Abstract
Sphingosine kinase 1 (SPHK1) is a bioactive lipid mediator that has been identified as a biomarker in various cancers and is considered to play an important role in tumor progression. In the present study, the expression level of SPHK1 was examined in breast cancer clinical specimens, and its association with patient survival was investigated to clarify the clinical significance of SPHK1 in breast cancer. SPHK1 mRNA expression was increased in breast cancer tissues compared with that in matched adjacent breast tissues in 19 of 32 paired tissue specimens (59.4%). Immunohistochemical analysis of 122 breast cancer cases revealed that the expression levels of SPHK1 were upregulated in 64 tumor tissues (52.5%), and increased expression levels of the protein were significantly associated with the presence of lymph node metastasis (P=0.0016), number of positive lymph nodes (P=0.0268) and presence of distant metastasis (P=0.0097). Increased SPHK1 protein expression was also associated with human epidermal growth factor receptor 2 status (P=0.0100), initial symptoms (P=0.0025) and tumor location (P=0.0457). Patients with increased SPHK1 protein expression had shorter overall survival and disease-free survival times compared with patients with lower SPHK1. Univariate and multivariate analyses indicated that high SPHK1 expression may be a poor prognostic factor. These results indicated that SPHK1 may perform an important role in breast cancer and may be a predictive factor in patients with breast cancer.
Keywords: sphingosine kinase 1, breast cancer, lymph node metastasis, prognosis, immunohistochemistry
Introduction
Breast cancer is the leading cause of cancer-associated mortality in women worldwide; ~1.38 million new breast cancer cases and ~0.46 million breast cancer-associated mortalities were estimated to have occurred in 2014 (1). In China, the incidence has increased more than twice as fast as global rates since the 1990s, and is now the most frequently diagnosed cancer and the sixth leading cause of cancer-associated mortality among Chinese women (2). Despite an increase in the five-year survival rate of breast cancer, as a result of early diagnosis and improved local and systemic treatment over the last 20 years, long-term prognosis remains unsatisfactory, mainly due to the recurrence and invasion rates following resection (3). However, little is known about this aggressive behavior. Finding new favorable prognostic biomarkers may help to predict the properties of the malignancy, thus decreasing the rate of unsatisfied outcomes in a high-risk population.
The oncogenic enzyme sphingosine kinase (SPHK) catalyzes the phosphorylation of sphingosine to form sphingosine-1-phosphate, which is suggested to be a bioactive lipid mediator that serves a vital role in regulating various biological processes during tumorigenesis (4). Two functional SPHK isoenzymes, SPHK1 and SPHK2, have been identified in humans (5). Multiple lines of evidence indicate that SPHK1 regulates various processes important for cancer progression (6,7); however, there are limited studies regarding biological functions of SPHK2 in cancer, and it remains unclear whether SPHK1 and SPHK2 have redundant, overlapping, complementary or antagonistic functions in human cancer cells. A previous study showed that downregulation of SPHK2 in MDA-MB-453 breast cancer cells completely eliminated migration towards epidermal growth factor (EGF), suggesting it is similar to SPHK1 (8). Other studies hypothesized that overexpression of SPHK2 suppresses growth and enhances apoptosis, preceded by cytochrome c release and activation of caspase-3 (9,10), indicating that the two isoenzymes have opposite effects. An additional study suggested that non-small cell lung cancer patients with higher SPHK2 expression had a shorter overall survival (OS) time (11). The present study was only focused on the role of SPHK1, instead of SPHK2, in breast cancer long-term survival, since there are a larger number of studies providing evidence of its role in patients with cancer prognosis, thereby supporting the hypothesis.
SPHK1 mRNA has been revealed to be frequently overexpressed in a variety of human solid tumors (12). Other studies have demonstrated that SPHK1 protein expression is unregulated in various types of cancer, including prostate cancer (13), gastric cancer (14), glioblastoma multiforme (15), intestinal adenoma (16), acute erythroleukemia (17), colon cancer (18), salivary gland carcinoma (19) and glioma (20). In addition, there is plenty of evidence indicating that activation of SPHK1 is associated with anti-apoptosis effects, and the transformation, proliferation and survival of tumor cells (21,22). Furthermore, while SPHK1 activity may be stimulated by a variety of cellular stimuli, and anticancer treatments may cause downregulation of SPHK1 activity, it has been suggested that the SPHK1 inhibitors camptothecin and docetaxel suppress tumor growth as well as reduce the occurrence and number of metastases in nude mice (23).
A previous study reported that downregulation of SPHK1 in MCF-7 cells could reduce EGF- and serum-stimulated growth and enhance sensitivity to doxorubicin (a potent chemotherapeutic agent), suggesting that SPHK1 may perform an important role in the migration of MCF-7 cells (24). Increased expression of SPHK1 has been detected in triple-negative human breast tumors compared with receptor-positive tumors, and the SPHK1 ectopic expression is associated with poor overall and progression-free survival in breast cancer patients, as well as poor response to doxorubicin-based treatment (25). These observations propose that SPHK1 may be involved in cell growth and transformation in cancer progression.
However, there are limited studies connecting a comprehensive investigation of the expression and significance of SPHK1 with the long-time prognosis in patients with breast cancer in China. In the present study, the expression of SPHK1 was assessed in mRNA and protein levels in breast cancer tissues and compared with the clinicopathological parameters and survival of patients in 122 breast cancer patients. The present results indicated that SPHK1 may be a promising potential biomarker for predicting the prognosis of patients with breast cancer and a promising new target for breast cancer therapy.
Materials and methods
Patients and specimens
The analysis of human tissues was approved by the Human Research Ethical Committee of Chongqing Medical University (CQMU; Chongqing, China). Informed consent was obtained from all patients or their relatives. A total of 32 breast tumors and paired surgical-margin tissues (>1 cm away from the tumor area) were obtained from the First Affiliated Hospital of CQMU (Chongqing, China). Tissues to be subjected to RNA extraction were frozen in liquid nitrogen. Tissue samples from 122 patients who underwent surgical resection for primary invasive breast cancer at the First Affiliated Hospital of CQMU between December 2006 and November 2013 were collected. All samples were evaluated and subject to histological diagnosis by pathologists. Subsequent to surgery, the majority of patients were treated with the standard practice guidelines at that time and were followed up regularly. In total, 15 normal breast specimens were obtained from the defect border while removing a benign breast tumor using the Mammotome biopsy technique (26). Formalin-fixed, paraffin-embedded materials were used for routine staining with hematoxylin and eosin (H&E; Zhongshan Jinqiao, Beijing, China) and for staining by immunohistochemical techniques. Grading of tumors was achieved by staining with H&E.
