Abstract
This paper identifies differences in adult Latino immigrant barriers to healthcare in the Cincinnati area in Hamilton County, OH on three levels: by region, by neighborhood, and by community health center. Secondary data analysis was performed on 439 surveys. Respondents were aggregated by the geographic regions and neighborhoods where they live and by two community health centers where they receive care. Outcome measures included pragmatic and skill barrier indices adapted from the Barriers to Care Questionnaire (BCQ); the pragmatics index consists logistical barriers, including transportation and cost; the skills index is made up of items related to navigating the healthcare system, including communicating with physicians and completing paperwork. The results indicate that immigrant Latinos living in western Cincinnati and northern Hamilton County face significantly higher pragmatic barriers to care, while Latino immigrants going to a community health center in western Cincinnati have significantly fewer pragmatic and skill barriers than immigrants utilizing a nearby community health center. Because healthcare options for undocumented immigrants do not improve with the Affordable Care Act, community health centers will continue to serve as their primary source of care. This is particularly true in non-traditional migration areas, where immigrants tend to be isolated and lack resources. Efforts to improve access to healthcare for immigrant Latinos require place-based approaches that allow for targeted resources to improve care in these locations. This study helps to fill that need by identifying variation in barriers to care on multiple levels and offering strategies to alleviate these barriers.
Keywords: place-based approaches, immigrant, Latinos, health disparities
Introduction
It is well established that Latinos face higher barriers to healthcare, including language, a lack of knowledge of the healthcare system, a lack of transportation options, high costs, and issues related to getting timely appointments and missing work [1–2]. Further, Latinos are more likely to be uninsured than non-Latino populations and less likely to have usual source of care or doctor visit [3–5]. These issues are exacerbated in non-traditional migration areas, which are areas outside of traditional Latino immigrant locations such as California, Texas, and Illinois, that have experienced rapid increases in Latino population over the past few decades. Latinos in non-traditional migration areas tend to live in isolated neighborhoods, lack established resources and networks of care, and report a lack of Spanish-speaking physicians and translation services [6–8]. Like other non-traditional migration areas, immigrant Latinos in Cincinnati face higher barriers than non-immigrant Latinos [9], and are utilizing community health centers as their primary source of healthcare [10]. As the Affordable Care Act (ACA) improves access to healthcare for many groups in the U.S., it has little impact on undocumented immigrants, who are not eligible for Medicaid or health insurance subsidies. Because they are not eligible for ACA-subsidized services, undocumented immigrants are most likely to rely on safety-net providers such as community health centers [11].
Cincinnati is located in Hamilton County and has experienced substantial growth in its Latino population over the last few decades. Census data indicates that almost 60,000 Latinos currently live in the Cincinnati Metropolitan Area [12], compared to less than 10,000 in 1990 and 22,000 in 2000 [13]. About a third of Latinos in the region live in Hamilton County (21,969), with the majority of them being of Mexican (41.5%) and Central American (27.1%) origins. In Hamilton County, about half of the Latino population is foreign-born (9,000), with almost three-quarters coming from Mexico (3,230) and Central America (3,258). The majority of Mexican (88.9%) and Central American immigrants (80.3%) are not U.S. citizens [14]. The true number of Latino immigrants living in the Cincinnati area is likely much higher, as Latino immigrants are a “hidden population” [15] and previous estimates of the Latino population by local researchers were significantly higher than those produced by the census [16]. In addition, Mexicans and Central American immigrants living in Hamilton County face obstacles related to language, transportation, and income. High percentages of foreign-born Mexicans live in households that are without an adult or adolescent who speaks English very well (38%) or less than very well (66%), that do not have access to a car (11%), and that are low-income (65%). The situation is even more challenging for Central American immigrants in Hamilton County, as 62% live in households without an adult or adolescent who speaks English very well, 20% live in households without a vehicle, 75% speak English less than very well, and 80% are low income [14]. Latinos in Hamilton County are concentrated in a few major areas, including in northern Hamilton County (Forest Park & Springdale), in the Price Hill (PH) neighborhoods in western Cincinnati, in the Carthage neighborhood in northern Cincinnati, and in the Norwood area, which is in the eastern part of the city (see Figure 1).
Figure 1.
