Abstract
Progress in the treatment options for small cell lung cancer (SCLC) remains poor. Concerns exist regarding the efficacy of bevacizumab in SCLC. The present study aimed to evaluate the efficacy of bevacizumab in extensive stage (ES)-SCLC. A meta-analysis on studies conducted and listed on the Medline, Cochrane Trials, ASCO, ESMO and ClinicalTrial databases, and Chinese databases prior to April 2015 was performed. All clinical trials in which patients with ES-SCLC were treated with bevacizumab were considered. Survival rates at specific time points were extracted from the reported survival curves. Hazard ratios (HR) for progression-free survival (PFS) and overall survival (OS), rates for PFS, OS, overall response rate (ORR), and side-effects were synthesized using random-effects or fixed-effects model. Two randomized control trials (RCT) (176 patients) and six single-arm trials (292 patients) were identified. In RCTs, no statistically significant differences were observed in PFS [HR, 0.70; 95% confidence interval (CI), 0.41–1.19; P=0.19] or OS (HR, 1.21; 95% CI, 0.84–1.75; P=0.31). In the first-line trials, pooled 6-month and 1-year PFS rates were 57% (95% CI, 39–76%) and 10% (95% CI, 4–16%), respectively. Synthesized 1-year and 2-year OS rates were 45% (95% CI, 36–54%) and 10% (95% CI, 6–14%), respectively. Reported median PFS and OS times for pretreated patients were 2.7–4.0 months and 6.3–7.4 months, respectively. Pooled ORRs were 71% (95% CI, 59–82%) in the first-line trials and 18% (95% CI, 11–25%) in the second-line trials. The most common types of reported toxicities were chemotherapy-associated, including neutropenia, leukopenia, fatigue and thrombocytopenia. According to the RCTs, bevacizumab did not appear to improve the PFS or OS for patients with ES-SCLC, with low quality of evidence. Due to the disappointing pooled efficacy in the single-arm trials, more clinical studies on bevacizumab in SCLC may not be valuable, although the evidence was with low quality.
Keywords: bevacizumab, small cell lung cancer
Introduction
Small cell lung cancer (SCLC) is a rare disease; however, it accounts for 12–15% of all lung cancer cases and the majority of patients with SCLC present with the extensive-stage (ES) at diagnosis (1). Since the introduction of platinum plus etoposide in the early 1980s, there has been limited progression in ES-SCLC therapy. Despite its chemosensitivity, SCLC demonstrates a high relapse rate, with a median progression free survival (PFS) time of 4–7 months. The median overall survival (OS) time following relapse rarely exceeds7 months (2–5). Thus, the development of novel therapies to improve the efficacy of treatment for patients with ES-SCLC is warranted.
Molecular targeted therapies have achieved evident efficacies in other types of solid tumor, providing a more promising direction for the treatment of SCLC. In SCLC, increased vascular endothelial growth factor (VEGF) expression within the tumor and the blood supply peripheral to the tumor, and increased microvasculature surrounding the tumor have been observed (6,7). Thus, it has been suggested that bevacizumab may be an effective therapeutic agent for SCLC. However, concerns regarding the efficacy of bevacizumab have been made apparent in various randomized control trials (RCT) (8,9). In the SALUTE trial, the duration of PFS for patients in the bevacizumab treatment group (5.5 months) was longer compared with the placebo group (4.4 months) (8). By contrast in the IFCT-0802 trial, no significant differences in PFS or OS times were identified between the bevacizumab and chemotherapy combination treatment group and the chemotherapy alone group (9). Therefore in the present study, a literature-based meta-analysis of clinical trials was performed to investigate the efficacy and side-effects of bevacizumab in ES-SCLC.
Materials and methods
Searching strategy
Relevant papers were identified through a systematic search until 2 April 2015 on Medline (PubMed; www.ncbi.nlm.nih.gov/pubmed), American Society of Clinical Oncology (www.asco.org), European Cancer Societies (www.esmo.org), ClinicalTrial (http://www.clinicaltrials.gov/), Cochrane Library (www.cochranelibrary.com/) and on Chinese databases, including VIP (http://qikan.cqvip.com/), CNKI (http://www.cnki.net/), CBM (www.sinomed.ac.cn/), and WANFANG DATA (www.wanfangdata.com.cn/). The words ‘small cell lung cancer’ or ‘SCLC’ and ‘avastin’ or ‘bevacizumab’ were used to search through all titles, abstracts and keywords. Furthermore, the reference sections of review and original papers were scanned in order to identify any missing trials.
Trial identification and data extraction
All control and single-arm trials in which patients with ES-SCLC were treated with bevacizumab were considered. Data for time to tumor progression (TTP) or PFS, OS, overall response rate (ORR) and side-effects were extracted by two separate researchers (Ms. Yan-juan Zhu and Ms. Yi-hong Liu; Guangdong Provincial Hospital of Chinese Medicine, Guangzhou, China). Survival data (survival rates) in the reported survival curves at specific time points were extracted using DigitizeIt (version 2.0; Braunschweig, Germany; http://www.digitizeit.de/) (10).
Trial quality evaluation
For the RCTs, bias assessments were performed by two separate researchers (Ms. Yan-juan Zhu and Mr. Hai-Bo Zhang, Guangdong Provincial Hospital of Chinese Medicine) using RevMan (version 5.3; The Cochrane Collaboration- Oxford, UK) following recommendations from the Cochrane Handbook (version 5.1.0) (11). Bias, including random sequence generation, allocation concealment, blinding, incomplete outcome data and selective reporting were assessed. For the single-arm trials, bias assessments were performed according to the Cochrane Handbook, as no alternative tool was identified following literature search or advice from senior colleagues. However, bias due to random sequence generation, allocation concealment or blinding was not assessed. For the first-line trials, bias assessments were completed by Ms. Yan-Juan Zhu and Mr. Yong Li. For the second-line trials, the assessments were performed by Ms. Li-Rong Liu and Mr. Jian-Ping Bai.
Data synthesis
For RCTs, hazard ratios (HR) with 95% confidence intervals (CI) for PFS and OS were extracted, and synthesized. As only two RCTs were identified, the random-effect model was used with RevMan 5.3 due to the known clinical heterogeneity, as indicated by the I2 index. PFS and OS rates at specific time points were extracted from the reported survival curves. Rates for survival, ORR and side-effects were pooled using Stata/SE (version 11.0; StataCorp LP, College Station, TX, USA) with the random-effect model if there was significant heterogeneity, or with the fixed-effect model if no heterogeneity was present.
Evidence quality evaluation
The quality of evidences for PFS, OS and ORR was evaluated according to the GRADE guidelines (http://www.gradeworkinggroup.org/publications/JCE_series.htm), using GRADEpro (GDT, http://www.gradepro.org).
