Abstract
The stability of the patellofemoral joint relies on the tenuous interplay of soft tissue and bony factors. Anatomic risk factors for instability include a shallow trochlea, an abnormally lateral tibial tubercle position, patella alta, hypermobility, or a secondary injury to the medial patellofemoral ligament (MPFL). There is an increasing interest in restoring normal anatomy to achieve stability, and at times more than 1 abnormality exists. This article describes the technique for combining a tibial tuberosity transfer and an MPFL reconstruction. The key features include planning of skin incisions to enable both operations to be undertaken, planning of the screw placement before osteotomy is performed and assessment of the joint through a superolateral portal to assess the need for MPFL reconstruction after tuberosity transfer.
The stability of the patellofemoral joint relies on the tenuous interplay of soft tissue and bony factors. The lateral vector on the patella ensures that if any one of the factors enabling stability is compromised then the joint may become unstable. These anatomic risk factors include a shallow trochlea, an abnormally lateral tibial tubercle position, patella alta, hypermobility, or a secondary injury to the medial patellofemoral ligament (MPFL).1 The MPFL fails at 49% strain, so when a patellar dislocation occurs the ligament is inevitably damaged and incompetent.2 The MPFL has the important function of guiding the patella into the trochlear groove through the first 30° of flexion.3 Although in the majority of cases the MPFL rupture is not the primary pathology, its injury will contribute to further lateral tracking and instability.1 The anatomy and insertion points of the MPFL have been described in detail and have been recently subject to a systematic review.4
Since Janssen's landmark paper, there has been a growing understanding of the different abnormalities that may cause instability and an increasing interest in addressing each of them.5 The objective of this anatomic approach is to restore normal anatomy to accomplish stability without magnifying the forces transmitted through the joint or reconstructed MPFL.
Procedures that may address anatomic abnormality include altering the insertion of the patellar tendon, creating a trochlear groove, reconstructing damaged soft tissue, or rotational osteotomies of the femur or tibia. Where abnormality on the tendon insertion or length exists (patella alta or an increased tibial tubercle–trochlear groove [TT-TG] distance) then a tuberosity transfer may restore a normal relationship between the trochlear groove and patella. An MPFL reconstruction may help guide the patella to engage with the trochlea appropriately.
There has been significant surgeon engagement with patellar instability therapies in recent years; the stabilization procedures already well established in Europe are now gaining popularity in North America.6
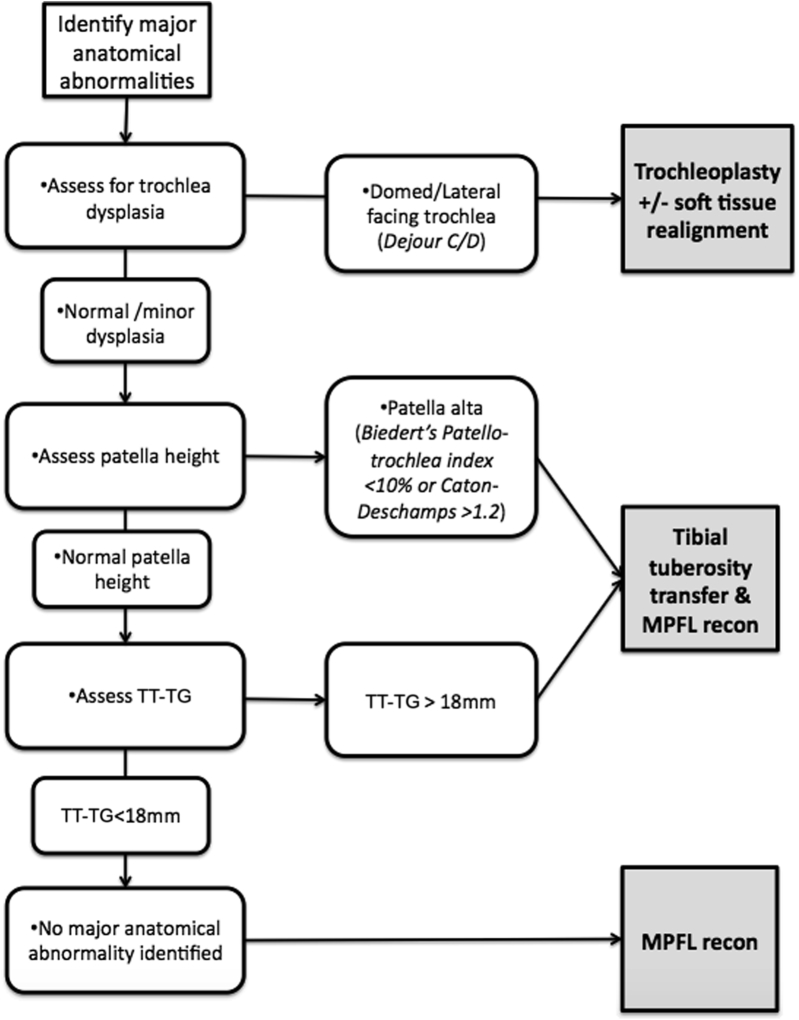
The purpose of this Technical Note is to describe a tibial tuberosity transfer technique with a MPFL reconstruction (Video 1). The indications for surgery have been summarized in Figure 1.
