Abstract
Background
The Changing Talk (CHAT) intervention successfully improves nursing home (NH) staff communication by reducing elderspeak. However, providing CHAT in NHs is challenging and costly due to presenter travel and staff scheduling. To facilitate dissemination of the CHAT communication training program, the traditional classroom format was modified and interactive online modules were created. The goal was to maintain the content and effectiveness of the original classroom format but to extend access to larger numbers of NH staff. This article reports on the process of transitioning the onsite didactic program to interactive online modules and reports the results of pilot testing evaluating the outcomes of the online modules in comparison to the traditional classroom format.
Methods
Interactive online modules were developed, pilot tested, and the evaluation results were compared to those of participants who previously completed the classroom format training.
Results
Online participants (N=9) demonstrated increased scores on pre and posttest assessments (improved from M=82.4 % to M=91.2 %). Participant ratings of a recorded staff-resident interaction showed improved recognition of elderspeak and person-centered communication after training. Online participants responded similarly to questions on the Modified Diffusion of Innovation Scale, suggesting that online participants had similar intentions to use learned skills in their practice. The majority of participants who completed the program evaluation rated the program highly on all aspects and reported “a great deal of improvement” on the training objectives.
Conclusions
These results suggest that an evidence-based intervention can be translated from traditional classroom to online format maintaining effects on increasing staff knowledge and intentions to use learned skills in practice. However, the modules should be tested in a larger and more representative sample.
The Changing Talk Communication Training Intervention (CHAT) successfully improves nursing home (NH) staff communication by reducing elderspeak and increasing person-centered topics (Williams, 2006; Williams, Ilten & Bower, 2005; Williams, Perkhounkova, et al., in press). Elderspeak is speech that sounds like baby talk that is commonly used by younger NH staff in conversations with older NH residents. Improved nursing staff communication has been demonstrated to improve resident outcomes including reducing behavioral symptoms of dementia and resistiveness to care (Williams, Perkhounkova, Herman, & Bossen, 2016). However, traditional inservice education is challenging to provide in long term care settings due to a number of factors including staff scheduling challenges and costs associated with time and travel for an inservice educator.
To facilitate dissemination of the CHAT communication training program, the traditional classroom format was modified and interactive online modules were created. The goal was to maintain the content and effectiveness of the original classroom format but to extend access to larger numbers of staff and in more NHs. This article reports on the process of transitioning the onsite didactic program to interactive online modules and reports the results of pilot testing evaluating the outcomes of the online modules in comparison to the traditional classroom format.
CHAT is an interactive evidence-based nonpharmacological intervention that reduces behavioral symptoms of dementia and is rated highly by staff (Williams, Perkhounkova, Herman, & Bossen, 2016). CHAT uses actual NH video recordings that illustrate communication and resident responses to engage staff in identifying and correcting ineffective and inappropriate elderspeak. The focus in CHAT is elderspeak communication that conveys negative messages to older adults including individuals with dementia. This limited complexity enables staff to self-monitor and modify their communication during their busy workday. The impact of this novel behavioral approach to improving NH care and reducing behavioral symptoms of dementia has been validated in over 20 NHs (Williams, 2006; Williams, Perhounkova et al., 2016).
Continuing education in NH settings is challenging and strategies to overcome multiple barriers to educating staff and supporting translation to practice are needed to achieve improvement in quality of care (Institute on Medicine, 2009; Silvestre, Bowers, & Gaard, 2015). The traditional classroom format limits staff access and participation, and feasibility of widespread dissemination. Providing CHAT in NHs required a skilled interventionist and extensive time to coordinate, travel, and provide each of the 3 sessions multiple times and days in each NH. In addition, we found that staff shortages, lack of staff to cover resident care, and personal scheduling conflicts limited participation and completion of CHAT in our research in 20 NHs. The percent of enrolled staff who participated in the traditional onsite CHAT training (completing at least 2 of 3 sessions on paid work time) ranged from 44 to 100% and only approximately 50% of participants attended all three sessions (Williams, Perkhoukova, et al., 2016).
CHAT Online (CHATO) modules were designed to overcome barriers to staff access to this communication education with the ultimate goal of promoting translation of this evidence-based intervention into practice. The modules provide flexible, asynchronous, just-in-time access to training, continuously accessible for NH staff via internet connection. CHATO modules maintain the interactivity of the original CHAT format and maximize engagement in learning for participants who must complete the online activities to progress through the modules.
