Abstract
Adaptive changes in oxygenation and hemodynamics are evaluated during pediatric laparoscopy. The children underwent laparoscopy (LAP Group, n=20) or open surgery (Open Group, n=10). Regional cerebral (rScO2) and peripheral oxygen saturation (SpO2), heart rate (HR), diastolic (DP) and systolic pressure (SP) were monitored at different intervals: basal (T0); anesthesia induction (T1); CO2PP insufflation (T2); surgery (T3); CO2PP cessation (T4); before extubation (T5). At T1, in both the LAP and Open groups significant changes in rScO2, DP and SP were recorded compared with T0; a decrease in SatO2 was also observed at T5. In the LAP group, at T2, changes in HR related to CO2PP pressure and in DP and SP related to IAP were noted; at T4, a SP change associated with CO2PP desufflation was recorded. Open group, at T3 and T5 showed lower rScO2 values compared with T1. Pneuperitoneum and anesthesia are influent to induce hemodynamics changes during laparoscopy.
Key words: laparoscopy, children, hemodinamics, changes
Competing interest statement
Conflict of interest: the authors declare no potential conflict of interest.
Introduction
The laparoscopic surgical technique in children and infants is still undergoing development and refinement. To date, its effects on systemic and cerebral oxygenation have not been completely investigated1-3 and the exact effects of surgical maneuvers in combination with conventional anesthesiological procedures in hemodynamic regulation are still debated. Hemodynamic alterations, associated with abdominal laparoscopy are mainly caused by the increased intra-abdominal pressure (IAP), brought on by pneumoperitoneum (PP) creation. A decrease in venous return secondary to inferior vena cava compression and the increase in central venous pressure and arterial blood pressure, in the absence of heart rate (HR) changes, seem to be the main adaptive responses.4-6 A 10% to 30% decrease in cardiac output with severe pathophysiologic modifications has also been reported in most studies,7-9 underscoring the need for dedicated anesthesiological support in pediatric laparoscopy, especially in infants. Pathophysiological hemodynamic alterations during laparoscopic procedures in children have not been fully investigated.10-15 Therefore, in small children and in surgical procedures of long duration, the standardization of mini invasive intraoperative assessment requires close anesthesiological monitoring to prevent adverse hemodynamic outcomes.16,17
The anesthesiologist should have a deep understanding of the consequences associated with PP creation; and it is critical that the anesthesiologist be prepared to detect and address possible alterations that may occur during laparoscopic interventions.
In the present study, we evaluated whether adaptive changes in cerebral and systemic oxygenation and in hemodynamics are intraoperatively induced by IAP increases and PP-associated CO2 changes. The contribution of knowledge on the real impact of anesthesia on hemodynamic regulation during pediatric laparoscopic procedures was also considered.
Materials and Methods
Patients
The initial inclusion criteria for recruitment in the study were as follows: thirty children (21M/9F), aged 1 to 18 years (mean age 8.1±5.1 yr), scheduled for elective abdominal surgical procedures for congenital unilateral inguinal hernia repair. The treatment group (LAP Group: 20 children, 12M/8F, mean age 9.6±5.1) underwent laparoscopic surgery, while the control group underwent traditional open surgery (Open Group: 10 children, 9M/1F, mean age 5.1±4.1).
Surgery was performed by an experienced surgeon, under general endotracheal anesthesia. To critically analyze and synthesize current evidence, we performed an analysis of the completed results from both groups. Patients were consecutively recruited between 1 February 2016 and 31 June 2016, at the Pediatric Surgery Unit of the Fondazione IRCCS Policlinico San Matteo, Pavia, Italy. Written consent was obtained from the parents of the children before the scheduled surgical procedure. The study was performed according to the Declaration of Helsinki and with the approval of the Institutional Review Board.
