Abstract
Heart failure (HF) is a global pandemic affecting at least 26 million people worldwide and is increasing in prevalence. HF health expenditures are considerable and will increase dramatically with an ageing population. Despite the significant advances in therapies and prevention, mortality and morbidity are still high and quality of life poor. The prevalence, incidence, mortality and morbidity rates reported show geographic variations, depending on the different aetiologies and clinical characteristics observed among patients with HF. In this review we focus on the global epidemiology of HF, providing data about prevalence, incidence, mortality and morbidity worldwide.
Keywords: Heart failure, heart failure with preserved ejection fraction, heart failure with reduced ejection fraction, heart failure with mid-range ejection fraction, prevalence, incidence, mortality, morbidity, clinical characteristics, geographic differences
Heart failure (HF) is a complex clinical syndrome characterised by the reduced ability of the heart to pump and/or fill with blood.[1,2] From a physiological point of view, HF can be defined as an inadequate cardiac output to meet metabolic demands or adequate cardiac output secondary to compensatory neurohormonal activation (generally manifesting as increased left ventricular filling pressure).[2] HF has recently been classified into three subtypes, namely HF with reduced ejection fraction (HFrEF), HF with preserved ejection fraction (HFpEF) and HF mid-range ejection fraction (HFmrEF), according to the ejection fraction, natriuretic peptide levels and the presence of structural heart disease and diastolic dysfunction.[3]
HF has been defined as global pandemic, since it affects around 26 million people worldwide.[4] In 2012 it was responsible for an estimated health expenditure of around $31 billion (£22.5 billion), equivalent to more than 10 % of the total health expenditure for cardiovascular diseases in the United States (US).[5] Projections are even more alarming, however, with total costs expected to increase by 127 % between 2012 and 2030.[5]
In this review we describe the epidemiology of HF, providing data about the prevalence, incidence, mortality and morbidity worldwide.
Prevalence and Incidence
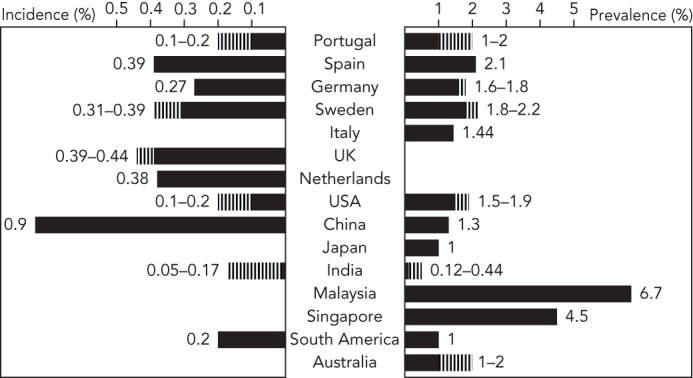
Currently 5.7 million people in the US have HF, but the projections are worrisome since it is expected that by 2030 more than 8 million people will have this condition, accounting for a 46 % increase in prevalence (see Figure 1).[5] In Europe, the EPidemiologia da Insuficiencia Cardiaca e Aprendizagem (Epidemiology of Heart Failure and Learning – EPICA) study performed in the late 1990s in Portugal reported HF prevalence of 1.36 % in the 25–49-year-old group, 2.93 % in the 50–59-year-old group, 7.63 % in the 60–69-year-old group, 12.67 % in the 70–79-year-old group, and 16.14 % in patients >80 years.[6] Another analysis in Spain showed HF prevalence steadily increasing from 895 per 100,000 population per year in 2000 to 2,126 cases in 2007, with higher rates in men than women. The prevalence of HFpEF was higher than that of HFrEF; in the former rates were higher in women, while in the latter they were higher in men. The overall HF prevalence significantly increased with ageing, particularly among patients >64 years and with HFpEF.[7] In Germany in 2006 the prevalence of HF was 1.6 % in women and 1.8 % in men, with numbers increasing considerably with advancing age.[8] In Sweden in 2010 the crude prevalence of HF was 1.8 % and was similar in men and women, but after adjustment for demographic composition the estimated rate was 2.2 %, with a weak decrease in temporal trend in women but not men between 2006 and 2010.[9] A recent survey reported HF prevalence of 1.44 % in Italy, with rates increasing with the ageing of the population.[10] HF is also an important health problem in Asia, and its prevalence seems to be even higher compared to Western countries, ranging between 1.3 % and 6.7 %.[11] Currently in China there are 4.2 million people with HF, with an estimated prevalence of 1.3 %.[12,13] In Japan around 1 million people have the condition, accounting for 1 % of the population.[14–16] In India the estimates range between 1.3 and 4.6 million, which translates to a prevalence of 0.12–0.44 %, although this may be underestimated.[17] In Southeast Asia 9 million people have HF; with a prevalence of 6.7 % in Malaysia and 4.5 % in Singapore.[4,18] In South America the HF prevalence is 1 % and in Australia it ranges between 1 % and 2 %, similar to Western countries (see Figure 2).[19,20] Although aetiologies and clinical characteristics have been studied in Sub-Saharan Africa,[21] there are actually no population studies providing insight into prevalence or incidence.[22]
Figure 1: Burden of Heart Failure.