Fig 1.
Flowchart summarizing the indications for surgery. (MPFL, medial patellofemoral ligament; TT-TG, tibial tubercle–trochlear groove.)
Surgical Technique
Preoperative planning includes history, examination, and imaging by magnetic resonance. Severe trochlear dysplasia is a relative contraindication; usually this should be addressed by trochleoplasty. Distalization is planned to normalize the Biedert patellotrochlear index (32%) and Caton-Deschamps (1.0) ratio. A plan of the exact distalization in millimeters is made based on the sagittal magnetic resonance image. Medialization is planned to bring the TT-TG distance into the normal range, not to overmedialize it.
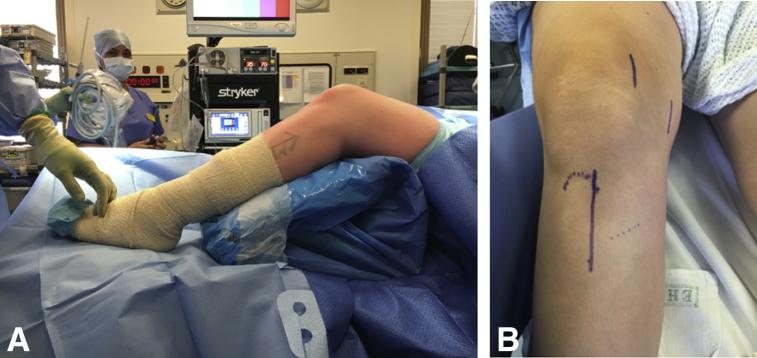
The patient is positioned supine with a lateral bolster and foot support. Figure 2A shows the patient positioning with the knee flexed. A high thigh tourniquet is applied. Care must be taken to avoid the bolster or tourniquet interfering with the arthroscope when in the superolateral portal.
Fig 2.
(A) Left knee view from lateral side. The knee is positioned over a sterile radiolucent triangle. This precludes the need for a lateral bolster, facilitating access to the superolateral portal. (B) Anterior view of the right knee. The incisions are planned to enable access for tibial tuberosity transfer and hamstring graft harvesting.
Our operative technique for tibial tubercle osteotomy includes an arthroscopy with a high superolateral portal to assess the patella position relative to the trochlea at the outset of the operation. We find that a 70° Stryker (Kalamazoo, MI) arthroscope permits excellent visualization of the patella, with a straight view down the trochlear groove.
The vertical skin incision follows the medial side of the tibial tuberosity from the tuberosity distally for 6 to 7 cm. The incision must permit access to the tuberosity and the gracilis so this may be harvested for the MPFL reconstruction. Figure 2B shows the planned skin incisions. The gracilis tendon is harvested, and the ends are prepared with a whipstitch.
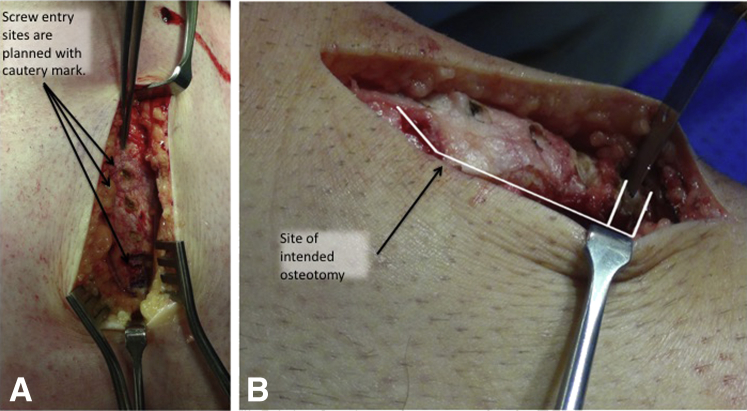
The anterior part of the tibialis anterior should be elevated from the tibia, and the patellar tendon insertion at the tibial tuberosity is identified and protected. Part of the planning includes the screw placement. Three marks are made on the tuberosity to indicate the intended position of the fixation screws so that an osteotomy of adequate length is planned.
