Abstract
Background:
Menopausal period is accompanied by numerous disorders and complications. Nowadays, hormone therapy is the most effective existing method to treat these complications, but many women cannot undergo that due to the known potentiality of risk. So, the present study aimed to investigate the effect of acupressure on early complications of menopause.
Materials and Methods:
This is a blind random clinical trial conducted on 70 menopaused women referring to selected health care centers in Tehran who were qualified to enter the study. The subjects were randomly assigned to study (wearing a special acupressure wrist brace, three times a week for 15 min, in both bands on Shenmen and Sanyinjiao acupoints, in addition to receiving conventional menopausal care) and placebo (wearing a special acupressure wrist brace, three times a week for 15 min, but in a counter wise way, in addition to receiving conventional menopausal care) groups. Length of intervention was 4 weeks. Early complications of menopause were evaluated before intervention and 2 and 4 weeks after intervention in both groups. Data were analyzed by descriptive and inferential statistical methods.
Results:
The findings revealed a significant reduction in the number and severity of hot flashes, the number of night sweats, and state–trait anxiety severity (P < 0.001), but with regard to the severity of night sweats and trait anxiety, there was no significant difference between groups.
Conclusions:
With regard to the obtained results on the effect of acupressure on reduction of early menopausal complications, acupressure along with conventional menopausal care is suggested as one of the complementary medicine methods to improve the complications of this period.
Keywords: Acupressure, anxiety, complications, hot flash, Iran, menopause
Introduction
Menopause, the most important and critical stage of middle-aged women, refers to a complete stop of menstruation for 12 straight months, resulting from lack of ovary follicles and a reduction in estrogen. It averagely occurs at the age of 51 years.[1,2] The signs, occurring in the first post-menopausal months, continue for 1–2 years among most of the women, while in some cases, they go on for up to 3–5 years and are named early menopausal complications. They include hot flash, night sweats, anxiety, palpitation, fatigue, headache, and a reduction in sexual desire.[3,4,5] Some studies have reported the prevalence of hot flash and anxiety to be between 48.9 and 87% and 22.7 and 54%, respectively, in Iran.[6,7] The mechanisms for early complications are not yet completely known. One of these mechanisms is shortage of estrogen, followed by a reduction in endorphins, especially serotonin.[8,9] The first step in treatment of menopausal complications is educating the patients and giving them counseling about related changes in lifestyle during this period.[3] Hormone therapy is the most efficient existing method to treat menopausal complications.[1] But due to its known potential risks including a cardiac arrest, brain stroke, etc., many women cannot undergo such a treatment.[3] Although there are other treatment options available, they are not free of complications or have relative therapeutic responses.[3,10] Therefore, the necessity for non-medicational methods is felt. Among the various types of non-medicational methods, especially complementary and alternative medicine, acupressure is the one which can be managed by physicians, midwives, nurses, or even the patients themselves.[11] Acupressure is a non-invasive and safe technique and is a sort of skill in traditional treatment in which fingers are used to press some key points on the skin.[12] Chinese believe that acupressure balances the vital energy by releasing neurotransmitters and neural hormones and, consequently, improves early menopausal complications.[13] Now, there is a vast research going on regarding the effect of acupressure and acupuncture in treating patients' problems.[14] Whiting et al. reported the effect of acupuncture on Shenmen and Sanyinjiao points on the level of patients' anxiety.[15] In a case–control clinical trial conducted on study group (receiving acupuncture and acupressure) and control group (hormone therapy), the researchers reported a significant reduction in the number of hot flashes in the study group compared to control.[16] As no study directly focusing on the effect of acupressure on early menopausal complications was found in the literature review and with respect to the rapid growth of menopaused women population, conducting the present study with the aim of investigating the effect of acupressure on early menopausal complications seemed necessary to reduce the treatment costs and improve menopaused women's quality of life (QOL) and health and hygiene.