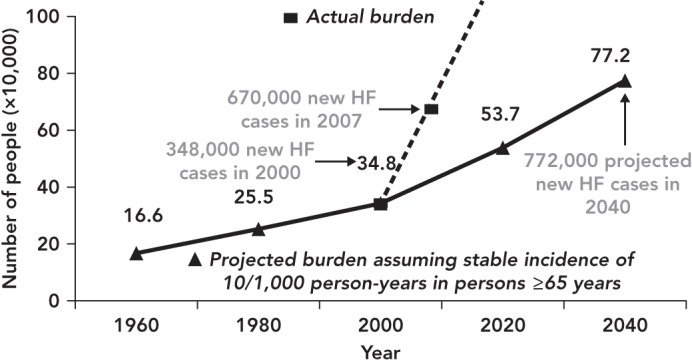
The actual annual incidence of heart failure (HF) reported in the US (squares and dotted line) exceeded the projected annual incidence (triangles and solid line) calculated based on a stable incidence of 10 per 1,000 person-years in persons aged ≥65 years. Source: Lam et al., 2011.[69] Reproduced with permission, © 2011 John Wiley & Sons.
Figure 2: Prevalence and Incidence of Heart Failure Worldwide.
Few studies have evaluated the different trends in HFrEF and HFpEF prevalence and there are currently no data on the emerging HfmrEF category. Data are heterogeneous and also depend on the definition used for HFpEF and HFrEF, but it might be that about half of HF patients have HFrEF and half HFpEF, with the proportion of individuals with HFpEF increasing, particularly if more unselected populations are considered (see Figure 3).[23–26] HFpEF could be dominant in driving the overall HF prevalence, since in the past 20 years secular trends have reported an increasing proportion of patients with HFpEF but relatively stable or even decreasing rates with HFrEF (see Figure 4); thus it is expected that by 2020 65 % of patients hospitalised for HF will have HFpEF.[27]
Figure 3: Distribution of Left Ventricular Ejection Fraction in Heart Failure.
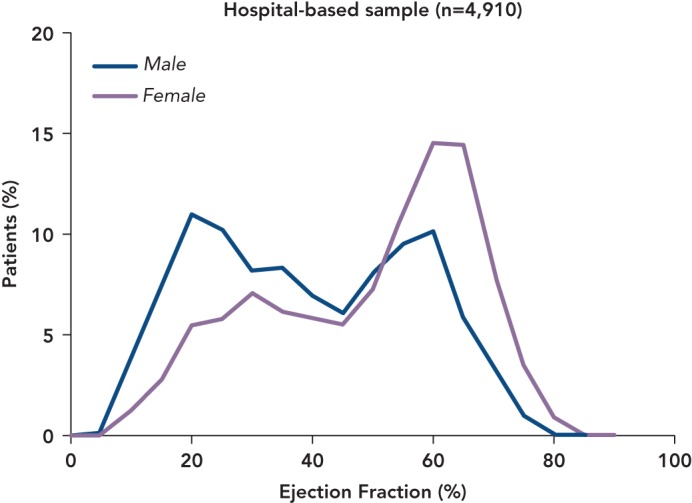
Bimodal distribution of left ventricular ejection fraction in Olmsted County heart failure population. Source: Borlaug and Redfield, 2011.70 Reproduced with permission, © 2011 Wolters Kluwer Health, Inc.
Figure 4: Temporal Trends in Heart Failure with Preserved Ejection Fraction and Heart Failure with Reduced Ejection Fraction.
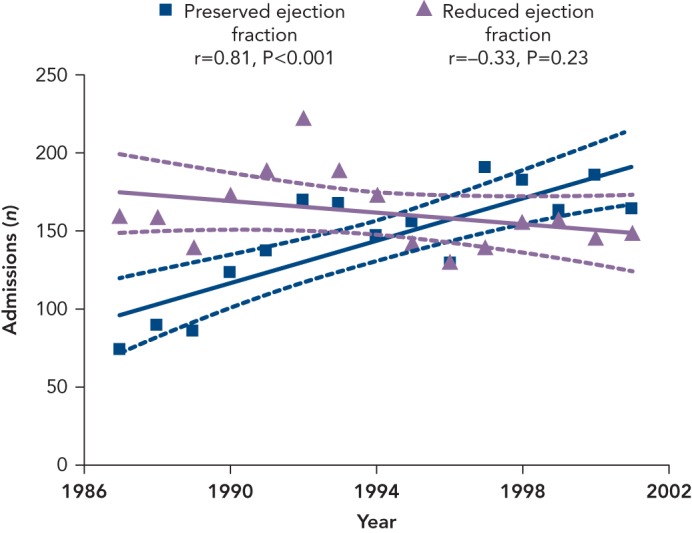
The solid lines represent the regression lines for the relation between the year of admission and the percentage of patients with HF. The dashed lines indicate 95 % confidence intervals. Source: Owan et al., 2006.[27] Reproduced with permission, Copyright © 2006, Massachusetts Medical Society.
Notably, the increase in HF prevalence observed worldwide may not necessarily be linked with an increase in HF incidence, which has been reported to be stable or even decreasing in several studies, particularly in women.[28,29] The ageing of the population, together with improved HF survival due to the advancement in treatments and diagnostic technology could explain the increase in prevalence, whereas the reduction in incidence (due to prevention programmes) may be determined by lower severity and better treatment of acute coronary syndromes.[29–32] In addition to this, the risk factors for HfpEF are multifactorial and complex and there is no known prevention other than treatment of the risk factors, such as hypertension, diabetes and obesity; whereas prevention and early treatment strategies (i.e. early revascularisation) appear to be effective in reducing the risk and severity of acute myocardial infarction. These observations may explain a reduction in the incidence of HFrEF but increasing incidence of HFpEF and HFmrEF.
