Abstract
Objective:
This study investigated the correlation between participation in the treatment decision-making process and satisfaction with the process among Japanese women with breast cancer. The influence of sociodemographic and clinical characteristics on satisfaction with the treatment decision-making process was also examined.
Methods:
We conducted a cross-sectional, self-administered internet survey of 650 Japanese women with breast cancer in March 2016. Decisional role (active, collaborative, passive) in the treatment decision-making was elicited using the Japanese version of the Control Preference Scale. Satisfaction with the decision-making process was assessed.
Result:
About half of the participants preferred to play a collaborative role, while half of the participants perceived that they played an active role. Satisfaction among the participants who made their treatment choice collaboratively with their physicians was significantly higher than that of participants who made the choice by themselves or entrusted their physicians to make the decision. However, two-way ANOVA demonstrated that satisfaction level was associated with the congruence between the participants’ preferred and actual decisional roles, but not with the actual decisional roles that they played. This association had no interaction with sociodemographic and clinical status, except for education level. A majority of the participants who participated in the roles they preferred in choosing their treatment option indicated that they would participate in the same role if they were to face a similar decision-making situation in the future.
Conclusion:
Regardless of their role played in the cancer treatment decision-making process, and irrespective of their sociodemographic and clinical status, Japanese women with breast cancer are more satisfied with the treatment decision-making process when their participation in the process matches their preferred role in the process.
Keywords: Decision-making, preferred role, actual role, breast cancer, satisfaction, Japanese
Introduction
The incidence of breast cancer (BC) among Japanese women has been increasing. The National Cancer Center Japan estimates that the breast was the leading site for cancer incidence and the fifth leading site for cancer mortality in female cancer patients in 2015 (The Editorial Board of Cancer Statistics in Japan, 2016). The relatively low mortality rate for BC in Japan is likely due to early detection, which has been mainly achieved through routine screening, and therapeutic improvements, suggesting that the life of a BC patient or survivor can be prolonged. A range of treatment options are available for women diagnosed with BC. The options they choose have an effect on their sense of value, their recovery, their overall experience with breast cancer, and their lives after their treatment is complete.
The patient’s participation in the treatment decision-making process can be categorized according to their role. Three basic categories can be identified: (1) the patient makes the decision without direct physician involvement once she has been informed (active role), (2) decisions are made through an interactive process wherein the patient may express her preference and/or values and discuss the best choice for her with the physician (collaborative role), and (3) the patient entrusts her physician to decide what is best for her (passive role).
The role of BC patients in their cancer treatment decision-making process varies across reports. The passive role was found to be preferable in treatment decision-making in studies conducted in Greece and Germany (Almyroudi et al., 2011; Hyphantis et al., 2013; Vogel et al., 2008); about half of the study population in Canada would choose a collaborative role in making their surgery-related decision (Hack et al., 2006); nearly half of the women in studies conducted in the US and Malaysia identified themselves as the final decision maker for their treatment decision-making (Kwait et al., 2013; Mely et al., 2004; Mohamed et al., 2013). In previous studies, 60-70% of Japanese patients with BC preferred an active or collaborative role, and about 40% perceived that they participated in collaborative decision-making (Kokufu, 2012; Nakashima et al., 2012). It is not fully understood what the effects are when BC patients are capable or incapable of playing a preferred decisional role. In addition, little is known of the extent to which decisional role affects satisfaction with the treatment decision-making process among BC patients.
Thus, we conducted an internet survey to examine how Japanese women with BC manage their cancer related treatment decision-making and their level of satisfaction with this process. The influence of sociodemographic and clinical characteristics on satisfaction with the treatment decision-making process were also investigated.
Materials and Methods
Study design
We conducted a cross-sectional internet survey with an online marketing research company to recruit participants from a variety of sociodemographic backgrounds and places of residence (Rakuten Research Inc., Tokyo, Japan). Women who registered with the marketing research company as breast cancer survivors were invited to participate with this survey by email from March 11 to 14, 2016. Study subjects were those who had BC-related surgery and/or treatments in Japan, and were diagnosed with BC between ages 20 to 69. Of 2,833 women who were enrolled as a BC patient or BC survivor in the marketing research company, 955 of them completed the online questionnaire. A total of 650 responders without missing data were used for analysis.