Surgery
All surgeries were performed in the same operating theater with a stable temperature of 22±1 °C. Patients were placed in the supine position on a heated operating table (36±1°C). Laparoscopic treatment was accomplished, following a standard protocol, via the trans-abdominal approach using one 3 mm telescope and two, 3 mm or 2 mm, surgical instruments, placed into the lower abdomen. The pneumoperitoneum (PP) was created with a 3 mm infra-umbilical camera-trocar placed via an open approach. The PP CO2 pressure, which ranged from 8 to 12 mmHg (8 mmHg in children weighing <15 kg; 10 mmHg: 15-40 kg; 12 mmHg: >40 kg), was achieved with a CO2 insufflation flow rate of 1 L/min.
Patients included in the control group underwent a traditional open-surgery procedure. All interventions were performed on a day hospital basis and patients were followed for one week.
Data acquisition
Intraoperative transcranial near-infrared spectroscopy (NIRS) was used to assess regional cerebral oxygen saturation (rScO2), pulse oximetry was used to measure peripheral oxygen saturation using (SpO2); and HR, diastolic (DP), systolic pressure (SP) and end-tidal CO2 were monitored continuously during the entire procedure.
Changes in rScO2 were measured using a near-infrared spectrometer. Prior to anesthesia induction, a transducer was placed on the frontal side of the child's head and attached with an elastic bandage to prevent displacement. The oximeter sensor was positioned on the middle finger of the left hand. HR was recorded during scanning also using pulse oximetry for heart timing and an index of pulse amplitude.
Indirect data on IAP during surgery were collected via dynamic urethral pressure measurements with a high-resolution manometry system and recorded with Medical Measurement Systems® (Enschede, the Netherlands).
The following parameters were analyzed, every minute for five minutes (mean values were used for the statistical analysis), at five intervals: basal (T0) in LAP and Open groups; induction of anesthesia (T1) in LAP and Open groups; CO2 PP insufflation (T2) in the LAP group; surgery (T3) in LAP and Open groups; cessation of CO2 PP (T4) in the LAP group; before extubation (T5) in LAP and Open groups.
The operative times were recorded, including data acquisition and anesthesia duration (interval from beginning of induction to cessation of sevoflurane inhalation). The anesthesiologists were not blinded to the data readings to prevent intraoperative alterations in the children.
Anesthesia protocol
All children were in good physical condition (ASA, American Society of Anesthesiologists, class 1) and received standard anesthesia. Induction was performed endovenously (e.v.) with propofol (2-4 mg/Kg) and fentanyl (1 μg/Kg); and for muscle relaxation, cisatracurium 0.1 mg/Kg was given e.v.
After tracheal tube positioning, patients underwent volume controlled mechanical ventilation with a tidal volume of 8 mL/Kg, the respiratory rate adjusted to achieve an end-tidal CO2 of 32–37 mmHg, an I:E ratio of 1:2 (avoiding dynamic hyperinflaction) with a low-flow breathing system and an inspired mixture of air and oxygen (fresh gas flow of 4 1 min–1 with 40% FiO2 during anesthesia). Anesthesia was maintained via administration of Sevoflurane gas (0.9 to 1.3 MAC range). The anesthesiology protocol did not include hypotension management with fluid expansion or inotropes. Twenty minutes before the end of the intervention, all patients received Paracetamol 15 mg/kg, as an analgesic. The analgesia was consolidated with surgical wound infiltration using levobupivacaine and lidocaine for both open and laparoscopic surgery.
Statistical analysis
Quantitative variables were described as the mean (SD) and compared among the different time intervals with population averaged mixed multilevel models to take into account the clustered nature of the data.
Probability values of less than 0.05 were considered statistically significant. All statistical analyses were performed using the SPSS statistical package (SPSS, Chicago IL, USA) and Stata 8.0.
