Abstract
Theories of anxiety disorders and phobias have ascribed a critical role to avoidance behavior in explaining the persistence of fear and anxiety, but knowledge about the role of avoidance behavior in the maintenance of anxiety in social anxiety disorder relative to specific phobia is lacking. This study examined the extent to which avoidance behavior moderates the relationship between general anxiety at baseline and 18 months later in women with a diagnosed social anxiety disorder (n = 91) and women with a diagnosed specific phobia (n = 130) at baseline. Circumscribed avoidance of social and specific situations were clinician-rated using the Anxiety Disorders Interview Schedule-Lifetime (ADIS-IV-L), and general anxiety was measured using the Beck Anxiety Inventory (BAI). Moderated regression analyses revealed that (a) general anxiety at baseline predicted general anxiety at follow-up in both women with a specific phobia and women with a social anxiety disorder and (b) avoidance behavior moderated this relationship in women with a specific phobia but not in women with a social anxiety disorder. Specifically, high avoidance behavior was found to amplify the effect between general anxiety at baseline and follow-up in specific phobia. Reasons for the absence of a similar moderating effect of avoidance behavior within social anxiety disorder are discussed.
Introduction
Social anxiety disorder and specific phobia are the most common lifetime anxiety disorders with prevalence rates in the United States estimated to be as high as 10.7 and 15.6 percent, respectively [1]. For Europe, these estimates were in the range of 1.9 to 13.7 percent for social anxiety disorder and 7.7 to 15.3 percent for specific phobia [2, 3]. Social anxiety disorder frequently emerges in adolescence or early adulthood and specific phobia in childhood [4–6]. Both social anxiety disorder and specific phobia are commonly accompanied by other mental disorders, including mood disorders and other anxiety disorders [7, 8], and it has been repeatedly shown that women are significantly more likely to be affected than men [9, 10].
Social anxiety disorder involves a marked and persistent fear of negative evaluation in social and/or performance situations. The individual fears that he or she will act in a way or show anxiety symptoms that will be humiliating or embarrassing [11]. One of the most common reported fears is public speaking [12]. Specific phobia is characterized as a marked and persistent fear that is excessive or unreasonable, cued by the presence or anticipation of a specific object or situation [11]. Animal phobia has been found to be one of the most prevalent types [9]. In each of these disorders, avoidance behavior (or endurance of feared situations with dread) is a defining feature [11].
Several theories of phobias and anxiety disorders have assigned a critical role to avoidance behavior in explaining the persistence of fear and anxiety (for an overview see [13]). In accordance with conditioning theory [14, 15], fear persists because avoidance of the conditioned stimulus (CS) prevents the extinction that normally occurs through repeated non-reinforced exposures. From a cognitive perspective, avoidance behavior prevents the gathering of information that disconfirms catastrophic misappraisals, and consequently such misappraisals and their resultant fear and anxiety are maintained [16, 17]. Another cognitive model emphasizes the role of fear prediction, with overprediction of fear [18, 19] motivating avoidance behavior, which in turn prevents disconfirmatory opportunities, so that anxiety remains high. A third cognitive model emphasizes the cognitive rehearsal of negative outcomes [20, 21] that sometimes occurs with rumination or mental reflection about aversive events in the absence of direct or vicarious experience (i.e., avoidance), thereby leading to inflations of fear.
Cognitive models of social anxiety disorder posit that socially anxious individuals engage in various ‘in-situation or subtle safety behaviors’, such as avoiding eye contact or avoiding pauses while talking [22–24]. These safety behaviors prevent socially phobic individuals from processing exposures accurately because they attribute the non-occurrence of feared outcomes (e.g., embarrassment, rejection) to the safety behaviors in which they engaged and, thus, their unrealistic beliefs maintain. Also, safety behaviors may increase feared anxiety symptoms (e.g., holding a glass tightly may increase the likelihood of shaking) or may inhibit performance in such a way as to negatively influence the responses of others (e.g., remaining quiet in social conversations may increase the likelihood of being ignored by others) [25, 26].