Questionnaire and Measures
We used a self-administered questionnaire that comprised questions related to treatment decision-making roles, satisfaction with the treatment decision-making process, and sociodemographic and clinical characteristics.
The treatment decision-making role was elicited using Japanese version of Control Preference Scale (CPS) created by Degner and Sloan (Degner et al., 1997; Nakashima et al., 2012). Participants indicated the final decision-making role that best described their involvement in the decision-making process: active role, ‘myself’ and ‘myself with consideration of the opinions of the physician’; collaborative role, ‘the physician and I together’; passive role, ‘the physician’ and ‘the physician with consideration of my opinions’. Their preferred role before diagnosis, actual role, and preferred role in the future were elicited.
Satisfaction with the decision-making process was evaluated with the item ‘how satisfied are you with the medical decision-making process you have experienced for your cancer?’ on a numerical rating scale of completely satisfied (100) to not satisfied at all (0).
Statistical Analysis
Data analysis was carried out using SPSS Version 24 (IBM, Armonk, NY, USA). The scores for satisfaction in the treatment decision-making process were transformed using a square root function to approximate a normal distribution. Influences of treatment decision-making role, decisional role congruity, sociodemographic and clinical status on the level of satisfaction with the treatment decision-making process were analyzed with Welch’s analysis of variance (ANOVA) and two-way ANOVA. A χ2 test was performed to examine between-group proportional differences. All tests were two-tailed and statistical significance was set at p <0.05.
Ethical consideration
This study was approved by the Clinical Ethical Review Board of Kurume University, School of Medicine. Prior to the investigation, the participants were provided with explanations via the internet as to the purpose and method of the study as well as information regarding the handling of the results. The study was carried out upon receiving their signed consent online.
Results
Correlation of preferred role and actual role in cancer related treatment decision-making
As shown in Table 1, 49.8% of the participants preferred to play a collaborative role in the treatment decision-making prior to being diagnosed with BC, while only 29.8% actually chose their cancer related treatment collaboratively with their physicians. Similarly, while 37.2% of the participants preferred to play an active role, 47.8% chose their treatment by themselves. Likewise, while 12.9% of the participants preferred to play a passive role, 22.3% actually entrusted their physicians to choose their treatment. Preferred and actual roles did not differ based on sociodemographic and clinical characteristics with the exception of cancer stage in the actual role.
Table 1.
Correlates of Preferred Role and Actual Role in Cancer Related Treatment Decision-Making
| Preferred decision role (n, %) | Χ2 test | Actual decision role (n, %) | Χ2 test | |||||
|---|---|---|---|---|---|---|---|---|
| Variables (n) | Active | Collaborative | Passive | p-value | Active | Collaborative | Passive | p-value |
| Total | 342 (37.2) | 324 (49.8) | 84 (12.9) | 311 (47.8) | 194 (29.8) | 145 (22.3) | ||
| Age | ||||||||
| Younger than 50 (202) | 79 (39.1) | 102 (50.5) | 21 (10.4) | 0.417 | 104 (51.5) | 59 (29.2) | 39 (19.3) | 0.362 |
| 50 years old or more (448) | 163 (36.4) | 222 (49.6) | 63 (14.1) | 207 (46.2) | 135 (30.1) | 106 (23.7) | ||