RNA extraction and reverse transcription-quantitative polymerase chain reaction (RT-qPCR)
Total RNA was isolated from the tissue of patients using TRIzol reagent (Molecular Research Center, Cincinnati, OH, USA). Levels of RNA expression were determined using the 7500 Fast System SDS software package (version 1.3.1; Applied Biosystems; Thermo Fisher Scientific, Inc., Waltham, MA, USA).
RT-qPCR was performed in triplicate with an Applied Biosystems Prism 7500 Fast Sequence Detection System (Thermo Fisher Scientific, Inc., USA) using Takara universal PCR master mix, according to the manufacturer's protocol (Takara Bio, Inc., Otsu, Japan). Primers were purchased from Shanghai Shenggong Genetech Co. (Shanghai, China). β-actin was used as an endogenous control. Melting curve analysis was performed to verify specificity of PCR products. In addition, PCR products were electrophoresed on 2% agarose gel to confirm product sizes and specificity. The sequences were as follows: SPHK1 forward, 5′-CTTGCAGCTCTTCCGGAGTC-3′ and reverse, 5′-GCTCAGTGAGCATCAGCGTG-3′; and β-actin forward, 5′-TCCTGTGGCATCCACGAAACT-3′ and reverse, 5′-GAAGCATTTGCGGTGGACGAT-3′. Reaction conditions were set as follows: 95°C for 30 sec; followed by 40 cycles of 95°C for 5 sec; and 60°C for 34 sec. The association stage was set to check the specificity of primers as follows: 95°C for 15 sec; followed by 60°C for 1 min; 95°C for 15 sec; and then 60°C for 15 sec. Each sample was performed in triplicate in a 20 µl reaction volume. Relative quantification of gene expression was performed using the 2−ΔΔCq calculation formula, based on Cq values for target and reference genes (27).
Immunohistochemistry
A rabbit polyclonal antibody against human SPHK1 (cat. no., ab16491; dilution, 1:300; Abgent, Inc., San Diego, CA, USA) was used. Immunohistochemistry was performed using a two-step method. Sections (4 µm) were deparaffinized by 100% xylene (4 times, 10 min each) and rehydrated in a series of ethanol (100, 95, 85 and 70% for 2 min each). The sections were hydrated and underwent sodium citrate (pH 6.0) antigen retrieval. Antigen retrieval was performed for 15 min in a microwave by intermittent heating to avoid boiling buffer, which may damage the tissue or dislodge it from the slide. Endogenous peroxidase activities were blocked by 3% hydrogen peroxide. The sections were then incubated with the primary antibody (cat. no., SP-9000; dilution, 1:250; Zhongshan Jinqiao) overnight for 18 h at 4°C, followed by incubation with horseradish peroxidase-conjugated goat anti-rabbit immunoglobulin G secondary antibody (cat. no., SP-9000; dilution, 1:1,000; Zhongshan Jinqiao) at 37°C for 1 h. Finally, slides were counterstained with hematoxylin. To eliminate nonspecific staining, a negative control was performed by replacing the primary antibody with PBS.
All staining was assessed by two pathologists blinded to the origination of the samples and subject outcome. The widely accepted German semi-quantitative scoring system was used to assess the staining intensity and area extent (28). Each specimen was assigned a score according to the intensity of the nucleic, cytoplasmic and/or membrane staining (no staining, 0; weak staining, 1; moderate staining, 2; and strong staining, 3; and the extent of stained cells (0%, 0; 1–24%, 1; 25–49%, 2; 50–74%, 3; and 75–100%, 4). The final score was calculated by multiplying the intensity score with the extent of staining score, ranging between 0 (the minimum score) and 12 (the maximum score). Scores ≥8 were defined as high expression and scores <8 were defined as low expression.
Outcome of patients
Following a median follow-up of 56.5 months (7–106 months), 41 recurrence or metastasis cases and 22 mortalities occurred in all patients.
Statistical analysis
Statistical analysis was performed using SPSS 17.0 software (SPSS, Inc., Chicago, IL, USA). The OS time was counted from the date of diagnosis being confirmed as breast carcinoma to the date of last follow-up or mortality. Disease-free survival (DFS) time was calculated from the date of confirmed diagnosis to the date of last follow-up or metastatic diseases. χ2 and Fisher's exact tests were used to compare variables. Survival analysis was performed using the log-rank test, and survival plots were created using Kaplan-Meier methods. Multivariate analysis was performed using Cox proportional hazard regression analysis. All P-values reported were two-sided, and P<0.05 was considered to indicate a statistically significant difference.
Results
Demographic and clinicopathological features
To validate the association between SPHK1, clinicopathological parameters and clinical outcome, an independent cohort of breast cancers with follow-up information was included in the present study. A total of 122 consecutive breast cancer specimens were collected, including 9 of carcinoma in situ and 113 of invasive ductal carcinoma. The mean age of the total patients enrolled was 52 years, ranging from 27–75 years. Histological types of the total 122 samples were defined according to the World Health Organization classification criteria (2007) into grade I (9 cases), grade II (76 cases), grade III (11 cases) and 26 cases with missing data.
SPHK1 mRNA expression
The mRNA level of SPHK1 in 32 tissues of patients, determined by RT-qPCR, revealed that the gene expression level of SPHK1 was significantly upregulated (P<0.0001). SPHK1 mRNA expression was upregulated [tumor/normal (T/N) ratio >1] in breast cancer tissues compared with that in matched adjacent breast tissues (expression=1) in 19 of 32 paired tissue specimens (59.4%). In 13 of 32 specimens (40.6%), SPHK1 was downregulated (T/N ratio >1; Fig. 1).
Figure 1.