Materials and Methods
This is a clinical trial (IRCT201112278537N) conducted on 70 menopaused women with sleep disorder in Shohada Yaftabad and Shadabad health care centers in on 2012. Sample size according to power was 0.80, effect size was 0.7 and significance level was 0.05 in each 35-member group. The researcher extracted the list of 48–51 year old women by referring to existing family profiles in the selected centers and invited them to the study with the help of health agents. After the congregation, the invited individuals in the centers and checking their height, weight, and BP by the researcher, the goal of the study was explained to them. The subjects meeting the inclusion criteria (purposive) and agreeing to attend the study were selected after giving them further explanations about the study, assuring them about the confidentiality of their information, and obtaining a written consent from them. Then, the subjects were assigned to study and placebo groups through a clinical trial random allocation software, and were coded with numbers (either 1 or 2). The inclusion criteria were: early complications of menopause such as hot flash and night sweats (based on a questionnaire and a daily record form) and anxiety (based on Spillburger questionnaire); reporting at least two times of hot flash during a day before the study; normal menopause; at least 12 months or more having passed after the menstruation stopped (based on subjects' self-report); no application of hormone therapy in the past 6 months; not taking any tranquilizers, Isoflaven complements, herbals, and vitamin E; no history of current systemic or chronic known diseases like diabetes, cardiovascular diseases, thyroid diseases, etc., (based on a physician's visit); absence of any serious events such as acute and serious diseases of a family member or their death, a divorce, unexpected events such as an accident during the past 6–12 months; absence of a current acute known disease in hands or legs acting as an obstacle for the administration of the technique; no addiction and drug abuse, drinking and smoking; and no current application of acupressure. The exclusion criteria were: development of medical problems during the study, loss of interest to stay in the study, incorrect use of the wrist braces, any diagnosed mental disorders leading to anxiety, and occurrence of miserable events during the study. The intervention lasted for 1 month. The intervention was administered as two sessions of 2 h duration. At the end of every 2 weeks, the confounding factors and exclusion criteria were rechecked based on number 2 questionnaire. State and trait anxiety was measured by Spillburger questionnaire, based on the supervisor's indication and literature review.[16,17] To administer routine menopausal care sessions including counseling and for educating the patient about the importance of lifestyle-related changes, health and menopausal complications, measurement of height, weight, BP, breast exam, and Pap smear test were conducted for each group separately on different days (to make the study blind to the subjects), once at the beginning of the first week and another time at the beginning of the third week. In these sessions, the subjects were given two wrist braces with a pressure button and the researcher educated them about the correct method of their usage. They were trained to wear the wrist braces three times a week (every other day) for 15 min once a day on the special points (Shenmen: On horizontal line of the wrist and in internal side of ulnar bone), (Sanyinjiao: 3 cuns superior to the internal malleolus prominence, one finger behind the inner edge of the tibia bone), and [fuliu: In the antero-external face of the leg and 2 cuns upper than Taixi point (between internal ankle and calcaneal tendon)], based on the supervisor's indication and related articles in this context and acupressure and acupuncture textbooks,[12,14] in such a way that the button was exactly laid on the points and the subjects had to press the button until their nails would change color. It should be noted that selection of these points was based on the references and various studies in this context.[13,18,19]
In the placebo group, in addition to routine care, the subject was given two wrist braces with a pressure button and was asked to wear the braces in a counter wise form in such a way that the pressure button was laid outward (no pressure was given to the points). The researcher observed and supervised the subjects while the subjects wore the wrist braces, and solved their problems in wearing them and gave them appropriate feedback. Also, an educational picture showing the exact location of the above-mentioned acupoints was given to each subject at the end of each week; the method of wearing the wrist braces by the subjects was checked through a telephone call. It should be noted the researcher learned the method of finding the acupoints and their use in several educational sessions from an expert of acupressure. Her proper administration of the technique was approved by that expert. Data collection tools were a questionnaire, a daily record form, a tape meter, and scales. Questionnaire number 1 was designed in three sections. The first section included demographic and midwifery characteristics, the second section contained questions on early menopausal complications, and the third section included questions on physical activities which were completed before intervention by the subjects.