Results
Selected trials
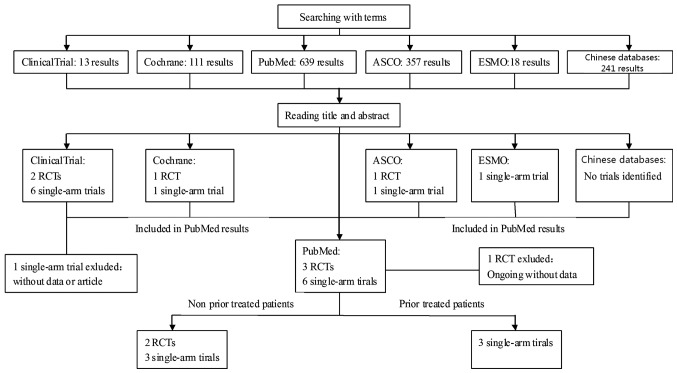
Three RCTs and six single-arm trials were identified (Fig. 1). One RCT (GOIRC-AIFA FARM6PMFJM trial) was excluded, as it is an ongoing trial without any reported data (12). The other two RCTs, IFCT-0802 (74 patients) (9) and SALUTE (102 patients) (8), and three of the single-arm trials, CALGB-30306 (64 patients) (13), LUN-90 (51 patients) (14) and ECOG-E3501 (63 patients) (15) evaluated the efficacy of bevacizumab as a first-line treatment for ES-SCLC. Survival curves for PFS and OS, in addition to the side-effects were reported in these five trials. ORRs were also reported, with the exception of in the IFCT-0802 trial. In the other three single-arm trials by Mountzios et al (16), Jalal et al (17) and Spigel et al (18), 114 prior treated patients were enrolled in total. Median OS, PFS, ORRs and side-effects were reported. The studies by Mountzios et al (16) and Spigel et al (18) reported survival curves for OS. Only the study by Spigel et al (18) reported the survival curve for PFS. Details of the nine studies described above are summarized in Table I.
Figure 1.
Outline of the search-flow diagram using multiple databases. ‘Small cell lung cancer’ or ‘SCLC’ and ‘avastin’ or ‘bevacizumab’ were used to search through all titles, abstracts, and keywords. ASCO, American Society of Clinical Oncology; ESMO, European Cancer Societies; RCTs, randomized clinical trials; SCLC, small cell lung cancer.
Table I.
Details of identified trials on patients with small cell lung cancer treated with bevacizumab.
| Study | No. of patients | Chemotherapy regimens | Bevacizumab strategy | Median PFS/TTP, months | Median OS, months | ORR, % | Most common types of toxicity (grades 3–4) | (Refs.) |
|---|---|---|---|---|---|---|---|---|
| First-line RCT | ||||||||
| IFCT-0802 | 37 (BC), 37 (C) | EP (81.1%): Etoposide 120 mg/m2 d1-3, cisplatin 80 mg/m2 d2 every 3 weeks; PCDE (18.9%): Etoposide 75 mg/m2 d1-3, cisplatin 75 mg/m2 d2, 4′-epidoxorubincin 30 mg/m2 d1, cyclophosphamide 300 mg/m2 d1-3 every 3 weeks | Chemo ×2 cycles, then chemo + Bev 7.5 mg/kg d1 every 3 weeks ×4 cycles, without maintenance | 6.8 (BC); 7.0 (C); HR, 0.91 (95% CI, 0.59–1.43)a | 12.6 (BC); 14.8 (C); HR, 1.25 (95% CI, 0.77–2.00)a | – | Neutropenia, 42.9 (BC), 35.1 (C); thrombocytopenia, 20 (BC), 10.7 (C); embolism, 11.4 (BC), 5.4 (C); mortality, 1 case with subdural hematoma and hypertension in bev group | (9) |
| SALUTE | 52 (BC), 50 (PC) | EP (31.4%): Etoposide 100 mg/m2 d1-3, cisplatin 75 mg/m2 d1 every 3 weeks; EC (68.6%): Etoposide 100 mg/m2 d1-3, carboplatin AUC 5 mg/ml/min d1 every 3 weeks | Chemo + Bev 15 mg/kg d1 every 3 weeks ×4 cycles, with maintenance | 5.5 (BC); 4.4 (PC); HR, 0.53 (95% CI, 0.32–0.86) | 9.4 (BC); 10.9 (PC); HR, 1.16 (95% CI, 0.66–2.04) | 58 (BC); 48 (BC) | Total, 75 (BC), 60 (PC); neutropenia, 35.3 (BC), 40.4 (PC); pneumonia, 5.9 (BC), 4.3 (PC); hypertension, 5.9 (BC), 4.3 (PC); mortality, 2 cases in bev group, including 1 with hemoptysis, 2 cases in the chemo group | (8) |
| First-line single arm trials | ||||||||
| CALGB-30306 | 64 | IP: Cisplatin 75 mg/m2 d1,8, irinotecan 65 mg/m2 d1,8 every 3 weeks | Chemo + Bev 15 mg/kg d1 every 3 weeks ×6 cycles, without maintenance | 7.00 | 11.6 | 75 | Total, 64; neutropenia, 25; electrocyte, 23; diarrhea, 16; mortality, 3 cases (congestive heart failure, pneumonia, CNS hemorrhage) | (13) |
| LUN-90 | 51 | IC: Carboplatin AUC 4 mg/ml/min d1, irinotecan 60 mg/m2 d1,8,15, every 4 weeks | Chemo + Bev 10 mg/kg d1,15 every 4 weeks ×6 cycles, with maintenance | 9.13 | 12.1 | 84 | Neutropenia, 39; thrombocytopenia, 22; diarrhea, 31; mortality, 3 cases (2 with infection and 1 with liver failure) | (14) |
| ECOG-E3501 | 63 | EP: Etoposide 120 mg/m2 d1-3, cisplatin 60 mg/m2 d1 every 3 weeks | Chemo + Bev 15 mg/kg d1 every 3 weeks ×4 cycles, with maintenance | 4.70 | 10.9 | 63.5 | Neutropenia, 57.8; thrombocytopenia, 14.1; fatigue, 14.1; mortality, 2 cases (1 with pneumonia caused by neutropenia, 1 with MOF) | (15) |
| Single arm trials in prior treated patients | ||||||||
| Mountzios et al | 30 | Paclitaxel 90 mg/m2 d1,8,15 every 4 weeks | Chemo + Bev 10 mg/kg d1,15 every 4 weeks ×6 cycles, without maintenance | 2.70 | 6.3 | 20.0 | Leukopenia, 20; neutropenia, 16.7; diarrhea, 10 | (16) |
| Jalal et al | 34 | Paclitaxel 90 mg/m2 d1,8,15 every 4 weeks | Chemo + Bev 10 mg/kg d1,15 every 4 weeks ×4–6 cycles, with maintenance | 3.40 | 7.0 | 18.1 | Fatigue, 26; neutropenia, 17.6; dyspnea, 14.7 | (17) |
| Spigel et al | 50 | Oral topotecan 2.3 mg/m2 d1-5 every 3 weeks | Chemo + Bev 15 mg/kg d1 every 3 weeks ≥ ×4 cycles, until progression | 4.01 | 7.4 | 16.0 | Thrombocytopenia, 32; neutropenia, 28; anemia, 18; mortality, 5 cases (4 were associated with the study medication, including 2 with sepsis, 1 with pneumonia andrespiratory failure, 1 with thrombocytopenia and GI hemorrhage) | (18) |
Median PFS reported was 5.3 (BC) vs. 5.5 (C) months, and median OS reported was 11.1 (BC) vs. 13.3 (C), which was 2 cycles of chemotherapy (6 weeks) subsequent to the initiation of treatment. PFS, progression-free survival; TTP, time to tumor progression; OS, overall survival; ORR, overall response rate; RCT, randomized control trial; BC, bevacizumab + chemotherapy; C, chemotherapy alone; EP, cisplatin + etoposide; EC, carboplatin + etoposide; PCDE, cisplatin + etoposide + 4′-epidoxorubincin + cyclophosphamide; chemo, chemotherapy; bev, bevacizumab; HR, hazard ratio; CI, confidence interval; PC, placebo + chemotherapy; AUC, area under the curve; IP, cisplatin + irinotecan; CNS, central nervous system; IC, carboplatin + irinotecan; MOF, multi-organ failure; GI, gastrointestinal.