SPHK1 messenger RNA expression levels in 32 paired breast cancer and adjacent normal tissues of patients. T/N, tumor/normal; SPHK1, sphingosine kinase 1; Q-PCR, quantitative-polymerase chain reaction.
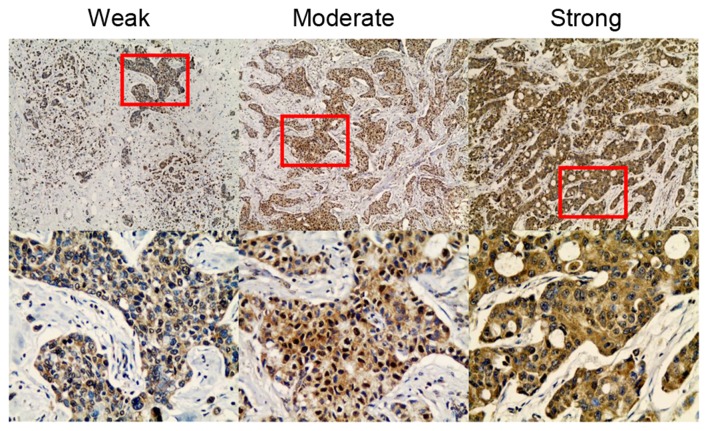
SPHK1 immunostaining
Immunohistochemical analysis was performed using 122 paraffin-embedded breast cancer tissue blocks to evaluate the expression of the SPHK1 protein. Negative staining was examined in all 15 normal breast cases (data not shown). Examples of the different SPHK1 staining of breast tumors are shown in Fig. 2, according to aforementioned methods. Positive staining for SPHK1 was mainly observed in the cytoplasm of the breast cancer cells. Among the 122 breast carcinomas, weak staining was observed in 26 specimens (21.3%), moderate expression was observed in 57 (46.7%) and strong staining was observed in 39 (32.0%).
Figure 2.
Immunohistochemical staining of SPHK1 in breast carcinomas. (left panel) Representative breast carcinomas stained weakly, moderately and strongly positive for SPHK1. Magnification, ×10 (top) and ×40 (bottom). SPHK1, sphingosine kinase 1.
Association between SPHK1 expression and clinicopathological features
The association between the expression of SPHK1 and various clinicopathological parameters is listed in Table I. A significant association was observed between the high and low expression groups in the presence of lymph node metastasis (P=0.0016), number of positive lymph nodes (P=0.0268) and presence of distant metastasis (P=0.0097). High SPHK1 expression was also associated with human epidermal growth factor receptor 2 (HER2) status (P=0.0100), initial symptoms (P=0.0025) and tumor location (P=0.0457). However, no significant association was observed between the expression level of SPHK1 and age, times of pregnancy, age at menarche, tumor histological types, histological grade, tumor size or hormonal receptor (HR; estrogen receptor or progesterone receptor) status. There was also no significant difference in SPHK1 expression among the different intrinsic subtypes of breast cancer, as defined by the St Gallen consensus conference (29). These data showed that the expression of SPHK1 increases as breast cancer clinically progresses, but cancer intrinsic subtypes do not appear to be associated with the level of SPHK1 expression in the samples included in the present study.
Table I.
Main characteristics of patients with breast cancer, and the association between the SPHK1 and clinicopathological parameters (n=122).
| SPHK1 expression | |||||
|---|---|---|---|---|---|
| Features | No. | High, n (%) | Low, n (%) | χ2 | P-value |
| Age, | 2.6011 | 0.1068 | |||
| <60 years | 93 | 45 (36.9) | 48 (39.3) | ||
| ≥60 years | 29 | 19 (15.6) | 10 (8.2) | ||
| Gravidity | 0.8801 | 0.9321 | |||
| 1 | 60 | 30 (24.6) | 30 (24.6) | ||
| 2 | 22 | 12 (9.8) | 10 (8.2) | ||
| 3 | 7 | 4 (3.3) | 3 (2.5) | ||
| 4 | 11 | 7 (5.7) | 4 (3.3) | ||
| ≥5 | 5 | 3 (2.5) | 2 (1.6) | ||
| Unknown | 17 | 7 (5.7) | 10 (8.2) | ||
| Age at menarche, years | 2.8928 | 0.4171 | |||
| ≤12 | 14 | 5 (4.1) | 11 (9.0) | ||
| 13–14 | 78 | 40 (32.8) | 38 (31.1) | ||
| 15–16 | 15 | 9 (7.4) | 6 (4.9) | ||
| ≥17 | 6 | 3 (2.5) | 3 (2.5) | ||
| Missing data | 7 | 7 (5.7) | 0 (0) | ||
| Initial symptoms | 14.3048 | 0.0025a | |||
| Lump | 92 | 39 (32.0) | 53 (43.5) | ||
| Pain | 13 | 12 (9.8) | 1 (0.8) | ||
| Nipple changes | 5 | 2 (1.6) | 3 (2.5) | ||
| Clinical screening | 6 | 5 (4.1) | 1 (0.8) | ||
| Unknown | 6 | 6 (4.9) | 0 (0) | ||
| Tumor location | 5.3123 | 0.0457a | |||
| Right | 61 | 26 (21.3) | 35 (28.7) | ||
| Left | 60 | 37 (30.3) | 23 (18.9) | ||