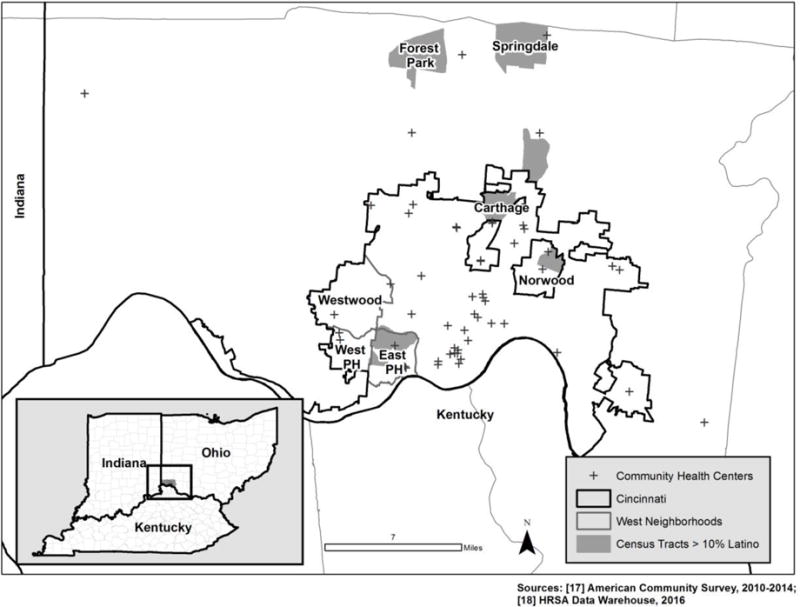
Hamilton County, City of Cincinnati, & High Percentage (>10%) Latino Census Tracts
Due to the obstacles related to Cincinnati’s status as a new immigrant destination and lack of infrastructure to provide services to the large influx of incoming immigrants, immigrant Latinos in the area have significantly higher barriers to care compared with U.S.-born Latinos, Blacks, and Whites, particularly in the northern and eastern parts of the region [9]. Consistent with previous research [19–20], results from a recent community-partnered research project in Cincinnati revealed Latino immigrants have much lower utilization of healthcare and identified lack of documentation, fear, and language as the most important barriers to healthcare [10]. The same study also revealed that community health centers (CHCs) were the primary source of care for immigrant Latinos in Cincinnati, with immigrants indicating that CHCs were less expensive, had shorter wait times, were closer, and had more friendly and welcoming staff. The use of CHCs by Latinos is expected given the large number of CHCs in the region (see Map 1) and the role of CHCs in providing access to care regardless of insurance status, income, and legal status [21]. CHCs are one of the only options for undocumented immigrants, two-thirds of which are estimated to be without health insurance [22]. Though the ACA has increased funding for CHCs and increased access to emergency Medicaid and language services, it is unclear if immigrants in Cincinnati are benefiting from the ACA, and cuts to Medicaid Disproportionate Share Hospital (DSH) payments may further reduce their access to care [11, 22–23].
There are limited resources in Cincinnati to provide quality healthcare to the growing Latino immigrant population; therefore, it is important to understand how access to care varies within the Cincinnati region so that we may accurately target specific neighborhoods and community health centers for interventions. In this paper, we use community-collected data to explore immigrant Latino barriers to healthcare in Hamilton County, Ohio on three levels: by region, by neighborhood, and by community health center. Within healthcare system research, place is increasingly recognized as a critical contributor to health disparities [24]. Place-based approaches address health disparities by engaging community stakeholders in a specified geography to improve community conditions and promote optimal health outcomes [25]. Unlike traditional research that focuses on one system, place-based approaches address the multiple contexts that contribute to negative health outcomes, including neighborhoods and healthcare providers. To date, few studies have used place-based approaches to explore the geographic variation of Latino access to healthcare within non-traditional migration areas. Edward and Biddle [26] focused on geographic barriers to care in Louisville, Kentucky, while Dulin et al. [27–28] identified where Hispanic immigrants would most benefit from increased access to primary care services in Charlotte, North Carolina. The current research builds on these studies by exploring immigrant Latino barriers to care on multiple levels and identifying specific places where immigrant Latinos face higher barriers to care.
Our primary research question is the following:
How do Latino immigrant barriers to healthcare vary by geographic region (East, West, and North), by neighborhood (Westwood, West Price Hill, and East Price Hill), and by community health center (Clinic A and Clinic B)?
Our three hypotheses are as follows:
Immigrant Latinos living in the northern and eastern regions of the study area will have higher barriers to care.
Immigrant Latinos living in the more isolated neighborhood of Westwood will have higher barriers to care.
Immigrant Latinos living in the West region that utilize Clinic A, which is located just outside of the West region, will have higher barriers to care than those utilizing Clinic B, which is located within the western region.
The overarching goal of the current study was to provide place-specific data to community partners in Cincinnati that would allow them to provide more targeted resource allocation and support to the geographic areas and healthcare settings where it is most needed. The authors are members of Latinos Unidos por la Salud (LU-Salud), a community-academic research team consisting of Latino immigrant researchers and academic partners dedicated to conducting research to improve the health of Latino immigrants in Cincinnati [29]. We have been collaborating with local Latino social service agencies in Cincinnati and providers at local health centers for more than eight years to address inequities in health and healthcare experienced by Latino immigrants in our area. Through our academic-community partnerships, the results of our place-based approach will be used to directly target interventions to specific regions, neighborhoods, and community health centers. Specifically, two local Latino-serving social service agencies and a coalition of more than 50 Latino-serving providers will use these results to advocate for resource allocation within their organizations and to develop new programs and services to areas that are experiencing disproportionate barriers to healthcare.
Methodology
Procedure
This study is part of a larger project in which the primary aim was to understand the healthcare experiences of immigrant Latinos in the Cincinnati metropolitan region. The University of Cincinnati Internal Review Board granted the project a “not human subjects research” determination because surveys were anonymous and were intended to improve local healthcare outcomes. Participants were approached by one of the community research members and asked to fill out an anonymous survey in order to understand their healthcare experiences. Community research members recruited participants by going door-to-door in their communities or through local organizations, schools, and stores with high level of Latino attendance. Participants were given the option to complete the questionnaire independently or in a verbal format facilitated by a community research member. Surveys were completed in either Spanish or English, depending on the participant’s language preference, with 94% the surveys completed in Spanish. Each questionnaire took approximately 30 minutes to complete and participants were compensated with a $5 gift card for their time and effort.