Trial quality
Randomization in the two RCTs was stratified, however the random sequence generation or the allocation concealment was not reported. The IFCT-0802 trial was an open randomized study without blinding of participants, personnel or outcome assessment. The SALUTE was a placebo-controlled study, but the blindness of the outcome assessment was not reported. Considering that PFS and OS are objective outcomes, non-blinding is unlikely to introduce bias. In the IFCT-0802 trial, 8.6% of the bevacizumab-treated and 16.2% of the chemotherapy-treated groups of patients did not complete the protocol program. In the SALUTE trial, 30.8% of the bevacizumab-treated and 34.0% in the chemotherapy-treated groups did not complete protocol program. The two trials reported the intention-to-treat population analysis and were registered on the ClinicalTrial database. The SALUTE trial reported all the pre-specified outcomes of the protocol, while the IFCT-0802 trial did not report complete response length or quality of life, although these were planned in the protocol. According to the protocol of the IFCT-0802 study, the planned enrollment number was 143, while 74 patients were studied. No other biases were identified in the SALUTE trial.
Completed planned cycles of treatment were achieved in 64% of patients in the CALGB-30306, 57% of patients in the LUN-90 and a minority of the patients in the Jalal et al (17) trials. However, the majority of the reasons for incomplete planned cycles were due to disease progression or side-effects. Reasons for incomplete planned cycles in the other three trials were due to accepted patient withdrawals. A total of 5/6 single-arm trials are registered on the ClinicalTrial database, with the exception of the Mountzios et al (16) trial. The Spigel et al (18) study did not report the duration of tumor response [period from the first time of complete response (CR) or partial response (PR) to the first time of progressive disease (PD)] or time to tumor response (period from randomization to the first time of CR/PR), although planned in the protocol, while the other four trials reported all the pre-specified outcomes. The risk of bias for these trials is illustrated in Fig. 2.
Figure 2.
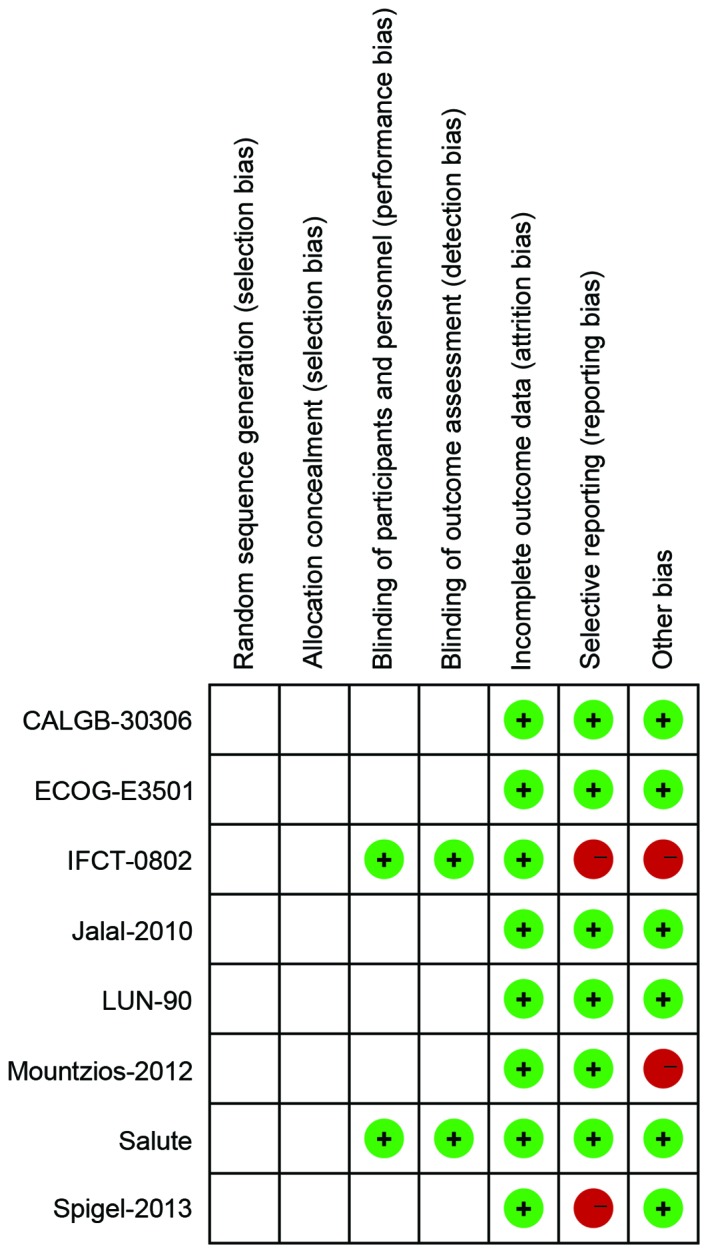
Risk of bias for each of the eight studies identified on the effects of bevacizumab on patients with small cell lung cancer.
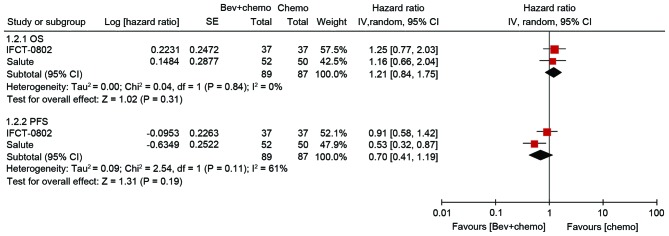
PFS and OS
In RCTs, no statistically significant differences were observed in PFS (HR, 0.70; 95% CI, 0.41–1.19; P=0.19) or OS (HR, 1.21; 95% CI, 0.84–1.75; P=0.31) between patients treated with or without bevacizumab. The heterogeneity for PFS was significant (I2=61%), but insignificant for OS (I2=0%; Fig. 3).
Figure 3.
Meta-analysis of the hazard ratios of PFS and OS for patients with small cell lung cancer treated with chemotherapy with or without bevacizumab. Bevacizumab and chemotherapy combination treatment appeared not to improve PFS or OS for ES-SCLC, compared with treatment with chemotherapy alone. PFS, progression-free survival; OS, overall survival; bev, bevacizumab; chemo, chemotherapy; SE, standard error of the mean; CI, confidence interval; df, degrees of freedom; I2, heterogeneity index; ES-SCLC, extensive stage small cell lung cancer.
A total of two RCTs and three single-arm trials evaluated the efficacy of bevacizumab as a first-line treatment for ES-SCLC. The PFS and OS rates were extracted from the survival curves reported, and the rates at specific time points were subsequently synthesized. The 6-month and 1-year PFS rates were 57% (95% CI, 39–76%; I2=91.3%), and 0.10 (95% CI, 4–16%; I2=55.2%), respectively. The 1-year and 2-year OS rates were 45% (95% CI, 36–54%; I2=60.8%), and 10% (95% CI, 6–14%; I2=0.0%), respectively. Pooled PFS and OS rates at specific time points are illustrated in Fig. 4 and Table II.