| Both-sides | 1 | 1 (0.8) | 0 (0) | ||
| Tumor histology | 0.7865 | 0.3752 | |||
| Carcinomas in situ | 9 | 6 (4.9) | 3 (2.5) | ||
| Invasive carcinomas | 113 | 58 (47.5) | 55 (45.1) | ||
| Types of invasive carcinomas | 5.5517 | 0.0843 | |||
| Ductal | 97 | 53 (46.9) | 44 (38.9) | ||
| Lobular | 4 | 2 (1.8) | 2 (1.8) | ||
| Mucinous adenocarcinoma | 5 | 0 (0) | 5 (4.4) | ||
| Cephaloma | 2 | 1 (0.9) | 1 (0.9) | ||
| Others | 5 | 2 (1.8) | 3 (2.6) | ||
| Histological grade | 2.9182 | 0.2531 | |||
| I | 10 | 8 (6.6) | 2 (1.6) | ||
| II | 70 | 38 (31.1) | 32 (26.3) | ||
| III | 11 | 5 (4.1) | 6 (4.9) | ||
| Unknown | 31 | 10 (8.2) | 21 (17.2) | ||
| Tumor size, cm | 0.4706 | 0.8883 | |||
| <2.0 | 36 | 15 (12.2) | 11 (9.0) | ||
| ≥2.0 and ≤5.0 | 78 | 39 (32.0) | 39 (32.0) | ||
| >5.0 | 6 | 3 (2.5) | 3 (2.5) | ||
| Unknown | 12 | 6 (4.9) | 6 (4.9) | ||
| Lymph nodes status | 10.3477 | 0.0013a | |||
| Positive | 62 | 41 (33.6) | 21 (17.2) | ||
| Negative | 55 | 20 (16.4) | 35 (28.7) | ||
| Unknown | 5 | 3 (2.5) | 2 (1.6) | ||
| No. of positive lymph nodes | 7.2395 | 0.0268a | |||
| <5 | 92 | 42 (34.4) | 50 (41.0) | ||
| 5–10 | 16 | 11 (9.0) | 5 (4.1) | ||
| >10 | 14 | 11 (9.0) | 3 (2.5) | ||
| Distant metastasis | 8.8374 | 0.0030a | |||
| Positive | 32 | 24 (19.7) | 8 (6.5) | ||
| Negative | 90 | 40 (32.8) | 50 (41.0) | ||
| ER status | 0.0104 | 0.9186 | |||
| Positive | 57 | 29 (23.8) | 26 (21.3) | ||
| Negative | 52 | 29 (23.8) | 25 (20.5) | ||
| Unknown | 13 | 6 (4.9) | 7 (5.7) | ||
| PR status | 1.2539 | 0.2628 | |||
| Positive | 38 | 23 (18.9) | 15 (12.3) | ||
| Negative | 71 | 35 (28.7) | 36 (29.5) | ||
| Unknown | 13 | 6 (4.9) | 7 (5.7) | ||
| HER2 status | 6.6422 | 0.0100a | |||
| Positive | 44 | 30 (24.6) | 14 (11.5) | ||
| Negative | 65 | 28 (23.0) | 37 (30.3) | ||
| Unknown | 13 | 6 (4.9) | 7 (5.7) | ||
| P53 status | 0.0778 | 0.7803 | |||
| Positive | 37 | 19 (15.6) | 18 (14.8) | ||
| Negative | 72 | 39 (32.0) | 33 (27.0) | ||
| Unknown | 13 | 6 (4.9) | 7 (5.7) | ||
| Intrinsic subtype | 1.5973 | 0.6600 | |||
| Luminal A | 54 | 28 (23.0) | 26 (21.3) | ||
| Luminal B | 7 | 4 (3.3) | 3 (2.5) | ||
| HER2 type | 5 | 4 (3.3) | 1 (0.8) | ||
| Basal-like | 43 | 22 (18.0) | 21 (17.2) | ||
| Undefined | 13 | 6 (4.9) | 7 (5.7) | ||
P-values were calculated using the χ2 test or Fisher's exact test. The significance of bold values is P<0.05. HER2, human epidermal growth factor receptor 2; ER, estrogen receptor; PR, progesterone receptor; SPHK1, sphingosine kinase 1.
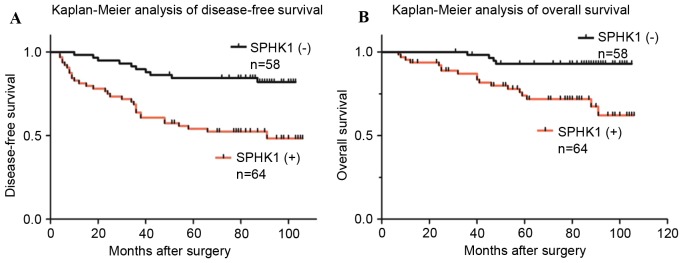
SPHK1 expression and survival of patients
Survival curves plotted using the Kaplan-Meier method demonstrated that increased expression of SPHK1 was associated with a decrease in OS and DFS (Fig. 3). Statistical analysis of the impact of classic clinicopathological features and protein expression by the log-rank (Mantel-Cox) test revealed that patients with SPHK1-positive tumors had a significantly poorer prognosis than those with SPHK1-negative tumors (P<0.05). Other features associated with decreased survival were lymph node status, distant metastasis, HER2 status and intrinsic subtype, whereas other clinicopathological variables were not significant (Table II). By multivariate analysis, high SPHK1 expression was independently associated with greater cancer-specific OS (HR, 0.196; 95% CI, 0.058–0.655; P=0.0081; Table III).
Figure 3.
Kaplan-Meier survival curves for patients of (A) disease-free survival and (B) overall survival, according to the levels of SPHK1 expression. SPHK1, sphingosine kinase 1.
Table II.
Survival of patients associated with clinicopathological features and biomarkers.