Results
During the surgical procedure, a significant variation in rScO2 was observed at the different time points in comparison with basal values (P<0.01). In the LAP group, a significant rScO2 increase was noted at T1 (P<0.00l). The intraoperative rScO2 values at T2 (P=0.6), T3 (P=0.4), T4 (P=0.5) and T5 (0.7) were not different compared with T1. The minimal rScO2 variations during the laparoscopic procedure were not related to PP pressure (P=0.5) or CO2 flow rate (P=0.8).
In the Open group a significant rScO2 increase was recorded at T1 (P<0.00l). At T3 (P=0.007) and T5 (P=0.007) rScO2 was significantly lower than at T1. The rScO2 profile and parameter mean values are reported in Figure 1A and Table 1.
Figure 1.
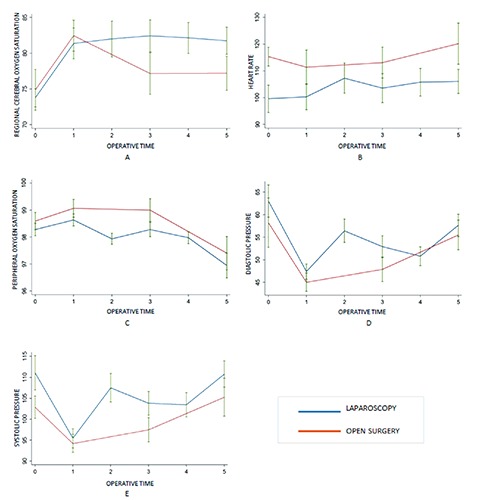
Profile of regional cerebral oxygen saturation (A), heart rate (B), peripheral oxygen saturation (C), diastolic pressure (D) and systolic pressure (E) in LAP and OPEN groups at the different surgical time points.
Table 1.
Hemodynamic mean values at the different surgical time points.
| Parameters | LAP group | Open group |
|---|---|---|
| Operative time (mean±SD) | 102±37.2 | 71±36.57 |
| NIRS | ||
| T0 | 73.8±5.7 | 74.9±9.0 |
| Tl | 81.3±9.6 | 82.4±6.8 |
| T2 | 82.0±11.1 | - |
| T3 | 82.4±10 | 77.1±9.2 |
| T4 | 82.1±9.7 | - |
| T5 | 81.7±8.4 | 77.2±7.5 |
| Heart rate | ||
| T0 | 99.5±22.9 | 115.3±11.1 |
| Tl | 100.3±21.6 | 111.4±20.3 |
| T2 | 107.3±25.2 | - |
| T3 | 103.5±24.1 | 113.1±18.3 |
| T4 | 105.7±23.0 | - |
| T5 | 106.1±20.3 | 120.2±24.3 |
| SatO2 | ||
| T0 | 98.2±1.0 | 98.6±1 |
| Tl | 98.6±1.0 | 99.0±1 |
| T2 | 97.9±0.9 | - |
| T3 | 98.3±1.2 | 99.0±1.3 |
| T4 | 97.9±0.1 | - |
| T5 Diastolic PA | 96.9±2.5 | 97.4±1.9 |
| T0 | 63.1±15.1 | 58.2±17.3 |
| Tl | 47.3±7.6 | 46.6±7.2 |
| T2 | 56.4±11.6 | 51.2±10.3 |
| T3 | 50.7±9.3 | 51.2±10.2 |
| T4 | 50.8±9.3 | - |
| T5 | 57.6±11.0 | 55.5±10.3 |
| Systolic PA | ||
| T0 | 111.1±17.4 | 102.9±8.5 |
| Tl | 94.2±6.8 | 95.0±9 |
| T2 | 107.5±15.2 | - |
| T3 | 103.8±12.7 | 101.7±11.9 |
| T4 | 103.4±13.0 | - |
| T5 | 110.8±13.7 | 105.3±13.5 |
| End-tidal CO2 | ||
| T0 | - | - |
| Tl | 35.8±5.8 | 41.9±6.7 |
| T2 | 36.7±5.3 | - |
| T3 | 38.3±4.8 | 37.5±6.3 |
| T4 | 37.8±4.8 | - |
| T5 | - | - |
Heart rate
HR showed significant changes during the entire surgical procedure in comparison with T0 (P=0.02). In the LAP group, HR was significantly higher at T2 compared with T0 (P=0.04). HR changes were related to CO2 PP pressure (P=0.002). An HR increase was also observed at T5 (P=0.009) compared with basal values.
