Abstract
Objective
Caregivers usually are not involved while planning the stroke survivor’s medical and rehabilitation goals and interventions. This review aimed to identify the needs of stroke survivors as perceived by their caregivers.
Design
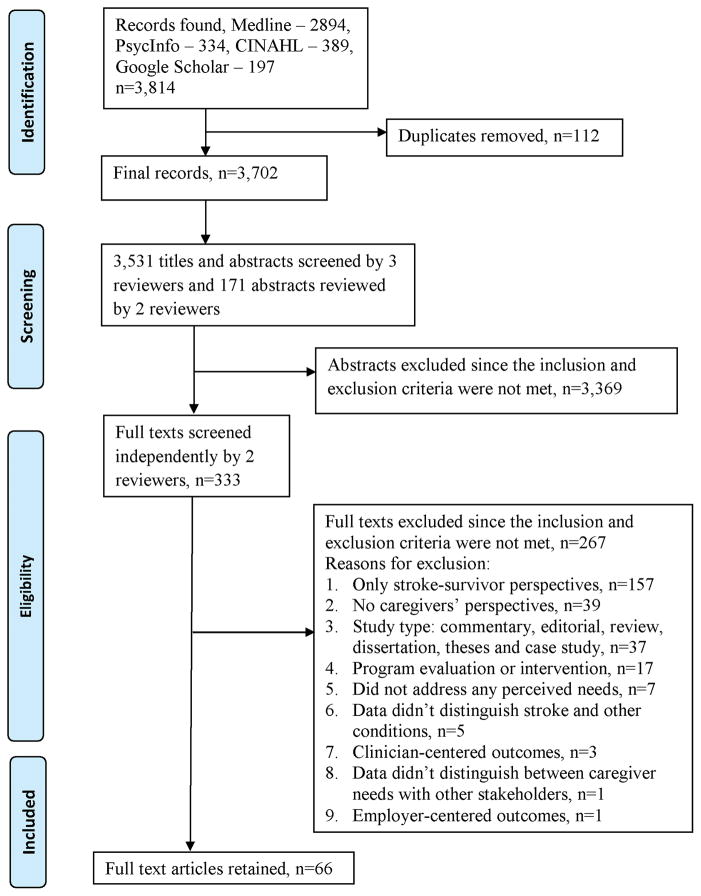
A literature search from 2003 until 2014 was conducted using Medline, CINAHL, PsychINFO and Google Scholar. Sixty-six studies were included. Most studies excluded did not encompass caregivers’ perspectives. Four reviewers screened the titles, abstracts, and full texts of the articles for inclusion. The data extracted from these studies were synthetized into meta-themes.
Results
Fifty-two qualitative, ten quantitative survey, and four mixed methods studies were included in the final synthesis. The studies came from eleven countries. The data synthesis produced three meta-themes: a) body functional needs, including psychological function, physical function, cognitive function, and uncertainty related to function; b) activity and participatory needs, including healthy lifestyle, physical activities, speech, independence, cognitive activities, and uncertainty related to activities and participation; and c) environmental needs, encompassing support, services, safety, accommodation and accessibility, and uncertainty related to environmental factors.
Conclusion
This scoping review identified a range of needs of stroke survivors as perceived by their caregivers. Incorporating the caregiver’s preference and values into clinical decisions may improve outcomes among stroke survivors.
Keywords: caregivers, rehabilitation, perspectives, patient-centered care, stroke, unmet needs
Introduction
Nearly 750,000 people are affected by new or recurrent stroke annually in the United States.1 These individuals often have complex needs that may include physical, cognitive, psychological emotional, and socioeconomic factors.2 Regardless of the severity of injury and age, most people experience diminished quality of life following the event, impacting their activities of daily living, relationship with their family members, and social lives.3
Informal caregivers help support and improve stroke survivors’ medical and rehabilitation outcomes. Approximately 3.5 million individuals with stroke receive care from others, including family, friends, and paid caregivers.4, 5 Among family members caring for individuals with stroke, spouses and children are often the primary caregivers.5 The sudden onset of stroke and consequential uncertainty increases caregiver burden and anxiety,6 as they undertake new roles and responsibilities not only for themselves but also for the stroke survivors.7 Mood and behavior changes in caregivers may affect the outcomes for stroke survivors.8 Considering the multidimensional recovery and rehabilitation process following stroke, it is essential to understand the needs and health care outcomes of stroke survivors as perceived by the caregivers and involve them in the decision making process.9
The Patient-Centered Outcomes Research Institute has identified the importance to inquire needs of stroke survivors as perceived by their caregivers, while making health care decisions 10 Thus recognizing, supporting, and involving the caregivers in the stroke survivors care can help improve survivors’ health outcomes. In addition, involving the caregivers enhances their experiences with health care, and also reduces the associated expenditures.11 Caregivers often provide a unique perspective as they are constantly involved in the stroke survivors’ care. For instance, a patient with a complicated health condition along with cognitive decline may be unable to participate fully in his care.12 Engaging caregivers in the decision-making process can supplement the patient-centered perspectives, which can further improve the appropriateness of prescribed clinical and rehabilitation interventions, and diagnostic tests.12
The needs of stroke survivors perceived by the caregivers are not usually included during the post-acute discharge planning,13 because of inadequate time, and availability of resources.14 The health care professionals (HCPs) must gauge a way to include the caregiver as a part of the care team. To address this issue, a scoping review was conducted to provide an overview of the needs of stroke survivors as perceived by their caregivers during the different phases post-stroke. A scoping review allows the presentation of the range of available evidence on a broad topic, or identifies the gaps in existing literature.15, 16 The purpose of this scoping review was to identify and synthetize the needs of stroke survivors as perceived by their caregivers by performing a secondary analyses of the studies included.
Methods
This study conforms to all PRISMA guidelines, and reports the required information accordingly (see Supplementary Checklist).
Search strategy
A medical librarian searched four electronic databases: Medline, CINAHL, PsycINFO, and Google Scholar from 2003 until 2014. The search included the following main keywords in various combinations: “stroke”, “survivors”, “cerebrovascular accident”, “convalescence”, “rehabilitation”, “psychology”, “post-stroke”, “ recovery”, “patient”, “caregiver”, “client”, “consumer”, “family”, “needs”, “hope”, “goals”, “goal attainment”, “objective”, “preferences”, “expectations”, “anticipation”, “attitudes”, “satisfaction”, “content”, “discontent”, “participation observation”, “decision making”, “shared decision making”, “participation”, “engagement”, “involvement”, “empowerment”, “perception”, “quality of life”, “aftercare”, “treatment outcomes”, “motivation”, “achievement”, “intention”, “drive”, “incentive”, “disincentive”, “discharge planning”, “attitude to health”, “psychology”, “recovery of function”, “outcome measures”, and “outcome assessment”. The reference lists were hand searched for relevant studies (See Search Strategy Supplemental Digital Content file).
Studies included were original peer-reviewed articles in English, addressing needs of stroke survivors throughout the survivors’ recovery process in all settings (acute, post-acute, or community) as perceived by the caregiver. The focus of this review was to explore needs of stroke survivors as perceived by the caregivers; hence, all studies included were those that explored this perspective. Studies excluded were those with only stroke survivors’ perspectives, did not distinguish caregivers’ perspectives from those of other stakeholders, did not distinguish stroke from other conditions, focused only on perspectives for a program/intervention evaluation. Although some studies included caregivers own needs or other stakeholders’ perspectives, the data extraction for this review only focused on the needs of stroke survivors perceived by their caregivers. Case studies, dissertation theses, editorials, reviews, and commentaries were also excluded.
Three reviewers independently screened the titles and abstracts (SK, MS, and AK) for inclusion. A fourth reviewer (TR) provided consensus in case of disagreement. Two reviewers (SK, MS) independently screened all full-text articles. The Kappa calculated for a subset of abstracts (n=171), and full text articles (n=50) was 0.74 and 0.73, respectively. Major subsets of full text articles (80%) were re-screened by an additional reviewer (AK) to ensure quality control.
Appraisal of selected studies
The quality of the included studies was evaluated using the Critical Appraisal Skills Programme (CASP)17 for qualitative studies, Critical Appraisal of a Survey by the Center for Evidence-Based Management (CEBMa)18 for surveys, and the Mixed Method Appraisal Tool (MMAT)19 for mixed-methods studies. Two reviewers (SK and MS) independently evaluated the quality of each article. Appraisal agreement between reviewers for a subset of the retained studies (n=39) was measured with Kappa: CASP=0.63, CEBMa =0.76, and MMAT=0.52. The low Kappa score for MMAT was a result of only four studies with mixed methods being included in the review. Disagreements were resolved through discussion with the additional reviewer (TR). Studies were not excluded based on quality, as the characteristics required to report the quality of research are not consistent.20
Data extraction
Characteristics of selected studies such as demographics including age and gender of caregivers, sample size, purpose of the study, setting and time point, and methodology were extracted by one reviewer (SK) and checked for accuracy by two reviewers (MS and TR). A codebook defining the themes and subthemes was created using NVivo.a Subthemes to discover caregivers’ perspectives emerging from the results of the full-text articles were identified using an inductive approach with line-by-line coding.21 To identify the themes, a balance between emic and etic approaches was sought.22 Two coders (SK and MS) read all articles independently, and sorted quotations from each article into relevant themes and subthemes. Techniques used to identify the themes included repetition, indigenous typologies, similarities and differences, and systematically comparing across the data extracted from different studies.21 At the early stages of analysis, all possible themes were identified; the consolidation of themes was done later. Consensus on each independently identified theme or subtheme was achieved through discussion. In case of disagreement, TR resolved differences via discussion. To ensure quality control, an additional reviewer (MP) independently re-coded the themes of family support and uncertainty. Kappa for these two themes was 0.60. In addition, the quotations under all themes and subthemes were reviewed by MP to ensure quality control. Having multiple coders maximized the likelihood of identifying all possible themes and minimized any bias during theme identification.21 The themes and subthemes were refined by grouping the related topics by SK and MP. During this process, some themes and subthemes were merged, separated, or relabeled.