Figure 4.
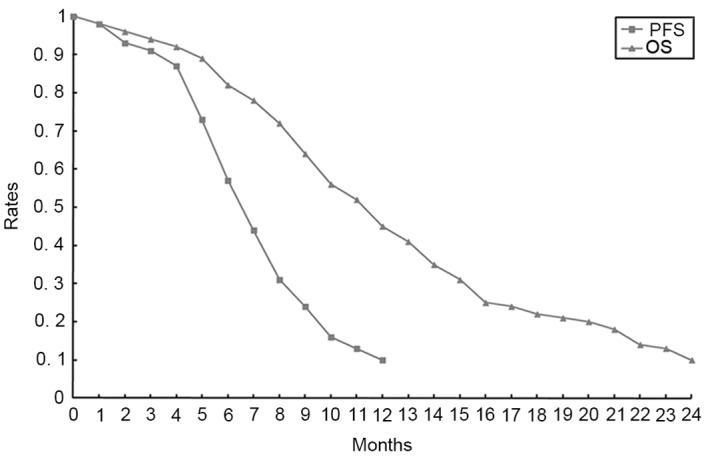
Pooled PFS and OS rates at specific time points for patients with small cell lung cancer treated with bevacizumab combined with chemotherapy as first-line therapy. PFS, progression-free survival; OS, overall survival.
Table II.
Pooled PFS and OS rates for patients with small cell lung cancer treated with bevacizumab as first-line therapy.
| Months | Rates % (95% CI) | I2 (%) | Months | Rates % (95% CI) | I2 (%) | Months | Rates % (95% CI) | I2 (%) |
|---|---|---|---|---|---|---|---|---|
| Pooled PFS rates | ||||||||
| 1 | 0.98 (0.96–1.00) | 38.6 | 2 | 0.93 (0.85–0.97) | 67.7 | 3 | 0.91 (0.86–0.95) | 44.1 |
| 4 | 0.87 (0.80–0.94) | 66.5 | 5 | 0.73 (0.58–0.87) | 87.7 | 6 | 0.57 (0.39–0.76) | 91.3 |
| 7 | 0.44 (0.27–0.61) | 89.5 | 8 | 0.31 (0.14–0.48) | 91.6 | 9 | 0.24 (0.10–0.38) | 89.7 |
| 10 | 0.16 (0.08–0.23) | 67.6 | 11 | 0.13 (0.05–0.22) | 75.9 | 12 | 0.10 (0.04–0.16) | 55.2 |
| Pooled OS rates | ||||||||
| 1 | 0.98 (0.97–1.00) | 0.0 | 2 | 0.96 (0.93–0.99) | 51.4 | 3 | 0.94 (0.90–0.98) | 64.3 |
| 4 | 0.92 (0.86–0.97) | 71.0 | 5 | 0.89 (0.84–0.89) | 35.1 | 6 | 0.82 (0.77–0.87) | 6.3 |
| 7 | 0.78 (0.73–0.83) | 0.0 | 8 | 0.72 (0.65–0.79) | 38.2 | 9 | 0.64 (0.55–0.72) | 55.7 |
| 10 | 0.56 (0.45–0.66) | 67.3 | 11 | 0.52 (0.43–0.60) | 53.7 | 12 | 0.45 (0.36–0.54) | 60.8 |
| 13 | 0.41 (0.33–0.50) | 52.7 | 14 | 0.35 (0.26–0.44) | 60.2 | 15 | 0.31 (0.24–0.38) | 43.8 |
| 16 | 0.25 (0.20–0.31) | 0.0 | 17 | 0.24 (0.19–0.29) | 0.0 | 18 | 0.22 (0.17–0.27) | 0.0 |
| 19 | 0.21 (0.16–0.26) | 0.0 | 20 | 0.20 (0.15–0.25) | 0.0 | 21 | 0.18 (0.13–0.22) | 0.0 |
| 22 | 0.14 (0.10–0.19) | 0.0 | 23 | 0.13 (0.09–0.18) | 0.0 | 24 | 0.10 (0.06–0.14) | 0.0 |
PFS, progression-free survival; OS, overall survival; CI, confidence interval; I2, heterogeneity index.
Three of the single-arm trials evaluated the efficacy of bevacizumab in patients with ES-SCLC who had received previous treatment. The median OS and PFS times are detailed in Table I. Only two trials reported survival curves for OS and one PFS survival curves. Survival rates were not synthesized due to the limited data reported.
ORR
ORRs for bevacizumab combined with chemotherapy as a first-line treatment were reported in one RCT and three single-arm trials. The synthesized ORR value for bevacizumab combined with chemotherapy from these four trials was 71% (95% CI, 59–82%), with significant heterogeneity (I2=75.9%; P=0.006). The synthesized ORR value for bevacizumab and chemotherapy combined treatment from the three single-arm trials for patients who had received prior treatment was 18% (95% CI, 11–25%), without significant heterogeneity (I2=0.0%; P=0.901).
Safety
In Table III, the synthesized grade 3–4 toxicities are detailed. No unexpected toxicity was reported. The most common types of reported toxicities were chemotherapy-associated, including neutropenia (39.8%), leukopenia (20.4%), fatigue (13.4%), diarrhea (13.0%) and thrombocytopenia (12.2%) in the first-line treatment patients. Thrombocytopenia (32.0%), neutropenia (21.0%) and fatigue (15.4%) were most common in patients who had received previous treatment. A total of 16 mortalities were reported, including seven with infection (two with sepsis), two with central nerve system hemorrhage, one with congestive heart failure, one with hemoptysis, one with gastrointestinal hemorrhage, one with liver failure and one with multi-organ failure.
Table III.
Pooled grade 3 to 4 toxicities for patients with small cell lung cancer treated with bevacizumab.
| Patients who did not receive prior treatment | Patients who received prior treatment | |||||
|---|---|---|---|---|---|---|
| Toxicity | Rates % (95% CI) | I2 (%) | No. of synthesized studies | Rates % (95% CI) | I2 (%) | No. of synthesized studies |
| Neutropenia | 39.8 (28.0–51.6) | 76.3 | 5 | 21.0 (13.6–28.4) | 0.0 | 3 |
| Febrile neutropenia | 6.4 (2.9–10.0) | 0.0 | 3 | 3.3 | – | 1 |
| Leukopenia | 20.4 (9.5–31.2) | 71.8 | 3 | 14.3 (6.6–21.9) | 0.0 | 2 |
| Thrombocytopenia | 12.2 (5.9–18.5) | 63.8 | 5 | 32.0 | – | 1 |
| Anemia | 6.2 (2.1–10.3) | 0.0 | 2 | 10.0 (0–24.4) | 81.4 | 2 |
| Hypertension | 7.1 (3.7–10.5) | 0.0 | 4 | – | – | 0 |
| Infection | 5.8 (2.6–9.0) | 0.0 | 4 | 3.3 | – | 1 |
| Dyspnea | 2.2 (0.2–4.2) | 0.0 | 4 | 14.7 | – | 1 |
| Dehydration | 5.8 (0.8–10.9) | 70.8 | 4 | – | – | 0 |
| Diarrhea | 13.0 (3.6–22.3) | 84.0 | 4 | 10.0 (3.4–16.6) | 0.0 | 2 |
| Gastrointestinal perforation | 2.0 (0–4.5) | 0.0 | 2 | – | – | 0 |
| Embolism | 2.1 (0.3–4.0) | 9.5 | 5 | – | – | 0 |
| Fatigue | 13.4 (8.5–18.4) | 0.0 | 3 | 15.4 (0.7–30.1) | 83.1 | 3 |
| Nausea/vomiting | 10.4 (5.3–15.5) | 17.3 | 3 | 8.5 (2.4–14.6) | 0.0 | 2 |
| Hemorrhage | 4.5 (0–9.9) | 68.4 | 3 | – | – | 0 |
| Electrocyte | 11.2 (6.1–16.4) | 34.9 | 4 | – | – | 0 |
CI, confidence interval; I2, heterogeneity index.
