google Scholar]
- Pacula RL, Powell D, Heaton P, Sevigny EL. Assessing the effects of medical cannabis laws on cannabis use: The devil is in the details. Journal of Policy Analysis And Management. 2015;34(1):7–31. doi: 10.1002/pam.21804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plunk AD, Agrawal A, Harrell PT, Tate WF, Will KE, Mellor JM, Grucza RA. The impact of adolescent exposure to medical marijuana laws on high school completion, college enrollment and college degree completion. Drug & Alcohol Dependence. 2016;168:320–327. doi: 10.1016/j.drugalcdep.2016.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Price RK, Risk NK, Spitznagel EL. Remission from drug abuse over a 25-year period: Patterns of remission and treatment use. American Journal of Public Health. 2001;91(7):1107–1113. doi: 10.2105/AJPH.91.7.1107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reinarman C, Nunberg H, Lanthier F, Heddleston T. Who are medical marijuana patients? Population characteristics from nine California assessment clinics. Journal of Psychoactive Drugs. 2011;43(2):128–135. doi: 10.1080/02791072.2011.587700. [DOI] [PubMed] [Google Scholar]
- Roy-Byrne P, Maynard C, Bumgardner K, Krupski A, Dunn C, West II, Ries R. Are medical marijuana users different from recreational users? The view from primary care. The American Journal On Addictions / American Academy Of Psychiatrists In Alcoholism And Addictions. 2015;24(7):599–606. doi: 10.1111/ajad.12270. [DOI] [PubMed] [Google Scholar]
- Ryan-Ibarra S, Induni M, Ewing D. Prevalence of medical marijuana use in California, 2012. Drug and Alcohol Review. 2015;34(2):141–146. doi: 10.1111/dar.12207. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Results from the 2008 National Survey on Drug Use and Health: National Findings. Rockville, MD: U.S.Department of Health and Human Services; 2009. (Office of Applied Studies, NSDUH Series H-36, HHS Publication No. SMA 09-4434). [Google Scholar]
- SAMHSA Center for Behavioral Health Statistics and Quality. The NSDUH Report: Illicit Drug Use Among Older Adults. Rockville, MD: 2011. Retrieved from: http://oas.samhsa.gov/2k11/013/WEB_SR_013_HTML.pdf. [Google Scholar]
- Schneider KM, O’Donnell BE, Dean D. Prevalence of multiple chronic conditions in the United States’ Medicare population. Health Quality Life Outcomes. 2009;7:82. doi: 10.1186/1477-7525-7-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sepehrmanesh Z, Ahmadvand A, Ghoreishi F. PW01-111 - Prevalence of insomnia in general population. European Psychiatry. 2010;25:1524. doi: 10.1016/S0924-9338(10)71507-8. [DOI] [Google Scholar]
- Simons J, Correia CJ, Carey KB, Borsari BE. Validating a five-factor cannabis motives measure: Relations with use, problems, and alcohol motives. Journal of Counseling Psychology. 1998;45(3):265–273. doi: 10.1037/0022-0167.45.3.26. [DOI] [Google Scholar]
- Watson D, O’Hara M, Simms L, Kotoc R, Chmieleski M, McDade-Montez E, Gamez W, Stuart S. Development and validation of the Inventory of Depression and Anxiety Symptoms (IDAS) Psychological Assessment. 2017;19:253–268. doi: 10.1037/1040-3590.19.3.253. [DOI] [PubMed] [Google Scholar]
- Wen H, Hockenberry JM, Cummings JR. The effect of medical cannabis laws on adolescent and adult use of cannabis, alcohol, and other substances. Journal of Health Economics. 2015;42:64–80. doi: 10.1016/j.jhealeco.2015.03.007. [DOI] [PubMed] [Google Scholar]
- Woodruff SI, Shillington AM. Sociodemographic and drug use severity differences between medical marijuana users and non-medical users visiting the emergency department. The American Journal On Addictions / American Academy Of Psychiatrists In Alcoholism And Addictions. 2016;25(5):385–391. doi: 10.1111/ajad.12401. [DOI] [PubMed] [Google Scholar]