CHAT Intervention
CHAT is conceptually based on the Communication Predicament of Aging that describes how stereotypes of older adults as incompetent prompt younger persons (NH staff) to alter their communication with older adults (NH residents), not considering individual communication and cognitive abilities. The simplification and clarification strategies of elderspeak result in communication that sounds like baby talk and is perceived as demeaning, contributing to isolation, depression, assumption of dependency, and behavioral symptoms (Kemper, Vandeputte, Rice, Cheung, & Gubarchuk, 1995; Ryan, Meredith, Maclean, & Orange, 1995).
CHAT alerts nursing staff to elderspeak and its negative effects, involves them in taking the older adult’s perspective, and guides self-evaluation of their own communication. The hypothesized mechanism of effect is increased awareness of communication from the resident’s perspective and practice of more effective communication without elderspeak (Williams, Kemper, & Hummert, 2004). Improved person-centered communication, tailored to individual resident abilities better meets needs for socialization and supports positive self-concept, improving resident engagement in meaningful interactions and reducing negative outcomes.
Other interventions have effectively trained staff in communication skills. CHAT adds review of actual NH communication examples and practice of improved communication strategies that staff readily apply and monitor in practice, significantly reducing elderspeak in just 3 sessions. CHAT targets adult learners using applied strategies tailored to NH staff to improve specific aspects of elderspeak that are described in the literature and are variable and modifiable. Limiting content and complexity minimizes the burden to NH staff and their employers and increases the likelihood of skill enactment (Banazak et al., 2000).
Session one introduces effective versus ineffective communication. Participants identify communication issues in video vignettes. Session two focuses on elderspeak, its identification and negative effects, and uses video recordings as examples. The final session includes strategies for improved communication based on assessment of each resident’s abilities. Participants critique videos and correct transcripts eliminating elderspeak. To assure a feasible program for today’s busy NH environment, the intervention was limited to 3, 1-hour sessions. Additional description of CHAT is provided in a related publication (Williams, Kemper, & Hummert, 2004).
The goal for designing and development of the online CHATO modules was to provide the same content as the CHAT training, but in a more accessible format that would motivate and engage adult learners and further improve learning outcomes. Online (distance-learning) training was chosen to extend the reach of training to a vast audience for whom training might not be otherwise available.
The subject matter expert nurse educator worked with an instructional designer, item writer, and media team to transition the face-to-face CHAT training into three hour-long online modules (CHATO) provided through a learning management system. The course was developed using Articulate Storyline and published as a Sharable Content Object Reference Model package and integrated into the learning management system. This technology creates an online module that can be shared across different systems and also provides’ tracking information and scoring for assessments, providing the ability to read, run, and report students’ progress on the online modules. Technical elements and functionality were alpha tested.
The ADDIE model is widely accepted as an instructional design framework for building effective training for adult learners and was used to guide preparation of the CHATO modules (Gagne, Wager, Golas, & Keller, 2010). Steps in the ADDIE model includes: Analysis, Design, Development, Implementation, and Evaluation. In the Analysis phase, the nurse educator and instructional designer worked together to identify characteristics of the target audience, and their knowledge gaps, and learning constraints. Pedagogical considerations, adult learning theory, and delivery options were all considered in developing the modules. Measurable outcomes were identified along with a timeline for project completion.
In the Design phase, measurable learning objectives were adapted from the original CHAT program, based on the desired outcomes. These learning objectives guided subsequent design of the content, interactivity, video, review questions, media selection, and assessment items (review questions, and pretest and posttest items). Storyboards of the thought processes were created with attention to detail in visualizing instructional ideas.
In the Development phase, the instructional designer, media specialists, item writer, and nurse educator worked to develop all the pieces, using technology and authoring tools. This phase included audio and video recording of text to accompany didactic information in the program. In the next phase, implementation, the materials were assembled and integrated into the learning management system. The process also included testing the functionality and user interface, the integration of pretest and posttest, and the addition of an evaluation instruments for assessing learning satisfaction and intention to use learned skills in practice.
The final Evaluation phase involved pilot testing of the eLearning CHATO program. Evaluative data were collected and analyzed, and revisions were made. The use of the ADDIE model ensured that all eLearning products were developed and evaluated systematically, thus ensuring the quality of the final product.