Results
The search strategy is shown in Figure 1. The 66 included full texts involved a combination of 1,926 caregivers along with other stakeholders such as stroke survivors, health care professionals (HCPs), and managers. Out of the 66 full texts included in the final review, 39 studies focused only on the caregivers’ perspectives, 23 studies focused on the perspectives of both stroke survivors and caregivers, two studies included the perspectives of caregivers and HCPs, and two studies identified the perspectives of stroke survivors, caregivers, and HCPs. Table 1 summarizes characteristics of the 66 articles. Fifty-two were qualitative, 4, 7, 9, 23–71 ten utilized a survey, 72–81 and four used a mixed methods approach.82–85 Most of the studies (n=45, 68%) were conducted in the community.
Figure 1.
Screening process of selected studies
Table 1.
Summary and characteristics of studies included in the review (n=66)
| Author | Purpose | Sample size | Caregiver characteristics | Setting and time point | Methodology | Data Collection |
|---|---|---|---|---|---|---|
| Backstrom, 2007 – Sweden70 | Illuminate meanings in the lived experience of being a middle-aged close relative of a person who has suffered a stroke 1 month after discharge from a medical rehabilitation clinic | 10 Caregivers | Age: 56 (40–64) Gender: F=8 Relationship: Partner=7, mother=2, other=1 |
Setting: Home/Community Time point: 20w post stroke (12–33w), 1m post discharge from rehabilitation clinic |
Phenomenology - hermeneutic | Interviews |
| Backstrom, 2009 – Sweden24 | Illuminate the experience of being a middle-aged close relative of a person with stroke; 1 year post-discharge | 9 Caregivers | Age: Median 55 (41–65) Gender: F=7 Relationship: Partner=7, parent =2 |
Setting: Home/Community Time after stroke: 1m and 6m post- discharge |
Latent CA | Narrative interviews |
| Backstrom, 2010 – Sweden23 | Illuminate the meanings of middle-aged female spouses’ lived experience of their relationship with a partner with stroke, during the first year post-discharge | 4 Caregivers | Age:52 (40–58) Gender: F=4 Relationship: Partner =4 |
Setting: Home/Community Time point: 1m, 6m and 12m post- discharge from rehab clinic |
Phenomenology- hermeneutic | Open-ended narrative interviews |
| Boter, 2004 – The Netherlands 72 | Describe the number and types of problems mentioned by home-dwelling stroke patients and their carers, and nursing interventions applied | 118 Caregivers 166 SSs Total=284 |
Age: 57 Gender: F=69 Relationship: Spouse/partner=88 |
Setting: Home/Community Time point: 1–4w, 4–8w, 10–14w, 18–24w post-discharge |
Cochran’s Q and Friedman test | Survey – telephone, home visit |
| Brittain, 2007 – UK25 | Explore the notion of the bounded body and dirty work in light of the role of informal carers looking after someone with incontinence | 20 Caregivers | Age: 51–86 Gender: F=13 Relationship: Partner, children |
Setting: Home/Community Time point: NR |
Constant comparative, deviant case analysis | Structured interview |
| Brown, 2011 – NR26 | Explore perspectives of family members of individuals with aphasia, the meaning of living successfully with aphasia | 24 Caregivers | Age: 62 (40–87) Gender: F=15 Relationship: Partner=19, children=1, parent=3, sibling=1 |
Setting: Home/Community Time point: ≥2y post-stroke |
Interpretative phenomenology | Semi structured interviews |
| Cameron, 2013 – Canada27 | Support needs over time from the perspective of caregivers, perspective of HCPs, compare and contrast caregivers’ and HCPs’ perspectives | 24 Caregivers 14 HCPs Total=38 |
Age: 66 (36–77) Gender: F=17 Relationship: Spouse=18, children=6 |
Setting: Rehabilitation, Home/Community Time point: 1m-11y post-stroke |
FW | Structured, in-person, telephone interviews |
| Cecil, 2013 – UK28 | Caring and coping among carers of stroke survivors and identify factors that had an impact on their lives | 30 Caregivers | Age: 36–84 Gender: F=23 Relationship: Spouse=19, children=7, sibling=3, other=1 |
Setting: Home/Community Time point: 6w post-discharge |
NR | Semi-structured interviews |
| Chang, 2013 – Taiwan29 | Examine the institutional contexts that contribute to the low priority given to the development of self-care independence in a rehabilitation ward | 12 Caregivers 15 HCPs Total=27 |
Age: NR Gender: NR Relationship: NR |
Setting: Rehabilitation Time point: NR |
Ethnography | Participant observation, interviews |
| Chow, 2014 – Hong Kong30 | Experiences of family caregivers in caring for community-dwelling strokes survivors, services that help or do not help the caregivers in managing their role | 29 Caregivers | Age: 42–87 Gender: F=21 Relationship: Spouse=17, children=12 |
Setting: Home/Community Time point: 1- >6 y post-stroke |
CA | FG |
| Cobley, 2013 – UK31 | Patients’ and carers’ experiences of Early Supported Discharge (ESD) services and inform future ESD service development and provision | 15 Caregivers 27 SSs Total=42 |
Age: 73 Gender: F=13 Relationship: Spouse=15 |
Setting: Home/Community Time after stroke: 14 d post-stroke |
TA | Semi-structured interviews |
| Coombs, 2007 – Canada71 | Examine the experiences of spousal caregivers for stroke survivors | 8 Caregivers | Age: 66 (57–81) Gender: F=8 Relationship: Partner=8 |
Setting: Home/Community Time point: 1y post-stroke |
Phenomenology | Semi-structured interviews |
| Danzl, 2013 – USA32 | Experience of stroke for survivors and their caregivers | 12 Caregivers 13 SSs Total=25 |
Age: 56 (38–75) Gender: F=7 Relationship: Spouse=6, children=6 |
Setting: Hospital, Rehabilitation, Home/Community Time point: 1–14y post-stroke |
CA | Semi-structured interviews |
| Dietz, 2013 – USA33 | Social role changes experienced by PWA, understand communication strategies to reclaim previous social roles, and determine discrepancies between PWA and their potential proxies regarding social role changes | 6 Caregivers 3 SSs Total=9 |
Age: 56 (39–88) Gender: F= 4 Relationship: Spouse=3, parent =1, children=1, other=1 |
Setting: Home/Community Time point: 2–15y post-stroke |
Phenomenology | Semi-structured interviews |
| Eames, 2010, – Australia34 | Identify patients’ and carers’ perceived barriers to accessing and understanding information about stroke | 18 Caregivers 34 SSs Total=52 |
Age: 60 (26–77) Gender: F=13 Relationship: Spouse=17, other=1 |
Setting: Hospital, Home/Community Time point: 1w prior discharge, 3m post-discharge |
CA | Semi-structured interviews |
| Egbert, 2006 – USA35 | Communicative processes by which social support to assist right-hemisphere stroke survivors in the process of community integration | 13 Caregivers 12 SSs Total=25 |
Age: 60 Gender: F=11 Relationship: NR |
Setting: Home/Community Time point: 6m post discharge |
GT | Open ended interviews |
| El Masry, 2013 – Australia36 | Psychosocial experiences and needs of caregivers | 20 Caregivers 10 SSs Total=30 |
Age: 56 (31–90) Gender: F=16 Relationship: Spouse=15, children=2, sibling=3 |
Setting: Hospital, Rehabilitation Time point: >3m post-stroke |
Interpretative phenomenology | Semi-structured interviews |
| Ellis-Hill, 2009 – NR37 | Understanding on what constitutes a ‘good’ or ‘poor’ experience in relation to the transition from hospital to home following a stroke | 13 Caregivers 20 SS Total=32 |
Age: NR Gender: NR Relationship: Spouse=10, children=3 |
Setting: Home/Community Time point: Up to 3y post-stroke at 2w post-acute care discharge |
FA | Semi-structured interviews |
| Garrett, 2005 – NR38 | Information needs of patients and carers at different intervals post stroke | NR Caregivers NR SSs Total=16 |
Age: NR Gender: NR Relationship: NR |
Setting: Hospital, Rehabilitation, Home/Community Time point: NR |
Modified GT | Open ended interviews |
| Gosman, 2012 – Sweden39 | Older women experiences of life situation and formal support as carers of their partners after stroke | 16 Caregivers | Age: Median 74 (67–83) Gender: F=16 Relationship: Partner=16 |
Setting: Home/Community Time point: NR |
NR | FG |
| Grant, 2004 – USA7 | Problems and associated feelings experienced by family caregivers of stroke survivors during the 1st month after returning home | 22 Caregivers | Age: 42–70 Gender: F=21 Relationship: Spouses = 9, daughter = 9 |
Setting: Home/Community Time point: 1m post-discharge |
CA | Telephonic interviews |
| Grant, 2006 – USA40 | Problems and associated feelings experienced by family caregivers of stroke survivors during the 2nd and 3rd month after discharge from rehabilitation facility to home | 22 Caregivers | Age: 56 Gender: F=21 Relationship: Spouse=9, children=9, others=4 |
Setting: Home/Community Time point: 1w post-discharge |
CA | Telephonic interviews |
| Green, 2009 – Canada9 | Explore male patients with minor stroke and their wife-caregivers’ perceptions of factors affecting quality of life and caregiver strain encountered during the first year post-discharge | 26 Caregivers 26 SSs Total=52 |
Age: Mean 59 (33–75) Gender: F=26 Relationship: Spouse=26 |
Setting: Home/Community Time point: >12m post-stroke at 1,2,3,6,9, and 12m post-discharge |
CA | Semi-structured, telephone interviews |
| Greenwood, 2010 – UK41 | Investigate the experiences of informal carers of stroke survivors from discharge to 3 months later | 31 Caregivers | Age: 40–65 Gender: F=22 Relationship: Spouse=16, children=13, other=2 |
Setting: Hospital, Rehabilitation, Home/Community Time point: before discharge, 1m, and 3m post-discharge |
Ethnography | Open-ended interviews |
| Greenwood, 2009 – UK42 | Investigate the experiences of informal carers of stroke survivors over time | 31 Caregivers | Age: >65 y =23, <65y = 8 Gender: F = 22 Relationship: Spouse=16, children=13, other=2 |
Setting: Rehabilitation, Home/Community Time point: close to discharge, 1m and 3m post-discharge |