Currently every year in US there are still 915,000 new cases of HF, accounting for an incidence approaching 10 per 1,000 population after 65 years of age. At 40 years of age the lifetime risk of developing HF is one in five and at 80 the remaining lifetime risk of developing HF remains at 20 %, despite the shorter life expectancy.[5] In Portugal the EPICA study reported an incidence of 1.3 cases per 1,000 population per year for those aged ≥25 years, increasing to 8.8 per 1,000 population at >65 years and 11.6 per 1,000 population at >85 years, with 1.75-fold higher rates in males versus females.[6] In UK, however, the overall incidence rate was 4.4 per 1,000 population per year in men and 3.9 per 1,000 in women, with rates doubling every 5 years after the age of 55.[33] In Spain between 2000 and 2007 the overall incidence of HF increased from 2.96 to 3.90 cases per 1,000 population per year, with a higher incidence among men (0.2 cases per 1,000 population per year). Notably, the incidence of HFrEF surpassed that of HFpEF by 0.24 cases per 1,000 population per year. There were 0.32 more HFrEF cases per 1,000 population per year in men; whereas HFpEF was 0.17 cases per 1,000 population per year higher in women.[7] However, when observing the trends over time, in 2007 the rise in overall incidence of HF plateaued, with HFrEF rates starting to slowly decrease in 2005 while HFpEF was still increasing.[7] In Germany in 2006 the age-and gender-standardised incidence of HF was 2.7 cases per 1,000 population per year, with rates being higher in men than women (2.3 versus 3.1 cases per 1,000 population per year). These incidences more than doubled in each of the higher age categories in both genders.[8] The Prevention of Renal and Vascular End-stage Disease (PREVEND) study that enrolled all 28–75-year-old inhabitants of Groningen (85,421 subjects) in the Netherlands in 1997–8 and followed them until the end of 2009 reported an overall HF incidence of 4.4 %, with 34 % of new-onset cases classified as HFpEF and 66 % as HFrEF.[34] In Sweden in 2010 the incidence of HF was 3.1 cases per 1,000 population per year, and was similar in women and men; however, after adjustment for demographic composition the estimated incidences were revised to 3.7 in women and 3.9 in men, with a decreasing temporal trend of 0.9 cases per 1,000 population per year in absolute terms between 2006 and 2010.[9] In Asia there are fewer data about the incidence of HF. In China every year 500,000 new HF cases are diagnosed, accounting for an incidence of 0.9 %,[12] whereas in India there are 0.5–1.8 million new cases per year (an incidence of 0.05–0.17 %), which again may be underrestimated.[17] In South America the incidence of HF, according to a single population study, is 199 cases per 100,000 person-years (see Figure 2).[19]
Demographic and Clinical Characteristics
The demographic and clinical characteristics of HF have been widely described in Europe and the US, and have been shown to differ considerably between HFpEF and HFrEF, with further variation according to the populations enrolled and the definitions of HfpEF and HFrEF adopted. In particular, it has emerged that HFpEF patients are more likely to be women and older, obese, with a higher New York Heart Association (NYHA) class and cardiovascular comorbidities (such as hypertension, diabetes, atrial fibrillation, valvular disease) and non-cardiovascular comorbidities (such as a anaemia, chronic kidney disease, chronic pulmonary disease, hypothyroidism, cancer, peptic ulcer and psychiatric disorders); whereas coronary artery disease is the main determinant of HFrEF.[23–27,35–38] Recently, HFmrEF has been recognised as a potentially distinct entity and the few observations available suggest that its characteristics are generally intermediate between those of HFpEF and HFrEF: a high prevalence of comorbidities as in HFpEF (i.e. hypertension, diabetes, atrial fibrillation, chronic pulmonary and kidney disease); and a high prevalence of coronary artery disease as in HFrEF, particularly in males and older patients.[36,39,40]
Most studies describing HF characteristics have been performed in North America and Europe; however the phenotypes of HF patients could be different in other regions due to different aetiologies, comorbidities, economic and health care systems. One study showed that in Africa HF patients are younger than in other regions, with most being NYHA class III/IV and having valve disease.[41] Half of these HF patients are male and 29 % have HFpEF. The leading causes of HF in Africa are hypertensive heart disease and dilated cardiomyopathy.[41]–43] In Asia the proportion of patients in NYHA class III/IV is similar to that in NYHA class II.[17,41,44] Coronary artery disease is the leading HF aetiology. More than the half of the HF population is male and has hypertension, and HFpEF is present in 41 % of patients.[17,41,44] It is notable that in Japan ischaemic aetiology is still lower than in Western countries. It has, however, increased over time, and the HFpEF prevalence ranges between 34 % and 68 %.[16] Middle Eastern HF patients are also young, and are more likely to be male. There is a high prevalence of several comorbidities as such obesity, diabetes, hypertension, hyperlipidaemia and valve disease, but only 10–30 % of the population has HfpEF. Coronary artery disease is the main cause of HF in the Middle East.[41,45] In South America the most common cause of HF is coronary artery disease. More than half of HF patients are male and have hypertension, and around half have dyslipidaemia and valve disease.[41,46,47] In Australia HF patients are more likely to be male and the leading HF aetiology is coronary artery disease; HFpEF is present in 25 % of cases.[48]
Outcomes
