Abstract
The purpose of this systematic review was to determine whether nurse-delivered weight management interventions improve weight outcomes across the lifespan. We conducted a comprehensive search of the PubMed, CINAHL, and PsycINFO electronic databases. We graded the trials using an adapted Jadad approach for methodological quality. The search identified a total of 1,159 citations; 23 articles from 20 studies were eligible for this review. Sixty-five percent of the studies reported significant findings related to body mass index (BMI) or weight reduction. Studies that were particularly successful at helping participants reduce weight and/or BMI involved nurses engaged in health promotion activities, operating within multidisciplinary teams and/or providing consultations, physical activity education, and coaching over the phone. Of the studies that involved longer-term follow-up assessments, three out of nine studies showed a significant loss in weight or BMI between the intervention and control groups at follow-up times ranging from 12 months to 2 years.
Keywords: nurse-delivered, weight management, weight loss, weight-loss maintenance, randomized controlled trials
Living a healthy lifestyle, namely exercising and increasing the consumption of whole fruits and vegetables, is essential to managing weight and preventing chronic disease U.S. Department of Health and Human Services and U.S. Department of Agriculture, 2015; Karfopoulou et al., 2016). With obesity doubling in its global prevalence over the last four decades, there is a tremendous threat to a rise in the incidence of heart disease, diabetes, and some cancers (World Health Organization [WHO], 2015). At least 2.8 million adults die every year as a result of being overweight or obese (WHO, 2015). Therefore, weight loss, which has been shown to improve heart health and diabetes, is necessary to improve morbidity and mortality (Wilson, DeJoy, Vandenberg, Padilla, & Davis, 2016). Lifestyle change interventions have been shown to provide a pragmatic, long-term and cost-effective solution for weight loss (Bogers et al., 2010; Curioni & Lourenço, 2005; Douketis, Macie, Thabane, & Williamson, 2005; Franz et al., 2007). The health care setting is typically the first place people receive lifestyle counseling after an unfavorable diagnosis. However, due to the rise in obesity and consequently chronic disease coupled with a shortage of primary care physicians, the health care system is experiencing a tremendous burden of care (Association of American Medical Colleges, 2012). Within their scope of practice, nurses can play a vital role in alleviating this burden by providing targeted health assessments, expanding their role in chronic disease management and providing evidence-based lifestyle education, counseling, and coaching (Berkowitz, 2009; Lazarou & Kouta, 2010). A systematic review conducted in 2010 examined the effect of primary health care nurse-delivered lifestyle interventions on chronic disease risk factors (between 1976–2010) and found that nurses were effective in influencing a positive change in factors such as blood pressure, cholesterol, weight and physical activity (Sargent, Forrest, & Parker, 2012). To our knowledge, there has not been a recent review that focuses solely on nurse-delivered interventions to improve weight or BMI. Hence, the purpose of this systematic review is to determine if nurse-delivered weight management interventions improve weight outcomes across the lifespan. Since the adult population became heavier between 2005 and 2006 than in previous years and was its heaviest since the 80s (Ogden, Carroll, McDowell, & Flegal, 2007), we examined literature reflecting the past ten years of published research related to nurse-led interventions in weight management research.
In this review, weight management research is defined as research involving weight loss or weight loss maintenance interventions with the desired goal of improving weight. A weight loss intervention is any type of intervention strategy in which the goal is to decrease weight (lbs/kg) or Body Mass Index (kg/m2). A weight loss maintenance intervention is any non-intensive strategy in which its purpose is to maintain improved weight outcomes.
We defined nurse-delivered interventions as any intervention (i.e. weight loss counseling, coaching, teaching, etc.) in which nurses, regardless of the type of nurse, has a direct role in delivering the intervention to research participants in which improved weight outcomes are the desired goals. They may operate alone or within a multidisciplinary team.
Methods
Search Strategy and Eligibility Criteria
We searched the following electronic databases for relevant articles published in English between 2006 and 2016: MEDLINE via PubMed, CINAHL via EBSCOhost, and PsycINFO via EBSCOhost. We used the keywords and controlled vocabulary terms in the following concept groups (Nurse OR Nurse-directed OR Nurse-led OR nurse-managed) AND (Weight OR Weight loss OR Weight loss maintenance, OR Weight regain) AND (Clinical Trials OR Randomized Controlled Trials) to identify candidate studies for review. The final search for each database was conducted on March 28th, 2016. The complete search strategy can be found in the online resource for this manuscript. Studies were eligible for inclusion if they were randomized controlled trials that consisted of weight loss or weight loss maintenance interventions delivered by nurses. Additionally, the primary outcomes had to be related to weight or Body Mass Index (BMI). We excluded pilot or feasibility studies (self-described or sample size < 50 without power calculations).
Screening Process
Each retrieved title and abstract were independently screened by at least two authors to determine eligibility (from LPF, ES, and RATO). Any discordant reviews concerning eligibility were discussed, and if disagreement persisted, a third and sometimes fourth author (JA) resolved the disagreement. If the identification of research staff delivering the intervention was unclear after screening the titles, abstracts, and occasional full-text, emails were sent to corresponding authors to seek clarification on the identity of research staff delivering the intervention to ensure that our eligibility requirement for nurse-delivered (nurses, regardless of the type of nurse, who have a direct role in delivering the intervention to research participants) was met. If there was not a response within two weeks or the author replied no to any nurse involvement in the intervention, we deemed the article ineligible.
Data Abstraction and Quality Assessment
Articles identified for full-text review were examined by at least two independent raters (LPF, ES, RATO). We recorded information on each study’s authors, year of publication, country, sample characteristics (sample size, mean age, % women and % minority), and description of the intervention, retention rate, and results. Studies were graded for methodological rigor using a modified Jadad scoring strategy. The Jadad is comprised of four questions including whether the strategy for randomization was described and appropriate, whether the study had a thorough description of withdrawals and dropouts, whether intent-to-treat analysis was used and if there was a justification of the sample size. A score of 1 was given if the study met the respective criterion. Therefore, the possible range for the quality score was from 0 to 4, with a score of 4 indicating a stronger likelihood of the trial design to engender unbiased results (Allen & Dennison, 2010).
Results
Results of the search
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guideline provided the structure for the flow of articles throughout the review process and is shown in Figure 1 (Moher, Liberati, Tetzlaff, Altman, & The PRISMA Group, 2009). A total of 1,159 records were identified from the three databases searched. Two-hundred and thirty-four duplicate records were removed, and the titles and abstracts of the remaining 925 records were screened for eligibility by at least two independent reviewers. Additionally, eight emails were sent to corresponding authors to seek clarification on the identity of research staff. Of the eight emails, 2 responded no nurse involvement in the intervention and the remaining six did not provide a response. Of the 925 records, 45 records were identified for full-text review. Twenty-two articles were excluded, and 23 articles were included in the systematic review. The 23 articles eligible for inclusion reported results from 20 studies.
Figure 1.