| Age at diagnosis | ||||||||
| 40 years or younger (142) | 59 (41.5) | 66 (46.5) | 17 (12.0) | 0.105 | 69 (48.6) | 36 (25.4) | 37 (26.1) | 0.141 |
| 41-50 (336) | 129 (38.4) | 171 (50.9) | 36 (10.7) | 166 (49.4) | 108 (32.1) | 62 (18.5) | ||
| 51 years or older (172) | 54 (31.4) | 87 (50.6) | 31 (18.0) | 76 (44.2) | 50 (29.1) | 46 (26.7) | ||
| Marital status | ||||||||
| Single (164) | 68 (41.5) | 79 (48.2) | 17 (10.4) | 0.455 | 89 (54.3) | 48 (29.3) | 27 (16.5) | 0.128 |
| Married (466) | 169 (36.3) | 234 (50.2) | 63 (13.5) | 210 (45.1) | 141 (30.3) | 115 (24.7) | ||
| Others (20) | 5 (25.0) | 11 (55.0) | 4 (20.0) | 12 (60.0) | 5 (25.0) | 3 (15.0) | ||
| Education | ||||||||
| High School or less (204) | 86 (42.2) | 88 (43.1) | 30 (14.7) | 0.069 | 95 (46.6) | 54 (26.5) | 55 (27.0) | 0.127 |
| More than High School (446) | 156 (35.0) | 236 (52.9) | 54 (12.1) | 216 (48.4) | 140 (31.4) | 90 (20.2) | ||
| Household income (JPN) | ||||||||
| Less than ¥5,000,000 (279) | 109 (39.1) | 131 (47.0) | 39 (14.0) | 0.75 | 140 (50.2) | 82 (29.4) | 57 (20.4) | 0.207 |
| ¥5,000,000 or more (251) | 91 (36.3) | 131 (52.2) | 29 (11.6) | 122 (48.6) | 67 (26.7) | 62 (24.7) | ||
| Don’t know/ don’t want (120) | 42 (35.0) | 62 (51.7) | 16 (13.3) | 49 (40.8) | 45 (37.5) | 26 (21.7) | ||
| Residential area at diagnosis | ||||||||
| Prefecture 5 million or more people (397) | 151 (38.0) | 200 (50.4) | 46 (11.6) | 0.719 | 195 (49.1) | 121 (30.5) | 81 (20.4) | 0.14 |
| Prefecture less than 5 million people (249) | 90 (36.1) | 122 (49.0) | 37 (14.9) | 112 (45.0) | 73 (29.3) | 64 (25.7) | ||
| Outside the country (4) | 1 (25.0) | 2 (50.0) | 1 (25.0) | 4 (100.0) | 0 (0.0) | 0 (0.0) | ||
| Employment status at diagnosis | ||||||||
| Full-time (192) | 80 (41.7) | 91 (47.4) | 21 (10.9) | 0.587 | 94 (49.0) | 56 (29.2) | 42 (21.9) | 0.729 |
| Contracted/ part-time (210) | 72 (34.3) | 108 (51.4) | 30(14.3) | 95 (45.2) | 70 (33.3) | 45 (21.4) | ||
| Others (248) | 90 (36.3) | 125 (50.4) | 33 (13.3) | 122 (49.2) | 68 (27.4) | 58 (23.4) | ||
| Time since diagnosis | ||||||||
| 5 years or less (321) | 113 (35.2) | 162 (50.5) | 46 (14.3) | 0.423 | 158 (49.2) | 98 (30.5) | 65 (20.2) | 0.46 |
| Longer than 5 years (329) | 129 (39.2) | 162 (49.2) | 38 (11.6) | 153 (46.5) | 96 (29.2) | 80 (24.3) | ||
| Stage of cancer | ||||||||
| 0-II (480) | 184 (38.3) | 239 (49.8) | 57 (11.9) | 0.341 | 239 (49.8) | 148 (30.8) | 93 (19.4) | 0.02 |
| III, IV (74) | 29 (39.2) | 36 (48.6) | 9 (12.2) | 36 (48.6) | 19 (25.7) | 19 (25.7) | ||
| Do not know (96) | 29 (30.2) | 49 (51.0) | 18 (18.8) | 36 (37.5) | 27 (28.1) | 33 (34.4) | ||
| Treatment status | ||||||||
| Undergoing (215) | 82 (38.1) | 103 (47.9) | 30 (14.0) | 0.689 | 114 (53.0) | 60 (27.9) | 41 (19.1) | 0.163 |
| Completed (285) | 99 (34.7) | 148 (51.9) | 38 (13.3) | 121 (42.5) | 91 (31.9) | 73 (25.6) | ||
| Others (150) | 61 (40.7) | 73 (48.7) | 16 (10.7) | 76 (50.7) | 43 (28.7) | 31 (20.7) | ||
| Surgery | ||||||||
| Modified radical mastectomy (248) | 103 (41.5) | 114 (46.0) | 31 (12.5) | 0.114 | 129 (52.0) | 64 (25.8) | 55 (22.2) | 0.192 |
| Breast conserving treatment (382) | 129 (33.8) | 204 (53.4) | 49 (12.8) | 170 (44.5) | 124 (32.5) | 88 (23.0) | ||
| No surgery/ others (20) | 10 (50.0) | 6 (30.0) | 4 (20.0) | 12 (60.0) | 6 (30.0) | 2 (10.0) | ||
| Adjuvant therapy Radiation | ||||||||
| Yes (383) | 137 (35.8) | 196 (51.2) | 50 (13.1) | 0.645 | 173 (45.2) | 116 (30.3) | 94 (24.5) | 0.17 |
| No (267) | 105 (39.3) | 128 (47.9) | 34 (12.7) | 138 (51.7) | 78 (29.2) | 51 (19.1) | ||