In the Open group, HR changes at T1 (P=0.4), T3 (P=0.6) and T5 (P=0.3) were not significantly different in comparison with T0. The HR profile and parameter mean values are given in Figure 1B and Table 1.
Peripheral oxygen saturation
The SatO2 values were significantly different during the surgical intervention (P<0.00l).
In the LAP group, a significant rScO2 increase was noted at T1 (P=0.00l). The SatO2 values at T2 were not significantly different in comparison with T0 (P0.3), but were lower than T1 (P=0.06). The SatO2 differences between T0 and T3 and T4 were not significant (P0.9 and P0.4, respectively). A relevant decrease in SatO2 was observed at T5 in comparison with T0 (P<0.00l). In the Open groups, SatO2 at T1 (P0.27) and T3 (P0.34) was not different in comparison with T0. A significant decrease in SatO2 was recorded at T5 compared to T0 (P<0.00l). The SatO2 profile and parameter mean values are reported in Figure 1C and Table 1.
Diastolic pressure
The changes in DP values were significant during the surgical intervention (P<0.00l). In the LAP group, a decrease in DP was significantly induced at T1 (P<0.00l). At T2, even though the DP was lower than at T0 (P=0.01), an increase in pressure was recorded compared with T1 (p<0.001); these changes were related to CO2 PP (P<0.00l). During the surgical procedure, DP values remained significantly lower compared with T0 (P<0.00l), without a significant difference between T4 and T1 (P0.13). A DP recovery was observed at T5 (P=0.05).
In the Open group, a significant decrease in DP was revealed at T1 (P<0.00l). A progressive DP increase was recorded at T3 (P=0.006) and T5 (P=0.05). The DP profile and parameter mean values are given in Figure 1D and Table 1.
Systolic pressure
The SP values were significantly different during the surgical intervention (P<0.00l). In the LAP group, a decrease in SP was significantly induced at T1 (P<0.00l). At T2, an increase in pressure was recorded (P=0.15 vs T0; P<0.001 vs T1); these changes were related to LAP (P<0.001). SP remained lower at T3 (P=0.006) and T4 (P=0.004) compared with T0. At T4, the SP change was related to CO2 PP desufflation (P<0.00l). At T5, no significant SP difference was noted in comparison with T0 (P0.6).
In the Open group, a significant decrease in SP was revealed at T1 (P=0.01). A progressive systolic PA increase was recorded at T3 (P0.13) and T5 (P0.5). The SP profile and parameter mean values are given in Figure 1E and Table 1.
End-tidal CO2
During the surgical procedure, no significant variations in End-tidal CO2 were observed at the different time points in comparison with T1 (P0.37). The End tidal mean values are provided in Table 1. In Table 1, the hemodynamic mean values at the different surgical time points are reported.