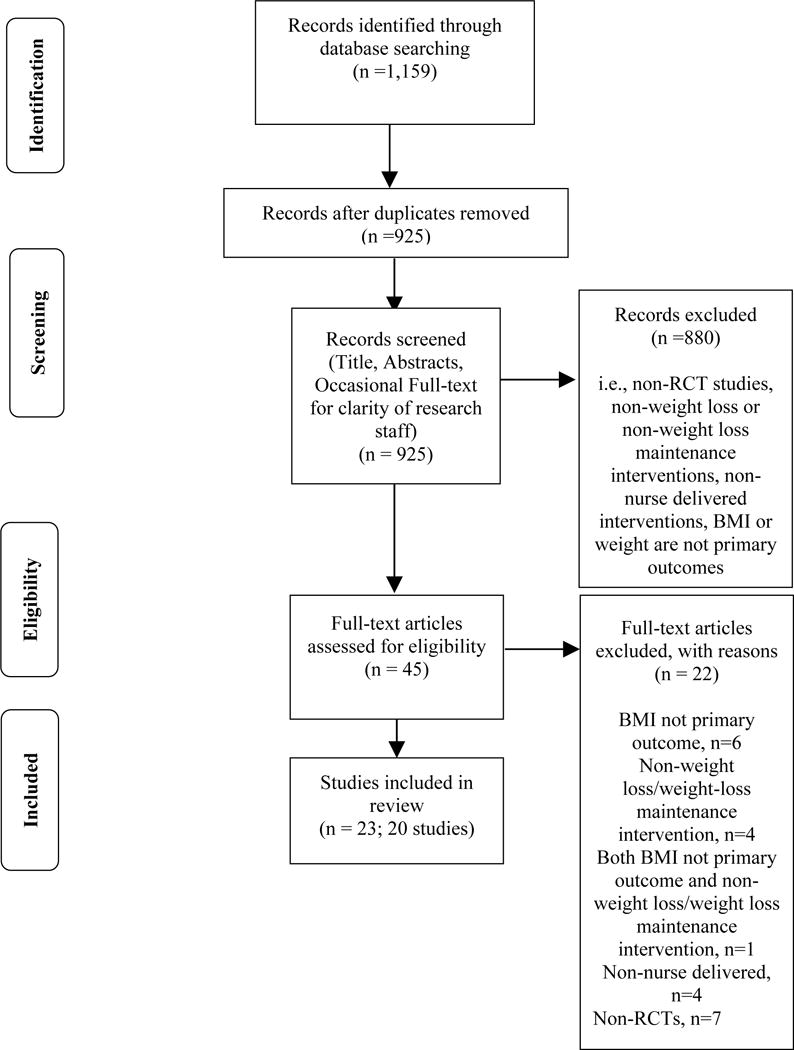
Preferred Reporting Items for Systematic Reviews and Meta-analyses diagram depicting the flow of records.
Note. BMI = Body mass index; RCT = Randomized Controlled Trial
Overview of study populations
The results abstracted from the studies are summarized in Table I. Total sample sizes ranged from 60 to 3,059 participants. Most studies included both men and women. Of the 18 studies that reported sex composition, half of the studies had less than 50% women represented in their sample with the studies ranging from 5.4% to 100%. One study reported having a 100% female sample (Valve et al., 2013). Three studies reported results by sex (Drevenhorn, Bengtson, Nilsson, Nyberg, & Kjellgren, 2012; ter Bogt et al., 2009, 2011; Wright, Giger, Norris, & Suro, 2013). Ages ranged from 3 years to late 60’s representing preschoolers to late adulthood. Of the studies that reported mean ages or age ranges, 30% of the studies included children and adolescents aged 2–19 years and 70% of the studies had participants in their middle to late adulthood years (40–65+ years). Only one study reported results by age category (Lemon et al., 2014). Most studies (70%) were conducted outside of the United States. Of those non-US studies, half are from Nordic countries and the Netherlands. Twelve studies did not report sample characteristics based on race and ethnicity with two reporting information only on nationality. Of the studies that reported minority (non-white) involvement, 78% reported less than 50% minority involvement. The average percent minority involvement was 38% with a range of 4.1 to 100%. One study had 100% minority participation (Wright et al., 2013). No studies reported results by race or ethnicity.
Table I.
Study Characteristics and Results of Included Studies
| Citation Year, Country | Population & Sample Sizes (%female & minority) |
Intervention & Control | Retention Rate | Primary Clinical Outcome Measure & Results | Scientific Quality Score |
|---|---|---|---|---|---|
| Children and Adolescents (2–19 years) | |||||
|
| |||||
| Alkon et al., 2014, United States of America | Children: N=552; age 3–5 yrs. I=260; 44% female C=292; 48% female Parents: N=549 I=258; 45% non- white C=291;63% non- white Child Care Providers: N=137 I=76; 55% non- white C=61; 51% non- white (46% children female, 54% parents & 53% providers non- white) |
Setting: Licensed Child Care Centers I: The Nutrition and Physical Activity Self - Assessment for Child Care (NAP SACC): educational nutrition & PA workshops for child care providers & parents and consultation visits by trained nurse child care consultant (7 mos.) C: Received delayed NAP SACC intervention in yr. two of study |
Children: Overall=38% (209/552) I=38% (99/260) C=38% (110/292) Center: Overall=94% (17/18) I=100% (9/9) C=89% (8/9) |
Child zBMI at 7 mos. Pre & Post Intervention zBMI: I:0.75(0.98) kg/m2 & 0.71(0.96) kg/m2, (P=0.79) C:0.61(0.93) kg/m2 & 0.67(0.98) kg/m2, (P=0.66) Sig. diff. in mean child zBMI changes btw intervention & control centers: −0.14(0.06) kg/m2, (P =0.02) controlling for state, parent education & family poverty No sig. changes in intervention or control across BMI categories |
2 |
|
| |||||
| Fulkerson et al., 2015, United States of America | N=160 children; mean age 10.3(1.4) yrs. I=81 C=79 (48% female, 29% non-white) |
Setting: Home I: HOME Plus: 10 monthly family group sessions (nutrition education; meal & snack planning, preparation, & skill dev.; screen time reduction) delivered by registered dietitians & a public health nurse & 5 motivational goal-setting phone calls delivered by registered dietitians (12 mos.) C: Monthly family-focused newsletter |
Overall=89% (143/160) I=86% (70/81) C=92% (73/79) |
Child zBMI post-intervention Mean BMI diff. btw groups: Post intervention (12 mo.): 0.03(0.04) kg/m2, (P=0.43) Follow-up (21 mo.): 0.07 (0.05) kg/m2, (P=0.210) |
4 |
|
| |||||
| Kokkvoll et al., 2015, Norway | N=97 I=48; age 10(1.7) yrs, 60% female C=49; age 10.5 (1.7) yrs, 48% female (54% female, no info. provided on race/ethnicity) |
Setting: Inpatient & Community I: Multiple-family intervention (MUFI): 3 day inpatient program w/ other families & care team (public health nurse, physiotherapist & coach), individual & group follow-up visits in hometown, organised group PA 2x/wk, & 4 day family camp post 6 mos. C: Single-family intervention (SIFI): individual inpatient counselling by pediatric nurse, consultant, & nutritionist & follow-up by public health nurse in community |
Overall=81% (79/97) I=87.5% (42/48) C=75.5% (37/49) |
Change in BMI & BMI Standard Deviation score at 2 yr. follow-up BMI: I:1.29 (0.74,1.84) kg/m2 C: 2.02 (1.44, 2.60) kg/m2 No diff. in BMI btw groups: −0.73 (−1.53, 0.07) kg/m2; group by time (P=0.075) BMI Standard Deviation score: I: −0.20 (−0.29, −0.12) C: −0.08 (−0.17, 0.01) Moderately sig. diff. in BMI SDS btw groups: −0.12 (−0.24, 0.00); at 24 mos. group by time (P=0.046) |
3 |
|
| |||||
| Valve et al., 2013, Finland | N=3,059 I=1,537, 8 centers; median age 19 yrs. (17–21) C=1,522, 7 centers, median age 19 yrs. (17–20) (100% female, 100% Finnish, no info provided on race/ethnicity) |
Setting: Community Vaccination centers I: LyhytINterventio DAameille (LINDA) Finnish for “brief intervention for ladies”:Control + 20 min. individualized lifestyle coaching (PA, dietary, & sleeping behaviors) from study nurses w/ support every 6 mos. at follow-up visits C: Sexual health & contraception counseling from study nurses |
Overall=88% (2,687/3,059) I=87.8% (1,349/1,537) intent-to-treat analysis I=71% (957/1,537), analyzed for BMI C=87.9% (1,338/1,522) |
BMI & Percentage of BMI Class Change Intention-to-treat analyses Median BMI: I: 0.55(1.59) kg/m2 C: 0.51(1.75) kg/m2 No sig. diff. by BMI class (P=0.769) Per protocol analyses Median BMI: I: 0.52 (1.53) kg/m2 C: 0.51 (1.75) kg/m2 No sig. diff. by BMI class (P=0.996) |
2 |
|
| |||||
| Wright et al., 2013, United States of America | N=305, ages 8–12 yrs I=165, 2 schools; 58% girls,100% minority C=140, 3 schools; 62% girls, 100% minority (60% female, 100% minorities) |
Setting: Elementary schools in urban low income neighborhoods I: Kids N Fitness©, 6 wk., nurse coordinated, culturally-sensitive, school health program. Two components: family-centered & environmental. Family-centered: wkly 45 min. structured PA for kids + 45 min. nutrition education class for parents & children conducted by a registered nurse, community health worker & physical education specialist Environmental: additional activities includes staff professional development, health & mental services and parental outreach via bi-monthly educational newsletters C: General Education - standard PA program given by their respective schools. No nutrition or PA education. |
