Abstract
African American (AA) men have a higher prevalence of many chronic disease risk behaviors compared to Caucasian men, including physical inactivity. Innovative ways to reach AA men with interventions to increase physical activity (PA) and decrease other key risk factors are needed to reduce health disparities in this population. The barbershop is a natural but underutilized setting for reaching AA men. In the Fitness in the Shop (FITShop) study, shop owners, barbers, and customers were recruited from four local barbershops to complete structured interviews and customer focus groups. We assessed knowledge, perceived barriers, and interests/concerns about PA, as well as explored how to best intervene in the barbershop. Barbers and customers endorsed the idea of receiving health and PA information in the barbershop. These formative research results generated information and strategies for developing a multilevel barbershop-based health intervention to promote PA in the barbershop. This article describes the formative research results and how PRECEDE was used to develop a culturally and contextually appropriate, multilevel barbershop-based intervention designed to promote PA and to reduce chronic disease disparities among AA men.
Keywords: African American, men, physical activity, health promotion, barbershop
Introduction
African American (AA) men have a higher prevalence of many risk behaviors related to chronic disease than Caucasian men, including physical inactivity (Pleis & Lucas, 2009). AA men are more likely to be sedentary (46%) compared with Caucasian men (33%) (Pleis & Lucas, 2009). Very little has been published about how to promote physical activity (PA) among AA men (Hooker, Harmon, Burroughs, Rheaume, & Wilcox, 2011). Thus, formative research plays a crucial role in determining how to best intervene to promote PA among AA men. Innovative ways to reach AA men with interventions to increase PA and decrease other key chronic disease risk factors are needed to reduce health disparities in this population. The barbershop is a natural but underutilized setting for reaching AA men.
Fitness in the Shop (FITShop) is a two-phase intervention study designed to develop (Phase 1) and then test (Phase 2) the effects of a PA intervention for AA men recruited from barbershops. Phase 1 was a series of interrelated formative research activities leading to the development of a theory and evidence-guided, multilevel intervention called “YourMove,” designed to promote PA among AA men who visit barbershops. This article will describe results of the Phase 1 formative research study and how the PRECEDE planning model incorporated the formative research results into a planning process used to develop the multilevel YourMove PA intervention.
Overview of PRECEDE Planning Model
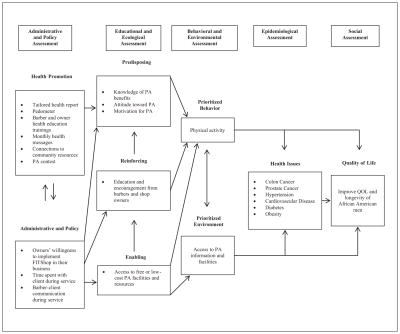
Developed as a planning model for designing and evaluating interventions, PRECEDE stands for Predisposing, Reinforcing, Enabling Constructs in Educational/Environmental Diagnosis, and Evaluation (Green & Kreuter, 1999, 2004). The PRECEDE planning process consists of a series of assessment steps (e.g., social assessment, epidemiological assessment, behavioral and environmental assessment, educational and ecological assessment, and administrative and policy assessment; Figure 1). The basic approach of the model involves first identifying the desired outcome, then determining the factors that would contribute to that outcome, and finally designing an intervention to reach the outcome.
Figure 1.
PRECEDE planning model for FITShop intervention.
Method
Formative Research
The University of North Carolina at Chapel Hill Institutional Review Board approved the formative research study and the consent procedures used. Consistent with a community-based participatory research (CBPR) approach, an essential aspect of our intervention development was incorporating the input of the intended beneficiaries (AA men who visit barbershops) into the intervention planning process. Sources and types of data collected during the formative study are summarized in Table 1.
Table 1.
Data Collection Methods for Planning the FITShop Intervention.
| Data source | Methods description |
|---|---|
| Literature review | Identified epidemiologic data to clarify health disparities, as well as quality of life issues that are of concern to AA men. Reviewed both qualitative data sources and intervention studies focused on AA men to help understand behavioral and environmental factors influencing health outcomes in AA men. |
| Environmental scans | Done at each participating barbershop to assess the availability of print materials, food and drink in the shop, as well as information about the physical layout and location of the shop. |
| Barbershop owner and barber interviews | Research team members conducted individual interviews with the four shop owners and seven barbers from each shop. Interviews assessed knowledge, perceived barriers, and interests/ concerns about PA in the barbershop. |
| Customer interviews | Research team members conducted individual interviews with 44 AA male barbershop customers. The interviews assessed PA levels, perceived PA barriers, and customer interests and concerns about promoting PA in the barbershop. |
| Customer focus groups | A barbershop advisory board member facilitated customer focus groups. Customers participated in one of two focus groups (physically active, n = 3, or physically inactive, n = 9), based on their self-reported answer to whether they obtain 150 minutes or more of PA per week. Focus groups assessed health concerns and priorities, and further assessed PA knowledge, perceived barriers, and interests/concerns about PA in the barbershop. |
Note. AA = African American; PA = physical activity.
A convenience sample of four barbershops was recruited for the formative research study. Shops were eligible for participation if they (1) were not part of a franchise, (2) signed up at least one licensed barber, (3) served at least 40 male customers per week, and (4) served primarily AA customers. An environmental scan was completed for each of the four participating shops. The environmental scan involved using a checklist to collect information about print materials, food and drinks found in the shop, as well as other information about the internal and external physical environment of the shop.
Structured interviews were administered to four barbershop owners and seven barbers from the participating shops by trained study personnel. All barbershop owners and barbers were male. Average length of shop ownership for owners was 6.9 years, and barbers had been licensed for an average of 20.2 years. Additionally, structured interviews were completed with 44 male customers from the participating shops. Average age of customers was 37.2 years (range = 22–72 years). Most customers were not married (72.6%), had at least some college experience (74.4%), and had health insurance (76.7%).