The role of avoidance behavior is further implicated by exposure-based treatments for anxiety disorders and phobias that replace avoidance with approach toward phobic stimuli [27–31]. More specifically, exposure-based therapies have been found to be effective for specific phobias [32, 33] and superior to placebo or alternative treatment approaches, including relaxation, progressive muscle relaxation, tension techniques, and cognitive therapy [34]. Several meta-analyses also report the efficacy of exposure based treatments for social anxiety disorder, with some showing equivalent effects when exposure is conducted alone or in combination with cognitive restructuring [35–39] and one finding provides additional support for the combination with cognitive restructuring [40]. A number of studies also support the superior efficacy of in vivo exposure combined with a decrease in safety behaviors relative to exposure alone in social anxiety disorder [26, 41, 42]. Finally, a recent study emphasizes the treatment of socially anxious individual’s fixed beliefs about their anxiety in cognitive behavioral therapy [43].
Looking across anxiety disorders, evidence exist that individuals with social anxiety disorder had a poorer treatment response after cognitive-behavioral therapy than those with generalized anxiety disorder [30, 44] and posttraumatic stress disorder [30]. These findings may support the differentiation between distress or misery disorders (which include depressive disorders, generalized anxiety disorder, and posttraumatic stress disorder) and the fear disorders (which include panic disorder, agoraphobia, social anxiety disorder, and specific phobia) [45]. In contrast, it was found that a lack of positive affect appears to be strongly associated with both social anxiety disorder and depression, which is at odds with the separation of social anxiety disorder as a fear and depression as a distress or misery disorder [46].
Although there are a number of studies showing that exposure is effective in treating social anxiety disorder and specific phobia, the influence of avoidance behavior on the maintenance of anxiety over time has not been investigated directly in individuals with social anxiety disorder and individuals with specific phobia. The aim of the present study was to examine the extent to which avoidance behavior moderates the relationship between general anxiety at baseline and 18 months later in women with a DSM-IV social anxiety disorder and women with a DSM-IV specific phobia. Specifically, we tested two main hypotheses derived from conditioning [14, 15] and cognitive models [16–21]. The first hypothesis was that general anxiety at baseline and circumscribed avoidance behavior between baseline and follow-up would both predict general anxiety at follow-up in women with social anxiety disorder and specific phobia. The second hypothesis was that the relationship between general anxiety at baseline and follow-up would be moderated by circumscribed avoidance behavior. Because socially anxious individuals can easily show ‘in-situation or subtle safety behaviors’ that maintains their social anxiety [22–24], we expect a stronger moderating effect of avoidance for the specific phobia group as compared to the social anxiety disorder group. Specifically, we assumed that low avoidance behavior would have a buffering effect, whereas high avoidance behavior would amplify the strength of the relationship between general anxiety at baseline and follow-up.
Method
Participants
The data were derived from the Dresden Prediction Study (DPS), a prospective epidemiological study designed to collect data on the prevalence rates, incidence, course, and risk factors of mental disorders in young women (for details about the study see [47–50]). The focus of the DPS was to investigate women during early adulthood because of the high prevalence rates of anxiety disorders in women [51, 52]. The protocol of the DPS was approved by the local ethics board, the ‘sächsischer Datenschutz’. The sample was drawn randomly from the German Dresden government registry of residents in 1996. Of the 9,000 addresses received from the registry office, 5,204 women were located and eligible for the study. Of these, 3,065 women responded, resulting in a response rate of 58.9%. A subsample of 1,877 were willing to take part in the diagnostic interview and to complete a package of self-report measures at baseline and 1,396 at the follow-up survey approximately 18 months apart (see [48] for a flow diagram of the number of respondents and response rates at baseline and follow-up). The baseline interviews were conducted between July 1996 and September 1997, and the follow-up interviews between December 1997 and February 1999. Inclusion criteria were being female and being 18–25 years of age at the time of the baseline investigation. There were no significant differences in overall mental disorders at baseline between women with complete data at baseline and follow-up and women with missing interview or self-report data at follow-up (t(802) = -1.40, p = .161). The present study refers to 1,396 women, aged between 18 to 24 years at the time of sampling, who completed a diagnostic interview and self-report questionnaires at baseline and follow-up.
Procedure and measures
The women received a letter with detailed information about the DPS and a reply card to provide written informed consent to participate in the study. The interested women were invited for the diagnostic interview conducted by trained clinical interviewers. In addition, a package of questionnaires was administered. Participants willing to join the second diagnostic interview were invited on average 18 months later. There were no financial reimbursements for participants in the study.
