Abstract
Background: A mobile health (mHealth) technology based application was developed to help rural health care providers (RHCPs) identify and refer presumptive tuberculosis (TB) patients to the nearest microscopy centre for sputum examination using mobile applications on their smart phones.
Objective: To determine the feasibility and yield of presumptive TB case referrals by RHCPs using mHealth technology.
Methods: The project was implemented in the tribal population of Khunti District, Jharkhand State, India, from April 2012 to February 2015. ‘ComCare’, a mobile application designed as an aid for health care providers, was introduced and RHCPs were trained in its use.
Results: Of 171 RHCPs who were formally trained to identify and refer presumptive TB patients, 30 were trained in the use of the mobile application. There were 35 referrals of presumptive TB patients per RHCP using the mobile application, and four each by RHCPs who were not using the application. Of the 194 TB cases diagnosed, RHCPs using the application contributed 127 (i.e., 4 TB cases per RHCP), while other RHCPs contributed 67 (0.5 TB case per RHCP).
Conclusion: mHealth technology was highly effective, and increased both public and private health care provider accountability to patients.
Keywords: mHealth, rural health care providers, RHCP, tuberculosis, India
Abstract
Contexte: Un modèle de soins de santé via une application mobile (mHealth) a été élaboré afin de donner davantage d'autonomie aux prestataires de soins ruraux (RHCP) pour identifier et référer les patients présumés atteints de tuberculose (TB) au centre de microscopie le plus proche pour un test basé sur une application mobile.
Objectif: Déterminer la faisabilité et le rendement de la référence des cas de TB présumés par les RHCP en utilisant mHealth.
Méthodes: Le projet a été mis en œuvre dans la population tribale du district de Khunti, dans l'état de Jharkhand, Inde, d'avril 2012 à février 2015. L'application mobile, appelée « ComCare », qui permet d'intégrer les prestataires de soins de santé, a été introduite et les prestataires de soins ont été formés à son utilisation.
Résultats: Ont bénéficié 171 RHCP d'une formation officielle afin d'identifier et de référer les patients présumés TB ; 30 d'entre eux ont été formés à l'utilisation de l'application mobile (mRHCP). Il y a eu 35 références pour TBP des cas présumés par les mRHCP (c'est-à-dire les utilisateurs de l'application mobile) et 4 références pour TBP par les RHCP parmi les oRHCP (ceux n'utilisant pas l'application mobile). Au total, 194 cas de TB ont été diagnostiqués : la contribution des mRHCP a été de 127 (soit 4 cas de TB par RHCP), tandis que les références des oRHCP ont été de 67 (soit 0,5 cas de TB par RHCP). Le nombre de patients TB diagnostiqués et mis sous traitement dans la journée suivant le diagnostic a été plus élevé parmi les patients référés par les mRHCP comparés aux oRHCP.
Conclusion: L'utilisation de la mHealth pour les RHCP est très efficace et elle augmente la responsabilité des prestataires de soins de santé à la fois publics et privés vis-à-vis des patients.
Abstract
Marco de referencia: Se elaboró un modelo de atención de salud utilizando una aplicación para teléfonos portátiles (mHealth), que faculta a los trabajadores de salud en medio rural (RHCP) a detectar a los pacientes con presunción clínica de tuberculosis (TB) y remitirlos al centro de microscopia más cercano, a fin de practicar las pruebas diagnósticas.
Objetivo: Determinar la viabilidad y el rendimiento de la remisión de casos con presunción de TB por parte de los RHCP mediante la utilización de una aplicación mHealth.
Métodos: El proyecto se ejecutó en la población tribal del distrito de Khunti, en el estado de Jharkhand de la India, de abril del 2012 a febrero del 2015. Se introdujo una aplicación para teléfonos portátiles denominada ‘ComCare’ que comporta una función de integración de los prestadores de atención de salud y se ofreció capacitación sobre su funcionamiento a estos usuarios.
Resultados: Se impartió la capacitación formal sobre la detección y la remisión de los pacientes con presunción de TB a 171 RHCP y 30 de ellos se capacitaron en la utilización de la aplicación para teléfonos portátiles (mRHCP). Los profesionales que utilizaban la aplicación remitieron 35 pacientes por RHCP con presunción de TB y los demás profesionales que no la utilizaban (oRHCP) remitieron cuatro pacientes por RHCP. Se diagnosticaron 194 casos de TB, de los cuales 127 por conducto del programa de telefonía móvil (4 casos por mRHCP) y 67 fueron remitidos por los RHCP que no utilizaban la aplicación (0,5 casos por oRHCP).