Ethnography | Open-ended interviews |
| Gustafsson, 2013 – Australia43 | Enhance understanding of the transition experience for clients with stroke and their carers during discharge and the first month at home | 5 Caregivers 5 SSs Total=10 |
Age: 57 (37 - 51) Gender: F=3 Relationship: Spouse=3, children=1, other:1 |
Setting: Home/Community Time point: 1m post-discharge from rehab |
Inductive TA | Semi-structured interview |
| Haley, 2009 – USA81 | Prevalence and stressfulness of stroke-related problems, perceived benefits of caregiving |
75 Caregivers | Age: 64 Gender: F=59 Relationship: Spouse=40, children=23 |
Setting: Home/Community Time point: 8–12 m post-stroke |
Descriptive | Survey |
| Hallé, 2014 – Canada44 | Understand significant others’ experience of aphasia rehabilitation | 12 Caregivers | Age: 58 (43–70) Gender: F=9 Relationship: Spouse=7, parents=2, other=3 |
Setting: Home/Community Time point: 3–36m post-stroke |
GT | Interviews |
| Hare, 2006 – UK45 | Long-term support needs of patients with prevalent stroke, and their carers | 6 Caregivers 27 SSs Total=33 |
Age: NR Gender: F=6 Relationship: NR |
Setting: Rehabilitation, Home/Community Time point: 6w-22y post-stroke |
NR | FG |
| Hinojosa, 2007 – USA and Puerto Rico76 | Information sources and needs of stroke caregivers | 120 Caregivers | Age:62 Gender: F=111 Relationship: Spouse/Partner=88, children=8, parents=5, other=19 |
Setting: Home/Community Time point: NR |
t-tests and chi-square tests | Survey |
| Hinojosa, 2009 – USA and Puerto Rico79 | Association between health education needs and physical injury sustained as a result of activities related to the caregiving role | 276 Caregivers | Age: Mean 66 (18–88) Gender: F=251 Relationship: NR |
Setting: Home/Community Time point: NR |
Descriptive, chi-square | Telephone survey |
| Howe, 2012 – Australia46 | Rehabilitation goals that family members of individuals with aphasia have for themselves | 48 Caregivers | Age: 61 (24–83) Gender: F=36 Relationship: Partner=28, children=7, parents=2, other=11 |
Setting: Home/Community Time point: 1–195m post-stroke |
CP, CA | Semi-structured interviews |
| Jullamate, 2007 – Thailand47 | Identify the reasons for the provision of informal rehabilitation services at home to stroke relatives by Thai caregivers. | 20 Caregivers | Age: 53 (28–79) Gender: F=15 Relationship: Spouse=9, children=8, other=3 |
Setting: Home/Community Time point: post-discharge from hospital |
CA | Semi-structured interviews |
| Kim, 2007 – South Korea 80 | needs of family members across rehabilitation treatment phases and treatment settings | 123 Caregivers | Age: <20 – 70 Gender: F=75 Relationship: Spouse=66, children =42, sibling=3, parent=6, other=6 |
Setting: Hospital, Rehabilitation Time point: NR |
t-test, one-way ANOVA | Surveys – in person and mail |
| Kniepman, 2014 – USA84 | Impact caregivers’ activities, and identify differences as per race/ethnicity through the lens of occupation | 12 Caregivers | Age: 62 (37–73) Gender: F=10 Relationship: Spouse = 12 |
Setting: Home/Community Time point: at least 6m post-stroke |
Quantitative: non-parametric Qualitative: Inductive CA | Quantitative: questionnaires Qualitative: Semi-structured interviews |
| Kong,2011 – Hong Kong73 | Investigate provision of speech-language pathology services and community resources for persons with aphasia and their families, family members’ perception of the service quality | 37 Caregivers | Age: NR Gender: NR Relationship: Spouse=30, Children=7 |
Setting: Home/Community Time point: 4–71m post-discharge from hospital |
Descriptive | Self-administered questionnaire |
| Lawrence, 2010 – UK48 | Explore the beliefs and perceptions of patients and family members regarding the provision of lifestyle information following stroke | 20 Caregivers 29 SSs 7 PWA Total=49 |
Age: Median 64 (42–79) Gender: F=9 Relationship: Family members |
Setting: Home/Community Time point:>6m post-stroke |
FW | Focus groups using semi-structured topic guide |
| Lawrence, 2013 – UK49 | Explore the experience of stroke from the perspective of family members of young adults with stroke | 12 Caregivers | Age: 17–71 Gender: F=9 Relationship: Spouse=4, children =4, parents=3, other = 1 |
Setting: Home/Community Time point: 3m-2y post-stroke |
Phenomenology Merleau-Ponty’s | Unstructured face-to-face interviews |
| Lee, 2011 – Hong Kong50 | Explore the coping strategies of Chinese family caregivers of stroke-impaired older relatives | 15 Caregivers | Age: 25–80+ Gender: F=10 Relationship: Spouse=12, children=3 |
Setting: Home/Community Time point: NR |
GT | Interviews |
| Lin, 2010 – USA51 | Needs of family caregivers in the Chinese-American community and to develop training videos for caregivers on dressing stroke survivors | 40 Caregivers | Age: 51–87 Gender: F=35 Relationship: Spouse=24, Parent=12, Friend=4 |
Setting: Home/Community Time point: 1m post-discharge |
NR | Semi-structured interviews |
| Lutz,2007 – USA52 | Identify postdischarge needs of veterans with stroke and their caregivers and design care coordination/home-telehealth program to address these needs |
10 Caregivers 12 SSs Total=22 |
Age: 70 (57–86) Gender: F=10 Relationship: Spouse/Partner n=10 |
Setting: Home/community Time point: 3m-5y post-stroke |
GT with dimensional analysis | Open-ended, unstructured interviews |
| Lutz, 2011 – USA4 | Explore the needs of stroke patients and their family caregivers as they transitioned through the stroke care continuum from acute care to inpatient rehabilitation to home | 19 Caregivers 19 SSs Total=38 |
Age: 58 (23–82) Gender: NR Relationship: Spouse=14, Children=4, Parent=1 |
Setting: Home/Community, Rehabilitation Time point: at rehab, 4d-6w post-discharge, within 6m post-discharge |
GT – dimensional, comparative analysis | Loosely structured interviews |
| Lynch, 2008 – USA53 | Perspectives on post-stroke QoL |
6 Caregivers 9 SSs Total=15 |
Age: 57 Gender: F=5 Relationship: Spouses=4, Parent=1 |
Setting: Home/Community Time point: 2–29y post-stroke |
NR | FG |
| MacIsaac, 2011 – Canada82 | Explore the use of the Supportive Care Needs Framework as an overall guide to identify the wide spectrum of needs of the family caregivers of patients with stroke |
10 Caregivers | Age: 55.7 (40–72) Gender: F=10 Relationship: Spouse=5, children=5 |
Setting: Hospital Time point: NR |
Quantitative: Descriptive Qualitative: NR | Survey and focus groups |
| Mackenzie, 2007 – UK78 | Support required by family carers for stroke survivors | 42 Caregivers | Age: 62 (28–84) Gender: F=29 Relationship: Spouse/Partner =29, children=10, parents=2, other=1 |
Setting: Hospital, Home/Community Time point: 1w before discharge and 4–6w post-discharge |
Descriptive | Survey |
| Mackenzie, 2013 – UK83 | Feedback of participants in the Living with Dysarthria programme, to inform its perceived usefulness and guide future development | 4 Caregivers 9 PWD Total=13 |
Age: NR Gender: F=4 Relationship: Spouse=3, other=1 |
Setting: Hospital Time point: 3–72m post-stroke |
Quantitative: Descriptive Qualitative: TA | Written questionnaire and focus group |
| Mak, 2007 – Hong Kong77 | Changing needs of Chinese family caregivers before and after stroke survivors’ discharge from hospital | 40 Caregivers | Age: 49 (28 – 70) Gender: F=30 Relationship: Spouse=16, children=21, other=3 |
Setting: Hospital, Home/Community Time point: 2w before discharge and 2w post-discharge from hospital |
Descriptive, Pearson’s correlation | Scale |
| McCarthy, 2015 – USA85 | Perspectives on survivor cognitive and physical functioning and incongruence between partners’ perceptions affecting spouse depressive symptoms and overall mental health |
35 Caregivers 35 SSs Total=70 |
Age: Mean 58 (22–86) Gender: F=20 Relationship: Spouse=35 |
Setting: Home/community Time point: 1–36m post-stroke |
Quantitative: paired t-tests Qualitative: interpretive | Structured interview, survey |
| Morris, 2014 – UK54 | Survivors’, carers’ and physiotherapists’ beliefs about physical activity (PA) to identify how these support or hinder PA participation | 12 Caregivers 38 SSs 15 Clinicians Total=75 |
Age: 41–80+ Gender: F=6 Relationship: Spouse=12 |
Setting: Home/Community Time point: 6m post rehab |
FA | FG |
| Obe-om, 2006 – Thailand55 | Experiences of families with long-term stroke survivors, and families to manage care of the patients and their families | 32 Caregivers | Age: 19–83 Gender: NR Relationship: Children=13 |
Setting: Home/Community Time point: >1y post-stroke |
Ethnography | Participant observation and interview |
| O’Connell, 2003 – Australia57 | Caregivers’ perspectives of their support and educational needs | 28 Caregivers | Age: 55(23–74) Gender: F=16 Relationship: Spouse=18 |
Setting: Hospital, Home/Community Time point: NR |
NR | Face-to-face or telephone interviews |
| O’Connell, 2004 – Australia56 | Perspectives on the support and educational needs they require and the coping strategies | 37 Caregivers | Age:56 (23–86) Gender: F=23 Relationship: Partner=21, children=13, other=3 |
Setting: Hospital, Rehabilitation, Home/Community Time point: NR |
NR | Semi-structured interviews |
| Payne, 2010 – UK58 | Patients’ and family members’ experiences of acute stroke and their preferences for end-of-life care | 25 Caregivers 28 SSs Total=53 |
Age: NR Gender: NR Relationship: Spouse=45% |
Setting: Hospital Time point: Hospital stay 1–49 d |
NR | Semi-structured interviews |
| Perry,2011 – Australia74 | Advance understanding of stroke caregiving using assessment methods and tools previously used | 32 Caregivers | Age: 59 Gender: F=18 Relationship: Spouse=24, Children=7, Parent=1 |
Setting: Home/Community Time after stroke: NR |
Descriptive | Survey via telephonic interviews |