The osteotomy is composed of 4 cuts, a single longitudinal coronal plane cut, 2 distal transverse cuts in the axial plane, and a proximal oblique cut proximal to the patellar tendon insertion. The longitudinal coronal cut is parallel to the tibia and does not exit distally or proximally. Figure 3A demonstrates how the screw placement is marked before the saw cuts are planned in Figure 3B. A slope in the coronal plane (as observed on the lateral radiograph) will cause anterior or posterior translation of the fragment. The osteotomy is made smooth and flat throughout so that it may slide to the new position and maximal surface area is available for union. This cut should be approximately 5 to 6 cm long. At the distal end of the osteotomy, an 8- to 15-mm segment of bone is removed, depending on the degree of distalization required. This step can be planned preoperatively with the assistance of the magnetic resonance imaging scan.
Fig 3.
(A) Anterior view of the right knee. Screw placement is planned prior to planning the osteotomy; here the intended positions have been marked with cautery. (B) View of right knee from the lateral side. The osteotomy is planned around the intended screw placement. The distalization has been planned on magnetic resonance imaging; the length of the removed segment plus 2 saw widths should equal the planned distalization. In the image, the planned osteotomy is marked with the white line.
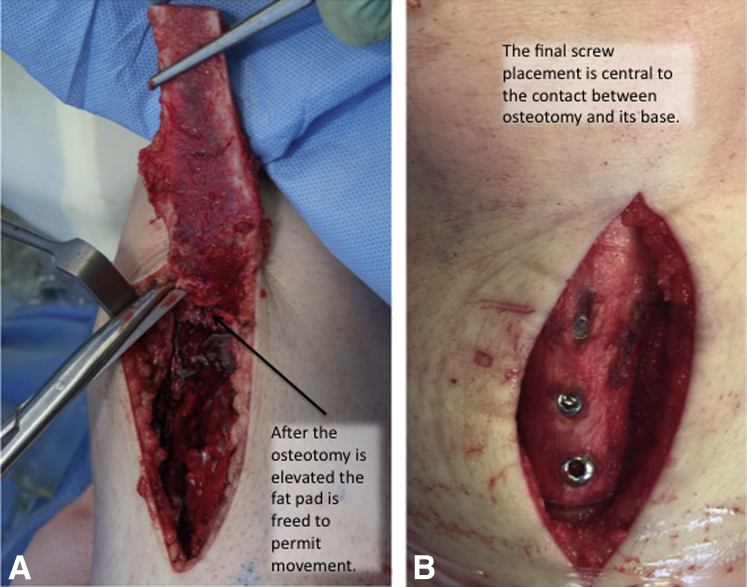
After the osteotomy is complete, the fragment is extended and freed from the fat pad, as shown in Figure 4A. If it does not move freely after release from the fat pad, then a release either side of the tendon may be required. The tuberosity fragment is moved to the new position with the desired distalization and medialization. It is held temporarily with a 2-mm K-wire. Where a medialization has been performed, attention must be paid to ensure that the fixation is in the center of the contact area between the fragment and tibia rather than merely at the center of the fragment.
Fig 4.
(A) View of right knee anterior. The osteotomy fragment is lifted from its base and extended to access the fat pad. (B) Anterior view of right knee. The screws are well countersunk.
Three small-fragment fully threaded screws are placed anteroposteriorly, with care to lag and countersink to achieve good compression without fracturing the tuberosity. Countersinking may also reduce the irritation that many patients experience over the tuberosity, though it by no means eliminates it. As demonstrated in Figure 4B, the screws should be well sunk in the fragment.