Conclusión: La utilización de aplicaciones sanitarias mHealth por parte de los RHCP es de gran eficiencia y fomenta la responsabilización de los trabajadores del sector público y el sector privado frente a los pacientes.
Mobile health (mHealth), i.e., the use of portable electronic devices with software applications to provide health services and manage patient information,1 has the potential to transform health service delivery worldwide.2 mHealth has a crucial role to play in health care systems, as it can improve communication and enhance the integration of health care processes.3 Low- and middle-income countries have extensive cellular networks, and the majority of the population has mobile phones.2
Tuberculosis (TB) remains a major public health problem in India, accounting for 23% of the global TB burden.4 Despite case-finding efforts by the Revised National TB Control Programme (RNTCP), the country is believed to have up to one third of the estimated three million TB cases that remain unnotified worldwide.4 Nearly 50% of TB patients are treated in the private sector, where health care providers include specialist physicians as well as unqualified providers.5
The RNTCP has various schemes for non-governmental organisations and private practitioners (PPs) that allow private health care providers to sign an official memorandum of understanding with the Government to provide RNTCP services, for which PPs are offered incentives.6,7 However, the involvement of PPs in these schemes is not optimal due to the complicated procedures involved and the RNTCP's delay in providing incentives; furthermore, much of the focus is on allopathic doctors and their health facilities, which are generally located in urban and semi-urban areas. In rural areas, public health services are difficult to access, as the facilities are often located far from the inhabitants and there is poor transport connectivity. In addition, health care personnel capable of providing these services are sometimes lacking at these facilities; similar problems are observed across the country. There are very few qualified private health care providers in rural areas.8,9 The first point of contact for any kind of ailment are health care providers who often lack formal training or are trained in alternative medicine.5,10 Nearly 72% of health care in rural areas is provided by the private sector, and nearly 81% of the doctors are unqualified.11 The provider-to-patient ratio in India is 1:2000.12
Until now, the RNTCP had not attempted to involve unqualified health care providers/rural health care providers (RHCPs) in TB care, although they are responsible for the management of a significant number of presumptive TB cases and TB patients. These practitioners play an important role in TB control. As the first point of contact for the majority of the rural population, they can be trained to identify presumptive TB cases early and refer them to diagnostic and treatment services, thus preventing delays. They can also be effective providers of directly observed therapy (DOT), as they have earned the confidence and trust of the community they serve. Global efforts have been made to involve all stakeholders in general, but do not specifically address the role of unqualified practitioners. A health care model was therefore envisioned to help RHCPs identify and refer presumptive TB cases to the nearest microscopy centre for testing. Referrals were tracked using an mHealth platform integrating communications between private and public health care providers and patients for the delivery of quality care services. The model was designed to increase the number of referrals of presumptive TB cases, reduce diagnostic and treatment delays and educate presumptive TB cases about TB.
The objective of the present study was to determine the feasibility of using mHealth technology to increase the yield of presumptive TB case referrals among RHCPs. The South-East Asia Office of the International Union Against Tuberculosis and Lung Disease, New Delhi, India, implemented the project in a tribal area of Khunti District in Jharkhand State, India.7,13
METHODS
The study was implemented in a project area covering a tribal population of 0.5 million in Khunti District from April 2012 to February 2015. The population in the region is mainly dependent on agriculture, and the availability and accessibility of health care services is suboptimal.14 The district has two RNTCP TB units (TUs, i.e., programme management units for a population of 0.25 million), Khunti TU and Torpa TU, with six microscopy centres located at public health facilities.
Under the current programme setting, any presumptive TB case who approaches a private health care provider is referred to a microscopy centre located at a public health facility for diagnosis. Referral mechanisms are paper-based, and feedback on results to the referring physicians is suboptimal.9 Communicating test results is vital for the next course of action for the patient.
