Abstract
Background
Over 10% of hospice patients experience a transition out of hospice care during the last months of life. Hospice transitions from home to hospital (ie, hospital-related hospice disenrollment) result in fragmented care, which can be burdensome for patients and caregivers. Nurses play a major role in delivering home hospice care, yet little is known about the association between nursing visits and disenrollment.
Objectives
The study’s purpose is to examine the association between the average number of nursing visits per week and hospital-related disenrollment in the home hospice population. We hypothesize that more nursing visits per week will be associated with reduced odds for disenrollment.
Design
A retrospective cohort study using Medicare data.
Participants
Medicare hospice beneficiaries who were ≥18 years old in 2012.
Outcome measured
Hospitalization within 2 days of hospice disenrollment.
Results
The sample included 115 103 home hospice patients, 6450 (5.6%) of whom experienced a hospital-related disenrollment. The median number of nursing visits per week was 2 (interquartile range 1.3–3.2), with a mean of 2.5 (standard deviation ± 1.6). There was a decreased likelihood of a hospital-related disenrollment when comparing enrollments that had <3 nursing visits per week on average to 3 to <4 visits (odds ratio [OR] 0.39; P value <.001), 4 to <5 visits (OR 0.29; P value <.001), and 5+ visits (OR 0.21; P value <.001).
Conclusions
More nursing visits per week was associated with a decreased likelihood of a hospital-related hospice disenrollment. Further research is needed to understand what components of nursing care influence care transitions in the home hospice setting.
Keywords: hospice, hospitalization, disenrollment, nursing care, continuous home care, inpatient hospice care
Introduction
Hospice care in America has grown tremendously since the enactment of the Medicare Hospice Benefit in 1982, with 45% of US deaths occurring in the program.1 A majority of hospice care is delivered at home, with an estimated 60% to 70% of hospice enrollees receiving care at home.2
Care transitions, the transition of a patient from one healthcare setting to another (eg, home hospice to an acute care hospital), occur in over 10% of hospice enrollees.3 These transitions can be burdensome for patients and caregivers, leading to fragmented care and higher health-care costs.4,5 The Department of Health and Human Services has labeled these transitions “burdensome,” and the Institute of Medicine has called for further research to improve transitions at the end of life.6,7 In particular, a transition from home hospice to an acute care hospital (ie, hospital-related disenrollments) is concerning to hospice staff, stressful for caregivers, and often signals challenges in providing end-of-life care at home.8,9 While factors contributing to hospital-related disenrollments in the home hospice population are complex, reasons vary but include symptoms that are distressing or worrisome to the caregiver, the burden caregivers bear when caring for a dying patient at home, and patients with difficult to manage end-of-life needs.8,9
Hospice team members and services may play an important role in reducing these care transitions. Nurses, the backbone of home hospice care delivery, provide for the physical and psychological needs of the dying patient while supporting the needs of the caregivers and families.10 Given their expertise in end-of-life care, nursing visits can potentially influence hospital-related disenrollments. Furthermore, the use of continuous home care (CHC), general inpatient (GIP) care, and respite care, hospice services which provide more intensive palliative care for patients and caregivers, have been shown to potentially reduce hospital-related disenrollment.11 The CHC is a 24-hour hospice service that delivers care at home to patients during a period of crisis, while GIP care is used for patients who need hospice care in an inpatient setting. Respite care allows home hospice patients to be cared for in an inpatient hospice setting for up to 5 days with the aim of providing a brief respite for the caregiver.
Increased nursing visits or the implementation of CHC, GIP, or respite care can potentially address some of the triggers (eg, distressing symptoms, caregiver burden) for hospital-related disenrollment. Given the importance of nursing care in the home hospice setting, this study’s primary aim is to ascertain whether there is an association between the frequencies of nursing visits with hospital-related disenrollment in home hospice patients. We hypothesize that a greater number of average nursing visits per week will be associated with lower odds for a hospital-related disenrollment. Our secondary objective is to examine whether the use of CHC, GIP care, and respite care will be associated with a decreased likelihood of a hospital-related disenrollment.
Methods
Study Design
Using claims data from the Centers for Medicare and Medicaid Services (CMS), we conducted a retrospective cohort study. The study was approved by the institutional review board of Weill Cornell Medicine.
Data Sources
We merged 3 data files from 2012 for this analysis: (1) hospice research identifiable file (RIF), (2) chronic conditions summary file, and (3) the medical provider analysis and review (MedPAR) RIF. The Hospice RIF provides patient demographic data and claims submitted by hospice providers, while the chronic conditions summary file identifies 26 chronic conditions in each beneficiary. The MedPAR RIF includes hospital claims data, which we used to confirm a hospital-related disenrollment from home hospice.
