Abstract
Hip fracture is a significant public health problem affecting an estimated 1.6 million persons annually. The consequences of hip fracture are also significant, with more than half of those who sustain a fracture either dying or not returning to functional abilities present before fracture required to function independently. The Baltimore Hip Studies (BHS) is a program of research that for more than 30 years has been doing investigations to identify, develop, and evaluate strategies to optimize recovery from hip fracture. This paper provides an overview of known outcomes and recovery patterns following a hip fracture, which are derived primarily from the BHS. Target areas and timing for interventions based on this recovery sequence are suggested. The paper concludes with a discussion of some of the areas that the next generation of studies needs to concentrate on in order to advance knowledge about the care of hip fracture patients to maximize their recovery.
Introduction
Hip fractures are a health problem of major significance, affecting over 1.6 million adults annually worldwide [1]. The worldwide annual incidence of hip fractures is projected to increase to 3.9 million by 2050 [2–4]. Outcomes following hip fracture include increased risk of mortality, subsequent hip and nonvertebral fractures, loss of independent function, and other adverse health and economic consequences for patients, families and the health care system [5–11]. The care given to hip fracture patients after discharge is often provided by a spouse, adult child, another family member, or a friend. These informal caregivers face significant burden in the early phases of recovery when the patient is first discharged from the hospital [12–14], which is important since the specific needs of these caregivers have been shown to affect the recovery of the patient [15].
Framework for Research on Hip Fracture Consequences
A framework for examining consequences of hip fracture considers the progression of clinical research which evolves from clinical observation, to description of those who have the condition, understanding of the etiology or causes of the condition, and eventually to understanding underlying mechanisms; the ultimate aim is to use this information to design, implement, and test treatments to ameliorate or reduce the burden of the condition. With hip fracture, we can use this framework and categorize consequences or outcomes into three groups: survival, recovery of functionality, and other consequences. Survival includes survival versus death, time until death, and causes of death. Functional areas of recovery include physical, instrumental, affective, social, and cognitive function, as well as strength, physical capacity, and pain. Other consequences that have been examined include refracture, changes in body composition, including bone mineral density (BMD) and muscle and fat mass, costs, rehospitalizations, health care, and community service use, caregiver burden, complications, and re-operations. More recently, emphasis has been placed on changing systems of care delivery to improve outcomes and reduce costs. The increase in utilization of patient-focused care models throughout the health care system has introduced a new challenge for clinical practice and research. It is now necessary to design and evaluate the efficacy and cost-effectiveness of patient-focused/need-based interventions that can be implemented in diverse health care delivery systems that are changing, and to evaluate the effectiveness of these new treatment and management strategies.
Overview of the Baltimore Hip Studies
The goal of the research program of the Baltimore Hip Studies (BHS) is to identify, develop, and evaluate strategies to optimize recovery from hip fracture. The BHS have enrolled and followed more than 3,500 hip fracture patients admitted to 25 hospitals in the Baltimore area over the past 30 years, and BHS leaders have participated in multiple single and multisite studies of hip fracture treatments and outcomes conducted outside of the BHS hospital network. BHS have assessed many diverse outcomes after hip fracture, including mortality and functional recovery, as well as changes in BMD, muscle mass and composition, and strength, balance, falls, medical complications, caregiver burden, and costs. The study designs have progressed from observational, etiological, mechanistic, and interventional over time. This paper provides an overview of known outcomes following a hip fracture derived primarily from the BHS, with a discussion of some of the areas that the next generation of studies needs to focus on to advance the knowledge and care of hip fracture patients.
Survival
Currently, 75% of hip fractures occur among women [2]. While the incidence of hip fracture in women appears to be stabilizing, the incidence in men is expected to increase over the next several decades [16]. Mortality rates are almost double in men compared to women [17]. One year after fracture, the probability of survival is 86% for women and 68% for men [17]. Similarly, 2 years after fracture, the probability of survival is 77% for women and 58% for men [17]. Even though men are often younger when they sustain a fracture, one explanation for the disparity in the mortality rate is that men are often sicker at the time of the fracture than women [17]. Interestingly, both men and women are dying at a higher rate due to infectious causes compared to the general population matched for age and sex, but the excess rate of deaths from infectious causes in men is 2–3 times higher than in women when compared to the general population of older men and women [17].