Participants
A total of 516 individuals participated in the study, all of which were first-generation immigrants born in Latin America. We limited our analysis to 439 participants living in Hamilton County, OH that could be linked to a specific neighborhood or ZIP code. Of these participants, 95% were under the age of 50, 70% were female, 94% indicated that Spanish is their preferred language, 43% were married, 73% had at least one child, and 84% worked at least part-time or were homemakers. Half of respondents identified their country of origin to be Mexico, while 30% came from Guatemala, and 15% came from elsewhere in Central America (Panama, Costa Rica, Nicaragua, Honduras, or El Salvador). The average household size of participants was 4 and the average number of years residing in the U.S. and Cincinnati were 10.6 years and 8.7 years, respectively.
Measures
Barriers to healthcare
We used two subscales of the Barriers to Care Questionnaire (BCQ) [30] originally developed for use with children suffering from asthma but successfully adapted for use with Spanish-speaking Latino populations [29]: 1) Pragmatics: logistical issues such as transportation, availability of appointments, child care and work responsibilities, and wait times, as well as cost issues that might prevent or delay health care use; 2) Skills: learned strategies to navigate through, manipulate, or function competently within the health care system; these include communicating with doctors and nurses, filling out paperwork, and getting referrals. These subscales of the BCQ are scored on a 1–100 scale so that higher scores reflect higher functioning (fewer barriers to care). Our outcome measures included pragmatic and skill barriers to care indices because they capture the large range of barriers reported by Latinos [1]. The original BCQ and our adapted BCQ with Latinos in Cincinnati both showed internal consistency reliability, with subscale alphas ranging from .74–.91 [29–30]. In order to help us understand the specific issues that may need to be addressed to improve access to care and to tailor interventions, we also report the results from a few key individual barriers, including the pragmatic barriers of transportation, costs, and availability (after hours and weekends), and the skill barriers of language, understanding the healthcare system, and filling out paperwork.
Other Measures
Participants were also asked to provide their home ZIP code and neighborhood, the number of years they have lived in the U.S. and Cincinnati, the number of doctor visits in the past year, and the name of the healthcare provider or clinic where they usually go to receive healthcare services.
Design
Latino immigrant respondents were grouped into neighborhoods based on their responses to the survey, which included asking participants to name their neighborhood and ZIP Code. If the neighborhood question was left blank, ZIP codes were used to assign respondents to their respective neighborhoods. Neighborhoods were combined based on proximity and regional groupings were created so we could compare Latino barriers to care across three major geographic regions in Hamilton County – East, West, and North (see Map 2). Because the majority of the respondents came from the West region and it is home to a large concentration of Latinos, we focused the rest of our analysis on respondents that reported living in the West region. Barriers to care were analyzed for three West region neighborhoods, which include East Price Hill, West Price Hill, and Westwood. The most recent census estimates indicate that the majority of Latinos residing in the West region live in East Price Hill, which has a population of about 15,000, 10% of which are Latino, and has an overall poverty rate of greater than 40%. West Price Hill (~500, 3% of population, 17% poverty) and Westwood (~700, 2% of population, 23% poverty) have smaller numbers of Latinos and lower rates of poverty [31]. In addition, Latino immigrant respondents living in the West region were further aggregated by community health center. The survey asked participants to indicate the specific location where they usually receive medical care. From this, we were able to group West respondents by the two most commonly listed community health centers (CHCs). For the purpose of preserving confidentiality, this paper will refer to the CHCs as Clinic A and Clinic B (see Figure 2 for their approximate locations).
Figure 2.
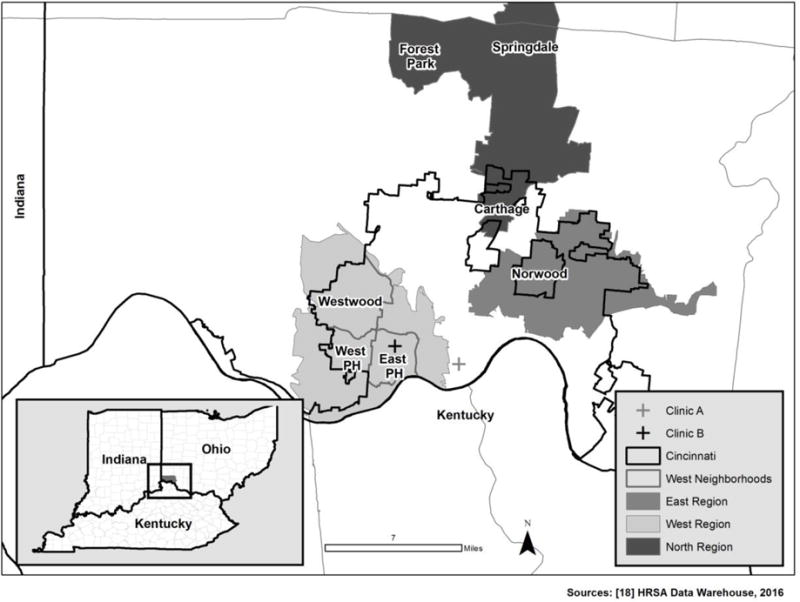
Regions, Neighborhoods, and Community Health Centers
Analytic Plan
Descriptive statistics were used to explore differences between the regional groupings, neighborhoods, and community health centers (CHCs). ANOVAs and independent t-tests were also performed to identify significant differences for pragmatic and skill barriers to care. All statistical analyses were performed using SAS statistical software (version 9.4; SAS Institute Inc, Cary, NC).