Overall=80% (244/305) I=82% (135/165) C=78% (109/140) |
BMI & zBMI changes from baseline to 12 mo. follow-up Girls: BMI: I: −3.65 (−5.81, −1.78) kg/m2 C: 1.23 (−4.12, 3.41) kg/m2 (P=0.047) zBMI: I: −0.70 (−1.00, −0.40) C: 0.58 (−1.82, 1.59) (P=0.05) Boys: BMI: I: −2.56 (−4.31, −1.25) kg/m2 C: 1.35 (−5.01, 4.10) kg/m2 (P=0.15) zBMI: I: −0.19 (−0.38, 1.01) C: 0.79 (−1.92, 1.85) (P=0.781) |
2 |
| Middle to Late Adulthood (40+ years) | |||||
| Anderson, Mizzari, Kain, & Webster, 2006, Australia | N=113; 61% age 55–60 yrs. I=47 C=66 (100% female, no info. provided on race/ethnicity) |
Setting: Outpatient I:Cognitive-behavioral intervention: 40 min. consultations w/ a registered nurse on positive lifestyle changes & goal-setting to decrease CVD risk factors. Received books & journals: The Menopause Made Simple Program & The Women’s Wellness Program Journal including a personal journal w/ daily or weekly focus points, A weekly Exercise planner to plan exercise ahead of time & a Daily Diet and Exercise Record to record exercise activities & food content (12 wks) C: Continue normal daily activities |
Overall= 81% (92/113) I=77% (36/47) C=85% (56/66) |
BMI Change of Intervention Group at 12 wks. Change in BMI: 0.37(0.94) kg/m2, (P=0.02) |
2 |
| Andryukhin et al.,, 2010, Russia | N=100; mean age 67 yrs. I=50; 72.7% female C=50; 65.8% female (69.4% female, no info. provided on race/ethnicity) |
Setting: Clinical; Primary Care Practice I: Nursing Program: Educational Program: 4 (90 min) wkly educational sessions on individual lifestyle changes & modification of heart disease risk factors taught by nurses (mo. 1) Exercise Training: 4 (30 min) sessions w/ physiotherapist to develop & encourage the use of an individualized home training program (mo. 2–6) Proactive and Supportive Nursing Care: wkly (15–30 min) consultations discussing challenges, checking for medication compliance & health assessment (mo. 2–6) C: Usual Care- prescription of meds & basic education on diet, alcohol intake, weight reduction, smoking cessation & PA |
Overall=75% (75/100) I=80% (40/50) C=70% (35/50) |
BMI at 6 mos. Pre-intervention BMI: I: 30 (28.8, 32) kg/m2 C: 30 (28.4, 31.3) kg/m2 Post Intervention BMI: I: 29.5 (28.2, 31.6) kg/m2 C: 29 (28.3, 31.2) kg/m2 Improvement in BMI: I: n=31 C: n=18 More participants in intervention than control group had a positive change in BMI (P=0.034) |
3 |
|
Brown et al., 2011, United States of America Brown et al., 2014, United States of America |
N=136; age 44.65(10.9) yrs, 45% female I=70; age 44.4 (11.7) yrs, 64% female, 40% non-white C=66; age 44.9 (10.1) yrs, 70% female, 41% non-white By site Urban sites(1&3): (16% female, 13.2% non- white) Suburban sites (2&4): (16.9% female, 7.4% non-white) |
Setting: Urban & Suburban Community Mental Health programs I: Multi-site (4), Recovering Energy Through Nutrition & Exercise for Weight Loss (RENEW): education & practice in modifying nutrition & PA (12 mos.) Intensive Phase: 3 hr wkly session delivered by graduate-trained nurse, occupational therapist, or dietician on nutrition education, partaking in PA, goal setting, & skill acquisition. Meal replacements 2× daily(1–3 mos.) Maintenance Phase: one 3 hr. monthly session & wkly phone support; no meal replacements(4–6 mos.) Intermittent support phase: feedback, reminders & support (wkly phone calls & monthly mailings w/ tips, reminders & encouragement) (7–12 mos.) C: Usual Care- medication & case management and voluntary participation in center wellness programs |
At 6 mos.: Overall=65% (89/136) I=67% (47/70) C=64% (42/66) At 12 mos: Overall=68% (92/136) I=67% (47/70) C=68% (45/66) |
Mean Weight Results at Baseline, 3, 6, & 12 mos: Baseline: I: 224.5(41.9) lbs C: 241.8(60.2) lbs *3 mos: I: 219.2(40.8) lbs C: 241.9(60.6) lbs Sig. diff. btw groups (F=6.936, P=0.01) *6 mos: I: 220.1(43.3) lbs C: 240.9(60.5) lbs Non sig. diff. btw groups (F= 1.526, P=0.22) 12 mos: I: 225.7(45.6) lbs C: 240.3(55.8) lbs Non sig. diff. btw groups (F= 0.522, P=0.47) *2014 article have slightly diff. mean weight results at 3 & 6 mos. Intervention lost more weight on average than control group at 3 mos. (−5.3 lbs vs. 0.1 lbs) & 6 mos. [−4.4 lbs vs. −0.9 lbs (F=5.74, df=2 & 82, P=.005)] I: 32% (n=15) of participants lost >10 lbs C: 10% (n=4) of participants lost >10 lbs Site Differences: Sig. interaction at 3 mos. (F=3.36, P=0.017) & 6 mos. F=2,831, P=0.043) Diff. in pattern of weight change for urban vs. suburban sites at 12 mos.: Urban sites (1&3): mean weight loss −10 lbs & −6.6 lbs, respectively Suburban sites (2&4): mean weight gain 18.6 lbs & 3.6 lbs, respectively Sig. diff. for time (F=7.329, P<.001) & sig. diff. for interaction btw time & site (F=3.36, P= 0.029) Urban sites (1&3): 3 mos: −9.4lbs 6 mos: −10.9 lbs 12 mos: −7lbs Suburban sites (2&4): 3 mos: −0.8 lbs 6 mos: +2.9 lbs 12 mos: +9.5 lbs |
2 |
| Drevenhorn et al., 2012, Sweden | N=210 patients *I=152 (153) *C=58 (60) (no info. provided on race/ethnicity) *Flow diagram & text are at odds |
Setting: Not adequately described I: Multifactorial tailored education for nurse on patient centeredness, CVD prevention, Stages of Change, Motivational Interviewing, lifestyle factors & pharmacological treatment (2 yrs.) C: Usual Care |
Overall=89.5% (188/210) I=90% (137/152) C=88% (51/58) |
BMI & Weight for Intervention Group BMI Baseline mean: I: 31.4(4.3) kg/m2, (30.7,32.1) BMI 2yr mean: I: 30.9(4.4)kg/m2, (30.2,31.7) Weight Baseline mean: I: 93.3(15.9) kg, (90.6,95.9) Weight 2 yr mean: I: 92(16) kg, (89.3,94.7) Decrease in BMI & weight at 2 yrs. w/in the intervention group (P<0.001) Decrease in BMI & weight at 2 yrs. for men & women: Men: Weight baseline mean: I: 99.5(15.7) kg Weight 2 yr mean: I: 98.1(15.2) kg, (P=0.009) BMI baseline mean: I: 31.2(4.2) kg/m2 BMI 2 yr mean: I: 30.8(4.3) kg/m2, (P=0.010) Women: Weight baseline mean I: 84.9(13.1) kg Weight 2 yr mean: I: 83.6(13.1) kg, (P=0.016) BMI baseline mean I: 31.7(4.6) kg/m2 BMI 2 yr mean: I: 31.2(4.6) kg/m2, (P=0.019) |
2 |
| Gallagher et al., 2012, Australia | N=148*; age 63.47(8.9) yrs. I=83; age 63.71 (8.16) yrs., 37% female, 17% non-white C=65, age 63.28 (9.49) yrs., 45% female, 26% non-white (41% female, 21% non-white) *paper reports 147 |