Study Sample
We used the enrollment of a patient into hospice as the unit of analysis. A random sample of 1 million Medicare beneficiaries enrolled into hospice during 2012 was obtained from CMS. We only included patients who were identified as receiving home hospice care and enrolled during the period April 1 through June 30, 2012. This time frame was selected in order to identify the number of acute care hospital admissions 3 months prior to enrollment while being able to follow patients for at least 6 months following hospice enrollment, consistent with the expected life expectancy for patients receiving hospice care. We excluded enrollments that had 2 or more hospice diagnoses since we were unable to clearly distinguish the patient’s terminal diagnosis, enrollments in which there were incongruent reasons for discharge (eg, a patient discharged from hospice and indicated both as having revoked care and dying on hospice), and disenrollments due to revoked care. In addition, we excluded enrollments that were not identified as having care delivered at home and enrollments with missing data in any of the following fields: age, gender, race/ethnicity, patient’s state of residence, hospice diagnosis. Finally, we excluded enrollments that did not have an indicator of the nursing visit code, 055x, given the assumption that many if not all patients should have at least 1 nursing visit during their hospice enrollment. The final analytical sample compared patients who were hospitalized after hospice to patients who died on hospice or were still alive and on hospice as of December 31, 2012.
Outcome Variable
The outcome of interest was a hospital-related disenrollment within 2 days of a hospice discharge, which has been used in a previous study examining care transitions in hospice.12 We identified this outcome by cross-referencing the date of hospice discharge from the Hospice RIF with the date of hospitalization from the MedPAR RIF. We were unable to identify enrollments that transitioned from a home hospice setting to an inpatient hospice setting or contracted facility, which placed these enrollments into the not hospitalized group.
Average Number of Nursing Visits Per Week
While hospices are paid a fixed rate per day, skilled nursing visits are designated with a revenue code of 055x and are required to be reported each day nursing care is delivered.13 We calculated the average number of nursing visits per week for each enrollment by dividing the total number of nursing visits by the total number of weeks in hospice.
Continuous Home Care, Inpatient Hospice Care, and Respite Care
We identified the utilization of CHC, GIP, and respite care by using the revenue codes outlined in the Medicare Claims Processing Manual (0652, 0656, and 0655, respectively).13
Definition of Covariates
Covariates extracted from the 3 data sets include age (categorized as 18–55, 56–65, 66–75, 76–85, and ≥85 years), gender, race (white, black, and other), region (Northeast, South, Midwest, West), hospice terminal diagnosis (dichotomized as cancer vs noncancer), median income by zip code, number of hospitalizations within 3 months prior to the date of enrollment, total number of previous hospice enrollments, length of stay on hospice, and number of chronic conditions. We condensed chronic conditions into 8 categories (heart disease, lung disease, renal disease, dementia disorders, stroke/transient ischemic attack, diabetes, history of hip fracture, and depression).
Statistical Analysis
We performed descriptive statistics and compared cohorts of low (>0 to <3) and high (3+) average nursing visits per week using χ2 tests for categorical variables and Wilcoxon rank sum tests for continuous variables to assess whether there were differences between the groups. Bivariate analyses were conducted to identify variables associated with hospital-related disenrollment. Covariates that were associated with hospital-related disenrollment (P value <.2) were entered into a multivariable logistic regression model and an area under the receiver–operating curve was calculated. Given the use of average number of nursing visits, we performed 2 sensitivity analyses. One excluded patients with a length of stay less than 7 days since these enrollments may have an inflated number of average nursing visits per week that may confound the results (eg, a patient on hospice for 1 day with 1 nursing visit would have an average of 7 nursing visits per week). The second excluded home hospice patients who also received CHC, GIP care, and/or respite care, which indicate an increased intensity of home hospice care that may influence our outcome of interest. We also examined the 2-way interactions between weekly nursing visits and each of the other independent variables. Statistical analysis was conducted using STATA MP 14.1 (College Station, Texas).
Results
Study Cohort Selection
Of the 1 million enrollments in our sample, we identified 384 484 unique hospice enrollments from April 1, 2012, through June 30, 2012. Figure 1 summarizes the selection of the analytic sample. Observations in which care was never delivered at home (N = 96 116), an enrollment that listed more than 1 hospice diagnosis (N = 134 773) or an enrollment with incongruent reasons for discharge (N = 24 257) were excluded. Furthermore, we dropped observations that had missing variables (N = 5750) or had no indicated nursing visits (N = 8485). As a result, our analytic sample included 115 103 enrollments, of which 6450 (5.6%) resulted in a hospital-related disenrollment.