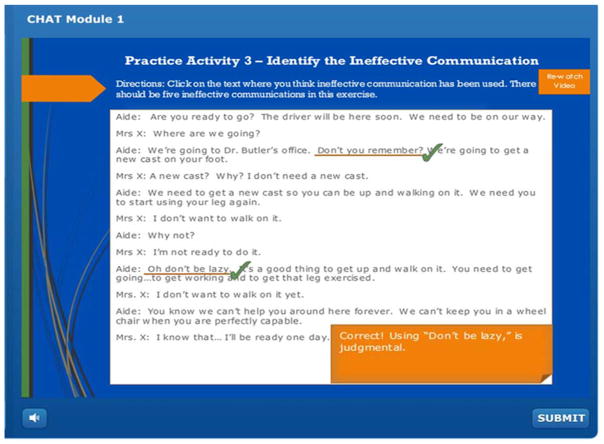
The design of the CHATO online course was also guided by the principles of adult learning theory. Knowles (1990) states that adults’ learners should play an active role, because their experience provides the most effective learning. Real life applications and benefits, including actual video footage recorded in NHs, were used in this eLearning course, with opportunities for the adult learners to test out and absorb information rather than memorizing it. See a screen shot of an example activity in Figure 1.
Figure 1.
Example of Interactive Activity in CHATO Module.
A total of 20 video clips and 9 interactive exercises were integrated into the CHATO modules. Ehlers (2004) established that multimedia can improve the quality of eLearning and Neo & Neo (2000) have identified that combinations of multimedia elements are needed to create interactive educational content, a stimulating learning environment, and increased knowledge retention. Attention was paid to effective visual design, established as essential for engaging learners in making inferences and acquiring new skills and also making an impact on learners’ emotions, increasing their sense of engagement and motivation (Malamed, 2015).
Module development was also based on five elements of game design that provide a robust and exciting way to ensure that learners are immersed in the learning process and that the learning is applied on the job (Kapp, 2012). Those elements are contextualization, curiosity, control, cooperation/socialization, and engagement/interactivity. Game-based learning engages learners, provides a safe environment in which to fail, increases motivation, and increases retention of knowledge and skills. The practice activities incorporated into the modules used the interactivity aspect of game design. For example students have the opportunity to try finding ineffective communication in a transcript, then, they are asked to type in how they think the dialog should be fixed, and lastly they compare their answers to the recommendation answer. Simulation-like or scenario-based questions were also included to present learners with realistic situations in which to make decisions or apply new knowledge. Students retain more from scenario-based learning than other forms of presentation with estimated retention rates of 78 percent for scenario-based activities, compared to 20 percent for audiovisual presentations, 10 percent for reading, and 5 percent for lecture (NTL Insititute for Applied Behavioral Sciences, 2005).
The CHATO modules are readily available using an internet hyperlink. Each participant establishes a password protected account and provides basic demographic information. Pre and posttest and evaluations are contained in the modules. Participants can log out and back in if more time is needed to complete modules. Content of the CHATO modules mirrors that of the CHAT program. Narrated PowerPoint content provides information followed by application exercises that engage the participant. The videos of actual staff-resident interactions (N=20) and simulated vignettes present alternative communication styles and are played online to illustrate features of elderspeak and how messages to residents can vary. Although group activities in the online modules are limited to an online discussion, participants are engaged and must pay attention and complete each activity to progress through the modules.
Pilot Testing
Following approval from the University Institutional Review Board for the Protection of Human Subjects, a small convenient sample (n = 9) was recruited to pilot test the modules. Evaluation tools were integrated into the modules. A scenario-based assessment and ratings of communication in a selected video recording were completed before and after the training. After the third and final module, participants completed the Modified Duke Diffusion of Innovation questionnaire (McConnell et al., 2012) and a program evaluation adapted from the original CHAT program.
The scenario-based assessment was developed by an item writer in conjunction with the nurse educator and administered before and after CHATO training. The assessment was designed to assess applied knowledge about appropriate communication. Each item tested knowledge of a specific concept using a unique scenario. Participants were tested prior to training with a set of 13 items, and after training with a corresponding set of different 13 items, each reflecting one of the 13 learning objectives that were identified at the beginning of the training. Each learning objective addressed specific content and contained an action verb, based on Bloom’s Taxonomy (Su & Osisek, 2011). To achieve equivalent difficulty of items before and after training, the same action verb was used for the corresponding questions. In addition, content experts reviewed the questions for difficulty level. A third set of questions addressing each learning objective was developed as a retest for participants who failed to score 70% or greater on the posttest. Examples of scenario-based items are presented in Table 1. After answering each question, the rationale explaining correct and incorrect answers was presented.
