Abstract
Background:
Psychological distress is one of the most common psychological symptoms in elderly cancer patients. However, many of these patients do not receive any treatment for distress management. Therefore, we aimed to assess the effect of a communication program on the psychological distress of elderly cancer patients.
Materials and Methods:
This two-group clinical trial with a before and after design was conducted in Al-Zahra and Seyed-Al-Shohada hospitals affiliated to the Isfahan University of Medical Sciences in 2015. A total of 64 elderly patients were randomly assigned to two groups: experimental and control groups. A 3-week intervention (communicational program) consisting of distributing educational booklets, practices, and phone follow-ups was performed for the intervention group. All sessions were held during the 3-week period with sessions held twice per week both in the form of personal attendance and phone tracking, and the patients were encouraged to do the tasks assigned to them. The control group received routine care, and at the end of the study, the content of the sessions was explained to them. The demographic and clinical data of the participants were recorded, and all participants completed Kessler's Psychological Distress inventory at baseline and at the end of the 3-week intervention.
Results:
We found a significant difference in the psychological distress scores between the two groups before and after the intervention (P < 0.001, independent t-test). Moreover, the mean psychological distress scores decreased significantly in the experimental group after the intervention (P < 0.001, paired t-test).
Conclusions:
Our communicational program had a positive effect on psychological distress in elderly patients with cancer. Therefore, this program could be used as an easy, cheap, and practical approach for reducing psychological distress in these patients.
Keywords: Cancer, communication, elderly, Iran, nursing, psychological distress
Introduction
Cancer is a major problem for global public health and is on a rise. Age is one of the risk factors for cancer, with 50% of all cancer patients over the age of 65 years.[1] The findings of a study from Iran showed that between 2001 and 2005, 5.33% of men and 5.66% women aged 60 years or above suffered from cancer,[2] suggesting that cancer in the elderly is a significant issue which should receive more attention.
After the diagnosis of cancer, patients start showing symptoms of psychological distress.[3] According to the National Comprehensive Cancer Network (NCCN), psychological distress is a multidimensional concern and an unpleasant experience of a psychological (in emotional, cognitive, and behavioral dimensions), social, and spiritual nature that can affect a person's ability to cope with cancer, its physical symptoms, and treatments.[1,4,5,6] Undiagnosed and untreated psychological distress results in more pain, lowered quality of life, long stay in the hospital, reduced coping and compatibility with treatment,[3,7] suicide, and severe psychological burden on the families.[8] Nevertheless, distress is not usually recognized[9] or is neglected in patients with cancer.[10] NCCN introduced psychological distress as the sixth vital sign after temperature, blood pressure, pulse, respiration, and pain, and made it a part of routine investigations in nursing care. Psychological distress is specifically common among elderly patients with cancer, and thus, it should be considered as a threat to their health.[1] Studies show that 27–48% of the elderly suffer from symptoms of psychological distress.[11] In developing societies, aging is a hidden issue, and this group of people are rather neglected.[12] Most cancer patients in Iran do not get more than routine treatment such as treatment for their psychological, social, and spiritual needs;[13] however, most cancer organizations recommend screening patients for psychological distress, and a number of countries routinely perform screening in order to identify and reduce distress.[3,14,15]
Appropriate interaction with cancer patients is necessary for better understanding of patients, managing side effects of cancer treatment, and improving their Quality of life (QoL).[16,17] However, communication barriers exist in oncology environment leading to an inappropriate relationship and lower understanding of patients'QoL.[18] Studies in Iran have also reported major obstacles in the interaction between nurses and the elderly.[19] Nurses are responsible to use the dynamic and mutual process of communication to direct their attention towards identifying distress and satisfying the psychological needs of their patients.[20]
Thus far, researchers have sought to overcome the psychological distress of cancer and non-cancer patients by implementing various interventions such as hope intervention, bibliotherapy manual, mindfulness-based stress reduction, expressive writing intervention, and tele-based psychological intervention,[21,22,23,24,25] yet each method has its own limitations and recommendations for further studies. Furthermore, the existing literature shows that these studies rarely targeted elderly patients with cancer or were mostly performed on outpatients.[3,6,10] Some studies were also administered in a single centre[3,8] and recommended more extensive studies and sampling in multiple centres. In the current study, the program covers different aspects including physical, psychological, social, and spiritual-existential aspects of patients and offers patient coping strategies for problems in any of the aforementioned areas. Above all, by assigning tasks to the patients and encouraging them to do them in an attempt to help them cope with their problems and by telephonically tracking them between the session intervals, this program creates an applicable, dynamic, mutual, patient-oriented interaction. Thus, this study aimed to determine the effect of a communication program on the psychological distress of elderly patients with cancer admitted to two centres.