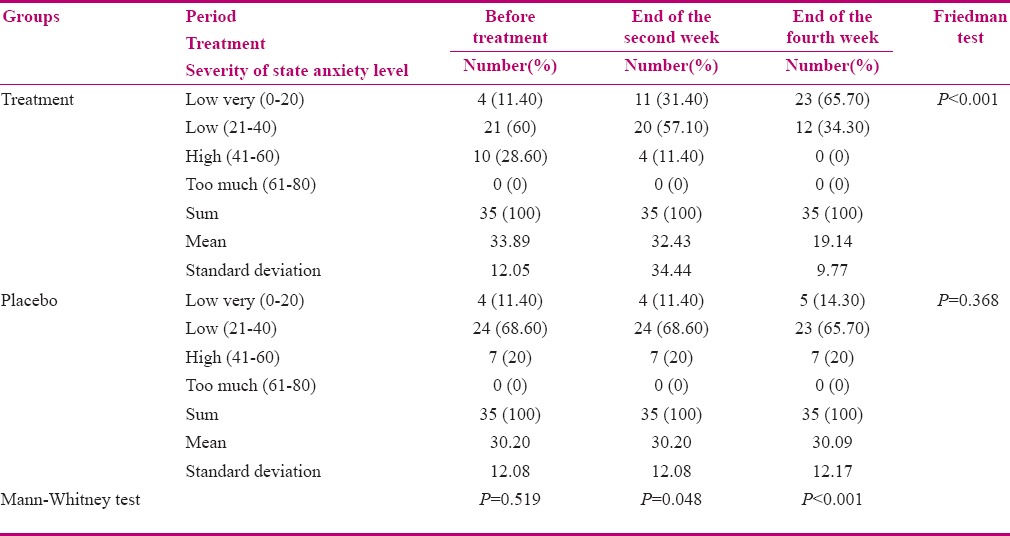
Questionnaire number 2 included the confounding factors and exclusion criteria, which was completed by the researcher through interviewing the subjects at the end of the second and the fourth weeks. Questionnaire number 3, Spillburger anxiety questionnaire, had 40 questions and was used to measure state and trait anxiety. In this questionnaire, each question has four options whose scoring is as follows: very few signs or almost never = score 1, a few signs or sometimes = score 2, many signs or most of the time = score 3, and almost always or many signs = score 4. The scores 0–20, 21–40, 41–60, and 61–80 indicated very low anxiety, low anxiety, high anxiety, and very high anxiety, respectively. This questionnaire was completed by the subjects before intervention and at the end of second fourth weeks of the intervention, based on its instructions as well as many other related conducted studies.[13,14]
Daily record form
This form was filled by the subjects and was associated with the daily number, severity, and the time of hot flash and night sweats. In this form, hot flash severity was scored as minor, moderate, and severe with scores of 1, 2, and 3, respectively. The total score of hot flash was calculated using the formula: (1 × number of minor hot flash) + (2 × number of moderate hot flash) + (3 × number of severe hot flash).[20,21] The severity of night sweats was scored as minor, moderate, and severe with scores of 1, 2, and 3, respectively, and was calculated using the formula: (1 × number of minor night sweats) + (2 × number of moderate night sweats) + (3 × number of severe night sweats).[21,22]
Subjects' weight was measured and recorded with minimum clothing and without shoes, using a digital scale. Height was measured with the subjects in standing position without shoes by a metal meter tape. The body mass index (BMI) was also calculated. Content validity was used to calculate the validity of the questionnaires 1 and 2 and the daily record form. Cronbach's alpha was used to confirm the reliability of the questionnaires 1 and 2 and the daily record form. Cronbach's alphas of the questionnaires 1 and 2 were 0.79 and 0.80, respectively, and for the daily record form, it was 0.83. Spillburger anxiety questionnaire has been used in various studies and has the needed validity and reliability.[23,24] To measure subjects' weight, a specific accurate and standard scale of Seca (made in Germany), model 840, with an accuracy of 0.1 kg was selected. To measure the height, an inflexible meter bar (Lika; made in Italy), with an accuracy of 0.1 cm was used. To establish the reliability of the scales, test re-test method (with a standard weight of 2 kg) was used. Then, the standard weight, after being weighed for 10 times, was again measured by the same scales and no difference was observed. In all cases, before the use of scales, the scale was tuned. The metal meter bar was also standardized. After collecting the data, they were analyzed by descriptive statistics and independent t-test (number and severity of hot flashes and night sweats in both groups), Mann–Whitney test (for the state–trait anxiety between the two groups), Friedman test (for severity of state–trait anxiety in the two groups), and repeated measures analysis of variance (ANOVA; number and severity of hot flash and night sweats) through SPSS18.