Figure 1.
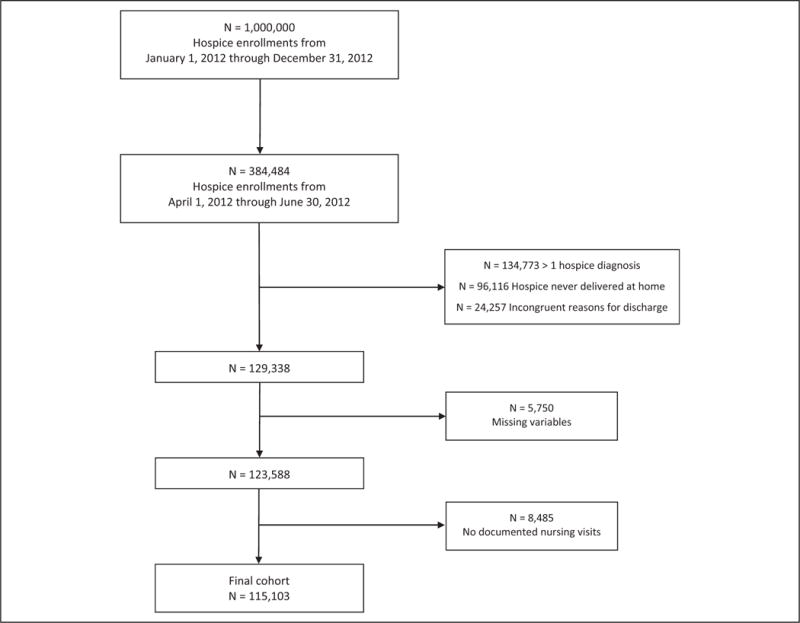
Flow diagram of final cohort selection.
Description of Study Cohort
Table 1 gives the descriptive statistics for the study cohort. The median number of nursing visits per week was 2 (interquartile range 1.3–3.2) with a mean of 2.5 (standard deviation ±1.6), and 73% (N = 84 399) of enrollments averaged <3 nursing visits per week. A minority of enrollments received CHC (N = 7554; 6.6%), while 12.2% (N = 14 043) received GIP care and 7.8% (N = 8948) received respite care.
Table 1.
Characteristics of Home Hospice Enrollments.
| Characteristics | Home Hospice Cohort (N = 115 103) |
|---|---|
| Age (years) | |
| 18–55 | 2387 (2.1) |
| 56–65 | 6847 (6.0) |
| 66–75 | 23 644 (20.5) |
| 76–85 | 38 797 (33.7) |
| 86+ | 43 428 (37.7) |
| Median (IQR) | 82 (74–89) |
| Gender | |
| Women | 67 405 (58.6) |
| Men | 47 698 (41.4) |
| Race/ethnicity | |
| White | 97 915 (85.1) |
| Black | 11 213 (9.7) |
| Other | 5975 (5.2) |
| Region | |
| Midwest | 22 338 (19.4) |
| West | 17 112 (14.9) |
| East | 29 090 (25.3) |
| South | 46 563 (40.4) |
| Hospice diagnosis | |
| Cancer | 38 373 (33.3) |
| Noncancer | 76 730 (66.7) |
| Number of chronic conditionsa | |
| 0–1 | 43 976 (38.2) |
| 2 | 22 853 (19.8) |
| 3 | 22 541 (19.6) |
| 4+ | 25 733 (22.4) |
| Median (IQR) | 1 (0–2) |
| Median income (by quartiles) | |
| $39 114 and lower | 30 812 (26.8) |
| $48 716–$63 709 | 28 401 (24.7) |
| $48 716–$63 709 | 28 191 (24.5) |
| $63 710+ | 27 699 (24.0) |
| Health service utilization | |
| Number of hospitalizations 3 months prior to date of enrollment | |
| 0 | 70 301 (61) |
| 1 or more | 44 802 (39) |
| Number of previous hospice enrollments | |
| 0 | 106 680 (92.7) |
| 1 | 7510 (6.5) |
| 2 or more | 913 (0.8) |
| Hospice length of stay (days) | |
| Median (IQR) | 64 (18–187) |
| Hospice utilization | |
| Continuous home care | 7554 (6.6) |
| Inpatient hospice care | 14 043 (12.2) |
| Respite care | 8948 (7.8) |
| Average nursing visits per week | |
| <3 | 84 399 (73.3) |
| 3 to <4 | 12 423 (10.8) |
| 4 to <5 | 6999 (6.1) |
| 5+ | 11 282 (9.8) |
| Mean (SD) | 2.5 (1.6) |
| Median (IQR) | 2.0 (1.3–3.2) |
Abbreviation: IQR, interquartile range; SD, standard deviation.
