Abstract
We estimate the effect of job loss on objective measures of physiological dysregulation using biomarker measures collected by the Health and Retirement Study in 2006 and 2008 and longitudinal self-reports of work status. We distinguishing between mass or individual layoffs, and business closures. Workers who are laid off from their job have lower biomarker measures of health, whereas workers laid off in the context of a business closure do not. Estimates matching respondents wave-by-wave on self-reported health conditions and subjective job loss expectations prior to job loss, suggest strong effects of layoffs on biomarkers, in particular for glycosylated hemoglobin (HbA1c). A Layoff could increase annual mortality rates by 10.3%, consistent with other evidence of the effect of mass layoffs on mortality.
Keywords: Job loss, Health, SES-health gradient, Biomarkers
1 Introduction
The positive relationship between socio-economic status and health (the SES-health gradient) becomes stronger over the working years (Smith, 1999) possibly because of shocks to health or SES: health shocks may lead to prolonged absence from the labor force, as well as reduced earnings and wealth. Similarly job loss may lead to worse health because of physiological stress and financial strain. Further, job loss could make it hard to access health care because of the loss of employer-provided health insurance. Thus economic and health instabilities may be powerful drivers of the strengthening of the SES-health gradient over the working years.
Job loss is typically associated with significant financial consequences (Moen, 1983), which can result in stress (Voydanoff, 1984). Several studies have found that job loss is followed by poorer health outcomes (Montgomery, Cook, Bartley and Wadsworth, 1999). Studies in countries with generous unemployment insurance tend to find smaller effects on health (Black, Devereux, and Salvanes, 2012) lending support to a causative effect of unemployment on health. Rege, Telle and Votruba (2009) find strong effects of plant downsizing on disability pension utilization in Norway.
There are two concerns with inferring causality about the relationship between health and job loss from this evidence. First, omitted unobserved variables which are related to job loss and health (confounders) may bias causal inference. An example would be SES and health earlier in life. Second, health status itself may lead to job loss, leading to so-called reverse causality. For example, employers may lay off sicker workers since health is correlated with higher absenteeism and lower productivity. For this reason, some studies have focused on the long-term effects of job displacement on mortality and a range of other health-related outcomes using more exogenous sources of job loss such as business closures or mass layoffs.
Sullivan and von Wachter (2009) find that, 20 years after job displacement, displaced workers in Pennsylvania faced a 10–15% increase in mortality rates compared with other workers. Studies in Europe have also found effects on mortality. For instance, Eliason and Storrie (2009) found important effects in Sweden, in particular for males, while Browning and Heinesen (2012) find effects in Denmark for many causes of mortality including circulatory disease. Using survey data in the U.S., Strully (2009) used particular plant closures in manufacturing. Estimating from three waves of the Panel Study of Income Dynamics, she finds statistically significant effects of involuntary job loss (mostly business closure) on self-reported health and health conditions; however, the estimations include few health controls, leaving open the possibility that health declines led to job loss (reverse causality). Schroder (2013) found mixed negative long-term effects of layoffs and business closure on self-reported health outcomes at older ages for a number of European countries, with the largest effects occurring for females. But, using self-reported health measures such as being diagnosed by a doctor may underestimate the health effects of job loss because of an accompanying loss of health insurance may reduce the likelihood of being diagnosed. Some studies find no effect of job loss on health, in particular when looking at short-run effects of job displacement due to business closure on self-reported health (Salm, 2009) and hospital visits (Browning et al., 2006). Short-run effects, however, may not be evident in increased self-reported doctor diagnoses or hospital visits which would result from a longer build-up of poor health.
Long-run effects of job loss on health may become evident if better markers of health are used for detection. Theories based on biological processes suggest a link from economic instability to stress and health (McEwen and Stellar, 1993). These postulate that experiencing frequent or prolonged episodes of stress can lead to wear and tear on the body, disrupting regulatory systems and ultimately worsening health. These theories emphasize that the allostatic load or physiological dysregulation associated with stressful events leads to worse health outcomes in the long term. Several studies provide evidence of the mediating role of physiological dysregulation between stresses associated with low socioeconomic status, poor work conditions including job demands, and future mortality (Seeman, Burton et al. 1997; Merkin et al. 2008). While there are multiple approaches to measuring physiological dysregulation, one common method is to use the count of biomarker values that fall within ranges indicative of clinical risk.
In this paper, we investigate the relationship between job loss and physiological dysregulation, an objective measure of health. To do so, we exploit the rich longitudinal content of the Health and Retirement Study (HRS), along with biomarker and anthropometric measures collected in 2006 and 2008. Because of the longitudinal design, we are able to distinguish between layoffs and business closures. The distinction is potentially interesting because the psychological effects of a layoff, which singles out individual employees or a group of employees, may be stronger than when an entire firm closes for reasons which are perhaps outside the control of workers (or the firm). We follow individuals for periods ranging from 2 to 14 years, allowing us to assess medium-term effects on a wide range of objective health biomarkers. Because we have access to a rich set of controls, including measures of childhood as well as adult health and SES, as well as ex ante subjective expectations of job loss, we are able to assess the potential risk of bias associated with left-out variables. To guard against health inducing job loss (reverse causality), we use a matching estimator which matches, for each wave, displaced workers with non-displaced workers, based on an extensive set of covariates, including a number of pre-job-loss health measures. The aim is to compare health outcomes subsequent to job loss between workers whose health was similar prior to job loss. The matching estimator then pools these matches over waves, controlling extensively for baseline differences across respondents. This is akin to a very flexible difference-in-difference estimator.
In section 2, we present the data and the construction of the variables used. In Section 3, we present the methods used. In Section 4, we present our results. We offer conclusions and note limitations in section 5.
2 Data
2.1 Biomarkers and Anthropometrics in the HRS
The HRS is a biennial panel survey of U.S. adults at least 50 years of age. The HRS was launched in 1992,with an initial cohort whose individuals were approximately 51–61. In 1998 a new cohort, whose members were approximately 51–56, were added. Since then, every six years a new cohort aged 51–56 was added. In 2006, the HRS began collecting blood spots, saliva, and anthropometric measures as part of enhanced face-to-face interviews. Half the respondents were randomly selected for the enhanced interviews in 2006, and the remaining half were asked to participate in 2008. Three of the biomarkers require people to allow blood pressure to be taken and five are blood-based measures that were collected using dried blood spots. In 2006 about 9% of respondents did not consent to having the physical measurements taken, including blood pressure; about 17% did not participate in the blood spot collection. Altogether, HRS files have biomarkers for 13,064 respondents. Details on the protocols for collection and assay of the biomarker data are in the documentation on the HRS website (Crimmins et al., 2013).1
We use data from two cohorts in the HRS. First, we use the HRS cohort (born 1931–1941) with respondents who were 51 to 61 years old at first interview in 1992 and 65 to 77 years old in the year when their biomarkers were assessed (2006 or 2008). The second cohort of respondents (born 1942–1947) entered the HRS in 1998 at the age of 51–56 and were 59 to 66 years old in 2006 or 2008. In these two cohorts, 3,724 respondents have complete biomarker information, are not missing information on important covariates for regression analysis, and were between 59 and 77 years of age in 2006–2008. Because exposure to job loss requires respondents to be working at baseline, regression analysis below is performed on the sample of respondents who were working at the first wave in which they were observed (n = 2572). Another set of analyses is done using wave by wave matching techniques. The sample for this analysis is somewhat larger because we select respondents who are working at a given wave (n = 3580). For these respondents, we can observe 8 to 16 years of job history. Table A.1 in the appendix gives details on observations lost due to sample selection and missing covariates. We used sample weights in our analysis.