Ethical considerations
This research was approved in ethical consideration committee of international Branch of Shahid Beheshti University of Medical Sciences, Tehran, Iran (registration number 1163743).
Results
Seventy subjects out of 79 participants of the research completed the study. The drop-outs comprised nine subjects (four in the study group and five in the placebo group). Three subjects were left out of the study due to their change in residence, one due to spouse's death, and five for irregularity in administration of intervention or absenteeism in the scheduled sessions. Findings showed that the mean ages of menopaused subjects in the study and placebo groups were 49.83 and 55.09 years, respectively, the mean lengths of time after the last menstruation in the study and placebo groups were 1.77 and 1.74 years, respectively, the mean BMI in the study and placebo groups were 24.75 and 24.97 kg/m2, respectively, and the mean numbers of pregnancies were 4.09 and 4.03 times, respectively.
Most of the subjects in both groups were married and had primary school education. There was no significant difference in the above-mentioned variables in the two groups. Findings showed a significant reduction in the number [Table 1] and severity [Table 2] of hot flash and also showed a significant reduction in the Frequency and severity of night sweats [Tables 3 and 4] and state anxiety [Table 5], but there was no significant difference in night sweats and trait anxiety (P > 0.05).
Table 1.
Mean and standard deviation of frequency of hot flashes before treatment and on the first, second, third, and fourth weeks after treatment
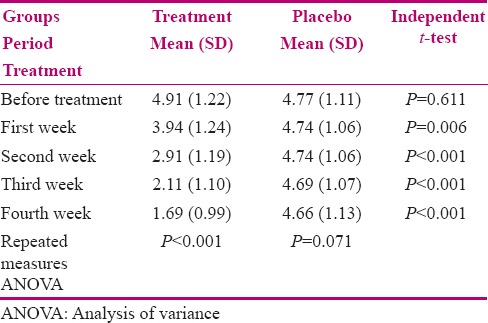
Table 2.
Mean and standard deviation of severity of hot flashes before treatment and on the first, second, third, and fourth weeks after treatment
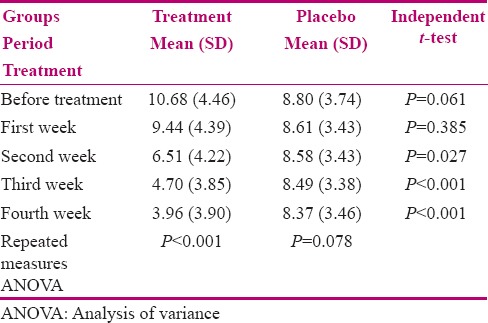
Table 3.
Mean and standard deviation of the frequency of night sweats before treatment and at the first, second, third, and fourth weeks after treatment
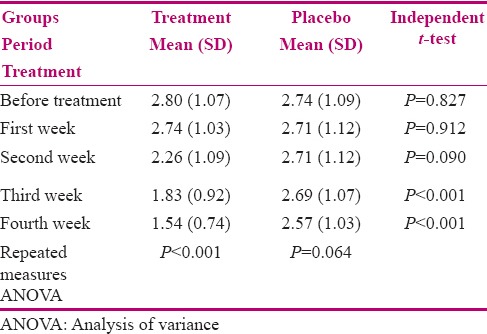
Table 4.
Mean and standard deviation of the severity of night sweats before treatment and at the first, second, third, and fourth weeks after treatment
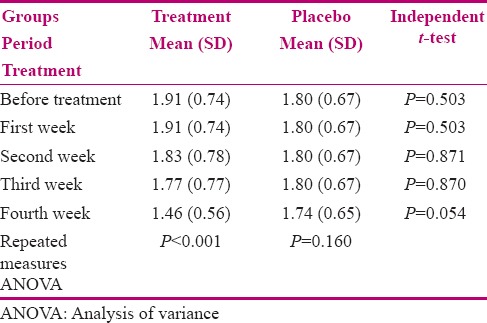
Table 5.