| Variables | Patients | Events | DFS rate, % | Median ± SE | P (log-rank) | Events | OS rate, % | Median ± SE | P (log-rank) |
|---|---|---|---|---|---|---|---|---|---|
| Age | 0.0938 | 0.0888 | |||||||
| <60 years | 93 | 13 | 14.0 | 84±2.6695592 | 8 | 8.6 | 84±3.1875801 | ||
| >60 years | 29 | 28 | 96.6 | 70±5.4070979 | 14 | 48.3 | 70±6.3744223 | ||
| Tumor size | 0.2281 | 0.3939 | |||||||
| <2.0 | 36 | 3 | 8.3 | 87±5.6198349 | 5 | 13.9 | 87±4.5836602 | ||
| ≥2.0 and ≤5.0 | 78 | 16 | 20.5 | 82±3.6060642 | 26 | 33.3 | 82±3.0635466 | ||
| >5.0 | 6 | 2 | 33.3 | 73±16.0603030 | 3 | 50 | 75±12.8443676 | ||
| Unknown | 12 | 1 | 8.3 | NA | 7 | 58.3 | NA | ||
| Lymph node status | <0.0001a | 0.0062a | |||||||
| Positive | 62 | 7 | 11.3 | 87±2.0293832 | 5 | 8.1 | 87±2.6739158 | ||
| Negative | 55 | 31 | 56.4 | 63±3.8471953 | 14 | 25.5 | 53±4.4754747 | ||
| Unknown | 5 | 3 | 60 | NA | 3 | 60 | NA | ||
| Distant metastasis | <0.0001a | <0.0001a | |||||||
| Positive | 32 | 32 | 100 | 87±2.4340914 | 22 | 68.8 | 88±2.0415520 | ||
| Negative | 90 | 9 | 0.03 | 27±3.5732850 | 0 | 0 | 40.5±3.7709387 | ||
| ER status | 0.0822 | 0.2415 | |||||||
| Positive | 57 | 16 | 28.1 | 87±3.6671959 | 8 | 14.0 | 86±4.1966608 | ||
| Negative | 52 | 22 | 42.3 | 75±3.6619246 | 12 | 23.1 | 73±4.5150288 | ||
| Unknown | 13 | 3 | 23.1 | NA | 2 | 14.4 | NA | ||
| PR status | 0.2300 | 0.6557 | |||||||
| Positive | 40 | 11 | 27.5 | 82±4.7006779 | 7 | 17.5 | 80±5.2390218 | ||
| Negative | 69 | 27 | 39.1 | 79±3.1488219 | 13 | 18.8 | 79±3.9022241 | ||
| Unknown | 13 | 3 | 23.1 | NA | 2 | 15.4 | NA | ||
| HER2 status | 0.0097a | 0.7220 | |||||||
| Positive | 48 | 5 | 10.4 | 60±4.8890965 | 5 | 10.4 | 53±5.6055087 | ||
| Negative | 61 | 32 | 52.5 | 82±2.7297154 | 14 | 23.0 | 80±3.4181057 | ||
| Unknown | 13 | 4 | 30.8 | NA | 3 | 23.1 | NA | ||
| P53 status | 0.1206 | 0.3823 | |||||||
| Positive | 37 | 16 | 43.2 | 82±5.5693640 | 7 | 18.9 | 82±6.3899854 | ||
| Negative | 72 | 22 | 30.6 | 79±2.7109243 | 12 | 16.7 | 79±3.3807911 | ||
| Unknown | 13 | 3 | 23.1 | NA | 2 | 15.4 | NA | ||
| SPHK1 | 0.0001a | 0.0007a | |||||||
| Positive | 64 | 31 | 48.4 | 70±3.6525019 | 18 | 28.1 | 62±4.2430458 | ||
| Negative | 58 | 10 | 17.2 | 88±2.4733977 | 4 | 6.9 | 88±3.1148016 | ||
| Intrinsic subtype | 0.0415a | 0.0005a | |||||||
| Luminal A | 53 | 16 | 30.2 | 86±3.7240436 | 9 | 17.0 | 85.5±4.2700536 | ||
| Luminal B | 8 | 1 | 12.5 | 80±11.8289970 | 0 | 0 | 80±13.0198697 | ||
| HER2 type | 6 | 4 | 66.7 | 59±13.6623570 | 4 | 66.7 | 30±13.9835618 | ||
| Basal-like | 42 | 17 | 40.5 | 75±3.9125198 | 8 | 19.0 | 75±5.0232251 | ||
| Undefined | 13 | 3 | 23.1 | NA | 1 | 7.8 | NA |
Statistically significant. ER, estrogen receptor; PR, progesterone receptor; HER2, human epidermal growth factor receptor 2; SPHK1, sphingosine kinase 1; OS, overall survival; DFS, disease-free survival; NA, not applicable; SE, standard error.
Table III.
Multivariate logistic regression analysis of different prognostic variables in patients with breast cancer by Cox regression analysis.
| Multivariate analysis | ||||||
|---|---|---|---|---|---|---|
| DFS | OS | |||||
| Characteristics | P-value | RR | Hazard ratio, 95% CI | P-value | RR | Hazard ratio, 95% CI |
| Age (<60 vs. ≥ 60 years) | 0.4648 | 1.343 | 0.609–2.958 | 0.4762 | 1.471 | 0.509–4.257 |
| Lymph node metastasis (yes vs. no) | 0.0003a | 6.067 | 2.28–16.082 | 0.0299a | 3.530 | 1.131–11.020 |
| SPHK1 expression (positive vs. negative) | 0.0518 | 0.453 | 0.204–1.006 | 0.0081a | 0.196 | 0.058–0.655 |
| ER (negative vs. positive) | 0.0671 | 3.339 | 0.919–12.131 | 0.0411a | 5.107 | 1.068–24.422 |
| PR (negative vs. positive) | 0.5753 | 1.335 | 0.486–3.666 | 0.3761 | 1.840 | 0.477–7.095 |
| HER2 score (negative vs. positive) | 0.3707 | 0.707 | 0.331–1.510 | 0.2559 | 1.893 | 0.630–5.692 |
Statistically significant. OS, overall survival; DFS, disease-free survival; RR, relative risk; CI, confidence interval; NA, not applicable; ER, estrogen receptor; PR, progesterone receptor; HER2, human epidermal growth factor receptor 2; SPHK1, sphingosine kinase 1.
Discussion
Breast cancer is one of the most common malignancies worldwide; thus, it has been the object of intensive research, which is now revealing the complexity of this disease. It was initially reviewed that breast cancer dissemination is a non-random, organotropic process, originally based on Paget's theory of seed and soil, which suggests that disseminated cancer cells (seeds) can form metastases as they reach a microenvironment (soil), which is congenial enough for their survival and proliferation (30,31). Nevertheless, how seeds fit in the exclusive soil has not been fully understood yet. The molecular subtypes of breast cancer have been proved to provide marginal metastasis site-specific prognostic information (32), but site-specific biomarkers with improved accuracy are required.
By contrast, the molecular mechanisms of tumor cell migration and metastasis to lymph nodes in vivo remain unclear, although several internal molecules in tumor cells have been reported to perform critical roles in the process of cell motility (33). Alteration in cell-cell adhesion and the secretion and activation of proteolytic enzymes is considered to be essential for optimal tumor cell invasion and migration through and across the extracellular barriers. In these aspects, several internal molecules have been reported to be associated with lymph node metastasis of breast carcinoma, including membrane-type 1 matrix metalloproteinase (34), microRNA-21 (35) and vascular endothelial growth factor C (36). SPHK1 was previously identified to be involved in cervical cancer development and progression and its expression was associated with well-known prognostic parameters, including lymph node metastasis, lymphovascular invasion, tumor size, Federation of Gynecology and Obstetrics stage and invasion depth (37).