Our objective health measures includes six blood-based biomarkers: glycosylated hemoglobin (HbA1c), C-reactive protein (CRP), high-density lipoprotein (HDL), high and low total cholesterol, and Cystatin C. We also include measures of high and low diastolic blood pressure, high systolic blood pressure and pulse. From these measures we create a set of 10 high-risk indicators of physiological dysrgulation using the thresholds reported in Crimmins et al. (2010). These thresholds are largely based on clinical guidelines. Table 1 reports the list of indicators, the risk threshold indicators for each, and the fraction of respondents with levels at high risk.
Table 1.
Definition of High Risk Markers from Biomarkers and Anthropometric Measures
| Threshold | Fraction | N | |
|---|---|---|---|
| High HbA1c | >6.4% | 0.149 | 4602 |
| High C-reactive protein | >3 mg/L | 0.394 | 4471 |
| High Cystatin C | >1.55 mg/L | 0.058 | 4436 |
| High total cholesterol | >=240 mg/L | 0.207 | 4406 |
| High diastolic blood pressure | >90 mmHg | 0.192 | 4521 |
| High systolic blood pressure | >140 mmHg | 0.289 | 4521 |
| High pulse over 60 seconds | >90 | 0.057 | 4521 |
| Low HDL | <40 mg/L | 0.198 | 3854 |
| Low total cholesterol | <160 mg/L | 0.136 | 4406 |
| Low diastolic blood pressure | <60 mmHg | 0.024 | 4521 |
Sample weights used. The number of observations varies across variables because of missing values.
Nearly 15% of respondents have high HbA1c, a measure of average blood glucose level over the past few months. Values above the threshold are an indicator of diabetes. Close to 40% of respondents have elevated levels of C-reactive protein, a measure of general inflammation in the body that has been associated with elevated risk of diabetes, hypertension, and cardiovascular disease. A smaller fraction of the sample, 5.8%, has high Cystatin C, a measure of poor kidney function. Regarding cholesterol levels, 20.7% have high total cholesterol, and 19.8% have low HDL cholesterol both of which are risk factors for cardiovascular problems. 13.6% have low total cholesterol which is also a risk factor for heart disease. As for blood pressure, 19.2% have high diastolic blood pressure and 28.9% have high systolic blood pressure. Just 6% of respondents have elevated pulse.
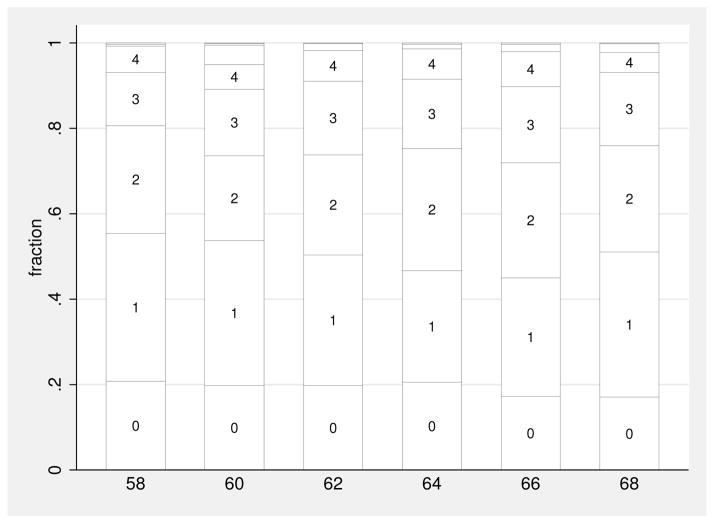
For each respondent, we sum the number of high-risk markers. This yields an objective measure of health that could range from 0 to 10 but in our sample ranges from zero to 8.2 Figure 1 shows the distribution of our measure for two-year age groups.
Figure 1. Distribution of the Count of High Risk Markers by Age.
Each bar gives the distribution of the number of high risk markers and sums to one within each 5-year age group. Sample weights used.
Fewer than one in five respondents (19.5%) have no high-risk markers, while one in four (24.4%) have more than 2 high-risk markers. We observe a general increase in the number of risk markers over 10 years. The HRS provides mortality tracking so we are able to compute mortality rates in the two years following biomarker collection. Conditional on age and basic socio-demographics (sex, education, race), those with no high-risk markers have a two-year mortality rate of 0.011, those with one have a 0.021 rate, those with two have a 0.030 rate, those with three have a 0.041 and those with four or more have a two-year mortality rate of 0.078. Those with four high-risk markers have two-year mortality rates 7.1 times as great as those with none, so these measures of health are important predictors of mortality.
2.2 Job Loss and Job Characteristics
The HRS collection information about each job termination and the reason for termination during the observation period. Respondents can report a job termination due to a layoff or they can report a job termination due to a business closure. We construct indicator variables for these two outcomes. Overall, 16.95% were laid off, while 9.8% lost their job because of business closure. Only 85 (2.61%) had both occur during the observation period, and few respondents were laid off twice or lost jobs because of multiple business closings during that period.
Because job loss varies by occupation and industry, we also construct two dummy variables, one indicating whether the longest-held job was in a manual occupation, and the other indicating whether it was in a primary, secondary, or tertiary industry (e.g., mining, manufacturing, or services, respectively).
2.3 Childhood, Family History, and Parent Characteristics
Because health differences may originate earlier in life, we construct variables for the childhood and family environment of each respondent. In addition to providing good controls for confounders in regression analysis, potential associations with health later in the life-cycle are also interesting. The HRS contains a battery of questions on the childhood environment. For more than half the respondents, the mother worked during childhood. In 71.2% of cases, at least one parent smoked when the respondent was a child. On average, respondents’ mothers had 10.3 years of education compared to 9.9 for fathers.
The HRS collects information on childhood health. For example, 80.6% considered their health as very good or excellent at age 16. Prior to age 16, respondents had an average of 1.41 infections (measles, mumps, or chicken pox) and an average of 0.35 out of the following 15 health conditions: vision problems, asthma, diabetes, respiratory problems, speech problems, allergy, heart trouble, ear problems, epilepsy, headache, stomach problems, high blood pressure, depression, drug problems, or some other psychological problem. We define indicator variables for those with missing information on these covariates and use them as controls in regression analyses.
We create variables which record the number of times the respondent was ever married, the number of children the respondent had, and the respondent’s age when the first child was born. On average, respondents had 1.41 marriages, with 2.50 children and an average age at first birth of 24.2.
2.4 Other Variables from the HRS Core
We construct a series of background characteristics from the Core Survey of the HRS. The average respondent is 64 years old, and 9.1% are black, 6.9% Hispanic, and 47% male. We recode the education variable in three groups (less than high school, high school, and college). We drop cases where observations of these variables are missing.