| Pierce, 2012 – USA69 |
Perceived dimensions of emotional strain expressed by new family caregivers of persons with stroke in the first year of caring |
73 Caregivers | Age: 55 Gender: F=55 Relationship: Partner=50, children=14, other=9 |
Setting: Home/Community Time point: NR |
CA | Email, telephonic interviews |
| Ringsberg, 2003 – Sweden59 | Stroke patients’ and their relatives’ conceptions of home rehabilitation, participation in the decision about home rehabilitation, participation in rehabilitation and experiences with rehabilitation team | 13 Caregivers 15 SSs Total=28 |
Age: 67 Gender: F=10 Relationship: NR |
Setting: Home/Community Time point: 1y post-discharge from stroke unit |
Phenomenography | FG semi-structured interviews |
| Rochette, 2014 – Canada60 | Ethical issues regarding the systematic inclusion of relatives as clients in the post-stroke rehabilitation process |
25 Caregivers 16 SSs Total=41 |
Age: 53 (31–72) Gender: F=21 Relationship: Spouse=8, children=10, parents=1, other=6 |
Setting: Hospital, Rehabilitation Time point: 4–6 w post-discharge |
Phenomenology | Semi-structured interviews and FG |
| Rosenberg, 2009 – Thailand61 | Informal rehabilitation caregiving provided to elderly stroke survivors | 20 Caregivers | Age: 74 Gender: F=15 Relationship: NR |
Setting: Home/Community Time point: post-discharged from hospital |
CA | Semi-structured interviews |
| Rudman, 2006 – NR62 | Occupational experiences of stroke survivors who use wheelchairs and their primary caregivers | 15 Caregivers 16 SSs Total=31 |
Age:68 (44–84) Gender: F=13 Relationship: Relative, formal care=2 |
Setting: Home/Community Time point: wheelchair use for at least 1y |
GT | Semi-structured interview |
| Saban,2012 – USA63 | Experience of female caregivers who care for an adult family member who has experienced a stroke | 46 Caregivers | Age: 56 (18–73) Gender: F=46 Relationship: Partner =24, children=18, parent=2, other=2 |
Setting: Home/Community Time point: 3–12m post-stroke |
CA | Open ended interviews |
| Sangvatanakul, 2010 – Australia75 | Engage consumers in research priority-setting using a quantitative approach and to determine consumer views on stroke research priorities for clinical practice | 6 Caregivers 12 SSs Total=18 |
Age: NR Gender: NR Relationship: NR |
Setting: Home/Community Time point: NR |
Descriptive | Survey |
| Smith, 2008 – Canada64 | Family caregivers’ experiences and support needs during the rehabilitation phase to inform program development | 9 Caregivers | Age: 57 (37–77) Gender: F= 6 Relationship: Spouse=6, children=2, other=1 |
Setting: Rehabilitation Time point: NR |
CA | Semi-structured interviews |
| Tellier, 2011 – Canada65 | Explore the QoL of spouses after a mild stroke | 8 Caregivers | Age: Mean 57 (45–69) Gender: F=6 Relationship: Spouses=8 |
Setting: NR Time point: 3m post-acute care discharge |
CP | Open-ended interviews |
| Van Dongen, 2014 – Austria66 | Working carers’ occupational experiences and strategies during a period of pronounced life changes | 3 Caregivers | Age: Mean 56 (49–59) Gender: F=3 Relationship: Wife=2, daughter=1 |
Setting: Home/Community Time point: NR |
Interpretative Phenomenology | Semi-structured interview |
| Vincent, 2007 – Canada67 | Met and unmet rehabilitation needs of older adults who had suffered a stroke | 12 Caregivers 17 SSs 25 HCPs 18 HCMs Total=72 |
Age: 41–69 Gender: F=9 Relationship: Spouse=10, daughter=2 |
Setting: Home/Community Time point: < 1 – 9+ y post-stroke |
NR | FG, individual interviews |
| Winkler, 2014 – USA and UK68 | Explore how carers of PWA perceive their roles and responsibilities; examine consequences of carrying out carer roles and duties, in terms of both the carer’s own well-being and their relationship with PWA; investigate facilitative factors in their adaptation to the carer role | 10 Caregivers | Age: NR Gender: F=9 Relationship: Spouse=6, children=3, parents=1 |
Setting: NR Time point: 7y post-stroke |
FW | Blogs |
Age is reported in years as mean and range unless noted otherwise, SS: Stroke survivors, HCP: health care professionals, PWA: Persons with aphasia, PWD: Persons with dysarthria, HCM: health care managers, GT: grounded theory, FW: framework, CA: content analysis, TA: thematic analysis, CP: Constructivist paradigm, FG: focus groups, y:years, m:months, w:weeks, NR: not reported
Appraisal of selected studies
Of the 52 qualitative studies appraised using CASP, all had a clear statement of the research aim, appropriately used qualitative methodology, presented clear findings, and mentioned the value of their study. Almost all studies reported the data collection process. Thirty studies provided the rationale for their research design,9, 11, 23, 25–27, 29, 31–33, 35, 39, 41, 42, 44–50, 52–54, 58, 62, 65, 66, 70, 71 nine discussed the relationship between researcher and participants,29, 42, 44, 46, 50, 54, 66, 70, 71 37 reported rigorous data analyses procedures,4, 7, 9, 11, 24, 26–28, 30–37, 39, 41–46, 48–50, 52–54, 58, 60, 63, 65, 67–70 45 reported the ethical considerations,4, 7, 9, 23–25, 27–29, 31, 32, 34, 36–50, 52–60, 62–66, 68–71 and 49 reported the recruitment strategy.7, 9, 11, 23–25, 27–32, 34–63, 65–71 Of the 10 quantitative studies appraised using CEBMa, all clearly addressed the research question, methods, selection of participants, and had a sample representing the population. None of the studies assessed the sample size a priori or reported confidence intervals. Seven studies achieved a response rate above 60%, 72, 74–76, 78, 79, 81 six utilized reliable and valid measurements,74, 77–81 and seven assessed statistical significance.72, 74, 76–80 All mixed-methods studies appraised using MMAT used the methodology appropriately, used relevant sources to collect the qualitative and quantitative data, and had sample representing the population. Although the integration of qualitative and quantitative approaches was relevant for three studies, 82, 83, 85 none of the studies discussed the limitations of integrating qualitative and quantitative studies. For the qualitative section of MMAT, none of the studies mentioned the researchers’ influence with the participants or the transferability of findings. For the quantitative section of MMAT, three studies had a response rate above 60%,82, 84, 85 and two used valid and reliable instruments.84, 85
Data synthesis
The subthemes were aggregated under three meta-themes using the International Classification of Functioning, Disability and Health (ICF)86 model, specifically utilizing the ICF Core Sets of Stroke framework. 87 Table 2 reflects the body functional needs, where the caregivers mentioned only functional needs for the stroke survivor and did not mention any structural need. Table 3 reflects the activity and participatory needs, and Table 4 lists the environmental needs. The stroke survivor needs in each table are listed in the order of most common need reported by the caregivers in the literature. The stage of care for each need is listed in respective tables as well. Most of the stroke survivor needs were identified in the community, following discharge from acute care and rehabilitation. The subthemes under each meta-themes are listed below.
Table 2.
Body functional needs identified from the synthesis of 66 articles (n=41, 62%)
| n=26 (39%) 4 Hospital 2 Rehabilitation 23 Community 2 Not Reported |
Psychosocial function –
|
| n=15 (23%) 2 Hospital 1 Rehabilitation 13 Community 2 Not Reported |
Physical function
|
| n=10 (15%) 2 Hospital 1 Rehabilitation 9 Community |
Cognitive function24, 40, 77– |
| n=9 (14%) 3 Hospital 3 Rehabilitation 8 Community |
Uncertainty related to functional impairments9, 32, 35, 42, 56, 58, 63, 70, 74 – “I don’t know what to expect after the first day or two whether he will change or be the way he is right now...”42 |
Table 3.
Activity and Participatory needs identified from the synthesis of 66 articles (n=43, 65%)
| n= 26 (39%) 3 Hospital 3 Rehabilitation 22 Community 2 Not Reported |
Healthy lifestyle –
|
| n=15 (23%) 2 Hospital 1 Rehabilitation 20 Community |
Physical activities –
|
| n=15 (23%) 1 Hospital 1 Rehabilitation 13 Community 1 Not Reported |
Independence –
|
| n=11 (17%) 2 Hospital 1 Rehabilitation 9 Community 1 Not Reported |
Speech and ability to talk – |
| n=2 (3%) 2 Community |
Cognitive activities – decision making,49 judgment40– “you end up having to make all the decisions, and, Och! It is wearing! I mean I love him, I love him dearly but just occasionally you think, Just decide”49 |
| n=2 (3%) 1 Hospital 1 Rehabilitation 2 Community |
Uncertainty related to limitations in activities and participation 41, 49 – “Everything gets a little bit more complicated and new even going to see friends or people who want to come up to see her”41 |
Table 4.
Environmental needs identified from the synthesis of 66 articles (n=61, 92%)
| n=50 (76%) 14 Hospital 12 Rehabilitation 40 Community 2 Not Reported |
Support –
|
| n= 44 (67%) 12 Hospital 10 Rehabilitation 34 Community 2 Not Reported |
Services –
|
| n=17 (26%) 1 Hospital 2 Rehabilitation 16 Community |
Safety –
|
| n=14 (21%) 2 Hospital 1 Rehabilitation 13 Community 1 Not Reported |
Accessibility and Accommodation –
|
| n=11 (17%) 2 Hospital 9 Community 1 Not Reported |
Uncertainty related to environmental factors 9, 30, 34, 42, 50, 52, 57, 63, 65, 71, 84 – “ everything was very difficult when we first got him home”52 |
Body functional needs, Table 2
Caregivers in 41 studies (62%) revealed the need for body functional needs following stroke. The most common body functional needs included, psychosocial function (n=26, 39%), followed by physical function (n=15, 23%), cognitive function (n=10, 15%) and uncertainty related to functional impairments (n=9, 14%).