Materials and Methods
This is a two-group clinical trial (reg. code: IRCT2016010725897N1) two-group with a before and after design that was administered in 2015 in Al-Zahra and Seyyed-Al-Shohada hospitals affiliated to the Isfahan University of Medical Sciences. These hospitals were among the reference centers to which patients from Isfahan as well as the neighbouring provinces were referred for care and treatment.
The study sample included 64 patients (32 patients in each group) for which the confidence level of 95% and statistical power of 80% were considered; the mean difference of the psychological distress score between the two groups had a standard deviation (SD) of 7.0. The inclusion criteria for the study included selecting elderly patients aged 60 years or above with a definite diagnosis of cancer by an oncology expert recorded in the log file, and with a life expectancy of at least 6 months; patient's awareness of the disease diagnosis; having the ability to talk and conduct verbal communication; willingness to participate in the study and being randomly placed in either of the groups; non-participation in other therapies such as psychotherapy, spiritual therapy, and communication therapy in the last six months; lack of other diseases besides cancer, such as chronic or acute physical disorders such as influenza, debilitating cardiovascular, endocrine, respiratory, liver, musculoskeletal, and renal diseases approved by specialist physicians and medical records; the absence of mental or psychological illness available in the patient's record; lack of addiction to narcotic and psychoactive substances according to the patient and his medical records; the absence of distressful incident as told and confirmed by the patient in the last 6 months (for example, death of a loved one such as a spouse or a close friend, loss of everything that is valuable for the patient, divorce, refractory or loss of limb, loss of jobs, a recent displacement to a new city or province, or severe financial ruin or debt, imprisonment, argument, and persistent marital discord).
The exclusion criteria included unwillingness to participate in the study, participation in other communication programs during the study, not being able to participate in the meetings on a regular basis, missing two or more consecutive sessions of the communication meetings, and death during the study.
The researcher referred to the hospitals and started convenience sampling. The participants were among patients hospitalized in all the units and departments of Seyyed-Al-Shohada and Al-Zahra hospitals who met the inclusion criteria and were randomly placed in either of the test or control groups. First, the researcher introduced herself to the given units and explained the objectives of the study; the demographic information questionnaire was completed by the researcher through questioning the participants, and the files were completed. Moreover, Kessler Psychological Distress questionnaire was explained to the two groups and was completed by the researcher through questioning the participants before the intervention was performed.
In the experimental group, the intervention included six 20-minute communication sessions according to the condition and needs of the patients. All sessions were held during a 3-week period, with sessions being held twice per week both by personal attendance and phone tracking. The patients were encouraged to performed the tasks assigned to them, and to confirm the time of the next meeting. All sessions were held at the hospital where the patients were hospitalized. In the first session, an educational manual was given to the test group and they were asked not to give it to the control group. It was an introductory session for mutual familiarity, expressing the goals and process of the intervention, simple and brief description about cancer, the treatment process, and its effect on the different aspects of the patients' life, and giving an opportunity to them to talk about issues surrounding their ambiguities, questions, worries, as well as to reveal their deepest emotions and concerns related to their experiences about their disease and distressful life events. During the interaction, the patients were evaluated from physical, psychological, social, and spiritual viewpoints as a basis for the theme of the consecutive sessions in order to help the patients to cope or to comply with the current problem using the tasks and strategies mentioned in the booklet.
From the second to the fifth sessions, the patients were asked to talk about the following topics:
Second session: Effect of cancer on physical aspects including effects of the disease on the patients' physical conditions and beliefs, their expectations with the disease, plans and hopes during the progression of the disease regarding their care.