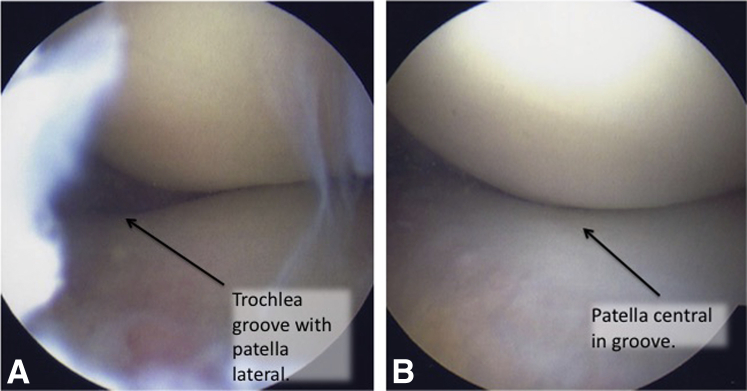
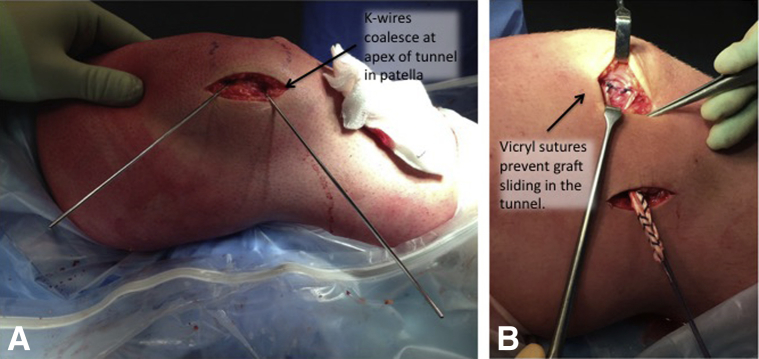
The superolateral arthroscopy (Fig 5A) may be repeated at this stage to confirm the need for MPFL reconstruction.7 The key features of the MPFL reconstruction are illustrated in Figure 6, they include a V-shaped patellar tunnel in the coronal plane for fixation of the gracilis graft. Vicryl sutures at the tunnel aperture prevent sliding in the tunnel. This broad patella insertion mimics the native MPFL. Femoral guidewire is placed under fluoroscopic control with the technique described by Schottle et al.,8 and then isometry is checked prior to definite tunnel placement. Correct graft tension is ascertained via appropriate position of the patella in the trochlear groove as confirmed by superolateral portal arthroscopic visualization (Fig 5B). Tension is maintained while the graft is fixed on the femoral side with a metal interference screw (usually 7 mm; Smith & Nephew, Nashville, TN) with the knee held at 30° of flexion.
Fig 5.
(A, B) Views from the superolateral portal. The superolateral portal arthroscopy can be repeated at 20° to conform the need for medial patellofemoral ligament reconstruction.
Fig 6.
(A). Right knee, lateral view. The tunnel is planned with two 1.8-mm K-wires and then drilled with a 4.5-mm cannulated drill (Smith & Nephew). The tunnel is in the coronal (long axis of the patella) plane. (B) Right knee, lateral view. The gracilis graft is secured to the tunnel aperture with a Vicryl suture to prevent sliding.
Discussion
The senior author has reported the results of this combined procedure in 21 cases.9 Some of the experiences of the senior author have been summarized in Tables 1 and 2. At 30 months, there was a significant improvement in patient-reported outcome measures. There were 3 complications—2 cases of stiffness and 1 nonunion. Although other authors have described transverse patellar fracture as a common complication when an axial plane patellar tunnel is used, this has not been the case with the longitudinal (coronal plane) tunnels.10
Table 1.
Pearls and Pitfalls
| Step | Pearls | Pitfalls |
|---|---|---|
| Preoperative planning | • Consider the underlying etiology. | • In the context of trochlear dysplasia, recurrent dislocation is likely. |
| • Template the required patella distalization. | • Indiscriminate medialization will lead to early arthritis. | |
| Osteotomy | • Mark the screw position on the proposed osteotomy fragment before making the bone cuts. | • An osteotomy fragment that is “too thin” increases the chances of nonunion. |
| • Keep the coronal cut parallel with the anterior tibia to avoid unintended anterior or posterior translation. | • An uneven coronal osteotomy may permit a pivot point when the fragment is compressed, resulting in fracture. | |
| • Start the coronal osteotomy and then use the initial cut as a slot for the saw to achieve a flat cut. | ||
| Fixation | • Avoid screw prominence and fracture by careful countersinking for the screw heads | • Fracture of the tuberosity fragment (can be addressed with a tension band construct over the screw heads). |
| MPFL reconstruction | • Assess the patella tracking by superolateral arthroscopy before proceeding to MPFL reconstruction. | • Avert fracture of the patellar tunnel by avoiding an axial plane tunnel. The tunnel should be V-shaped and in the coronal plane. |
Table 2.