HF outcomes have been extensively investigated in the US. The Organized Program to Initiate Lifesaving Treatment in Hospitalized Patients With Heart Failure (OPTIMIZE-HF) study enrolling 20,118 patients with HFrEF and 21,149 with HFpEF (EF ≥40 %) reported no differences between HFrEF and HFpEF in 60–90-day mortality (9.8 % versus 9.5 %) and rehospitalisation (29.9 % versus 29.2 %), but higher in-hospital mortality in those with HFrEF (3.9 %) versus HFpEF (2.9 %). When the comparison between HFpEF (EF >50 %) and HFmrEF (EF 40–50 %) was performed, no differences in outcomes were observed.[36] Similarly, the Get With The Guidelines (GWTG) registry that enrolled 15,716 patients with HFrEF, 5,626 with HFmrEF and 18,897 with HFpEF observed 37.5 %, 35.1 % and 35.6 % mortality at 1 yearm respectively, with no differences in risk after several adjustments. The 1-year HF hospital readmission rates were 30.9 %, 28.4 % and 24.3 % in HFrEF, HFmrEF and HfpEF, respectively, but there was a higher risk in HFrEF and HFmrEF compared with HFpEF.[49] The Management Predischarge Process for Assessment of Carvedilol Therapy for Heart Failure (IMPACT-HF) study reported that >50 % of patients were discharged with unresolved symptoms, and within 60 days half had worsening symptoms, a quarter were re-hospitalised and >10 % died.[50] The Canadian Enhanced Feedback for Effective Cardiac Treatment (EFFECT) study enrolling 1,570 patients with HFrEF and 880 with HFpEF reported no differences in mortality at 30 days (7.1 % and 5.3 %, respectively) and 1 year (25.5 % and 22.2 %, respectively). Similarly, for HFrEF and HFpEF there were no differences between HF readmissions at 30 days (4.9 % and 4.5 %, respectively) and at 1-year (16.1 % and 13.5 %, respectively).[51]
In Europe, the EuroHeart Failure Survey compared prognosis in 3,148 patients with HFpEF and 3,658 with HFrEF, reporting higher 90-day mortality in those with HFrEF (12 %) compared with HFpEF (10 %), but similar readmission rates (21 % versus 22 %, respectively).[23] In the EuroHeart Failure Survey II, which enrolled 3,580 patients hospitalised for HF, overall in-hospital mortality was 6.4 %.[52][,53] Recently, in the European Society of Cardiology Heart Failure Long-Term (ESC-HF-LT) registry that enrolled 12,440 patients with acute and chronic HF from 21 European and/or Mediterranean countries, the 1-year mortality rate was estimated to be 23.6 % for acute HF and 6.4 for chronic HF; whereas the rates for the combined endpoint of mortality or HF hospitalisation within 1 year were 36 % for acute HF and 14.5 % for chronic HF. Mortality rates ranged across the different regions from 21.6 % to 36.5 % for acute HF and from 6.9 % to 15.6 % for chronic HF.[54]
Fewer studies have evaluated outcomes in other world regions. Thirty-day mortality reported in China was 5.3 %, while it was 3.9 % in Taiwan.[55] In Singapore, in a cohort of 15,774 HF patients followed from 1991 to 1998, total mortality was 2.5 %.[56] In a more recent study with 2-year follow-up, however, there was a trend towards a higher mortality among Malays compared with Indians or Chinese (27.0 % versus 14.3 % versus 18.6 %, respectively) living in Singapore.[57] In Korea an analysis of 1,527 patients with HFrEF showed 3.8 % mortality at 60 days and 9.2 % at 1 year, whereas hospitalisation rates were 3.1 % at 60 days and 9.8 % at 1 year.[58] In Japan, an analysis from the Japanese Cardiac Registry of Heart Failure in Cardiology (JCARE-CARD) reported an 8.9 % 1-year mortality rate in HFrEF versus 11.6 % in HFpEF, with higher in-hospital mortality in HFpEF (6.5 %) versus HFrEF (3.9 %).[59] Similar 1-year mortality (17 %) was found in the Acute Decompensated Heart Failure Syndromes (ATTEND) registry, which enrolled 4,842 Japanese patients hospitalised for HF.[60] Rates were lower (4.2 %), however, in the more recent Chronic Heart failure Analysis and Registry in Tohoku district (CHART)-2 study.[11,16] In Australia mortality of 20.5–20.7 % at 1 year has been reported in HF patients,[61] with a trend towards reduction over time.[62] In South America, reported hospital readmission rates were 33 %, 28 %, 31 % and 35 % at follow up of 3, 6, 12 and 24–60 months, respectively; whereas the 1-year mortality was 24.5 % and the in-hospital mortality was 11.7 %, with rates being higher in patients with HFrEF.[19]
Since many episodes of worsening of HF are treated by modifying oral therapy or by temporary intravenous treatments in community departments without hospital admission, ambulatory care has a role in HF management. The Prospective Comparison of ARNI With ACEI to Determine Impact on Global Mortality and Morbidity in Heart Failure (PARADIGM-HF) trial recently showed that episodes of outpatient treatment-intensification could significantly contribute to accrue a target number of endpoints in an event-driven trial.[63] According the most recent US reports, in 2011 there were 553,000 emergency department visits and 257,000 outpatient department visits for HF; whereas in 2012 there were 1,774,000 physician office visits with a primary diagnosis of HF.[5] No similar estimates are available in Europe, but the quality of outpatient care has been evaluated by the ESC-HF-LT registry, which reported only 3.2–5.4 % non-adherence to guidelinesuggested drugs, although enrolment in this registry was highly selective.[64] A report from the nationwide and generalisable Swedish Heart Failure Registry suggests poor treatment utilisation, particularly of mineralocorticoid receptor antagonists and device therapy.[65]
Quality of life in HF is worse than in many other chronic diseases.[66] Indeed, a national registry in Sweden has reported that 66,318 and 59,535 premature life-years are lost due to HF compared to 55,364 and 64,533 due to cancer in men and women, respectively.[67] In the Candesartan in Heart Failure: Assessment of Reduction in Mortality and Morbidity (CHARM) trial, health-related quality of life was similarly impaired in patients with HFpEF and HFrEF (41.1 versus 40.8) and independent factors were associated with worse health-related quality of life in both populations (female gender, younger age, higher body mass index, lower systolic blood pressure, greater symptom burden and worse functional status).[68]
Limitation
The current review reports data from studies with different designs and settings, thus the prevalence, incidence and outcome rates might not be fully comparable.