Table 1.
Scenario-based Questions Addressing Same Content (* indicates correct answer).
| Pre-test Question | Post-test Question |
|---|---|
|
| |
| Martina, a nurse aide working in a nursing home, is challenged to communicate effectively with Bernie, a resident with dementia who is stealing items that he has mislaid due to memory loss. This challenge illustrates which of these components of effective interpersonal communication? | Dana is a nursing home resident who often complains that, “no one in my family ever comes to see me. They must not love me.” Helen, one of her CNAs, expresses empathy for Dana’s perspectives on family without criticizing anything she says. Helen’s approach demonstrates which of the components of effective interpersonal communication? |
| Answer choices: Environment, Shared language, Mental Abilities*, Expectation of response | Answer choices: Environment, Shared language, Common frame of reference, Openness* |
|
| |
| A CNA tells Mrs. Sherman, a nursing home resident, to wait in her room while she goes to get some answers to her questions about a medication. Mrs. Sherman says, “How long do I have to wait?” Which of these responses is the most affirming? | Mrs. Howard, a nursing home resident, tells you her room is too cold and she wants the heat turned up. Which of these responses to her request is the most affirming? |
| Answer Choices: “It shouldn’t take long, Mrs. Sherman. Thanks for waiting.”* “Don’t worry about a thing, dear. It should only take a minute.” “You sure are an impatient little thing. It should only take a minute.” “I’m not sure, but you know what they say, ‘All good things come to those who wait.’” |
Answer Choices: “Here, put this sweater on. That’ll fix the problem.” “It sounds like we’re feeling chilly today. Let me get you a sweater.” “The thermostat says 68, Mrs. Howard. Do you want it turned up?”* “A good way to warm up is to take a walk. Why don’t you do that?” |
|
| |
| Imagine you are a nursing home resident named Mrs. Abrams who tells a CNA, “I could kick myself for forgetting yesterday’s hair appointment. I hate it when my hair looks all scraggly like this.” Which of the following responses is most likely to make you feel respected and valued as a person? | Imagine you are a nursing home resident named Mr. McCaffrey who’s getting dressed for a holiday lunch. You tell the CNA who is helping you pick out your clothes, “I don’t want that blue shirt. I want my favorite plaid flannel one over there in the basket.” Which of the following responses is most likely to make you feel respected and valued as a person? |
| Answer choices: “How could you forget something important like that?” “You’re such a perfectionist: I wouldn’t let it bother me.” “I can see why you’re upset. Do you need help calling for another appointment?”* “That’s too bad, Mrs. Abrams, but you can’t change the past, so stop kicking yourself.” |
Answer choices: “You can’t wear the plaid shirt. You wore it yesterday. Please put this one on.” “We can’t wear the same clothes every day, Mr. McCaffrey. No one will sit next to you..” “I’m sorry, Mr. McCaffrey, but your favorite shirt is headed for the laundry. Is there another one that will work for the holiday lunch today?”* |
Ratings of communication in a selected staff-resident interaction video recording were also obtained pre and post CHATO training. The Communication Rating Scale was developed to assess the staff’s ability to identify elderspeak and other appropriate and inappropriate communication practices, and to evaluate the applied knowledge gain of participants. Each participant watched a video of a staff-resident interaction recorded in an actual NH and rated staff communication at the start of session one and also reviewed the same clip after the final session. One item each was used to rate both global effectiveness and overall appropriateness of staff communication. The items assessed effectiveness and overall appropriateness on a five-point Likert-type scale with ratings ranging from 1=ineffective/inappropriate to 5=effective/appropriate (lower scores indicating recognition of less effective and appropriate communication).
To assess recognition of patronizing elderspeak communication, six questions measured the ability to detect the presence of patronizing communication or elderspeak (1=present, 0=absent) in the video. The questions asked participants to recognize baby talk, inappropriately intimate terms of endearment, speaking too loud, speaking too slow, and substituting “we” and “us” when talking about things only the resident would do. The total count of elderspeak features used in the video ranged from 0 to 6 and indicated an overall recognition of elderspeak communication.
Four additional questions measured recognition of person-centered communication by asking participants to detect communication acknowledging the resident and their statements, asking clarifying questions, and addressing the resident by their preferred name (1=present, 0=absent). The total number of the features of person-centered communication in the video ranged from 0 to 4 and indicated an overall recognition of person-centered communication.