A total of 12 customers were recruited to participate in two focus groups from the participating barbershops. One group included men who reported at least 150 minutes of PA per week and were considered “active” (n = 3), while men in the other focus group did not meet PA recommendations and were considered the “inactive” group (n = 9). Mean age was 29.8 years (range = 18.9–47.5 years), most focus group participants were never married (83.3%), and had 1 or more years of college education (83.3%). Each focus group was audio recorded, was facilitated by a trained barbershop advisory board member, and lasted approximately 1 hour.
Interview and focus group participants received a $25 stipend for their time. Key domains within the structured interviews and focus groups included PA knowledge, perceived facilitators, and barriers and interest in promoting PA in the barbershop. Data collection materials are available on request from the authors. See appendix for focus group questions.
Data Analysis
Structured interview data were summarized using SPSS Version 20.0. Frequency distributions and percentages were used to summarize categorical data. Means were calculated for continuous data. Focus group data were transcribed by a trained research team member and then coded and analyzed by three trained research team members. Using a grounded theory approach, emergent themes were identified and coded on review of the transcripts. Analyses were stratified by focus group (physically active vs. inactive).
PRECEDE Phase 1: Social Assessment
The first step in the PRECEDE process is to conduct a social assessment, which identifies the quality of life priorities and concerns of the target population. First, we reviewed the literature to identify possible quality of life concerns among AA men. Results of a focus group study by Ravenell, Johnson, and Whitaker (2006) provided insight regarding AA men’s perceptions of health, where they defined health in terms of physical, mental, emotional, economic, and spiritual well-being. Being healthy also was associated with the ability to engage in social roles, such as being a provider for one’s family. Having a supportive social network and feeling valued by loved ones were cited as factors that positively influence AA men’s health. Similar findings were observed by Thompson, Talley, Caito, and Kreuter (2009), where AA focus group participants described health as being the absence of pain and symptoms and also described being healthy as the ability to fulfill daily roles. Additionally, the mind and spirit were identified as important aspects that AA men relate to physical health.
To augment the findings of our literature search, we used our focus groups to assess the health/quality of life concerns of AA men who visit barbershops. Specifically, we asked, “When you think about health, what comes to mind?” and “What does being healthy mean to you?” Both active and inactive participants associated health with longevity. They also associated health with mental and emotional stability. Additional factors associated with health included genetics, diet/nutrition, and physical and social environmental influences. Interestingly, physical activity was the most commonly cited behavior associated with health among inactive participants. Despite being sedentary, several inactive participants’ statements suggested that being physically fit is a primary indicator of health. For example, one participant said that “health boils down to your lifestyle, your strength, your endurance, and fitness …” Both active and inactive men expressed the belief that the importance of health and practicing preventive behaviors increased with age. Among inactive participants, this belief was associated with family health history. For example, two inactive men discussed how their fathers had heart attacks at an age similar to their current age and expressed a desire to prevent heart disease.
Overall, both active and inactive focus group participants emphasized the importance of being healthy, and PA was identified as a key component of health. Thus, we prioritized promoting PA to improve overall health and quality of life for an intervention to influence AA men who visit barbershops.
PRECEDE Phase 2: Epidemiological Assessment
The PRECEDE epidemiological assessment identifies health issues that have the greatest impact on quality of life and contribute to increased morbidity and mortality among AA men. To gather this information, we first reviewed the literature and national health statistics, searching for health issues linked to the priority health/quality of life concerns identified in the social assessment phase.
AA men experience many chronic disease disparities. Heart disease is the leading cause of death in the United States (Hoyert & Xu, 2012), and AA men suffer from higher rates of cardiovascular disease than Caucasian men, a 30% greater risk of hypertension diagnosis (U.S. Department of Health & Human Services, 2012), and are also 1.3 times more likely to die from hypertension than Caucasian men (Kochanek, Xu, Murphy, Minino, & Kung, 2011). In addition, AA men are 40% more likely to be diagnosed with diabetes (Centers for Disease Control and Prevention, 2013), and they have a diabetes-related death rate that is twice that of Caucasian men (Kochanek et al., 2011). AA men also have a 25% higher cancer incidence and 40% higher cancer mortality than Caucasian men (Ward et al., 2004).
Inactive focus group participants identified diabetes, hypertension, colon and prostate cancer, cardiovascular disease, and obesity as primary health concerns. Overall, current epidemiological data suggests that chronic disease prevention is a concern of and priority for AA men. Thus, we sought to develop a chronic disease prevention intervention for AA men, with a particular focus on physical inactivity, a behavioral risk associated with most leading chronic diseases and identified as a priority behavior among AA men.
PRECEDE Phase 3: Behavioral and Environmental Assessment
In the PRECEDE model, the behavioral and environmental assessment phase identifies factors which influence the prioritized health outcome (e.g., chronic disease). A literature review was conducted to gain an understanding of the behavioral and environmental factors that contribute to chronic disease development among AA men. Additionally, our study interviews and focus groups clarified key behavioral and/or environmental factors that may influence chronic disease prevention. We created a list of key factors and then rated each on importance and changeability. Importance was defined as the extent to which the determinant influences the onset of chronic disease. Changeability was defined as the likelihood that the determinant can be changed by an intervention. Table 2 presents the prioritized behavioral and environmental determinants for the study, as well as an assessment of their importance and changeability.
Table 2.