Results
Differences by Region
Most respondents resided in the West region, where about half identified as Guatemalan and a third identified as Mexican. In the East region, respondents were primarily of Mexican origin, had spent more time in the U.S. and Cincinnati, and had the lowest percentage utilizing community health centers as a usual source of care. In general, the results do not support our hypothesis as Latino immigrants living in the East region have fewer pragmatic and skill barriers than those living in the North and West regions. ANOVAs did not reveal significant differences in pragmatics or skill barriers across the three geographic areas. However, when comparing the East to other regions, independent t-tests revealed significantly higher pragmatic barriers, t(366) = 1.65, p=0.05, and skill barriers, t(208) = 2.10, p=.02, for immigrants living in the West, and significantly higher pragmatic barriers (but not skills) for immigrants living the North, t(352) = 2.08, p=0.02.
Overall, the most significant individual pragmatic barrier is cost, where more than half of Latino immigrants reported often or always having problems. The North region reported the highest cost barriers, while the East region had the lowest. Relative to other barriers, transportation was not seen as a major issue, though almost one-quarter of West region immigrants reported that they often or always have problems accessing transportation to get needed medical care. The individual skill barrier items varied considerably across the three regions, with language being the most important skill barrier for the study area as a whole. More than half of immigrants living in the West region reported that they often or always have problems with doctors or nurses who do not speak Spanish. The West region also reported the highest barriers related to understanding how the healthcare system works and getting help filling out paperwork.
Difference by Neighborhood
Our place-based approach focused on the West region, where we explored differences in barriers to care for three neighborhoods: East Price Hill, West Price Hill, and Westwood. The data supported our hypothesis as Westwood had the highest barriers for both pragmatics and skills, while East Price Hill had the fewest barriers for both. ANOVAs for West neighborhoods revealed significant differences in pragmatic barriers, F(2,222) = 3.08, p=0.05, but no significant differences for skill barriers.
Pragmatic barriers varied considerably across the three neighborhoods with Westwood and West Price Hill reporting the most problems with costs, transportation, and availability (accessing care outside of normal hours and on weekends). No consistent patterns of variation existed for the skill barriers, with about half of immigrants from the three neighborhoods reporting often or always having problems with nurses or doctors who do not speak Spanish.
Differences by Community Health Center (CHC)
Latino immigrant respondents living in the West region were also aggregated by the community health center in which they usually receive care. Two community health centers had an adequate sample size: Clinic A and Clinic B. Clinic A is located in downtown Cincinnati, near the West region, while Clinic B is located within the West region. Compared to other CHCs, higher percentages of Guatemalan immigrants utilized Clinic A and Clinic B. Immigrants utilizing Clinic A had a higher percentage not visiting a doctor in past year, and reported living in the U.S. and Cincinnati for a longer period. The results support our hypothesis as immigrants utilizing Clinic A had higher pragmatic and skill barriers to care than those utilizing Clinic B. Independent t-tests revealed significantly higher barriers for both skills, t(101) = 2.19, p=0.02, and pragmatics, t(98) = 2.17, p=0.02, for immigrants utilizing Clinic A.
While the pragmatic and skill barriers indices clearly show that immigrants utilizing Clinic A face higher barriers, the individual items reveal the extent of the problems. More than 70% of immigrants utilizing Clinic A reported often or always having problems with costs and language, while more than 40% reported often or always having problems accessing transportation to medical care, compared to about 20% for immigrants utilizing Clinic B. In addition, more than half of immigrants utilizing Clinic A reported often or always having problems getting medical attention after hours or on weekends, and almost two-thirds reported often or always having problems filling out paperwork.
Discussion
While it is well established that immigrant Latinos living in non-traditional migration areas face significant barriers to accessing healthcare, this study is the first to explore the geographic variation of barriers within a region on multiple levels. This is important because Latinos in non-traditional migration areas often live in isolated neighborhoods and lack the necessary healthcare and resource infrastructure to support their needs [6–8]. Specifically, we were interested in exploring the variation in barriers to care by region, by neighborhood, and by community health center. While there were no significant differences for pragmatics or skill barriers based on healthcare utilization (self-reported doctor visits) on any level, the results demonstrate variation in barriers to care for Latino immigrants on all three levels. Latino immigrants in northern Hamilton County and western Cincinnati experience more barriers to care than Latino immigrants in eastern Cincinnati. This does not support our hypothesis and may in part be due to immigrant Latinos living in the East region having more experience as they had significantly higher number of years living in the U.S. and Cincinnati area. In addition, the majority of immigrants from the East region identified as Mexican (66%) and previous analysis revealed fewer skill barriers for Mexicans than Guatemalans in Cincinnati [10] While cost was identified as a major pragmatic barrier throughout the entire study area, higher percentages of immigrants living in the West and North reported often or always having problems with the cost of healthcare. Immigrants in the West region also reported having more problems with transportation, language, and filling out paperwork.
The analysis also revealed significant differences in barriers for Latino immigrants living within the West region, where immigrants from the West Price Hill and Westwood neighborhoods experienced significantly higher pragmatic barriers to care than immigrants from East Price Hill. East Price Hill had more respondents identify as Guatemalan than the other two neighborhoods and we found no significant differences in years lived in the U.S. and Cincinnati for residents from the three neighborhoods. The most important pragmatic barriers confronting immigrant Latinos in Westwood and West Price Hill were costs, transportation, and availability (accessing medical care after hours or on weekends). Skill barriers were consistent throughout the three neighborhoods, with language reported as the most significant barrier overall. Unlike the differences between the larger regions which may be explained by experience and country of origin, the fewer pragmatic barriers in East Price Hill are likely due to the number of resources available in the neighborhood, which include community health centers and a major social service agency serving Latinos. These within-region differences are important because it demonstrates how barriers can vary significantly within a relatively small geographic area, and the critical role of CHCs and social service agencies in providing services and outreach to a traditionally marginalized population.