Setting: Outpatient Cardiac Rehab I: Healthy Eating & Exercise Lifestyle Program (HEELP): supervised exercise by exercise physiologist & info. and group support sessions delivered by cardiac rehab clinical nurse consultant & other team members on exercise, nutrition, & behavior change (16 wks.) C: Info. on hospital/ community programs; delayed intervention post 16 wks. |
Overall=*90% (133/148) I=**90% (75/83) C=89% (58/65) paper reports *91% & **87% |
Mean Weight & BMI Change at 16 wks. Weight: I: −2.19(3.16) kg C: −0.13(2.08) kg Mean diff. btw groups: 2.06 kg, (P<.001) BMI: I: −0.74(1.11) kg/m2 C: −0.06(.76) kg/m2 Mean diff. btw groups: 0.68 kg/m2, (P<.001) |
3 |
| Goodman et al., 2008, United Kingdom | N=183; mean age 64.8 yrs. I=90; 23.4% female C=93; 14% female (18.7% female, no info. provided on race/ethnicity) |
Setting: Home Care I: Nurse-led support & education program including monthly pre-op. appointment w/ homecare nurse involving cardiac risk assessment, counseling on lifestyle changes to affect BP, BMI, cholesterol, address questions & concerns of operation C: Standard/Usual Care: hospital helpline & a pre-surgery info. day |
Overall=*100%, although 6 died postoperative *not clear on true retention rate because intent- to-treat analysis was used as rationale for 100% retention |
Mean Change in BMI I: −0.16(1.48) kg/m2, (P=0.32) C: −0.08(1.27) kg/m2, (P=0.57) Mean diff. btw groups: −0.05 kg/m2, (P=0.70) |
4 |
| Hacihasanoǧlu & Gözüm, 2011, Turkey | N=130; age 56.8 (8.5) yrs. Intervention A (IA) =43; 50% female Intervention B (IB) =43; 50% female C=44; 55% female (52% female, no info. provided on race/ethnicity) |
Setting: Primary Health Care Facilities & at Home I: Six monthly education sessions on medication adherence & lifestyle changes delivered by a nurse (4 clinic visits & 2 home visits). (6 mo) Intervention A (IA): Medication Adherence Education + ask questions about general health related to healthy lifestyle behaviors (nutrition, weight loss, exercise, etc.) & general info on HTN Intervention B (IB): Medication compliance, Specific Healthy Lifestyle Education (nutrition, relevant diet, importance of reduced salt intake, dealing w/ stress, weight control, exercise, risks of alcohol & smoking, etc.) & general info. on HTN C: 6 interviews after pretest, only BP & weight measurements collected (no education) |
Overall=92% (120/130) IA=93% (40/43) IB=93% (40/43) C=91% (40/44) |
BMI For BMI, no diff. btw IA & IB nor btw IA & C; sig. diff. btw IB & C (P<0.05) Pre & Posttest BMI: IA: 25.27(2.87) kg/m2 & 24.42 (2.81) kg/m2, (t=12.302, P=0.000) IB: 25.62(2.87) kg/m2 & 24.26 (2.76) kg/m2, (t=20.222, P=0.000) C: 26.07(4.09) kg/m2 & 26.04 (4.21) kg/m2, (t=0.274, P=0.786) Mean diff. in BMI across groups: Pre-test: IA: 25.27(2.87) kg/m2 IB: 25.62 (2.87) kg/m2 C: 26.07(4.09) kg/m2 (F= 0.581, P=0.561) Post-test: IA: 24.42(2.81) kg/m2 IB: 24.26(2.76) kg/m2 C: 26.04(4.21) kg/m2 (F=3.478, P= 0.034) |
4 |
| Hesselink et al., 2015, Netherlands | N=366, 26 primary care practices; 45+ yrs. I=197, 11 practices; age 62.4(9.8) yrs., 46.8% female C=169, 11 practices; age 65.1(9.7) yrs., 46.5% female (46.7% female, no info. provided on race/ethnicity) |
Setting: Rural Primary Care Practices I: “Road map towards diabetes prevention” protocol-Nurse-led consultations (assessment, coaching, motivational interviewing, referrals) w/ aim to improve PA & dietary habits [1 year + 1 year follow-up (Usual Care)] C: Usual care- people w/ impaired fasting glucose (IFG) should be tested for diabetes every year.; Usual Care is not structured for patients w/ IFG but w/o HTN or dyslipidemia |
Overall=78% (286/366) I=81% (160/197) C=75% (126/169) |
Change in BMI & Weight at 2 yrs. (BMI primary & weight secondary) Intervention & control groups exhibited reduction in BMI, but no sig. diff. btw groups post intervention (1 yr.) or at follow-up (2 yr.) Change (baseline to 2 yrs.): BMI: I: −0.6(4.9) kg/m2 C: −0.3(5.3) kg/m2 Weight: I: −1.4(16) kg C: −1.1(18.3) kg Btw group diff. at 2yrs.: BMI: −0.98 (−2.23,0.28) kg/m2 Weight: −0.46 (−1.86, 0.94) kg |
4 |
| Leemrijse et al., 2016, Netherlands | N=374; age 60.4(10.2) yrs. I=173; age 61.0 (10.0) yrs., 21.4% female C=201; age 60.0 (10.4) yrs., 16.9% female (19% female, 16.8% non- Dutch) |
Setting: Medical Call Center/Over telephone I: 20–30 min. telephone coaching by nurses every 4–6 wks. on lifestyle modification (healthy dietary & exercise behavior), goal- setting, planning, self- monitoring & feedback + Usual Care for CVD (6 mos.) C: Usual care- visits to a cardiologist, cardiac nurse, general practitioner, physical therapist, & dietician. May include cardiac rehab. |
Overall=88.5% (331/374) I=91.3% (158/173) C=86.1% (173/201) |
Adjusted Mean Change in BMI Baseline BMI: I: 27.3 (3.71) kg/m2 C: 27.7 (4.20) kg/m2 6 mo. BMI: I: 27.3(3.54) kg/m2 C: 28(4.34) kg/m2 Adj. mean change in BMI: −0.32 (−2.73, −0.70) kg/m2, (P= 0.048) |
3 |
| Lemon et al., 2014, United States of America | N=841* employees, 12 schools; 49.6% 45+ yrs I=482, 6 schools; 70.2% female C=359, 6 schools; 62.8% female (67.0% female, 4.1% non-white) *Paper reports 782 |
Setting: Schools I: Multi-level intervention targeting the individual, interpersonal & organizational (school) coordinated by predominantly by school nurses. Organizational: focus on political & environment aspects of school (i.e. access to fitness facilities, healthy lunch options, etc.). Interpersonal: social environment interventions (i.e. walking groups, healthy potluck meals, etc.) Individual: periodic health promotion displays, healthy food tastings, & weight challenges. Print & electronic materials provided; 1 & 2 year follow-up C: Print & electronic materials related to healthy eating, physical activity, & weight management. |
Overall=76.1% (640/841) I=73.4% (354/482) C=80% (286/359) |
Diff. in Mean Weight Loss & BMI at 24 mos. Baseline Weight: I: 173.9 lbs. C: 173.9 lbs. 24 mo. Weight: I: 172.6 lbs. C: 176.1 lbs. Sig. diff. in net change in weight loss btw groups: −3.03 (−5.85, −0.22) lbs., (P=0.04) Moderately sig. mean diff. in net change in BMI btw groups: −0.48 BMI kg/m2, (P=0.05) Sig. diff. for participants aged 35–44 yrs.: −5.4 lbs., (P=0.05) |
3 |
|
ter Bogt et al., 2009, Netherlands ter Bogt et al., 2011, Netherlands |
N=457 overweight or obese patients; mean age 56 yrs., 52% female I=225; mean age 55.3 yrs., 49.8% female C=232; mean age 56.9 yrs., 53.9% female (no info. provided on race/ethnicity) |