Frequency distribution of subjects according to severity of state anxiety level before treatment and at the end of the second week and fourth week
Discussion
This study, through control of confounding factors, showed that acupressure can relieve early menopausal complications. The findings also showed that acupressure led to a reduction in the number and severity of hot flash, the number of night sweats, and state anxiety, but had no effect on severity of night sweats and trait anxiety. The main mechanism of hot flash is vasodilatation in response to changes in temperature regulation area in the hypothalamus. A sophisticated network of neuroendocrine pathways that includes estrogen or epinephrine and β-endorphin have the role of body temperature regulation through their effect on temperature regulation nucleolus in the hypothalamus.[9] In studies conducted on humans and animals, acupuncture and acupressure were found to cause stimulation of β-endorphins and other neurotransmitters such as serotonin and norepinephrine.[25] With regard to low number of clinical studies on the effect of acupressure on early menopausal complications, the studies with a mechanism of effect, similar to the effect of acupressure on early menopausal complications, are discussed in the following. Our results are in line with those of Kun et al. (2010) on the effect of acupressure on peri- and post-menopausal women's hot flash. In their study, after 4 weeks of intervention, mean number of hot flashes showed a significant intra-group reduction in the groups (P < 0.0001). This reduction was also significant between the groups (P < 0.0001). They also reported a reduction in the number of hot flashes up to 62%.[22] Venzke et al. (2010), in a study on the effect of acupuncture on vasomotor symptoms, reported a significant reduction in vasomotor disorders including hot flash 16 weeks after intervention in the group undergoing acupuncture, compared to placebo group (P < 0.05). The number of hot flashes decreased to 2.6 from 4 in the study group and to 2.5 from 4.5 in the placebo group.[17] Meanwhile, in our study, it decreased to 1.69 from 4.91 in the study group and to 4.66 from 4.77 in the placebo group. The reduction in mean number of hot flash in the study group was more compared to that reported in the study of Venzke et al. The reason can possibly be the subjects' minor to moderate depression (based on Beck depression questionnaire) and the difference in selected acupoints for acupressure in Venzke's study compared to our study. In another study, Giv et al. (2008) investigated the effect of ear acupuncture and acupressure on women's hot flash. They reported no significant difference in severity of hot flash 12 weeks after intervention (P > 0.05), which is not consistent with our results. The difference is possibly due to the difference in study population; in our study, the study population consisted of those with normal menopause, while in Giv's study, the study population consisted of women who had undergone bilateral ovary removal surgery.
On the other hand, the selected acupoints for acupressure in our study were on the wrist and ankle, while in Giv's study acupressure and acupuncture were administered on the ear.[21] Venzke et al. (2010), in a study on the effect of acupuncture on vasomotor disorders, reported a significant reduction in the number of night sweats after intervention (P < 0.05), which is consistent with our study.[17] In their study, they reported a significant difference in mean severity of night sweats 16 weeks after intervention between study and placebo groups, which was not in line with our study. The difference is possibly due to the fact that mean severity of night sweats was 7.39 before intervention in Venzke's study, while it was 6.58 in our study. On the other hand, shorter length of intervention in our study, compared to Venzke's, and using several acupoints (different acupoints) to administer acupuncture in their study can be the reasons for this difference. Although there is no available information about the main mechanism of acupuncture and acupressure, Chinese believe it can improve anxiety disorders and affect individuals' relaxation through regulation of neurotransmitters of central nervous system, including serotonin.[18] Our findings are consistent with the study findings of Ching Ling et al. (2010) who investigated the effect of acupressure on women's anxiety during peri- and post-menopausal periods in a controlled, double-blind clinical trial. They reported a significant reduction in anxiety after intervention (pressure on Shenmen and occipital acupoints) (P < 0.05). They pressed these acupoints four times a day for 3 min. Ching Ling et al. did not consider some of the confounding factors including physical exercise and its length, consumption of herbals, BMI, and economic status.[19] The advantages of our study, compared with Ching Ling's study, is the shorter length of intervention and investigating both state and trait anxiety, as well as controlling the confounding factors.