Under the psychosocial function subtheme, ten articles mentioned the need to improve the mood of the survivor, and nine studies heighted the changes in behavior including anger, agitation etc. Caregivers in seven studies highlighted the importance of dealing with depression. The need to motivate and encourage the stroke survivor was emphasized in ten studies. Under the physical function subtheme, six articles highlighted that the caregivers were concerned for the overall physical function, and caregiver in one study specified the need to improve limb function. Caregivers in six studies also identified the importance of managing pain and fatigue. In addition, two studies emphasized the need for visual and hearing function, and four studies revealed the need to improve the voice functions. Under the cognitive function subtheme, ten articles revealed the need to improve the stroke survivors’ cognitive function including, comprehension, memory, orientation, etc. Under the uncertainty related to functional impairments subtheme, caregivers in nine studies were uncertain of the stroke recovery process because of functional changes in the stroke survivor’s body.
Activity and participatory needs, Table 3
Caregivers in 43 studies (65%) highlighted the activity and participatory needs for stroke survivors. The most common activity and participatory need included, healthy lifestyle (n=26, 39%), followed by physical activities and independence (n=15, 23% each), speech (n=11, 17%), cognitive activities and uncertainty related to limitations in activity and participation (n=2, 3% each).
Under the healthy lifestyle subtheme, the caregivers in 11 studies valued stroke survivors’ social and leisure activities. Seven studies indicated the need to improve nutrition among stroke survivors. Caregivers were concerned with the overall health, including spiritual health of the stroke survivor in four studies and they highlighted the need to prevent future strokes in 13 studies. Under the physical activities subtheme, ten studies indicated the caregivers’ perspectives related to self-care needs. Caregivers wanted to improve the mobility of the stroke survivors, and wanted them to walk, transfer independently, improve their balance and posture, increase physical activity, and independently climb stairs. Under the speech subtheme, in 11 studies the caregivers highlighted the need for the stroke survivor to communicate, express, and speak efficiently. Under the independence subtheme, 11 articles identified the need for the stroke survivor to return to normalcy and pre-stroke activities. Most of the caregivers wanted to preserve the survivor’s autonomy, and wanted them to go back to work, and be able to drive. Under the cognitive activities subtheme, caregivers in two studies wanted to improve the stroke survivor’s decision making and judgement. In addition, caregivers in two studies expressed uncertainty to plan for the future because of the survivor’s limitations in activities.
Environmental needs, Table 4
In most of the studies (62 studies, 92% of the studies), the caregivers stressed the importance of some form of environmental need. The most common environmental needs included, support (n=50, 76%), followed by services (n=44, 67%), safety (n=17, 26%), accessibility and accommodation (n=14, 21%), and uncertainty related to environmental factors (n=11, 17%).
Under the support subtheme, 32 articles indicated a need for communication with HCPs, 27 studies highlighted the importance of support from family and friends. Nineteen studies indicated that the caregivers had difficulty paying for the survivors’ medical bills, rehabilitation services, and other household expenditures, and four studies highlighted the need for support groups. Some supportive needs would benefit both stroke survivors and caregivers, but in some of the original texts, it was not possible to distinguish between needs of survivors and caregivers. Under the services subtheme, 28 articles indicated the need for rehabilitation services. The details on specifics of rehabilitation needs is listed in Table 4. Twenty-nine studies revealed the need for information on various aspects for the stroke survivor. The specific information needs are listed in Table 4. Fourteen studies highlighted the importance of other supportive services including but not limited to having paid caregivers, meals etc. Under the safety subtheme, caregivers ensured survivors’ safety to prevent falls in 12 studies because of impaired cognition,40 restricted mobility,49 lack of sleep,4 inadequate support,4 etc. In nine studies, caregivers were worried about leaving the survivor alone, and in four studies the caregivers wanted to safely administer these medications to avoid any mistakes. Under the accessibility and accommodation subtheme, six studies highlighted the need for accessibility at public toilets, travel and transportation. In addition, six studies revealed the need for equipment and other assistive devices for stroke survivors such as wheelchairs, walking frames, and augmented or alternative communications; and four studies highlighted the need for home and vehicle accommodation. Under the uncertainty related to environmental factors subtheme, the caregivers in 11 studies were unable to anticipate the stroke survivor’s needs at home and community post-discharge.
Discussion
The current scoping review synthetizes the needs of stroke survivors as perceived by their caregivers. Researchers may have focused their inquiry only on a specific aspect of the recovery experience; hence, many may not have elicited all aspects of concern or their relative importance. Thus, the goal of this review was to provide a comprehensive listing of all needs mentioned, rather than attempting to interpret the relative importance of concerns. The synthesis revealed the outcome preferences under three meta-themes: body functional needs, activity and participatory needs, and environmental needs. The subthemes under these meta-themes align with the International Classification of Functioning, Disability and Health (ICF) model.86, 87 The overview of the needs of stroke survivors as perceived by their caregivers provides clinicians with a framework for involving the caregivers during various stages of care. It was not clear from most of the studies if the needs of stroke survivors perceived by the caregivers were met or not; however, based on the secondary analyses of the texts, these are continuing or incompletely met needs.
The environmental needs were the most common need for the stroke survivor. In addition, most of these stroke survivor needs were identified by their caregivers when the survivor was in the community following discharge from acute care or rehabilitation. It is therefore important to include the stroke survivors needs during initial stages of care itself. Individuals with unmet needs usually have decreased satisfaction with health care services.88 Lack of support from family and friends has been previously associated with poorer health outcomes including increased institutionalization among stroke survivors.89 Also, lack of information on the stroke recovery process is associated with increased anxiety, stress, fear, and uncertainty about the future.90 Around 47% of survivors fall at least once following stroke,91 hence; caregivers are unlikely to leave the survivors alone unless they are in a safe environment with adequate accomodations.92 Environmental barriers such as lack of accommodation, accessibility, need for assistive devices impacts safety of the stroke survivors to move independently.93
Clinical practice implications
An increased rate of post-stroke disability interferes with the individual’s ability to perform activities of daily living. Since older stroke survivors have higher levels of inactivity,94 caregivers in this review wished to improve stroke survivors’ independence under the activity and participatory needs theme. The caregivers were also concerned with stroke survivors’ speech. Stroke survivors with aphasia usually have difficulty interacting with their caregivers and their clinicians effectively, which puts them at risk of receiving inadequate health care.88 In addition to motor and sensory activities, the clinicians should encourage the survivors to participate in social and leisure activities. The caregivers also valued the importance of stroke survivors’ social and leisure activities under the activity and participatory needs theme, as the stroke survivors are at a higher risk of inactivity and feel isolated.94
The findings of this review suggest that the caregivers wished for increased support and services including under the environmental needs theme. Effective communication with the patients helps the health care professionals arrive at an accurate diagnosis, develop optimal treatment plans, and encourage participation in rehabilitation, which enhances patients’ and families’ satisfaction with overall care. In addition, lack of support from family and friends is known to be associated with poorer health outcomes among stroke survivors.89 Being involved in support groups and services, and having additional assistance from paid caregivers is known to reduce stroke survivors’ institutionalization.89 This additional support makes the caregivers return to their caregiving duties with enthusiasm.95 Health care professionals must educate the stroke survivors and their caregivers on the locally and regionally available community services. In addition, the provision of community-based services would help facilitate access to supportive services to address the long-term post-stroke needs of stroke survivors and their caregivers. The caregivers face increasing financial and economic burden post-stroke which may be due to the direct costs of medical expenditures, and the indirect costs of loss of productivity.96 Identifying cost-effective interventions tailored to the individual stroke survivor and his/her caregiver can be cost-effective and yield positive outcomes.
In this review under the service needs subtheme, the caregivers identified the importance of information and education focused on stroke survivors’ disease process, prognosis, interventions, and recovery. To maximize the stroke survivors’ rehabilitation process, the caregivers must be informed on the various aspects of recovery, the disease process, and prevention of secondary complications. Lack of education on the stroke recovery process is known to be associated with increased anxiety, stress, fear, and uncertainty about the future.90 Conversely, educating caregivers on the management of stroke improves health outcomes.89 Providing stroke education may be one way to eliminate caregivers’ feelings of uncertainty post-stroke. When communicating with stroke survivors and their families, clinicians should set realistic expectations and provide encouragement in working together on patient recovery. Maintaining a routine, and incorporating the caregivers’ preferences can enhance stroke survivors’ outcomes. The HCPs must educate the caregivers that the survivors’ future may not be predictable, and work with them as a team through the recovery process.
In this review under the environmental needs theme, the caregivers were concerned with stroke survivors’ safety and wanted to prevent falls, and administer medications appropriately. Caregivers were concerned with the stroke survivors’ medication administration, fearing the adverse consequences of improper administration.97 Engaging the caregivers during the stroke survivors’ recovery process, educating them on the intrinsic as well as the extrinsic factors related to falls, and the adverse side effects of medications can improve the survivors’ outcomes as their caregivers learn to manage these problems effectively.
The caregivers in this review also identified the importance of accessibility, accommodations, and assistive devices under the environmental needs subtheme. The increasing need for accommodation following deficits post-stroke includes a necessity for mobility devices such as canes, walkers, wheelchairs, and safety devices. The use of assistive devices, and appropriate accommodations are known to decrease caregiver burden and maximize the survivors’ independence.93 Most stroke survivors do not have adequate access to assistive devices and accommodations in spite of the associated benefits. The HCP’s must prescribe assistive technology when appropriate.
Future research directions
Although poorer health care outcomes have been associated with ethnic minorities, 98 none of the studies in this review compared the perspectives of caregivers from different racial/ethnic backgrounds; which future studies must accomplish. The outcome preferences differs among patients, caregivers, and clinicians and across rehabilitation settings;99 none of these studies compared the caregivers outcome preferences across post-acute settings. Information, rehabilitation, and heath care needs may vary at different time points of recovery; future studies must investigate the caregivers’ perceived needs by various type of stroke (ischemic, hemorrhagic, and transient ischemic attack) and across settings (acute hospitalization, inpatient rehabilitation, skilled nursing rehabilitation, and community). Future studies/reviews must also focus the physical and emotional needs of caregivers themselves.
