Abstract
Purpose
To assess the relationship between corneal thinning measured by clinician-graded slit lamp exam compared to ultrasound pachymetry (USP), anterior segment optical coherence tomography (AS-OCT), and Pentacam.
Methods
Patients with corneal thinning underwent USP, AS-OCT, Pentacam measurements as well as standardized clinical grading by two cornea specialists estimating thinning on slit lamp examination. Reproducibility of each testing modality was assessed using the Intraclass Correlation Coefficient (ICC). Bland-Altman plots were used to determine precision and limits of agreement (LOA) between imaging modalities and clinical grading.
Results
We included 22 patients with corneal thinning secondary to infectious or inflammatory keratitis. Mean percent stromal thinning estimated by grader 1 was 51% (SD 31) and grader 2 was 49% (SD 33). ICC between the masked examiners was 0.95 (95% CI 0.88 to 0.98). Graders were more similar to each other than to any other modality with 2% difference and 4.55% of measurements outside the LOA. When measuring the area of maximal thinning, AS-OCT measured approximately 10% thicker than human graders while Pentacam measured approximately 10% thinner than human graders with 16.67% outside the LOA. USP measured approximately 20% thinner than human graders with 5.56% outside the LOA.
Conclusions
Trained corneal specialists have a high degree of agreement in location and degree of corneal thinning when measured in a standardized fashion on the same day. Other testing modalities had acceptable reproducibility and agreement with clinical examination and each other, although Scheimpflug imaging fared worse for corneal thinning, particularly in the periphery, than the other modalities.
Introduction
Corneal thinning occurs in a number of conditions including infectious and inflammatory disorders. Ophthalmologists have been using thickness (CCT) measured by ultrasonic pachymetry (USP) for many years to monitor progression of endothelial disease, plan for refractive surgery and in patients with healthy corneas being followed for glaucoma. Clinicians generally rely on estimating a certain percentage of corneal thinning as documented on slit lamp examination to guide the clinical management of corneal melts or thinning in infectious ulcers over time. Recent advances in technology have led to an increased number of devices available to measure corneal thickness with an interest in using these technologies clinically to measure disease activity and additionally as potential outcomes in clinical trials.
Multiple studies have shown relatively good agreement between USP, Pentacam, and anterior segment optical coherence tomography (AS-OCT) in normal eyes.1–3 Fewer studies are available comparing these technologies in eyes with corneal pathology, and those that do exist focus predominantly on patients with keratoconus or those who have undergone refractive surgery.4,5 The purpose of this study is to determine the reproducibility and agreement of slit lamp examination, USP, AS-OCT and Pentacam in the evaluation of patients with pathological corneal thinning.
Materials and Methods
After obtaining Institutional Review Board approval at the University of California, San Francisco, the medical records of all patients seen in the cornea clinic between January 1, 2015 and November 1, 2015 were reviewed. Patients with corneal thinning documented in any part of the progress note were asked to return for a one-time clinical examination by two cornea specialists as well as imaging including USP, AS-OCT, and Pentacam. Informed consent was obtained for all study participants.
Clinical Exam
Two cornea specialists served as independent examiners (JR and JK) who remained masked to each others grading as well as measurements on USP, AS-OCT and Pentacam. A calibrated slitlamp biomicroscope (BM 900; Haag-Streit, Koeniz, Switzerland) was used to examine each study participant, scoring the corneal thinning in terms of location, area and percent thinning to the nearest 5%. Location of maximal thinning was recorded by noting the clock hour and millimeters from the limbus. The total area of thinning was assessed by measuring the longest dimension and the longest perpendicular to the first measurement, a protocol adapted from the Herpetic Eye Disease Study.6 Percent thinning was determined by comparison to the corresponding mirror image in the normal fellow eye, or by comparison to an “ideal cornea” if no normal cornea was available for comparison.