Physiological Losses after Fracture
Body composition changes have been assessed in the BHS through 12 months after fracture. From 3 to 10 days after fracture, there are minimal changes in total hip and femoral neck BMD [10]. Greater decreases occur from 10 days to 2 months after fracture [18], with significant decreases in total hip BMD (1.3%) and femoral neck BMD (2.0%) [18], and continued decreases through 12 months after fracture with approximate BMD losses of 2.5% in total hip and 4.5% at the femoral neck [19]. When these losses are compared to BMD loss in older women with the same average age (79 years) and with total hip BMD in the same low range (average total hip in hip fx = 0.595 g/cm2; comparison group from the Study of Osteoporotic Fractures = 0.610 g/cm2), the loss of femoral neck BMD in hip fracture patients is more than 12 times greater than expected over the year following hip fracture [19]. In contrast, lean mass experiences a minimal increase from 3 to 10 days after fracture, followed by a steady decrease of 5.4% from 10 days to 2 months after fracture and little change thereafter [18, 20]. Interestingly, fat mass decreases minimally from 3 to 10 days, and continues to decrease until 2 months after fracture [18, 20]. However, from 2 through 12 months, fat mass steadily increases by about 7%, exceeding levels before fracture (need reference here). Sarcopenia, a condition of muscle loss and muscle wasting is prevalent in about 35% of female hip fracture patients within a week of hip fracture and increases to about 50% between day 10 and 2 months, and to about 60% by 1 year after fracture [21].
Additionally, an inflammatory response occurs after fracture. IL-6 levels 3-10 days after fracture are higher than in those of the same age group with functional limitations but no fracture, decrease by 2 months, and remain low through 12 months, but still do not reach the level of similar comparison subjects matched for age and sex [22]. Further, these changes in inflammation are associated with lower levels of physical performance on tests that assess tasks that are relevant to hip fracture patients and their caregivers, such as walking, getting up from a chair, and picking something up from the ground [22, 23].
Functional Recovery
The functional consequences of a hip fracture can be assessed through self-report of Activities of Daily Living (ADLs). Many hip fracture patients who had ADL limitations before fracture experience new limitations that persist for 1 year or more after fracture. While there is steady recovery in ADL from 2 to 12 months, a range of 20–90% of participants who were not impaired in specific tasks prior to their fracture are still experiencing limitations in those tasks 12 months after fracture [10].
Specifically, 20% of participants who were able to put on their own pants prior to fracture are now unable to do so without assistance. For those able to perform tasks without assistance before fracture, 50% used assistance to walk across a room, 50% used assistance to rise from a chair, 55% used assistance to walk a block, 66% used assistance to get on and off of the toilet, and a striking 90% used assistance to climb stairs 1 year later. These disability levels remain through 24 months after fracture. Similarly, participants experience increased limitations with Instrumental ADLs (IADLs), including shopping and housework. We also assessed the percentage of participants after fracture with a dependency in walking 10 feet or across a small room and found that 2 months after fracture, over 90% of participants had a dependency [10]. By 6 months after fracture, the percentage of dependent patients decreased to around 60% but remained at around 55% through 2 years after fracture [10].
Beyond physical disabilities, 50% of patients after a hip fracture experience increases in cognitive deficits in the hospital, and 25% have cognitive deficits 2 months after fracture. Depressive symptoms are similarly experienced among 50% of patients in the hospital, and 25% of patients 2 months after fracture [10]. Further, those who are persistently impaired in cognitive function and who have persistent depressive symptoms do the most poorly in functional recovery over the following 10 months [24–26]. Changes in social function are also experienced, with many patients visiting with others and participating in activities less often than before their fracture [8].