Creating awareness in the community to improve the referral of presumptive TB cases can be done through programme advocacy, communication and social mobilisation, and is especially important in tribal and hard-to-reach areas. Under the project, efforts were made to mobilise all the RHCPs identified by project staff in the area to participate in the RNTCP training programme. The RHCPs were encouraged to refer presumptive TB cases to RNTCP-designated microscopy centres for sputum examination and were asked to use mobile applications for case referrals and feedback. Those RHCPs who were proficient in using social media mobile applications, such as WhatsApp and Facebook, and who were interested in using mobile applications provided written consent to participate in the mHealth referral system; they then installed the mobile application onto their own phones with the help of the project staff.
As strengthening the referral system for presumptive TB cases is a routine programme activity, ethics clearance was not required; however, permission to conduct the activity was obtained from the District and State TB Officers, with whom the project was implemented.
An mHealth application named ‘ComCare’ was developed in collaboration with Dimagi® (Cambridge, MA, USA). This downloadable application is designed for health care providers and manages patient information. As the mobile application is not available in the public domain for free download, the project staff transferred the application to the RHCPs' mobile phones using freely available sharing technologies. The application was developed to support android mobile phones, and the programme managers had access to the internet.
Data flow and management of patient information is shown in Figure 1: 1) health care providers (RHCPs, laboratory technicians and supervisors) download and install the mobile application. The application can be accessed by different user interfaces, such as RHCP, laboratory technician and supervisor; 2) any presumptive TB cases identified by RHCPs are referred to a microscopy centre after the patient details (name, age, sex, contact number, name of village, referred microscopy centre and date of referral) have been entered using the options available in the application; 3) the laboratory technician of the microscopy centre and the supervisors can view the information on the cases referred by the RHCPs on their mobile phones; 4) the laboratory technicians confirm the arrival of the patient and transmit the examination results to the referring RHCP and supervisors using the application; 5) the laboratory technicians also transmit the results to the presumptive TB cases/patients via in-built text messages; 6) if the referred cases fail to visit the microscopy centre within 7 days of referral, the application generates a reminder via short messaging service (SMS) to the patient, the RHCP and the supervisor; and finally, 7) the application assists health care providers in providing guidance and counselling to patients. Various messages reinforced by images and audio clips are used to help health care providers educate their clients, and different counselling messages are displayed depending on the results of the sputum examination. For example, if the sputum result is positive, messages such as ‘strict adherence to treatment for complete cure’ and ‘DOT cures you’ appear; if the sputum result is negative, then the message ‘If symptoms persist, report again to concerned medical officer’ appears. General messages that display regardless of the result of sputum examination focus on themes such as ‘shared air, safe air’ and ‘cough hygiene’.
FIGURE 1.
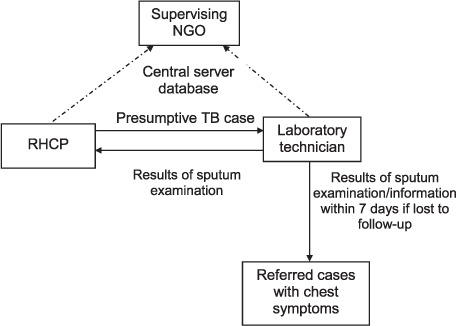
Data flow among mHealth care providers. NGO = non-governmental organisation; RHCP = rural health care provider; TB = tuberculosis.
Training on the use of the mobile application was provided by project staff using handouts and Powerpoint presentations (Microsoft, Redmond, WA, USA) and by demonstrating the steps involved. Training content mainly included steps to be followed to install the application and the processes involved in referring presumptive TB cases. Training lasted for 3–4 h, and practitioners took 15–60 min to familiarise themselves with the application. A unique ID was generated for each patient when the RHCP entered the patient details into the mobile application, and all results sent to the RHCP were linked to the unique ID. As case data were not available to any person other than the programme manager, patient confidentiality was maintained. Cases were informed about the mobile-based referral mechanism, and verbal consent was obtained before referral.
Project supervisors monitored the overall implementation of the project. For the purpose of the study, those RHCPs who had installed the mobile application and were trained in mobile use were termed ‘mRHCPs’, while the other RHCPs were termed ‘oRHCPs’.
