With the noninvasive, convenient, and unique value in the quick diagnosis and dynamic monitoring during the course of treatment, critical ultrasonography has been widely used in critical care medicine, regarded as the “visual stethoscope” and applied in medical education and training system.[1] Based on years of experience in the application and promotion of critical ultrasonography, the authors of this study suggested that a proper understanding of critical ultrasonography is of most importance, and a consistent quality control system is required to minimize misdiagnosis, missed diagnosis, and dependence on operators. To ensure the clinical value of critical ultrasonography, avoid misdiagnosis and missed diagnosis, and improve the quality control system, this study established ten basic principles for critical care ultrasound.
First: Critical Ultrasonography is Problem Oriented and Imperative Both in Respiratory and Circulatory Dysfunctions
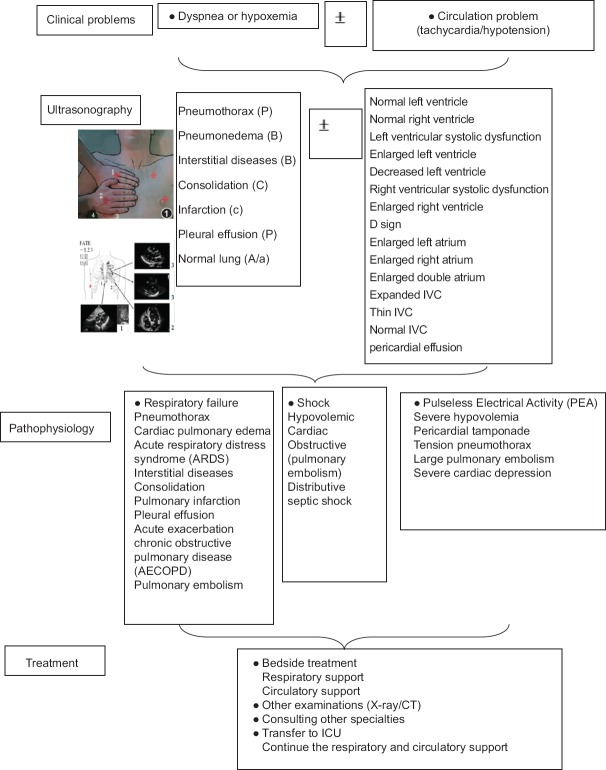
Critical ultrasonography is different from the conventional ultrasound. It is based on clinical problems, which finds the essence of problems quickly. Circulatory and respiratory dysfunctions are the most common and critical clinical situations. When the patient is in shock and hypoxia, decisions on diagnosis and treatment should be made quickly. However, due to the instability of the vital signs, imaging diagnosis such as magnetic resonance imaging and computed tomography (CT) often cannot be performed. Traditional clinical history, manifestations, and laboratory examinations often take a lot of time, which delay the diagnosis and treatment. Thus, critical care ultrasound is particularly important when the patient has respiratory and circulatory dysfunctions. For example, critical ultrasonography can distinguish several common reversible factors that lead to pseoudo-pulseless electrical activity (PEA), such as pericardial tamponade, severe hypovolemia, severe cardiac dysfunction, pulmonary embolism, aortic dissection, and pneumothorax, thus can save the life of patients. In studies, expert commentaries, and various guidelines, the first-time application of critical ultrasonography was recommended for patients in shock and dyspnea to help rapid diagnosis, narrow the etiology, and make medical decisions.[2,3,4,5,6] Thus, critical ultrasonography is imperative in respiratory and circulatory dysfunctions.