Ultrasound Pachymetry
Ultrasound pachymetry measurements were performed by one of the examiners in triplicate using a handheld pachymeter (Pachmate; DGH technology, Inc., San Diego, CA, USA). The cornea was first anesthetized with one drop of proparacaine hydrochloride 0.5% (Alcaine; Alcon Labs, Fort Worth, Texas, USA). For each measurement, twenty-five sequential measurements were obtained and averaged. Values with standard deviation (SD) of 5 μm or less were considered suitable for inclusion. Central corneal thickness measurements were obtained with the probe tip at the center of the cornea and the probe perpendicular to the surface of the cornea. Measurements of the area of maximal thinning were performed using the same technique at the location deemed thinnest by each of the examiners. Clinician gradings were reviewed by a third party, and if there was discrepancy in the location of maximal thinning between examiners, USP measurements were obtained at both locations.
AS-OCT
AS-OCT images were obtained using a Heidelberg Spectralis with an anterior segment module (Heidelberg Engineering, Heidelberg, Germany). An initial large scan was performed centered over the pupil. Subsequently, a dense scan over the thinnest area (as determined by examining the initial scan) was performed using line scans 3 mm in length with 0.125 mm spacing with an automatic real time (ART) setting of 9 frames. Quantitative data were obtained using the caliper function by 3 masked examiners.
Pentacam
Scheimpflug images were obtained using Pentacam (Oculus, Wetzlar, Germany) with the manufacturer’s software set to 50 images over 2 seconds. Measurements were taken in a dark room with all lights turned off except for the Pentacam computer monitor. The patient was seated with chin on the chinrest and forehead against the forehead strap and asked to fixate on a target. The operator visualized a real-time image of the patient’s eye and manually focused and aligned the image. Automatic release mode was used, therefore the instrument determined when correct focus and alignment had been achieved and performed the scan. All measurements were performed in triplicate and taken by a single observer blinded to the results of the clinical examination. Topographic variables recorded by the Pentacam used for analysis included CCT and thickness at area of maximal thinning, which is automatically calculated and annotated by the instrument.
Statistical Analysis
Reproducibility of each measurement was assessed using the intraclass correlation coefficient (ICC). Separate ICCs were estimated between the two clinical observers, as well as after repeated measurements of the USP, AS-OCT and Pentacam. Measurements were converted to percent for USP, AS-OCT and Pentacam by calculating the percent of thinning compared with the mirror image in the fellow eye. Agreement between examiners and devices was determined using Bland-Altman plots to determine precision, bias and limits of agreement (LOA). Absolute differences were used to compare modalities. A p-value less than 0.05 was considered statistically significant. Calculations were performed using Stata 13.0.
Results
Of the 48 patients identified with corneal thinning on chart review, 22 (11 men and 11 women) were available for grading. Corneal thinning was secondary to infectious keratitis in 6 (27%), herpetic interstitial keratitis in 4 (18%), peripheral ulcerative keratitis in 4 (18%), neurotrophic keratitis in 4 (18%), radiation in 2 (9%), trauma in 1 (4.5%) and Fuchs marginal keratitis in 1 (4.5%). Thinning was unilateral in 17 (77%) and bilateral in 5 (23%). Age range was 9–84 years with mean ± standard deviation of 55 ± 22 years.
Table 1 outlines the reproducibility of each testing modality as measured by the ICC including standardized slit lamp examination (between masked examiners), USP, AS-OCT and Pentacam. Mean percent stromal thinning as estimated by grader 1 was 51% (SD 31) and grader 2 was 49% (SD 33) and ICC between the two masked examiners was 0.95 (95% CI 0.88 to 0.98). Mean percentage of total corneal thinning, including epithelium estimated by grader 1 was 47% (SD 33) and grader 2 was 45% (SD 33) and ICC between the two graders was 0.92 (95% CI 0.82 to 0.97). The mean distance from the limbus of maximal thinning for grader 1 was 3.4 mm (SD 1.3) and for grader 2 was 3.3 mm (SD 1.6). ICC was 0.85 (95% CI 0.67 to 0.94) for exact clock hour of the thinning and 0.85 (95% CI 0.80 to 0.97) for location of maximal thinning from the corneal limbus in millimeters.
Table 1.