Conclusion
Dataindicate that HF is a major and growing public health problem worldwide. Even though the incidence of HF is stable, the prevalence is going to rise because of the ageing population and improvements in treatment. This will cause further increases in hospitalisation rates and, consequently, in health care costs. HF is a common disease not only in Europe and the US, but worldwide. The switch toward a Western lifestyle in developing countries may be contributing to a real HF pandemic. Phenotyping of HFpEF and HFmrEF, testing existing drugs and developing novel interventions for these categories represents an important future challenge. Currently HFpEF and HFmrEF are poorly investigated, particularly in developing countries, and there are no effective therapies. In order to reduce the number of hospitalisations and related costs, appropriate treatments are needed and further epidemiological studies are required to better characterise the HF population and improve trial design.
References
- 1.Coronel R, de Groot JR, van Lieshout JJ. Defining heart failure. Cardiovasc Res. 2001;50:419–422. doi: 10.1016/s0008-6363(01)00284-x. [DOI] [PubMed] [Google Scholar]
- 2.Tan LB, Williams SG, Tan DK et al. So many definitions of heart failure: are they all universally valid? A critical appraisal. Expert Rev Cardiovasc Ther. 2010;8:217–228. doi: 10.1586/erc.09.187. [DOI] [PubMed] [Google Scholar]
- 3.Ponikowski P, Voors AA, Anker SD et al. Authors/Task Force Members. 2016 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2016;37:2129–200. doi: 10.1093/eurheartj/ehw128. [DOI] [PubMed] [Google Scholar]
- 4.Ponikowski P, Anker SD, AlHabib KF et al. Heart failure: preventing disease and death worldwide. ESC Heart Failure. 2014;1:4–25. doi: 10.1002/ehf2.12005. [DOI] [PubMed] [Google Scholar]
- 5.Mozaffarian D, Benjamin EJ, Go AS et al. American Heart Association Statistics Committee; Stroke Statistics Subcommittee. Heart Disease and Stroke Statistics-2016 Update: A report from the American Heart Association. Circulation. 2016;133:e38–e360. doi: 10.1161/CIR.0000000000000350]. [DOI] [PubMed] [Google Scholar]
- 6.Ceia F, Fonseca C, Mota T et al. EPICA Investigators. Prevalence of chronic heart failure in Southwestern Europe: the EPICA study. Eur J Heart Fail. 2002;4:531–539. doi: 10.1016/s1388-9842(02)00034-x. [DOI] [PubMed] [Google Scholar]
- 7.Gomez-Soto FM, Andrey JL, Garcia-Egido AA et al. Incidence and mortality of heart failure: a community-based study. Int J Cardiol. 2011;151:40–45. doi: 10.1016/j.ijcard.2010.04.055. [DOI] [PubMed] [Google Scholar]
- 8.Ohlmeier C, Mikolajczyk R, Frick J et al. Incidence, prevalence and 1-year all-cause mortality of heart failure in Germany: a study based on electronic healthcare data of more than six million persons. Clin Res Cardiol. 2015;104:688–696. doi: 10.1007/s00392-015-0841-4. [DOI] [PubMed] [Google Scholar]
- 9.Zarrinkoub R, Wettermark B, Wandell P et al. The epidemiology of heart failure, based on data for 2.1 million inhabitants in Sweden. Eur J Heart Fail. 2013;15:995–1002. doi: 10.1093/eurjhf/hft064. [DOI] [PubMed] [Google Scholar]
- 10.Buja A, Solinas G, Visca M et al. Prevalence of heart failure and adherence to process indicators: which sociodemographic determinants are involved? Int J Environ Res Public Health. 2016;13:238. doi: 10.3390/ijerph13020238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sakata Y, Shimokawa H. Epidemiology of heart failure in Asia. Circ J. 2013;77:2209–17. doi: 10.1253/circj.cj-13-0971. [DOI] [PubMed] [Google Scholar]
- 12.Hu SS, Kong LZ, Gao RL et al. Outline of the report on cardiovascular disease in China, 2010. Biomed Environ Sci. 2012;25:251–256. doi: 10.3967/0895-3988.2012.03.001. [DOI] [PubMed] [Google Scholar]
- 13.Yang YN, Ma YT, Liu F et al. [Incidence and distributing feature of chronic heart failure in adult population of Xinjiang]. Zhonghua Xin Xue Guan Bing Za Zhi. 2010;38:460–464. [PubMed] [Google Scholar]
- 14.Okamoto H, Kitabatake A. [The epidemiology of heart failure in Japan]. Nihon Rinsho. 2003;61:709–714. [PubMed] [Google Scholar]
- 15.Okura Y, Ramadan MM, Ohno Y et al. Impending epidemic: future projection of heart failure in Japan to the year 2055. Circ J. 2008;72:489–491. doi: 10.1253/circj.72.489. [DOI] [PubMed] [Google Scholar]
- 16.Konishi M, Ishida J, Springer J et al. Heart failure epidemiology and novel treatments in Japan: facts and numbers. ESC Heart Failure. 2016;3:145–151. doi: 10.1002/ehf2.12103;. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Huffman MD, Prabhakaran D. Heart failure: epidemiology and prevention in India. Natl Med J India. 2010;23:283–288. [PMC free article] [PubMed] [Google Scholar]