Importance and Changeability of Diagnosed Behavioral and Environmental Determinants of Chronic Disease.
| Determinant | Importance | Changeability | Interest of Target Population |
|---|---|---|---|
| Behavioral | |||
| Tobacco use | High | Low | Low |
| Fruit and vegetable intake | High | Moderate | High |
| Physical activity | High | High | High |
| Environmental | |||
| Lack of access to physical activity resources | High | Moderate | High |
| Lack of access to healthy food | High | Moderate | Moderate |
Note. Boldfaced entries indicate prioritized determinants.
Behavioral Determinants
Multiple modifiable behaviors, including smoking tobacco, low fruit and vegetable (FV) consumption, and physical inactivity were identified as determinants of a wide range of chronic diseases among AA men. Tobacco use, the leading preventable cause of death, has been associated with morbidity and mortality from multiple chronic diseases. Thus, tobacco use was categorized as being of high importance. However, it was categorized as having low changeability, given its addictive nature. Tobacco use was not mentioned as a health concern among our focus group participants. A majority of customers who completed our structured interviews (77%) were nonsmokers, and most (66.7%) were not interested in learning about smoking cessation. Therefore, we rated tobacco use as being of low interest among the priority population.
FV consumption is especially low among AA men (Stables et al., 2002), and they are less likely to meet nationally recommended daily servings than non-His-panic Whites (Casagrande, Wang, Anderson, & Gary, 2007). Only 2.3% of customers interviewed in our study reported eating five servings of FV a day. Similarly, all barbers interviewed reported that they do not eat five servings of FV a day, despite most (85.7%) reporting that information and advice on eating habits is “very important” or “extremely important.” Healthy eating was a common focus group topic, especially among active men. Given the strong evidence for low FV consumption among AA men, the low rates of reported FV consumption by our participants, and the perceived importance of health eating by our participants, FV intake was categorized as being of high importance for AA men. Results of previous studies demonstrate that AA men respond favorably to interventions designed to increase FV consumption. Wolf, Lepore, Vandergrift, Basch, and Yaroch (2009) conducted a FV education intervention, where 230 AA men received a mailed FV brochure and telephone-based support from a health educator. Participants in the study had a significant increase in FV consumption from baseline to the 8-month follow-up: t(239) = −5.83; p < .001. The results of previous FV intervention research with AA men informed our decision to rate FV consumption as having moderate changeability for our study population.
Current PA recommendations indicate that adults should engage in at least 150 minutes of moderate intensity activity per week (U.S. Department of Health & Human Services, 2008). AA men are more likely to be inactive (46%) compared with Caucasian men (33%; Pleis & Lucas, 2009). In North Carolina, only 38% of AA men get the recommended amount of PA as compared with 47% of Caucasian men (Centers for Disease Control and Prevention, 2007). In a secondary analysis of 1988 to 1994 National Health and Nutrition Examination Survey (NHANES) data, Thorpe et al. (2013) found that being physically inactive was associated with an increased risk (odds ratio = 1.53, 95% confidence interval = [1.08, 2.17]) of mortality in AA men aged 45 to 64 years. Additionally, a significant, inverse relationship between PA and colon cancer has been demonstrated (Friedenreich & Orenstein, 2002; Wolin, Yan, Colditz, & Lee, 2009), while the evidence that PA decreases risk has been classified as “probable” for prostate cancer and “possible” for lung cancers (Friedenreich & Orenstein, 2002).
Recent PA behavioral intervention studies have yielded favorable outcomes for AA men. In a pilot study by Hooker, Harmon, et al. (2011), middle-aged AA men (N = 25) attended 90-minute PA programs twice a week for 8 weeks, where they learned about overcoming barriers, gaining social support, setting goals, and tracking progress. Significant positive improvements (p < .05), from baseline to follow-up, were found for weekly average of moderate to vigorous PA (MVPA; +7.3 hours per week), weekly average of overall PA (+9.4 hours per week), goal setting (+48%), perceived self-efficacy for PA (+12%), as well as perceived social support from family (+28%) and friends (+53%). Similar results were found in a recent pilot study by Griffith, Allen, Johnson-Lawrence, and Langford (2014), where groups of 5 to 10 middle-aged and older AA men met once a week with a personal trainer for 10 weeks to improve flexibility, strength, balance, and conditioning. The trainer also assisted participants with problem solving, by addressing barriers to PA and providing information about community resources for PA. Significant improvements (p < .05) from baseline to follow-up were found for perceived self-efficacy to sustain PA, endurance, overall perceived health status, and self-reported stress level. Additionally, there was a 28% improvement among participants for meeting the recommendation of 150 minutes of MVPA per week (40% baseline vs. 68% at follow-up). Most customers interviewed in our study (72.2%) reported being moderately to extremely interested in learning about getting more exercise. Similarly, most barbers (85%) agreed that it was “very important” to “extremely important” to provide information and advice on exercise habits. Participants in both active and inactive focus groups also discussed PA as being beneficial. Because our participants expressed a strong interest in PA and because it was determined to have high importance and changeability among AA men, PA was the prioritized behavioral determinant of the proposed intervention.
Environmental Determinants
Environmental determinants of chronic disease involve a combination of factors, including access to health services, as well as the factors in the social and physical environment. Access to commercial fitness facilities, parks, and walkable areas has been identified as an environmental determinant of PA. Moreover, racial disparities exist in access to resources that promote PA (Abercrombie et al., 2008). A study by Powell, Slater, Chaloupka, and Harper (2006) reported that commercial PA facilities are less likely to be located in low-income, AA neighborhoods. These findings are mirrored in a study by Moore, Diez Roux, Evenson, McGinn, and Brines (2008), where minority neighborhoods were less likely to have recreational facilities than White neighborhoods. Limited access to PA facilities was a common barrier cited among our study participants, and it was determined to be of high interest among the target population. Strong evidence for access as a barrier to PA informed our high importance and changeability ratings.