Diagnostic assessment
The diagnostic assessments were based on the German version of the Anxiety Disorders Interview Schedule-Lifetime (ADIS-IV-L) [53, 54]. The ADIS-IV-L is a structured interview for diagnosing Axis I disorders, including anxiety disorders, affective disorders, somatoform disorders, substance use disorders, eating disorders, and children’s disorders according to DSM-IV [55]. In the baseline interview, questions were asked about mental problems during the entire lifetime and during the last seven days (lifetime and point prevalence, respectively). The follow-up interviews referred to the mental problems that had occurred since the baseline interview and during the last seven days (period and point prevalence, respectively). In the current study, the seven-day point prevalence at baseline was used to compose the two groups, women with a baseline social anxiety disorder and women with a baseline specific phobia. The inter-rater reliabilities of the German version of the ADIS-IV-L in a patient sample (n = 237) were between .61 and .98 (Yule’s Y coefficient) for social anxiety disorder and between .73 and .98 (Yule’s Y coefficient) for specific phobia [56]. Retest-reliabilities across the groups of disorders were between .68 and .79 (Kappa coefficient) and between .67 and 1.0 (Yule’s coefficient) [56, 57]. In addition, the interview has demonstrated high validity [58, 59] as well as good acceptance in clinical practice and research settings [60].
Clinical severity rating
Based on the ADIS, the clinicians rated the severity of distress and interference for each disorder, on a scale ranging from 0 (not severe at all) to 8 (very severe). A diagnosis was considered clinically severe when the clinical severity rating was of 4 or above.
Interviewers, training procedure, and supervision
Interviewers were clinical psychologists, physicians, or advanced graduate students of clinical psychology. They underwent an intensive 40-hour training on mental disorders, their rating and the conduct of the interviews and subsequently attended supervision meetings every two weeks. The written protocol for each interview was proof read by supervisors (e.g., were all answers complete, and did the answers match the diagnosis assigned). Unclear cases were discussed, and if necessary a consensus diagnosis was given.
Avoidance behavior
Avoidance behavior at baseline and follow–up were measured by the German version of the ADIS-IV-L [53, 54]. In this structured interview, the interviewer read a list of 13 social situations (e.g., public speaking, talking to people in authority) and 17 specific situations (e.g., animals, heights) and asked the women to indicate if they ‘wanted to avoid’ each situation. If the answer was ‘yes’, the interviewer enquired about the degree of avoidance, which were rated on a scale of 0 (no avoidance) to 8 (very severe avoidance).
In the current study, the avoidance scores were summed separately for social and specific situations at the follow-up interview, with ratings anchored to ‘since the baseline interview’. The possible ranges are 0–104 for avoidance of social situations and 0–136 for avoidance of specific situations, respectively. These sum scores reflect circumscribed avoidance with higher scores indicating greater avoidance. In the current sample, the internal consistency (Cronbach’s α) was .76 for social situations and .70 for specific situations.
Beck Anxiety Inventory (BAI)
The Beck Anxiety Inventory (BAI) [61, 62] is a 21-item self-report inventory of the severity of anxiety symptoms (e.g., feeling hot, or fear of losing control). Participants were asked to rate how much each symptom bothered them ‘during the past week, including today’ on a 4-point-rating scale ranging from ‘not at all’ (0) to ‘severely–I could barely stand it’ (3). The possible range of the total score goes from 0 to 63 with scores between 0 and 21 indicating low anxiety, scores between 22 and 35 moderate anxiety, and scores of 36 and above indicating potentially concerning levels of anxiety. In the current sample, the BAI had good internal consistency (Cronbach’s α = .82).