- 18.Lam CSP. Heart failure in Southeast Asia: facts and numbers. ESC Heart Failure. 2015;2:46–49. doi: 10.1002/ehf2.12036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ciapponi A, Alcaraz A, Calderon M et al. Burden of heart failure in Latin America: a systematic review and metaanalysis. Rev Esp Cardiol (Engl Ed) 2016;69:1051–60. doi: 10.1016/j.rec.2016.04.054. [DOI] [PubMed] [Google Scholar]
- 20.Sahle BW, Owen AJ, Mutowo MP et al. Prevalence of heart failure in Australia: a systematic review. BMC Cardiovasc Disord. 2016;16:32. doi: 10.1186/s12872-016-0208-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Makubi A, Hage C, Lwakatare J et al. Contemporary aetiology, clinical characteristics and prognosis of adults with heart failure observed in a tertiary hospital in Tanzania: the prospective Tanzania Heart Failure (TaHeF) study. Heart. 2014;100:1235–41. doi: 10.1136/heartjnl-2014-305599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ntusi NB, Mayosi BM. Epidemiology of heart failure in sub- Saharan Africa. Expert Rev Cardiovasc Ther. 2009;7:169–180. doi: 10.1586/14779072.7.2.169. [DOI] [PubMed] [Google Scholar]
- 23.Lenzen MJ, Scholte op Reimer WJ, Boersma E et al. Differences between patients with a preserved and a depressed left ventricular function: a report from the EuroHeart Failure Survey. Eur Heart J. 2004;25:1214–20. doi: 10.1016/j.ehj.2004.06.006. [DOI] [PubMed] [Google Scholar]
- 24.Bursi F, Weston SA, Redfield MM et al. Systolic and diastolic heart failure in the community. JAMA. 2006;296:2209–16. doi: 10.1001/jama.296.18.2209. [DOI] [PubMed] [Google Scholar]
- 25.Goyal P, Almarzooq ZI, Horn EM et al. Characteristics of hospitalizations for heart failure with preserved ejection fraction. Am J Med. 2016;129(635):e15–26. doi: 10.1016/j.amjmed.2016.02.007. [DOI] [PubMed] [Google Scholar]
- 26.Lee DS, Gona P, Vasan RS et al. Relation of disease pathogenesis and risk factors to heart failure with preserved or reduced ejection fraction: insights from the Framingham Heart Study of the National Heart, Lung, and Blood Institute. Circulation. 2009;119:3070–7. doi: 10.1161/CIRCULATIONAHA.108.815944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Owan TE, Hodge DO, Herges RM et al. Trends in prevalence and outcome of heart failure with preserved ejection fraction. N Engl J Med. 2006;355:251–259. doi: 10.1056/NEJMoa052256. [DOI] [PubMed] [Google Scholar]
- 28.Levy D, Kenchaiah S, Larson MG et al. Long-term trends in the incidence of and survival with heart failure. N Engl J Med. 2002;347:1397–402. doi: 10.1056/NEJMoa020265. [DOI] [PubMed] [Google Scholar]
- 29.Najafi F, Jamrozik K, Dobson AJ. Understanding the‘epidemic of heart failure’: a systematic review of trends in determinants of heart failure. Eur J Heart Fail. 2009;11:472–479. doi: 10.1093/eurjhf/hfp029. [DOI] [PubMed] [Google Scholar]
- 30.Roger VL, Weston SA, Redfield MM et al. Trends in heart failure incidence and survival in a communitybased population. JAMA. 2004;292:344–350. doi: 10.1001/jama.292.3.344. [DOI] [PubMed] [Google Scholar]
- 31.Heidenreich PA, Albert NM, Allen LA et al. American Heart Association Advocacy Coordinating Committee; Council on Arteriosclerosis, Thrombosis and Vascular Biology; Council on Cardiovascular Radiology and Intervention; Council on Clinical Cardiology; Council on Epidemiology and Prevention; Stroke Council. Forecasting the impact of heart failure in the United States: a policy statement from the American Heart Association. Circ Heart Fail. 2013;6:606–619. doi: 10.1161/HHF.0b013e318291329a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Journath G, Hammar N, Elofsson S et al. Time trends in incidence and mortality of acute myocardial infarction, and all-cause mortality following a cardiovascular prevention program in Sweden. PLoS One. 2015;10:e0140201. doi: 10.1371/journal.pone.0140201]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Johansson S, Wallander MA, Ruigomez A et al. Incidence of newly diagnosed heart failure in UK general practice. Eur J Heart Fail. 2001;3:225–231. doi: 10.1016/S1388-9842(00)00131-8. [DOI] [PubMed] [Google Scholar]
- 34.Brouwers FP, de Boer RA, van der Harst P et al. Incidence and epidemiology of new onset heart failure with preserved vs. reduced ejection fraction in a community-based cohort: 11-year follow-up of PREVEND. Eur Heart J. 2013;34:1424–31. doi: 10.1093/eurheartj/eht066. [DOI] [PubMed] [Google Scholar]
- 35.Gottdiener JS, McClelland RL, Marshall R et al. Outcome of congestive heart failure in elderly persons: influence of left ventricular systolic function. The Cardiovascular Health Study. Ann Intern Med. 2002;137:631–639. doi: 10.7326/0003-4819-137-8-200210150-00006. [DOI] [PubMed] [Google Scholar]
- 36.Fonarow GC, Stough WG, Abraham WT et al. OPTIMIZE-HF Investigators and Hospitals. Characteristics, treatments, and outcomes of patients with preserved systolic function hospitalized for heart failure: a report from the OPTIMIZEHF Registry. J Am Coll Cardiol. 2007;50:768–777. doi: 10.1016/j.jacc.2007.04.064. [DOI] [PubMed] [Google Scholar]