Evidence quality
Considering the serious risk of bias, inconsistency and imprecision, the quality of evidence for PFS in the RCTs was very low. The quality of evidence for OS in the RCTs was low, with serious risk of bias and imprecision. Since the risk of bias, inconsistency, indirectness and imprecision are all serious, the quality of evidence for PFS rates, OS rates, ORR and side-effects was very low (Table IV).
Table IV.
Quality of evidence for bevacizuamb in small cell lung cancer, according to the GRADE guidelines.
| Quality assessment | |||||||
|---|---|---|---|---|---|---|---|
| Outcome | Study design | Risk of bias | Inconsistency | Indirectness | Imprecision | Other considerations | Quality of evidencea |
| PFS | RCTs | Serious (−1)b | Serious (−1) | Not serious | Serious (−1) | None | Very low |
| OS | RCTs | Serious (−1) | Not serious | Not serious | Serious (−1) | None | Low |
| PFS, OS, ORR rates and side-effects | RCTs and single arm trials | Serious (−1) | Serious (−1) | Serious (−1) | Serious (−1) | None | Very low |
Quality of evidence ranks four grades, which are high, moderate, low and very low.
The risk of bias is serious, so the grade of evidence quality should be reduced 1 level from the high grade, which was marked as ‘-1’. PFS, progression-free survival; RCTs, randomized clinical trials; OS, overall survival; ORR, overall response rate.
Discussion
The standard treatment strategy for SCLC has not changed in decades, with disappointing therapeutic progress. First line chemotherapy with etoposide-platinum (EP) or irinotecan-platinum (IP) are able to achieve a median PFS time of 4–7 months and a median OS time of 9–11 months in patients with ES-SCLC (3,19–22). Furthermore, second-line therapy with paclitaxel, docetaxel, topotecan, or amrubicin have been demonstrated to achieve a median PFS of ~3 months and OS of 6–8 months (23–26). According to the two reported RCTs, the addition of bevacizumab to the first-line therapy did not improve OS (HR, 1.21; P=0.31) or PFS (HR, 0.70; P=0.19) durations. The pooled survival data from the five first-line trials revealed a median PFS time of 6–7 months for bevacizumab and chemotherapy combined treatment and a median OS time of ~11 months, which are similar with values reported in other previous trials with chemotherapy alone (3,19–22). Compared with previous reports on the use of second-line chemotherapy (median PFS, ~3 months; OS, 6–8 months) (23–26), treatment with a combination of bevacizumab and chemotherapy failed to prolong PFS or OS in previously treated patients with ES-SCLC.
Bevacizumab is a recombinant humanized monoclonal antibody, which inhibits VEGF-A binding to VEGF receptors (VEGFRs), primarily VEGFR-2 (27). There are other VEGFs, including VEGF-B that primarily binds to VEGFR-1 and VEGF-C/D, which binds to VEGFR-3 (28). The inhibition of VEGF-A causes an up regulation of the other VEGFs (29). However, other VEGF antibodies or VEGFR inhibitors failed to improve efficacy for ES-SCLC. Studies performed by the Francophone Intergroup on Thoracic Cancer and the National Cancer Institute of Canada reported no benefit of maintenance thalidomide or vandetanib in ES-SCLC (30,31). A phase II study at the Southwest Oncology Group demonstrated an improvement of 3 months in PFS, but no improvement in OS following treatment with aflibercept, a soluble VEGF receptor (32). In fact, there are different types of angiogenic factors, including VEGF, platelet-derived growth factor, fibroblast growth factor (aFGF and bFGF), transforming growth factor-β, pleiotrophin, angiogenin and angiotropin (33). An important challenge is that SCLC often occurs with multiple coexisting genomic abnormalities, the majority of which promote the expression of angiogenesis factors, including: Widespread inactivation of Tumor protein 53 and RB transcriptional corepressor 1; MYC proto-oncogene bHLH transcription factor, FGFR1, SRY-box 2, and epidermal growth factor receptor amplification; phosphatase and tensin homolog mutation, rearranged L-myc fusion-MYC1 fusion; and alterations in histone modification genes, including KRAS proto-oncogene GTPase, B-Raf proto-oncogene serine/threonine kinase, MET proto-oncogene receptor tyrosine kinase, FGFR2 and Janus kinase 3 and phosphatidylinositol-4 5-bisphosphate 3-kinase catalytic subunit α (34–37).
As a result, the efficacy of VEGF/VEGFR inhibitors is limited. Previous studies have demonstrated that elevated circulating VEGF levels predict poor overall survival in patients with SCLC (38,39). Notably, circulating VEGF levels (13,15) or polymorphisms (17) have not been identified to be associated with bevacizumab efficacy. This may be partially due to the multi-genomic abnormalities that co-exist with SCLC. Therefore, next generation sequencing may improve the understanding on SCLC, and may aid in directing the choice of therapeutic agents for the treatment of SCLC.
Shojaei et al (40) reported that granulocyte-colony stimulating factor (G-CSF), which is overexpressed in SCLC, stimulates Cd11b+Gr1+ myeloid cells, and may subsequently cause resistance to bevacizumab. In addition, anti-G-CSF was revealed to increase the efficacy of anti-VEGF in a mouse model (41). In the identified studies of the present meta-analysis, as well as in clinical practice, grade 3–4 neutropenia and leukopenia have been reported as common side-effects, and recombinant G-CSF is widely used to prevent and treat myelosuppression. Thus, the efficacy of bevacizumab may also be limited due to the use of recombinant G-CSF as part of the therapeutic regimen for patients with SCLC.