Heart disease, lung disease, renal disease, dementia disorders, stroke/TIA, diabetes, depression, history of hip fracture.
Comparison of Cohorts of High- and Low-Average Nursing Visits Per Week
Table 2 compares the characteristics of enrollments based on a low-versus high-average number of nursing visits per week. Of note, men (30.3% vs 24.1%, P value <.001) and patients with cancer (36.9% vs 21.6%, P value <.001) were more likely to receive 3 or more average nursing visits per week compared to their counterparts. Enrollments with more visits had a shorter length of stay (10 vs 116 days, P value <.001).
Table 2.
Characteristics of Home Hospice Enrollments Based on Average Nursing Visits Per Week: Home Hospice Cohort (N = 115 103).
| Characteristics | Average Nursing Visits Per Week <3 (N = 84 399; 73%) | Average Nursing Visits Per Week ≥3(N = 30 704; 27%) | P Value |
|---|---|---|---|
| Age (years) | |||
| 18–55 | 1661 (69.6) | 726 (30.4) | |
| 56–65 | 4718 (68.9) | 2129 (31.1) | |
| 66–75 | 15 992 (67.6) | 7652 (32.4) | |
| 76–85 | 28 176 (72.6) | 10 621 (27.4) | |
| 86+ | 33 852 (78) | 9576 (22) | |
| Median (IQR) | 83 (75–89) | 80 (72–87) | <.001 |
| Gender | <.00l | ||
| Women | 51 159 (75.9) | 16 246 (24.1) | |
| Men | 33 240 (69.7) | 14 458 (30.3) | |
| Race/ethnicity | <.001 | ||
| White | 71 167 (72.7) | 26 748 (27.3) | |
| Black | 8845 (78.9) | 2368 (21.1) | |
| Other | 4387 (73.4) | 1588 (26.6) | |
| Region | <.001 | ||
| Midwest | 15 423 (69) | 6915 (3l) | |
| West | 12 050 (70.4) | 5062 (29.6) | |
| East | 21 378 (73.5) | 7712 (26.5) | |
| South | 35 548 (76.3) | 11 015 (23.7) | |
| Hospice diagnosis | <.001 | ||
| Cancer | 24 213 (63.1) | 14 160 (36.9) | |
| Noncancer | 60 186 (78.4) | 16 544 (21.6) | |
| Number of chronic conditionsa | <.001 | ||
| 0–1 | 32 593 (74.1) | 11 383 (25.9) | |
| 2 | 17 040 (74.6) | 5813 (25.4) | |
| 3 | 16 462 (73) | 6079 (27) | |
| 4+ | 18 304 (71.1) | 7426 (28.9) | |
| Median (IQR) | 1 (0–2) | 1 (0–2) | <.001 |
| Median income (by quartiles) | <.001 | ||
| $39 114 and lower | 20 047 (72.4) | 7652 (27.6) | |
| $48 716–$63 709 | 20 454 (72.6) | 7737 (27.4) | |
| $48 716-$63 709 | 20 705 (72.9) | 7696 (27.1) | |
| $63 710+ | 23 193 (75.3) | 7619 (24.7) | |
| Health services utilization | |||
| Number of hospitalizations 3 months prior to date of enrollment | <.001 | ||
| 0 | 57 868 (82.3) | 12 433 (17.7) | |
| 1 or more | 26 531 (59.2) | 18 271 (40.8) | |
| Number of previous hospice enrollments | .005 | ||
| 0 | 78 096 (73.2) | 28 584 (26.8) | |
| 1 | 5624 (74.9) | 1886 (25.1) | |
| 2 or more | 679 (74.4) | 234 (25.6) | |
| Hospice length of stay (days) | 116 (44–213) | 10 (5–21) | <.001 |
| Continuous home care | <.001 | ||
| Yes | 4462 (59.1) | 3092 (40.9) | |
| No | 79 937 (74.3) | 27 612 (25.7) | |
| Inpatient hospice care | <.001 | ||
| Yes | 10 571 (75.3) | 3472 (24.7) | |
| No | 73 828 (73.1) | 27 232 (26.9) | |
| Respite care | <.001 | ||
| Yes | 7767 (86.8) | 1181 (13.2) | |
| No | 76 632 (72.2) | 29 523 (27.8) | |
Abbreviation: IQR, interquartile range.
Heart disease, lung disease, renal disease, dementia disorders, stroke/TIA, diabetes, depression, history of hip fracture.