- 37.Philbin EF, Rocco TA, Jr., Lindenmuth NW et al. Systolic versus diastolic heart failure in community practice: clinical features, outcomes, and the use of angiotensin-converting enzyme inhibitors. Am J Med. 2000;109:605–613. doi: 10.1016/s0002-9343(00)00601-x. [DOI] [PubMed] [Google Scholar]
- 38.Solomon SD, Anavekar N, Skali H et al. Candesartan in Heart Failure Reduction in Mortality (CHARM) Investigators. Influence of ejection fraction on cardiovascular outcomes in a broad spectrum of heart failure patients. Circulation. 2005;112:3738–44. doi: 10.1161/CIRCULATIONAHA.105.561423. [DOI] [PubMed] [Google Scholar]
- 39.He KL, Burkhoff D, Leng WX et al. Comparison of ventricular structure and function in Chinese patients with heart failure and ejection fractions >55% versus 40% to 55% versus <40. Am J Cardiol. 2009;103:845–851. doi: 10.1016/j.amjcard.2008.11.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kapoor JR, Kapoor R, Ju C et al. Precipitating clinical factors, heart failure characterization, and outcomes in patients hospitalized with heart failure with reduced, borderline, and preserved ejection fraction. JACC Heart Fail. 2016;4:464–472. doi: 10.1016/j.jchf.2016.02.017. [DOI] [PubMed] [Google Scholar]
- 41.Dokainish H, Teo K, Zhu J et al. INTER-CHF Investigators. Heart failure in Africa, Asia, the Middle East and South America: The INTER-CHF study. Int J Cardiol. 2016;204:133–141. doi: 10.1016/j.ijcard.2015.11.183. [DOI] [PubMed] [Google Scholar]
- 42.Sliwa K, Damasceno A, Mayosi BM. Epidemiology and etiology of cardiomyopathy in Africa. Circulation. 2005;112:3577–83. doi: 10.1161/CIRCULATIONAHA.105.542894. [DOI] [PubMed] [Google Scholar]
- 43.Sliwa K, Wilkinson D, Hansen C et al. Spectrum of heart disease and risk factors in a black urban population in South Africa (the Heart of Soweto Study): a cohort study. Lancet. 2008;371:915–922. doi: 10.1016/S0140-6736(08)60417-1. [DOI] [PubMed] [Google Scholar]
- 44.Harikrishnan S, Sanjay G, Anees T et al. Trivandrum Heart Failure Registry. Clinical presentation, management, in-hospital and 90-day outcomes of heart failure patients in Trivandrum, Kerala, India: the Trivandrum Heart Failure Registry. Eur J Heart Fail. 2015;17:794–800. doi: 10.1002/ejhf.283. [DOI] [PubMed] [Google Scholar]
- 45.Sulaiman K, Panduranga P, Al-Zakwani I et al. Clinical characteristics, management, and outcomes of acute heart failure patients: observations from the Gulf acute heart failure registry (Gulf CARE). Eur J Heart Fail. 2015;17:374–384. doi: 10.1002/ejhf.245. [DOI] [PubMed] [Google Scholar]
- 46.Bocchi EA. Heart failure in South America. Curr Cardiol Rev. 2013;9:147–156. doi: 10.2174/1573403X11309020007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bocchi EA, Guimaraes G, Tarasoutshi F et al. Cardiomyopathy, adult valve disease and heart failure in South America. Heart. 2009;95:181–189. doi: 10.1136/hrt.2008.151225. [DOI] [PubMed] [Google Scholar]
- 48.Clark RA, McLennan S, Dawson A et al. Uncovering a hidden epidemic: a study of the current burden of heart failure in Australia. Heart Lung Circ. 2004;13:266–273. doi: 10.1016/j.hlc.2004.06.007. [DOI] [PubMed] [Google Scholar]
- 49.Cheng RK, Cox M, Neely ML et al. Outcomes in patients with heart failure with preserved, borderline, and reduced ejection fraction in the Medicare population. Am Heart J. 2014;168:721–730. doi: 10.1016/j.ahj.2014.07.008. [DOI] [PubMed] [Google Scholar]
- 50.Gheorghiade M, Filippatos G, De Luca L et al. Congestion in acute heart failure syndromes: an essential target of evaluation and treatment. Am J Med. 2006;119:S3–S10. doi: 10.1016/j.amjmed.2006.09.011. [DOI] [PubMed] [Google Scholar]
- 51.Bhatia RS, Tu JV, Lee DS et al. Outcome of heart failure with preserved ejection fraction in a population-based study. N Engl J Med. 2006;355:260–269. doi: 10.1056/NEJMoa051530. [DOI] [PubMed] [Google Scholar]
- 52.Nieminen MS, Brutsaert D, Dickstein K et al. EuroHeart Survey Investigators; Heart Failure Association; European Society of Cardiology. EuroHeart Failure Survey II (EHFS II): a survey on hospitalized acute heart failure patients: description of population. Eur Heart J. 2006;27:2725–36. doi: 10.1093/eurheartj/ehl193. [DOI] [PubMed] [Google Scholar]
- 53.Lund LH, Benson L, Dahlstrom U et al. Association between use of beta-blockers and outcomes in patients with heart failure and preserved ejection fraction. JAMA. 2014;312:2008–18. doi: 10.1001/jama.2014.15241. [DOI] [PubMed] [Google Scholar]
- 54.Crespo-Leiro MG, Anker SD, Maggioni AP et al. Heart Failure Association (HFA) of the European Society of Cardiology (ESC). European Society of Cardiology Heart Failure Long-Term Registry (ESC-HF-LT): 1-year follow-up outcomes and differences across regions. Eur J Heart Fail. 2016;18:613–625. doi: 10.1002/ejhf.566. [DOI] [PubMed] [Google Scholar]