We construct a series of prevalence variables for diabetes, hypertension, heart disease, stroke, cancer, and lung disease. These are used as alternative-outcome variables in the analysis as well as controls to match respondents based on health prior to job loss. More than half the respondents report they have hypertension, 20.6% have heart disease, 13.5% cancer, 6.3% stroke, 18.6% diabetes, and 9.8% have lung disease. These controls are used in the econometric analysis to control for baseline health (prior to job loss exposure).
3 Methods
Our empirical strategy exploits the rich longitudinal information contained in the HRS. We proceed in two steps. The first step, exploits the variation in the occurrence of job loss between baseline and the time of measurement of biomarkers with biomarkers measured in 2006/2008, controlling for a rich set of covariates at baseline. Hence job loss occurs prior to the measurement of biomarkers. This strategy is prone to omitted variables bias to the extent that we have not controlled for other baseline characteristics not included in the HRS. We use the sensitivity of our estimates to changing the set of controls in order to assess the potential of this bias. This strategy, although informal, is akin to the strategy proposed by Altonji, Elder and Taber (2005). Another threat to the identification strategy is that health deteriorates prior to job loss and causes job loss. We test for this possibility by regressing future job loss, measured in 2008 (2010), on measurement of biomarkers in 2006 (2008), controlling for a large set of controls measured along with the biomarkers in 2006 (2008). If predictive of future job loss, this would be consistent with reverse causality. To account for reverse-causality, we match for each wave respondents who experienced job loss which a similar respondent from the same wave with similar characteristics, including health status prior to job loss as well as subjective job loss expectations. We then combine these matched pairs of respondents to obtain an estimate of the effect of job loss on health. This matching estimator, akin to a very flexible difference-in-difference estimator, relaxes many of the assumptions made with regression analysis, in particular the assumption that health did not change between baseline and the time when job loss occurred.
3.1 Controls for Baseline Characteristics
Denote by ni the count of risk markers for respondent i either in 2006 or 2008. Let zi be an indicator variable for the occurrence of either a layoff or business closure since the first interview (when respondents were working). Let xi be a vector of socio-economic characteristics at the time of interview and wi be a vector of childhood and life history variables. We postulate that ni conditional on (zi; xi; wi) has a Poisson distribution, with conditional expectation:
| (1) |
This strategy assumes that zi is independent of unobservables conditional on (xi; wi).
3.2 Reverse Causality: Is Health Predictive of Future Job Loss?
We use data on job loss subsequent to measurement of biomarkers to estimate a model predicting job loss based on poor health. Specifically, we estimate the following logit model:
| (2) |
where Λ() is the logistic distribution function. A test of reverse causality can be implemented by examining whether αh = 0. If we reject the null hypothesis, reverse causality may be a concern since we only control for baseline health and health may have deteriorated differentially since baseline until the occurrence of job loss.
3.3 Matching on Health Prior to Job Loss
We use a matching estimator that targets the period around the occurrence of job loss rather than the situation at baseline. For each job loss, we know the termination date of the job. Hence, we have information on the health status of the respondent from the interview prior to job loss. Let the vector of health status variables be hi. For each respondent with job loss in wave s and with characteristics qi;s = (hi;s−1; xi; wi) , we want to find a respondent with similar characteristics who did not experience job loss. To do that, we estimate for each wave s, a logit model predicting job loss in that wave as a function of qi;s among those working at the previous wave. Let ps(qi;s) be the predicted job loss probability of someone with characteristics qi;s. We use the nearest neighbor of each respondent based on this propensity score ps(qi;s). Let r(i; j) = 1 if observation j is the nearest neighbor of observation i and zero otherwise (j = minj |ps(qi;s) − ps(qj;s)|). Then the matching estimator of the effect of job loss on ni, matching exactly on the wave, is given by
| (3) |
where Nz is the number of respondents with a job loss. The estimate is the average difference in the number of high-risk biomarkers between workers with job loss and similar workers without job lost over wave s. Standard errors are computed using Abadie and Imbens (2006) and bias-correction is implemented following Imbens and Abadie (2011). Compared to the regression approach, the matching estimator has two distinctive features: a) it is more flexible that a regression based estimator b) it allows to control for pre job loss chacteristics.
4 Results
4.1 Health and Job Loss
In Table 2, we report differences in health by the type of job loss respondents experienced since the first interview. We do this for the count of risk markers (ni) as well as for each marker separately. We also report differences using self-reported health conditions in 2006/2008.
Table 2.
Differences in Health Outcomes by Incidence of Layoff and Business Closed Since the First Interview
| Ever had layoff | Ever had bus. closed | |||||
|---|---|---|---|---|---|---|
| No | Yes | T-test | No | Yes | T-test | |
| Count of risk markers | 1.597 | 1.807 | 3.062 | 1.615 | 1.785 | 1.940 |
| High HbA1c | 0.132 | 0.155 | 1.240 | 0.133 | 0.163 | 1.267 |
| High CRP | 0.364 | 0.420 | 2.125 | 0.367 | 0.436 | 2.059 |
| High Cystatin C | 0.045 | 0.045 | −0.028 | 0.045 | 0.042 | −0.181 |
| High total cholesterol | 0.207 | 0.233 | 1.181 | 0.211 | 0.209 | −0.082 |
| High diastolic BP | 0.198 | 0.203 | 0.220 | 0.198 | 0.205 | 0.249 |
| High systolic BP. | 0.287 | 0.293 | 0.277 | 0.284 | 0.323 | 1.251 |
| High pulse over 60 sec. | 0.048 | 0.088 | 3.307 | 0.053 | 0.070 | 1.087 |
| Low HDL | 0.189 | 0.207 | 0.838 | 0.191 | 0.196 | 0.170 |
| Low total cholesterol | 0.107 | 0.146 | 2.274 | 0.112 | 0.120 | 0.355 |
| Low diastolic BP | 0.021 | 0.017 | −0.496 | 0.021 | 0.021 | 0.023 |
| Diabetes | 0.176 | 0.167 | −0.431 | 0.175 | 0.173 | −0.078 |
| Hypertension | 0.520 | 0.564 | 1.640 | 0.522 | 0.572 | 1.432 |
| Heart disease | 0.186 | 0.171 | −0.693 | 0.181 | 0.210 | 1.069 |
| Stroke | 0.054 | 0.052 | −0.119 | 0.054 | 0.049 | −0.294 |
| Cancer | 0.122 | 0.151 | 1.607 | 0.127 | 0.122 | −0.203 |
| Lung disease | 0.082 | 0.098 | 1.104 | 0.082 | 0.110 | 1.462 |
| Died | 0.019 | 0.028 | 1.163 | 0.019 | 0.036 | 1.712 |
|
| ||||||
| Observations | 2174 | 444 | 2360 | 258 | ||
Sample weights used. The sample is restricted to respondents who are employed at the first observation CRP: C-reactive protein, BP: blood pressure, HDL: high-density lipoprotein. T statistics based on weighted regressions.