Third session: Psychological distress caused by the disease, the interrelationship between patients' different emotions, physical symptoms, and disabilities caused by the disease, and patients' concerns about the ability to adapt, loss of control, and preparation to accept help, as well as discussions surrounding death.
Fourth session: Social effects of the disease including the effect of the disease on patients' behavior and ability to perform their role completely, as well as the effect of the disease on patients' loved ones.
Fifth session: Spiritual and existential effects of the disease including discussion regarding the concept of the disease, suicide and death, ability to improve and make spiritual changes, compliance with self from a spiritual viewpoint, forgiving others, and accepting incomplete tasks.
Sixth session: Concluding the issues discussed during the previous sessions and termination of the sessions.
During each session, first, the feedback of the patients from the previous session was studied, and then, after conversing about the topics discussed in each session, some applicable coping strategies were offered based on the educational manual in accordance with the condition and problems of each patient. These strategies also provided a basis for the assignments given to the patient, and they were required to perform the tasks by the next meeting. Moreover, during the session intervals, phone tracking was used to encourage patients to perform the tasks. In the last session, the psychological distress questionnaire was completed again by the test group.
The control group received routine care, and after 3 weeks, the questionnaire was completed again by them. At the end, an educational manual was given to the patients and their families in a 2-hour meeting; the content of the manual was briefly explained to the control group. A phone number was given to the patients in the test and control groups so that they can contact the researcher and question about the contents of the manual in case of a problem. The inclusion and exclusion status of the study sample is shown in Figure 1.
Figure 1.
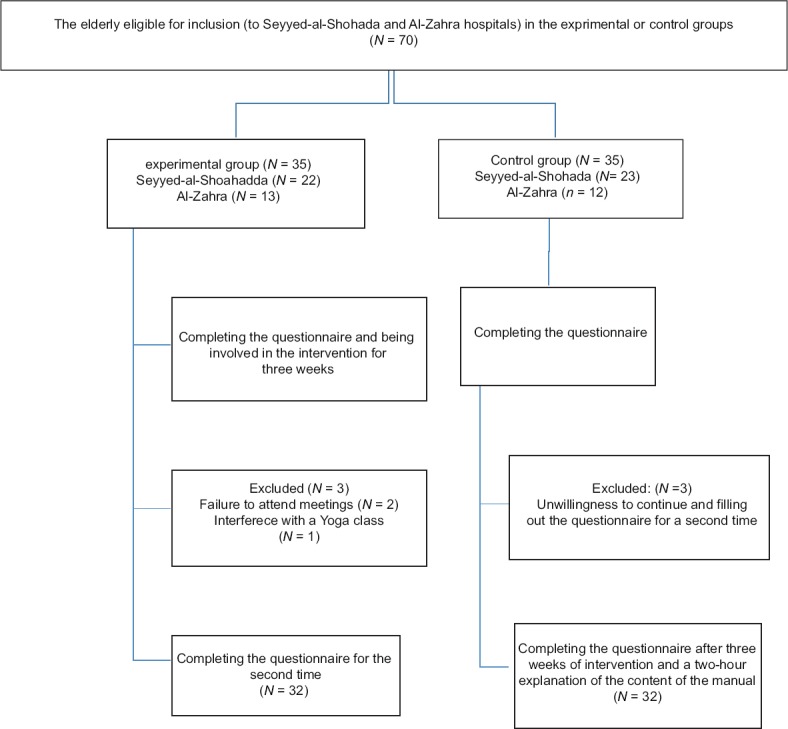
Inclusion and exclusion status of the study sample (consort chart)
In this study, data were collected using two questionnaires. The first questionnaire was related to the patients' demographic information including age, sex, marital status, education, occupation, income, lifestyle, type of cancer, duration of the disease, current treatments and therapies, previous therapies, and usage of narcotic substances. The second tool was Kessler Psychological Distress Scale including 10 questions (K10) to be scored on a 5-point Likert scoring system (never, sometimes, rarely, sometimes, often, or always); thus, the total score obtained ranged from 10 to 50. The questionnaire evaluates different emotions of patients including causeless uncaused fatigue, nervousness, frustration, restlessness and agitation, depression, inability to get things done, and sadness and feeling of worthlessness.[26] For the purposes of this study, the mean scores obtained by patients were used to measure their psychological distress. The questionnaire can be completed within 5 minutes, and the patients should complete it according to their condition during the last 4 weeks.