- 55.Guo Y, Lip GY, Banerjee A. Heart failure in East Asia. Curr Cardiol Rev. 2013 May;9(2):112–122. doi: 10.2174/1573403X11309020004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Ng TP, Niti M. Trends and ethnic differences in hospital admissions and mortality for congestive heart failure in the elderly in Singapore, 1991 to 1998. Heart. 2003;89:865–870. doi: 10.1136/heart.89.8.865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Lee R, Chan SP, Chan YH et al. Impact of race on morbidity and mortality in patients with congestive heart failure: a study of the multiracial population in Singapore. Int J Cardiol. 2009;134:422–425. doi: 10.1016/j.ijcard.2007.12.107. [DOI] [PubMed] [Google Scholar]
- 58.Youn YJ, Yoo BS, Lee JW et al. Treatment performance measures affect clinical outcomes in patients with acute systolic heart failure: report from the Korean Heart Failure Registry. Circ J. 2012;76:1151–8. doi: 10.1253/circj.cj-11-1093. [DOI] [PubMed] [Google Scholar]
- 59.Tsuchihashi-Makaya M, Hamaguchi S, Kinugawa S et al. JCARE-CARD Investigators. Characteristics and outcomes of hospitalized patients with heart failure and reduced vs preserved ejection fraction. Report from the Japanese Cardiac Registry of Heart Failure in Cardiology (JCARE-CARD). Circ J. 2009;73:1893–900. doi: 10.1253/circj.cj-09-0254. [DOI] [PubMed] [Google Scholar]
- 60.Kajimoto K, Sato N. Takano T; Investigators of the Acute Decompensated Heart Failure Syndromes (ATTEND) Registry. Association of age and baseline systolic blood pressure with outcomes in patients hospitalized for acute heart failure syndromes. Int J Cardiol. 2015;191:100–106. doi: 10.1016/j.ijcard.2015.04.258. [DOI] [PubMed] [Google Scholar]
- 61.Teng TH, Katzenellenbogen JM, Hung J et al. Rural-urban differentials in 30-day and 1-year mortality following first-ever heart failure hospitalisation in Western Australia: a populationbased study using data linkage. BMJ Open. 2014;4:e004724. doi: 10.1136/bmjopen-2013-004724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.McLean AS, Eslick GD, Coats AJ. The epidemiology of heart failure in Australia. Int J Cardiol. 2007;118:370–374. doi: 10.1016/j.ijcard.2006.07.050. [DOI] [PubMed] [Google Scholar]
- 63.Okumura N, Jhund PS, Gong J et al. PARADIGM-HF Investigators and Committees. Importance of clinical worsening of heart failure treated in the outpatient setting: evidence from the Prospective Comparison of ARNI With ACEI to Determine Impact on Global Mortality and Morbidity in Heart Failure Trial (PARADIGM-HF). Circulation. 2016;133:2254–62. doi: 10.1161/CIRCULATIONAHA.115.020729. [DOI] [PubMed] [Google Scholar]
- 64.Maggioni AP, Anker SD, Dahlstrom U et al. Heart Failure Association of the ESC. Are hospitalized or ambulatory patients with heart failure treated in accordance with European Society of Cardiology guidelines? Evidence from 12,440 patients of the ESC Heart Failure Long-Term Registry. Eur J Heart Fail. 2013;15:1173–84. doi: 10.1093/eurjhf/hft134. [DOI] [PubMed] [Google Scholar]
- 65.Thorvaldsen T, Benson L, Dahlstrom U et al. Use of evidencebased therapy and survival in heart failure in Sweden 2003–2012. Eur J Heart Fail. 2016;18:503–511. doi: 10.1002/ejhf.496. [DOI] [PubMed] [Google Scholar]
- 66.Hobbs FD, Kenkre JE, Roalfe AK et al. Impact of heart failure and left ventricular systolic dysfunction on quality of life: a cross-sectional study comparing common chronic cardiac and medical disorders and a representative adult population. Eur Heart J. 2002;23:1867–76. doi: 10.1053/euhj.2002.3255. [DOI] [PubMed] [Google Scholar]
- 67.Stewart S, Ekman I, Ekman T et al. Population impact of heart failure and the most common forms of cancer: a study of 1 162 309 hospital cases in Sweden (1988 to 2004). Circ Cardiovasc Qual Outcomes. 2010;3:573–580. doi: 10.1161/CIRCOUTCOMES.110.957571. [DOI] [PubMed] [Google Scholar]
- 68.Lewis EF, Lamas GA, O’Meara E et al. CHARM Investigators. Characterization of health-related quality of life in heart failure patients with preserved versus low ejection fraction in CHARM. Eur J Heart Fail. 2007;9:83–91. doi: 10.1016/j.ejheart.2006.10.012. [DOI] [PubMed] [Google Scholar]
- 69.Lam CS, Donal E, Kraigher-Krainer E et al. Epidemiology and clinical course of heart failure with preserved ejection fraction. Eur J Heart Fail. 2011;13:18–28. doi: 10.1093/eurjhf/hfq121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Borlaug BA, Redfield MM. Diastolic and systolic heart failure are distinct phenotypes within the heart failure spectrum. Circulation. 2011;123:2006–13. doi: 10.1161/CIRCULATIONAHA.110.954388. [DOI] [PMC free article] [PubMed] [Google Scholar]