RESULTS
In the project area, 171 RHCPs were formally trained by the RNTCP, 30 of whom were also trained in the use of the mobile intervention. The sociodemographic characteristics of the mRHCPs involved were as follows: 1) all were male, with a mean age of 39 years; 2) the average distance of the microscopy centre from the health provider was 11 km; and 3) the providers' qualifications were not health-related: educational qualifications ranged from secondary school completed, pre-university, graduate to post-graduate; 4) the average experience in providing full-time health care services among RHCPs was 11 years (range 6–35 years); 5) the average number of patients seen by RHCPs per day was 12 (range 5–30); and 6) only 50% of the providers had any knowledge about using a mobile application.
During the study period, there were 1578 referrals (Figure 2), 1056 of which came from the mRHCPs (i.e., 35 referrals per RHCP) and 522 were referred by oRHCPs (4 referrals per RHCP). Of the total 194 TB cases diagnosed, the number of mRHCP referrals was 127 (4 TB cases per RHCP), while oRHCPs contributed 67 (0.5 TB cases per RHCP). The number of TB patients diagnosed on day 1 (day of referral) was 158/194 (82%); 99/194 (51%) were referred by mRHCPs (3.3/mRHCP and 0.4/oRHCP). All 194 cases diagnosed were started on treatment. The number of diagnosed TB patients started on treatment on day 1 was 80/194 (41%); 48/80 (60%) were referred by mRHCPs (1.6/mRHCP and 0.2/oRHCP). The remaining patients were started on treatment within 7 days of diagnosis. The number of patients who received DOT from RHCPs was 99: 60 from mRHCPs (2/mRHCP) and 39 from oRHCPs (0.3/oRHCP).
FIGURE 2.
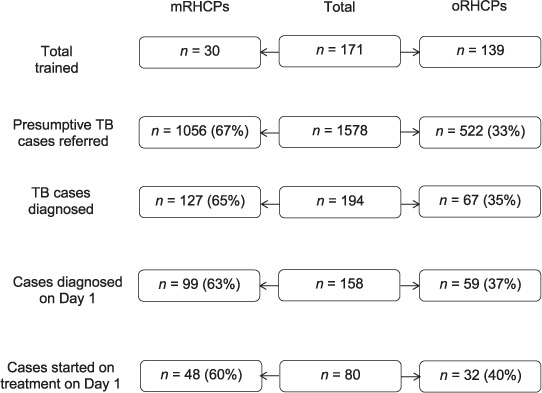
Flow diagram showing the results of referred and diagnosed TB cases among mRHCPs and oRHCPs. mRHCP = rural health care providers trained in mobile use; oRHCP = other rural health care providers; TB = tuberculosis.
DISCUSSION
This is one of the few mHealth projects conducted in India using information technology-enabled mobiles to help RCHPs refer presumptive TB cases for diagnosis and treatment initiation. Our experience suggests that this intervention was effective, it enhanced the number of referrals and it reduced the time taken for diagnosis and treatment initiation. Through this mechanism, providers were informed about referrals in real time, and this enhanced their enthusiasm for further engagement with the programme. Although other studies have described the use of mobile services for better treatment outcomes, literature on the use of mobile technology for TB referral services and treatment initiation in India is scarce.15,16
The findings of the intervention have the following programmatic implications. First, RHCPs using mobile technology referred nearly nine times more presumptive TB cases than other RHCPs. This underlines the fact that there are large numbers of presumptive TB cases in the community who are not evaluated due to the lack of proper mechanisms. RHCPs have so far remained untapped by the RNTCP, and there is huge potential in systematically engaging them in mHealth. Second, the activity and effectiveness of the health care system are greatly enhanced through the technology; diagnosis and treatment initiation via the application were 8–9 times more rapid than the time taken by oRHCP referrals. This integrated approach of including private and public health care providers along with patients on a single mobile platform synergised the delivery of health care services. This improved the quality of programme implementation, which can be measured by the programme process indicators such as the reduction in dropouts among referred patients, timely dissemination of sputum results to patients and providers and early treatment initiation. Third, educational materials used to raise awareness among presumptive TB cases and the guidance tool used to direct the patient's next steps indirectly helped the community in the early identification of presumptive TB cases and the prompt initiation of appropriate treatment. The mRHCPs were highly motivated and were more likely to become DOT providers for the patients (2 TB patients per mRHCP) than other RHCPs (0.3 TB patients per oRHCP).
A study limitation is the possible bias in selecting only those RHCPs who volunteered, and who could use android phones and applications; also, not all RHCPs who possessed android mobile phones volunteered. Although there was a steep learning curve for those who volunteered for mobile usage, they were proficient in using the application immediately after training.