Bivariate Analyses of Hospital-Related Disenrollment
Table 3 presents bivariate analyses of variables associated with hospital-related disenrollment. There was no statistically significant difference in the odds of hospital-related disenrollment when comparing enrollments with an average weekly nursing visits of less than 1 to enrollments with 1 to less than 2 visits, and 2 to less than 3 visits. However, as the average nursing visits per week increased to 3 or more, there was a statistically significant lower odds of a hospital-related disenrollment compared to enrollments with less than 3 visits per week on average. Compared to enrollments that received an average of <3 nursing visits per week, enrollments that received 3 to <4 visits had an odds ratio (OR) of 0.69 (95% confidence interval [CI] 0.63–0.76) in hospital-related disenrollments, while those that received 4 to <5 visits had an OR of 0.58 (95% CI 0.52–0.66) and 5+ visits had an OR of 0.49 (95% CI 0.44–0.55). Bivariate analysis of CHC, GIP care, and respite care use showed a reduction in odds of hospital-related disenrollment associated with receiving these services with an OR of 0.35 (95% CI 0.30–0.41), 0.55 (95% CI 0.50–0.60), and 0.80 (95% CI 0.72–0.88), respectively.
Table 3.
Bivariate Analysis of Variables Associated With Hospital-Related Disenrollment.
| Predictor Variables | Hospitalized (%) | Not Hospitalized (%) | OR (95% CI) |
|---|---|---|---|
| Age (years) | |||
| 86+ | 1916 (4.4) | 41 512 (95.6) | 1 |
| 76–85 | 2092 (5.4) | 36 705 (94.6) | 1.23 (1.16–1.32) |
| 66–75 | 1595 (6.8) | 22 049 (93.2) | 1.57 (1.46–1.68) |
| 56–65 | 582 (8.5) | 6265 (91.5) | 2.01 (1.83–2.22) |
| 18–55 | 265 (11.1) | 2122 (88.9) | 2.71 (2.36–3.10) |
| Gender | |||
| Women | 3743 (5.6) | 63 662 (94.4) | 1 |
| Men | 2707 (5.7) | 44 991 (94.3) | 1.02 (0.97–1.08) |
| Race/ethnicity | |||
| White | 4722 (4.8) | 93 193 (95.2) | 1 |
| Black | 1344 (12) | 9869 (88) | 2.69 (2.52–2.87) |
| Other | 384 (6.4) | 5591 (93.6) | 1.36 (1.22–1.51) |
| Region | |||
| Midwest | 909 (4.1) | 21 429 (95.9) | 1 |
| West | 1078 (6.3) | 16 034 (93.7) | 1.58 (1.45–1.74) |
| East | 1461 (5) | 27 629 (95) | 1.25 (1.15–1.36) |
| South | 3002 (6.5) | 43 561 (93.5) | 1.62 (1.51–1.75) |
| Hospice diagnosis | |||
| Cancer | 1536 (4) | 36 837 (96) | 1 |
| Noncancer | 4914 (6.4) | 71 816 (93.6) | 1.64 (1.55–1.74) |
| Number of chronic conditionsa | |||
| 0–1 | 664 (1.5) | 43 312 (98.5) | 1 |
| 2 | 1028 (4.5) | 21 825 (95.5) | 3.07 (2.78–3.39) |
| 3 | 1658 (7.4) | 20 883 (92.6) | 5.18 (4.73–5.68) |
| 4+ | 3100 (12.1) | 22 633 (87.9) | 8.93 (8.20–9.73) |
| Median income (by quartiles) | |||
| $39 114 and lower | 2316 (7.5) | 28 496 (92.5) | 1.77 (1.65–1.90) |
| $487 16–$63 709 | 1562 (5.5) | 26 839 (94.5) | 1.26 (1.17-1.37) |
| $48 716–$63 709 | 1357 (4.8) | 26 834 (95.2) | 1.10 (1.02–1.19) |
| $63 710+ | 1215 (4.4) | 26 484 (95.6) | 1 |
| Health services utilization | |||
| Number of hospitalizations 3 months prior to date of enrollment | |||
| 0 | 3336 (4.8) | 66 965 (95.2) | 1 |
| 1 or more | 3114 (7.0) | 41 688 (93) | 1.50 (1.43–1.58) |
| Number of previous hospice enrollments | |||
| 0 | 5609 (5.3) | 101 071 (94.7) | 1 |
| 1 | 701 (9.3) | 6809 (90.7) | 1.86 (1.71–2.01) |
| 2 or more | 140 (15.3) | 773 (84.7) | 3.26 (2.72–3.92) |
| Hospice length of stay | 0.99 (0.99–0.99) | ||
| Hospice utilization | |||
| Continuous home care | |||
| Yes | 162 (2.1) | 7392 (97.9) | 0.35 (0.30–0.41) |
| No | 6288 (5.9) | 101 261 (94.1) | 1 |
| Inpatient hospice care | |||
| Yes | 467 (3.3) | 13 576 (96.7) | 0.55 (0.50–0.60) |