A revised version of the Modified Duke Diffusion of Innovations in Long Term Care Battery (McConnell et al., 2012) assesses participant perceptions of the communication practices taught in CHATO and the likelihood that they will use the skills in practice. This scale includes 20 items in four subscales, each rated on a six-point scale. Subscales include relative advantage, complexity and compatibility with current care practices, ability to observe new practices and effect on image, and organizational support for the innovation. The subscales have demonstrated internal consistency reliability (Cronbach’s alpha ranging from .77 to .95), and the scale highly correlates with intention to adopt new practices for nurses (Spearman Rho = .41 to .68, p< .001) and certified nursing assistants working in long term care (Spearman Rho = .26 to .54, p< .05) (McConnell et al., 2012).
Program evaluation included ten questions about increasing knowledge, usefulness in care, intention to implement, usefulness of materials, clarity and overall satisfaction. Participants rated the program for these qualities using a 1=”Strongly Disagree” to 5=”Strongly Agree” scale. An additional thirteen questions asked participants to rate the degree to which their knowledge and abilities improved after taking the course, using a 1 to 4 scale (1=”No Improvement,” 2=”Little Improvement,” 3=”Moderate Improvement,” and 4=”A Great Deal of Improvement”). A question about difficulty of the training was also included with possible replies as “too difficult,” “challenging, but not too difficult,” “fairly easy”, and “too easy”.
Analysis of data
Descriptive data for each variable were summarized, and paired samples two-tailed t-tests were used to compare scores on the scenario-based assessment and communication ratings pre- and post-training. Diffusion of Innovation in Long Term Care scores of CHATO participants were compared to those of participants in the earlier classroom format CHAT program using independent samples two-sided t-tests. The t-tests were chosen despite the small sample size (total n = 9, matched n = 7) to evaluate preliminary the effectiveness of CHATO. Additionally, Cohen’s ds, a measure of effect size, were calculated for changes in communication ratings to assess the magnitudes of the changes.
Results
CHATO was pilot tested by a convenient sample of 2 RNs, 4 CNAs, and 3 nursing students (n=9), enrolled in a university setting with current or past NH practice experience. They were all female ranging from 18 to 41 years of age. Time spent in completing the modules ranged from 24 to 56 (M = 40) minutes for module 1, 19 to 45 (M = 36) minutes for module 2, and 18 to 56 (M = 32) minutes for module 3. The time between participant completion of the pre and post assessments ranged from 1 to 7 (M = 4) days.
Mean percentage of correct responses on the scenario-based assessment improved from 82.4% (SD = 10.6) to 91.2% (SD = 8.2) with a mean change of 8.8 percentage points (SD = 12.1, n = 7, p = .10). Mean communication ratings of staff communication are provided in Table 2 for pre- and post-training (n = 7), along with p-values for paired sample, two-tailed t tests and effect sizes. Mean ratings of effectiveness and appropriateness of communication in the video decreased significantly (from 2.3, SD = 0.8, to 1.2, SD = 0.4, p = .02, d = 1.22 for effectiveness; and from 2.6, SD = 0.8, to 1.1, SD = 0.5, p = .005, d = 1.65 for appropriateness). The ability to recognize elderspeak and person-centered communication also improved, although not significantly.
TABLE 2.
Communication Ratings Pre and Post CHATO Training (n=7)
| Pre | Post | t (df) | p | Cohen’s d | |
|---|---|---|---|---|---|
|
| |||||
| M ± SD | M ± SD | ||||
| Communication effectiveness | 2.3 ± 0.8 | 1.2 ± 0.4 | 3.2 (6) | .02 | 1.22 |
| Communication appropriateness | 2.6 ± 0.8 | 1.3 ± 0.5 | 4.4 (6) | .005 | 1.65 |
| Recognizes elderspeak | 0.8 ± 0.2 | 0.9 ± 0.2 | −0.6 (6) | .60 | 0.22 |
| Recognizes person-centered communication | 0.3 ± 0.2 | 0.1 ± 0.2 | 2.0 (6) | .09 | 0.76 |
Note: Ratings of communication range from 1=ineffective/inappropriate to 5=effective/appropriate (lower scores indicate better recognition of ineffective/inappropriate communication); recognition indicates number of features of elderspeak (ranging 0–6, higher score is better) or person-centered communication (ranging 0–4, lower score is better) identified in the video clip; p is p-value for paired samples 2-tailed t-test.