The count of high-risk markers is statistically significantly higher among those who experienced layoffs (diff=0.21, t = 3.02) but only statistically significant at the 10% level among those who experienced a business closure (diff = 0.17, t = 1.94). For layoffs, CRP and pulse are significantly higher, while there are no significant differences in self-reported conditions between those who experienced job loss and those who did not. Only self-reported hypertension is statistically significant at the 10% level. Those with layoffs did not experience a higher mortality in the subsequent two years. For those who experienced a business closure, only CRP was notably different from those who did not. This is also true for self-reported health conditions while mortality rates are slightly higher among those who experienced business closure and statistically significant at the 10% level.
4.2 Characteristics of Respondents with Job Loss
Differences reported in Table 2 are subject to important confounders which include general socio-economic status as well as initial (childhood) health differences. Those may differ importantly between those who suffered a job loss and those who did not. We report this analysis in Table 3.
Table 3.
Differences in Socio-Economic Characteristics by Incidence of Layoff and Business Closed Since First Interview
| Ever had layoff | Ever had business closed | |||||
|---|---|---|---|---|---|---|
| No | Yes | T-test | No | Yes | T-test | |
| Age | 63.81 | 64.45 | 3.975 | 63.84 | 64.57 | 3.679 |
| Male | 0.521 | 0.511 | −0.415 | 0.522 | 0.492 | −1.002 |
| High school | 0.606 | 0.550 | −2.389 | 0.592 | 0.657 | 2.194 |
| College | 0.291 | 0.294 | 0.110 | 0.303 | 0.180 | −4.469 |
| Black | 0.084 | 0.059 | −1.866 | 0.080 | 0.084 | 0.283 |
| Hispanic | 0.062 | 0.071 | 0.747 | 0.060 | 0.103 | 2.912 |
| Mother worked | 0.547 | 0.603 | 1.825 | 0.544 | 0.668 | 3.203 |
| # inf. in child | 1.401 | 1.301 | −1.561 | 1.387 | 1.375 | −0.152 |
| Child health v.good | 0.825 | 0.833 | 0.308 | 0.829 | 0.803 | −0.912 |
| # health cond. | 0.302 | 0.284 | −0.517 | 0.303 | 0.262 | −0.942 |
| 1+ parent smoke | 0.711 | 0.737 | 0.915 | 0.714 | 0.723 | 0.263 |
| # of marriage | 1.378 | 1.419 | 1.178 | 1.375 | 1.477 | 2.333 |
| # of children | 2.460 | 2.465 | 0.067 | 2.455 | 2.516 | 0.658 |
| Age first child | 24.67 | 24.75 | 0.31 | 24.78 | 23.73 | −3.41 |
| Mother education | 10.51 | 10.59 | 0.467 | 10.57 | 10.097 | −2.088 |
| Father education | 10.063 | 10.291 | 1.159 | 10.152 | 9.522 | −2.511 |
| Primary industry | 0.075 | 0.102 | 2.091 | 0.079 | 0.075 | −0.221 |
| Secondary industry | 0.304 | 0.339 | 1.536 | 0.300 | 0.401 | 3.494 |
| Tertiary industry | 0.621 | 0.558 | −2.614 | 0.620 | 0.523 | −3.190 |
| Manual occupation | 0.268 | 0.250 | −0.825 | 0.259 | 0.334 | 2.725 |
Sample weights used. The sample is restricted to respondents who are employed at the first observation. In the sample, when restricting to those with non-missing information, we have 2,572 observations with 434 layoff and 248 business closed
As may be expected, those who were laid off were older on average. They were also less likely to be black, and more likely to be in a secondary than a tertiary industry. Overall differences in characteristics, even where statistically significant, are not large for those with layoffs.
Differences for those who experienced a business closure are more pronounced. In particular, they are likely to be older, to be less educated, to be Hispanic, and to have had a working mother with less education. Most importantly, respondents who experienced a business closure are more likely to be in a manual occupation in the secondary sector of the economy. This could be explained by the fact that business closures have been more pronounced in this sector than in other sectors during the last 20 years.
4.3 Controls for Baseline Characteristics
We first consider models of the count of high-risk markers, controlling for baseline characteristics, using Poisson models. The Poisson specification imposes the strong assumption of equi-dispersion (variance equals mean). We tested for over-dispersion and could not reject the null hypothesis of equi-dispersion. Hence, we report Poisson estimates. The parameters reported are the average marginal effects. Table 4 reports the results of four specifications where we vary the set of explanatory variables.
Table 4.
Poisson Models of the Effect of Job Loss on Number of High Risk Biomarkers
| Variable | (1) | (2) | (3) | (4) |
|---|---|---|---|---|
| Ever had layoff | 0.216*** (0.0666) | 0.215*** (0.0667) | 0.231*** (0.0671) | 0.229*** (0.0671) |
| Ever had business closed | −0.0832 (0.0876) | −0.0843 (0.0876) | −0.0696 (0.0879) | −0.0699 (0.0879) |
| Age in years | −0.0158 (0.00996) | −0.0177* (0.0102) | −0.0200** (0.0101) | −0.0216** (0.0103) |
| Respondent is male | 0.207*** (0.0604) | 0.211*** (0.0619) | 0.185*** (0.0609) | 0.183*** (0.0624) |
| Black | 0.436*** (0.0733) | 0.423*** (0.0743) | 0.287*** (0.0784) | 0.279*** (0.0794) |
| Hispanic | 0.143 (0.0974) | 0.126 (0.0989) | 0.0378 (0.105) | 0.0245 (0.107) |
| High school | −0.222*** (0.0856) | −0.212** (0.0860) | −0.137 (0.0864) | −0.132 (0.0870) |
| College | −0.529*** (0.0980) | −0.512*** (0.101) | −0.365*** (0.105) | −0.357*** (0.108) |
| Manual occupation | 0.0165 (0.0750) | 0.0136 (0.0751) | 0.0207 (0.0756) | 0.0197 (0.0757) |
| Mother worked | 0.0403 (0.0533) | 0.0407 (0.0534) | ||
| 1+ parent smoke (miss=0) | 0.0269 (0.0446) | 0.0273 (0.0446) | ||
| Mother education | −0.000402 (0.0103) | −0.000275 (0.0103) | ||
| Father education | −0.0191** (0.00924) | −0.0191** (0.00925) | ||
| Number of marriages | −0.00982 (0.0353) | −0.00104 (0.0355) | ||
| Number of children | 0.0211 (0.0192) | 0.0175 (0.0192) | ||
| Age first child | 3.46e-06 (0.00596) | 0.00205 (0.00598) | ||
| Control health in childhood | no | no | yes | yes |
| Control health at the first obs | no | no | yes | yes |
| Control for indus. and occ. | yes | yes | yes | yes |
|
| ||||
| Observations | 2,572 | 2,572 | 2,572 | 2,572 |
The dependent variable is the count of high risk markers. Estimation is performed by maximum likelihood. Marginal effects on the count of high risk markers along with standard errors (in parenthesis) are reported.
p < 0.01,
p < 0.05,
p < 0.1.