| Chemotherapy | ||||||||
| Yes (286) | 107 (37.4) | 140 (49.0) | 39 (13.6) | 0.866 | 135 (47.2) | 80 (28.0) | 71 (24.8) | 0.351 |
| No (364) | 135 (37.1) | 184 (50.5) | 45 (12.4) | 176 (48.4) | 114 (31.3) | 74 (20.3) | ||
| Hormone | ||||||||
| Yes (454) | 169 (37.2) | 227 (50.0) | 58 (12.8) | 0.984 | 219 (48.2) | 137 (30.2) | 98 (21.6) | 0.797 |
| No (196) | 73 (37.2) | 97 (49.5) | 26 (13.3) | 92 (46.9) | 57 (29.1) | 47 (24.0) | ||
Association between satisfaction with treatment decision-making process and decisional role congruity
The satisfaction level of participants who participated in a collaborative role was significantly higher than that of participants who played an active or passive role in the actual decision role; no difference in satisfaction level between active and passive roles was observed (Figure 1(A)). The two-way ANOVA demonstrated that the main effect of decisional role congruity (preferred vs. actual role) was significant-satisfaction of participants whose decisional roles were congruent was significantly higher than that of participants whose decisional roles were incongruent (Figure 1(B)). In both active and collaborative roles, satisfaction level did not differ based on decisional role congruity. In the passive role, participants whose decisional roles were congruent showed the highest satisfaction of all, while participants whose decisional roles were incongruent showed the lowest satisfaction of all; there was a statistically significant difference in the satisfaction level between congruent and incongruent roles. The main effect of the actual decisional role and the interaction of the actual decisional role and decisional role congruity were not significant.
Figure 1.
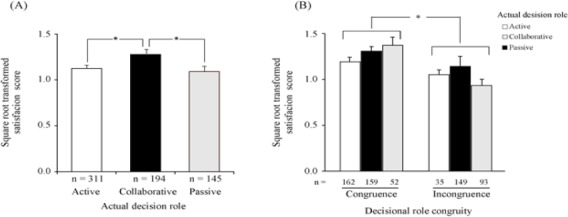
Association between Satisfaction with Treatment Decision-Making Process and Decisional Role Congruity. Data are Presented as Mean of Square Root Transformed Satisfaction Score in the Decision-Making Process ± Standard Error of the Mean. (A) Level of satisfaction was compared in actual decision roles. p = 0.012 (ANOVA). (B) Participants were categorized based on actual decisional role. p-value: main effect of decisional role congruity, <0.001; main effect of actual role, 0.338; interaction of (decisional role congruity) × (actual role), 0.075; congruence vs. incongruence in passive, <0.001. *:p< 0.001.
Influences of sociodemographic and clinical characteristics on association between satisfaction level and decisional role congruity
We examined whether sociodemographic and clinical characteristics influence the association of the satisfaction level with the treatment decision-making process and decisional role congruity (Table 2). Irrespective of sociodemographic and clinical characteristic except surgical procedure, the satisfaction level among those whose preferred and actual decisional roles were congruent was significantly higher than that of those whose decisional roles were incongruent. There were no significant between-group differences in the satisfaction level based on sociodemographic and clinical variables. On the other hand, there was a significant interaction between education level and decisional role congruity in the satisfaction level. When decisional roles were incongruent, the satisfaction among participants with no more than a high school education were lower than that of highly educated participants; however, when decisional roles were congruent, the satisfaction among participants with no more than a high school education were higher than that of highly educated participants.
Table 2.