In this study, the Kessler questionnaire was utilized which is a nonspecific psychological distress measurement scale with high internal consistency and reliability, which is widely used in clinical and epidemiologic settings. Because of the briefness and normality of the questions, this questionnaire is suitable for busy clinical environments,[27] and the brief assessment tool is an efficient means for examining distress of patients with cancer.[9] The use of such a questionnaire can lead to further validity of the results.
Kessler Psychological Distress Scale has been used in various studies. To determine the validity and reliability of this questionnaire in the context of Iran, it was administered to 500 students in Tehran University of Medical Sciences who were selected by relative sampling. A Cronbach's alpha coefficient of 93% and Spearman–Brown reliability of 91% were obtained. In a study by Darvishi et al. conducted on patients with obsessive-compulsive disorder, the Cronbach alpha was 87%.[28] In studies among patients with alcohol-related disorders, the Cronbach's alpha for K10 was 84%.[29] Moreover, in a study conducted regarding distress of medical students, Cronbach's alpha for K10 was 95%,[26] all representing the high reliability of this instrument.
To analyse that the data obtained from this study were of continuous quantitative and qualitative (nominal, ordinal) type, the Statistical Package for the Social Sciences (SPSS) version 18 (SPSS Inc., Chicago, IL, USA) was used, and descriptive and inferential statistical methods (Chi-square and paired and independent t-test) were performed. The significant level was set at P < 0.05.
Ethical considerations
Approval for conducting the study was received from ethics committee of the Isfahan University of Medical Sciences. After offering the recommendation letter to the hospital staff, written informed consent was provided by patients; the participants could withdraw from the study at any time if they so desired.
Results
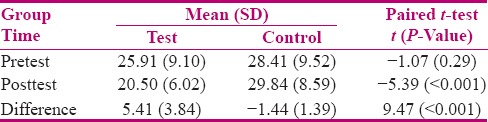
The study sample included 64 patients with a mean age of 69.86 (SD = 6.6). The experimental and control groups were homogeneous in terms of demographic and disease-related characteristics (P > 0.05) [Tables 1 and 2]. The difference in the psychological distress scores of the elderly patients with cancer in the experimental and control groups was significant (P < 0.001) before and after the intervention, whereas the mean score between the two groups before the intervention did not have a significant difference (P < 0.05) [Table 3]. In the experimental group, the mean score of psychological distress was lower after the intervention 20.5 (SD = 6.2), t = 7.96, and P < 0.001, whereas in the control group, the mean of psychological distress score had an increase 32.56 (SD = 7.50), t = −5.85 and P < 0.001 after the intervention.
Table 1.
Comparison of the frequency of clinical and demographic information of the experimental and control groups before the intervention
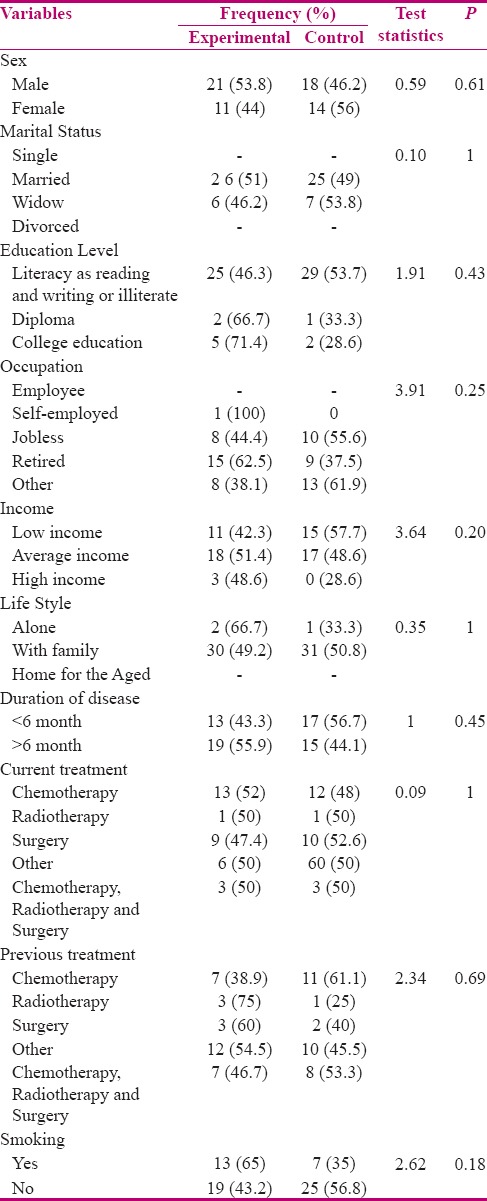
Table 2.