The heterogeneity of the identified studies was significant, resulting partially from different bevacizumab strategies and chemotherapy regimens applied. Bevacizumab with maintenance in the SALUTE study achieved beneficial PFS rates, whereas in the IFCT-0802 study, without maintenance, no significant improvements were observed. Furthermore, the dose of bevacizumab in the IFCT-0802 study was lower compared with that in the other studies discussed. In the LUN-90 and CALGB-30306 studies, which use similar chemotherapy regimens with IP as the first-line chemotherapy, addition of bevacizumab with maintenance in the LUN-90 study achieved a median PFS and OS time of 9.13 and 12.10 months, respectively, which were longer compared with the PFS and OS observed in CALGB-30306 without maintenance (7.0 and 11.6 months, respectively). The efficacy of bevacizumab maintenance remains controversial. Preclinical studies also suggested that cessation of anti-VEGF therapy may be associated with accelerated recurrence, more aggressive tumors upon recurrence and increased mortality rates. However, the efficacy of maintenance of bevacizumab remains controversial. Bevacizumab has been used as part of the maintenance therapy in NSCLC (42). However in the treatment of colorectal cancer, the efficacy of bevacizumab maintenance has not been demonstrated to be higher compared with discontinuation (43). A meta-analysis of five placebo-controlled randomized phase III trials, including on colorectal, breast, renal and pancreatic cancer, identified no significant difference in TTP or mortality between patients with or without continuation of bevacizumab (44). An ongoing multicenter phase III study on SCLC conducted by the Italian Oncology Group for Clinical Research, is investigating the effects of bevacizumab combined with EP chemotherapy as a first-line treatment and maintenance therapy; however, the results remain pending (12).
Another cause of heterogeneity may be the different chemotherapy regimens in the first-line studies discussed. It appears that patients on the irinotecan-platinum (IP) regimen and bevacizumab treatment achieve longer PFS and OS times compared with those on the etoposide-platinum (EP) regimen. In certain multicenter phase III trials, no significant difference in PFS and OS times between EP or IP regimens as a first-line therapy was observed (3,19–22). However, in a number of phase II trials, the efficacy of IP regimen (median PFS, 9.0; median OS, 12.8 months) has demonstrated to be improved compared with EP regimen (median PFS, 6.0; median OS, 9.4 months) (2,45). Therefore, it remains unclear whether the longer PFS and OS times are due to the combination of IP and bevacizumab treatment or results from a greater efficacy of IP compared with EP regimen.
The main limitation of the present meta-analysis derives from the limited studies identified, with a moderate risk of bias. However, synthesized survival rates and ORRs were provided. The pooled data indicated limited efficacy of bevacizumab treatment in SCLC, although the quality of evidence was low. Thus, more clinical trials may not be valuable. Additionally, no tool was identified to evaluate the risk of bias for single-arm trials. Thus, the bias evaluation may be subjective. In order to compare the efficacy of chemotherapy with the bevacizumab and chemotherapy combination treatment in SCLC, the survival data for patients with SCLC treated with chemotherapy should be only pooled based on literature search. However, it is suggested that this would not be valuable, since the efficacy of bevacizumab treatment in the present studies discussed was weak.
In conclusion, according to the RCTs, bevacizumab treatment did not appear to improve the PFS or OS for patients with ES-SCLC, with a low quality of evidence. Due to the weak pooled efficacy in the single-arm trials, although the quality of evidence was low, further clinical studies on the use of bevacizumab in the treatment of SCLC may not be valuable.
Acknowledgements
The present study was supported by the National Natural Science Foundation of China (grant no. NSFC 81273966/H2902).
Glossary
Abbreviations
- ES-SCLC
extensive stage small cell lung cancer
- PFS
progression free survival
- OS
overall survival
- HR
hazard ratio
- ORR
overall response rate
- RCT
randomized control trial
- CI
confidence interval
- VEGF
vascular endothelial growth factor
- VEGFR
vascular endothelial growth factor receptor
- TTP
time to progression
- FGF
fibroblast growth factor
- G-CSF
granulocyte-colony stimulating factor
References
- 1.Jemal A, Siegel R, Ward E, Hao Y, Xu J, Murray T, Thun MJ. Cancer statistics, 2008. CA Cancer J Clin. 2008;58:71–96. doi: 10.3322/CA.2007.0010. [DOI] [PubMed] [Google Scholar]
- 2.Noda K, Nishiwaki Y, Kawahara M, Negoro S, Sugiura T, Yokoyama A, Fukuoka M, Mori K, Watanabe K, Tamura T, et al. Irinotecan plus cisplatin compared with etoposide plus cisplatin for extensive small-cell lung cancer. N Engl J Med. 2002;346:85–91. doi: 10.1056/NEJMoa003034. [DOI] [PubMed] [Google Scholar]
- 3.Hanna N, Bunn PA, Jr, Langer C, Einhorn L, Guthrie T, Jr, Beck T, Ansari R, Ellis P, Byrne M, Morrison M, et al. Randomized phase III trial comparing irinotecan/cisplatin with etoposide/cisplatin in patients with previously untreated extensive-stage disease small-cell lung cancer. J Clin Oncol. 2006;24:2038–2043. doi: 10.1200/JCO.2005.04.8595. [DOI] [PubMed] [Google Scholar]
- 4.Okamoto H, Watanabe K, Kunikane H, Yokoyama A, Kudoh S, Asakawa T, Shibata T, Kunitoh H, Tamura T, Saijo N. Randomised phase III trial of carboplatin plus etoposide vs split doses of cisplatin plus etoposide in elderly or poor-risk patients with extensive disease small-cell lung cancer: JCOG 9702. Br J Cancer. 2007;97:162–169. doi: 10.1038/sj.bjc.6603810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hermes A, Bergman B, Bremnes R, Ek L, Fluge S, Sederholm C, Sundstrøm S, Thaning L, Vilsvik J, Aasebø U, Sörenson S. Irinotecan plus carboplatin versus oral etoposide plus carboplatin in extensive small-cell lung cancer: A randomized phase III trial. J Clin Oncol. 2008;26:4261–4267. doi: 10.1200/JCO.2007.15.7545. [DOI] [PubMed] [Google Scholar]
- 6.Stefanou D, Batistatou A, Arkoumani E, Ntzani E, Agnantis NJ. Expression of vascular endothelial growth factor (VEGF) and association with microvessel density in small-cell and non-small-cell lung carcinomas. Histol Histopathol. 2004;19:37–42. doi: 10.14670/HH-19.37. [DOI] [PubMed] [Google Scholar]