Setting: General Practices I: Nurse Practitioner (NP) led a lifestyle intervention guided by standardized computerized software program, The Groningen Overweight and Lifestyle (GOAL) study, consisting of four, 4 hour sessions & 1 feedback session by telephone. Info. delivered included promoting awareness of lifestyle & bodyweight, critique of food diaries, instruction on the history of slimming, goal-setting & evaluation of goals (1 yr.) C: Usual Care (UC) from a general practitioner (GP): 1 visit, ~10 mins. to discuss screening results w/ follow-up usual care. |
Year 1: Overall=91% (416/457) I=89.3% (201/225) C=92.7%, (215/232) Year 3: Overall=78.1% (357/457) I=76% (171/225) C=80.2% (186/232) Diff. in dropout rate not sig., (P=0.28) |
Percent Change in Body Weight & Mean Weight Change at yr 1 & 3 follow-up Year 1 Weight losers/stabilizers: I: 77% losers & stabilizers C: 65% losers & stabilizers Sig. diff. btw groups: (P<0.05) Mean weight change: I: −1.9(4.9)% C: −0.9(5.0)% Sig. diff. btw groups: (P<0.05) Mean weight losses by sex: I: men −2.3% (−3.2, −1.3) & women −1.6% (−2.5, −0.6) C: men −0.1% (−1.1, 0.8) & women −1.6% (−2.5, −0.7); women lost sig. more weight than men within control group (P<0.05) NP visits: >3 visits: avg. 3.0% body weight loss (BMI 30) & 1.3% body weight loss (BMI<30), no sig diff. 0–3 visits: avg. 2.3% body weight loss (BMI 30) & 0.4% body weight loss (BMI<30), (P<0.05) Year 3 Weight losers/stabilizers: I: 62% losers & stabilizers C: 63% losers & stabilizers No sig. diff. btw groups: (P=0.78) Mean weight change* I: −1.2(5.8)% C: −0.6(5.6)% No sig. diff. btw groups: (P=0.37) *1 yr follow-up results differ in 2009 paper No diff. in weight change at 3 yrs btw the NP & GP-UC groups or in subgroups of patients’ characteristics at baseline Within NP group 3 attempts to lose weight during past 5 yrs lost more weight after 3 yrs than participants w/ 4 attempts, −1.5 (−2.5, −0.5) vs.1.4 (−0.9, 3.7); (P<0.05) 1 yr. vs. 3 yr. follow-up Weight losers/stabilizers: I: 80% C: 64% Sig diff. btw groups: (P=0.001) Mean weight change (total, adjusted) I: 1 yr −2.2 (−2.9, −1.5) kg, 3 yr −1.2 (−2.1, −0.4) kg C:1 yr −0.7 (−1.4, −0.0) kg, 3 yr −0.5 (−1.3, 0.3) kg No sig. diff w/in groups |
4 |
| Usher et al., 2013, Australia | N=101 I=51 C=50 (47% female, 29% non-white Australians) |
Setting: Outpatient. Local mental health services I: Provided w/ a healthy lifestyle booklet & met wkly for support and nutrition & exercise education/30min activity led by mental health nurses (12 wks.) C: Provided w/ a healthy lifestyle booklet |
Not available |
Diff. in Mean Weight & BMI Diff. in mean weight: I: 0.74(3.78) kg C: 0.17(3.36) kg (P=0.420) Diff. in mean BMI: I: 0.25(1.34) kg/m2 C: 0.06(1.17) kg/m2 (P=0.435) |
1 |
|
Vermunt et al., 2011, Netherlands Vermunt et al., 2012, Netherlands |
N=1,065 I=543 C=522 (Overall sample demographics not provided) |
Setting: Primary Care I: Active Prevention in High-Risk Individuals of Diabetes Type 2 in and around Eindhoven (APHRODITE). Individual consultation w/ both a GP & NPs w/ NP intensively guiding the behavioral- change process, 5 group meetings for info. on diet & exercise conducted by dieticians & physiotherapists, and an individual consultation w/ dietician to discuss 3 day food record & ways to improve C: Usual Care- received oral & written info. at start of study on Type 2 Diabetes risk & healthy lifestyle |
Not available for 1.5 yrs 2.5 yrs: Overall=66.6% I=67.8% (368/543) C=65.3% (341/522) |
Change in BMI & Weight at 0.5, 1.5 & 2.5 yrs Change in BMI w/in Intervention group over time: 0.5 yrs: −0.3 (−1.4, 0.8) kg/m2 1.5 yrs: −0.2 (−1.9, 1.5) kg/m2 2.5 yrs: −0.3 (−2.1, 1.5) kg/m2 (P=0.0003) Change in BMI w/in Control group over time: 0.5 yrs: −0.2 (−1.2, 0.8) kg/m2 1.5 yrs: −0.1 (−1.7, 1.5) kg/m2 2.5 yrs: −0.1 (−1.8, 1.6) kg/m2 (P=0.0006) Diff. in change over time btw groups (P=0.70) Change in weight w/in Intervention & Control Group: Intervention: 0.5 yrs: −0.8 (−4.1, 2.5) kg 1.5 yrs: −0.6 (−5.7, 4.4) kg 2.5 yrs: −0.8 (−5.9, 4.3) kg (P<0.0001) Control: 0.5 yrs: −0.5 (−3.5, 2.5) kg 1.5 yrs: −0.3 (−4.8, 4.2) kg 2.5 yrs: −0.4 (−5.1, 4.3) kg (P=0.003) Diff. in change over time btw groups (P=0.69) |
3 |
| Wang et al., 2012, Taiwan | N=60 I=30; age 45.9 (9.8) yrs.; 75% female C=30; age 47.5 (6.6) yrs.; 61.5% female (68.3% female, no info. provided on race/ethnicity) |
Setting: District health center in rural community I: Mandatory 6 class (over 3 wks.) program on obesity, weight loss, behavior modification, etc.; class 1 taught by Public Health Nurse. Instructions on how to record diet & exercise details in a structured, graphics-based diary. Diaries reviewed wkly by researcher & nurse w/ participants (12 wks.) C: Attended same classes as intervention group w/ the exception on how to use self-monitoring diary |
Overall=83% (50/60) I=80% (24/30) C:=87% (26/30) |
Mean Diff. in Body Weight at 12 wks. Mean diff. in body weight: I: −5.6(2.6) kg, (P<.001) C: −2.7(1.4) kg, (P<.001) Diff. btw groups (ANCOVA F=21.3, P<.001) |
3 |
| Wilson et al., 2016, United States of America | N=2,819, 6 sites I=1,518, 3 sites; mean age 44 yrs., 5.4% female, 28.4% non-white C=1,301, 3 sites; mean age 47 yrs., 6.3% female, 19.4% non-white (5.9% female, 23.9% minority) |
Setting: Railroad maintenance facilities of Union Pacific Railroad I: Fuel Your Life (FYL) program- adapted Diabetes Prevention Program (DPP). Individual session w/ dietician or health educator to discuss weight loss & PA goals. Program manual for content & self-monitoring, health coach to provide basic info. & support, occupational nurse to provide support to health coaches & participants & lead 3 group sessions, frequent contact (nurses held 6 group sessions) + environmental supports (6 mos.+12 mos follow up) C: Sites had no planned intervention but may have had ongoing health & safety operations |
Overall=13% (362/2,819) I=15% (227/1518) C=10% (135/1301) |
Mean Change in BMI & Body Weight 12 mos. (pretest to follow-up) BMI: I: −0.1 kg/m2, (P=0.45) C: 0.3 kg/m2, (P=0.27) Body Weight: I: −1.6 lbs, (P=0.39) C: 3.1 lbs, (P=0.17) % Body Weight change: I: 44.8% (No loss/weight gain), 44.0% (0.01–4.9% loss) C: 64.8% (No loss/weight gain), 26.8% (0.01–4.9% loss) |
1 |
Note. BMI = body mass index; PA = physical activity; MUFI = multiple-family intervention; SIFI = Single-family Intervention; CVD = cardiovascular disease; BP = blood pressure; HTN = hypertension; IFG = impaired fasting glucose; NP = nurse practitioner; GOAL = Groningen Overweight and Lifestyle; ANCOVA = analysis of covariance; FYL = Fuel Your Life; DPP = Diabetes Prevention Program.