This review has some limitations. First, the influence of culture on preferred outcomes (e.g., the expectations of caregivers from Asian countries) was not assessed. Many qualitative and mixed methods studies did not comply with the quality measurement tools. Since the goal of the study was to encompass all the caregivers’ perspectives of stroke survivors’ needs, studies were included regardless of quality or country of origin. The review included the perceived needs of caregivers found using four databases, and did not include gray literature. Most of the studies included in this review did not distinguish between unmet, partially met, and met needs. However, we can assume that since the caregivers mentioned the importance of these needs for the stroke survivor, they may not have been completely met during hospitalization or rehabilitation. In spite of these limitations, this review had several strengths. A multidisciplinary group including physical and occupational therapists, psychologist, and sociologist interpreted the results from the included studies. In addition, as this was an interpretative review rather than an integration of the results, the synthesis can be transferred to similar population and settings.
Conclusion
This scoping review provides an overview of the needs of stroke survivors as perceived by their caregivers. The caregivers’ perspectives of stroke survivors’ needs were summarized under three domains that included body functional needs, activity and participatory needs, and environmental needs. This review underscores the important role of caregivers in the care and outcomes of stroke survivors. The findings of this review indicate that the caregivers recognized various needs for the stroke survivors, which may or may not have been met throughout their various phases of recovery continuum. Stroke survivors’ needs as perceived by the caregivers must be included in rehabilitation along with the survivors’ and clinicians’ perspective to maximize their recovery by regaining independence.
Supplementary Material
Acknowledgments
Funding
Supported with funding from the National Institute of Health, NICHD (K01-H0055929); Agency for Health Care Research and Quality (R24 HS022134); National Institute on Disability and Rehabilitation Research (H133P110012); UTMB Institute for Translational Sciences support by an NIH Clinical & Translational Science Award (UL1RR029876); UTMB Claude D. Pepper Older Americans Independence Center NIH/NIA (P30 AG024832).
The authors would like to thank Ms. Janet Burk for her contributions for organizing and assisting with the literature review for this manuscript.
Footnotes
Conflicts of Interest
The authors declare that no conflicts exist in connection with this paper. Preliminary results were presented at the Academy Health Scientific Meeting, Minneapolis, Minnesota, June 2015; the Gerontological Society of America’s Annual Scientific Meeting in Orlando, Florida, November 2015; and the Topics of Patient Centered Outcomes Research, UTMB, Galveston TX, February 2016.
NVivo 10 for Windows, QSR International.
References
- 1.Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, et al. Heart disease and stroke statistics: a report from the American Heart Association. Circulation. 2015;131(4):e29–322. doi: 10.1161/CIR.0000000000000152. [DOI] [PubMed] [Google Scholar]
- 2.White CL, Barrientos R, Dunn K. Dimensions of Uncertainty After Stroke: Perspectives of the Stroke Survivor and Family Caregiver. J Neurosci Nurs. 2014;46(4):233–40. doi: 10.1097/JNN.0000000000000066. [DOI] [PubMed] [Google Scholar]
- 3.Divani AA, Majidi S, Barrett AM, Noorbaloochi S, Luft AR. Consequences of Stroke in Community-Dwelling Elderly The Health and Retirement Study, 1998 to 2008. Stroke. 2011;42(7):1821–5. doi: 10.1161/STROKEAHA.110.607630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lutz BJ, Ellen Young M, Cox KJ, Martz C, Rae Creasy K. The crisis of stroke: experiences of patients and their family caregivers. Top Stroke Rehabil. 2011;18(6):786–97. doi: 10.1310/tsr1806-786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Houser A, Gibson MJ, Redfoot DL. Trends in family caregiving and paid home care for older people with disabilities in the community: Data from the National Long-Term Care Survey. 2010 [Google Scholar]
- 6.Greenwood N, Mackenzie A. An exploratory study of anxiety in carers of stroke survivors. J Clin Nurs. 2010;19(13–14):2032–8. doi: 10.1111/j.1365-2702.2009.03163.x. [DOI] [PubMed] [Google Scholar]
- 7.Grant JS, Glandon GL, Elliott TR, Giger JN, Weaver M. Caregiving problems and feelings experienced by family caregivers of stroke survivors the first month after discharge. Int J Rehabil Res. 2004;27(2):105–11. doi: 10.1097/01.mrr.0000127639.47494.e3. [DOI] [PubMed] [Google Scholar]
- 8.Tooth L, Mckenna K, Barnett A, Prescott C, Murphy S. Caregiver burden, time spent caring and health status in the first 12 months following stroke. Brain Inj. 2005;19(12):963–74. doi: 10.1080/02699050500110785. [DOI] [PubMed] [Google Scholar]
- 9.Green TL, King KM. Experiences of male patients and wife-caregivers in the first year post-discharge following minor stroke: a descriptive qualitative study. Int J Nurs Stud. 2009;46(9):1194–200. doi: 10.1016/j.ijnurstu.2009.02.008. [DOI] [PubMed] [Google Scholar]
- 10.Patient-Centered Outcomes Research Institute. National Priorities for Research and Research Agenda. May, 2012. p. 9. [Google Scholar]
- 11.Smith M, Saunders R, Stuckhardt L, McGinnis JM. Best care at lower cost: the path to continuously learning health care in America. National Academies Press; 2013. [PubMed] [Google Scholar]
- 12.Giovannetti ER, Reider L, Wolff JL, Frick KD, Boult C, Steinwachs D, et al. Do older patients and their family caregivers agree about the quality of chronic illness care? Int J Qual Health Care. 2013;25(5):515–24. doi: 10.1093/intqhc/mzt052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Department of Health and Human Services. Federal Register. 2015 Nov 3;80(212):68127. [PubMed] [Google Scholar]
- 14.Creasy KR, Lutz BJ, Young ME, Stacciarini JM. Clinical Implications of Family-Centered Care in Stroke Rehabilitation. Rehabilitation nursing: the official journal of the Association of Rehabilitation Nurses. 2015;40(6):349–59. doi: 10.1002/rnj.188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Armstrong R, Hall BJ, Doyle J, Waters E. Cochrane Update‘Scoping the scope’ of a cochrane review. J Public Health. 2011;33(1):147–50. doi: 10.1093/pubmed/fdr015. [DOI] [PubMed] [Google Scholar]
- 16.Peters M, Godfrey C, McInerney P, Soares C, Hanan K, Parker D. The Joanna Briggs Institute Reviewers’ Manual 2015: Methodology for JBI Scoping Reviews. 2015 [Google Scholar]
- 17.Critical Appraisal Skills Programme (CASP) 2014 http://media.wix.com/ugd/dded87_29c5b002d99342f788c6ac670e49f274.pdf.
- 18.Center for Evidence-Based Management. Critical Appraisal of a Survey. http://www.cebma.org/wp-content/uploads/Critical-Appraisal-Questions-for-a-Survey.pdf.
- 19.Pace R, Pluye P, Bartlett G, Macaulay AC, Salsberg J, Jagosh J, et al. Testing the reliability and efficiency of the pilot Mixed Methods Appraisal Tool (MMAT) for systematic mixed studies review. Int J Nurs Stud. 2012;49(1):47–53. doi: 10.1016/j.ijnurstu.2011.07.002. [DOI] [PubMed] [Google Scholar]
- 20.Dixon-Woods M, Shaw RL, Agarwal S, Smith JA. The problem of appraising qualitative research. Qual Saf Health Care. 2004;13(3):223–5. doi: 10.1136/qshc.2003.008714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bernard HR, Ryan GW. Analyzing qualitative data: Systematic approaches. 1. Washington DC: SAGE publications; 2010. [Google Scholar]
- 22.Morris MW, Leung K, Ames D, Lickel B. Views from inside and outside: Integrating emic and etic insights about culture and justice judgment. Acad Manage Rev. 1999;24(4):781–96. [Google Scholar]
- 23.Bäckström B, Asplund K, Sundin K. The meaning of middle-aged female spouses’ lived experience of the relationship with a partner who has suffered a stroke, during the first year postdischarge. Nurs Inq. 2010;17(3):257–68. doi: 10.1111/j.1440-1800.2010.00490.x. [DOI] [PubMed] [Google Scholar]
- 24.Bäckström B, Sundin K. The experience of being a middle-aged close relative of a person who has suffered a stroke, 1 year after discharge from a rehabilitation clinic: A qualitative study. Int J Nurs Stud. 2009;46(11):1475–84. doi: 10.1016/j.ijnurstu.2009.04.009. [DOI] [PubMed] [Google Scholar]
- 25.Brittain KR, Shaw C. The social consequences of living with and dealing with incontinence—A carers perspective. Soc Sci Med. 2007;65(6):1274–83. doi: 10.1016/j.socscimed.2007.04.002. [DOI] [PubMed] [Google Scholar]
- 26.Brown K, Worrall L, Davidson B, Howe T. Living successfully with aphasia: Family members share their views. Top Stroke Rehabil. 2011;18(5):536–48. doi: 10.1310/tsr1805-536. [DOI] [PubMed] [Google Scholar]
