Pedicle screw placement is an advanced posterior fixation technique that can provide patients with great biomechanical benefits. However, the morphology of the vertebrae is complex and it is very difficult to insert screws without penetrating the cortex. Thus, new techniques for improving the accuracy of pedicle screw placement and safety are required. Herein, we propose a novel surgical robot system for percutaneous pedicle insertion based on three-dimensional (3D) fluoroscopy and present the first case of robot-assisted minimally invasive fixation of thoracic vertebrae.
A 28-year-old male fell from a height of 4 m; he experienced progressive pain of the lower back and could not stand or walk. There was no relevant prior medical history. On neurological examination, there was no paresthesia of the lower extremities, and all muscles had full motor strength (V/V). X-ray and computed tomography (CT) images demonstrated an L1 vertebral burst fracture without compression of the related vertebral canal. Magnetic resonance imaging demonstrated a high signal change in the L1 vertebra.
After approval by the ethics committee (JST-20150504) and obtaining informed consent from the patient, robot-assisted percutaneous pedicle screw fixation was performed on August 6, 2015. The patient was placed in prone position under general anesthesia, a patient tracker was placed on the T10 spinal process, and a set of images were obtained by intraoperative C-arm scan. Based on these images, the TiRobot system (co-designed by Beijing Jishuitan Hospital and TINAVI Medical Technologies Co., Ltd.) was autoregistered, and surgeons used the TiRobot planning system to plan the trajectories of six pedicle screws. The robot arm of the TiRobot system was covered with sterilized plastic and docked along the side of the operating table; the trajectories were then confirmed before movement of the robot arm was initiated. The robot arm with a guidance tube on its end was automatically moved to the entry point of each trajectory and held still. After checking the position with the optical tracking system, a 2 cm skin incision was made through the guidance tube, and the guidance wire for the screw was placed through the tube using a drill. The position of each guidance wire was verified by fluoroscopy. A total of six pedicle screws (J&J Depuy Viper) were placed into the vertebrae through guidance wires; screws 6.0 mm in diameter and 50 mm in length were used for T12 and L2, and screws 5.0 mm in diameter and 35 mm in length were used for L1. There were no intraoperative complications.
Postoperatively, the patient maintained full strength of the extremities. CT images taken 4 days postoperatively showed no perforations or loosening of the screws [Figure 1]. The merging of postoperative CT images and trajectory planning images demonstrated that the deviation between the planned and actual trajectories was 0.70 ± 0.82 mm in the sagittal plane and 1.27 ± 1.08 mm in the axial plane.
Figure 1.
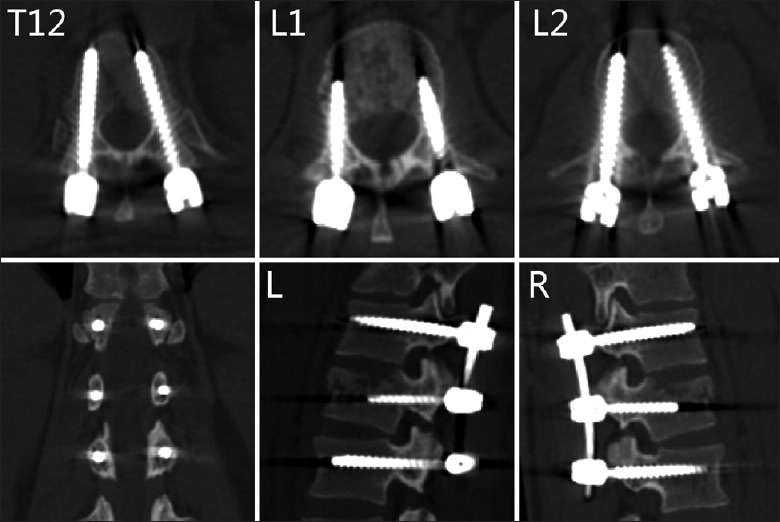
Postoperative computed tomography images demonstrated that there were no perforations or loosening of the screws.
Spine surgeons always have two types of limitations: visual and manipulative. Insufficient vision and force control can cause severe problems during spine surgery. Various methods have been introduced to improve the accuracy and safety of pedicle screw placement.[1] The TiRobot system is a novel surgical robot system for pedicle screw insertion. It can be used for surgical planning based on intraoperative 3D fluoroscopy images, and the serial-structured mechanical arm then guides the surgeon to the exact planned trajectories for the screws.[2]
The main aspect that caused deviation of screws in the present study was system error. System error is generated during the image reconstruction, image auto-registration, and optical tracking process. C-arm fluoroscopy was used to capture the image data, which can result in image distortion caused by electromagnetic fields generated from the C-arm machine itself;[3] this kind of system error remains unresolved, as fluoroscopic imaging devices are still being used. The intraoperative image auto-registration process also results in registration error, which is limited by the physical principle of reflection; the image auto-registration error in the present case was 0.11 mm. The optical tracking system also contributes to system error; the optical tracking camera used in the TiRobot system has a system error of about 0.30 mm (supported by the NDI Company).
A lot of time and money is required to train a spine surgeon, as the success of the surgical procedures relies on the surgeon's experience.[4] The TiRobot system has shown its ability to improve the accuracy and safety of pedicle screw insertion and was sufficient for clinical use. This system will be helpful in shortening the learning curve for spinal surgery.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
This study was supported by grants from the Yangfan project from Beijing Municipal Administration of Hospitals (No. ZYLX 201405), and Medical Development and Scientific Research Fund from Beijing Municipal Bureau of Health (No. ShouFa-2014-1-2071).
Conflicts of interest
There are no conflicts of interest.
Footnotes
Edited by: Li-Min Chen
References
- 1.Bertelsen A, Melo J, Sánchez E, Borro D. A review of surgical robots for spinal interventions. Int J Med Robot. 2013;9:407–22. doi: 10.1002/rcs.1469. doi: 10.1002/rcs.1469. [DOI] [PubMed] [Google Scholar]
- 2.Tian W. Robot-assisted posterior C1-2 transarticular screw fixation for atlantoaxial instability: A case report. Spine (Phila Pa 1976) 2016;41(Suppl 19):B2–5. doi: 10.1097/BRS.0000000000001674. doi: 10.1097/BRS.0000000000001674. [DOI] [PubMed] [Google Scholar]
- 3.L’Orsa R, Macnab CJ, Tavakoli M. Introduction to haptics for neurosurgeons. Neurosurgery. 2013;72(Suppl 1):139–53. doi: 10.1227/NEU.0b013e318273a1a3. doi: 10.1227/NEU.0b013e318273a1a3. [DOI] [PubMed] [Google Scholar]
- 4.Hu X, Lieberman IH. What is the learning curve for robotic-assisted pedicle screw placement in spine surgery? Clin Orthop Relat Res. 2014;472:1839–44. doi: 10.1007/s11999-013-3291-1. doi: 10.1007/s11999-013-3291-1. [DOI] [PMC free article] [PubMed] [Google Scholar]