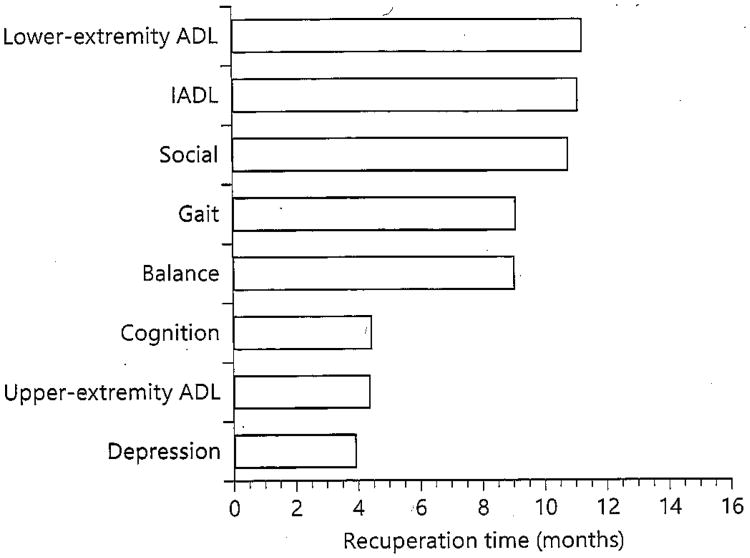
The overall time to maximal recovery under usual care conditions differs across several areas of functioning [10] (fig. 1). While depression, upper-extremity ADLs, and cognition require around 4 months for recuperation, the time is greater for balance and gait recovery at approximately 9 months, and greatest for social function, IADLs, and lower-extremity ADLs, which peak at around 12 months following fracture. From these findings, it can be deduced that the hip fracture recovery process evolves first from recovery from the hip fracture itself at the level of the bone and muscle, then recovery in functional limitations including gait and balance, cognition, and strength, and finally recovery in lower-extremity ADLs and IADLs and social activities [10].
Fig. 1.
Time until recuperation following hip fracture in eight areas of function (from Magaziner et al. [10] with permission of Oxford University Press).
Intervention Timing
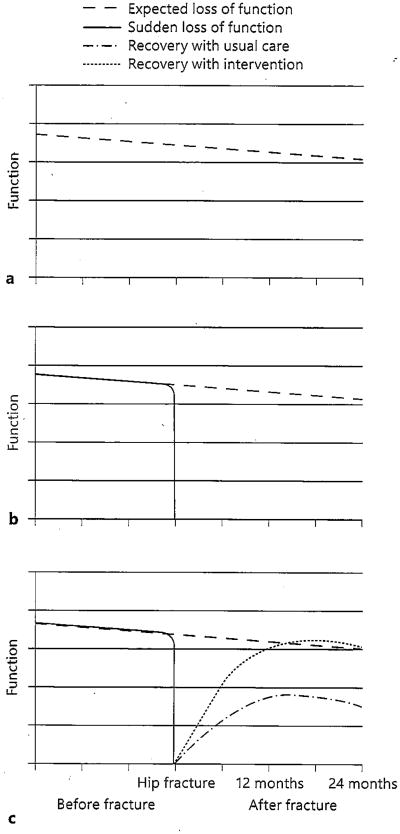
Older adults are expected to experience a gradual loss of function over time (fig. 2a). After a hip fracture, however, older adults experience a sudden loss of function (fig. 2b). With usual care, as described above, there is variation in the rate of recovery by specific area of function and the point at which peak recovery is reached in each. It is also apparent that with usual care, most patients never recover to the functional levels present before the fracture (fig. 2c, dot-dash). With an intervention, the goal is to help patients restore functional levels and, if possible, continue intervening to improve function to surpass functional levels they had before fracture (fig. 2c, dots). While we have an understanding of the losses that occur following a hip fracture, as well as knowledge of how recovery progresses across several physiologic and functional domains, there is, as yet, only limited evidence on what specific interventions to deliver and when to provide interventions to get maximal benefit.
Fig. 2.
Expected loss and recovery of function after hip fracture compared to loss of function from frailty. a Expected loss of function in frail older persons. b Sudden loss of function with hip fracture. c Recovery of function after hip fracture with intervention.
Treatment and Intervention Options
We know that hip fractures are a multifaceted problem requiring multiple treatments and/or interventions. Again, the goal of treatment and interventions is to return patients to or beyond the function levels they had prior to their fracture. In addition to the limited evidence on when treatments should be provided, there is also limited evidence on what specific treatments should be provided.