Deferent Nutrition situations amongst individuals and different moods of them when answering the questionnaires, where limitations of this study.
Conclusion
With regard to the obtained results on the effect of acupressure on reduction of early menopausal complications, acupressure along with conventional menopausal care is suggested as one of the complementary medicine methods to improve the complications of this period.
Financial support and sponsorship
International Branch of Shahid Beheshti University of Medical Sciences, Tehran, Iran.
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
It should be noted that this article was derived from a master's dissertation (registration number 1163743) and has been registered in clinical trial database of Ministry of Health and Medical Education.
References
- 1.Nelson HD. Menopause. Lancet. 2008;371:760–70. doi: 10.1016/S0140-6736(08)60346-3. [DOI] [PubMed] [Google Scholar]
- 2.Kase NG. Impact of hormone therapy for women aged 35 to 65 years, from contraception to hormone replacement. Menopause, Gend Med. 2009;6:37–59. doi: 10.1016/j.genm.2009.02.001. [DOI] [PubMed] [Google Scholar]
- 3.Berek JS, Adashy Y, Anderson R, Alvares A, Amesses S, Baker V. Berek and Novaks Gynecology. 15th ed. Philadelphia: Lippincott Williams and Wilkins; 2011. pp. 1323–37. [Google Scholar]
- 4.Deecher DC, Dorries K. Understanding the pathophysiology of vasomotor symptoms (hot flushes and night sweats) that occur in perimenopause, menopause, and postmenopause life stages. Arch Women’s Ment Health. 2007;10:247–57. doi: 10.1007/s00737-007-0209-5. [DOI] [PubMed] [Google Scholar]
- 5.Lyytinen H. Helsinki, Finland: Helsinki University print; 2009. A Nationwide study on breast cancer risk in post menopaus al women using hormone therapy in Finland. Academic dissertation. [Google Scholar]
- 6.parhizgar A. Knowledge and Practice of Women The physiological changes and prevent Menopausal symptoms in a health clinic in Sanandaj. J Nurs Midwifery Kordstan. 2004;2:21–6. [Google Scholar]
- 7.Tarvirdy M, Shabani A. Study of menopausal women with mental health problems And its relationship with socio-demographic characteristics and symptoms of menopause. J Nurs Midwifery Oromieh. 2005;5:1–7. [Google Scholar]
- 8.Sturdee DW. The menopausal hot flush-anything new? Maturitas. 2008;60:42–9. doi: 10.1016/j.maturitas.2008.02.006. [DOI] [PubMed] [Google Scholar]
- 9.Rossmanith WG, Ruebbert W. The Noroendocrine Origin of Vasomotor Symptoms in the Menopause. Gynecol Endocrinol. 2009;5:303–14. doi: 10.1080/09513590802632514. [DOI] [PubMed] [Google Scholar]
- 10.Sperof L, Fritz MA. Clinical Gynecologyc Endocrinology and Infertility. 8th ed. Philadelphia: Lippincott; 2010. pp. 621–73. [Google Scholar]
- 11.Maa Sh, Tsou TS, Wang KY, Wang CH, Lin HC, Huang YH. Self-administered acupressure reduces the symptoms that limit daily activities in bronchiectasis patients: Pilot study findings. J Clin Nurs. 2007;16:794–804. doi: 10.1111/j.1365-2702.2005.01515.x. [DOI] [PubMed] [Google Scholar]
- 12.Marcus B, Michael G. Acupuncture in the Treatment of Pain: An Integrative Approach. Elsevier Health Sciences. 1st ed. Edinburgh, London: Churchill Livingstone; 2010. pp. 370–80. [Google Scholar]
- 13.Tsay SL, Chen HL, Chen SC. Effects of reflexology on acute postoperation pain and anxiety among patients with digestive cancer. Cancer Nurs. 2008;31:109–15. doi: 10.1097/01.NCC.0000305694.74754.7b. [DOI] [PubMed] [Google Scholar]