Discussion
During laparoscopic procedures in children, adaptive changes in cerebral and systemic oxygenation and hemodynamic parameters are observed. These changes are related to pathophysiological consequences induced by PP creation and the impact of general anesthesia. Adverse hemodynamic events may be prevented with stringent intraoperative technical monitoring and strict standardization of the pediatric anesthesiological protocol. As in adults, pediatric laparoscopy is less invasive in nature, thereby providing a more rapid recovery, shorter hospital stay, decreased postoperative pain and improved cosmetic outcome when compared with traditional open surgery. Nevertheless, the procedure may be associated with hemodynamic alterations generated by the high intra-abdominal pressure brought on by PP creation and by the existence of insufflation gas that is absorbed by the blood. These systemic hemodynamic alterations may result in changes in end-organ blood flow and oxygen delivery. In addition, the impact of anesthesia on hemodynamic changes during laparoscopy should be considered.15,18-21 To date, data regarding hemodynamic changes during laparoscopy are conflicting and further evaluations in very small children represent new research perspectives for the near future. The most commonly studied parameters are HR, systemic vascular resistance, mean arterial pressure and central venous pressure. Increases and decreases in virtually all of the parameters noted above have been described after the institution of PP. The data vary in relation to the many factors affecting these values such as the child's weight and age.22
Significant changes in cerebral oxygenation occur in some patients during CO2 insufflation. To date, the data collected regarding alterations in cerebral oxygenation during laparoscopic procedures in children have been limited and non-homogenous.11-15
Previously, we reported on changes in cerebral oxygenation during laparoscopic procedures in pediatric patients, when stringent monitoring was not adopted.15 In this study, we closely monitored cerebral oxygenation with NIRS and the anesthesiologists were not blinded to the readings to prevent intraoperative alterations. Under these conditions, we showed that CO2 insufflation during PP may not influence cerebral oxygenation during laparoscopic surgery. These results suggest that the impact of anesthesia on adaptive changes should not be underestimated and confirm that this technology may be useful to anticipate any potential decrease in brain oxygenation. Rapid recognition of low cerebral perfusion and prompt correction is a challenge and the main goal is to avoid negative postoperative neurodevelopmental outcomes following pediatric surgical procedures. The anesthesiologist should be specifically prepared to manage this vulnerable population.23,24
In this study we also collected data on the impact of CO2 insufflation on peripheral oxygenation. Anesthesia induction and intraoperative management are critical determinants in peripheral oxygenation stability during laparoscopic procedures; in fact, during the latter part of surgery (last ten minutes), especially in very young children (whose muscles are very weak and do not intrude with surgical activity), a gradual reduction in ventilator assistance was adopted in order to facilitate gradual recovery of spontaneous breathing.25,26
According to the literature, increases in arterial pressure during peritoneal insufflation have been noted. Moreover, we showed that a significant decrease in diastolic and systolic pressures, occurred at induction of anesthesia and during intraoperative surgical time points.
The pressure profile was similar in both open surgery and the laparoscopic surgical approach; this observation supports the hypothesis that PP creation is only partially responsible for pressure variations and underlines the importance of dedicated anesthesiological management in pediatrics even for traditional surgery.
As previously reported,15 during PP creation, an HR increase was recorded. The correlation between HR changes and CO2 flow rate support the role of a neurohumoral CO2 effect. CO2 stimulates the sympathoadrenal system causing a significant release of catecholamines and Cortisol and thus increased HR. The absorption of CO2 during positive pressure pneumoperitoneum may lead to an increased CO2 load. While a different CO2 reabsorption in infants and children has already been reported based on the different characteristics in their peritoneal surface, CO2 elimination is related to age with younger children eliminating more CO2 than older children.27
In most patients undergoing controlled ventilation, end-tidal CO2 closely reflects arterial CO2 tension.27 We did not measure arterial CO2 and arterial pH levels in this study, but we assume that because there were only minor changes in end-tidal CO2, that the blood gases did not change significantly. Clinically, we did not observe any adverse cardiovascular or respiratory events in our patients.