Several treatments have been suggested for hip fracture patients based on the deficit and recovery sequence, including bone-strengthening medications; other pharmacologic agents, and nutritional and vitamin supplements to address some of the preexisting and emerging deficits in BMD and muscle mass; surgical management to repair the broken bone so that patients have less pain and can stand again; psychological treatments to help re-orient patients from cognitive losses and help them to feel better, which in turn may lead to better adherence to other interventions; gait, balance, and strength training to further increase bone and muscle mass and to help patients regain their ability to stand, walk, and carry out tasks of daily living, and physical, and occupational therapy to help patients perform tasks of daily living. A list of possible treatment areas appears in table 1.
Table 1. Hip fracture treatments suggested by recovery sequence.
| Recovery process | Possible treatments |
|---|---|
| Treat pathology | |
| Osteoporosis | Bone-strengthening medications |
| Chronic conditions | Stabilize exacerbations/control complications |
| Sarcopenia | Anabolic agents/protein/nutritional supplements |
|
| |
| Treat impairment | |
| Hip fracture | Surgical management to repair bone |
| Pain management | |
|
| |
| Reduce functional limitations | |
| Neuromuscular | Gait, balance, and strength training |
| Cognitive | Medical stabilization, orientation therapy |
| Affective | Medication, psychological therapy |
|
| |
| Minimize disability | |
| ADL | Physical therapy |
| IADL | Occupational therapy |
| Social activity | Social engagement therapies |
Patient-, provider-, and intervention-specific considerations exist for designing efficacious and cost-effective interventions for hip fracture patients. Due to the multifaceted nature of hip fracture recovery, a multidisciplinary/multicom-ponent intervention program may be best. The content of this multifaceted program is a work in progress. To be effective, we believe it needs to include multiple components, yet we have not yet determined which specific components are best, nor at what point following the fracture they are most suitably introduced to the recovering hip fracture patient. Most of what we know and do is based on what clinicians and teams of clinicians believe will work best for individual patients; evidence for multimodal programs is limited at best.
Rehabilitation Programs
The multidisciplinary rehabilitation team has been suggested as one way to address the many deficits and needs of hip fracture patients. This team could consist of a geriatrician, specially trained general practitioner, geriatric nurse practitioner, geriatric nursing staff, occupational therapist, physical therapist, social worker, and neuropsychologist. By the team approach, intervention programs should include geriatric assessments with the team, accelerated rehabilitation for the patient, and discharge planning with the multidisciplinary team, the patient, and caregivers. There also should be an assessment of the home environment before discharge, as well as in-home and long-term rehabilitation either in the home or at an outpatient or fitness facility.
We have conducted an extensive review of the recent literature on multidisciplinary hip fracture rehabilitation interventions and found mixed results. We reviewed both early multidisciplinary interventions that include physical activity, as well as long-term interventions that emphasize physical activity. For the early interventions, some studies did show improvements in strength, gait speed, and functional performance. For the long-term interventions, some studies showed improvements in strength, faster walking speed, and functional performance. Center- or community-based programs were usually more beneficial than home-based programs as they were more intensive. Neither center- nor home-based intervention programs demonstrated strong benefits for ‘real-world’ functioning, e.g. ADL, IADL, or quality of life.
The results from the reviews of rehabilitation programs were also not consistent. Some of the studies suggested that interventions with physical activity are beneficial in proximal outcomes, such as strength, gait speed, and functional performance. Studies also did not usually provide precise descriptions of the interventions, which makes it difficult to know what was done and which aspects of interventions are most beneficial.