| No | 5983 (5.9) | 95 077 (94.1) | 1 |
| Respite care | |||
| Yes | 410 (4.6) | 8538 (95.4) | 0.80 (0.72–0.88) |
| No | 6040 (5.7) | 100 115 (94.3) | 1 |
| Average nursing visits per week | |||
| <1 | 659 (6.4) | 9654 (93.6) | 1 |
| 1 to <2 | 2860 (6.3) | 42 596 (93.7) | 0.98 (0.90–1.07) |
| 2 to <3 | 1762 (6.2) | 26 868 (93.8) | 0.96 (0.88–1.05) |
| 3 to <4 | 549 (4.4) | 11 874 (95.6) | 0.68 (0.60–0.76) |
| 4 to <5 | 263 (3.8) | 6736 (96.2) | 0.57 (0.49–0.66) |
| 5+ | 357 (3.2) | 10 925 (96.8) | 0.48 (0.42–0.55) |
| <3 | 5281 (6.3) | 79 118 (93.7) | 1 |
| 3 to <4 | 549 (4.4) | 11 874 (95.6) | 0.69 (0.63–0.76) |
| 4 to <5 | 263 (3.8) | 6736 (96.2) | 0.58 (0.52–0.66) |
| 5+ | 357 (3.2) | 10 925 (96.8) | 0.49 (0.44–0.55) |
Abbreviations: OD, odds ratio; CI, confidence interval.
Heart disease, lung disease, renal disease, dementia disorders, stroke/TIA, diabetes, depression, history of hip fracture.
Multivariable Analysis
In our multivariable analysis, age, race, region, hospice diagnosis, number of chronic conditions, median income, and number of hospitalizations 3 months prior to enrollment were significantly associated with hospital-related disenrollment. Regarding average nursing visits per week, there was a statistically significant reduction in the odds of hospital-related disenrollment when comparing <3 visits to 3 to <4 (OR 0.39; 95% CI 0.35–0.43), 4 to <5 (OR 0.29; 95% CI 0.25–0.33), and 5+ (OR 0.21; 95% CI 0.19–0.24). The area under the receiver– operating characteristic curve for this model was 0.80. Post hoc 2-way interaction analysis revealed a stronger effect of nursing visits among patients with a greater number of chronic conditions and with greater number of previous hospice enrollments.
The utilization of CHC (OR 0.40; 95% CI 0.34–0.47) and GIP care (OR 0.46; 95% CI 0.42–0.51) also were associated with a lower odds of hospital-related disenrollment; however, respite care use (OR 1.05; 95% CI 0.94–1.17) was not found to be significantly associated with the odds of a hospital-related disenrollment (Table 4).
Table 4.
Multivariable Logistic Regression of CHC and GIP Care on Hospital-Related Disenrollment.
| Odds Ratio (95% CI) | ||
|---|---|---|
| Age (years) | 85+ | 1 |
| 76–85 | 1.27 (1.19–1.36) | |
| 66–75 | 1.80 (1.67–1.94) | |
| 56–65 | 2.36 (2.13–2.62) | |
| 18–55 | 3.28 (2.83–3.81) | |
| Race | White | 1 |
| Black | 2.11 (1.96–2.26) | |
| Other | 1.43 (1.27–1.60) | |
| Region | Midwest | 1 |
| West | 1.51 (1.38–1.65) | |
| East | 1.77 (1.61–1.95) | |
| South | 1.41 (1.30–1.53) | |
| Hospice diagnosis | Cancer | 1 |
| Noncancer | 1.66 (1.55–1.77) | |
| Number of chronic conditionsa | 0–1 | 1 |
| 2 | 3.22 (2.91–3.56) | |
| 3 | 5.16 (4.70–5.68) | |
| 4+ | 8.31 (7.59–9.10) | |
| Median income (by quartiles) | $63710+ | 1 |
| $48716–$63709 | 1.09 (1.01–1.19) | |
| $39115–$48715 | 1.20 (1.10–1.30) | |
| $39114 and lower | 1.43 (1.32–1.55) | |
| Number of hospitalizations 3 months prior to date of enrollment | 0 | 1 |
| 1 or more | 0.86 (0.81–0.91) | |
| Number of previous hospice enrollments | 0 | 1 |
| 1 | 0.99 (0.91-1.08) | |
| 2 or more | 1.14 (0.93–1.38) | |
| Hospice length of stay (continuous) | 0.99 (0.99–0.99) | |
| Use of continuous home care | 0.40 (0.34–0.47) | |
| Use of inpatient hospice care | 0.46 (0.42–0.51) | |
| Use of respite care | 1.05 (0.94–1.17) | |
| Average nursing visits per week | <3 | 1 |
| 3 to <4 | 0.39 (0.35–0.43) | |
| 4 to <5 | 0.29 (0.25–0.33) | |
| 5+ | 0.21 (0.19–0.24) |
Abbreviations: CHC, continuous home care; GIP, general inpatient; CI, confidence interval.