Comparison of the frequency of cancer type in the experimental and control groups before the intervention
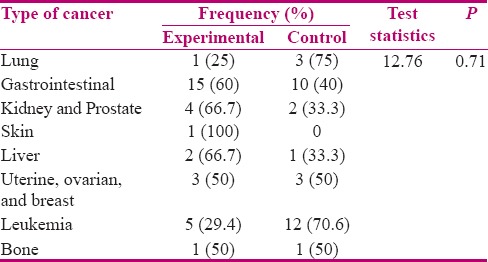
Table 3.
Comparison the psychological distress of elderly patients’ mean scores and mean differences between the two groups before and after the intervention
Discussion
This study is one of the first studies to examine the impact of an intervention on the level of psychological distress of the elderly with cancer in Iran. The results indicated that there was no statistically significant difference between demographic variables and clinical information of the elderly before the intervention, and thus, the two groups were homogeneous. The findings indicated that the mean score of psychological distress in the test group significantly decreased after the intervention compared to the control group, suggesting that the intervention can reduce psychological distress of the elderly suffering from cancer. The current intervention program can easily be applied by nurses and the care team, and it is acceptable, satisfactory, and within the patience levels of the elderly. Moreover, this program covers different aspects including physical, psychological, social, and spiritual-existential aspects of patients and offers coping strategies for problems in any of the aforementioned areas. Above all, by giving tasks to the patients and encouraging them to do them in an attempt to help them to cope with the current problems and by phone tracking between the session intervals, this program creates an applicable, dynamic, mutual, patient-oriented interaction.
The findings of this study are consistent with those of the similar studies addressing psychological distress among cancer and non-cancer patients. For example, Chamber et al. conducted a study with the goal of reducing distress in patients with cancer by a telephonic psychological intervention, and observed that the psychological distress reduced after the intervention in the experimental group. The present study was similar to that study in that the intervention was a combination of both personal attendance, phone tracking, and assigning tasks to the patients to perform; however, the fact that the intervention were carried out by a nurse in one group and by psychologists in the other group could have influenced the results. Moreover, the study had no control group[25] while the intervention in this study was carried out by the same person in both the groups and the study also had a control group.
Johnson et al. studied the effectiveness of expressing emotions in a written mode on the cancer-related distress of patients who survived from breast cancer while only phone interventions were involved. After the intervention, the psychological symptoms in both the groups reduced; however, because the patients were those who survived from cancer, the researchers called for a need to conduct further studies to reveal the impact of cancer-related distress.[22] While the participants of our study were struggling with cancer during the study, it is likely that changes in the level of distress be more cancer-related.
The study by Schellekens et al. aimed to reduce distress in patients with lung cancer. To this end, they dealt with tranquilizing the patients' mind by reducing their distress by giving them educational CDs and tasks to perform. Although the intervention reduced the level of distress in the patients, studying patients with lung cancer imposed some limitations on the results; many patients were excluded from the study given the fluctuation in health status and poor health during chemotherapy and radiotherapy.[23] This has been conducted among patients with different cancer types.