Table 3 displays scores on the Diffusion of Innovation in Long Term Care scale for participants in this CHATO study (n = 9) and the original classroom CHAT study (n = 196). With the exception of the Observability/Image factor (that CHATO participants rated higher, p = .001), the CHATO group expressed intentions for translating learned skills to practice similar to CHAT participants.
TABLE 3.
Modified Diffusion of Innovation Scale Scores for CHAT and CHATO
| CHAT (n=197*) | CHATO (n=9) | t (df) | p | |
|---|---|---|---|---|
|
| ||||
| M ± SD | M ± SD | |||
| Relative Advantage | 1.5 ± 0.6 | 1.4 ± 0.4 | −0.8 (203) | .40 |
| Complexity and Compatibility | 2.9 ± 0.9 | 2.7 ± 0.7 | −0.7 (204) | .46 |
| Observability/Image | 1.5 ± 0.6 | 2.1 ± 0.8 | 3.4 (202) | .001 |
| Organizational Support | 1.7 ± 0.8 | 2.1 ± 1.2 | 1.2 (202) | .23 |
| Intention to Use | 2.0 ± 1.0 | 1.6 ± 0.9 | −1.2 (203) | .21 |
| Total Score | 2.0 ± 0.5 | 2.0 ± 0.6 | −0.3 (204) | .75 |
Note: Modified Diffusion of Innovation in Long Term Care scores range from 1 = strongly agree to 6 = strongly disagree;
ns for scales ranged from 195 to 197; p is p-value for independent samples two-tailed t-test
Eight participants who completed program evaluation rated the program highly on all aspects: the majority of their ratings was highest (5 =strongly agree), and the mean rating for each of the ten program qualities was at least 4.6. Four participants rated CHATO as fairly easy and four participants found it challenging, but not too difficult. Six participants reported “a great deal of improvement” on outcomes reflecting the 13 program objectives, and the remaining two participants reported “little” or “moderate improvement” on some of these outcomes.
Discussion
Although pilot testing included only a small sample, we found preliminary evidence of effectiveness for the interactive online modules. Mean percentage of correct responses on the scenario-based assessment increased by 8.8 percentage points on average. While the questions were different for pre and post assessments, we made an effort to make the versions of the assessment as similar as possible in terms of content coverage and difficulty. Thus, an increase in correct replies should indicate improved knowledge of appropriate communication. However, further testing of this assessment is needed in a larger sample to determine whether the difficulty levels of different versions are similar.
Ratings of communication effectiveness and appropriateness in the video clip decreased significantly after the CHATO training: that is, participants learned to recognize the lack of communication effectiveness and appropriateness. The average decreases in ratings were more substantial (from 2.3 to 1.2 for effectiveness and from 2.6 to 1.3 for appropriateness) than corresponding statistically significant decreases in the classroom CHAT study that used unmatched samples pre and post training (from 2.4 to 2.1 for effectiveness and from 3 to 2.5 for appropriateness). At the same time, the observed improvements in the ability to recognize elderspeak and person-centered communication were not statistically significant in the current study, while they were statistically significant (p < .001 and p = .02, respectively) in the study of classroom CHAT which had a larger sample (n ranging from 194 to 199, depending on the measure).
Evidence of improved ability to evaluate communication after the online modules was found despite concern that the group consensus regarding appropriate and inappropriate communication from group discussions in the classroom would be lost in the online module format. A CHAT trainer who reviewed the CHATO modules commented that CHATO effectiveness may be due to the fact that participants must individually complete the interactive activities spaced throughout the modules and thus become more engaged in learning online, compared to classroom training sessions.
Generally, the CHATO group expressed intentions for translating learned skills to practice similar to CHAT participants. However, CHATO participants rated the Observability/Image factor higher than the CHAT group; that is; they perceived that their new communication practices would result in a greater improvement in their professional image. The majority of participants who completed the program evaluation rated the program highly on all aspects and reported “a great deal of improvement” on the training objectives. The participants split on their rating of CHATO as fairly easy or challenging, but not too difficult.
However, the results for the CHATO study should be interpreted with caution considering the small convenient sample of persons affiliated with a university that may not represent characteristics of NH staff. Future larger scale testing in NH staff is indicated to validate these preliminary findings.