Association between Satisfaction with Treatment Decision-Making Process and Decisional Role Congruity
| Variables | Decisional role congruity | Two-way ANOVA | p-value | ||
|---|---|---|---|---|---|
| Congruence (n = 373) Mean ± SD | Incongruence (n = 277) Mean ± SD | Congruence vs. Incongruence (A) | Variable (B) | A × B | |
| Total | 1.27± 0.66** | 1.02 ± 0.63 | |||
| Age at diagnosis | |||||
| Younger than 50 | 1.32 ± 0.67** | 0.96 ± 0.64 | <0.001 | 0.891 | 0.348 |
| 50 years old or more | 1.28 ± 0.65** | 1.04 ± 0.62 | |||
| Younger than 50 | 1.20 ± 0.66 | 1.06 ± 0.66 | |||
| Marital status | |||||
| Married | 1.28 ± 0.66** | 1.02 ± 0.64 | <0.001 | 0.661 | 0.643 |
| Others | 1.23 ± 0.64** | 1.02 ± 0.62 | |||
| Education | |||||
| High School or less | 1.33 ± 0.66** | 0.93 ± 0.61 | <0.001 | 0.694 | 0.032 |
| More than High School | 1.24 ± 0.65** | 1.07 ±0.64 | |||
| Household income (JPN) | |||||
| Less than ¥5,000,000 | 1.27 ± 0.66** | 0.97 ± 0.62 | <0.001 | 0.718 | 0.324 |
| ¥5,000,000 or more | 1.29 ± 0.65** | 1.04 ± 0.65 | |||
| Don’t know/ don’t want | 1.20 ± 0.64 | 1.11 ± 0.64 | |||
| Residential area at diagnosis | |||||
| Prefecture 5 million or more people | 1.27 ± 0.65** | 1.02 ± 0.63 | 0.018 | 0.88 | 0.302 |
| Prefecture less than 5 million people | 1.25 ± 0.67* | 1.04 ± 0.64 | |||
| Outside the country | 2.00 ± 0.00 | 0.67 ± 0.50 | |||
| Employment status at diagnosis | |||||
| Full-time | 1.31 ± 0.67** | 0.99 ± 0.65 | <0.001 | 0.846 | 0.611 |
| Contracted/ part-time | 1.26 ± 0.66* | 1.06 ± 0.61 | |||
| Others | 1.23 ± 0.64** | 1.02 ± 0.64 | |||
| Time since diagnosis | |||||
| 5 years or less | 1.26 ± 0.67** | 0.97 ± 0.60 | <0.001 | 0.208 | 0.324 |
| Longer than 5 years | 1.27 ± 0.65* | 1.08 ± 0.67 | |||
| Stage of cancer | |||||
| 0-II | 1.28 ± 0.65** | 1.00 ± 0.61 | <0.001 | 0.55 | 0.164 |
| Others | 1.23 ± 0.68 | 1.11 ± 0.69 | |||
| Treatment status | |||||
| Undergoing | 1.23 ± 0.64** | 0.96 ± 0.63 | <0.001 | 0.075 | 0.906 |
| Completed | 1.33 ± 0.66** | 1.09 ± 0.66 | |||
| Others | 1.19 ± 0.66 | 0.99 ± 0.58 | |||
| Surgery | |||||
| Modified radical mastectomy | 1.21 ± 0.66* | 1.02 ± 0.69 | 0.066 | 0.376 | 0.596 |
| Breast conserving treatment | 1.31 ± 0.65** | 1.03 ± 0.60 | |||
| Others | 1.05 ± 0.72 | 0.94 ± 0.54 | |||
| Adjuvant therapy | |||||
| Radiation | |||||
| Yes | 1.26 ± 0.65** | 1.00 ± 0.58 | <0.001 | 0.444 | 0.765 |
| No | 1.28 ± 0.67** | 1.06 ± 0.70 | |||
| Chemotherapy | |||||
| Yes | 1.27 ± 0.66** | 0.91 ± 0.60 | <0.001 | 0.062 | 0.065 |
| No | 1.27 ± 0.66* | 1.10 ± 0.65 | |||
| Hormone | |||||
| Yes | 1.27 ± 0.65** | 1.03 ± 0.62 | <0.001 | 0.718 | 0.874 |
| No | 1.26 ± 0.67** | 1.00 ± 0.66 | |||
p<0.05 vs. incongruence;
p<0.001 vs. incongruence
Treatment decision-making role in the future
A majority of participants whose actual decisional role in their cancer treatment was congruent with their preferred roles indicated that they would play same role if they were to face a similar situation in the future (81.8%) (Table 3). In contrast, participants who experienced incongruence between their actual and preferred decisional roles had a tendency to change their decisional roles in the future; 33.9% would play a more active role and 33.6% would play a more passive role.