- 14.Pilkington K. Anxiety, depression and acupuncture: A review of the clinical research. Auton Neurosci. 2010;157:91–5. doi: 10.1016/j.autneu.2010.04.002. [DOI] [PubMed] [Google Scholar]
- 15.Whiting M, Leavey G, Scammell A, Au S, King M. Using acupuncture to treat depression: A feasibility study. Complement Ther Med. 2008;16:87–91. doi: 10.1016/j.ctim.2007.07.005. [DOI] [PubMed] [Google Scholar]
- 16.Kun HK, Kyung WK, Hyung JK, Hyun MY, Jae CJ, Myeong SL, et al. Effects of acupuncture on hot flashes in perimenopausal and postmenopausal women Va multicenter randomized clinical trial. Menopause. 2010;17:269–80. doi: 10.1097/gme.0b013e3181bfac3b. [DOI] [PubMed] [Google Scholar]
- 17.Venzke L, Calvert JR, Gilbertson B. A randomized trial of acupuncture for vasomotor symptoms in post-menopausal women. Complement Ther Med. 2010;18:59–66. doi: 10.1016/j.ctim.2010.02.002. [DOI] [PubMed] [Google Scholar]
- 18.Chen HM, Chen CH. Effects of acupressure on menstrual distress in adolescent girls: A comparison between Hegu-Sanyinjiao matched points and Hegu, Zusanli single point. [Last accessed on 2010 Apr 19];J Clin Nurs. 2010 19:998–1007. doi: 10.1111/j.1365-2702.2009.02872.x. Available from: http://wwwncbinlmnihgov/pubmed/20492044 . [DOI] [PubMed] [Google Scholar]
- 19.Kao CL, Chen CH, Lin WY, Chiao YC, Hsieh CL. Effect of Auricular Acupressure on Peri-and Early Postmenopausal Women with Anxiety: A Double-Blinded, Randomized, and Controlled Pilot Study. Evid Based Complement Alternat Med. 2012;2012:567639. doi: 10.1155/2012/567639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zhou J, Qu F, Sang X, Wang X, Nan R. Acupuncture and auricular acupressure in relieving menopausal hot flashes of bilaterally ovariectomized chinese women: A randomized controlled trial. [Last accessed on 2009 Jan 12];Evid Based Complement Alternat Med. 2011 2011:713274. doi: 10.1093/ecam/nep001. Available from: http://www.hindawi.com/journals/ecam/2011/713274/abs . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Heather GM. Measuring hot flashes: Summary of national institute of health workshop. Mayo Clin Proc. 2004;79:777–81. doi: 10.4065/79.6.777. [DOI] [PubMed] [Google Scholar]
- 22.Lucas M, Asselin G, Mérette C, Poulin MJ, Dodin S. Effects of ethyl-eicosapentaenoic acid omega-3 fatty acid supplementation on hot flashes and quality of life among middle-aged women: A double-blind, placebo-controlled, randomized clinical trial. Menopaus. 2009;16:357–66. doi: 10.1097/gme.0b013e3181865386. [DOI] [PubMed] [Google Scholar]
- 23.Giakoumaki Q, Vasilaki K, Lili L, Skouroliakou M, Liosis G. The role of maternal anxiety in the early postpartum priod: Screening for anxiety and depressive sympatology in Greece. J Psychosom Obstet Gynaecol. 2009;3:21–8. doi: 10.1080/01674820802604839. [DOI] [PubMed] [Google Scholar]
- 24.Skouteris H, Wertheim EH, Rallis S, Milgrom J, Paxton SJ. Affective Disorders Depression and anxiety through pregnancy and the early post partum: An examination of prospective relationship. J Affect Disord. 2009;113:303–8. doi: 10.1016/j.jad.2008.06.002. [DOI] [PubMed] [Google Scholar]
- 25.Avis NE, Pian-Smith MC. Acupuncture for hot flashes. Menopause. 2007;14:10–3. doi: 10.1097/01.gme.0000252908.72738.9f. [DOI] [PubMed] [Google Scholar]