The sample is restricted to respondents who are employed at the first observation. Dummy variables for missing information have been added for childhood variables, occupation and industry and age of the first child. The number of observations is voluntarily kept constant across columns
If we focus on layoffs and business closure, we see an unambiguous positive association between layoff and the count of high-risk biomarkers The effect is relatively large (in column 4, marginal effect (me) = 0.229, se = 0.067)– similar to that of male-female differences.
We detect a negative association between the incidence of business closure and the count of high-risk markers. The point estimates are relatively stable across specifications suggesting that the effects are not particularly sensitive to these controls. Of the covariates, some current health condition prevalences and the number of one’s children have an association with the count of high-risk markers. Father’s education appears to be associated with a reduced number of high-risk markers. The largest differences are found between college and high school dropouts (for example, in column 4, me = 0.357, se = 0.108). These large differences in terms of education highlight the importance of socio-economic status as a determinant of health differences.
The marginal effect for both layoffs and business closure are highly stable across specifications. Nevertheless, there is the potential for other omitted variables to bias estimates. In Table 5 (column 1), we repeat the specification in column 4 of Table 4 but add current household income and net wealth (column 2). Of course, this is likely to lead to over-controlling, given that layoffs and business closure may have an effect on health through income and wealth. Yet adding these controls does not much change the observed effects of layoff and business closure. Both household income and wealth have small effects in this model, with those for income being statistically insignificant as well. This finding supports the view that the differences in effects of layoffs and business closure on health are not purely driven by differences in socio-economic status.
Table 5.
Alternative Poisson Models of the Effect of Job Loss on Health Outcomes
| Variables | (1) | (2) | (3) |
|---|---|---|---|
| Ever had layoff | 0.229*** (0.0671) | 0.215*** (0.0672) | 0.0957* (0.0521) |
| Ever had business closed | −0.0699 (0.0879) | −0.0873 (0.0880) | −0.0247 (0.0657) |
| Household income in 1000$ | −0.000261 (0.000587) | −0.000746 (0.000463) | |
| Household net wealth in 1000$ | −0.000518*** (9.90e-05) | −0.000181** (7.54e-05) | |
|
| |||
| Observations | 2,572 | 2,572 | 3,230 |
The dependent variable is the count of risk markers for the first two specifications and the count of self-reported health conditions for the last one. The sample is restricted to respondents who are employed at the first observation. Estimation by maximum likelihood. Marginal effects along with standard errors (in parenthesis).
p < 0.01,
p < 0.05,
p < 0.1.
Same controls as in the last column of Table 4 are included in all specifications.
In the last column, we estimate a Poisson model where the dependent variable is the count of self-reported health conditions in 2006/2008. Here, the effect of layoffs on health is substantially attenuated and statistically significant only at the 10% level (me = 0.0957). Below, we investigate whether health care use increases following job loss.
We also tested whether effects vary by the time since the layoff or business closure occurred. Allowing for wave-specific effects, we cannot reject the null hypothesis that effects are constant with exposure. This suggests that effects are long-lasting (p-value = 0.4853 for layoffs and p-value = 0.7956 for business closures). 3
A good comparison for assessing the magnitude of the effect found is to look at the induced effect on mortality. Because our sample of workers experiencing layoffs is already small and an even smaller group dies within 2 years after biomarker collection, it is not possible to detect direct effects of layoffs on mortality. We can, however, compute the effect of a layoff on the count of biomarkers and then use a mortality regression on age, socio-economic characteristics, and the count of high-risk markers to get an idea of the magnitudes. When we do this, we find that a layoff increases annual mortality risk by 10.3% (Table A.3 in the appendix provides details on how this number is obtained). This effect is large but in line with results reported by Sullivan and von Wachter (2009), who found job displacement to increase annual mortality risk by 10–15%.
4.4 Reverse Causality: Is Health Predictive of Future Job Loss?
One potential bias in our multivariate regressions is reverse causality. Health events may trigger job loss and be correlated with future health. In regression analysis, we controlled for baseline health but this may not be sufficient. To test for this possibility, we estimate a logit model for the probability of losing a job in 2008/2010 for respondents who were employed at the time of biomarker record collection. For example, we find whether someone who was employed in 2006, and had biomarkers measured in that year, is more likely to have experienced a job loss at the next wave (2008) if he had a higher number of high risk markers in 2006. We do the same for those for whom we measured biomarkers in 2008, looking at job loss in 2010. We control for the same controls as in Table 4 and add controls for health in 2006/2008. In Table 6, we report marginal effects for different health variables.
Table 6.
Assessment of Reverse Causality
| Model | Layoff | Business closure |
|---|---|---|
| Count of risk markers | −0.01055* (0.0056) | 0.00083 (0.0030) |
| More than two risk markers | −0.02625** (0.0131) | −0.00940 (0.0088) |
| Count of health conditions | −0.00740 (0.0055) | 0.00202 (0.0034) |
| More than one health condition | −0.01843 (0.0126) | 0.00471 (0.0080) |
Estimates by maximum likelihood of the effect of each health measure on the probability of a layoff or business closure at the following interview. Marginal effects along with standard errors (in parenthesis).
p < 0.01,
p < 0.05,
p < 0.1.
Separate logit regressions have been performed for each job lost type and for each variables of health. The health variable is the count of the following health problems: diabetes, hypertension, heart disease, stroke, cancer, lung disease. The sample is restricted to respondents who are employed at the first observation (1537 obs). 6.1% of these observations experienced a layoff and 2.3% experienced a business closure. Controls are the same as in the main specification in column 4 of Table 4.
When using the count of risk markers, we find evidence that health does influence layoffs but with an unexpected sign. Specifically, we find those with a higher count of risk markers were less likely to subsequently experience a layoff (marginal effect (me) = −0.01055, statistically significant at 10% level). However, we find no evidence regarding reverse causality for business-closure job loss, that is, we do not find that health conditions predict such job losses.
4.5 Matching on Health Prior to Job Loss
Because there is some (albeit negative) evidence of reverse causality for layoffs, we adopt the matching estimator suggested earlier to control for health prior to job loss. The quality of the match can be assessed using estimates of the matching standard bias, which is a measure of how different means of the different variables used to match are different in the treatment and matched-control samples. Table A.4 in the appendix reports estimates of match standard bias. Unmatched differences are large for a number of variables, often exceeding 10 percent. The matched-control means are much closer and larger deviations exist only for a handful of covariates (occupation and industry). Overall, the matched control sample appears to be very similar to the sample of those with job loss. Table 7 reports matching estimates of the effect of job loss on health.
Table 7.