Heart disease, lung disease, renal disease, dementia disorders, stroke/TIA, diabetes, depression, history of hip fracture.
Discussion
To our knowledge, this is the first study to examine the association between number of nursing visits and hospital-related disenrollment in a population receiving home hospice care. Our results indicate that a greater number of nursing visits is associated with decreased odds of a hospital-related disenrollment, with an average of 3 visits per week to be a critical threshold to achieve this association. In addition, enrollments that received either CHC or GIP care were found to have reduced odds of hospital-related disenrollment, while no significant association was seen with the use of respite care.
Although an increase in the average number of nursing visits per week was associated with a reduction in hospital-related disenrollment, further studies are needed to elucidate the potential mechanisms underlying this finding. Likely mechanisms include the specific types of care delivered by hospice nurses. Not only do nurses manage the medical care of patients at the end of life, they ensure goal-consistent care and support both patients and families.10 Therefore, an increased frequency of visits may result in better symptom management. This is an important aspect of home hospice care since as many as 90% of patients at the end of life exhibit some type of symptom burden, and past studies have found that distressing symptoms frequently trigger a hospital-related disenrollment.8,14,15 Furthermore, caregiver burden can play a significant role in triggering hospitalization of home hospice patients.8 More frequent nursing visits may also help to relieve caregiver burden, leading to better patient care thereby reducing the risk of hospital-related disenrollment. Given the finite allocation of health-care resources, further research is needed to understand how to best utilize nursing care and whether frequency or intensity of visits lead to improvements not only in hospital-related disenrollment but in other important outcomes such as caregiver satisfaction, quality of death, and costs.
Our results build upon and support a previous study that found CHC reduced hospice disenrollment and hospitalization.11 Our findings reiterate that the use of CHC or GIP care by hospices is associated with a reduction in odds of a hospital-related disenrollment. Further research is needed to understand how to best utilize and promote these resources when they are needed. A previous study found that only 42.7% of US hospices provided CHC care, which is concerning, given that many patients who could benefit from this service do not have access to it.11 Although we did not find a significant association between hospital-related disenrollment and the use of respite care, we believe this may be due to the role of respite services as a resource for caregivers rather than a mechanism to prevent hospital-related disenrollment.
There are limitations and caveats to consider when interpreting these results. While hospices have been required to enter the revenue code 055x to identify nursing visits, a proportion of our sample (N = 8485; 6.8%) did not have a single code for 055x, which suggests nursing visits may be under-reported as it is unlikely that a patient would have no nursing visits when on home hospice. Since we excluded any enrollments that did not document a 055x code for our final analysis, this exclusion may have biased our sample. In addition, we excluded enrollments that listed 2 or more hospice diagnoses, which was a significant portion of our original cohort. This exclusion may have selected for a relatively healthier group of hospice patients. Furthermore, while we measured the average number of weekly nursing visits over a course of hospice enrollment, we recognize that in end-of-life care, there can be fluctuations in a patient’s health, which may influence intensity and frequency of nursing visits over the course of a hospice enrollment. For example, a patient on home hospice who has a pain crisis may be seen more frequently or intensely by a nurse over a period of a few days to better control his or her pain and reduce the chance of a care transition. A scenario such as this may be more meaningful for understanding hospital-related disenrollment but cannot be captured in a claims data set.
Additionally, we did not distinguish among nursing visits provided in regular home care, CHC, and inpatient hospice care. These 3 different types of hospice services offer different levels and types of nursing care. However, when we conducted the same analysis excluding patients who were on CHC and/or GIP care, we found similar results. In addition, we understand that by using average nursing visits per week as our independent variable, patients who had a hospice stay of less than 7 days may have an inflated number of average nursing visits per week (eg, a patient on hospice for 1 day with 1 nursing visit would have an average of 7 nursing visits per week). Therefore, we conducted the same analysis excluding patients with less than 7 days on hospice and found similar results. Finally, we were unable to examine hospital-related transitions that did not result in a disenrollment. Hospices can negotiate contracts with hospitals and patients who transition to those hospitals would not be disenrolled and captured in this study. Further research examining whether there are differences between these 2 home hospice groups (disenrolled vs not disenrolled) who get hospitalized and the quality of care they receive should be examined.