Intervention Settings and Strategies
Most of the interventions took place in outpatient clinical settings (58%). However, there were studies conducted in participants’ workplaces (Lemon et al., 2014; Wilson et al., 2016), homes (Fulkerson et al., 2015; Goodman et al., 2008; Hacihasanoǧlu & Gözüm, 2011), school settings (Wright et al., 2013), licensed child care facilities (Alkon et al., 2014) and remotely over the phone (Leemrijse et al., 2016). Interventions were targeted towards obese patients, employees, school-aged children, child care providers, parents of young children and patients with hypertension, heart failure, coronary heart disease, diabetes type 2 and severe mental illness.
The majority of the interventions were weight loss interventions with only one study consisting of a multi-phase weight loss and weight loss maintenance intervention (Brown, Goetz, & Hamera, 2011). The majority of the interventions involved any combination of consultations with an element of goal setting, motivational interviewing or coaching, and lifestyle change education. Many interventions were nutrition and/or physical activity education accompanied with support services. Other interventions involved coaching over the phone and oversight of organized physical activity. The length of the interventions ranged from six weeks to two years. Nine studies had outcome assessments at follow-up times ranging from six months to 3 years (Fulkerson et al., 2015; Hesselink et al., 2015; Kokkvoll, Grimsgaard, Steinsbekk, Flaegstad, & Njolstad, 2015; Lemon et al., 2014; ter Bogt et al., 2011; Valve et al., 2013; Vermunt et al., 2012; Wilson et al., 2016; Wright et al., 2013). Furthermore, nine studies reported nurses delivering interventions within multidisciplinary teams (Andryukhin, Frolova, Vaes, & Degryse, 2010; Brown et al., 2011; Brown, Goetz, Hamera, & Gajewski, 2014; Fulkerson et al., 2015; Gallagher et al., 2012; Kokkvoll et al., 2015; Lemon et al., 2014; Vermunt et al., 2012; Wilson et al., 2016; Wright et al., 2013).
Outcome Evaluation
The average measure of study quality, modified Jadad score, was 2.75. The overall study scores can be found in Table I under the title heading “Scientific Quality Score.”
There were two approaches studies used to report significant results: one was examining within-group change in BMI or weight. The other was examining between-group (intervention and control) differences. Sixty-five percent of the studies reported significant findings related to BMI or weight reduction. Within these studies, 77 percent reported significant results in weight or BMI reduction in the intervention group compared to the control group (Alkon et al., 2014; Brown et al., 2011, 2014; Gallagher et al., 2012; Hacihasanoǧlu & Gözüm, 2011; Kokkvoll et al., 2015; Leemrijse et al., 2016; Lemon et al., 2014; ter Bogt et al., 2009, 2011; Wang, Fetzer, Yang, & Wang, 2012; Wright et al., 2013). Additionally, several of these studies with significant results also reported nonsignificant findings related to sex (Wright et al., 2013), follow-up assessment (Brown et al., 2011, 2014; ter Bogt et al., 2011), and within-group changes in BMI or weight (Alkon et al., 2014). Seven studies report no significant findings in all outcome measures (Andryukhin et al., 2010; Fulkerson et al., 2015; Goodman et al., 2008; Hesselink et al., 2015; Usher, Park, Foster, & Buettner, 2013; Valve et al., 2013; Wilson et al., 2016). In terms of weight loss at follow-up assessments, three out of nine studies reported significant weight loss, albeit one only for girls, between groups at follow-up times ranging from twelve months to 2 years (Kokkvoll et al., 2015; Lemon et al., 2014; Wright et al., 2013). One study had a significant loss of weight and BMI after the first year of the intervention but when the number of lifestyle counseling visits decreased by three for two years, the participants did not continue to experience significant loss in weight and BMI in the third year of the study (ter Bogt et al., 2009, 2011).
Seven out of 9 studies that reported nurses working within multidisciplinary teams showed significant weight or BMI reduction; five of them significant between-group differences. Nurses working alone were also effective in reducing BMI and/or weight (64% of nurse intervention only studies; 30% out of total studies).
Of the studies that reported no significant findings, there was no noticeable trend related to the quality of study or study population. The modified Jadad score for these studies with non-significant results ranged from 1–4 with a median of 3. Additionally, these studies with non-significant findings were conducted in a variety of countries represented in the review.
Of the three studies that reported results by sex, one study showed a decrease in BMI and weight for both men and women within the intervention (Drevenhorn et al., 2012). Another study showed that women lost more weight than men within the control group, but men lost more weight than women within the intervention group; however, the results were non-significant for the latter. (ter Bogt et al., 2009, 2011). In a study involving elementary school children, sex appeared to affect the results as the BMI and BMI z-score (weight adjusted for child age and sex) were significantly reduced in the intervention group compared to the control group but only for the girls (Wright et al., 2013).
Regarding age, of the studies that primarily focused on children and adolescents, 3 out of 5 (60%) studies showed significant findings related to BMI or weight loss. One study showed a significant difference in mean BMI z-scores for 3 to 5 year-olds between the intervention and the control group with a marked reduction by 0.14 BMI z-scores when adjusting for the state where the intervention was conducted, parent education and family poverty (Alkon et al., 2014). Two studies that involved children with mean ages of 10 or age ranges 8–12 showed a reduction in BMI by 0.12 (Kokkvoll et al., 2015) and 3.65 or 0.7 in BMI z-scores (Wright et al., 2013) albeit the latter only for girls. The interventions in these studies with significant findings tend to have nurses working in multidisciplinary teams, are family or provider centered, and incorporate physical activity and nutrition workshops with coaching or consultations.
More studies involved mostly adult participants. Of these studies, 8 of 12 studies (67%) reported significant findings related to BMI or weight reduction. The interventions for the adults typically included a combination of nutrition and physical activity education, supervised physical activity, consultations, goal setting, journaling and self-monitoring with the use of food diaries. Unlike the studies involving children and adolescents, studies involving adults included the use of telephones as part of the coaching and consulting. Regarding age differences as a specific outcome, one study showed that participants aged 35 to 44 in a study sample with half of the participants aged 45 and above, experienced a marked reduction in BMI between the intervention and control groups (Lemon et al., 2014).
Discussion
In summary, this systematic review shows that nurses involved in delivering interventions aimed at reducing BMI or weight are useful at helping participants achieve a healthier weight. Only three studies looked at sex differences in weight or BMI loss. Although we cannot confidently draw conclusions from these studies, men may benefit slightly more than women from these interventions. In a recent systematic review examining sex differences in the effectiveness of weight loss interventions, analysis of effect sizes showed that although the difference in weight loss between men and women were minimal, weight loss interventions slightly favored men (Williams, Wood, Collins, & Callister, 2015).
The results of this review indicate that researchers need to make a concerted effort in recruiting minority participants into their research, especially since minorities are disproportionately overweight and obese. Culturally sensitive interventions for obesity prevention have been shown to have higher participant engagement among African-Americans than non-culturally sensitive interventions (Whitt-Glover & Kumanyika, 2010). In this review, only one study had a culturally sensitive-designed intervention in which the aim was to reach underserved minorities (Wright et al., 2013)
Our review also shows that nurses are working within multidisciplinary teams to be effective in achieving positive weight outcomes (78% of multidisciplinary studies; 35% out of total studies). Despite the plethora of research that shows that a multidisciplinary approach is most effective in addressing obesity, many do not highlight the significant role nurses can play in achieving desirable weight outcomes and helping to relieve the burden of care in primary care settings brought upon by the high rate of obesity (Bernstein, Manning, & Julian, 2016; Frank, 1998). There is a great need to explore cost-effective models that would augment the role of nurses in providing care to obese and overweight patients.
Finally, this review demonstrates the need for nurse researchers to augment their research efforts in addressing obesity among children and adolescents. Only a quarter of the studies published had children and adolescents as research participants. Given the rise in obesity among this population, with 17% characterized as obese (Ogden et al., 2016), nurses should play an instrumental role in helping to prevent and manage obesity in this population at risk.