Differential access to healthy foods also contributes to chronic disease health disparities (Franco, Diez Roux, Glass, Caballero, & Brancati, 2008). In a study by Powell, Chaloupka, and Bao (2007), AA neighborhoods were found to have a higher prevalence of fast food restaurants than White neighborhoods, a potential contributor to racial disparities in obesity. Thus, lack of access to healthy food was ranked as having high importance for AA men. Access to healthy food was ranked as having moderate changeability, after considering the cost and availability of healthy food options. Access to healthy food was determined to be of moderate interest among the target population.
In the PRECEDE social assessment phase, we prioritized PA because it was linked to the quality of life and health outcomes of greatest interest to AA men and because PA has a direct link to multiple chronic diseases. In the behavioral/environmental assessment phase, we learned that AA men who frequent barbershops identified PA as the health behavior that they most wanted to focus on in the barbershop, and that access to PA programs and services is an important and changeable environmental determinant. Thus, we prioritized PA and access to PA programs and services in Phase 3, consistent with the expressed interests of our priority population.
PRECEDE Phase 4: Educational and Ecological Assessment
In the educational and ecological assessment phase of PRECEDE, planners identify factors essential to the initiation and sustainability of the Phase 3 priority (Green & Kreuter, 2004). Three types of factors are hypothesized to influence any behavior: predisposing, enabling, and reinforcing. Predisposing factors, such as knowledge, attitudes, and beliefs, are the factors that motivate individuals to act. Enabling factors include resources, assistance, services, skills, and policies which support individuals who act on their predispositions to perform behaviors. Reinforcing factors operate after a behavior, such as PA, has been initiated, and they encourage continuation of the behavior by providing rewards and incentives, either tangible or in the form of social support, praise, and reassurance. Our research team sought to identify predisposing, enabling, and reinforcing factors influencing the prioritized behavior (e.g., PA) and the prioritized environmental determinant (access to PA) among AA men, in an effort to gain insight about existing knowledge, resources, and supports that can be used or enhanced through the FITShop intervention (see Table 3).
Table 3.
Importance and Changeability of Predisposing, Reinforcing, and Enabling Factors for Physical Activity.
| Determinant | Type of determinant | Importance | Changeability | Interest of target population |
|---|---|---|---|---|
| Motivation | Predisposing | High | High | High |
| Attitude toward physical activity | Predisposing | High | High | High |
| Self-efficacy | Predisposing | High | High | Moderate |
| Knowledge | Predisposing | High | High | High |
| Access to physical activity facilities | Enabling | High | Moderate | High |
| Social support | Reinforcing | High | High | High |
Note. Boldfaced entries indicate prioritized determinants
Predisposing Factors
Motivation, attitudes and beliefs, perceived self-efficacy, and knowledge have been identified as predisposing factors for PA among AA men. In a qualitative study by Bopp et al. (2007), older and younger AA men described lack of motivation as a barrier to being physically active. In particular, the men discussed having a lack of will-power and desire to exercise. Similarly, participants in our study also identified lack of motivation as a primary reason that keeps them from being physically active. This was a prevalent theme among “active” men. One participant who discussed his motivation for PA said, “I was working out a little bit, then it just stopped … now it’s just like ‘Get back on track.’ I think a lot of it is motivation.” Because motivation has been identified as a barrier to PA in multiple studies, as well as among our study participants, we categorized motivation as having high importance, high changeability, and high interest to target population.
Study results show that positive attitudes and beliefs regarding PA act as facilitators to PA among AA men. In a study by Affuso, Cox, Durant, and Allison (2011) with a sample of 510 AA men, perceived importance and necessity of exercise for health were found to be associated with PA. In a telephone survey study conducted with 165 AA men, Bopp et al. (2006) found that “enjoyment” was associated with meeting recommendations for MVPA. Closely related, AA male focus group participants in a study by Hooker, Harmon, et al. (2011) suggested that PA promotion programs for AA men should be fun, incorporate elements of camaraderie and fellowship, and feature a competition as part of the program. Participants in our study also emphasized the importance of ensuring that a barbershop-based health promotion intervention for men is fun. Men suggested that perceived enjoyment of the PA program would influence participation. Attitude toward PA was categorized as being a high priority for AA men and was rated as being highly changeable.
Perceived self-efficacy for engaging in PA has been associated with strength training and meeting MVPA recommendations among AA men (Bopp et al., 2006). Recent studies by Hooker, Harmon, et al. (2011) and Griffith et al. (2014) demonstrate the potential for group-based PA interventions to increase perceived self-efficacy for PA among middle-aged and older AA men, where both studies yielded significant positive improvements (p < .05) in perceived self-efficacy, from baseline to follow-up. Given the results of previous studies, we rated self-efficacy as being of high importance and changeability for AA men. PA self-efficacy was not a prevalent theme of the discussions among our participants, and it was therefore determined to be of moderate interest among the target population.
Knowledge has also been observed to influence PA among AA men. In a qualitative study by Bopp et al. (2007), both older and younger men (>55 and <55 years, respectively) described lack of knowledge as a barrier to PA, where participants indicated that individuals have a lack of understanding about how to exercise. Several participants in our study also discussed a lack of knowledge about how to exercise, suggesting that PA knowledge is of high interest among AA men. We rated PA knowledge as being a high priority for AA men and also rated it high for changeability, as barbershops are natural settings for information exchange.