Conclusion
Hip fracture results in significant mortality and, for those who do not die, significant impairment and functional deficits across multiple physiological and functional areas, all of which need to be considered when designing an effective rehabilitative program. Multidisciplinary/multicomponent interventions have the greatest potential to improve long-term outcomes. Apparent gaps in investigating interventions for hip fracture patients include attention to the optimal timing for specific interventions and the way interventions should be combined to yield the best outcomes. There is also a dearth of information on extended treatment options and long-term outcomes of extended treatment. Ultimately, given the multifaceted losses and changes that take place after a hip fracture, there is a need to identify components of multidisciplinary/multicomponent interventions that have the greatest impact on these deficits at different times during the recovery period after fracture. There also is a need to design programs using effective components that target individual patient needs and evaluate their combined effects. With the growing emphasis on care pathways for hip fracture patients, and the major changes that are taking place across the globe in the way care systems manage hip fracture patients using the best evidence available, there is an ongoing need to develop better evidence that addresses the needs of hip fracture patients, their families, and caregivers. With this information, care systems can include improved strategies for increasing the likelihood that hip fracture patients will recover more fully.
Acknowledgments
The authors would like to thank the National Institute on Aging for their support of research on hip fracture recovery for more than 25 years, which has allowed investigators in the BHS to address issues relevant to recovery from hip fracture. We also would like to thank the orthopedic surgery, medical, nursing, social work, and physical therapy providers in the 25 hospitals in the BHS network who have enabled us to pursue this important work, and of course, the many patients and families of patients who have participated in this research.
Footnotes
Disclosure Statement: During the past two years, Dr. Magaziner was consultant, advisory board member, or grant recipient from the following organizations: National Institute of Health, American Orthopaedic Association, Ammonett, Novartis, Merck, Regeneron, Sanofi, Viking. Dr. Orwig was consultant to Kinexum, Sanofi and Viking during this period.
References
- 1.Johnell O. The socioeconomic burden of fractures: today and in the 21st century. Am J Med. 1997;103:20S–25S. doi: 10.1016/s0002-9343(97)90023-1. discussion 25S-26S. [DOI] [PubMed] [Google Scholar]
- 2.Stevens JA, Olson S. Reducing falls and resuiting hip fractures among older women. MMWR Recomm Rep. 2000;49(RR-2):3–12. [PubMed] [Google Scholar]
- 3.Cooper C, Campion G, Melton LJ., III Hip fractures in the elderly: a world-wide projection. Osteoporos Int. 1992;2:285–289. doi: 10.1007/BF01623184. [DOI] [PubMed] [Google Scholar]
- 4.Gullberg B, Johnell O, Kanis JA. World-wide projections for hip fracture. Osteoporos Int. 1997;7:407–413. doi: 10.1007/pl00004148. [DOI] [PubMed] [Google Scholar]
- 5.Stevens JA, Rudd RA. The impact of decreasing US hip fracture rates on future hip fracture estimates. Osteoporos Int. 2013;24:2725–2728. doi: 10.1007/s00198-013-2375-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Burge R, Dawson-Hughes B, Solomon DH, et al. Incidence and economic burden of osteoporosis-related fractures in the United States, 2005-2025. J Bone Miner Res. 2007;22:465–475. doi: 10.1359/jbmr.061113. [DOI] [PubMed] [Google Scholar]
- 7.Dempster DW. Osteoporosis and the burden of osteoporosis-related fractures. Am J Manag Care. 2011;17(suppl 6):S164–S169. [PubMed] [Google Scholar]
- 8.Magaziner J, Simonsick EM, Kashner TM, et al. Predictors of functional recovery one year following hospital discharge for hip fracture: a prospective study. J Gerontol. 1990;45:M101–M107. doi: 10.1093/geronj/45.3.m101. [DOI] [PubMed] [Google Scholar]