- 7.Lucchi M, Mussi A, Fontanini G, Faviana P, Ribechini A, Angeletti CA. Small cell lung carcinoma (SCLC): The angiogenic phenomenon. Eur J Cardiothorac Surg. 2002;21:1105–1110. doi: 10.1016/S1010-7940(02)00112-4. [DOI] [PubMed] [Google Scholar]
- 8.Spigel DR, Townley PM, Waterhouse DM, Fang L, Adiguzel I, Huang JE, Karlin DA, Faoro L, Scappaticci FA, Socinski MA. Randomized phase II study of bevacizumab in combination with chemotherapy in previously untreated extensive-stage small-cell lung cancer: Results from the SALUTE trial. J Clin Oncol. 2011;29:2215–2222. doi: 10.1200/JCO.2010.29.3423. [DOI] [PubMed] [Google Scholar]
- 9.Pujol JL, Lavole A, Quoix E, Molinier O, Souquet PJ, Barlesi F, Le Caer H, Moro-Sibilot D, Fournel P, Oster JP, et al. Randomized phase II–III study of bevacizumab in combination with chemotherapy in previously untreated extensive small-cell lung cancer: Results from the IFCT-0802 trialdagger. Ann Oncol. 2015;26:908–914. doi: 10.1093/annonc/mdv065. [DOI] [PubMed] [Google Scholar]
- 10.Guyot P, Ades AE, Ouwens MJ, Welton NJ. Enhanced secondary analysis of survival data: Reconstructing the data from published Kaplan-Meier survival curves. BMC Med Res Methodol. 2012;12:9. doi: 10.1186/1471-2288-12-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.John T. Role of immunotherapy in lung cancer: Preliminary results of new vaccines and immune checkpoint inhibitors. Asia Pac J Clin Oncol. 2015;11(Suppl 1):2–8. doi: 10.1111/ajco.12361. [DOI] [PubMed] [Google Scholar]
- 12.Tiseo M, Boni L, Ambrosio F, Camerini A, Vitale MG, Baldini E, Cinieri S, Zanelli F, Defraia E, Passalacqua R, et al. Italian multicenter phase III randomized study of cisplatin-etoposide with or without bevacizumab as first-line treatment in extensive stage small cell lung cancer: Treatment rationale and protocol design of the GOIRC-AIFA FARM6PMFJM trial. Clin Lung Cancer. 2015;16:67–70. doi: 10.1016/j.cllc.2014.09.001. [DOI] [PubMed] [Google Scholar]
- 13.Ready NE, Dudek AZ, Pang HH, Hodgson LD, Graziano SL, Green MR, Vokes EE. Cisplatin, irinotecan, and bevacizumab for untreated extensive-stage small-cell lung cancer: CALGB 30306, a phase II study. J Clin Oncol. 2011;29:4436–4441. doi: 10.1200/JCO.2011.35.6923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Spigel DR, Greco FA, Zubkus JD, Murphy PB, Saez RA, Farley C, Yardley DA, Burris HA, III, Hainsworth JD. Phase II trial of irinotecan, carboplatin, and bevacizumab in the treatment of patients with extensive-stage small-cell lung cancer. J Thorac Oncol. 2009;4:1555–1560. doi: 10.1097/JTO.0b013e3181bbc540. [DOI] [PubMed] [Google Scholar]
- 15.Horn L, Dahlberg SE, Sandler AB, Dowlati A, Moore DF, Murren JR, Schiller JH. Phase II study of cisplatin plus etoposide and bevacizumab for previously untreated, extensive-stage small-cell lung cancer: Eastern Cooperative Oncology Group Study E3501. J Clin Oncol. 2009;27:6006–6011. doi: 10.1200/JCO.2009.23.7545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mountzios G, Emmanouilidis C, Vardakis N, Kontopodis E, Hatzidaki D, Popis E, Karachaliou N, Kotsakis A, Agelidou M, Georgoulias V. Paclitaxel plus bevacizumab in patients with chemoresistant relapsed small cell lung cancer as salvage treatment: A phase II multicenter study of the Hellenic Oncology Research Group. Lung Cancer. 2012;77:146–150. doi: 10.1016/j.lungcan.2012.02.002. [DOI] [PubMed] [Google Scholar]
- 17.Jalal S, Bedano P, Einhorn L, Bhatia S, Ansari R, Bechar N, Koneru K, Govindan R, Wu J, Yu M, et al. Paclitaxel plus bevacizumab in patients with chemosensitive relapsed small cell lung cancer: A safety, feasibility, and efficacy study from the Hoosier Oncology Group. J Thorac Oncol. 2010;5:2008–2011. doi: 10.1097/JTO.0b013e3181f77b6e. [DOI] [PubMed] [Google Scholar]
- 18.Spigel DR, Waterhouse DM, Lane S, Legenne P, Bhatt K. Efficacy and safety of oral topotecan and bevacizumab combination as second-line treatment for relapsed small-cell lung cancer: An open-label multicenter single-arm phase II study. Clin Lung Cancer. 2013;14:356–363. doi: 10.1016/j.cllc.2012.12.003. [DOI] [PubMed] [Google Scholar]
- 19.Rossi A, Di Maio M, Chiodini P, Rudd RM, Okamoto H, Skarlos DV, Früh M, Qian W, Tamura T, Samantas E, et al. Carboplatin- or cisplatin-based chemotherapy in first-line treatment of small-cell lung cancer: The COCIS meta-analysis of individual patient data. J Clin Oncol. 2012;30:1692–1698. doi: 10.1200/JCO.2011.40.4905. [DOI] [PubMed] [Google Scholar]
- 20.Lara PN, Jr, Natale R, Crowley J, Lenz HJ, Redman MW, Carleton JE, Jett J, Langer CJ, Kuebler JP, Dakhil SR, et al. Phase III trial of irinotecan/cisplatin compared with etoposide/cisplatin in extensive-stage small-cell lung cancer: Clinical and pharmacogenomic results from SWOG S0124. J Clin Oncol. 2009;27:2530–2535. doi: 10.1200/JCO.2008.20.1061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zatloukal P, Cardenal F, Szczesna A, Gorbunova V, Moiseyenko V, Zhang X, Cisar L, Soria JC, Domine M, Thomas M. A multicenter international randomized phase III study comparing cisplatin in combination with irinotecan or etoposide in previously untreated small-cell lung cancer patients with extensive disease. Ann Oncol. 2010;21:1810–1816. doi: 10.1093/annonc/mdq036. [DOI] [PubMed] [Google Scholar]
- 22.Schmittel A, Sebastian M, von Weikersthal L Fischer, Martus P, Gauler TC, Kaufmann C, Hortig P, Fischer JR, Link H, Binder D, et al. A German multicenter, randomized phase III trial comparing irinotecan-carboplatin with etoposide-carboplatin as first-line therapy for extensive-disease small-cell lung cancer. Ann Oncol. 2011;22:1798–1804. doi: 10.1093/annonc/mdq652. [DOI] [PubMed] [Google Scholar]
- 23.von Pawel J, Schiller JH, Shepherd FA, Fields SZ, Kleisbauer JP, Chrysson NG, Stewart DJ, Clark PI, Palmer MC, Depierre A, et al. Topotecan versus cyclophosphamide, doxorubicin, and vincristine for the treatment of recurrent small-cell lung cancer. J Clin Oncol. 1999;17:658–667. doi: 10.1200/JCO.1999.17.2.658. [DOI] [PubMed] [Google Scholar]
- 24.von Pawel J, Jotte R, Spigel DR, O'Brien ME, Socinski MA, Mezger J, Steins M, Bosquée L, Bubis J, Nackaerts K, et al. Randomized phase III trial of amrubicin versus topotecan as second-line treatment for patients with small-cell lung cancer. J Clin Oncol. 2014;32:4012–4019. doi: 10.1200/JCO.2013.54.5392. [DOI] [PubMed] [Google Scholar]