Enabling Factors
Lack of access to resources has been identified as a barrier to PA among AA men, including access to and affordability of PA facilities. In a qualitative study by Hooker, Wilcox, Rheaume, Burroughs, and Friedman (2011), AA men discussed having limited access to PA facilities and offered recommendations for locations for incorporating and accessing PA resources, including churches and local parks. Similar results were found in a focus group study by Bopp et al. (2007), where young AA men (age <55 years) described limited access to outdoor PA resources, such as walking trails and sidewalks, as a barrier to PA. Participants in our study also described lack of access as a barrier to PA. In particular, cost was seen as a barrier to accessing PA facilities for both active and inactive men. One “active” focus group participant discussed how cost limits the type of PA that AA men engage in, saying, “With the exception of basketball or walking or jogging, many of the other activities require some type of fee either to get into the building or membership or a program or registration of some sort … it’s not free.” Inactive men discussed the lack of availability of PA facilities. One man shared with the group, saying, “[I] can’t go there if there’s no place to go. Where I live, there’s no place to go” A recent intervention study by Gustat, Rice, Parker, Becker, and Farley (2012) observed an increase in PA among low-income AA adults, following changes to the physical environment, where a 6-block walking path was built into the intervention neighborhood. Compared with two matched neighborhoods, the proportion of active residents in the intervention neighborhood increased significantly, and these residents were also observed to engage in more MVPA than those in the comparison neighborhoods. Given the strong evidence supporting the importance of PA access for AA men and recognition of that importance by members of our focus groups, we rated access as high for importance and interest. We rated the changeability of access as moderate because we felt that though affordable PA options may be limited, we could increase men’s awareness of existing free and low-cost PA resources by disseminating information about those resources within barbershops.
Reinforcing Factors
Social support from family, friends, and peers has been identified as a key facilitator of PA initiation and maintenance among AA men. In a qualitative study by Bopp et al. (2007), AA men reported that having a social support system facilitated their participation in regular PA. Participation in group-based PA programs has been associated with an increase in perceived social support among AA men (Griffith et al., 2014; Hooker, Harmon, et al., 2011), where the groups create a sense of camaraderie among members. Thus, social support was rated as being of high importance and changeability among AA men through PA interventions. Also, because camaraderie was emphasized as an important aspect of a PA intervention by shop owners, barbers, and customers, social support was determined to be of high interest among the target population.
To summarize the PRECEDE educational and ecological assessment phase, we prioritized knowledge, attitudes toward PA, and motivation as key predisposing factors for PA among men for the FITShop intervention. It is essential to educate AA men about the health benefits of exercise and about how to exercise in a safe and effective manner. It is also important to motivate AA men to initiate and sustain PA by promoting enjoyable options. We identified access to PA resources and facilities as a key enabling factor for increasing PA among AA men, given the strong qualitative evidence that cost and availability are barriers to PA. Finally, encouragement from barbershop owners and barbers was prioritized as a reinforcing factor for the FITShop intervention, as multiple studies report positive benefits of social support for PA among AA men.
PRECEDE Phase 5: Administrative and Policy Assessment
A final step in planning an intervention to promote PA among AA men who visit the barbershop involved identifying and understanding administrative factors and organizational policies that could potentially influence the implementation of the intervention. We assessed owners’ willingness to promote PA in their barbershop, and most (75%) indicated that they were “very interested” in distributing pamphlets or written materials promoting PA to their customers. Most owners (75%) were also very interested in displaying posters in their shop.
We also asked barbershop owners about their days and hours of operation. Thursday, Friday, and Saturday were identified as the busiest work days in most barbershops. Additionally, we assessed the number of barbers working in each shop, to consider who might be available to deliver or promote the PA intervention. Shops assessed in our formative study had an average of 4.5 licensed barbers who had worked an average of 5 years at the shop. This information was useful for determining the best implementation strategy for our barbershop-based intervention.
Results of the PRECEDE Intervention Planning Process
The PRECEDE planning model and collaborations with barbershop owners, barbers, and customers assisted our research team with developing a multilevel intervention focused on increasing PA among AA men who visit the barbershop. PA was prioritized as the key behavioral determinant, and access to free/low-cost PA facilities/services as the key environmental determinant. Next, we identified key predisposing, enabling, and reinforcing factors to address in order to increase PA and create an environment which supports a physically active lifestyle among AA men who visit the barbershop. These factors included the following: knowledge, motivation, attitude toward PA, access to free and low-cost PA resources, as well as support and encouragement for PA in the barbershop. Finally, using PRECEDE allowed us to examine administrative and organizational factors that could facilitate or hinder successful implementation of an intervention to promote PA in the barbershop, including buy-in from barbers for study participation and the most appropriate days and hours to promote PA at the barbershops.
The FITShop “YourMove” Intervention Overview
Working with members of the NC BEAUTY and Barbershop Advisory Board, data from previous work in beauty salons and barbershops, as well as primary data from formative research conducted with owners, barbers, and customers, we used the PRECEDE planning model to guide our development of a multilevel intervention to promote PA in the barbershop. The efficacy of this intervention was tested in Phase 2 of the FITShop study. Phase 2 was a 6-month, two-armed randomized controlled intervention study, consisting of YourMove (PA intervention barbershops) and YourMoney (Financial empowerment control barbershops). A detailed description of the study is presented in Hall, Linnan, Jolly, Dixon, and Scarlett (2014).
The YourMove multilevel PA intervention that emerged was organized around a social ecological approach at the intrapersonal, interpersonal, organizational, and community levels to promote PA among AA men in the barbershop (Table 4). The intervention included the following: (a) Personal feedback on self-reported PA, recommendations for PA, and pedometers for self-monitoring (intrapersonal); (b) barber workshops and barbershop cues to action to promote PA discussion between customers and barbers (interpersonal); (c) PA contests in the barbershops including culturally targeted educational materials (organizational); and (d) referrals to free or low-cost local health and PA resources (community). The intervention was delivered by the research team with critical support from shop owners and barbers.
Table 4.