Second: Echocardiography and Lung Ultrasonography are the Cornerstones of Critical Ultrasonography; A Multigoal-integrated Examination Including Heart and Lungs is Essential for Critical Ultrasonography
Integrity and balance are two important rules of critical care. A critically ill patient is an organic integrity. Thus, respiratory and circulatory dysfunctions are often combined with multiple-organ dysfunction. Therefore, to realize heart- and lungs-centered and multigoal-integrated critical ultrasonography, attention should be paid not only to one point but to the whole body. For example, consider the case of acute respiratory distress syndrome (ARDS) that majorly affects the lungs. Due to the similarity in the mechanisms of lung ultrasound and CT, the heterogeneity of lung lesions can be fully reflected in ultrasound. However, the focus should not just be on the lung lesions during the clinical application of ultrasound. Ischemia and hypoxia due to ARDS can lead to pulmonary vasoconstriction, increase of pulmonary artery pressure, and right ventricular overload, whereas high-positive end-expiratory pressure (PEEP) in respiratory support and permissive hypercapnia might further aggravate the right heart dysfunction. With the clinical application of critical ultrasonography, the proportion of ARDS patients who had acute pulmonary artery hypertension was reportedly as high as 25%, and thus a new concept called right heart protective ventilation strategy arose. When there is refractory hypoxia that does not match with the severity of ARDS, practitioners are required to be particularly vigilant about the presence of an intracardiac shunt due to the reopening of foramen ovale.[7] Thus, due to the interaction between organs, it is essential to take a look in the critical ultrasonography to realize the heart- and lungs-centered and multigoal-integrated treatment.
Third: To Achieve the Above Target, Ten Standard Views of Critical Consultation Ultrasonic Examination are Necessary
The critical consultation ultrasonic examination or critical care chest ultrasonic examination (CCUE) is an ultrasonic protocol for emergency consultation that was first used in Peking Union Hospital since 2012 for patients who needed to be transferred to the intensive care unit (ICU) due to respiratory and circulatory dysfunctions. The CCUE protocol was found to effectively improve the bedside treatment of critically ill patients and reduce the length of time in the ICU.[8] Later, the Chinese Critical Ultrasound Study Group spread this protocol in its basic training program and found that it had very high value in clinical practice for critically ill patients with respiratory and circulatory dysfunctions. This protocol consists of ten standard views, five views each for the heart and the lungs. Each view has a different functional feature [Figure 1]. The subcostal 4-chamber view is mainly used to eliminate obvious pathological states such as pericardial tamponade and acute pulmonary artery hypertension; parasternal long-axis and short-axis views’ focus on the qualitative assessment of ventricular wall thickness, chamber diameter, left ventricular systolic function, and segmental dyskinesia; and inferior vena cava (IVC) and apical 4-chamber views are used to qualitatively evaluate the state of volume (apparent low volume and volume overload) and fluid responsiveness. The upper and lower blue points are used to find the pneumothorax (P1) and alveolar interstitial syndrome (B3/B7, B lines with the distance of 3 or 7 mm). The diaphragm and posterolateral alveolar and/or pleural syndrome points are mainly used to observe the movement of lung, pleural effusion (P2) and lung consolidation and atelectasis (C). The posterior blue point is used to observe lung consolidation and atelectasis. And, finally, the ultrasound observation should be interpreted together with clinical information. Any of these ten views is indispensable. If all these ten views could be obtained, the functional characteristics and the focus of evaluation for each view should be assessed. However, if all these ten views could not be obtained, the function of those views obtained should be understood and the goal-oriented images should be interpreted. These results should then be analyzed in combination with clinical information, thereby guiding the clinical treatment.
Figure 1.
Flow chart of the critical care chest ultrasonic examination for emergency consultation. IVC: Inferior vena cava.
Fourth: Inferior Vena Cava, Left Ventricular Output Tract Velocity-Time Integral, and Ejection Fraction are the Three Basic Quantitative Hemodynamic Measurements
Continuous and dynamic are the characteristics of critical care. It is essential to continuously evaluate the effect of treatment, adjust the treatment, and therefore get the best prognosis. Thus, in addition to qualitative assessment, simple quantitative monitoring is also required to achieve the purpose of continuous and dynamic and improve the accuracy of assessment. In quantitative measurements, three indexes are recommended, including IVC, left ventricular output tract velocity-time integral (VTI), and left ventricle ejection fraction (EF), which represent the volume status and fluid responsiveness, blood flow (cardiac output [CO]), and cardiac function, respectively, including the most important information of hemodynamics in critically ill patients.