- 9.Fox KM, Hawkes WG, Hebel JR, et al. Mobility after hip fracture predicts health outcomes. J Am Geriatr Soc. 1998;46:169–173. doi: 10.1111/j.1532-5415.1998.tb02534.x. [DOI] [PubMed] [Google Scholar]
- 10.Magaziner J, Hawkes W, Hebel JR, et al. Recovery from hip fracture in eight areas of function. J Gerontol A Biol Sci Med Sci. 2000;55:M498–M507. doi: 10.1093/gerona/55.9.m498. [DOI] [PubMed] [Google Scholar]
- 11.Magaziner J, Fredman L, Hawkes W, et al. Changes in functional status attributable to hip fracture: a comparison of hip fracture patients to community-dwelling aged. Am J Epidemiol. 2003;157:1023–1031. doi: 10.1093/aje/kwg081. [DOI] [PubMed] [Google Scholar]
- 12.Nahm ES, Resnick B, Orwig D, et al. Exploration of informal caregiving following hip fracture. Geriatr Nurs. 2010;31:254–262. doi: 10.1016/j.gerinurse.2010.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Siddiqui MQ, Sim L, Koh J, et al. Stress levels amongst caregivers of patients with osteoporotic hip fractures - a prospective cohort study. Ann Acad Med Singapore. 2010;39:38–42. [PubMed] [Google Scholar]
- 14.Lin PC, Lu CM. Hip fracture: family caregivers' burden and related factors for older people in Taiwan. J Clin Nurs. 2005;14:719–726. doi: 10.1111/j.1365-2702.2005.01130.x. [DOI] [PubMed] [Google Scholar]
- 15.Shyu YI, Chen MC, Liang J, Tseng MY. Trends in health outcomes for family caregivers of hip-fractured elders during the first 12 months after discharge. J Adv Nurs. 2012;68:658–666. doi: 10.1111/j.1365-2648.2011.05778.x. [DOI] [PubMed] [Google Scholar]
- 16.Orwig DL, Chan J, Magaziner J. Hip fracture and its consequences: differences between men and women. Orfhop Clin North Am. 2006;37:611–622. doi: 10.1016/j.ocl.2006.08.003. [DOI] [PubMed] [Google Scholar]
- 17.Wehren LE, Hawkes WG, Orwig D, et al. Gender differences in mortality after hip fracture: the role of infection. J Bone Miner Res. 2003;18:2231–2237. doi: 10.1359/jbmr.2003.18.12.2231. [DOI] [PubMed] [Google Scholar]
- 18.D'Adamo CR, Hawkes WG, Miller RR, et al. Short-term changes in body composition after surgical repair of hip fracture. Age Ageing. 2014;43:275–280. doi: 10.1093/ageing/aft198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Magaziner J, Wehren L, Hawkes WG, et al. Women with hip fracture have a greater rate of decline in bone mineral density than expected: another significant consequence of a common geriatric problem. Osteoporos Int. 2006;17:971–977. doi: 10.1007/s00198-006-0092-3. [DOI] [PubMed] [Google Scholar]
- 20.Fox KM, Magaziner J, Hawkes WG, et al. Loss of bone density and lean body mass after hip fracture. Osteoporos Int. 2000;11:31–35. doi: 10.1007/s001980050003. [DOI] [PubMed] [Google Scholar]
- 21.Chiles N, Alley D, Hawkes W, Orwig D. Sarcopenia and functional recovery after a hip fracture. Gerontologist. 2011;54:343. [Google Scholar]
- 22.Miller RR, Cappola AR, Shardell MD, et al. Persistent changes in interleukin-6 and lower extremity function following hip fracture. J Gerontol A Biol Sci Med Sci. 2006;61:1053–1058. doi: 10.1093/gerona/61.10.1053. [DOI] [PubMed] [Google Scholar]
- 23.Miller RR, Shardell MD, Hicks GE, et al. Association between interleukin-6 and lower extremity function after hip fracture - the role of muscle mass and strength. J Am Geriatr Soc. 2008;56:1050–1056. doi: 10.1111/j.1532-5415.2008.01708.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gruber-Baldini AL, Zimmerman S, Morrison RS, et al. Cognitive impairment in hip fracture patients: timing of detection and longitudinal follow-up. J Am Geriatr Soc. 2003;51:1227–1236. doi: 10.1046/j.1532-5415.2003.51406.x. [DOI] [PubMed] [Google Scholar]
- 25.Dolan MM, Hawkes WG, Zimmerman SI, et al. Delirium on hospital admission in aged hip fracture patients: prediction of mortality and 2-year functional outcomes. J Gerontol A Biol Sci Med Sci. 2000;55:M527–M534. doi: 10.1093/gerona/55.9.m527. [DOI] [PubMed] [Google Scholar]
- 26.Zimmerman SI, Smith HD, Gruber-Baldini A, et al. Short-term persistent depression following hip fracture: a risk factor and target to increase resilience in elderly people. Soc Work Res. 1999;23:187–196. [Google Scholar]