Multiple studies have revealed that SPHK1 is a key enzyme critical to the sphingolipid metabolic pathway, which serves a vital role in cancer progression. Studies have shown that ectopic expression of SPHK1 in NIH3T3 fibroblasts may promote the growth of cells in soft agar and the ability to form tumors in non-obese diabetic/severe combined immunodeficiency mice (6), and it may be due to its association with Ras and extracellular-signal regulated kinase 1/2 signaling (38). The expression of SPHK1 was revealed to be upregulated in breast cancer by using a microarray data of 1,269 tumor samples, and the expression status was positively associated with the survival of patients, indicating a potential prognostic value of this enzyme (39). It was suggested that SPHK1 is involved in EGF-mediated activation and migration of breast cancer MDA-MB-453 cells (40). Consistently, SPHK1 was revealed to be induced by transforming growth factor-β (TGF-β) in fibroblasts and mesangioblasts, demonstrating that SPHK1 protein is an important component of the TGF-β signaling pathway (41,42). A previous study identified that the regulation of SPHK1 gene expression and kinase activity was mediated by TGF-β, which is critical to MDA-MB-231 cell viability (43).
These results support the evidence that SPHK1 has oncogenic potential in breast cancer progression. The prognostic role of SPHK1 has been studied in several cancer types, including gastric cancer (14) and astrocytoma (44), suggesting that patients with increased SPHK1 expression had shorter OS time, whereas those with lower SPHK1 survived longer. These studies indicate that SPHK1 is a prognostic indicator for a number of diseases. However, the roles of SPHK1 have not been extensively studied, particularly in the long-term survival of patients with breast cancer. In the present study, SPHK1 expression was associated with lymph node metastasis and the number of metastatic lymph nodes, indicating a role for SPHK1 in enhancing the progression of tumor cell migration and metastasis. Significant differences were also observed in other clinicopathological features and long-term prognosis among SPHK1-positive and SPHK1-negative samples. Previous studies along with the present study supported a hypothesis that SPHK1 is involved in functions other than its intracellular regulating function; it may also perform a vital role in breast cancer progression.
However, the present study has certain limitations, including a lack of intensive study into biological mechanisms involved in the association of SPHK1 expression and tumor metastasis. Additional investigations into the mechanisms of SPHK1 in breast cancer metastasis will be performed in future studies, using a larger sample size with longer follow-up time periods.
In conclusion, SPHK1 may be a potential novel drug-interfering target for cancer, and additional understanding of the function and molecular mechanisms of SPHK1 in regulating the progression of breast cancer may provide new insights into breast cancer therapy.
Acknowledgments
The authors would like to thank Ms. Ke Yang and Qian Liu from the Clinical and Pathological Diagnosis Center of Chongqing Medical University for technical support and assistance. The present study was supported by the National Natural Science Foundation of China to Dr Ke Zheng (grant no. 81202090).
References
- 1.Siegel R, Ma J, Zou Z, Jemal A. Cancer statistics, 2014. CA Cancer J Clin. 2014;64:9–29. doi: 10.3322/caac.21208. [DOI] [PubMed] [Google Scholar]
- 2.Fan L, Strasser-Weippl K, Li JJ, St Louis J, Finkelstein DM, Yu KD, Chen WQ, Shao ZM, Goss PE. Breast cancer in China. Lancet Oncol. 2014;15:e279–e289. doi: 10.1016/S1470-2045(13)70567-9. [DOI] [PubMed] [Google Scholar]
- 3.Weigelt B, Peterse JL, van't Veer LJ. Breast cancer metastasis: Markers and models. Nat Rev Cancer. 2005;5:591–602. doi: 10.1038/nrc1670. [DOI] [PubMed] [Google Scholar]
- 4.Espaillat MP, Shamseddine AA, Adada MM, Hannun YA, Obeid LM. Ceramide and sphingosine-1-phosphate in cancer, two faces of the sphinx. Transl Cancer Res. 2015;4:484–499. [Google Scholar]
- 5.Wymann MP, Schneiter R. Lipid signalling in disease. Nat Rev Mol Cell Biol. 2008;9:162–176. doi: 10.1038/nrm2335. [DOI] [PubMed] [Google Scholar]
- 6.Xia P, Gamble JR, Wang L, Pitson SM, Moretti PA, Wattenberg BW, D'Andrea RJ, Vadas MA. An oncogenic role of sphingosine kinase. Curr Biol. 2000;10:1527–1530. doi: 10.1016/S0960-9822(00)00834-4. [DOI] [PubMed] [Google Scholar]
- 7.Limaye V, Li X, Hahn C, Xia P, Berndt MC, Vadas MA, Gamble JR. Sphingosine kinase-1 enhances endothelial cell survival through a PECAM-1-dependent activation of PI-3K/Akt and regulation of Bcl-2 family members. Blood. 2005;105:3169–3177. doi: 10.1182/blood-2004-02-0452. [DOI] [PubMed] [Google Scholar]
- 8.Maceyka M, Sankala H, Hait NC, Le Stunff H, Liu H, Toman R, Collier C, Zhang M, Satin LS, Merrill AH, Jr, et al. SphK1 and SphK2, sphingosine kinase isoenzymes with opposing functions in sphingolipid metabolism. J Biol Chem. 2005;280:37118–37129. doi: 10.1074/jbc.M502207200. [DOI] [PubMed] [Google Scholar]