FITShop Multilevel YourMove Intervention.
| Social ecological framework | Behavioral change theory/constructs | Intervention strategies |
|---|---|---|
| Intrapersonal level | Social cognitive theory
|
|
| Interpersonal level | Social support
|
|
| Organizational level | Social cognitive theory
|
|
| Community level | Social cognitive theory
|
|
Personal Feedback/Recommendations and Pedometers
Following customer enrollment and the completion of a baseline survey called the Carolina Health Assessment and Resource Tool (CHART), a tailored feedback report was mailed to each participant based on his responses to health behavior questions which explains how his current PA levels compare with recommended national guidelines. Previous research suggests that tailored health information has positive effects on health (Kreuter, Oswald, Bull, & Clark, 2000; Noar, Benac, & Harris, 2007) and PA outcomes (Marcus et al., 1998). In YourMove, tailored feedback provided encouragement and specific, personalized information to reduce barriers to PA by increasing motivation, self-efficacy, and knowledge. Each participant received a pedometer to monitor steps and to work toward a goal of achieving 10,000 steps per day of PA (or at least increasing PA incrementally). The combination of immediate feedback from a pedometer and personalized incremental goals for increasing daily steps has proven to be an effective approach for promoting PA (Merom et al., 2007).
Barber Workshops
To help build organizational retention and business sustainability, we offered four 2-hour workshops to all owners and barbers, regardless of their study arm. Each workshop consisted of a business development presentation, followed by discussion sessions on the FITShop study. The first workshop, “Small Business Resources” (n = 18), included an orientation to the overall FITShop study, so all attendees benefitted from that information. After the main business development presentation during second, third, and fourth workshops (Business Expansion/Social Media [n = 5], Taxes and Workers’ Compensation [n = 12], and Business Plan Basics [n = 8], respectively), we held breakout sessions by study arm to cover topics relevant to the YourMove or YourMoney shops. YourMove breakout sessions were designed to help barbers provide support/encouragement for PA to customers in their shops. During the sessions, staff discussed the importance of encouraging customers to report their weekly PA minutes. The breakout sessions were also an opportunity to identify any potential challenges and/or issues that barbers faced in their own PA efforts and when encouraging customers to participate in the YourMove intervention. YourMoney breakout sessions covered similar content, with a focus on financial empowerment. The research team assisted barbers with any perceived program implementation challenges.
Contest
During focus groups and structured interviews, both customers and barbers indicated that a PA contest would be well received by shop customers. A monthly PA contest within and between participating shops was offered in the YourMove arm of the study. Specifically, customers/barbers from the YourMove barbershops competed against one another in a monthly contest with award categories for the following: percentage of participants who logged weekly minutes of PA each month, percentage of participants who completed the contest each month, total number of minutes of PA reported each month, and percent increase in PA minutes over the course of the 6-month contest. Each participant was asked to document daily minutes of PA in a written log. Participants also received email, text, and/or phone call reminders to report total PA minutes each week during the 6-month intervention period. Each month, PA summary reports were posted in YourMove barbershops. The reports ranked YourMove barbershops based on each shop’s total reported PA for the month and identified the customer who reported the most PA that month, thus promoting a friendly competition. Individual and shop contest winners received a $50 cash prize each month.
Educational Messages
Print materials were placed in YourMove shops and contained educational messages known as “keys to success” on the following topics: (a) “get moving”—tips for initiating PA, (b) “holiday moving”—tips for exercising during the holidays, (c) “New Year moving”—tips for adopting and committing to new PA habits, (d) “strong moving”—tips for strength training, (e) “safe moving”—tips for exercising safely, and (f) “keep moving”—tips for sustaining PA. Each month, participating barbers received a mirror cling that included key messages to cue discussions between customers and barbers.
Community Connections
Customer focus groups, barber/owner structured interviews, and Barbershop Advisory Board meetings provided the research team with information about free or low-cost PA resources in the local community surrounding each shop. These resources included information on local parks, gyms, sports teams, and events. This information was shared with customers on the backside of the “keys to success” print materials which were distributed in all YourMove shops each month.
Strengths and Limitations
A major strength of the current study was the use of multiple data sources to plan the multilevel YourMove intervention. Another strength was collecting primary data through structured interviews and focus groups, which was consistent with CBPR principles and allowed for a more thorough understanding of the health-related needs and preferences of AA men. In order to meet the health-related needs of this hard to reach population, it is imperative to understand what men want, and how they want it delivered (Caperchione et al., 2012; Vandelanotte et al., 2013). An additional strength was our use of the PRECEDE planning model, which yields interventions which operate at multiple levels of influence. Despite these strengths, our study had several limitations, including the use of self-reported PA data, which has been found to be a source of participant bias (Prince et al., 2008; Shephard, 2003). In addition, our primary data were collected from small samples, and thus caution should be exercised in generalizing these results to other types of barbershops and/or in other regions of the country.
Conclusion
Given the lack of intervention studies to promote PA among AA men, it is imperative that formative research is conducted prior to developing new interventions like the one planned for the FITShop study. Our study used the PRECEDE planning process to develop a health promotion intervention for AA men. Specifically, the study generated information and strategies for a culturally and contextually relevant barbershop-based PA promotion for AA men. The YourMove intervention has implications for reducing chronic disease health disparities among AA men, by increasing PA, a preventive behavior. By improving AA men’s health, the YourMove intervention also has significant potential to improve their quality of life. The YourMove intervention was tested in a group randomized controlled, two-arm initial efficacy trial. Analyses are currently being conducted to determine the effectiveness of YourMove in promoting PA among participating AA men.
Acknowledgments
We would like to thank barbershop owners and customers who participated in this phase of the research, as well as members of the NC BEAUTY and Barbershop Advisory Board who have guided all aspects of this work.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was funded by the National Cancer Institute (Grant No. 1-U54-CA 156735-01).