Reproducibility of Testing Modalities using the Intraclass Correlation Coefficient
| Testing Modality | ICC | 95% CI |
|---|---|---|
| Slit Lamp Examination | ||
| Stromal thinning (%) | 0.95 | 0.88 to 0.98 |
| Total thinning (%) | 0.92 | 0.82 to 0.97 |
| Maximal thinning clock hour | 0.85 | 0.67 to 0.94 |
| Maximal thinning distance (mm) | 0.85 | 0.80 to 0.97 |
| Ultrasonic Pachymetry | ||
| Central Pachymetry (μm) | 0.87 | 0.76 to 0.94 |
| Total thickness* (μm) | 0.93 | 0.87 to 0.97 |
| AS-OCT | ||
| Maximal thinning clock hour | 0.43 | 0.17 to 0.68 |
| Maximal thinning distance (mm) | 0.71 | 0.52 to 0.86 |
| Total thickness* (μm) | 0.95 | 0.89 to 0.98 |
| Pentacam | ||
| Central Pachymetry (μm) | 0.75 | 0.56 to 0.88 |
| Total thickness* (μm) | 0.87 | 0.74 to 0.95 |
Abbreviations: ICC, Intraclass Correlation Coefficient; 95% CI, 95% Confidence Intervals; mm, millimeters; AS-OCT, Anterior Segment Optical Coherence Tomography.
Total corneal thickness in area of maximal cornea thinning in microns.
The other testing modalities all demonstrated excellent reproducibility for measurement of stromal thinning as well. ICC of USP when measuring CCT repeated three times was 0.87 (95% CI 0.76 to 0.94), and was 0.93 (95% CI 0.87 to 0.97) when repeated three times in the area of maximal corneal thinning. Reproducibility of AS-OCT for identifying the maximal stromal thinning as identified by three independent masked graders using the caliper function was 0.95 (95% CI 0.89 to 0.98). Identifying the distance from the limbus and clock hour of the maximal area of thinning on AS-OCT was less reliable demonstrating an ICC of 0.71 (95% CI 0.52 to 0.86) and 0.43 (95% CI 0.17 to 0.68) respectively. Pentacam had an ICC of 0.87 (95% CI 0.74 to 0.95) when identifying the maximal corneal thinning in microns. This was somewhat dependent on whether the pathology was central (ICC 0.89, 95% CI 63 to 99) versus peripheral (ICC 0.86, 95% CI 67 to 96). ICC of Scheimflug imaging with Pentacam demonstrated an ICC of 0.75 (95% CI 0.56 to 0.88) in the central cornea, although this improved significantly when study participants with central corneal thinning were excluded to 0.90 (95% CI 0.77 to 0.96). Additionally the ICC of Pentacam in the central cornea in the fellow eye was improved at 0.93 (95% CI 0.86 to 0.97) but improved further to 0.98 (95% CI 0.95 to 0.99) if the patient did not have bilateral corneal pathology.