In addition to the variation by region and neighborhood, we found significant differences in barriers to care for West region immigrants utilizing two community health centers. West region immigrants utilizing Clinic B as a usual source of care had significantly fewer pragmatic and skill barriers than those utilizing Clinic A. The variation may be explained in part by proximity. Clinic B is located within the neighborhood of East Price Hill, an area with potentially more resources available to immigrant Latinos, and Clinic A is located just outside of the region. The majority of immigrants utilizing both clinics were Guatemalan, though immigrants going to Clinic B had significantly fewer years of living in Cincinnati than those going to Clinic A. West region immigrants utilizing Clinic A also had the most problems related to costs, language, availability, and transportation. This raises questions about potential reasons for why immigrants are utilizing a clinic that is located further away, such as fear of deportation, which is not included in the barriers to care indices and has been identified as a major barrier for Latino immigrants in Cincinnati [10].
Several limitations of the current study suggest avenues for future research. First, we were challenged by the lack of data regarding documentation status of participants. Latino immigrants who were co-researchers on our community-academic research team administered surveys for this project. As equal collaborators with shared decision-making in the research process, our community partners believed it would be inappropriate to ask participants (most of whom were approached as strangers in community settings) about their documentation status. Although we know from previous research that a large portion of Cincinnati’s Latino immigrants are undocumented [16] and the social service agencies and public schools that we work with serve a mostly undocumented adult population, our data does not reflect the number of our participants who are legally in the United States and eligible for ACA services. In order to more fully address health inequities experience by immigrant Latinos, future research must specifically document the barriers to care experienced by undocumented immigrants and determine how they differ from those Latinos covered by the ACA. Second, an additional limit in our data was the representation across regions, neighborhoods, and community health centers. Although our overall sample is quite large, when broken down some categories are less represented than others (e.g., only 41 Latino immigrants utilized Clinic A). Because the overarching goal of our study was to work with community partners to collect data to inform local interventions, we utilized a convenience sample with the goal of reaching as many Latino immigrants as possible. Our resulting sample was the largest survey of Latino immigrants that has been conducted in our area, but our analyses were limited by the uneven representation across neighborhoods and health centers.
Conclusions and Implications
Our non-traditional migration area has seen substantial growth in the population of Latino immigrants in the past 10 years, but the local healthcare and social service support infrastructure has not expanded to keep up with growing demand [32]. To address the needs of social service agencies, advocacy groups, and healthcare providers in Cincinnati, we investigated patterns in healthcare barriers across the regions, neighborhoods, and healthcare clinics in our area. The most important outcome of this research is that we have identified specific locations in Cincinnati where immigrant Latinos experience higher barriers to accessing healthcare. The next step is to determine how we can use the results to improve access to care in these locations. In addition to the community connections we have through the community research team (LU-Salud) who collected these data, we have strong relationships with the primary Latino social service agencies and community health centers in the region. Below we suggest place-based strategies for improving access to care for Latino immigrants, all of which will flow through local Latino social service agencies and community health centers.
On a regional level, immigrant Latinos in Cincinnati struggle most with cost and language barriers. However, some resources such as language, literacy, and translation services, health insurance/Medicaid enrollment assistance, and emergency financial assistance are already available through weekly or monthly programs from local social service agencies. It is possible that some immigrants are not aware of these services or do not believe they are eligible, as previous research in non-traditional migration areas has found that a lack of knowledge of available resources was more of a barrier than availability [33]. Thus, our first strategy involves education campaigns that promote existing services, particularly to neighborhoods in northern Hamilton County and western Cincinnati. In addition, we propose to supplement existing health literacy, screening, referral programs with additional resources such as help filling out paperwork, identifying viable transportation options, or even providing transportation services to the most isolated neighborhoods in the region. A final strategy is to work with community health centers (focusing on Clinics A) to evaluate their current capacity for serving Latino immigrants, help with outreach (so Latino immigrants are aware of the low-cost healthcare services they provide regardless of legal status), and identify strategies for improving care this population. One potential strategy for community health centers that has been proven to be efficacious in other settings is to train and use promotoras de salud, or community health workers, to promote information on health education, healthcare utilization and access [34]. Ideally, these promotoras de salud would be trained and immersed within the specific neighborhoods, beginning with the Westwood neighborhood in the West region, and the Carthage neighborhood in northern Cincinnati.
In addition to the local implications described above, this research contributes to the non-traditional migration area literature through its emphasis on place and community-based partnerships. Future research can use our place-based approach as a model for collecting data on where Latino immigrants are living and accessing healthcare resources. The results revealed the wide variation in barriers to care within the region as a whole and within particular sub-regions (such as western Cincinnati), while also revealing inconsistencies in the factors that impact immigrant Latino access. For example, immigrants from the East region had the highest number of years in the U.S. and Cincinnati and had the fewest barriers. Previous analysis revealed that Guatemalan immigrants in Cincinnati reported higher barriers to care (only significantly higher for skill barriers) [10]. Despite these findings, immigrants living in the West region utilizing Clinic B (located in the West region) were primarily Guatemalan and had spent the least amount of years in Cincinnati, while having fewer barriers than immigrants utilizing other community health centers. Taken together, these results suggest that a place-based approach is necessary to appropriately target resources and develop appropriate interventions in non-traditional migration areas. Typical interventions focus on Latinos as a homogeneous group or on individuals from a particular country of origin. Our results show that understanding barriers to care and developing appropriate interventions for Latino immigrants require a nuanced understanding of the multiple levels that affect access to healthcare, including geographic regions, neighborhoods, and community health centers.