Appendix
FITShop Formative Study Focus Group Questions
Health
-
1)
When you think about health, what comes to your mind?
-
2)
What does “being healthy” mean to you?
-
3)
What are the top two to three health problems that you worry about?
Barriers
-
4)
What makes it difficult for people, and specifically let’s focus on Black men if we could, to be physically active?
-
5)
Of all the reasons or obstacles to being physically active we have mentioned, which create the most trouble for you?
Intervention Planning
-
6)
What do you think of the idea of getting health and physical activity information in the barbershop? Do you like this idea or not? Tell us what you think …
-
7)
If you had to come up with some ideas about what we could do to promote physical activity in the barbershop—What ideas do you have? There are no right or wrong answers, and we want you to think as creatively as you can to help us figure out what would work in the barbershop to get Black men to be more physically active …
-
8)
In your barbershop, what would you suggest we do to let men know about this study and to get them to sign up?
Footnotes
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Abercrombie LC, Sallis JF, Conway TL, Frank LD, Saelens BE, Chapman JE. Income and racial disparities in access to public parks and private recreation facilities. American Journal of Preventive Medicine. 2008;34:9–15. doi: 10.1016/j.amepre.2007.09.030. [DOI] [PubMed] [Google Scholar]
- Affuso O, Cox TL, Durant NH, Allison DB. Attitudes and beliefs associated with leisure-time physical activity among African American adults. Ethnicity & Disease. 2011;21:63–67. [PMC free article] [PubMed] [Google Scholar]
- Bopp M, Lattimore D, Wilcox S, Laken M, McClorin L, Swinton R, … Bryant D. Understanding physical activity participation in members of an African American church: A qualitative study. Health Education Research. 2007;22:815–826. doi: 10.1093/her/cyl149. [DOI] [PubMed] [Google Scholar]
- Bopp M, Wilcox S, Laken M, Butler K, Carter RE, McClorin L, Yancey A. Factors associated with physical activity among African-American men and women. American Journal of Preventive Medicine. 2006;30:340–346. doi: 10.1016/j.amepre.2005.11.007. [DOI] [PubMed] [Google Scholar]
- Caperchione CM, Vandelanotte C, Kolt GS, Duncan M, Ellison M, George E, Mummery WK. What a man wants: Understanding the challenges and motivations to physical activity participation and healthy eating in middle-aged Australian men. American Journal of Men’s Health. 2012;6:453–461. doi: 10.1177/1557988312444718. [DOI] [PubMed] [Google Scholar]
- Casagrande SS, Wang Y, Anderson C, Gary TL. Have Americans increased their fruit and vegetable intake? The trends between 1988 and 2002. American Journal of Preventive Medicine. 2007;32:257–263. doi: 10.1016/j.amepre.2006.12.002. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Behavioral Risk Factor Surveillance System (BRFSS) survey data. 2007 Retrieved from http://www.cdc.gov/brfss/annual_data/annual_2007.htm.
- Centers for Disease Control and Prevention. Diagnosed diabetes by race/ethnicity, sex, and age. National Diabetes Surveillance System; 2013. Retrieved from http://www.cdc.gov/diabetes/statistics/prev/national/menuage.htm. [Google Scholar]
- Franco M, Diez Roux AV, Glass TA, Caballero B, Brancati FL. Neighborhood characteristics and availability of healthy foods in Baltimore. American Journal of Preventive Medicine. 2008;35:561–567. doi: 10.1016/j.amepre.2008.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedenreich CM, Orenstein MR. Physical activity and cancer prevention: Etiologic evidence and biological mechanisms. Journal of Nutrition. 2002;132(11 Suppl):3456s–3464s. doi: 10.1093/jn/132.11.3456S. [DOI] [PubMed] [Google Scholar]
- Green LW, Kreuter MW. Health program planning: An educational and ecological approach. 3. New York, NY: McGraw-Hill; 1999. [Google Scholar]
- Green LW, Kreuter MW. Health program planning: An educational and ecological approach. 4. New York, NY: McGraw-Hill; 2004. [Google Scholar]
- Griffith DM, Allen JO, Johnson-Lawrence V, Langford A. Men on the move: A pilot program to increase physical activity among African American men. Health Education & Behavior. 2014;41:164–172. doi: 10.1177/1090198113496788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gustat J, Rice J, Parker KM, Becker AB, Farley TA. Effect of changes to the neighborhood built environment on physical activity in a low-income African American neighborhood. Preventing Chronic Disease. 2012;9:E57. [PMC free article] [PubMed] [Google Scholar]
- Hall M, Linnan L, Jolly D, Dixon C, Scarlett R. Reaching African American men in all the right places: FITShop barbershop recruitment results. 2014 Manuscript submitted for publication. [Google Scholar]
- Hooker SP, Harmon B, Burroughs EL, Rheaume CE, Wilcox S. Exploring the feasibility of a physical activity intervention for midlife African American men. Health Education Research. 2011;26:732–738. doi: 10.1093/her/cyr034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hooker SP, Wilcox S, Rheaume CE, Burroughs EL, Friedman DB. Factors related to physical activity and recommended intervention strategies as told by midlife and older African American men. Ethnicity & Disease. 2011;21:261–267. [PubMed] [Google Scholar]
- Hoyert DL, Xu J. Deaths: Preliminary data for 2011. National Vital Statistics Reports. 2012;61(6):65. [PubMed] [Google Scholar]