Definition of the groups
To study the moderating role of avoidance behavior on general anxiety over time in women with a social anxiety disorder and women with a specific phobia, two subgroups of the initial sample of 1,396 participants were composed based on the seven-day point prevalence at baseline of the ADIS-IV-L: The first group were 91 women with a baseline social anxiety disorder and the second group were 130 women with a baseline specific phobia. Comorbid cases were included in both groups. The datasets used in the present study are available in S1 and S2 Datasets. These group sizes resulted in more statistical power to detect substantial effects in the group of specific phobia relative to the group of social anxiety disorder [63]. Using the software program G*Power 3 [64], the power to detect a medium effect for the interaction (f2 = 0.15) with an alpha level of five percent is 99.2 percent for the model with 130 women (specific phobia group) and 95.5 percent for the model with 91 women (social anxiety disorder group). These power estimates drop drastically to 36.0% and 26.6% when the interaction effects turn out to be small (f2 = 0.02). To detect a small interaction effect with a power of .80, a sample size of 395 would be required. Thus, in addition to results of the significance tests, we rely on effect sizes as well. The average age at baseline was 21 years (SD = 1.8 to 1.9) for both groups.
Statistical analyses
Ordinary least squares (OLS) regression analysis was used to examine the moderating effect of circumscribed avoidance behavior between baseline and follow-up on the relationship between general anxiety at baseline and 18 months later. The predictor and moderator variables were mean-centered prior to the analyses [65]. The centered predictor and moderator variables were then multiplied to form the interaction terms. Conducting hierarchical regression analysis, the simple effects of general anxiety at baseline (General anxiety baseline) and avoidance of situations between baseline and follow-up (Avoidance) were entered on the first step and the interaction term (General anxiety baseline × Avoidance) was entered on the second step. We used f2 as a measure of effect size for the interaction effect and considered effect sizes of .02, .15, and .35 as small, medium, and large, respectively [63].
Results
Preliminary analyses
Women with a baseline social anxiety disorder mostly feared public speaking (Mdn = 4.00, M = 4.04, SD = 2.12; possible range of anxiety severity: 0–8, with 0 = no anxiety and 8 = very severe anxiety). Less feared situations were talking to people in authority (Mdn = 2.00, M = 2.21, SD = 1.95), starting a conversation (Mdn = 2.00, M = 1.95, SD = 1.92), rejecting a senseless claim or asking someone to change his or her behavior (Mdn = 1.00, M = 1.77, SD = 1.65), and talking to strangers (Mdn = 1.00, M = 1.45, SD = 1.73). Women with a baseline specific phobia mostly feared animals (Mdn = 4.00, M = 3.99, SD = 2.60; possible range of anxiety severity: 0–8, with 0 = no anxiety and 8 = very severe anxiety). Less feared situations were heights (Mdn = 0.00, M = 1.66, SD = 2.20) and blood, injuries, and injections (Mdn = 0.58, M = 1.12, SD = 1.50). As expected, the means of clinical severity in women with a baseline social anxiety disorder and specific phobia were above the clinical cut-off of 4, providing further evidence that these individuals can be considered to be clinically severe (baseline social anxiety disorder: Mdn = 4.00, M = 4.24, SD = 1.30; baseline specific phobia: Mdn = 4.00, M = 4.32, SD = 1.25).
The co-occurring diagnoses at baseline and follow-up for the social anxiety disorder and specific phobia groups are given in Table 1. Among the 91 women with a social anxiety disorder diagnosis, 39 (42.9%) had comorbid diagnoses at baseline. The most frequent co-occurring diagnoses were another anxiety disorder, namely specific phobia, agoraphobia without panic disorder, and generalized anxiety disorder. Of the 91 women with baseline social anxiety disorder, 33 (36.3%) fulfilled the diagnostic criteria for social anxiety disorder also at follow-up. Among the 130 women with a specific phobia diagnosis, 32 (24.6%) had comorbid diagnoses at baseline. The most frequent co-occuring diagnoses were another anxiety disorder, namely social anxiety disorder, agoraphobia without panic disorder, and generalized anxiety disorder. Of the 130 women with baseline specific phobia, 52 (40.0%) fulfilled the diagnostic criteria for specific phobia also at follow-up.