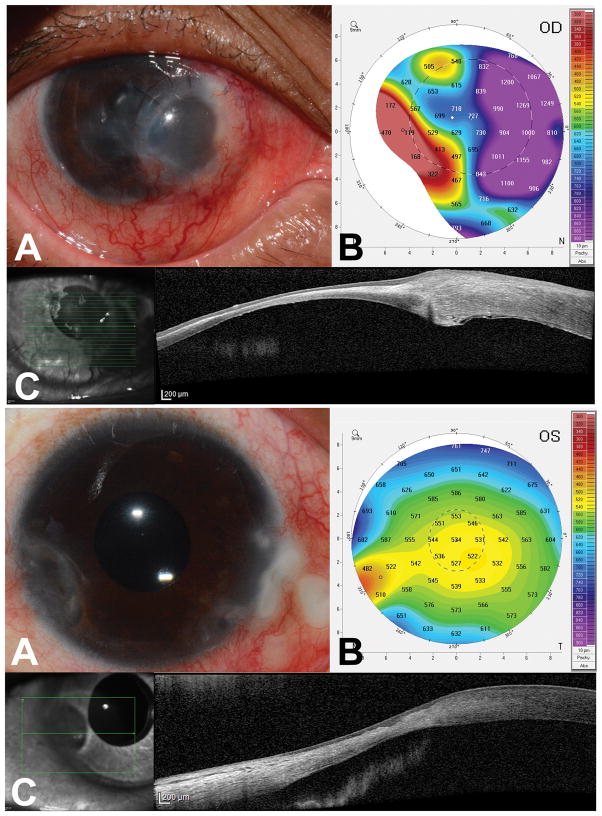
The area of greatest total corneal thinning was identified on each testing modality. USP gave a mean maximal thinning measurement of 426 μm (SD 136 μm), AS-OCT of 393 μm (SD 182 μm), and Pentacam of 385 μm (SD 124 μm). When a masked grader identified the area of maximal thinning on AS-OCT, it corresponded to the area of maximal thinning as identified by slit lamp examination 52% of the time. The area of maximal thinning identified by Pentacam software corresponding to the area of maximal thinning as identified by slit lamp exam 27% of the time. Representative images from two patients are show in Figure 1.
Figure 1. Examples of different diagnostic modalities and clinical photographs.
Anterior segment photographs (A), Pentacam pachymetry maps (B) and anterior segment optical coherence tomography scans (C, AS-OCT) for two patients with corneal thinning. Patient 1 (above) was a 38 year old woman with a history of peripheral ulcerative keratitis. Both physicians identified the area of maximal thinning 1–1.5 mm from the limbus at 8 o’clock which corresponded to Pentacam and AS-OCT. Patient 2 (below) was a 52 year old man with a history of rheumatoid arthritis related corneal thinning which led to perforation a nasal tectonic graft 11 months prior to the study. Both physicians identified the area of maximal thinning 4–4.5 mm from the limbus at 8 o’clock which did not correspond to Pentacam or AS-OCT.
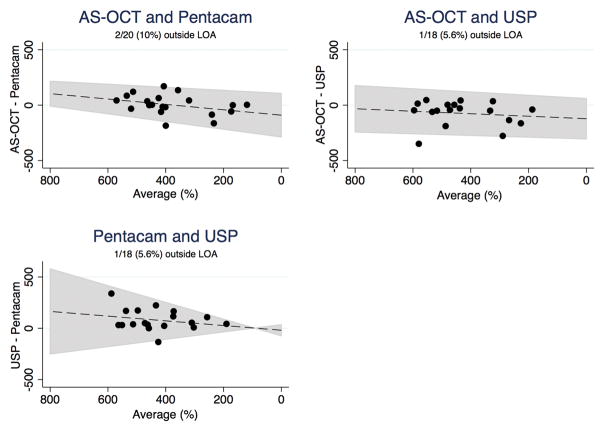
Bland-Altman plots were used to compare maximal corneal thinning identified on each of the imaging modalities to mean clinical examiner (Figure 2). Table 2 compares the percent difference of each of the imaging modalities to mean clinical examiner using the limits of agreement (LOA) and the Pitman test of difference. The two graders were more similar to each other than to any other modality with about 2% difference (mean difference −1.77, SE −6.35 to 2.81) and only 4.55% of measurements outside of the LOA. AS-OCT was the testing modality most similar to the mean examiner grade, on average measuring about 10% thicker than human graders (−9.6, SE −18.66 to −0.54). There was a statistically significant trend where AS-OCT measured thicker than human graders when there was less than 20% thinning (P = 0.008). By contrast, Pentacam and USP measured on average thinner than human graders. Pentacam measured about 10% thinner than human graders with 16.67% outside the LOA (mean difference 10.35, SE −3.63 to 24.32) while USP measured a little over 20% thinner on average with 5.56% outside the LOA (mean difference 21.83, SE 5.44 to 30.82).
Figure 2. Comparison of different diagnostic modalities to clinical examiners with Bland-Altman plots.