In conclusion, our study found that a greater average number of weekly nursing visits was associated with a reduction in the odds of hospital-related disenrollment in the home hospice population. This work highlights the importance of nursing care in the home hospice setting and may provide guidance on how home hospice can best utilize resources. Further studies are needed to examine the services nurses provide during visits and which of these components influence care transitions and other patient/caregiver outcomes.
Acknowledgments
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work is supported by a grant from the Empire Clinical Research Investigator Program and the John A. Hartford Foundation. Clara Oromendia was partially supported by the following grant: Clinical and Translational Science Center at Weill Cornell Medical College (UL1-TR000457-06).
Footnotes
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- 1.National Hospice and Palliative Care Organization. NHPCO’s Facts and Figures: Hospice Care in America. 2012. National Hospice and Palliative Care Organization; 2012. http://www.nhpco.org/sites/default/files/public/Statistics_Research/2012_Facts_Figures.pdf. Accessed November 22, 2016. [Google Scholar]
- 2.National Hospice and Palliative Care Organization. NHPCO’s Facts and Figures: Hospice Care in America. 2014. National Hospice and Palliative Care Organization; 2014. http://www.nhpco.org/sites/default/files/public/Statistics_Research/2014_Facts_Figures.pdf. Accessed December 11, 2016. [Google Scholar]
- 3.Wang SY, Aldridge MD, Gross CP, et al. Transitions between healthcare settings of hospice enrollees at the end of life. J Am Geriatr Soc. 2016;64(2):314–322. doi: 10.1111/jgs.13939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brennan TA, Leape LL, Laird NM, et al. Incidence of adverse events and negligence in hospitalized patients: results of the Harvard Medical Practice Study I. 1991. Qual Saf Health Care. 2004;13(2):145–152. doi: 10.1136/qshc.2002.003822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Smith AK, Fisher J, Schonberg MA, et al. Am I doing the right thing? Provider perspectives on improving palliative care in the emergency department. Ann Emerg Med. 2009;54(1):86–93, 93.e1. doi: 10.1016/j.annemergmed.2008.08.022. [DOI] [PubMed] [Google Scholar]
- 6.Institute of Medicine. Dying in America: Improving Quality and Honoring Individual Preferences Near the End of Life the Pressing Need to Improve End-Of-Life Care. Washington DC, USA: National Academy of Sciences; 2014. [Google Scholar]
- 7.Department of Health and Human Services. Fed Regist. 2015 doi: 10.3109/15360288.2015.1037530. [DOI] [PubMed] [Google Scholar]
- 8.Phongtankuel V, Scherban BA, Reid MC, et al. Why do home hospice patients return to the hospital? A Study of Hospice Provider Perspectives. J Palliat Med. 2016;19(1):51–56. doi: 10.1089/jpm.2015.0178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Phongtankuel V, Paustian S, Reid MC, et al. Events leading to hospitalization of home hospice patients: a study of primary caregivers’ perspectives [Published online November 28, 2016] J Palliat Med. 2016;20(3):1–6. doi: 10.1089/jpm.2015.0550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Riggio RE, Taylor SJ. Personality and communication skills as predictors of hospice nurse performance. J Bus Psychol. 2000;15(2):351–359. [Google Scholar]
- 11.Wang SY, Aldridge MD, Canavan M, Cherlin E, Bradley E. Continuous home care reduces hospice disenrollment and hospitalization after hospice enrollment. J Pain Symptom Manage. 2016;52(6):813–821. doi: 10.1016/j.jpainsymman.2016.05.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Teno JM, Bowman J, Plotzke M, et al. Characteristics of hospice programs with problematic live discharges. J Pain Symptom Manage. 2015;50(4):548–552. doi: 10.1016/j.jpainsymman.2015.05.001. [DOI] [PubMed] [Google Scholar]
- 13.CMS Medicare Claims Processing Manual. 2009:1–126. [Google Scholar]
- 14.Kutner JS, Kassner CT, Nowels DE. Symptom burden at the end of life: hospice providers’ perceptions. J Pain Symptom Manage. 2001;21(6):473–480. doi: 10.1016/s0885-3924(01)00281-0. [DOI] [PubMed] [Google Scholar]
- 15.Zeppetella G, O’Doherty CA, Collins S. Prevalence and characteristics of breakthrough pain in cancer patients admitted to a hospice. J Pain Symptom Manage. 2000;20(2):87–92. doi: 10.1016/s0885-3924(00)00161-5. [DOI] [PubMed] [Google Scholar]