The present preliminary report has several limitations. The sample size was limited and a study on a larger number of children is mandatory to confirm the results. Secondly, it concerns a population with a broad range of ages, from 1 to 18 years, and the impact of IAP, absorption and elimination of CO2 and anesthesia protocols are different for infants, children and adolescents. The initial inclusion criteria for recruitment in the study selected an homogenous group of procedures, however the influence of the different operative times on the rScO2 cannot be excluded. The anesthesiologist's anesthesia technique and ventilation strategy to obtain the best parameters were not standardized. Additionally, the exact impact of the anesthesia on hemodynamics could be supported by hemodynamic evaluation during the standard anesthesia protocol and using different anesthesiological agents. Finally, arterial blood gas analysis monitoring would be useful during laparoscopic procedures; in our study, the routine procedure, did not call for invasive PaCO2 monitoring. This study points to new study directions to ameliorate our knowledge on the combined surgical and anesthesiological role on hemodynamic status in pediatric laparoscopy. With the advent of new mini invasive surgical approaches, there is a need for specific and dedicated anesthesiological procedures, particularly in children. Although anesthesia for laparoscopic surgery does not require a major extension of the traditional methods for pediatric abdominal surgery, special consideration must be given to alterations in cardiovascular and respiratory status that occur during the laparoscopic procedure.18-21 Children, infants and neonates represent an anesthesiological challenge because of age-specific anatomical and physiological issues. Apart from these pediatric-specific considerations, the pediatric anesthesiologist must understand the implications of laparoscopic surgery, and prevent or act accordingly to changes that will occur during these procedures.18-21 There is room for improvement in quality of care during the laparoscopic surgical approach in pediatrics.
Conclusions
This study demonstrates that pathophysiological hemodynamic alterations are influenced by both the procedure and the anesthesia during pediatric abdominal laparoscopic surgery. However, the exact role of each factor needs further research. Due to age-related homeostatic vulnerability, hemodynamic status should not be underestimated in pediatrics. Knowledge of the pathophysiological changes, the standardization of intraoperative surgical assessment and anesthesia management are all mandatory to prevent adverse hemodynamic outcomes. Future challenges will include appropriate application of combined minimally invasive surgery and anesthesiological protocols, while maintaining the child's safety during and after laparoscopic procedures.
Acknowledgments
The authors would thank Dr. L. Kelly for English revision of the manuscript.
References
- 1.Maesani M, Pares F, Michelet D, et al. Haemodynamic and cerebral oxygenation during paediatric laparoscopy in fluid optimized patients. Br J Anaesth 2016;116:564-6. [DOI] [PubMed] [Google Scholar]
- 2.de Waal EE, de Vries JW, Kruitwagen CL, et al. The effects of low-pressure carbon dioxide pneumoperitoneum on cerebral oxygenation and cerebral blood volume in children. Anesth Analg 2002;94:500-5. [DOI] [PubMed] [Google Scholar]
- 3.Schauer PR, Schwesinger WH. Hemodynamic effects of laparoscopy. Surg Endosc 1995;9:119-20. [DOI] [PubMed] [Google Scholar]
- 4.Gupta R, Singh S. Challenges in paediatric laparoscopic surgeries. Indian J Anaesth 2009;53:560-6. [PMC free article] [PubMed] [Google Scholar]
- 5.Tarn PK. Laparoscopic surgery in children. Arch Dis Child 2000;82:240-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hodgson C, McClelland R, Newton J. Some effects of the peritoneal insufflation of carbon dioxide at laparoscopy. Anaesthesia 1970;25:382-90. [DOI] [PubMed] [Google Scholar]