Advantages and Disadvantages
| Advantages | Disadvantages |
|---|---|
| The objective is to restore joint stability without overloading the cartilage. | Combined procedures may require more protracted rehabilitation. |
| Joint congruence and stability can be directly assessed intraoperatively. | |
| If the tibial tuberosity osteotomy surface is kept flat, then a fracture is unlikely. | |
| If the patellar tunnel is made longitudinally (coronal plane) rather than transversely (sagittal plane), then a patellar fracture is unlikely. |
There has been a recent vogue for MPFL reconstruction, with many surgeons using the operation as ubiquitous treatment for patellar instability. However, because an approach that does not aim to achieve normal anatomy is unlikely to attain normal biomechanics, we aim to restore normal patella height and laterality. The objective is to attain a Biedert patellotrochlear index of approximately 32%. However, at what threshold we should make the decision to distalize remains uncertain. Barnett and Eldridge found that among patients with trochlear dysplasia, the patellotrochlear index was 15.3%; we use an arbitrary 10% as the threshold (Fig 1).11
Stephen et al. have found that if the lateralized tuberosity is moved medially then abnormal cartilage pressures can be resolved. They showed that an MPFL reconstruction may restore joint alignment and normal cartilage pressures when the TT-TG is less than 15 mm.12 When the TT-TG is greater, the MPFL reconstruction will not normalize the patellofemoral kinematics. We use 15 mm as the threshold for medialization (Fig 1).
The injudicious use of a medializing tuberosity transfer is also problematic. Arnbjornsson et al. described a small series of patients who had bilateral patellar instability but underwent a unilateral operation, most of which were medializing osteotomies. They found rates of late osteoarthritis (OA) of 75% in the operated knees compared with 29% without operation.13 Other studies have also found good early stability but degenerative changes in the longer term. A recent study by Tigchelaar et al.14 found a lower rate of OA progression (30%) at 10 years, although a more functional approach was used to determine the degree of medialization. These studies do not report the prevalence of trochlear dysplasia or patella alta in their populations. The older studies that show progression to arthritis do not report the TT-TG or the amount of medialization. It is difficult to comment on the cause of arthritis, whether this be medialization or overt medialization.
Naveed et al.15 found that the development of OA was related to pre-existing chondral damage at the time of surgery; nevertheless, some of those with normal surfaces developed early radiographic OA. As a result of these concerns, we would caution against the indiscriminate use of a medializing osteotomy in patients with instability. Where medialization is performed, this should be to create a normal TT-TG and not to overmedialize it.
The complications of tubercle osteotomy were reported in a systematic review of 787 osteotomies, where the complication rate was 4.6%.16 Hardware removal was required in 36.7%. This review did not examine the outcomes.
We are optimistic that improved understanding of anatomy and indications may lead to improved patient outcomes. There is a building body of evidence that creating a new abnormality accelerates arthritis. The limitations of tuberosity transfer or MPFL reconstruction are in cases where the underlying cause is trochlear dysplasia or where there is established degeneration of the trochlea.
MPFL reconstruction may be indicated as a treatment for patellar instability in the absence of osseous abnormality such as patella alta, trochlear dysplasia, or TT-TG more than 15 mm. Tibial tuberosity transfer is indicated for patellar instability with abnormalities of patella height or TT-TG. Where indications for both exist, they may be combined with the objective of restoring normal joint kinematics.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: V.M. receives consultancy fees from Stryker.
Supplementary Data
Technique for measured tibial tuberosity distalization and medial patellofemoral ligament reconstruction. The video describes how the 2 procedures may be combined, including dual access to the tuberosity and hamstrings through 1 incision. The video focuses on preoperative planning and the technical aspects of the surgery, including several tips and tricks that should assist you in avoiding the commonly described complications.