- 9.Igarashi N, Okada T, Hayashi S, Fujita T, Jahangeer S, Nakamura S. Sphingosine kinase 2 is a nuclear protein and inhibits DNA synthesis. J Biol Chem. 2003;278:46832–46839. doi: 10.1074/jbc.M306577200. [DOI] [PubMed] [Google Scholar]
- 10.Liu H, Toman RE, Goparaju SK, Maceyka M, Nava VE, Sankala H, Payne SG, Bektas M, Ishii I, Chun J, et al. Sphingosine kinase type 2 is a putative BH3-only protein that induces apoptosis. J Biol Chem. 2003;278:40330–40336. doi: 10.1074/jbc.M304455200. [DOI] [PubMed] [Google Scholar]
- 11.Wang Q, Li J, Li G, Li Y, Xu C, Li M, Xu G, Fu S. Prognostic significance of sphingosine kinase 2 expression in non-small cell lung cancer. Tumor Biol. 2014;35:363–368. doi: 10.1007/s13277-013-1051-1. [DOI] [PubMed] [Google Scholar]
- 12.French KJ, Schrecengost RS, Lee BD, Zhuang Y, Smith SN, Eberly JL, Yun JK, Smith CD. Discovery and evaluation of inhibitors of human sphingosine kinase. Cancer Res. 2003;63:5962–5969. [PubMed] [Google Scholar]
- 13.Malavaud B, Pchejetski D, Mazerolles C, De Paiva GR, Calvet C, Doumerc N, Pitson S, Rischmann P, Cuvillier O. Sphingosine kinase-1 activity and expression in human prostate cancer resection specimens. Eur J Cancer. 2010;46:3417–3424. doi: 10.1016/j.ejca.2010.07.053. [DOI] [PubMed] [Google Scholar]
- 14.Li W, Yu CP, Xia JT, Zhang L, Weng GX, Zheng HQ, Kong QL, Hu LJ, Zeng MS, Zeng YX, et al. Sphingosine kinase 1 is associated with gastric cancer progression and poor survival of patients. Clin Cancer Res. 2009;15:1393–1399. doi: 10.1158/1078-0432.CCR-08-1158. [DOI] [PubMed] [Google Scholar]
- 15.van Brocklyn JR, Jackson CA, Pearl DK, Kotur MS, Snyder PJ, Prior TW. Sphingosine kinase-1 expression correlates with poor survival of patients with glioblastoma multiforme: Roles of sphingosine kinase isoforms in growth of glioblastoma cell lines. J Neuropathol Exp Neurol. 2005;64:695–705. doi: 10.1097/01.jnen.0000175329.59092.2c. [DOI] [PubMed] [Google Scholar]
- 16.Kohno M, Momoi M, Oo ML, Paik JH, Lee YM, Venkataraman K, Ai Y, Ristimaki AP, Fyrst H, Sano H, et al. Intracellular role for sphingosine kinase 1 in intestinal adenoma cell proliferation. Mol Cell Biol. 2006;26:7211–7223. doi: 10.1128/MCB.02341-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Le Scolan E, Pchejetski D, Banno Y, Denis N, Mayeux P, Vainchenker W, Levade T, Moreau-Gachelin F. Overexpression of sphingosine kinase 1 is an oncogenic event in erythroleukemic progression. Blood. 2005;106:1808–1816. doi: 10.1182/blood-2004-12-4832. [DOI] [PubMed] [Google Scholar]
- 18.Liu SQ, Su YJ, Qin MB, Mao YB, Huang JA, Tang GD. Sphingosine kinase 1 promotes tumor progression and confers malignancy phenotypes of colon cancer by regulating the focal adhesion kinase pathway and adhesion molecules. Int J Oncol. 2013;42:617–626. doi: 10.3892/ijo.2012.1733. [DOI] [PubMed] [Google Scholar]
- 19.Liu G, Zheng H, Zhang Z, Wu Z, Xiong H, Li J, Song L. Overexpression of sphingosine kinase 1 is associated with salivary gland carcinoma progression and might be a novel predictive marker for adjuvant therapy. BMC Cancer. 2010;10:495. doi: 10.1186/1471-2407-10-495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Guan H, Song L, Cai J, Huang Y, Wu J, Yuan J, Li J, Li M. Sphingosine kinase 1 regulates the Akt/FOXO3a/Bim pathway and contributes to apoptosis resistance in glioma cells. PLoS One. 2011;6:e19946. doi: 10.1371/journal.pone.0019946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Akao Y, Banno Y, Nakagawa Y, Hasegawa N, Kim TJ, Murate T, Igarashi Y, Nozawa Y. High expression of sphingosine kinase 1 and S1P receptors in chemotherapy-resistant prostate cancer PC3 cells and their camptothecin-induced up-regulation. Biochem Biophys Res Commun. 2006;342:1284–1290. doi: 10.1016/j.bbrc.2006.02.070. [DOI] [PubMed] [Google Scholar]
- 22.Kawamori T, Osta W, Johnson KR, Pettus BJ, Bielawski J, Tanaka T, Wargovich MJ, Reddy BS, Hannun YA, Obeid LM, Zhou D. Sphingosine kinase 1 is up-regulated in colon carcinogenesis. FASEB J. 2006;20:386–388. doi: 10.1096/fj.05-4331fje. [DOI] [PubMed] [Google Scholar]
- 23.Pchejetski D, Golzio M, Bonhoure E, Calvet C, Doumerc N, Garcia V, Mazerolles C, Rischmann P, Teissié J, Malavaud B, Cuvillier O. Sphingosine kinase-1 as a chemotherapy sensor in prostate adenocarcinoma cell and mouse models. Cancer Res. 2005;65:11667–11675. doi: 10.1158/0008-5472.CAN-05-2702. [DOI] [PubMed] [Google Scholar]
- 24.Sarkar S, Maceyka M, Hait NC, Paugh SW, Sankala H, Milstien S, Spiegel S. Sphingosine kinase 1 is required for migration, proliferation and survival of MCF-7 human breast cancer cells. FEBS Lett. 2005;579:5313–5317. doi: 10.1016/j.febslet.2005.08.055. [DOI] [PubMed] [Google Scholar]
- 25.Datta A, Loo SY, Huang B, Wong L, Tan SS, Tan TZ, Lee SC, Thiery JP, Lim YC, Yong WP, et al. SPHK1 regulates proliferation and survival responses in triple-negative breast cancer. Oncotarget. 2014;5:5920–5933. doi: 10.18632/oncotarget.1874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Luo HJ, Chen X, Tu G, Wang J, Wu CY, Yang GL. Therapeutic application of ultrasound-guided 8-gauge mammotome system in presumed benign breast lesions. Breast J. 2011;17:490–497. doi: 10.1111/j.1524-4741.2011.01125.x. [DOI] [PubMed] [Google Scholar]