Table 1. Diagnoses at baseline and follow-up for the social anxiety disorder and specific phobia groups.
| Diagnoses | Baseline SAD (n = 91) |
Baseline SP (n = 130) |
||||||
|---|---|---|---|---|---|---|---|---|
| Baseline | Follow-up | Baseline | Follow-up | |||||
| n | % | n | % | n | % | n | % | |
| Anxiety disorders | ||||||||
| PD without AGR | 1 | 1.1 | 1 | 1.1 | 0 | 0.0 | 4 | 3.1 |
| PD with AGR | 2 | 2.2 | 2 | 2.2 | 1 | 0.8 | 2 | 1.5 |
| AGR without PD | 7 | 7.7 | 5 | 5.5 | 6 | 4.6 | 4 | 3.1 |
| SAD | 91 | 100 | 33 | 36.3 | 18 | 13.8 | 13 | 10.0 |
| SP | 18 | 19.8 | 19 | 20.9 | 130 | 100 | 52 | 40.0 |
| GAD | 5 | 5.5 | 5 | 5.5 | 4 | 3.1 | 7 | 5.4 |
| OCD | 3 | 3.3 | 4 | 4.4 | 2 | 1.5 | 2 | 1.5 |
| PTSD | 3 | 3.3 | 0 | 0.0 | 1 | 0.8 | 0 | 0.0 |
| Affective disorders | 3 | 3.3 | 7 | 7.7 | 3 | 2.3 | 6 | 4.6 |
| Somatoform disorders | 0 | 0.0 | 3 | 3.3 | 3 | 2.3 | 3 | 2.3 |
| Substance use disorders | 4 | 4.4 | 3 | 3.3 | 2 | 1.5 | 3 | 2.3 |
| Eating disorders | 4 | 4.4 | 5 | 5.5 | 1 | 0.8 | 3 | 2.3 |
Note. PD = panic disorder. AGR = agoraphobia. SAD = social anxiety disorder. SP = specific phobia. GAD = generalized anxiety disorder. OCD = obsessive-compulsive disorder. PTSD = posttraumatic stress disorder.
Product-moment correlations between baseline general anxiety and avoidance were .02 for the social anxiety disorder group and .09 for the specific phobia group. Descriptive statistics are given in Table 2. In the specific phobia group, the general anxiety measure at baseline was in average significantly higher than at follow-up, t(128) = 2.726, p = .007, Cohen’s d = 0.240, but not in the social anxiety disorder group, t(90) = 1.852, p = .067, Cohen’s d = 0.194.
Table 2. Means, standard deviations, and empirical ranges for the study variables for the social anxiety disorder and specific phobia groups.
| Variable | Baseline SAD (n = 91) |
Baseline SP (n = 130) |
||||
|---|---|---|---|---|---|---|
| M | SD | Range | M | SD | Range | |
| Avoidance | 10.45 | 8.19 | 0–31 | 12.13 | 10.96 | 0–45 |
| General anxiety baseline | 8.09 | 6.70 | 0–28 | 6.07 | 5.64 | 0–28 |
| General anxiety follow-up | 6.82 | 6.73 | 0–31 | 4.75 | 5.77 | 0–28 |
| Number of disorders | 1.56 | 0.75 | 1–4 | 1.33 | 0.68 | 1–5 |
Note. SAD = social anxiety disorder. SP = specific phobia. Avoidance = Avoidance between baseline and follow-up. M = Mean, SD = Standard deviation. Number of disorders = Number of disorders total at baseline. Possible ranges: 0–104 for avoidance of social situations, 0–136 for avoidance of specific situations, 0–63 for general anxiety.
Main analyses
The moderating effect of circumscribed avoidance behavior between baseline and follow-up on the relationship between general anxiety at baseline and general anxiety at follow-up was analyzed separately for women with social anxiety disorder and women with specific phobia. The results of these models are given in Table 3.
Table 3. Regression analyses for the social anxiety disorder and specific phobia groups testing whether the relationship between general anxiety at baseline and at follow-up is moderated by avoidance behavior between baseline and follow-up.
| Predictor | Baseline SAD (n = 91) |
Baseline SP (n = 130) |
||||
|---|---|---|---|---|---|---|
| b | SE | R2 | b | SE | R2 | |
| General anxiety baseline | 0.491*** | 0.091 | .840 | 0.492*** | 0.082 | .881 |
| Avoidance | 0.151* | 0.072 | .118 | 0.047 | 0.038 | .051 |
| General anxiety baseline × Avoidance | 0.012 | 0.009 | .042 | 0.012* | 0.005 | .068 |
| Intercept | 6.801*** | 0.591 | 4.707*** | 0.419 | ||
Note. SAD = social anxiety disorder. SP = specific phobia. General anxiety baseline and Avoidance were mean-centered prior to the analyses.