- 7.Joris JL, Hinque VL, Laurent PE, et al. Pulmonary function and pain after gastroplasty performed via laparotomy or laparoscopy in morbidly obese patients. Br J Anaesth 1998;80:283-8. [DOI] [PubMed] [Google Scholar]
- 8.Joris JL, Chiche JD, Canivet JL, et al. Hemodynamic changes induced by laparoscopy and their endocrine correlates: effects of clonidine. J Am Coll Cardiol 1998;32:1389-96. [DOI] [PubMed] [Google Scholar]
- 9.Wahba RW, Béïque F, Kleiman SJ. Cardiopulmonary function and laparoscopic cholecystectomy. Can J Anaesth. 1995;42:51-63. [DOI] [PubMed] [Google Scholar]
- 10.Tuna AT, Akkoyun I, Darcin S, et al. Effects of carbon dioxide insufflation on regional cerebral oxygenation during laparoscopic surgery in children: a prospective study. Braz J Anesthesiol 2016;66:249-53. [DOI] [PubMed] [Google Scholar]
- 11.Tsypin LE, Mikhel'son VA, Chusov KP, et al. Central and cerebral hemodynamics during gynecological laparoscopic interventions in children. Anesteziol Reanimatol 2007;1:30-2. [PubMed] [Google Scholar]
- 12.Tytgat SH, Stolwijk LJ, Keunen K, et al. Brain oxygenation during laparoscopic correction of hypertrophic pyloric stenosis. J Laparoendosc Adv Surg Tech 2015;A25:352-7. [DOI] [PubMed] [Google Scholar]
- 13.Tytgat SH, van Herwaarden MY, Stolwijk LJ, et al. Neonatal brain oxygenation during thoracoscopic correction of esophageal atresia. Surg Endosc Surg Endosc 2016;30:2811-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bishay M, Giacomello L, Retrosi G, et al. Decreased cerebral oxygen saturation during thoracoscopic repair of congenital diaphragmatic hernia and esophageal atresia in infants. J Pediatr Surg 2011;46:47-51. [DOI] [PubMed] [Google Scholar]
- 15.Pelizzo G, Bernardi L, Carlini V, et al. Laparoscopy in children and its impact on brain oxygenation during routine inguinal hernia repair. J Minim Access Surg 2017;13:51-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jackson HT, Kane TD. Advances in minimally invasive surgery in pediatric patients. Adv Pediatr 2014;61:149-95. [DOI] [PubMed] [Google Scholar]
- 17.Truchon R. Anaesthetic considerations for laparoscopic surgery in neonates and infants: a practical review. Best Pract Res Clin Anaesthesiol 2004;18:343-55. [DOI] [PubMed] [Google Scholar]
- 18.Lasersohn L. Anaesthetic considerations for paediatric laparoscopy. S Afr J Surg 2011;49:22-6. [PubMed] [Google Scholar]
- 19.Srivastava A, Niranjan A. Secrets of safe laparoscopic surgery: Anaesthetic and surgical considerations. J Minim Access Surg 2010;6:91-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ahmed A. Laparoscopic surgery in children: anaesthetic considerations. J Pak Med Assoc 2006;56:75-9. [PubMed] [Google Scholar]
- 21.Ahmed M, Nessa M, Islam MS, et al. Effects of pneumoperitoneum during laparoscopic surgery in young children. JAFCM Bangledesh 2009;5:18-20. [Google Scholar]
- 22.Hardacre JM, Talamini MA. Pulmonary and hemodynamic changes during laparoscopy: are they important? Surgery 2000;127:241-4. [DOI] [PubMed] [Google Scholar]
- 23.Rhondali O, Pouyau A, Mahr A, et al. Sevoflurane anesthesia and brain perfusion. Paediatr Anaesth 2015;25:180-5. [DOI] [PubMed] [Google Scholar]
- 24.Rhondali O, Juhel S, Mathews S, et al. Impact of sevoflurane anesthesia on brain oxygenation in children younger than 2 years. Paediatr Anaesth 2014;24:734-40. [DOI] [PubMed] [Google Scholar]
- 25.Goligher EC, Ferguson ND, Brochard LJ. Clinical challenges in mechanical ventilation. Lancet. 2016;387:1856-66. [DOI] [PubMed] [Google Scholar]
- 26.El-Khatib MF, Bou-Khalil P. Clinical review: liberation from mechanical ventilation. Crit Care 2008;12:221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.McHoney M, Corizia L, Eaton S, et al. Carbon dioxide elimination during laparoscopy in children is age dependent. J Pediatr Surg 2003;38:105-10. [DOI] [PubMed] [Google Scholar]