Fifth: The Standard View of Inferior Vena Cava Measurement is the Subxiphoid View, in Which We Choose a Point at 2 cm Distal from the Right Atrium
The most reliable method of quality control is a uniform protocol of operation and standard for measurement. At the same time, continuous and dynamic monitoring also requires relative consistent measurement. It is recommended that the standard view of IVC measurement is the subxiphoid view, and the definition of this view is the smallest depth that can show the complete IVC under sword, with suitable gain, stable image, stable display of inferior caval vein linking to the right atrium, clear echo of the anterior, and rear wall of IVC, 2 cm distal from the right atrium [Figure 2].
Figure 2.
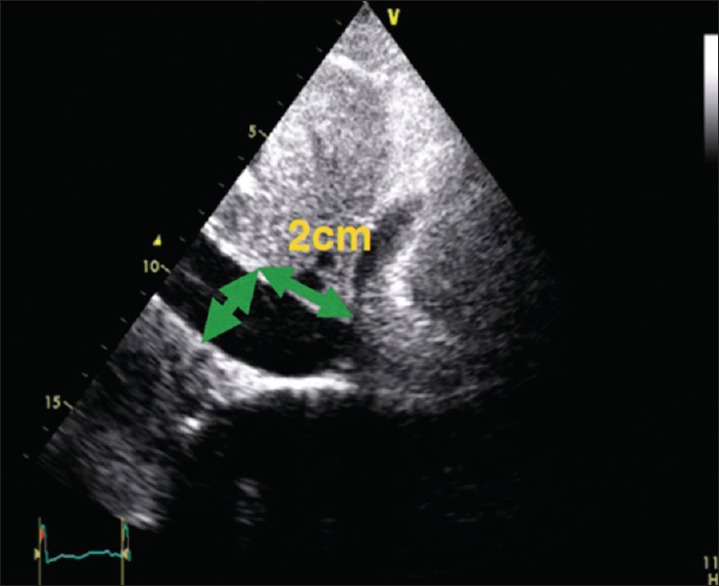
Standard view of inferior vena cava and its measurement.
Sixth: The Standard View of Velocity-time Integral Measurement is the Apical 5-chamber View, in Which We Choose a Point at 0.5 cm Under the Aortic Valve
Ultrasound measurement of CO is mainly determined by VTI and left ventricular outflow tract (LVOT) calculation. The formula for calculating CO is as follows: CO = stroke volume × heart rate = Cross-sectional area = (LVOT/2)2 × VTI × HR. VTI and LVOT are the basis of CO measurement, and LVOT has more influence on the accuracy of CO measurement. The LVOT diameter of a patient is basically constant, about 2 cm in Chinese, so VTI measurement can indirectly quantitate CO, especially its dynamic changes, and the results are relatively accurate. VTI was recommended to be measured in the apical 5-chamber view. To reduce the interference of mitral valve blood flow, the Doppler sampling volume is located 0.5 cm under the aortic valve to trace the left ventricular outflow wave [Figure 3].
Figure 3.
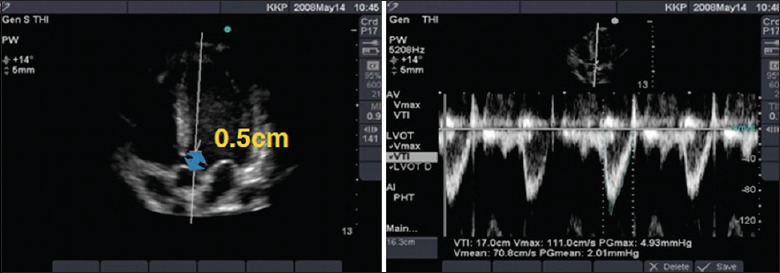
Standard view of velocity-time integral measurement and its waves.