- 25.O'Brien ME, Ciuleanu TE, Tsekov H, Shparyk Y, Cuceviá B, Juhasz G, Thatcher N, Ross GA, Dane GC, Crofts T. Phase III trial comparing supportive care alone with supportive care with oral topotecan in patients with relapsed small-cell lung cancer. J Clin Oncol. 2006;24:5441–5447. doi: 10.1200/JCO.2006.06.5821. [DOI] [PubMed] [Google Scholar]
- 26.Eckardt JR, von Pawel J, Pujol JL, Papai Z, Quoix E, Ardizzoni A, Poulin R, Preston AJ, Dane G, Ross G. Phase III study of oral compared with intravenous topotecan as second-line therapy in small-cell lung cancer. J Clin Oncol. 2007;25:2086–2092. doi: 10.1200/JCO.2006.08.3998. [DOI] [PubMed] [Google Scholar]
- 27.Singh M, Ferrara N. Modeling and predicting clinical efficacy for drugs targeting the tumor milieu. Nat Biotechnol. 2012;30:648–657. doi: 10.1038/nbt.2286. [DOI] [PubMed] [Google Scholar]
- 28.Kowanetz M, Ferrara N. Vascular endothelial growth factor signaling pathways: Therapeutic perspective. Clin Cancer Res. 2006;12:5018–5022. doi: 10.1158/1078-0432.CCR-06-1520. [DOI] [PubMed] [Google Scholar]
- 29.Moffat BA, Chen M, Kariaapper MS, Hamstra DA, Hall DE, Stojanovska J, Johnson TD, Blaivas M, Kumar M, Chenevert TL, et al. Inhibition of vascular endothelial growth factor (VEGF)-A causes a paradoxical increase in tumor blood flow and up-regulation of VEGF-D. Clin Cancer Res. 2006;12:1525–1532. doi: 10.1158/1078-0432.CCR-05-1408. [DOI] [PubMed] [Google Scholar]
- 30.Pujol JL, Breton JL, Gervais R, Tanguy ML, Quoix E, David P, Janicot H, Westeel V, Gameroff S, Genève J, Maraninchi D. Phase III double-blind, placebo-controlled study of thalidomide in extensive-disease small-cell lung cancer after response to chemotherapy: An intergroup study FNCLCC cleo04 IFCT 00–01. J Clin Oncol. 2007;25:3945–3951. doi: 10.1200/JCO.2007.11.8109. [DOI] [PubMed] [Google Scholar]
- 31.Arnold AM, Seymour L, Smylie M, Ding K, Ung Y, Findlay B, Lee CW, Djurfeldt M, Whitehead M, Ellis P, et al. Phase II study of vandetanib or placebo in small-cell lung cancer patients after complete or partial response to induction chemotherapy with or without radiation therapy: National Cancer Institute of Canada Clinical Trials Group Study BR.20. J Clin Oncol. 2007;25:4278–4284. doi: 10.1200/JCO.2007.12.3083. [DOI] [PubMed] [Google Scholar]
- 32.Allen JW, Moon J, Redman M, Gadgeel SM, Kelly K, Mack PC, Saba HM, Mohamed MK, Jahanzeb M, Gandara DR. Southwest Oncology Group S0802: A randomized, phase II trial of weekly topotecan with and without ziv-aflibercept in patients with platinum-treated small-cell lung cancer. J Clin Oncol. 2014;32:2463–2470. doi: 10.1200/JCO.2013.51.4109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Klagsbrun M, D'Amore PA. Regulators of angiogenesis. Annu Rev Physiol. 1991;53:217–239. doi: 10.1146/annurev.ph.53.030191.001245. [DOI] [PubMed] [Google Scholar]
- 34.Peifer M, Fernandez-Cuesta L, Sos ML, George J, Seidel D, Kasper LH, Plenker D, Leenders F, Sun R, Zander T, et al. Integrative genome analyses identify key somatic driver mutations of small-cell lung cancer. Nat Genet. 2012;44:1104–1110. doi: 10.1038/ng.2396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rudin CM, Durinck S, Stawiski EW, Poirier JT, Modrusan Z, Shames DS, Bergbower EA, Guan Y, Shin J, Guillory J, et al. Comprehensive genomic analysis identifies SOX2 as a frequently amplified gene in small-cell lung cancer. Nat Genet. 2012;44:1111–1116. doi: 10.1038/ng.2405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pietanza MC, Ladanyi M. Bringing the genomic landscape of small-cell lung cancer into focus. Nat Genet. 2012;44:1074–1075. doi: 10.1038/ng.2415. [DOI] [PubMed] [Google Scholar]
- 37.Kerbel R, Folkman J. Clinical translation of angiogenesis inhibitors. Nat Rev Cancer. 2002;2:727–739. doi: 10.1038/nrc905. [DOI] [PubMed] [Google Scholar]
- 38.Hasegawa Y, Takanashi S, Okudera K, Kumagai M, Hayashi A, Morimoto T, Okumura K. Vascular endothelial growth factor level as a prognostic determinant of small cell lung cancer in Japanese patients. Intern Med. 2005;44:26–34. doi: 10.2169/internalmedicine.44.26. [DOI] [PubMed] [Google Scholar]
- 39.Salven P, Ruotsalainen T, Mattson K, Joensuu H. High pre-treatment serum level of vascular endothelial growth factor (VEGF) is associated with poor outcome in small-cell lung cancer. Int J Cancer. 1998;79:144–146. doi: 10.1002/(SICI)1097-0215(19980417)79:2<144::AID-IJC8>3.0.CO;2-T. [DOI] [PubMed] [Google Scholar]
- 40.Shojaei F, Wu X, Malik AK, Zhong C, Baldwin ME, Schanz S, Fuh G, Gerber HP, Ferrara N. Tumor refractoriness to anti-VEGF treatment is mediated by CD11b+Gr1+ myeloid cells. Nat Biotechnol. 2007;25:911–920. doi: 10.1038/nbt1323. [DOI] [PubMed] [Google Scholar]
- 41.Phan VT, Wu X, Cheng JH, Sheng RX, Chung AS, Zhuang G, Tran C, Song Q, Kowanetz M, Sambrone A, et al. Oncogenic RAS pathway activation promotes resistance to anti-VEGF therapy through G-CSF-induced neutrophil recruitment; Proc Natl Acad Sci USA; 2013; pp. 6079–6084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Reck M, von Pawel J, Zatloukal P, Ramlau R, Gorbounova V, Hirsh V, Leighl N, Mezger J, Archer V, Moore N, Manegold C. Phase III trial of cisplatin plus gemcitabine with either placebo or bevacizumab as first-line therapy for nonsquamous non-small-cell lung cancer: AVAil. J Clin Oncol. 2009;27:1227–1234. doi: 10.1200/JCO.2007.14.5466. [DOI] [PubMed] [Google Scholar]
- 43.Koeberle D, Betticher DC, von Moos R, Dietrich D, Brauchli P, Baertschi D, Matter K, Winterhalder R, Borner M, Anchisi S, et al. Bevacizumab continuation versus no continuation after first-line chemotherapy plus bevacizumab in patients with metastatic colorectal cancer: A randomized phase III non-inferiority trial (SAKK 41/06) Ann Oncol. 2015;26:709–714. doi: 10.1093/annonc/mdv011. [DOI] [PubMed] [Google Scholar]
- 44.Miles D, Harbeck N, Escudier B, Hurwitz H, Saltz L, van Cutsem E, Cassidy J, Mueller B, Sirzén F. Disease course patterns after discontinuation of bevacizumab: Pooled analysis of randomized phase III trials. J Clin Oncol. 2011;29:83–88. doi: 10.1200/JCO.2010.30.2794. [DOI] [PubMed] [Google Scholar]
- 45.Schmittel A, von Weikersthal L Fischer, Sebastian M, Martus P, Schulze K, Hortig P, Reeb M, Thiel E, Keilholz U. A randomized phase II trial of irinotecan plus carboplatin versus etoposide plus carboplatin treatment in patients with extended disease small-cell lung cancer. Ann Oncol. 2006;17:663–667. doi: 10.1093/annonc/mdj137. [DOI] [PubMed] [Google Scholar]