Data indicated that each module was completed within a one-hour time for completion, similar to the classroom format CHAT program. Time to complete all of the modules, including pre and post assessments, ranged from 1 to 7 days with an average of 4 days. Ongoing monitoring of time to complete each module may be used to identify areas for additional content and interactive activities to engage participants.
Minor revisions were made to the modules after this pilot, including clarifying directions for completing the interactive exercises and some of the pre- and post-training questions and requiring completion of the interactive exercises to advance in the modules. However, further evaluation of the modules in a larger sample of nursing home staff is recommended prior to wide-scale dissemination of the modules.
Longstanding issues in providing continuing education for NH and other long term care staff may be overcome if effective online training is used. Staff perceptions of relative advantage, complexity, compatibility, trial ability, and observability all determine likelihood of use of learned skills in practice (McConnell et al., 2012). CHATO is easily implemented because staff self-monitor and modify communication in practice using simple CHATO communication techniques. Within the Diffusion of Innovations Framework (Cain & Mittman, 2002), 10 critical dynamics supporting diffusion are met. CHATO alerts staff to relative advantages of CHATO communication and provides opportunities to try out improved communication. The limited focus on a few key features of elderspeak also facilitates adoption. CHATO leads staff through the innovation-decision process by engaging them in taking the perspective of the resident in viewing and correcting vignettes of NH communication. Participants evaluate and confirm their decision to improve communication with residents through interactive exercises.
Partnering with a professional team provided the expertise needed to make the online modules truly interactive with varied, engaging activities, based on evidence-based teaching and learning strategies. Despite an initial cost investment to create the modules, online delivery is a more cost-effective way to reach increasing numbers of staff, through asynchronous and independent access for busy NH staff, readily available via internet access.
Even with added up-front costs for design, and costs for ongoing maintenance on a server and technical assistance, online CHATO eliminates costs for interventionist preparation, coordination, and travel and time to provide CHAT onsite on multiple days and times. While maintaining the expert instruction, encouragement, and video illustrations that result in reductions in elderspeak, we estimate reduced costs for CHATO will average $39.09 per staff participant (for 500 staff CHATO participants per year) compared to $79.69 in our CHAT (traditional classroom format) study (Williams, Ayyagari, et al., in press). Costs will be further reduced if CHATO is disseminated to larger numbers of NHs and NH staff.
CHATO and other online education is ideal for rural NHs or small independent facilities that frequently have unmet needs for staff education, fewer resources, less access to programs, and greater costs to provide staff education. For those NHs with high turnover, CHATO accessibility provides a convenient way to educate new staff as they are hired.
CHATO has potential for application across NHs and long term care settings such as assisted living, adult day care, and home care and may be adapted for the service sector in the future. However, access to online education alone may not improve staff participation. Research is needed to determine whether the improved access to education such as CHATO will result in greater participation rates by staff and NHs and how best to provide CHATO and other online education for successful widespread dissemination.
CHATO is an online adaptation of an evidence-based intervention that provides increased accessibility for staff in NH and other settings. Online education is one approach to continuing education for NH staff. As the population ages, it is increasingly important to assure care quality and to ensure a workforce with high-quality care skills (Borson et al., 2016; Institute on Medicine, 2009). Online education is one approach to accomplish this goal.
Acknowledgments
This research was supported by NIH grant NR011455-04, Changing Talk to Reduce Resistiveness in Dementia Care, K. Williams, PI. The sponsor was not involved in study design, data collection and analysis, interpretation of findings, and manuscript preparation. ClinicalTrials.gov Identifier: NCT01324219.
The authors wish to thank Maria Hein, MSW, & Ann Bossen, PhD for assistance with this project.
References
- Banazak DA, Mickus M, Averill M, Colenda CC. Herding cats: Barriers to implementing a nurse aide educational program. Annals of Long-Term Care. 2000;8(10):68–71. [Google Scholar]
- Borson S, Boustani MA, Buckwalter KC, Burgio LD, Chodosh J, Fortinsky RH, … Geiger A. Report on milestones for care and support under the U.S. National Plan to Address Alzheimer’s Disease. Alzheimer’s & Dementia: The Journal of the Alzheimer’s Association. 2016;12(3):334–369. doi: 10.1016/j.jalz.2016.01.005. [DOI] [PubMed] [Google Scholar]
- Cain M, Mittman R. Diffusion of Innovation in Health Care. 2002 Retrieved from Oakland, CA: http://www.chcf.org/documents/healthit/DiffusionofInnovation.pdf.