Matching Estimates of the Effect of Job Loss on Health Outcomes
| Layoff | Business closure | |
|---|---|---|
| Count of risk markers | 0.3462*** (0.0955) | 0.0809 (0.1194) |
| By markers | ||
| High HbA1c | 0.0562** (0.0248) | 0.0146 (0.0279) |
| High C-reactive protein | 0.0124 (0.0352) | −0.0137 (0.0405) |
| High Cystatin C | 0.0088 (0.0141) | 0.0235 (0.0182) |
| High total cholesterol | 0.0600** (0.0296) | 0.0343 (0.0344) |
| High diastolic blood pressure | 0.0458* (0.0276) | 0.0098 (0.0317) |
| High systolic blood pressure | 0.0163 (0.0342) | 0.0299 (0.0368) |
| High pulse over 60 seconds | 0.0236 (0.0182) | 0.0318* (0.0187) |
| Low HDL | 0.0747** (0.0293) | −0.0691** (0.0334) |
| Low total cholesterol | 0.0360 (0.0240) | 0.0225 (0.0283) |
| Low diastolic blood pressure | 0.0125 (0.0097) | 0.0080 (0.0135) |
| Count of health condition | 0.1026* (0.0573) | −0.0078 (0.0747) |
| More than one health condition | 0.0028 (0.0042) | −0.0054 (0.0062) |
|
| ||
| Observation (control + treated) | 798 | 492 |
Estimation using the nearest-neighbor matching estimator (NNM) with one neighbour by treated observation. The average of the difference between the observed and matched observation along with standard errors ( in parenthesis) is reported.
p < 0.01,
p < 0.05,
p < 0.1.
The match is done exactly by wave, and by the nearest-neighbor on a propensity score. The propensity score is obtained using a logit regression with the same set of variables as those used in Table 4 and in which we add variable health condition. Finally we add the health variables directly to the NNM matching set to obtain a better match on these variables. The sample is restricted to respondents who are employed at the current wave.
After controlling for prior health, the effect of layoff on the count of risk markers remains and is even stronger than suggested by Poisson models (point estimate (pe) = 0.3462, standard error (se) = 0.0955). The effect for business-closure termination remains statistically insignificant and much smaller in magnitude. Turning to individual markers, three key markers are statistically significant: HbA1c, total cholesterol, and low HDL. Effects of business closure remain small and statistically insignificant in the model for Table 7. Across all our different specifications, we could not detect any evidence of a positive relationship between business-closure job loss and subsequent biomarker measurements.
4.6 Adding Job Loss Expectations
One concern with these estimates is that some workers may anticipate layoffs (in particular mass layoffs) and leave their jobs prior to the events. This could bias results depending on who leaves or changes employment. Fortunately, the HRS collects information on job-loss expectations. Each worker is asked for the probability that he may lose his job in the near future. To assess the effect of expectations on our estimates, we repeat the matching exercise, adding job-loss expectations in the wave prior to the layoff to our control variables. Although the samples are not exactly identical because the question was not asked in some waves, we find evidence that the results are virtually unchanged once we add expectations to our control variables. 4
4.7 Health Care Use
We investigate whether those with a layoff or business closure use more health care. To do so, we consider the number of doctor visits and hospital nights as well as medication use for respondents in 2006/2008. We use the matching estimator developed earlier to look at the effect of job loss. Results are reported in Table 8. Overall, there is little effect of job loss on health-care use. Despite being sicker, according to biomarkers, respondents do not use more health care following job loss. This is consistent with under diagnosis and results reported earlier that the relationship between job loss and reports of diagnosed conditions is weaker.
Table 8.
Matching Estimates of the Effect of Job Loss on Health Care Use
| Layoff | Bussiness closure | |
|---|---|---|
| Regulary take drugs | 0.0175 (0.0222) | −0.0127 (0.0298) |
| Doctors visits | 1.0482 (0.6546) | 0.6272 (0.7349) |
| 6+ Doctors visits | 0.0114 (0.0324) | 0.0335 (0.0390) |
| Num. night hosp | 0.4506 (0.3545) | 1.1279 (0.9206) |
| 1+ night hosp | 0.0368 (0.0255) | 0.0022 (0.0340) |
|
| ||
| Observation (control + treated) | 1000 | 636 |
p < 0.01,
p < 0.05,
p < 0.1.
Estimation using the nearest-neighbor matching estimator (NNM) with one neighbour by treated observation. The average of the difference between the observed and matched observation along with standard errors ( in parenthesis) is reported.
The match is done exactly by wave, and by the nearest-neighbor on a propensity score. The propensity score is obtained using a logit regression with the same set of variables as those used in Table 4 and in which we add variable health condition. Finally we add the health variables directly to the NNM matching set to obtain a better match on these variables. The sample is restricted to respondents who are employed at the current wave.
4.8 Retirement and Job Loss
Because our sample covers the period around which respondents retire, it is possible that some of the effects we estimated are mediated by workers deciding to retire upon losing their jobs. The health effects could be lower in this case for two reasons: a) retirement benefits may cushion the drop in income due to job loss, b) those workers were perhaps already thinking of retirement before they lost their jobs and therefore stress associated with losing a job (and finding another one) may be lower. To explore this issue, we make use of subjective work expectations. At baseline, workers were asked about the likelihood of working past age 62 and 65 years old. We create an indicator variable denoting high expectations of working past a certain age using the median as a cutoff for each subjective expectation question. Hence, the group with subjective expectations above the median is a group who planned to work longer than the other group. We re-estimated the specification from column 4 of Table 4 allowing for the effect of layoffs and business closure to differ across the two groups. Table 9 reports results both for subjective expectations of working past 62 and past 65. Interestingly, the effect of a layoff are largest for those who planned to work longer but experienced a layoff. This is true for both expectation to work at age 62 and 65 although the effect is particularly strong for those who reported that the probability they would work past 62 was more than 50%. The effect of a business closure does not appear to depend on whether or not workers had a strong attachment to the labor force.
Table 9.
Poisson Regression Results - Effect of Job Loss Varying According to Work Expectations
| Direct Control | Interaction Age 65 | Interaction Age 62 | |
|---|---|---|---|
| Probability work after 62 P(62) | 0.00117 (0.00101) | ||
| Probability work after 65 P(65) | 0.000392 (0.00118) | ||
| Ever had layoff | 0.232*** (0.0672) | ||
| Ever had business closed | −0.0776 (0.0879) | ||
| Layoff - P(65) > 10% | 0.302*** (0.0962) | ||
| Layoff - P(65) <= 10% | 0.173** (0.0867) | ||
| Business closed - P(65) > 10% | 0.0253 (0.125) | ||
| Business closed - P(65) <= 10% | −0.168 (0.120) | ||
| Layoff - P(62) >= 50% | 0.408*** (0.103) | ||
| Layoff - P(62) < 50% | 0.136 (0.0827) | ||
| Business closed - P(62) >= 50% | 0.128 (0.141) | ||
| Business closed - P(62) < 50% | −0.172 (0.110) | ||
| Observations | 2,572 | 2,572 | 2,572 |
Estimation by maximum likelihood. The dependent variable is the count of high risk markers.
The first column reports results from the specification in the last column of Table 4 to which we have added expectation variables as controls. The second column allows for a different effect of job loss on the count of high risk markers depending on whether the respondent had at baseline expectations to work past age 65 above the median. The third column implements the same for expectations to work beyond age 62. Point estimates along with standard errors (in parenthesis). Overall, we use the same controls as in the last column of Table 4 *denotes p<0.1, **, p<0.05, ***, p<0.01.
5 Discussion
The strengthening of the poor health and low SES relationship during working life is likely the result of health and SES shocks. A key SES shock that may occur over someone’s life is job loss, either through a layoff or a business closure. In this paper, we investigate this relationship using biomarker data on a sample of respondents aged 59–70 for whom we have detailed job history going back 8 to 16 years.