There were several limitations to this systematic review. Since studies published only in English were included, we may have missed studies, thus leaving this review vulnerable to potential selection bias. Additionally, since nurses often work in multi-disciplinary teams, it is difficult to isolate the true effect of nurses on obesity prevention and management. Conversely, some of the studies that reported insignificant results might be due to the intervention and not the nature of the intervention being nurse-delivered.
In conclusion, we see that nurse-delivered interventions can achieve positive weight outcomes. More rigorous research incorporating various intervention strategies using a multi-level and multi-method approach needs to be done to test variable models in weight management research with nurses operating within their scope of practice. Specifically, there is a need for more research using rigorous research designs, such as factorial designs, to directly compare multidisciplinary teams with nurse and non-nurse delivered interventions in weight management research. Strengthening the rigor of the research will enable us to isolate the effect nurses can have on weight management. Additionally, nurse researchers need to be intentional about engaging minorities and children and adolescents in their program of research. Improving the research and scholarship in these ways in the area of weight management research would provide a strong evidence base to inform health care policy makers on expanding the role of nurses in obesity prevention and management.
Supplementary Material
Acknowledgments
We would like to acknowledge the help and advice of Stella Seal, Johns Hopkins librarian, for running the search strategy.
Funding
NIH/NINR F31 NR015399-01, Ruth L. Kirschstein National Research Service Award NIH/NINR T32 NR012704, Pre-Doctoral Fellowship in Interdisciplinary Cardiovascular Health Research
Footnotes
Conflict of Interests
We, authors, declare no conflicts of interest with respect to this review, authorship, and publication of this article.
References
- Association of American Medical Colleges. Recent Studies and Reports on Physician Shortages in the US Center for Workforce Studies. Association of American Medical Colleges; 2012. Oct, p. 19. Retrieved from https://www.aamc.org/download/100598/data/ [Google Scholar]
- Alkon A, Crowley AA, Neelon SE, Hill S, Pan Y, Nguyen V, Kotch JB. Nutrition and physical activity randomized control trial in child care centers improves knowledge, policies, and children’s body mass index. BMC Public Health. 2014;14(215) doi: 10.1186/1471-2458-14-215. http://doi.org/10.1186/1471-2458-14-215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allen JK, Dennison CR. Randomized trials of nursing interventions for secondary prevention in patients with coronary artery disease and heart failure: systematic review. Journal of Cardiovascular Nursing. 2010;25:207–220. doi: 10.1097/JCN.0b013e3181cc79be. http://doi.org/10.1097/JCN.0b013e3181cc79be. [DOI] [PubMed] [Google Scholar]
- Anderson D, Mizzari K, Kain V, Webster J. The effects of a multimodal intervention trial to promote lifestyle factors associated with the prevention of cardiovascular disease in menopausal and postmenopausal Australian women. Health Care for Women International. 2006;27(3):238–253. doi: 10.1080/07399330500506543. http://doi.org/10.1080/07399330500506543. [DOI] [PubMed] [Google Scholar]
- Andryukhin A, Frolova E, Vaes B, Degryse J. The impact of a nurse-led care programme on events and physical and psychosocial parameters in patients with heart failure with preserved ejection fraction: A randomized clinical trial in primary care in Russia. The European Journal of General Practice. 2010;16(4):205–214. doi: 10.3109/13814788.2010.527938. http://doi.org/10.3109/13814788.2010.527938. [DOI] [PubMed] [Google Scholar]
- Berkowitz B. Advocating for the prevention of childhood obesity: A call to action for nursing. The Online Journal of Issues in Nursing. 2009;14(1):1–9. http://doi.org/10.3912/OJIN.Vol14No1Man02. [Google Scholar]
- Bernstein KM, Manning DA, Julian RM. Multidisciplinary teams and obesity. Primary Care: Clinics in Office Practice. 2016;43(1):53–59. doi: 10.1016/j.pop.2015.08.010. http://doi.org/10.1016/j.pop.2015.08.010. [DOI] [PubMed] [Google Scholar]
- Bogers RP, Barte JCM, Schipper CMA, Vijgen SMC, De Hollander EL, Tariq L, Bemelmans WJE. Relationship between costs of lifestyle interventions and weight loss in overweight adults. Obesity Reviews. 2010;11(1):51–61. doi: 10.1111/j.1467-789X.2009.00606.x. http://doi.org/10.1111/j.1467-789X.2009.00606.x. [DOI] [PubMed] [Google Scholar]
- Brown C, Goetz J, Hamera E. Weight loss intervention for people with serious mental illness: A randomized controlled trial of the RENEW Program. Psychiatric Services. 2011;62(7):800–802. doi: 10.1176/appi.ps.62.7.800. http://doi.org/10.1176/appi.ps.62.7.800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown C, Goetz J, Hamera E, Gajewski B. Treatment response to the RENEW weight loss intervention in schizophrenia: Impact of intervention setting. Schizophrenia Research. 2014;159(2–3):421–425. doi: 10.1016/j.schres.2014.09.018. http://doi.org/10.1016/j.schres.2014.09.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curioni CC, Lourenço PM. Long-term weight loss after diet and exercise: A systematic review. International Journal of Obesity. 2005;29(10):1168–1174. doi: 10.1038/sj.ijo.0803015. http://doi.org/10.1038/sj.ijo.0803015. [DOI] [PubMed] [Google Scholar]
- Douketis JD, Macie C, Thabane L, Williamson DF. Systematic review of long-term weight loss studies in obese adults: clinical significance and applicability to clinical practice. International Journal of Obesity (2005) 2005;29(10):1153–1167. doi: 10.1038/sj.ijo.0802982. http://doi.org/10.1038/sj.ijo.0802982. [DOI] [PubMed] [Google Scholar]
- Drevenhorn E, Bengtson A, Nilsson PM, Nyberg P, Kjellgren KI. Consultation training of nurses for cardiovascular prevention – A randomized study of 2 years duration. Blood Pressure. 2012;21(5):293–299. doi: 10.3109/08037051.2012.680734. http://doi.org/10.3109/08037051.2012.680734. [DOI] [PubMed] [Google Scholar]
- Frank A. A multidiciplinary approuch to obesity management the physicians role and team care alternatives. Journal of the American Dietetic Association. 1998;98(10):S44–S48. doi: 10.1016/s0002-8223(98)00710-x. http://doi.org/10.1016/S0002-8223(98)00710-X. [DOI] [PubMed] [Google Scholar]
- Franz MJ, VanWormer JJ, Crain AL, Boucher JL, Histon T, Caplan W, Pronk NP. Weight-loss outcomes: A systematic review and meta-analysis of weight-loss clinical trials with a minimum 1-year follow-up. Journal of the American Dietetic Association. 2007;107(10):1755–1767. doi: 10.1016/j.jada.2007.07.017. http://doi.org/10.1016/j.jada.2007.07.017. [DOI] [PubMed] [Google Scholar]
- Fulkerson JA, Friend S, Flattum C, Horning M, Draxten M, Neumark-Sztainer D, Kubik MY. Promoting healthful family meals to prevent obesity: HOME Plus, a randomized controlled trial. The International Journal of Behavioral Nutrition and Physical Activity. 2015;12(154) doi: 10.1186/s12966-015-0320-3. http://doi.org/10.1186/s12966-015-0320-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gallagher R, Kirkness A, Zelestis E, Hollams D, Kneale C, Armari E, Tofler G. A randomised trial of a weight loss intervention for overweight and obese people diagnosed with coronary heart disease and/or type 2 diabetes. Annals of Behavioral Medicine. 2012;44:119–128. doi: 10.1007/s12160-012-9369-2. http://doi.org/10.1007/s12160-012-9369-2. [DOI] [PubMed] [Google Scholar]