- Ehlers U. European Journal of Vocational Training. 2004. Quality in E-Learning. The Learners Perspective. [Google Scholar]
- Gagne RW, Wager WW, Golas KC, Keller JM. Principles of Intructional Design. 5. Belmont, CA: Wadsworth; 2010. [Google Scholar]
- Institute on Medicine. Redesigning Continuing Education in the Health Professions. 2009 Retrieved from https://www.nap.edu/catalog/12704/redesigning-continuing-education-in-the-health-professions.
- Kapp K. Training Industry Quarterly. 2012. Fall Five Gaming Elements for Effective e-Learning. [Google Scholar]
- Kemper S, Vandeputte D, Rice K, Cheung H, Gubarchuk J. Speech adjustments to aging during a referential communication task. Journal of Language and Social Psychology. 1995;14(1–2):40–59. [Google Scholar]
- Knowles M. The adult learner: A neglected species. 4. Houston, TX: Gulf Publishing; 1990. [Google Scholar]
- Malamed C. Visual Design Solutions: Principles and Creative Inspiration for Learning Professionals. Hoboken, NJ: John Wiley and Sons, Inc; 2015. [Google Scholar]
- McConnell ES, Corazzini KN, Lekan D, Bailey DE, Sloane R, Landerman LR, Champagne MT. Diffusion of innovations in long-term care measurement battery. Research in Gerontological Nursing. 2012;5(1):54–76. doi: 10.3928/19404921-20110602-04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neo M, Neo TK. Multimedia learning: Using multimedia as a platform for instruction and learning in higher education. Paper presented at the Multimedia University Inteernational Symposium on Information and Communication Technologies 2000 (M2USIC’2000); Kuala Lumpur, Malaysia. Oct 5–6, 2000. [Google Scholar]
- NTL Insititute for Applied Behavioral Sciences. The Learning Triangle: Retention Rates from Different Ways of Learning. Bethel, Maine: 2005. [Google Scholar]
- Ryan EB, Meredith SD, Maclean MJ, Orange JB. Changing the way we talk with elders: Promoting health using the communication enhancement model. International Journal of Aging and Human Development. 1995;41(2):89–107. doi: 10.2190/FP05-FM8V-0Y9F-53FX. [DOI] [PubMed] [Google Scholar]
- Silvestre JH, Bowers BJ, Gaard S. Improving the Quality of Long-Term Care. Journal of Nursing Regulation. 2015;6(2):52–56. doi: 10.1016/S2155-8256(15)30389-6. [DOI] [Google Scholar]
- Su W, Osisek P. The Revised Bloom’s Taxonomy: Implications for Educating Nurses. Journal of Continuing Education in Nursing. 2011;42(7):321–327. doi: 10.3928/00220124-20110621-05. [DOI] [PubMed] [Google Scholar]
- Williams K. Improving outcomes of nursing home interactions. Research in Nursing and Health. 2006;29:121–133. doi: 10.1002/nur.20117. [DOI] [PubMed] [Google Scholar]
- Williams K, Ayyagari P, Perkhounkova Y, Bott M, Herman R, Bossen A. Costs of a Staff Communication Intervention to Reduce Dementia Behaviors in Nursing Home Care. Journal of Nursing Home Research Studies. doi: 10.14283/jnhrs.2017.4. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams K, Ilten T, Bower H. Meeting communication needs: Topics of talk in the nursing home. J Psychosoc Nurs Ment Health Serv. 2005;43:38–45. doi: 10.3928/02793695-20050701-05. [DOI] [PubMed] [Google Scholar]
- Williams K, Kemper S, Hummert ML. Enhancing communication with older adults: Overcoming elderspeak. The Journal of Gerontological Nursing. 2004;30:1–10. doi: 10.3928/0098-9134-20041001-08. [DOI] [PubMed] [Google Scholar]
- Williams K, Perkhounkova Y, Herman R, Bossen A. A Communication Intervention to Reduce Resistiveness in Dementia Care: A Cluster Randomized Controlled Trial. The Gerontologist. 2016:1–12. doi: 10.1093/geront/gnw047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams K, Perkhounkova Y, Jao Y-L, Bossen A, Hein M, Chung SJ, … Turk M. Person-Centered Communication for Nursing Home Residents with Dementia: Four Communication Analysis Methods. Western Journal of Nursing Research. doi: 10.1177/0193945917697226. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]