- 27.Cameron JI, Naglie G, Silver FL, Gignac MA. Stroke family caregivers’ support needs change across the care continuum: a qualitative study using the timing it right framework. Disabil Rehabil. 2013;35(4):315–24. doi: 10.3109/09638288.2012.691937. [DOI] [PubMed] [Google Scholar]
- 28.Cecil R, Thompson K, Parahoo K, McCaughan E. Towards an understanding of the lives of families affected by stroke: a qualitative study of home carers. J Adv Nurs. 2013;69(8):1761–70. doi: 10.1111/jan.12037. [DOI] [PubMed] [Google Scholar]
- 29.Chang L-H, Wang J. Institutional contexts contribute to the low priority given to developing self-care independence in a rehabilitation ward: a qualitative study. Clin Rehabil. 2013;27(6):538–45. doi: 10.1177/0269215512461264. [DOI] [PubMed] [Google Scholar]
- 30.Chow C, Tiwari T. Experience of family caregivers of community-dwelling stroke survivors and risk of elder abuse: a qualitative study. J Adult Pro. 2014;16(5):276–93. [Google Scholar]
- 31.Cobley CS, Fisher RJ, Chouliara N, Kerr M, Walker MF. A qualitative study exploring patients’ and carers’ experiences of Early Supported Discharge services after stroke. Clin Rehabil. 2013;27(8):750–7. doi: 10.1177/0269215512474030. [DOI] [PubMed] [Google Scholar]
- 32.Danzl MM, Hunter EG, Campbell S, Sylvia V, Kuperstein J, Maddy K, et al. Living With a Ball and Chain”: The Experience of Stroke for Individuals and Their Caregivers in Rural Appalachian Kentucky. J Rural Health. 2013;29(4):368–82. doi: 10.1111/jrh.12023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Dietz A, Thiessen A, Griffith J, Peterson A, Sawyer E, McKelvey M. The renegotiation of social roles in chronic aphasia: Finding a voice through AAC. Aphasiology. 2013;27(3):309–25. [Google Scholar]
- 34.Eames S, Hoffmann T, Worrall L, Read S. Stroke patients’ and carers’ perception of barriers to accessing stroke information. Top Stroke Rehabil. 2010;17(2):69–78. doi: 10.1310/tsr1702-69. [DOI] [PubMed] [Google Scholar]
- 35.Egbert N, Koch L, Coeling H, Ayers D. The role of social support in the family and community integration of right-hemisphere stroke survivors. Health Commun. 2006;20(1):45–55. doi: 10.1207/s15327027hc2001_5. [DOI] [PubMed] [Google Scholar]
- 36.El Masry Y, Mullan B, Hackett M. Psychosocial Experiences and Needs of Australian Caregivers of People with Stroke: Prognosis Messages, Caregiver Resilience, and Relationships. Top Stroke Rehabil. 2013;20(4):356–68. doi: 10.1310/tsr2004-356. [DOI] [PubMed] [Google Scholar]
- 37.Ellis-Hill C, Robison J, Wiles R, McPherson K, Hyndman D, Ashburn A, et al. Going home to get on with life: patients and carers experiences of being discharged from hospital following a stroke. Disabil Rehabil. 2009;31(2):61–72. doi: 10.1080/09638280701775289. [DOI] [PubMed] [Google Scholar]
- 38.Garrett D, Cowdell F. Information needs of patients and carers following stroke. Nurs Older People. 2005;17(6):14–6. doi: 10.7748/nop2005.09.17.6.14.c2386. [DOI] [PubMed] [Google Scholar]
- 39.Gosman-Hedström G, Dahlin-Ivanoff S. Mastering an unpredictable everyday life after stroke’–older women’s experiences of caring and living with their partners. Scand J Occup Ther. 2012;26(3):587–97. doi: 10.1111/j.1471-6712.2012.00975.x. [DOI] [PubMed] [Google Scholar]
- 40.Grant JS, Glandon GL, Elliott TR, Giger JN, Weaver M. Problems and associated feelings experienced by family caregivers of stroke survivors the second and third month postdischarge. Top Stroke Rehabil. 2006;13(3):66–74. doi: 10.1310/6UL6-5X89-B05M-36TH. [DOI] [PubMed] [Google Scholar]
- 41.Greenwood N, Mackenzie A, Cloud G, Wilson N. Loss of autonomy, control and independence when caring: a qualitative study of informal carers of stroke survivors in the first three months after discharge. Disabil Rehabil. 2010;32(2):125–33. doi: 10.3109/09638280903050069. [DOI] [PubMed] [Google Scholar]
- 42.Greenwood N, Mackenzie A, Wilson N, Cloud G. Managing uncertainty in life after stroke: a qualitative study of the experiences of established and new informal carers in the first 3 months after discharge. Int J Nurs Stud. 2009;46(8):1122–33. doi: 10.1016/j.ijnurstu.2009.02.011. [DOI] [PubMed] [Google Scholar]
- 43.Gustafsson L, Bootle K. Client and carer experience of transition home from inpatient stroke rehabilitation. Disabil Rehabil. 2013;35(16):1380–6. doi: 10.3109/09638288.2012.740134. [DOI] [PubMed] [Google Scholar]
- 44.Hallé M-C, Le Dorze G. Understanding significant others’ experience of aphasia and rehabilitation following stroke. Disabil Rehabil. 2014;36(21):1774–82. doi: 10.3109/09638288.2013.870608. [DOI] [PubMed] [Google Scholar]
- 45.Hare R, Rogers H, Lester H, McManus R, Mant J. What do stroke patients and their carers want from community services? Fam Pract. 2006;23(1):131–6. doi: 10.1093/fampra/cmi098. [DOI] [PubMed] [Google Scholar]
- 46.Howe T, Davidson B, Worrall L, Hersh D, Ferguson A, Sherratt S, et al. ‘You needed to rehab… families as well’: family members’ own goals for aphasia rehabilitation. Int J Lang Commun Disord. 2012;47(5):511–21. doi: 10.1111/j.1460-6984.2012.00159.x. [DOI] [PubMed] [Google Scholar]
- 47.Jullamate P, de Azeredo Z, Rosenberg E, Pàul C, Subgranon R. Informal stroke rehabilitation: what are the main reasons of Thai caregivers? Int J Rehabil Res. 2007;30(4):315–20. doi: 10.1097/MRR.0b013e3282f14539. [DOI] [PubMed] [Google Scholar]
- 48.Lawrence M, Kerr S, Watson H, Paton G, Ellis G. An exploration of lifestyle beliefs and lifestyle behaviour following stroke: findings from a focus group study of patients and family members. BMC Fam Pract. 2010;11(1):97. doi: 10.1186/1471-2296-11-97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lawrence M, Kinn S. Needs, priorities, and desired rehabilitation outcomes of family members of young adults who have had a stroke: findings from a phenomenological study. Disabil Rehabil. 2013;35(7):586–95. doi: 10.3109/09638288.2012.711895. [DOI] [PubMed] [Google Scholar]
- 50.Lee RL, Mok ES. Seeking harmony in the provision of care to the stroke-impaired: views of Chinese family caregivers. J Clin Nurs. 2011;20(9–10):1436–44. doi: 10.1111/j.1365-2702.2010.03500.x. [DOI] [PubMed] [Google Scholar]
- 51.Lin SH. Exploratory analysis of Chinese-American family caregivers’ needs and instructional video on dressing stroke survivors. Int J Consum Stud. 2010;34(5):581–6. [Google Scholar]
- 52.Lutz BJ, Chumbler NR, Roland K. Care coordination/home-telehealth for veterans with stroke and their caregivers: addressing an unmet need. Top Stroke Rehabil. 2007;14(2):32–42. doi: 10.1310/tsr1402-32. [DOI] [PubMed] [Google Scholar]
- 53.Lynch EB, Butt Z, Heinemann A, Victorson D, Nowinski CJ, Perez L, et al. A qualitative study of quality of life after stroke: the importance of social relationships. J Rehabil Med. 2008;40(7):518–23. doi: 10.2340/16501977-0203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Morris JH, Oliver T, Kroll T, Joice S, Williams B. From physical and functional to continuity with pre-stroke self and participation in valued activities: A qualitative exploration of stroke survivors’, carers’ and physiotherapists’ perceptions of physical activity after stroke. Disabil Rehabil. 2014;37(1):64–77. doi: 10.3109/09638288.2014.907828. [DOI] [PubMed] [Google Scholar]
- 55.Obe-om T, Fongkeaw W, Panya P, Senaratana W. Experiences of Families with Stroke Survivors in Chiang Mai Province. Thai J Nurs Res. 2006;10(4):276–87. [Google Scholar]
- 56.O’Connell B, Baker L. Managing as carers of stroke survivors: strategies from the field. Int J Nurs Pract. 2004;10(3):121–6. doi: 10.1111/j.1440-172X.2004.00469.x. [DOI] [PubMed] [Google Scholar]
- 57.O’Connell B, Baker L, Prosser A. The educational needs of caregivers of stroke survivors in acute and community settings. J Neurosci Nurs. 2003;35(1):21–8. doi: 10.1097/01376517-200302000-00006. [DOI] [PubMed] [Google Scholar]
- 58.Payne S, Burton C, Addington-Hall J, Jones A. End-of-life issues in acute stroke care: a qualitative study of the experiences and preferences of patients and families. Palliat Med. 2010;24(2):146–53. doi: 10.1177/0269216309350252. [DOI] [PubMed] [Google Scholar]
- 59.Ringsberg K, Holmgren B. Home rehabilitation of stroke patients from the perspective of the patients and their relatives. Nordisk Fysioterapi. 2003;7:21–31. [Google Scholar]
- 60.Rochette A, Racine E, Lefebvre H, Lacombe J, Bastien J, Tellier M. Ethical issues relating to the inclusion of relatives as clients in the post-stroke rehabilitation process as perceived by patients, relatives and health professionals. Patient Educ Couns. 2014;94(3):384–9. doi: 10.1016/j.pec.2013.10.028. [DOI] [PubMed] [Google Scholar]
- 61.Rosenberg E, Jullamate P, Azeredo Z. Informal caregiving: cross-cultural applicability of the person-environment model. Health Sociol Rev. 2009;18(4):399–411. [Google Scholar]
- 62.Rudman DL, Hebert D, Reid D. Living in a restricted occupational world: the occupational experiences of stroke survivors who are wheelchair users and their caregivers. Can J Occup Ther. 2006;73(3):141–52. doi: 10.2182/cjot.05.0014. [DOI] [PubMed] [Google Scholar]