Table 3.
Treatment Decision-Making Role in the Future
| Decision-making role in the future1, (n, %) | Χ2 test | |||||
|---|---|---|---|---|---|---|
| Same | More active | More passive | p-value | |||
| Decisional role congruity of preferred and actual roles | Congruence | 305 (81.8) | 39 (10.5) | 29 (7.8) | 373 | <0.001 |
| Incongruence | 90 (32.5) | 94 (33.9) | 93 (33.6) | 277 | ||
, Diffrence between actual decision making role and decision-making role in the future
Discussion
Our cross-sectional study results indicate that Japanese women with BC were most satisfied with the treatment decision-making process when they played their preferred roles in the process, rather than the actual role. Decisional role congruity had no interaction with clinical status or sociodemographic factors, except for education level.
In previous studies where decisional roles were elicited using the CPS among Japanese patients with BC, Kokufu (2012) found that 71% of inpatients preferred to play an active or collaborative decision-making role; Nakashima (2012) reported 87% of patients who were diagnosed with BC within three years preferred to play active or collaborative roles, while 70% of the patients perceived that they actually played such decisional roles. In our current study with 650 self-identified patients with BC, active and collaborative roles were preferred by the majority of participants (87%) and these roles were actually played (78%) (Table 1). These data suggest that Japanese patients with BC are more likely to prefer and perform affirmative involvement in the treatment decision-making process rather than entrusting their physicians to make the decision for them.
Using the same CPS questionnaire in this study, a high proportion of passive role was determined among German patients with BC (Vogel et al., 2008). Among study subjects, 40% preferred passive involvement, while 52% played a passive role. Additionally, the number of patients who thought that they did not have a choice in treatment was higher in the passive preference group (42%) as compared with the active (23%) and collaborative (35%) groups. This suggests that limited treatment choices for patients who are diagnosed with advanced cancer are a determinant for BC patients to choose a more passive role in treatment decision-making. Participants in the present study were mostly diagnosed with early stage cancer and they were more likely to play active roles in their cancer treatment choice (Table 1), suggesting that having more treatment choices led to a relatively low proportion of both preferred and actual passive roles in Japanese participants. Two studies, in which about 90% of participants had early stage BC, suggest that treatment choices affect decisional roles in treatment-decision making. In the study conducted in Canada, 78% of BC patients preferred an active or collaborative role (Hack et al., 2006). Similar to results observed in Japanese BC patients, a study conducted in an Asian country reported that 83% of participants perceived that they played an active or collaborative role (Mohamed et al., 2013). In our study, preferred and actual roles did not differ by sociodemographic and clinical status except for a difference in actual roles based on cancer stage. This suggests that patients who do not have treatment choices are more likely to entrust their physicians with the decision-making.
As the practice of shared decision-making has been recommended in oncological settings, questions have been raised as to whether this approach is beneficial to patients who prefer making their own decisions or trusting their physicians to decide on their behalf. In the present study, satisfaction among the participants who were involved in a collaborative decision-making was higher than that among the participants who played an active or a passive role (Figure 1(A)). However, previous studies of Japanese BC patients have shown that study subjects are highly satisfied with the decision-making process, regardless of their preferred and actual roles (Kokufu et al., 2012; Nakashima et al., 2012). Consequently, we investigated how decisional role congruity that is, the congruity of preferred and actual roles influences patient satisfaction with the decision-making process. Results in Figure 1(B) indicate that satisfaction level was significantly higher for participants when their preferred and actual roles were congruent in contrast to when they were incongruent, while the main effect of the actual role was not significant. This suggests that playing their preferred role, rather than the actual role played, is the key to increasing their satisfaction with the decision-making process. Decisional role congruity was found to be the most influential among participants who played a passive role. Specifically, participants who willingly entrusted their doctors with making their medical decisions showed significantly higher satisfaction when compared to those who preferred a more active role but were nevertheless consigned to a passive role (Figure 1(B)). Atherton (2013) reported that QOL, evaluated using SF-36, did not differ according to the decisional role played by cancer patients, however, QOL scores were significantly higher when preferred and actual decisional roles were incongruent. This was interpreted to mean that the higher QOL found for patients whose decisional roles were congruent was a consequence of satisfaction with the treatment decision-making. Our results are consistent with these findings, emphasizing that engagement in the decision-making in the patient’s preferred manner increases satisfaction with the process, which in turn, can positively affect the patient’s overall QOL.