Comparing Agreement in percent maximal corneal thinning between: examiners, anterior segment optical coherence tomography scans (AS-OCT) and mean Examiners, mean examiner and Pentacam, mean examiner and ultrasound pachymetry (USP).
Table 2.
Comparison of Agreement with Diagnostic Modalities Compared with Slit Lamp Examination
| Testing Modality | Mean Difference, % (SE) | Limits of Agreement | % Outside LOA | P value* |
|---|---|---|---|---|
| Examiners | −1.77 (−6.35 to 2.81) | −22.44 to 18.89 | 4.55 | 0.31 |
| AS-OCT | −9.60 (−18.66 to −0.54) | −50.47 to 31.27 | 13.64 | 0.008 |
| Pentacam | 10.35 (−3.63 to 24.32) | −45.85 to 66.54 | 16.67 | 0.12 |
| USP | 21.83 (5.44 to 30.82) | −38.93 to 82.49 | 5.56 | 0.07 |
Paired comparisons of % corneal thinning as measured by two masked graders with slit lamp examination, and mean grade by slit lamp compared with AS-OCT, Pentacam and USP. Abbreviations: SE, Standard Error of the measurement; LOA, Limits of Agreement; AS-OCT, Anterior Segment Optical Coherence Tomography; USP, Ultrasonic Pachymetry
Pitman’s test of difference in variance
Bland-Altman plots were also used to compare imaging modalities to each other (Figure 3). USP pachymetry measured overall thicker than the other modalities, measuring 76 μm (SE −128 to −24) greater than AS-OCT on average and 98 μm (SE 35 to 160) greater than Pentacam on average. Pentacam and AS-OCT were the most similar to each other, with a mean difference of 16 μm (SE −34 to 67) and 4.76% outside the LOA. There was a statistically significant trend with AS-OCT measuring greater than Pentacam when there was less thinning (P = 0.01). Table 3 outlines the mean difference measured in microns, the LOA and Pitman test of difference for each of these comparisons.
Figure 3. Comparison of different diagnostic modalities with Bland-Altman plots.
Comparing agreement of maximal corneal thinning in microns between: Pentacam and anterior segment optical coherence tomography scans (AS-OCT), AS-OCT and ultrasound pachymetry (USP), Pentacam and USP.
Table 3.
Comparison of Agreement Between Diagnostic Modalities
| Testing Modality | Mean Difference, μm (SE) | Limits of Agreement | % Outside LOA | P value* |
|---|---|---|---|---|
| AS-OCT - Pentacam | 16.37 (−34.41 to 67.14) | −206.72 to 239.45 | 4.76 | 0.01 |
| AS-OCT - USP | −76.42 (−128.45 to −24.40) | −292.27 to 139.42 | 5.26 | 0.88 |
| USP - Pentacam | 97.77 (35.08 to 160.46) | −162.37 to 357.91 | 5.26 | 0.18 |
Paired comparisons of remaining microns of cornea in area of maximal corneal thinning for AS-OCT, Pentacam, and USP. Abbreviations: SE, Standard Error of the measurement; LOA, Limits of Agreement; AS-OCT, Anterior Segment Optical Coherence Tomography; USP, Ultrasonic Pachymetry
Pitman’s test of difference in variance
Discussion
In this study we found that the reproducibility of estimates of corneal thinning measured by standardized slit lamp examination, AS-OCT, USP and Pentacam were all excellent, although slit lamp examination and AS-OCT had the highest ICC. The majority of previous diagnostic studies have compared measurements in normal corneas. The reproducibility and accuracy of these devices in corneal pathology is highly clinically relevant. One of the challenges in this type of comparison is the lack of a gold standard for measuring corneal thickness since it is unclear which modality most accurately reflects true corneal thickness. The Bland-Altman plot displays the mean difference between testing modalities (y axis) plotted against the average measurement (x axis). When there is a lack of gold standard, this is the preferred method of comparison, as the average measurement of the two modalities is more likely to represent the actual corneal thickness.7
Ultrasonic pachymetry (USP) relies on the density and compressibility of the cornea to measure the amount of time needed for an ultrasound pulse to pass from the transducer through the corneal structures and back to the transducer.8 Measurement of non-central corneal thickness with USP has previously been demonstrated in normal corneas.9 In patients with keratoconus or previous laser in situ keratomileusis (LASIK), both Pentacam and AS-OCT measurements were reproducible but always thinner than USP.5 We also found USP to be highly repeatable, both in the central cornea and in the area of maximal thinning. In our study, as in previous reports, USP graded the area of maximal corneal thinning thicker than human graders, AS-OCT and Pentacam.