A similar study[10] compared the effect of two interventions, i.e., cognitive behavioral therapy and aromatherapy, on the distress of cancer patients. The results showed that through both the methods, the patients' distress reduced significantly after the intervention with routine care. In a longitudinal study,[21] hope-oriented intervention reduced psychological distress in patients with cancer. Further, in a study[24] conducted on people suffering from depression, the level of distress in the experimental group was significantly lower than that in the control group; hence, the results were consistent with those of the present study.
The results of this study showed that, in the control group, the psychological distress score increased after the intervention. One of the probable reasons for the increase in the psychological distress score of the control group can be the acuteness of the cancer and worsening physiological condition of the elderly in the course of three weeks, because during cancer, patients are confronted with increasing psychological pressures.[9] Similarly, in a study[30] that evaluated the psychological distress of the elderly with lung cancer who were under treatment with palliative radiotherapy before and after the intervention, a worsening trend in psychological distress was identified after treatment, however, the results were not statistically significant.
It is likely that talking to the test group over 3 weeks, apart from psychological distress intervention, could have been responsible for the reduction of the psychological distress scores of the elderly. In a similar study[31] examining the impact of nurse–patient relationship, patients in the intervention group showed a decrease in the level of their distress after the intervention which was not statistically significant, whereas in the present study, the psychological distress of the experimental group decreased significantly after the intervention.
The findings of this study should be considered along with its limitations. First, the presumption underpinning the study was that all the patients involved in the study had similar perceptions regarding the questions in the questionnaire. However, because some of the patients were illiterate, the questions were read and explained to them, and hence, their perception might be different from the perception of those who read and completed the questionnaire by their own. Second, there is no awareness about whether there is a difference between the distress level among those who agreed to participate in the study and those who did not. Third, one of the inclusion criteria was the ability of the elderly to talk and communicate verbally, so people with poor physical performance and advanced stages of cancers were excluded from the study; therefore, the results may not be generalizable to patients with more advanced stages of cancer. Fourth, the sample of the current study suffered from different types of cancer, but the effect of the type of cancer on the level of distress was not evaluated, which needs to be addressed in future studies. Finally, due to possible mortality problems in the elderly, follow-up tracking was not done this study, and hence, it is recommended that future studies include follow ups.
Conclusions
The findings of this study indicated that the communication program had a positive and meaningful effect on reducing the psychological distress among elderly patients with cancer. This program which focuses on the different aspects of distress can be an effective, safe, affordable, and applicable solution to reduce psychological distress of elderly patients suffering from cancer, preventing further worsening of their condition. It is recommended that more extensive longitudinal studies with a lasting impression be conducted to strengthen the current findings and overcome the limitations of the current study.
Financial support and sponsorship
Funding for this study was provided by Isfahan University of Medical Sciences.
Conflicts of interest
There are no conflflicts of interest.
Acknowledgment
This article was derived from a master thesis of Fateme Hejazi with project number 394588, Isfahan University of Medical Sciences, Isfahan, Iran. We appreciate the Clinical Research Development Centres of Al-Zahra hospital and Seyyed-Al-Shohada cancer association. The authors would also like to thank the centre for development of clinical studies of Nemazee Hospital for Statistical assistance.