To conclude, mHealth use among RHCPs was highly effective and increased the accountability of both public and private health care providers to patients. The programme can become more effective by involving RHCPs, and innovative mHealth use has the potential for replication across the country.
Acknowledgments
The project was undertaken by the International Union Against Tuberculosis and Lung Disease, New Delhi, India, with support from Lilly MDR-TB Partnership, Geneva, Switzerland.
Footnotes
Conflicts of interest: none declared.
References
- 1. Källander K, Tibenderana J K, Akpogheneta O J, . et al. Mobile health (mHealth) approaches and lessons for increased performance and retention of community health workers in low- and middle-income countries: a review. J Med Internet Res 2013; 15: e17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. World Health Organization. . mHealth: New horizons for health through mobile technologies. Geneva, Switzerland: WHO, 2011. [Google Scholar]
- 3. Nasi G, Cucciniello M, Guerrazzi C.. The role of mobile technologies in health care processes: the case of cancer supportive care. J Med Internet Res 2015; 17: e26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. World Health Organization. . Global tuberculosis report, 2015. WHO/HTM/TB/2015.22 Geneva, Switzerland: WHO, 2015. [Google Scholar]
- 5. Satyanarayana S, Nair S A, Chadha S S, . et al. From where are tuberculosis patients accessing treatment in India? Results from a cross-sectional community based survey of 30 districts. PLOS ONE 2011; 6: e24160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Central TB Division, Government of India. . Revised schemes for NGOs and private providers. New Delhi, India: Revised National TB Control Programme, 2009. [Google Scholar]
- 7. Central TB Division, Government of India. . National guideline for partnership. New Delhi, India: Ministry of Health and Family Welfare, 2014. http://www.tbcindia.nic.in/showfile.php?lid=3143 Accessed April 2017. [Google Scholar]
- 8. Samal J. Health seeking behaviour among tuberculosis patients in India: a systematic review. J Clin Diagn Res 2016; 10: LE01– LE06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Patel V, Parikh R, Nandraj S, . et al. Assuring health coverage for all in India. Lancet 2015; 386: 2422– 2435. [DOI] [PubMed] [Google Scholar]
- 10. May C, Roth K, Panda P.. Non-degree allopathic practitioners as first contact points for acute illness episodes: insights from a qualitative study in rural northern India. BMC Health Serv Res 2014; 14: 182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Bansal S. WHO report sounds alarm on ‘doctors’ in India. The Hindu, 18 July 2016. Chennai, India: http://www.thehindu.com/data/WHO-report-sounds-alarm-on-%E2%80%98doctors%E2%80%99-in-India/article14495884.ece Accessed April 2017. [Google Scholar]
- 12. Sharma N C. Grim picture of doctor-patient ratio, 1 doctor for 2,000 people. Mail Today News. India Today, 29 April 2016. http://indiatoday.intoday.in/story/grim-picture-of-doctor-patient-ratio/1/654589.html Accessed April 2017. [Google Scholar]
- 13. International Union Against Tuberculosis and Lung Disease. . Eli Lilly and The Union collaborate to launch mobile application for TB referrals. 23 May 2013. Paris, France: International Union Against Tuberculosis and Lung Disease, 2015. http://old.theunion.org/index.php/en/what-we-do/tuberculosis/tb-news/item/2461-eli-lilly-and-the-union-collaborate-to-launch-mobile-application-for-tb-referrals Accessed April 2017. [Google Scholar]
- 14. Ministry of Tribal Affairs, Government of India. . Report of the high level committee on socioeconomic, health and educational status of tribal communities of India. New Delhi, India: Ministry of Tribal Affairs, 2014. http://www.indiaenvironmentportal.org.in/files/file/TribalCommitteeReport,May-June2014.pdf Accessed April 2017. [Google Scholar]
- 15. Elangovan R, Arulchelvan S.. A Study on the role of mobile phone communication in tuberculosis DOTS treatment. Indian J Community Med 2013; 38: 229– 233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Iribarren S J, Schnall R, Stone P W, Carballo-Diéguez A.. Smartphone applications to support tuberculosis prevention and treatment: review and evaluation. JMIR Mhealth Uhealth 2016; 4: e25. [DOI] [PMC free article] [PubMed] [Google Scholar]