- 63.Saban KL, Hogan NS. Female caregivers of stroke survivors: coping and adapting to a life that once was. J Neurosci Nurs. 2012;44(1):2–14. doi: 10.1097/JNN.0b013e31823ae4f9. [DOI] [PubMed] [Google Scholar]
- 64.Smith SD, Gignac MA, Richardson D, Cameron JI. Differences in the experiences and support needs of family caregivers to stroke survivors: does age matter? Top Stroke Rehabil. 2008;15(6):593–601. doi: 10.1310/tsr1506-593. [DOI] [PubMed] [Google Scholar]
- 65.Tellier M, Rochette A, Lefebvre H. Impact of mild stroke on the quality of life of spouses. Int J Rehabil Res. 2011;34(3):209–14. doi: 10.1097/MRR.0b013e328343d540. [DOI] [PubMed] [Google Scholar]
- 66.Van Dongen I, Josephsson S, Ekstam L. Changes in daily occupations and the meaning of work for three women caring for relatives post-stroke. Scand J Occup Ther. 2014;21(5):348–58. doi: 10.3109/11038128.2014.903995. [DOI] [PubMed] [Google Scholar]
- 67.Vincent C, Deaudelin I, Robichaud L, Rousseau J, Viscogliosi C, Talbot LR, et al. Rehabilitation needs for older adults with stroke living at home: perceptions of four populations. BMC Geriatr. 2007;7(1):20. doi: 10.1186/1471-2318-7-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Winkler M, Bedford V, Northcott S, Hilari K. Aphasia blog talk: How does stroke and aphasia affect the carer and their relationship with the person with aphasia? Aphasiology. 2014;28(11):1301–19. [Google Scholar]
- 69.Pierce LL, Thompson TL, Govoni AL, Steiner V. Caregivers’ incongruence: Emotional strain in caring for persons with stroke. Rehabilitation nursing: the official journal of the Association of Rehabilitation Nurses. 2012;37(5):258–66. doi: 10.1002/rnj.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Bäckström B, Sundin K. The meaning of being a middle-aged close relative of a person who has suffered a stroke, 1 month after discharge from a rehabilitation clinic. Nurs Inq. 2007;14(3):243–54. doi: 10.1111/j.1440-1800.2007.00373.x. [DOI] [PubMed] [Google Scholar]
- 71.Coombs UE. Spousal caregiving for stroke survivors. J Neurosci Nurs. 2007;39(2):112–9. doi: 10.1097/01376517-200704000-00008. [DOI] [PubMed] [Google Scholar]
- 72.Boter H, Rinkel GJ, De Haan RJ. Outreach nurse support after stroke: a descriptive study on patients’ and carers’ needs, and applied nursing interventions. Clin Rehabil. 2004;18(2):156–63. doi: 10.1191/0269215504cr713oa. [DOI] [PubMed] [Google Scholar]
- 73.Kong AP-H. Family members’ report on speech-language pathology and community services for persons with aphasia in Hong Kong. Disabil Rehabil. 2011;33(25–26):2633–45. doi: 10.3109/09638288.2011.579220. [DOI] [PubMed] [Google Scholar]
- 74.Perry L, Middleton S. An investigation of family carers’ needs following stroke survivors’ discharge from acute hospital care in Australia. Disabil Rehabil. 2011;33(19–20):1890–900. doi: 10.3109/09638288.2011.553702. [DOI] [PubMed] [Google Scholar]
- 75.Sangvatanakul P, Hillege S, Lalor E, Levi C, Hill K, Middleton S. Setting stroke research priorities: The consumer perspective. J Vasc Nurs. 2010;28(4):121–31. doi: 10.1016/j.jvn.2010.09.001. [DOI] [PubMed] [Google Scholar]
- 76.Hinojosa MS, Rittman MR. Stroke caregiver information needs: Comparison of Mainland and Puerto Rican caregivers. J Rehabil Res Dev. 2007;44(5):649–58. doi: 10.1682/jrrd.2006.10.0131. [DOI] [PubMed] [Google Scholar]
- 77.Mak AK, Mackenzie A, Lui MH. Changing needs of Chinese family caregivers of stroke survivors. J Clin Nurs. 2007;16(5):971–9. doi: 10.1111/j.1365-2702.2006.01754.x. [DOI] [PubMed] [Google Scholar]
- 78.Mackenzie A, Perry L, Lockhart E, Cottee M, Cloud G, Mann H. Family carers of stroke survivors: needs, knowledge, satisfaction and competence in caring. Disabil Rehabil. 2007;29(2):111–21. doi: 10.1080/09638280600731599. [DOI] [PubMed] [Google Scholar]
- 79.Hinojosa MS, Rittman M. Association between health education needs and stroke caregiver injury. J Aging Health. 2009;21(7):1040–58. doi: 10.1177/0898264309344321. [DOI] [PubMed] [Google Scholar]
- 80.Kim JW, Moon SS. Needs of family caregivers caring for stroke patients: based on the rehabilitation treatment phase and the treatment setting. Soc Work Health Care. 2007;45(1):81–97. doi: 10.1300/J010v45n01_06. [DOI] [PubMed] [Google Scholar]
- 81.Haley WE, Allen JY, Grant JS, Clay OJ, Perkins M, Roth DL. Problems and Benefits Reported by Stroke Family Caregivers Results From a Prospective Epidemiological Study. Stroke. 2009;40(6):2129–33. doi: 10.1161/STROKEAHA.108.545269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.MacIsaac L, Harrison MB, Buchanan D, Hopman WM. Supportive care needs after an acute stroke: A descriptive enquiry of caregivers’ perspective. J Neurosci Nurs. 2011;43(3):132–40. doi: 10.1097/JNN.0b013e3182135b28. [DOI] [PubMed] [Google Scholar]
- 83.Mackenzie C, Kelly S, Paton G, Brady M, Muir M. The Living with Dysarthria group for post-stroke dysarthria: the participant voice. Int J Lang Commun Disord. 2013;48(4):402–20. doi: 10.1111/1460-6984.12017. [DOI] [PubMed] [Google Scholar]
- 84.Kniepmann K, Cupler MH. Occupational changes in caregivers for spouses with stroke and aphasia. Br J Occup The. 2014;77(1):10–8. [Google Scholar]
- 85.McCarthy MJ, Lyons KS. Incongruence between stroke survivor and spouse perceptions of survivor functioning and effects on spouse mental health: a mixed-methods pilot study. Aging Ment Health. 2015;19(1):46–54. doi: 10.1080/13607863.2014.913551. [DOI] [PubMed] [Google Scholar]
- 86.World Health Organization. Exposure draft for comment. Geneva: WHO; 2013. How to use the ICF: A practical manual for using the International Classification of Functioning, Disability and Health (ICF) [Google Scholar]
- 87.Geyh S, Cieza A, Schouten J, Dickson H, Frommelt P, Omar Z, et al. ICF Core Sets for stroke. J Rehabil Med. 2004;(44 Suppl):135–41. doi: 10.1080/16501960410016776. [DOI] [PubMed] [Google Scholar]
- 88.O’Halloran R, Grohn B, Worrall L. Environmental factors that influence communication for patients with a communication disability in acute hospital stroke units: A qualitative metasynthesis. Arch Phys Med Rehabil. 2012;93(1):S77–S85. doi: 10.1016/j.apmr.2011.06.039. [DOI] [PubMed] [Google Scholar]
- 89.McCullagh E, Brigstocke G, Donaldson N, Kalra L. Determinants of caregiving burden and quality of life in caregivers of stroke patients. Stroke. 2005;36(10):2181–6. doi: 10.1161/01.STR.0000181755.23914.53. [DOI] [PubMed] [Google Scholar]
- 90.Rodgers H, Bond S, Curless R. Inadequacies in the provision of information to stroke patients and their families. Age Ageing. 2001;30(2):129–33. doi: 10.1093/ageing/30.2.129. [DOI] [PubMed] [Google Scholar]
- 91.Wong JS, Brooks D, Mansfield A. Do falls experienced during in-patient stroke rehabilitation affect length of stay, functional status, and discharge destination? Arch Phys Med Rehabil. 2015;97(4):561–6. doi: 10.1016/j.apmr.2015.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Wottrich AW, Von Koch L, Tham K. The meaning of rehabilitation in the home environment after acute stroke from the perspective of a multiprofessional team. Phys Ther. 2007;87(6):778–88. doi: 10.2522/ptj.20060152. [DOI] [PubMed] [Google Scholar]
- 93.Agree EM, Freedman VA, Cornman JC, Wolf DA, Marcotte JE. Reconsidering substitution in long-term care: when does assistive technology take the place of personal care? J Gerontol B Psychol Sci Soc Sci. 2005;60(5):S272–S80. doi: 10.1093/geronb/60.5.s272. [DOI] [PubMed] [Google Scholar]
- 94.Norlander A, Jonsson AC, Stahl A, Lindgren A, Iwarsson S. Activity among long-term stroke survivors. A study based on an ICF-oriented analysis of two established ADL and social activity instruments. Disabil Rehabil. 2016;38(20):2028–37. doi: 10.3109/09638288.2015.1111437. [DOI] [PubMed] [Google Scholar]
- 95.Jaracz K, Grabowska-Fudala B, Górna K, Jaracz J, Moczko J, Kozubski W. Burden in caregivers of long-term stroke survivors: prevalence and determinants at 6 months and 5 years after stroke. Patient Educ Couns. 2015;98(8):1011–6. doi: 10.1016/j.pec.2015.04.008. [DOI] [PubMed] [Google Scholar]
- 96.Taylor TN, Davis PH, Torner JC, Holmes J, Meyer JW, Jacobson MF. Lifetime cost of stroke in the United States. Stroke. 1996;27(9):1459–66. doi: 10.1161/01.str.27.9.1459. [DOI] [PubMed] [Google Scholar]
- 97.Yetzer E, Blake K, Goetsch N, Shook M. SAFE Medication Management for Patients with Physical Impairments of Stroke, Part One. Rehabilitation nursing: the official journal of the Association of Rehabilitation Nurses. 2015;40(4):260–6. doi: 10.1002/rnj.194. [DOI] [PubMed] [Google Scholar]
- 98.Kleindorfer D. Sociodemographic groups at risk: race/ethnicity. Stroke. 2009;40(3 suppl 1):S75–8. doi: 10.1161/STROKEAHA.108.534909. [DOI] [PubMed] [Google Scholar]
- 99.Stineman MG, Rist PM, Kurichi JE, Maislin G. Disability meanings according to patients and clinicians: imagined recovery choice pathways. Qual Life Res. 2009;18(3):389–98. doi: 10.1007/s11136-009-9441-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.