- Kochanek KD, Xu J, Murphy SL, Minino AM, Kung HC. Deaths: Final data for 2009. National Vital Statistics Reports. 2011;60(3):117. [PubMed] [Google Scholar]
- Kreuter MW, Oswald DL, Bull FC, Clark EM. Are tailored health education materials always more effective than non-tailored materials? Health Education Research. 2000;15:305–315. doi: 10.1093/her/15.3.305. [DOI] [PubMed] [Google Scholar]
- Marcus BH, Emmons KM, Simkin-Silverman LR, Linnan LA, Taylor ER, Bock BC, … Abrams DB. Evaluation of motivationally tailored vs. standard self-help physical activity interventions at the workplace. American Journal of Health Promotion. 1998;12:246–253. doi: 10.4278/0890-1171-12.4.246. [DOI] [PubMed] [Google Scholar]
- Merom D, Rissel C, Phongsavan P, Smith BJ, Van Kemenade C, Brown WJ, Bauman AE. Promoting walking with pedometers in the community: The step-by-step trial. American Journal of Preventive Medicine. 2007;32:290–297. doi: 10.1016/j.amepre.2006.12.007. [DOI] [PubMed] [Google Scholar]
- Moore LV, Diez Roux AV, Evenson KR, McGinn AP, Brines SJ. Availability of recreational resources in minority and low socioeconomic status areas. American Journal of Preventive Medicine. 2008;34:16–22. doi: 10.1016/j.amepre.2007.09.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noar SM, Benac CN, Harris MS. Does tailoring matter? Meta-analytic review of tailored print health behavior change interventions. Psychological Bulletin. 2007;133:673–693. doi: 10.1037/0033-2909.133.4.673. [DOI] [PubMed] [Google Scholar]
- Pleis JR, Lucas JW. Summary health statistics for U.S. adults: National Health Interview Survey, 2007. Vital and Health Statistics. 2009;10(240):1–159. [PubMed] [Google Scholar]
- Powell LM, Chaloupka FJ, Bao Y. The availability of fast-food and full-service restaurants in the United States: Associations with neighborhood characteristics. American Journal of Preventive Medicine. 2007;33(4 Suppl):S240–S245. doi: 10.1016/j.amepre.2007.07.005. [DOI] [PubMed] [Google Scholar]
- Powell LM, Slater S, Chaloupka FJ, Harper D. Availability of physical activity-related facilities and neighborhood demographic and socioeconomic characteristics: A national study. American Journal of Public Health. 2006;96:1676–1680. doi: 10.2105/ajph.2005.065573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prince SA, Adamo KB, Hamel ME, Hardt J, Connor Gorber S, Tremblay M. A comparison of direct versus self-report measures for assessing physical activity in adults: A systematic review. International Journal of Behavioral Nutrition and Physical Activity. 2008;5:56. doi: 10.1186/1479-5868-5-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ravenell JE, Johnson WE, Jr, Whitaker EE. African-American men’s perceptions of health: A focus group study. Journal of the National Medical Association. 2006;98(4):544–550. [PMC free article] [PubMed] [Google Scholar]
- Shephard RJ. Limits to the measurement of habitual physical activity by questionnaires. British Journal of Sports Medicine. 2003;37(3):197–206. doi: 10.1136/bjsm.37.3.197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stables GJ, Subar AF, Patterson BH, Dodd K, Heimendinger J, Van Duyn MA, Nebeling L. Changes in vegetable and fruit consumption and awareness among US adults: Results of the 1991 and 1997 5 A Day for Better Health Program surveys. Journal of the American Dietetic Association. 2002;102:809–817. doi: 10.1016/s0002-8223(02)90181-1. [DOI] [PubMed] [Google Scholar]
- Thompson VL, Talley M, Caito N, Kreuter M. African American men’s perceptions of factors influencing health-information seeking. American Journal of Men’s Health. 2009;3:6–15. doi: 10.1177/1557988307304630. [DOI] [PubMed] [Google Scholar]
- Thorpe RJ, Jr, Wilson-Frederick SM, Bowie JV, Coa K, Clay OJ, LaVeist TA, Whitfield KE. Health behaviors and all-cause mortality in African American men. American Journal of Men’s Health. 2013;7(4 Suppl):8S–18S. doi: 10.1177/1557988313487552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Health & Human Services. 2008 physical activity guidelines for Americans. 2008 Retrieved from http://www.health.gov/paguidelines/guidelines/default.aspx.
- U.S. Department of Health and Human Services. Health, United States, 2011 with special feature on socioeconomic status and health. 2012 Retrieved from http://www.cdc.gov/nchs/data/hus/hus11.pdf. [PubMed]
- Vandelanotte C, Caperchione CM, Ellison M, George ES, Maeder A, Kolt GS, … Mummery WK. What kinds of website and mobile phone-delivered physical activity and nutrition interventions do middle-aged men want? Journal of Health Communication. 2013;18:1070–1083. doi: 10.1080/10810730.2013.768731. [DOI] [PubMed] [Google Scholar]
- Ward E, Jemal A, Cokkinides V, Singh GK, Cardinez C, Ghafoor A, Thun M. Cancer disparities by race/ethnicity and socioeconomic status. CA: A Cancer Journal for Clinicians. 2004;54:78–93. doi: 10.3322/canjclin.54.2.78. [DOI] [PubMed] [Google Scholar]
- Wolf RL, Lepore SJ, Vandergrift JL, Basch CE, Yaroch AL. Tailored telephone education to promote awareness and adoption of fruit and vegetable recommendations among urban and mostly immigrant black men: A randomized controlled trial. Preventive Medicine. 2009;48:32–38. doi: 10.1016/j.ypmed.2008.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolin KY, Yan Y, Colditz GA, Lee IM. Physical activity and colon cancer prevention: A meta-analysis. British Journal of Cancer. 2009;100:611–616. doi: 10.1038/sj.bjc.6604917. [DOI] [PMC free article] [PubMed] [Google Scholar]