References
- 1.Hong JF, Zhang W, Song YX, Xie LF, Wang WL. Psychological distress in elderly cancer patients. Int J Nurs Sci. 2015;2:23–7. [Google Scholar]
- 2.Eshrati B, Hatami H, Alizadeh M, Rafie M, Akbari MS. Geograghical distribution and survival rate of cancers among elderly Iranians. Payesh. 1391;11:603–9. [Google Scholar]
- 3.Kim SJ, Rha SY, Song SK, Namkoong K, Chung HC, Yoon SH, et al. prevalence and associated factor of psychological distress among Korean cancer patients. Gen Hosp Psychiatry. 2011;33:246–52. doi: 10.1016/j.genhosppsych.2011.02.008. [DOI] [PubMed] [Google Scholar]
- 4.Clark PG, Rochon E, Brethwaite D, Edmiston KK. Screening for psychological and physical distress in a cancer inpatient treatment setting: A pilot study. Psychooncology. 2011;20:664–8. doi: 10.1002/pon.1908. [DOI] [PubMed] [Google Scholar]
- 5.Smith AB, Armes J, Richardson A, Stark DP. Psychological distress in cancer survivors: The further development of an item bank. Psychooncology. 2013;22:308–14. doi: 10.1002/pon.2090. [DOI] [PubMed] [Google Scholar]
- 6.Gao W, Bennett MI, Stark D, Murry S, Higginson IJ. psychological distress in cancer from survivorship to end of life care: Prevalence associated factors and clinical implications. Eur J Cancer. 2010;46:2036–44. doi: 10.1016/j.ejca.2010.03.033. [DOI] [PubMed] [Google Scholar]
- 7.Bonacchi A, Rossi A, Bellotti L, Franco S, Toccafondi A, Miccinesi G, et al. Assessment of psychological distress in cancer patients: A pivotal role for clinical interview. Psychooncology. 2010;19:1294–302. doi: 10.1002/pon.1693. [DOI] [PubMed] [Google Scholar]
- 8.Akechi T, Okuyama T, Endo CH, Sagawa R, Uchida M, Nakaguchi T, et al. Patient's perceived need and psychological distress and/or quality of life in ambulatory breast cancer patients in Japan. Psychooncology. 2011;20:497–505. doi: 10.1002/pon.1757. [DOI] [PubMed] [Google Scholar]
- 9.Ryan DA, Gallagher P, Wright SH, Cassidy EM. Sensitivity and specificity of the Distress Thermometer and a two-item depression screen (Patient Health Questionnaire-2) with a 'help' question for psychological distress and psychiatric morbidity in patients with advanced cancer. Psychooncology. 2012;21:1275–84. doi: 10.1002/pon.2042. [DOI] [PubMed] [Google Scholar]
- 10.Serfaty M, Wilkinson S, Freeman C, Mannix K, King M. The ToT Study: Helping with Touch or Talk (ToT): A pilot randomised controlled trial to examine the clinical effectiveness of aromatherapy massage versus cognitive behaviour therapy for emotional distress in patients in cancer/palliative care. Psychooncology. 2012;21:563–9. doi: 10.1002/pon.1921. [DOI] [PubMed] [Google Scholar]
- 11.Couture M, Lariviere N, Lefrancois R. Psychological distress in older adults with low functional independence: A multidimensional perspective. Arch Gerontol Geriat. 2005;41:101–11. doi: 10.1016/j.archger.2004.12.004. [DOI] [PubMed] [Google Scholar]
- 12.Baljani E, Salari lak Sh, Salimi S, Safari S, Alavi E, Abdollahi Movahed S. Health Promotion Practices and Cancer Screening in Older Adults of Urmia. Urmia Medical Journal summer. 2010;21:217–23. [Google Scholar]
- 13.Asadi-Lari M, Madjd Z, Afkari ME, Goushegir A, Baradaran HR. The Concept of Palliative Care Practice among Iranian General Practitioners. Iran J Cancer Prev. 2009;2:111–6. [Google Scholar]
- 14.Meijer A, Roseman M, Delisle VC, Milette K, Levis B, Syamchandra A, et al. effects of screening for psychological distress on patients outcomes in cancer: A systematic review. J Psychosom Res. 2013;75:1–17. doi: 10.1016/j.jpsychores.2013.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Salmon P, Clark L, McGrath E, Fisher P. Screening for psychological distress in cancer: Renewing the research agenda. Psychooncology. 2015;24:262–8. doi: 10.1002/pon.3640. [DOI] [PubMed] [Google Scholar]
- 16.Bahrami M. Why differences exist? an interpretive approach to nurses' perceptions of cancer patients' quality of life. Iran J Nurs Midwifery Res. 2011;16:117–24. [PMC free article] [PubMed] [Google Scholar]