*p < .05.
***p < .001 (2-tailed).
Social anxiety disorder
Both simple effects were, as expected, positive and statistically significant for the social anxiety disorder group, revealing that the higher the general anxiety at baseline and the higher avoidance behavior the higher the level of general anxiety at follow-up. Contrary to our second hypothesis, the interaction effect was not statistically significant, indicating that the relationship between general anxiety at baseline and at follow-up was not moderated by the level of avoidance behavior. The total explained variance was 32.1%, and the variance explained by the two simple effects was 30.7%. The effect size f2 of the interaction was .019, indicating no substantial interaction effect.
Specific phobia
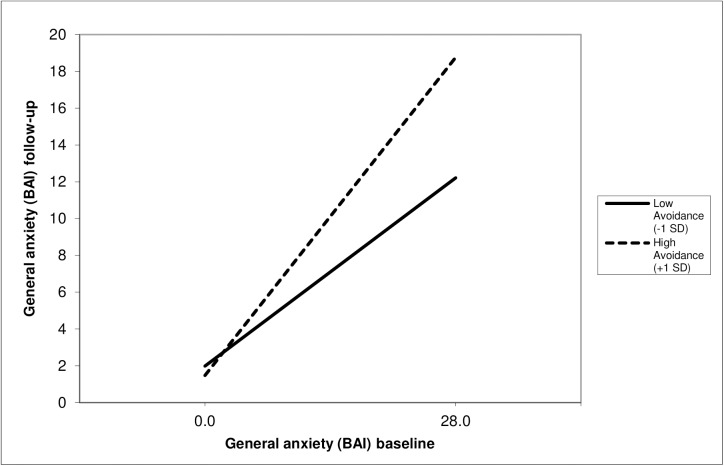
As expected, the simple effect of general anxiety at baseline was positive and statistically significant for the specific phobia group but the effect from avoidance was not significant, indicating that the higher the level of general anxiety at baseline the higher the level of general anxiety at follow-up. The interaction effect was, in line with the second hypothesis, statistically significant, indicating that the relationship between general anxiety at baseline and at follow-up was moderated by the level of avoidance behavior. The relationship between anxiety at baseline and follow-up for low avoidance, defined as the mean minus 1 SD (i.e., -10.96), and high avoidance, defined as the mean plus one SD (i.e., 10.96), is presented in Fig 1. As can be seen, in both, women with low avoidance and women with high avoidance general anxiety decreased, yet this decrease was substantially lower in women with low avoidance. Using the Johnson-Neyman [66] technique to identify regions of significance, the effect between general anxiety at baseline and follow-up was statistically significant for the whole range of avoidance behavior. This means that for any possible value of avoidance behavior the relationship between general anxiety at baseline and follow-up is statistically significant. The total explained variance was 34.5%, the variance explained by the two simple effects was 32.1%. The effect size of the interaction was .036, which–although small in size according to Cohen’s thumb of role–is substantially bigger than the interaction in the social anxiety disorder group.
Fig 1. Regression lines of the specific phobia group showing the moderating effect of avoidance behavior of specific situations on the relationship between general anxiety at baseline and follow-up.
In sum, these results suggest that avoidance behavior seems to have a more direct influence on general anxiety at follow-up for women with a social anxiety disorder. In contrast, in women with a specific phobia avoidance behavior seems to have a moderating effect on the relationship between general anxiety at baseline and follow-up.
Expected change
A question of practical interest may be how much change we can expect in general anxiety from baseline to follow-up depending on the level of avoidance behavior between baseline and follow-up for a particular person. For instance, for a woman with a social anxiety disorder and a score of general anxiety at baseline of 5.0, the expected general anxiety score at follow-up is 4.7 if her avoidance score is 0 and 9.0 if her avoidance score is 30. For a woman with a specific phobia and a score of general anxiety at baseline of 5.0, the expected general anxiety score at follow-up is 3.9 if her avoidance score is 0 and 5.1 if her avoidance is 30.