Table 1.
Characteristics by Regional Grouping
| West | East | North | Total | |
|---|---|---|---|---|
| # of respondents | 227 | 143 | 69 | 439 |
| Mexican (%) | 84 (37) | 97 (66) | 38 (55) | 218 (50) |
| Guatemalan (%) | 112 (49) | 5 (3) | 17 (25) | 132 (30) |
| Years in U.S.*** (Cincinnati)**** |
9.9 (8.0) |
11.8 (9.8) |
10.3 (8.0) |
10.6 (8.7) |
| CHC as Usual Source of Care (%) | 122 (52) | 58 (40) | 41 (58) | 221 (50) |
| No Doctor Visits in Past Year (%) | 71 (34) | 42 (32) | 16 (24) | 129 (32) |
| Pragmatics* (SD) [Range] |
53.2 (24.5) [2.8–100] |
57.4 (26.2) [2.8–100] |
49.8 (21.8) [8.3–100] |
54.1 (24.8) [2.8–100] |
| Costs (% respondents who often or always had problems) | 54.5 | 47.4 | 59.1 | 52.9 |
| Transportation (% respondents who often or always had problems) | 23.1 | 12.9 | 15.9 | 18.7 |
| Availability (% respondents who often or always had problems finding medical attention after hours or on weekends) | 40.8 | 42.7 | 42.0 | 41.6 |
| Skills** (SD) [Range] |
50.5 (29.2) [3.1–100] |
56.2 (27.3) [6.3–100] |
50.7 (24.3) [3.1–100] |
52.6 (27.8) [3.1–100] |
| Language (% respondents who often or always had problems) | 51.6 | 46.1 | 47.8 | 49.2 |
| Understanding Healthcare System (% respondents who often or always had problems) | 40.2 | 36.4 | 31.4 | 36.7 |
| Paperwork (% respondents who often or always had problems) | 48.7 | 38.0 | 42.6 | 44.2 |
SD, Standard Deviation
F(2,430) = 2.63, p=0.07
F(2,415) = 2.42, p=0.09
F(2,436) = 4.94, p=0.01
F(2,430) = 6.46, p=0.002
Table 2.
Characteristics by Neighborhood
| East Price Hill | West Price Hill | Westwood | |
|---|---|---|---|
| # of respondents | 102 | 84 | 41 |
| Mexican (%) | 36 (36) | 31 (37) | 15 (38) |
| Guatemalan (%) | 57 (56) | 40 (48) | 14 (35) |
| Years in U.S. (Cincinnati) |
9.8 (7.9) |
10.2 (8.7) |
9.4 (7.4) |
| CHC as Usual Source of Care (%) | 52 (51) | 49 (58) | 18 (43) |
| No Doctor Visits in Past Year (%) | 36 (37) | 21 (30) | 14 (35) |
| Pragmatics* (SD) [Range] |
57.7 (24.2) [13.9–100] |
50.3 (25.5) [2.8–100] |
48.5 (20.7) [11.1–100] |
| Costs (% respondents who often or always had problems) | 53.0 | 56.1 | 55.0 |
| Transportation (% respondents who often or always had problems) | 20.8 | 24.1 | 26.8 |
| Availability (% respondents who often or always had problems finding medical attention after hours or on weekends) | 32.0 | 45.8 | 52.5 |
| Skills (SD) [Range] |
52.7 (30.1) [3.1–100] |
49.1 (29.9) [3.1–100] |
50.2 (24.2) [3.1–100] |
| Language (% respondents who often or always had problems) | 51.5 | 53.0 | 48.8 |
| Understanding Healthcare System (% respondents who often or always had problems) | 38.8 | 38.3 | 47.5 |
| Paperwork (% respondents who often or always had problems) | 50.5 | 51.2 | 39.0 |
SD, Standard Deviation
F(2,222) = 3.08, p=0.05
Table 3.
Characteristics by Community Health Center (CHC) for West Region Respondents
| Respondents going to a CHC | Respondents going to Clinic A | Respondents going to Clinic B | |
|---|---|---|---|
| # of respondents (from West region) | 119 | 41 | 64 |
| Mexican (%) | 41 (34) | 10 (25) | 21 (33) |
| Guatemalan (%) | 68 (57) | 31 (75) | 35 (55) |
| Years in U.S. (Cincinnati)*** |
9.5 (8.4) |
10.3 (9.9) |
9.0 (7.4) |
| No Doctor Visits in Past Year (%) | 20 (15) | 9 (22) | 10 (16) |
| Pragmatics* (SD) [Range] |
49.6 (23.9) [2.8–100] |
41.8 (26.2) [2.8–100] |
53.3 (21.2) [2.8–100] |
| Costs (% respondents who often or always had problems) | 55.3 | 70.7 | 48.3 |
| Transportation (% respondents who often or always had problems) | 29.3 | 41.5 | 22.6 |
| Availability (% respondents who often or always had problems finding medical attention after hours or on weekends) | 42.7 | 53.7 | 36.7 |
| Skills** (SD) [Range] |
47.5 (28.8) [3.1–100] |
39.3 (27.4) [3.1–100] |
52.2 (29.3) [3.1–100] |
| Language (% respondents who often or always had problems) | 55.6 | 73.2 | 47.6 |
| Understanding Healthcare System (% respondents who often or always had problems) | 39.3 | 46.2 | 36.7 |
| Paperwork (% respondents who often or always had problems) | 55.6 | 65.9 | 50.8 |
SD, Standard Deviation
t(101) = 2.19, p=0.02
t(98) = 2.17, p=0.02
t(94) = 3.43, p=.000
Acknowledgments
Funding
This work was supported by a Community Health Grant from the Center for Clinical and Translational Science and Training, an organization supported by the National Center for Advancing Translational Sciences of the National Institutes of Health, under Award Number UL1TR000077. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Footnotes
Conflict of Interest
Author Topmiller, Author Zhen-Duan, Author Jacquez, and Author Vaughn declare that they have no conflict of interest.