Seventh: The Standard View of Ejection Fraction Measurement is in the Left Ventricular Parasternal Long-axis View/Papillary Muscle Short-axis View, with the Cursor Perpendicular to the Interventricular Septum
Despite the eyeballing qualitative assessment of cardiac function in CCUE and other rapid diagnostic procedures, quantitative assessment is sometimes necessary to facilitate complementary and dynamic monitoring of therapeutic effects. EF values are measured in the left ventricular long-axis view/papillary muscle short-axis view, with the cursor perpendicular to the interventricular septum [Figure 4]. The EF measurement does not reflect the overall left ventricular systolic function in patients with segmental motion disorders.
Figure 4.
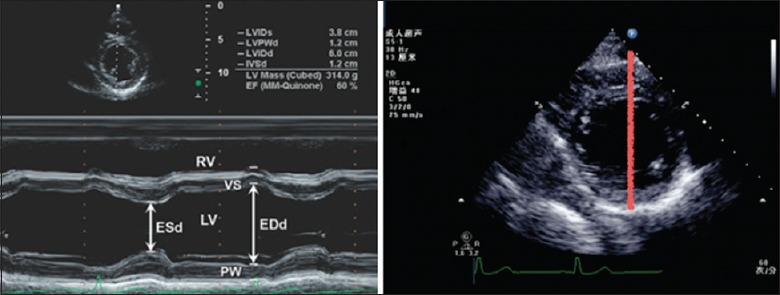
Standard view of ejection fraction measurement (left ventricular papillary muscle short-axis view).
Eighth: Either Normal Findings or Abnormal Findings Should Be Double Checked
Adherence to double check contains two meanings. The first is to use two views to confirm a result, to prevent misdiagnosis. The second is double check by two operators to reduce operator dependence. Double checking either normal findings or abnormal findings is imperative for the quality control and assurance of the accuracy of data.
Ninth: Critical Ultrasonography Needs Mutual Aid, Either in Technique, or by Critical Care Practitioner
The clinical practice of critical ultrasonography needs supplement. First, in technique, mutual help is required between the transthoracic echo (TTE) and the transesophageal echocardiogram (TEE). TTE and TEE both have their advantages in the evaluation of critically ill patients.[9] TTE is relatively noninvasive, good for measuring specific parts such as apical thrombus, pericardium, and the structure of IVC, especially the Doppler ultrasound measurement in the inter-lobe area, while the clinical value of TTE is often limited by the patient factors (such as obesity, heart surgery, high PEEP, and lung hyperinflation) and the severity of the disease (such as endocarditis, aortic dissection, and cardiac surgery evaluation). TEE is good at measuring deep structures, such as deep large blood vessels, heart valves, tendon cable, and left atrial appendage, and can better assess the superior vena cava and variability compared with TTE. However, compared with TTE, TEE has more complications, and it is difficult to implement dynamic repetitive monitoring and evaluation. Therefore, when some diseases need comprehensive assessment or the assessment of special views, TEE needs to be combined with TTE. Second, by technician, critical ultrasonography practitioners have different professional levels, especially for the understanding of its concept. Therefore, they need mutual help.
Tenth: Critical Ultrasonography Demonstrates the Underlying Pathophysiology of Critical Illness
Critical ultrasonography focuses on the understanding of critical care. The development of critical care medicine promotes the development of critical ultrasonography, while the application of critical ultrasonography promotes the clinical interpretation of the pathophysiological changes in diseases. Critical ultrasonography needs a combination of critical care physicians, clinical problems, implementation of ultrasound monitoring, and finally analysis of the disease based on detailed interpretation and dynamic monitoring of the treatment effect. For example, in the diagnosis of pericardial tamponade, acute pulmonary embolism, and pneumothorax, the combination of ultrasound and clinical manifestations should be combined to increase the diagnostic accuracy. Although there are ultrasonic temponade signs, such as pericardial effusion, end-systolic right atrial collapse, early-diastolic right ventricular collapse, the clockwise rotation of the heart, and IVC expansion, the diagnosis of pericardial tamponade depends on its hemodynamic consequences. On the contrary, when a clinical shock cannot be explained by other reasons and pericardial effusion is limited, although without typical diffused effusion and typical sonographic signs of tamponade, focal temponade might still be clinically diagnosed and treatment can be started. Therefore, critical care ultrasound is based on the clinical problems. The results of ultrasound should not be simply interpreted without combining clinical manifestations. Ultrasound without clinical information is terrible.