Additional analyses
We rerun the regression analyses controlling for a set of potential confounding variables. First we controlled for the number of other mental disorders at baseline for the social anxiety disorder and specific phobia group and found that the pattern did not change. Second, we controlled for whether participants received treatment because a few participants received treatment for personal or emotional problems in the intermediate interval (9 women or 9.9% with social anxiety disorder and 13 women or 10.0% with specific phobia). Again, controlling for possible treatment did not significantly alter the interaction effects or the simple effects. We note, however, that the inclusion of these control variables had a negative effect on the distribution of the residuals, violating the assumption of normally distributed residuals.
Discussion
The current study aimed to examine the mechanism by which circumscribed avoidance behavior contributes to the maintenance of general anxiety in women with a baseline social anxiety disorder and a baseline specific phobia. In line with findings of studies investigating the effect of exposure-based treatments [32, 33, 35, 39], the current results support that low circumscribed avoidance behavior can lower general anxiety over time. However, the mechanism by which avoidance behavior did so was different for women with a DSM-IV specific phobia and women with a DSM-IV social anxiety disorder. As would be expected from cognitive theory [15] and overprediction of fear [18], avoidance behavior moderated the strength of the association between general anxiety at baseline and at follow-up in women with a specific phobia. As illustrated in the example, low avoidance had a buffering effect, whereas very high avoidance amplified the strength of the relationship between baseline and follow-up general anxiety. In contrast, in women with a diagnosed social anxiety disorder, circumscribed avoidance behavior was found to have a direct but no moderating effect on general anxiety at follow up.
There are several explanations for the different role avoidance behavior plays in explaining the maintenance of anxiety in specific phobia and social anxiety disorder. One explanation is that individuals with a specific phobia may be more successful in their avoidance of feared situations than individuals with a social anxiety disorder, since social situations (e.g., starting a conversation) are often more unavoidable to a certain degree than specific situations (e.g., heights). Another explanation is, that individuals with a specific phobia may experience more positive outcomes after approach behavior than individuals with a social anxiety disorder due to biases in information processing [67–69]. For instance, individuals with a social anxiety disorder may interpret ambiguous stimuli (e.g., frowns, signs of boredom) as indicators of disapproval, which increases their anxiety. Hence, avoidance behavior may, in line with the current results, more directly influence anxiety in specific phobia, whereas the effects of approach interfere with the disconfirmation of negative beliefs in social anxiety disorder. Moreover, avoidance behavior may be more subtle in social anxiety disorder than specific phobia, such as the reliance on ‘in-situation or subtle safety behaviors’ that contribute to the maintenance or exacerbation of anxiety [25, 26]. The ratings of avoidance employed herein did not cover such ‘in-situation or subtle safety behaviors’, resulting in lower sensitivity for measuring the effects of avoidance in social anxiety disorder.
The findings of this study add to the growing number of studies investigating the role of important moderating variables (e.g., attentional control, anxiety sensitivity) in anxiety and phobia research [70, 71]. In addition, our study supports the finding that young adolescents in the general population have a relatively high likelihood of remission for social anxiety disorder and specific phobia. In our study, 64% of the women with a baseline social anxiety disorder did not fulfill all criteria for a DSM-IV social anxiety disorder 18 months later. This finding is in line with results from other community-based prospective studies with remission rates for social anxiety disorder between 54 and 93 percent over a time interval of 1 to 4 years in 14- to 65-year olds [72, 73]. In the current study, 60% of the women with a baseline specific phobia did not fulfill all criteria for a DSM-IV specific phobia at follow-up. A similar rate was reported in another prospective community-based study, with 70% of the 14-to 17-year old adolescents showing remission of threshold and subthreshold specific phobia over a 19-month time interval [74]. Other major strengths of the present study include the longitudinal design, the standardized assessment of DSM-IV diagnoses of specific phobia and social anxiety disorder, and the large sample size of 221 women with a corresponding anxiety disorder. However, there are also a few limitations. First, the measure of avoidance was based on retrospective reports covering the period between the baseline and follow-up interview. Nonetheless, retrospective reports of anxiety symptoms have been shown to be fairly accurate in past studies [75, 76]. Second, there may be differences in the effect of the moderating role of avoidance behavior for singular social and specific situations, such as public speaking or animals. This could be addressed in further studies since our data did not enable a meaningful examination of single situations. Third, although we have made attempts to address issues of overlap of diagnoses in the two groups, it would be interesting to examine women with a pure social anxiety disorder relative to women with a pure specific phobia. However, the limited number of diagnosed women in our study did not allow us to examine this question. Finally, our sample consisted of a community sample of young women aged between 18 and 24 years only, all of whom lived in Germany. The results need to be verified for younger and older populations as well as males.