Informed Consent
‘All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000 (5). Informed consent was obtained from all patients for being included in the study.’
Contributor Information
Michael Topmiller, HealthLandscape Division, American Academy of Family Physicians.
Jenny Zhen-Duan, Department of Psychology, University of Cincinnati.
Farrah J. Jacquez, Department of Psychology, University of Cincinnati.
Lisa M. Vaughn, Cincinnati Children’s Hospital Medical Center.
References
- 1.Vissman AT, Bloom FR, Leichliter JS, Bachmann LH, Montano J, Topmiller M, Rhodes SD. Exploring the Use of Nonmedical Sources of Prescription Drugs Among Immigrant Latinos in the Rural Southeastern USA. J Rural Health. 2011;27(2):159–167. doi: 10.1111/j.1748-0361.2010.00323.x. [DOI] [PubMed] [Google Scholar]
- 2.Rhodes SD, Hergenrather KC, Zometa C, Lindstrom K, Montano J. Characteristics of Immigrant Latino Men Who Utilize Formal Healthcare Services: Baseline Findings from the HoMBReS Study. J Natl Med Assoc. 2008;100(10):1177–1185. doi: 10.1016/s0027-9684(15)31476-0. [DOI] [PubMed] [Google Scholar]
- 3.Gresenz CR, Derose KP, Ruder T, Escarce JJ. Health care experiences of Hispanics in new and traditional US destinations. Med Care Res Rev. 2012;69(6):663–678. doi: 10.1177/1077558712457242. [DOI] [PubMed] [Google Scholar]
- 4.Balluz LS, Okoro CA, Strine TW, National Center for Chronic Disease Prevention and Health Promotion Access to health-care and preventive services among Hispanics and non-Hispanics – United States, 2001–2002. JAMA. 2004;292:2331–2333. [Google Scholar]
- 5.Escarce JJ, Kapur K. Access to and Quality of Health Care. In: Tienda M, Mitchell F, editors. Hispanics and the Future of America. National Academies Press; 2006. [PubMed] [Google Scholar]
- 6.Engstrom DW. Outsiders and exclusions: Immigrants in the United States. In: Engstrom DW, Piedra LM, editors. Our diverse society: Race and ethnicity – Implications for 21st century American society. Washington DC: NASW Press; 2006. [Google Scholar]
- 7.Waters MC, Jimenez TR. Assessing immigrant assimilation: New empirical and theoretical challenges. Ann Rev Sociology. 2005;31:105–125. [Google Scholar]
- 8.Perez DJ, Fortuna L, Alegria M. Prevalence and correlates of everyday discrimination among US Latinos. J Comm Psych. 2008;36:421–433. doi: 10.1002/jcop.20221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jacquez F, Vaughn LM, Pelley T, Topmiller M. Healthcare experiences of Latinos in a nontraditional destination area. J Community Pract. 2015;23(1):76–101. [Google Scholar]
- 10.Jacquez FM, Vaughn LM, Zhen-Duan J, Graham C. Healthcare Utilization and Barriers to Care among Latino Immigrants in a New Migration Area. J Healthcare Poor Underserved. doi: 10.1353/hpu.2016.0161. in press. [DOI] [PubMed] [Google Scholar]
- 11.Kenney GM, Huntress M. The Affordable Care Act: Coverage Implications and Issues for Immigrant Families. Urban Institute ASPE Issue Brief. 2012 Apr; [Google Scholar]
- 12.U.S. Census Bureau. (2014 American Community Survey 5-Year Estimates).Cincinnati Metropolitan Area, Ohio-Kentucky-Indiana; DP03 Selected Social Characteristics [Data] http://factfinder.census.gov/faces/nav/jsf/pages/searchresults.xhtml?refresh=t [April 12, 2016]
- 13.U.S. Census Bureau. (2010 Decennial Census).Cincinnati Metropolitan Area, Ohio-Kentucky-Indiana; SF1 100% [Data] 2000 http://factfinder.census.gov/faces/nav/jsf/pages/searchresults.xhtml?refresh=t [April 7, 2016]
- 14.U.S. Census Bureau. (2014 American Community Survey 5-Year Estimates).Hamilton County, Ohio; DP03 Selected Social Characteristics [Data] http://factfinder.census.gov/faces/nav/jsf/pages/searchresults.xhtml?refresh=t [April 12, 2016]
- 15.Gassoumis ZD, Wilber KH, Baker LA, Torres-Gil FM. Who are Latino baby boomers? Demographic and economic characteristics of a hidden population. J Aging Soc Policy. 2009;22(1):53–68. doi: 10.1080/08959420903408452. [DOI] [PubMed] [Google Scholar]
- 16.Zandvakili S, Passty B, von Hofe R, Mueller A. Economic Impact of Hispanic Community in the Cincinnati MSA. Cincinnati: University of Cincinnati; 2010. [Google Scholar]
- 17.U.S. Census Bureau. (2014 American Community Survey 5-Year Estimates).Hamilton County, Ohio, Census Tracts; DP03 Selected Social Characteristics [Data] http://factfinder.census.gov/faces/nav/jsf/pages/searchresults.xhtml?refresh=t [April 12, 2016]