Our results are fivefold. First, we find no relationship between business closures and health, whether measured using biomarkers or self-reported conditions. This finding is robust to varying sets of controls and tests for reverse causality. Second, we find a robust effect of layoffs on health, measured using biomarkers. Third, although there is weak evidence of reverse causality (poor health may cause layoffs), matching estimates, which account for self-reported health prior to job loss and allows to control for other observable differences in a flexible way, corroborate estimates from Poisson regressions and show an even larger effect. One potential mechanism that could explain the difference between layoffs and business closures is that psychological stress, or loss of confidence, is larger for those singled out by a firm to be laid off rather than because of a business closure which is likely due to reasons outside a worker’s control. Finally, the effect of a layoff is stronger for those who expected to remain in the labor market longer suggesting that layoffs that disrupt career plans (and therefore the timing of retirement) may have stronger effects on health. Because of sample size, we are not able to detect effects on mortality. However, using our estimates and the estimated effect of our health measures on mortality, we find that our estimates could explain a 10.3% increase in annual mortality rates in the long run. This compares well, for example, to estimates obtained by Sullivan and von Wachter (2009).
Our analysis has a number of limitations. First, sample size and the low frequency of both job loss and some risk markers may imply that our study is underpowered. Second, our measure of job loss is self-reported, so it may be measured with error. Third, each respondent’s biomarkers are measured just once. In particular, it was not possible to obtain measures of biomarkers prior to job loss. Our sampling frame and the quality of retrospective data implied that we could not investigate job loss prior to the first interview, leading us to focus on job loss after the age of 50. Hence, results are not necessarily generalizable to the entire working life. Finally, although a two-year look back period for health status prior to job loss allows us to control for reverse causality, there remains the potential for health shocks to cause job loss within this two year period. However, the fact that the matching estimates, which, among other things, better control for health before job loss than regression estimates using controls for baseline health, are in fact larger than regression estimates, makes us think that this issue is unlikely to be a major concern.
Despite these limitations, our results suggest that layoffs and business closure have truly distinct effects on health. One conjecture for the cause of this is that layoffs are often more personal and as a result may give rise to more-negative worker self-perceptions of their abilities, as well as to greater social stigma, either of which might lead to worse health outcomes, in particular when they disrupt plans to work at older ages.
Appendix
Table A.1.
Summary of Sample selection
| Observations | |
|---|---|
| Had bio-markers information in 2006/2008 | 13064 |
| Cohort HRS | 6507 |
| Cohort Warbabies | 1668 |
| Total HRS-Warbabies | 8175 |
| Age: 59–70 in 2006/2008 | 4747 |
| Had information on all bio-makers | 3724 |
| Complete record, working at current wave | 3580 |
| Complete record, working at initial wave | 2572 |
Table A.2.
Percent Distribution of the Count of High Risk Markers by Age
| Count of risk markers | Age 58 | Age 60 | Age 62 | Age 64 | Age 66 | Age 68 |
|---|---|---|---|---|---|---|
| 0 | 20.77 | 19.80 | 19.76 | 20.54 | 17.24 | 17.05 |
| 1 | 34.63 | 33.91 | 30.62 | 26.14 | 27.77 | 33.97 |
| 2 | 25.23 | 19.86 | 23.43 | 28.61 | 26.92 | 24.97 |
| 3 | 12.49 | 15.58 | 17.23 | 16.21 | 17.81 | 17.16 |
| 4 | 6.11 | 5.79 | 7.18 | 7.10 | 8.22 | 4.53 |
| 5 | 0.47 | 4.56 | 1.62 | 1.10 | 1.63 | 2.13 |
| 6 | 0.30 | 0.33 | 0.17 | 0.31 | 0.41 | 0.20 |
| 7 | 0.00 | 0.17 | 0.00 | 0.00 | 0.00 | 0.00 |
Sample weights used. Data used in constructing Figure 1.
Table A.3.
Effect of the Count of High Risk Markers on Mortality
| Baseline mortality risk | 0.0326 |
| Effect of one risk marker | 0.00338 ** (0.00157) |
| Observations | 5261 |
| Relative Change | 0.103 |
We perform a linear regression of mortality on the count of high risk markers, socio-demographic characteristics and doctor diagnosed health conditions. The sample slightly differs from our main sample as we do not condition on having job loss information which yields 5261 observations.
Table A.4.
Standard Bias Estimates from Matching
| Layoff | Business closed | |||
|---|---|---|---|---|
| Not Matched | Matched | Not matched | Matched | |
| Heart disease | 5.52% | 0.00% | 0.53% | 0.00% |
| Diabetes | 0.56% | 0.00% | 18.15% | 0.00% |
| Stroke | −3.00% | 0.00% | 2.38% | 0.00% |
| Hypertension | −2.02% | −1.06% | 9.27% | 0.00% |
| Cancer | −0.29% | 0.00% | 3.41% | 0.00% |
| Lung disease | −7.78% | −1.26% | −7.81% | 0.00% |
| Age | 10.25% | 2.72% | 6.80% | −1.67% |
| Male | 1.97% | 5.04% | 15.56% | 0.00% |
| Less than high school | −11.17% | 2.52% | −17.33% | −0.99% |
| High school | 0.59% | −6.63% | −9.55% | −3.39% |
| College | 9.42% | 5.52% | 29.02% | 5.77% |
| Black | 7.03% | 0.00% | 2.44% | −5.11% |
| Hispanic | −5.54% | 4.15% | −12.67% | −7.92% |
| Mother worked | −10.46% | −7.14% | −8.37% | 0.00% |
| # inf. in child | 2.99% | 3.26% | −5.05% | 11.83% |
| # health cond. | −5.13% | 2.60% | −2.67% | 3.73% |
| 1+ parent smoke | −7.78% | 1.01% | −8.89% | 8.15% |
| Child health v.good | −4.01% | −4.52% | 1.46% | −6.49% |
| Child info. Missing | 1.85% | 3.14% | 5.65% | −4.35% |
| Mother education | 6.37% | −4.72% | 28.29% | 4.58% |
| Father education | 3.98% | −8.08% | 19.52% | 5.67% |
| # of marriage | −10.40% | −1.78% | −6.31% | 18.35% |
| # of children | −8.38% | 4.38% | −8.29% | −9.39% |
| Age first child | −1.06% | −3.20% | 21.58% | 6.77% |
| Manual occupation | −7.84% | −5.57% | −16.50% | −0.86% |
| Occupation missing | −11.60% | −2.24% | −6.40% | −2.01% |
| Primary industry | −17.34% | 8.89% | 3.59% | 8.75% |
| Secondary industry | −13.56% | −6.94% | −24.26% | −4.18% |
| Tertiary industry | 24.98% | −0.50% | 20.68% | −1.62% |
| Industry missing | −14.94% | −6.20% | −5.37% | 0.00% |
|
| ||||
| Observations | 798 | 492 | ||
We compare a standardized difference in means before and after matching where
Footnotes
This research was supported by the National Institute on Aging, under grant R01AG040176. We thank David Boisclair, Nancy Campbell, Francois Laliberte-Auger and Clifford Grammich for excellent research assistance. We thank Fabian Lange, Italo Guttierez and seminar participants at McGill University and 2015 SOLE meetings in Montreal. Errors are our own.