We examined whether sociodemographic and clinical characteristics interact with decisional role congruity in influencing satisfaction with the treatment decision-making process. Hack (2006) showed that congruence of decisional roles was not associated with either sociodemographic or clinical characteristics, which is consistent with our findings except for one variable. Our study result showed that education level was the only sociodemographic status that interacted with decisional role congruity (Table 3). Compared with participants with more than high school education, participants with high school or lower education had significantly high satisfaction when decisional roles were congruent; however, they had significantly low satisfaction when decisional roles were incongruent. Regarding this association of education level with decisional roles, the meta-analysis conducted by Singh (2010) showed that the preferred roles differed by educational level: patients who had graduated with a high school education preferred a passive role compared to patients who had more than a high school education. A previous Japanese study showed that BC patients who have a high school degree preferred a more passive role than patients with a college degree or higher (Nakashima et al., 2012). Our study showed that when decisional roles were congruent, the satisfaction among participants with no more than a high school education were higher than that of highly educated participants. This result suggests that engaging in decision-making in their preferred manner leads to satisfaction in this process for BC patients with a low education background. Further study is required to understand the interaction of educational level with decisional role congruity in the satisfaction with the treatment decision-making process.
The expression of preference for the role that a BC patient would like to play, if she were confronted with a similar situation in the future, can reflect the current level of satisfaction with the role that she has played. The present study found that if they played their preferred role, 80% of the women would play the same role if they were to face a similar situation in the future. However, only one third of the women who played an unwanted role would play the same, and remaining two thirds would move to a more active or passive role. The high satisfaction with the decision-making process among Japanese BC patients was discussed based on their expression at the time the studies were conducted (Kokufu et al., 2012; Nakashima et al., 2012), leading to overestimation of their satisfaction. Hack (2006) assessed the satisfaction among women who had BC surgery three years prior to the study based on the patients’ preference if they had to redo the decision-making for surgery. Even then, approximately 90% stated that they were satisfied with treatment they received, only 48% would like to play same decisional role and 41% would like to play a more active. Most of their dissatisfaction was related to inadequate communication with their healthcare providers. Similarly, satisfaction based on decisional role congruity and preferred role in the future was high in our study; however, 66% of the participants who played unwilling roles would not choose same role in the future, implying their dissatisfaction. In order to provide better healthcare, we have to elucidate the factors that result in dissatisfaction with the decision-making process in women with BC and the barriers preventing them from participating in the process in their preferred manner.
There are a few limitations in this study. Firstly, the participants in this study had registered with an online marketing research company in advance, implying the possibility of differences in attitude on the part of these participants as compared to those who had not registered. We will need to expand our investigation to a more diverse of sampling of people, including women who are unwilling to talk openly about their experience with cancer. However, internet survey enabled us to recruit participants from a variety of regions and age groups. This survey method lowers the bias such as differences in healthcare level and access to specialists over the residential area. This is a study strength as previous studies with Japanese BC patients were conducted in a single city with small number of subjects. In terms of clinical application to Japanese BC patients, our results from a wider area in Japan may have a greater potential to be generalized. Regardless, our results increase knowledge about the association between treatment decision–making satisfaction and decisional roles.
Secondly, we did not elicit information on the barriers that prevented study participants from engaging in their preferred manner in the decision-making process. This would include details about their dissatisfaction. Gathering such information will help to implement our findings and allow practitioners to act on our conclusion that congruence between preferred and actual role in the treatment decision-making process increases satisfaction among women diagnosed with BC.