- 18.U.S. Department of Health and Human Service. (Health Care Service Delivery and Look-Alike Sites Data Download [Data]).HRSA Data Warehouse. 2016 http://datawarehouse.hrsa.gov/data/datadownload/hccdownload.aspx [May, 2016]
- 19.Blewett LA, Smaida SA, Fuentes C, Zuehlke EU. Health care needs of the growing Latino population in rural America: Focus group findings in one midwestern state. J Rural Health. 2003;19(1):33–41. doi: 10.1111/j.1748-0361.2003.tb00539.x. [DOI] [PubMed] [Google Scholar]
- 20.Cristancho S, Garces DM, Peters KE, Mueller BC. Listening to rural Hispanic immigrants in the Midwest: A community-based participatory assessment of major barriers to health care access and use. Qual Health Res. 2008;18(5):633–646. doi: 10.1177/1049732308316669. [DOI] [PubMed] [Google Scholar]
- 21.Ortega AN, Rodriguez HP, Bustamente AV. Policy dilemmas in Latino health care and implementation of the Affordable Care Act. Annu Rev Public Health. 2015;36:525–544. doi: 10.1146/annurev-publhealth-031914-122421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sommers BD. Stuck between Health and Immigration Reform – Care for Undocumented Immigrants. N Engl J Med. 2013;369(7):593–595. doi: 10.1056/NEJMp1306636. [DOI] [PubMed] [Google Scholar]
- 23.Applebaum B, Robbins S. Language Access and Health Equity: Changes under the Affordable Care Act. J Healthcare Poor Underserved. 2016;27(2):416–426. doi: 10.1353/hpu.2016.0064. [DOI] [PubMed] [Google Scholar]
- 24.Schreier HMC, Chen E. Socieconomic status and the health of youth: A multilevel, multidomain approach to conceptualizing pathways. Psychol Bull. 2013;139(3):606–654. doi: 10.1037/a0029416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dankwa-Mullen I, Perez-Stable EJ. Addressing Health Disparities is a Place-Based Issue. Am J Public Health. 2016;106(4):637–639. doi: 10.2105/AJPH.2016.303077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Edward J, Biddle DJ. Using Geographic Information Systems (GIS) to Examine Barriers to Healthcare Access for Hispanic and Latino Immigrants in the U.S. South. J Racial Ethn Health Disparities. 2016:1–11. doi: 10.1007/s40615-016-0229-9. [DOI] [PubMed] [Google Scholar]
- 27.Dulin MF, Tapp H, Smith HA, De Hernandez BU, Furuseth OJ. A community based participatory approach to improving health in a Hispanic population. Implement Sci. 2011;6(1):38. doi: 10.1186/1748-5908-6-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dulin MF, Tapp H, Smith HA, Urquieta de Hernandez B, Coffmann MJ, Ludden T, Sorensen J, Furuseth OJ. A trans-disciplinary approach to the evaluation of social determinants of health in a Hispanic population. BMC Public Health. 2012;12:769. doi: 10.1186/1471-2458-12-769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Vaughn LM, Jacquez FM, Zhen Duan J, Graham C, Marschner D. Improving Research Quality and Reaching a Hidden Population through an Immigrant Community Research Team. Collaborations: A Journal of Community-Based Research and Practice. under review. [Google Scholar]
- 30.Seid M, Opipari-Arrigan L, Gelhard LR, Varni JW, Driscoll K. Barriers to care questionnaire: Reliability, validity, and responsiveness to change among parents of children with asthma. Acad Pediatr. 2009;9(2):106–113. doi: 10.1016/j.acap.2008.12.003. [DOI] [PubMed] [Google Scholar]
- 31.U.S. Census Bureau. (2014 American Community Survey 5-Year Estimates).Hamilton County, Ohio, Zip Code Tabulation Areas (ZCTAs); DP03 Selected Social Characteristics [Data] http://factfinder.census.gov/faces/nav/jsf/pages/searchresults.xhtml?refresh=t [December 12, 2016]
- 32.Eiler BA, Bologna DA, Vaughn LM, Jacquez FM. A social network analysis of Latino service providers in a new migration area. J Community Psychol. in press. [Google Scholar]
- 33.Raffaelli M, Wiley AR. Challenges and Strengths of Immigrant Latino Families in the Rural Midwest. J Family Issues. 2013;34(3):347–372. [Google Scholar]
- 34.Rhodes S, Long Foley K, Zometa CS, Bloom FR. Lay Health Advisor Interventions Among Hispanics/Latinos: A Qualitative Systematic Review. Am J Prev Med. 2007;33(5):418–427. doi: 10.1016/j.amepre.2007.07.023. [DOI] [PubMed] [Google Scholar]