In conclusion, a standardized medical treatment and a perfect quality control system are the best guarantee for the safety of patients. Critical ultrasonography has become an important part of critical care medicine, and it is important for the evaluation and treatment of critically ill patients. Adhering to the aforementioned ten basic principles for critical ultrasonography will minimize misdiagnosis and missed diagnosis and maximize the consistency among different operators in clinic practice.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
All ultrasound images in this article were collected from a volunteer: Dr. Huai-wu He, Department of Critical Care Medicine, Peking Union Medical College Hospital. The authors would like to thank Dr. Huai-wu He for his contribution to the medical profession and providing permission for use of the images in this article.
Footnotes
Edited by: Yi Cui
References
- 1.Solomon SD, Saldana F. Point-of-care ultrasound in medical education – Stop listening and look. N Engl J Med. 2014;370:1083–5. doi: 10.1056/NEJMp1311944. doi: 10.1056/NEJMp1311944. [DOI] [PubMed] [Google Scholar]
- 2.Finfer SR, Vincent JL. Circulatory shock. N Engl J Med. 2013;369:1726–34. doi: 10.1056/NEJMra1208943. doi: 10.1056/NEJMra1208943. [DOI] [PubMed] [Google Scholar]
- 3.Via G, Hussain A, Wells M, Reardon R, ElBarbary M, Noble VE, et al. International evidence-based recommendations for focused cardiac ultrasound. J Am Soc Echocardiogr. 2014;27:683.e1–683.e33. doi: 10.1016/j.echo.2014.05.001. doi: 10.1016/j.echo.2014.05.001. [DOI] [PubMed] [Google Scholar]
- 4.Kanji HD, Sirounis D, Boyd JH. Once is enough: Limited echocardiography in subacute shock. J Crit Care. 2015;30:431–2. doi: 10.1016/j.jcrc.2014.12.011. doi: 10.1016/j.jcrc.2014.12.011. [DOI] [PubMed] [Google Scholar]
- 5.Lichtenstein D, van Hooland S, Elbers P, Malbrain ML. Ten good reasons to practice ultrasound in critical care. Anaesthesiol Intensive Ther. 2014;46:323–35. doi: 10.5603/AIT.2014.0056. doi: 10.5603/AIT.2014.0056. [DOI] [PubMed] [Google Scholar]
- 6.Volpicelli G, Elbarbary M, Blaivas M, Lichtenstein DA, Mathis G, Kirkpatrick AW, et al. International evidence-based recommendations for point-of-care lung ultrasound. Intensive Care Med. 2012;38:577–91. doi: 10.1007/s00134-012-2513-4. doi: 10.1097/CCM.0000000000001216. [DOI] [PubMed] [Google Scholar]
- 7.Legras A, Caille A, Begot E, Lhéritier G, Lherm T, Mathonnet A, et al. Acute respiratory distress syndrome (ARDS)-associated acute cor pulmonale and patent foramen ovale: A multicenter noninvasive hemodynamic study. Crit Care. 2015;19:174. doi: 10.1186/s13054-015-0898-5. doi: 10.1186/s13054-015-0898-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wang X, Liu D, He H, Du W, Zhang H, Liu Y, et al. Using critical care chest ultrasonic examination in emergency consultation: A pilot study. Ultrasound Med Biol. 2015;41:401–6. doi: 10.1016/j.ultrasmedbio.2014.09.010. doi: 10.1016/j.ultrasmedbio.2014.09.010. [DOI] [PubMed] [Google Scholar]
- 9.Mayo PH, Narasimhan M, Koenig S. Critical care transesophageal echocardiography. Chest. 2015;148:1323–32. doi: 10.1378/chest.15-0260. doi: 10.1378/chest. 15-0260. [DOI] [PubMed] [Google Scholar]