Anterior segment optical coherence tomography uses infrared light and interferometrically detects backscattered reflections returning from ocular structures to produce real-time images.10 This offers the advantage of high-resolution cross-sectional imaging of the cornea as well as regional pachymetry made more precise by the point-to-point correlation between real time images and AS-OCT scans. Prior studies in normal corneas have found the reproducibility of Pentacam to be comparable to AS-OCT.11 When comparing CCT in normal corneas, variable results have been reported, some finding lower values in USP compared to AS-OCT, and others reporting higher.3,12 We found a high degree of agreement between AS-OCT and mean examiner grade as well as AS-OCT and Pentacam. There was a trend for AS-OCT to measure thicker than Pentacam and mean human grader, particularly in corneas with less thinning.
The Pentacam uses a rotating Scheimpflug camera to take optical cross-sections of the anterior segment. The rotating camera captures up to 50 slit images, while eye movements are captured and corrected by a second camera. Single-point pachymetric measurements are calculated from the front and back surfaces using ray tracing.2 In addition to providing pachymetric data, the Pentacam also provides corneal topography and 3D anterior chamber analysis. Given the center of rotation, measurements of CCT are thought to be reliable, particularly in normal corneas.13 Good correlation has been reported between Pentacam and USP in normal corneas.1,14 A study comparing Pentacam to USP in patients with keratoconus found that measurements of CCT with Pentacam were more repeatable than those obtained with USP.4 We found that Pentacam performed best in CCT measurements in normal corneas. When the corneal thinning was peripheral, Pentacam performed particularly poorly. It may be that the central rotation may not be conducive to documenting peripheral corneal pathology, and this may explain its lower reproducibility in our series.
One limitation of our study is the fact that it is cross-sectional. We were surprised that measurements of the masked ophthalmologists were so close to each other. Rounding of clinical measurements of thinning to the nearest 5% might have slightly increased the likelihood of intra-grader agreement than if a more rigid linear scale was used. It may be that imaging would be more reproducible than standardized slit lamp examination over time. A longitudinal study looking at standardized slit lamp examination as well as the other testing modalities would be interesting. Additionally, there was a difference in determining the point of maximal thinning (manually for ultrasound and AS-OCT and automatically for Pentacam), which could represent a limitation.
Pathologic corneal thinning requires close monitoring for progression to identify patients who would benefit from an increase in therapy. It is also important to identify reliable outcome measures for clinical trials. We found that trained corneal specialists have a high degree of agreement in location and degree of corneal thinning when examining patients in a standardized manner on the same day. Considering a clinically acceptable difference of 10% or less in measurement of corneal thinning, the other testing modalities also had acceptable reproducibility and agreement with clinical examination and each other, although Scheimpflug photography fared worse for corneal thinning, particularly in the corneal periphery, than the other modalities.
Acknowledgments
Financial Support: Research to Prevent Blindness, National Institutes of Health Grant k23025025
Footnotes
Conflict of Interest: No conflicting relationship exists for any author.