- 27.Livak KJ, Schmittgen TD. Analysis of relative gene expression data using real-time quantitative PCR and the 2(−Delta Delta C(T)) Method. Methods. 2001;25:402–408. doi: 10.1006/meth.2001.1262. [DOI] [PubMed] [Google Scholar]
- 28.Pan X, Zhou T, Tai YH, Wang C, Zhao J, Cao Y, Chen Y, Zhang PJ, Yu M, Zhen C, et al. Elevated expression of CUEDC2 protein confers endocrine resistance in breast cancer. Nat Med. 2011;17:708–714. doi: 10.1038/nm.2369. [DOI] [PubMed] [Google Scholar]
- 29.Goldhirsch A, Wood W, Coates A, Gelber R, Thürlimann B, Senn HJ. Panel members: Strategies for subtypes-dealing with the diversity of breast cancer: Highlights of the St. Gallen International Expert Consensus on the Primary Therapy of Early Breast Cancer 2011. Ann Oncol. 2011;22:1736–1747. doi: 10.1093/annonc/mdr304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Paget S. The distribution of secondary growths in cancer of the breast. Cancer Metastasis Rev. 1889;8:98–101. [PubMed] [Google Scholar]
- 31.Fidler IJ. The pathogenesis of cancer metastasis: The ‘seed and soil’ hypothesis revisited. Nat Rev Cancer. 2003;3:453–458. doi: 10.1038/nrc1098. [DOI] [PubMed] [Google Scholar]
- 32.Rakha EA, El-Sayed ME, Green AR, Lee AH, Robertson JF, Ellis IO. Prognostic markers in triple-negative breast cancer. Cancer. 2007;109:25–32. doi: 10.1002/cncr.22381. [DOI] [PubMed] [Google Scholar]
- 33.Wang W, Goswami S, Sahai E, Wyckoff JB, Segall JE, Condeelis JS. Tumor cells caught in the act of invading: Their strategy for enhanced cell motility. Trends Cell Biol. 2005;15:138–145. doi: 10.1016/j.tcb.2005.01.003. [DOI] [PubMed] [Google Scholar]
- 34.Yao G, He P, Chen L, Hu X, Gu F, Ye C. MT1-MMP in breast cancer: Induction of VEGF-C correlates with metastasis and poor prognosis. Cancer Cell Int. 2013;13:98. doi: 10.1186/1475-2867-13-98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Yan LX, Huang XF, Shao Q, Huang MY, Deng L, Wu QL, Zeng YX, Shao JY. MicroRNA miR-21 overexpression in human breast cancer is associated with advanced clinical stage, lymph node metastasis and patient poor prognosis. RNA. 2008;14:2348–2360. doi: 10.1261/rna.1034808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Skobe M, Hawighorst T, Jackson DG, Prevo R, Janes L, Velasco P, Riccardi L, Alitalo K, Claffey K, Detmar M. Induction of tumor lymphangiogenesis by VEGF-C promotes breast cancer metastasis. Nat Med. 2001;7:192–198. doi: 10.1038/84643. [DOI] [PubMed] [Google Scholar]
- 37.Kim HS, Yoon G, Ryu JY, Cho YJ, Choi JJ, Lee YY, Kim TJ, Choi CH, Song SY, Kim BG, et al. Sphingosine kinase 1 is a reliable prognostic factor and a novel therapeutic target for uterine cervical cancer. Oncotarget. 2015;6:26746–26756. doi: 10.18632/oncotarget.4818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Shu X, Wu W, Mosteller RD, Broek D. Sphingosine kinase mediates vascular endothelial growth factor-induced activation of ras and mitogen-activated protein kinases. Mol Cell Biol. 2002;22:7758–7768. doi: 10.1128/MCB.22.22.7758-7768.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ruckhäberle E, Rody A, Engels K, Gaetje R, von Minckwitz G, Schiffmann S, Grösch S, Geisslinger G, Holtrich U, Karn T, Kaufmann M. Microarray analysis of altered sphingolipid metabolism reveals prognostic significance of sphingosine kinase 1 in breast cancer. Breast Cancer Res Treat. 2008;112:41–52. doi: 10.1007/s10549-007-9836-9. [DOI] [PubMed] [Google Scholar]
- 40.Hait NC, Sarkar S, Le Stunff H, Mikami A, Maceyka M, Milstien S, Spiegel S. Role of sphingosine kinase 2 in cell migration toward epidermal growth factor. J Biol Chem. 2005;280:29462–29469. doi: 10.1074/jbc.M502922200. [DOI] [PubMed] [Google Scholar]
- 41.Yamanaka M, Shegogue D, Pei H, Bu S, Bielawska A, Bielawski J, Pettus B, Hannun YA, Obeid L, Trojanowska M. Sphingosine kinase 1 (SPHK1) is induced by transforming growth factor-beta and mediates TIMP-1 up-regulation. J Biol Chem. 2004;279:53994–54001. doi: 10.1074/jbc.M410144200. [DOI] [PubMed] [Google Scholar]
- 42.Donati C, Cencetti F, De Palma C, Rapizzi E, Brunelli S, Cossu G, Clementi E, Bruni P. TGFbeta protects mesoangioblasts from apoptosis via sphingosine kinase-1 regulation. Cell Signal. 2009;21:228–236. doi: 10.1016/j.cellsig.2008.10.007. [DOI] [PubMed] [Google Scholar]
- 43.Stayrook KR, Mack JK, Cerabona D, Edwards DF, Bui HH, Niewolna M, Fournier PG, Mohammad KS, Waning DL, Guise TA. TGFβ-mediated induction of SphK1 as a potential determinant in human MDA-MB-231 breast cancer cell bone metastasis. Bonekey Rep. 2015;4:719. doi: 10.1038/bonekey.2015.88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Li J, Guan HY, Gong LY, Song LB, Zhang N, Wu J, Yuan J, Zheng YJ, Huang ZS, Li M. Clinical significance of sphingosine kinase-1 expression in human astrocytomas progression and overall patient survival. Clin Cancer Res. 2008;14:6996–7003. doi: 10.1158/1078-0432.CCR-08-0754. [DOI] [PubMed] [Google Scholar]