- 17.Bahrami M. Iranian Nurses Perceptions of Cancer Patients Quality of Life. Iran J Cancer Prev. 2016;9:e4076. doi: 10.17795/ijcp-4076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bahrami M, Arbon P. How do nurses assess quality of life of cancer patients in oncology wards and palliative settings? Eur J Oncol Nurs. 2012:16. doi: 10.1016/j.ejon.2011.05.003. [DOI] [PubMed] [Google Scholar]
- 19.Stevens K. Therapeutic Communication with Older Adults. In: Mauk KL, editor. Gerontological nursing competencies for care. 2nd ed. Sudbury, Massachusetts: Jones & Bartlett publishers; 2010. p. 106. [Google Scholar]
- 20.Bakhtiari S, Mohammadzade Sh, Moshtagh Z. Obstacles in nurse-elderly patient relationship from the patients' point of view. Iran J Nurs Midwifery Res. 2009;14:77–82. [Google Scholar]
- 21.Sharif Nia SH, Hojjati H, Nazari R, Qorbani M, Akhoondzade G. The effect of prayer on mental health of hemodialysis patients. Iran J Crit Care Nurs. 2012;5:29–34. [Google Scholar]
- 22.Jensen-Johansen MB, Christensen S, Valdimarsdottir H, Zakowski S, Jensen AB, Bovbjeg DH, et al. Effects of an expressive writing intervention on cancer-related distress in Danish breast cancer survivors – Results from a nationwide randomized clinical trial. Psychooncology. 2013;22:1492–500. doi: 10.1002/pon.3193. [DOI] [PubMed] [Google Scholar]
- 23.Schellekens MP, Hurk GM, Prins JB, Molema J, Donders AR, Woertman WH, et al. Study protocol of a randomized controlled trial comparing Mindfulness-Based Stress Reduction with treatment as usual in reducing psychological distress in patients with lung cancer and their partners: The MILON study. BMC Cancer. 2014;14:1–9. doi: 10.1186/1471-2407-14-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Songprakun W, McCann TV. Evaluation of a bibliotherapy manual for reducing psychological distress in people with depression: A randomized controlled trial. J Adv Nurs. 2012;68:2674–84. doi: 10.1111/j.1365-2648.2012.05966.x. [DOI] [PubMed] [Google Scholar]
- 25.Chambers SK, Girgis A, Occhipinti S, Hutchison S, Turner J, Carter R, et al. Beating the blues after Cancer: Randomised controlled trial of a tele-based psychological intervention for high distress patients and carers. BMC Cancer. 2009;9:1–7. doi: 10.1186/1471-2407-9-189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Saravanan C, Kingston R. A randomized control study of psychological intervention to reduce anxiety, amotivation and psychological distress among medical students: An effectiveness of psychological intervention for test anxiety. J Res Med Sci. 2014;25:494–7. [PMC free article] [PubMed] [Google Scholar]
- 27.Bahramkhani M, Farnam A, Bakhshipour A, Mahmoud Alilou M, Darvishi N. Theory of Mind in Obsessive- Compulsive Disorder patients versus Normal Individuals. Adv Cogn Sci. 2013;15:77–89. [Google Scholar]
- 28.Arnaud B, Malet L, Teissedre F, Izaute M, Moustafa F, Geneste J, et al. Validity Study of Kessler's Psychological Distress Scales Conducted Among Patients Admitted to French Emergency Department for Alcohol Consumption–Related Disorders. Alcohol Clin Exp Res. 2010;34:1235–45. doi: 10.1111/j.1530-0277.2010.01201.x. [DOI] [PubMed] [Google Scholar]
- 29.Stallman HM, McDermott BM, Beckmann MM, Wilson MK, Adam K. women who miscarry: The effectiveness and clinical utility of the Kessler 10 questionnaire in screening for ongoing psychological distress. Aust N Z J Obstet Gynaecol. 2010;50:70–6. doi: 10.1111/j.1479-828X.2009.01110.x. [DOI] [PubMed] [Google Scholar]
- 30.Turner NJ, Muers MF, Haward RA, Mulley GP. Psychological distress and concerns of elderly patients treated with palliative radiotherapy for lung cancer. Psychooncology. 2007;16:707–13. doi: 10.1002/pon.1109. [DOI] [PubMed] [Google Scholar]
- 31.Mahmoudi H, Ebadi A, Salimi SH, Najafi Mehri S, Mokhtari Nouri J, Shokrollahi F. Effect of nurse communication with patients on anxiety, depression and stress level of emergency ward patients. J Crit Care Nurs. 2010;3:7–12. [Google Scholar]