Thirdly, we need to study the healthcare providers’ satisfaction and dissatisfaction in the treatment decision-making process since our ultimate goal is to provide information for better intervention to increase BC patients’ satisfaction with treatment-decision making,
In conclusion, irrespective of their actual decision role, sociodemographic and clinical status, satisfaction with the medical decision-making process among Japanese women with breast cancer is increased when their participation matches their preferred manner of participation.
Funding Statement
This study was supported in part by Grant-in-Aid for Challenging Exploratory Research 25670254 from Japan Society for the Promotion of Science, Japan.
Abbreviations
ANOVA, Analysis of variance; BC, Breast cancer; CPS, Control preference scale; SF-36, 36-item short-form health survey; QOL, Quality of life.
Acknowledgements
We would like to thank Ms. Tomoe Terasaki for manuscript preparation. We are also grateful to the women who participated in this study.
References
- Almyroudi A, Degner LF, Paika V, Pavlidis N, Hyphantis T. Decision-making preferences and information needs among greek breast cancer patients. Psychooncology. 2011;20:871–9. doi: 10.1002/pon.1798. [DOI] [PubMed] [Google Scholar]
- Atherton P, Smith T, Singh J, et al. The relation between cancer patient treatment decision-making roles and quality of life. Cancer. 2013;119:2342–9. doi: 10.1002/cncr.28046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Degner LF, Kristjanson LJ, Bowman D, et al. Information needs and decisional preferences in women with breast cancer. JAMA. 1997;277:1485–92. [PubMed] [Google Scholar]
- Hack TF, Degner LF, Watson P, Sinha L. Do patients benefit from participating in medical decision making? Longitudinal follow-up of women with breast cancer. Psychooncology. 2006;15:9–19. doi: 10.1002/pon.907. [DOI] [PubMed] [Google Scholar]
- Hyphantis T, Almyroudi A, Paika V, et al. Anxiety, depression and defense mechanisms associated with treatment decisional preferences and quality of life in non-metastatic breast cancer:A 1-year prospective study. Psychooncology. 2013;22:2470–7. doi: 10.1002/pon.3308. [DOI] [PubMed] [Google Scholar]
- Kokufu H. Conflict accompanying the choice of initial treatment in breast cancer patients. Jpn J of Nurs Sci. 2012;9:177–84. doi: 10.1111/j.1742-7924.2011.00200.x. [DOI] [PubMed] [Google Scholar]
- Kwait RM, Pesek S, Onstad M, et al. Influential forces in breast cancer surgical decision making and the impact on body image and sexual function. Ann Surg Oncol. 2016;23:3403–11. doi: 10.1245/s10434-016-5365-2. [DOI] [PubMed] [Google Scholar]
- Maly RC, Umezawa Y, Leake B, Silliman RA. Determinants of participation in treatment decision-making by older breast cancer patients. Breast Cancer Res Treat. 2004;85:201–9. doi: 10.1023/B:BREA.0000025408.46234.66. [DOI] [PubMed] [Google Scholar]
- Mohamed N, Muhamad M. Older women breast cancer survivors:Decision making, sources of information and wellness activities in Malaysia. Asian Pac J Cancer Prev. 2013;14:2043–8. doi: 10.7314/apjcp.2013.14.3.2043. [DOI] [PubMed] [Google Scholar]
- Nakashima M, Kuroki S, Shinkoda H, et al. Information-seeking experiences and decision-making roles of Japanese women with breast cancer. Fukuoka Igaku Zasshi. 2012;103:120–30. [PubMed] [Google Scholar]
- Singh JA, Sloan JA, Atherton PJ, et al. Preferred roles in treatment decision making among patients with cancer:A pooled analysis of studies using the control preferences scale. Am J Manag Care. 2010;16:688–96. [PMC free article] [PubMed] [Google Scholar]
- The Editorial Board of Cancer Statistics in Japan. ‘Projection of cancer mortality and incidence in 2015’. Tokyo: Foundation for Promotion of Cancer Research; 2016. Cancer statistics in Japan 2015; p. 14. [Google Scholar]
- Vogel BA, Helmes AW, Hasenburg A. Concordance between patients’ desired and actual decision-making roles in breast cancer care. Psychooncology. 2008;17:182–9. doi: 10.1002/pon.1215. [DOI] [PubMed] [Google Scholar]