References
- 1.Dejour H., Walch G., Nove-Josserand L., Guier C. Factors of patellar instability: An anatomic radiographic study. Knee Surg Sports Traumatol Arthrosc. 1994;2:19–26. doi: 10.1007/BF01552649. [DOI] [PubMed] [Google Scholar]
- 2.Mountney J., Senavongse W., Amis A.A., Thomas N.P. Tensile strength of the medial patellofemoral ligament before and after repair or reconstruction. J Bone Joint Surg Br. 2005;87:36–40. [PubMed] [Google Scholar]
- 3.Stephen J.M., Kader D., Lumpaopong P., Deehan D.J., Amis A.A. Sectioning the medial patellofemoral ligament alters patellofemoral joint kinematics and contact mechanics. J Orthop Res. 2013;31:1423–1429. doi: 10.1002/jor.22371. [DOI] [PubMed] [Google Scholar]
- 4.Aframian A, Smith TO, Tennent TD, Cobb JP, Hing CB. Origin and insertion of the medial patellofemoral ligament: A systematic review of anatomy. Knee Surg Sports Traumatol Arthrosc September 8, 2016. [Epub ahead of print.] [DOI] [PMC free article] [PubMed]
- 5.Janssen G. Zur Atiologie der Patella luxation. Z Orthop. 1978;116:656–666. [PubMed] [Google Scholar]
- 6.Arshi A., Cohen J.R., Wang J.C., Hame S.L., McAllister D.R., Jones K.J. Operative management of patellar instability in the United States: An evaluation of national practice patterns, surgical trends, and complications. Orthop J Sports Med. 2016;4 doi: 10.1177/2325967116662873. 2325967116662873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ahmad R., Jayasekera N., Schranz P., Mandalia V. Medial patellofemoral ligament reconstruction: A technique with a “v”-shaped patellar tunnel. Arthrosc Tech. 2014;3:e589–e592. doi: 10.1016/j.eats.2014.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schottle P.B., Schmeling A., Rosenstiel N., Weiler A. Radiographic landmarks for femoral tunnel placement in medial patellofemoral ligament reconstruction. Am J Sports Med. 2007;35:801–804. doi: 10.1177/0363546506296415. [DOI] [PubMed] [Google Scholar]
- 9.Ahmad R., Calciu M., Jayasekera N., Schranz P., Mandalia V. Combined medial patellofemoral ligament reconstruction and tibial tubercle transfer results at a follow-up of 2 years. J Knee Surg. 2017;30:42–46. doi: 10.1055/s-0036-1579665. [DOI] [PubMed] [Google Scholar]
- 10.Parikh S.N., Nathan S.T., Wall E.J., Eismann E.A. Complications of medial patellofemoral ligament reconstruction in young patients. Am J Sports Med. 2013;41:1030–1038. doi: 10.1177/0363546513482085. [DOI] [PubMed] [Google Scholar]
- 11.Barnett A.J., Prentice M., Mandalia V., Wakeley C.J., Eldridge J.D. Patellar height measurement in trochlear dysplasia. Knee Surg Sports Traumatol Arthrosc. 2009;17:1412–1415. doi: 10.1007/s00167-009-0801-5. [DOI] [PubMed] [Google Scholar]
- 12.Stephen J.M., Dodds A.L., Lumpaopong P., Kader D., Williams A., Amis A.A. The ability of medial patellofemoral ligament reconstruction to correct patellar kinematics and contact mechanics in the presence of a lateralized tibial tubercle. Am J Sports Med. 2015;43:2198–2207. doi: 10.1177/0363546515597906. [DOI] [PubMed] [Google Scholar]
- 13.Arnbjornsson A., Egund N., Rydling O., Stockerup R., Ryd L. The natural history of recurrent dislocation of the patella. Long-term results of conservative and operative treatment. J Bone Joint Surg Br. 1992;74:140–142. doi: 10.1302/0301-620X.74B1.1732244. [DOI] [PubMed] [Google Scholar]
- 14.Tigchelaar S., van Essen P., Benard M., Koeter S., Wymenga A. A self-centring osteotomy of the tibial tubercle for patellar maltracking or instability: Results with ten-years' follow-up. J Bone Joint Br. 2015;97:329–336. doi: 10.1302/0301-620X.97B3.34515. [DOI] [PubMed] [Google Scholar]
- 15.Naveed M.A., Ackroyd C.E., Porteous A.J. Long-term (ten- to 15-year) outcome of arthroscopically assisted Elmslie-Trillat tibial tubercle osteotomy. J Bone Joint Br. 2013;95:478–485. doi: 10.1302/0301-620X.95B4.29681. [DOI] [PubMed] [Google Scholar]
- 16.Payne J., Rimmke N., Schmitt L.C., Flanigan D.C., Magnussen R.A. The incidence of complications of tibial tubercle osteotomy: A systematic review. Arthroscopy. 2015;31:1819–1825. doi: 10.1016/j.arthro.2015.03.028. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Technique for measured tibial tuberosity distalization and medial patellofemoral ligament reconstruction. The video describes how the 2 procedures may be combined, including dual access to the tuberosity and hamstrings through 1 incision. The video focuses on preoperative planning and the technical aspects of the surgery, including several tips and tricks that should assist you in avoiding the commonly described complications.