- Goodman H, Parsons A, Davison J, Preedy M, Peters E, Shuldham C, Cowie MR. A randomised controlled trial to evaluate a nurse-led programme of support and lifestyle management for patients awaiting cardiac surgery: “Fit for surgery: Fit for life” study. European Journal of Cardiovascular Nursing. 2008;7:189–195. doi: 10.1016/j.ejcnurse.2007.11.001. [DOI] [PubMed] [Google Scholar]
- Hacihasanoǧlu R, Gözüm S. The effect of patient education and home monitoring on medication compliance, hypertension management, healthy lifestyle behaviours and BMI in a primary health care setting. Journal of Clinical Nursing. 2011;20(5–6):692–705. doi: 10.1111/j.1365-2702.2010.03534.x. http://doi.org/10.1111/j.1365-2702.2010.03534.x. [DOI] [PubMed] [Google Scholar]
- Hesselink AE, Rutten GE, Slootmaker SM, de Weerdt I, Raaijmakers LG, Jonkers R, Bilo HJ. Effects of a lifestyle program in subjects with Impaired Fasting Glucose, a pragmatic cluster-randomized controlled trial. BMC Family Practice. 2015;16:183. doi: 10.1186/s12875-015-0394-7. http://doi.org/10.1186/s12875-015-0394-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karfopoulou E, Brikou D, Mamalaki E, Bersimis F, Anastasiou CA, Hill JO, Yannakoulia M. Dietary patterns in weight loss maintenance: Results from the MedWeight study. European Journal of Nutrition. 2016:1–12. doi: 10.1007/s00394-015-1147-z. http://doi.org/10.1007/s00394-015-1147-z. [DOI] [PubMed]
- Kokkvoll A, Grimsgaard S, Steinsbekk S, Flaegstad T, Njolstad I. Health in overweight children: 2-year follow-up of Finnmark Activity School–A randomised trial. Archives of Disease in Childhood. 2015;100:441–448. doi: 10.1136/archdischild-2014-307107. http://doi.org/10.1136/archdischild-2014-307107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lazarou C, Kouta C. The role of nurses in the prevention and management of obesity. The British Journal of Nursing. 2010;19(10):641–647. doi: 10.12968/bjon.2010.19.10.48203. http://doi.org/10.12968/bjon.2010.19.10.48203. [DOI] [PubMed] [Google Scholar]
- Leemrijse CJ, Peters RJ, von Birgelen C, van Dijk L, van Hal JM, Kuijper AF, Veenhof C. The telephone lifestyle intervention “Hartcoach” has modest impact on coronary risk factors: A randomised multicentre trial. European Journal of Preventive Cardiology. 2016;23(15):1658–1668. doi: 10.1177/2047487316639681. http://doi.org/10.1177/2047487316639681. [DOI] [PubMed] [Google Scholar]
- Lemon SC, Wang ML, Wedick NM, Estabrook B, Druker S, Schneider KL, Pbert L. Weight gain prevention in the school worksite setting: Results of a multi-level cluster randomized trial. Preventive Medicine: An International Journal Devoted to Practice and Theory. 2014;60:41–47. doi: 10.1016/j.ypmed.2013.12.010. http://doi.org/10.1016/j.ypmed.2013.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009;6(7):e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogden CL, Carroll MD, Lawman HG, Fryar CD, Kruszon-Moran D, Kit BK, Flegal KM. Trends in obesity prevalence among children and adolescents in the United States, 1988–1994 through 2013–2014. JAMA. 2016;315(21):2292–2299. doi: 10.1001/jama.2016.6361. http://doi.org/10.1001/jama.2016.6361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogden CL, Carroll MD, McDowell MA, Flegal KM. Obesity among adults in the United States- No statistically significant chance since 2003-2004. NCHS Data Brief. 2007;(1):1–8. [PubMed] [Google Scholar]
- Sargent GM, Forrest LE, Parker RM. Nurse delivered lifestyle interventions in primary health care to treat chronic disease risk factors associated with obesity: A systematic review. Obesity Reviews. 2012;13(12):1148–1171. doi: 10.1111/j.1467-789X.2012.01029.x. http://doi.org/10.1111/j.1467-789X.2012.01029.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ter Bogt NC, Bemelmans WJ, Beltman FW, Broer J, Smit AJ, Meer K. Preventing weight gain: One-year results of a randomized lifestyle intervention. American Journal of Preventive Medicine. 2009;37(4):270–277. doi: 10.1016/j.amepre.2009.06.011. http://doi.org/10.1016/j.amepre.2009.06.011. [DOI] [PubMed] [Google Scholar]
- ter Bogt NC, Bemelmans WJE, Beltman FW, Broer J, Smit AJ, van der Meer K. Preventing weight gain by lifestyle intervention in a general practice setting. Archives of Internal Medicine. 2011;171(4):306–313. doi: 10.1001/archinternmed.2011.22. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services and U.S. Department of Agriculture. 2015 – 2020 Dietary guidelines for Americans. (8th) 2015 Retrieved from http://health.gov/dietaryguidelines/2015/guidelines/
- Usher K, Park T, Foster K, Buettner P. A randomized controlled trial undertaken to test a nurse-led weight management and exercise intervention designed for people with serious mental illness who take second generation antipsychotics. Journal of Advanced Nursing. 2013;69:1539–1548. doi: 10.1111/jan.12012. http://doi.org/10.1111/jan.12012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valve P, Lehtinen-Jacks S, Eriksson T, Lehtinen M, Lindfors P, Saha MT, Anglé S. LINDA - a solution-focused low-intensity intervention aimed at improving health behaviors of young females: A cluster-randomized controlled trial. BMC Public Health. 2013;13:1044. doi: 10.1186/1471-2458-13-1044. http://doi.org/10.1186/1471-2458-13-1044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vermunt PWA, Milder IEJ, Wielaard F, de Vries JHM, Van oers H. Lifestyle counseling for Type 2 diabetes risk reduction in Dutch primary care. Diabetes Care. 2011;34:1919–1925. doi: 10.2337/dc10-2293. http://doi.org/10.2337/dc10-2293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vermunt PWA, Milder IEJ, Wielaard F, de Vries JHM, Baan CA, van Oers JAM, Westert GP. A lifestyle intervention to reduce Type 2 diabetes risk in Dutch primary care: 2.5-year results of a randomized controlled trial. Diabetic Medicine. 2012;29(8):223–232. doi: 10.1111/j.1464-5491.2012.03648.x. http://doi.org/10.1111/j.1464-5491.2012.03648.x. [DOI] [PubMed] [Google Scholar]
- Wang CJ, Fetzer SJ, Yang YC, Wang WL. The efficacy of using self-monitoring diaries in a weight loss program for chronically ill obese adults in a rural area. Journal of Nursing Research. 2012;20(3):181–188. doi: 10.1097/jnr.0b013e318263d89b. http://doi.org/10.1097/jnr.0b013e318263d89b. [DOI] [PubMed] [Google Scholar]
- Whitt-Glover MC, Kumanyika SK. Systematic review of interventions to increase physical activity and physical fitness in African-Americans. American Journal of Health Promotion. 2010;23(6):S33–S56. doi: 10.4278/ajhp.070924101. http://doi.org/10.4278/ajhp.070924101. [DOI] [PubMed] [Google Scholar]
- Williams RL, Wood LG, Collins CE, Callister R. Effectiveness of weight loss interventions - Is there a difference between men and women: A systematic review. Obesity Reviews. 2015;16(2):171–186. doi: 10.1111/obr.12241. http://doi.org/10.1111/obr.12241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson GM, DeJoy MD, Vandenberg R, Padilla H, Davis M. FUEL Your Life: A translation of the diabetes prevention program to worksites. American Journal of Health Promotion. 2016;30:188–197. doi: 10.4278/ajhp.130411-QUAN-169. http://doi.org/10.4278/ajhp.130411-QUAN-169. [DOI] [PubMed] [Google Scholar]
- World Health Organization. Obesity and overweight. Geneva, Switzerland: Author; 2015. Retrieved from http://www.who.int/mediacentre/factsheets/fs311/en/ [Google Scholar]
- Wright K, Giger JN, Norris K, Suro Z. Impact of a nurse-directed, coordinated school health program to enhance physical activity behaviors and reduce body mass index among minority children: A parallel-group, randomized control trial. International Journal of Nursing Studies. 2013;50(6):727–737. doi: 10.1016/j.ijnurstu.2012.09.004. http://doi.org/10.1016/j.ijnurstu.2012.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