JEL Codes: I14, J10, J14.
The blood collection was not designated for individual markers, and the respondents did not know what markers would be assayed and could not choose not to have some assays. The response rate to the invitation for the blood spot procedure was 83% (Sakshaug, Cooper and Ofstedal , 2010). Selection into the sample based on health has the potential to bias the results because those whose health was most affected by unemployment would not be in our analyses. However Sakshaug, Cooper and Ofstedal (2010) found little relationship between willingness to particulate and health or health conditions: “There were no statistically significant associations between consent and self-reported health status, BMI, Medicare status, pain limitations, or ever having had high blood pressure, cancer, lung disease, heart condition, stroke, or arthritis.” Diabetes was significantly different among those who participated and those who did not; but it increased the likelihood of consenting. We conclude that with respect to the our objectives the assumption of missingness at random is consistent with the available data analyses.
The literature on biological risk in older populations regularly uses count variables as summary indicators of physiological status in older populations (Seeman et al. 1997). A number of researchers have investigated approaches which provide different weights for the indicators such as Z-scoring, canonical correlations, recursive partitioning, k-means cluster analysis, genetic programming based symbolic regression algorithms and grade of membership methods (Juster et al., 2010). The comparison of different composite measures with the initial count measure has indicated little advantage in predictive ability of the measures but extreme complexity and variability in the weighting approaches for different outcomes and in different samples (Seeman et al., 2001). The current literature relies almost exclusively on count variables to reflect biological risk.
Results available upon request.
Results available upon request.
References
- Abadie A, Imbens GW. Large Sample Properties of Matching Estimators for Average Treatment Effects. Econometrica. 2006;74( 1):235–67. [Google Scholar]
- Altonji JG, Elder TE, Taber CR. Selection on Observed and Unobserved Variables: Assessing the Effectiveness of Catholic Schools. Journal of Political Economy. 2005;113(1):151–184. [Google Scholar]
- Black SE, Deveneux PJ, Salvanes KG. National Bureau of Economic Research Working Paper No. w18660. 2012. Losing Heart? The Effect of Job Displacement on Health. [Google Scholar]
- Blake T. Economic Context and the Health Effects of Unemployment. Journal of Health and Social Behavior. 1995;36(3):213–230. [PubMed] [Google Scholar]
- Browning M, Moller Dano A, Heinesen E. Job Displacement and Stress-related Health Outcomes. Health Economics. 2006;15(10):1061–1075. doi: 10.1002/hec.1101. [DOI] [PubMed] [Google Scholar]
- Browning M, Heinesen E. Effect of Job Loss Due to Plant Closure on Mortality and Hospitalization. Journal of Health Economics. 2012;31(4):599–616. doi: 10.1016/j.jhealeco.2012.03.001. [DOI] [PubMed] [Google Scholar]
- Crimmins E, Kim JK, Vasunilashorn S. Biodemography: New Approaches to Understanding Trends and Differences in Population Health and Mortality. Demography. 2010;47(Suppl):S41–64. doi: 10.1353/dem.2010.0005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crimmins E, Faul J, Kim JK, et al. Documentation of Biomarkers in the 2006 and 2008: Health and Retirement Study. Survey Research Center, University of Michigan; Ann Arbor, MI: 2013. [Google Scholar]
- Eliason M, Storrie D. Does Job Loss Shorten Life? Journal of Human Resources. 2009;44(2):277–302. [Google Scholar]
- Seeman TE, McEwen BS, Rowe JW, Singer BH. Allostatic load as a marker of cumulative biological risk: MacArthur studies of successful aging. Proceedings of the National Academy of Sciences of the United States of America. 2001;98(8):4770–4775. doi: 10.1073/pnas.081072698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Imbens G, Abadie A. Bias-Corrected Matching Estimators for Average Treatment Effects. Journal of Business and Economic Statistics. 2011;29(1):1–11. [Google Scholar]
- Juster RP, McEwen BS, Lupien SJ. Allostatic Load Biomarkers of Chronic Stress and Impact on Health and Cognition. Neuroscience Biobehavioral Review. 2010;35(1):2–16. doi: 10.1016/j.neubiorev.2009.10.002. [DOI] [PubMed] [Google Scholar]
- McEwen BS, Stellar E. Stress and the Individual Mechanisms Leading to Disease. Archives of Internal Medicine. 1993;153(18):2093–2101. [PubMed] [Google Scholar]
- Moen P. Unemployment, Public Policy, and Families: Forecasts for the 1980s. Journal of Marriage and the Family. 1983;45(75):1–60. [Google Scholar]
- Montgomery SM, Cook DG, Bartley MJ, Wadsworth ME. Unemployment Pre-dates Symptoms of Depression and Anxiety Resulting in Medical Consultation in Young Men. International Journal of Epidemiology. 1999;28(1):95–100. doi: 10.1093/ije/28.1.95. [DOI] [PubMed] [Google Scholar]
- Rege M, Telle K, Votruba M. The Effect of Plant Downsizing on Disability Pension Utilization. Journal of the European Economic Association. 2009;7(4):754–785. [Google Scholar]
- Salm M. Does Job Loss Cause Ill Health. Health Economics. 2009;18:1075–1089. doi: 10.1002/hec.1537. [DOI] [PubMed] [Google Scholar]
- Sakshaug JW, Couper MP, Ofstedal MB. Characteristics of Physical Measurement Consent in a Population-Based Survey of Older Adults. Medical Care. 2010;48(1):64–71. doi: 10.1097/mlr.0b013e3181adcbd3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schroder M. Jobless Now, Sick Later? Investigating the Long-term Consequences of Involuntary Job Loss on Health. Advances in Life Course Research. 2013;18(1):5–15. doi: 10.1016/j.alcr.2012.08.001. [DOI] [PubMed] [Google Scholar]
- Seeman TE, Burton SH, Rowe JW, Horwitz RI, McEwen BS. Price of Adaptation - Allostatic Load and Its Health Consequences: MacArthur Studies of Successful Aging. Archives of Internal Medicine. 1997;157(19):2259–2268. [PubMed] [Google Scholar]
- Seeman TE, Merkin SS, et al. Education, Income and Ethnic Differences in Cumulative Biological Risk Profiles in a National Sample of US adults: NHANES III (1988–1994) Social Science & Medicine. 2008;66:72–87. doi: 10.1016/j.socscimed.2007.08.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith J. Healthy Bodies and Thick Wallets: The Dual Relation Between Health and Wealth. Journal of Economic Perspectives. 1999;13(2):144–166. [PMC free article] [PubMed] [Google Scholar]
- Strully KW. Job Loss and Health in the U.S. Labor Market. Demography. 2009;46(2):221–246. doi: 10.1353/dem.0.0050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sullivan D, von Wachter T. Job Displacement and Mortality: An Analysis Using Administrative Data. The Quarterly Journal of Economics. 2009;124(3):1265–1306. [Google Scholar]
- Voydanoff P. Economic Distress and Families: Policy Issues. Journal of Family Issues. 1984;5:273–288. [Google Scholar]