References
- 1.Al-Mezaine HS, Al-Amro SA, Kangave D, et al. Comparison between central corneal thickness measurements by oculus pentacam and ultrasonic pachymetry. Int Ophthalmol. 2008;28:333–338. doi: 10.1007/s10792-007-9143-9. [DOI] [PubMed] [Google Scholar]
- 2.Barkana Y, Gerber Y, Elbaz U, et al. Central corneal thickness measurement with the Pentacam Scheimpflug system, optical low-coherence reflectometry pachymeter, and ultrasound pachymetry. J Cataract Refract Surg. 2005;31:1729–1735. doi: 10.1016/j.jcrs.2005.03.058. [DOI] [PubMed] [Google Scholar]
- 3.Kim HY, Budenz DL, Lee PS, et al. Comparison of central corneal thickness using anterior segment optical coherence tomography vs ultrasound pachymetry. Am J Ophthalmol. 2008;145:228–232. doi: 10.1016/j.ajo.2007.09.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.de Sanctis U, Missolungi A, Mutani B, et al. Reproducibility and repeatability of central corneal thickness measurement in keratoconus using the rotating Scheimpflug camera and ultrasound pachymetry. Am J Ophthalmol. 2007;144:712–718. doi: 10.1016/j.ajo.2007.07.021. [DOI] [PubMed] [Google Scholar]
- 5.Prospero Ponce CM, Rocha KM, Smith SD, et al. Central and peripheral corneal thickness measured with optical coherence tomography, Scheimpflug imaging, and ultrasound pachymetry in normal, keratoconus-suspect, and post-laser in situ keratomileusis eyes. J Cataract Refract Surg. 2009;35:1055–1062. doi: 10.1016/j.jcrs.2009.01.022. [DOI] [PubMed] [Google Scholar]
- 6.Wilhelmus KR, Gee L, Hauck WW, et al. Herpetic Eye Disease Study. A controlled trial of topical corticosteroids for herpes simplex stromal keratitis. Ophthalmology. 1994;101:1883–1895. doi: 10.1016/s0161-6420(94)31087-6. [DOI] [PubMed] [Google Scholar]
- 7.Bland JM, Altman DG. Comparing methods of measurement: why plotting difference against standard method is misleading. Lancet. 1995;346:1085–1087. doi: 10.1016/s0140-6736(95)91748-9. [DOI] [PubMed] [Google Scholar]
- 8.Silverman RH. High-resolution ultrasound imaging of the eye - a review. Clin Experiment Ophthalmol. 2009;37:54–67. doi: 10.1111/j.1442-9071.2008.01892.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.González-Méijome JM, Cerviño A, Yebra-Pimentel E, et al. Central and peripheral corneal thickness measurement with Orbscan II and topographical ultrasound pachymetry. J Cataract Refract Surg. 2003;29:125–132. doi: 10.1016/s0886-3350(02)01815-1. [DOI] [PubMed] [Google Scholar]
- 10.Nolan W. Anterior segment imaging: ultrasound biomicroscopy and anterior segment optical coherence tomography. Curr Opin Ophthalmol. 2008;19:115–121. doi: 10.1097/ICU.0b013e3282f40bba. [DOI] [PubMed] [Google Scholar]
- 11.Chen S, Huang J, Wen D, et al. Measurement of central corneal thickness by high-resolution Scheimpflug imaging, Fourier-domain optical coherence tomography and ultrasound pachymetry. Acta Ophthalmol. 2012;90:449–455. doi: 10.1111/j.1755-3768.2010.01947.x. [DOI] [PubMed] [Google Scholar]
- 12.Leung DY, Lam DK, Yeung BY, et al. Comparison between central corneal thickness measurements by ultrasound pachymetry and optical coherence tomography. Clin Experiment Ophthalmol. 2006;34:751–754. doi: 10.1111/j.1442-9071.2006.01343.x. [DOI] [PubMed] [Google Scholar]
- 13.Rozema JJ, Wouters K, Mathysen DG, et al. Overview of the repeatability, reproducibility, and agreement of the biometry values provided by various ophthalmic devices. Am J Ophthalmol. 2014;158:1111–1120. e1111. doi: 10.1016/j.ajo.2014.08.014. [DOI] [PubMed] [Google Scholar]
- 14.O’Donnell C, Maldonado-Codina C. Agreement and repeatability of central thickness measurement in normal corneas using ultrasound pachymetry and the OCULUS Pentacam. Cornea. 2005;24:920–924. doi: 10.1097/01.ico.0000157422.01146.e9. [DOI] [PubMed] [Google Scholar]