In conclusion, the current study showed that circumscribed avoidance behavior moderated the relationship between general anxiety at baseline and at follow-up in women with a baseline specific phobia, whereas in women with a baseline social anxiety disorder circumscribed avoidance behavior was directly associated with general anxiety at follow-up. The findings also highlight the crucial role that avoidance behavior plays in the maintenance of general anxiety in both women with a social anxiety disorder and women with a specific phobia.
Supporting information
(XLSX)
(XLSX)
Acknowledgments
We would like to thank the many people who helped with the study. This study was supported by the German Ministry of Science, Research and Education grant no. DLR 01EG9410 and by the National Centre of Competence in Research sesam, Swiss National Science Foundation grant no. 51A240-104890. The research of the first and second authors were supported by a grant from the Swiss National Science Foundation no. PBBS1-120509 and PBFR1-120897.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
This study was supported by the German Ministry of Science, Research and Education grant no. DLR 01EG9410 and by the National Centre of Competence in Research sesam, Swiss National Science Foundation grant no. 51A240-104890. The research of the first and second authors was supported by grants from the Swiss National Science Foundation, no. PBBS1-120509 and PBFR1-120897.
References
- 1.Kessler RC, Petukhova M, Sampson NA, Zaslavsky AM, Wittchen HU. Twelve‐month and lifetime prevalence and lifetime morbid risk of anxiety and mood disorders in the United States. International Journal of Methods in Psychiatric Research. 2012;21(3):169–84. doi: 10.1002/mpr.1359 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jacobi F, Höfler M, Siegert J, Mack S, Gerschler A, Scholl L, et al. Twelve‐month prevalence, comorbidity and correlates of mental disorders in Germany: The Mental Health Module of the German Health Interview and Examination Survey for Adults (DEGS1-MH). International Journal of Methods in Psychiatric Research. 2014;23(3):304–19. doi: 10.1002/mpr.1439 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Michael T, Zetsche U, Margraf J. Epidemiology of anxiety disorders. Psychiatry. 2007. 6:136–42. [Google Scholar]
- 4.Beesdo-Baum K, Knappe S. Developmental epidemiology of anxiety disorders. Child and Adolescent Psychiatric Clinics of North America. 2012;21(3):457–78. doi: 10.1016/j.chc.2012.05.001 [DOI] [PubMed] [Google Scholar]
- 5.Beesdo K, Knappe S, Pine DS. Anxiety and anxiety disorders in children and adolescents: Developmental issues and implications for DSM-V. Psychiatric Clinics of North America. 2009;32(3):483–524. doi: 10.1016/j.psc.2009.06.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kessler RC, Amminger GP, Aguilar-Gaxiola S, Alonso J, Lee S, Üstün TB. Age of onset of mental disorders: A review of recent literature. Current Opinion in Psychiatry. 2007;20(4):359–64. doi: 10.1097/YCO.0b013e32816ebc8c [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fehm L, Pelissolo A, Furmark T, Wittchen H-U. Size and burden of social phobia in Europe. European Neuropsychopharmacology. 2005;15(4):453–62. doi: 10.1016/j.euroneuro.2005.04.002 [DOI] [PubMed] [Google Scholar]
- 8.Ollendick TH, Öst L-G, Reuterskiöld L, Costa N. Comorbidity in youth with specific phobias: Impact of comorbidity on treatment outcome and the impact of treatment on comorbid disorders. Behaviour Research and Therapy. 2010;48(9):827–31. doi: 10.1016/j.brat.2010.05.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.LeBeau RT, Glenn D, Liao B, Wittchen H-U, Beesdo-Baum K, Ollendick T, et al. Specific phobia: A review of DSM-IV specific phobia and preliminary recommendations for DSM-V. Depression and Anxiety. 2010;27(2):148–67. doi: 10.1002/da.20655 [DOI] [PubMed] [Google Scholar]
- 10.Wittchen H-U, Stein MB, Kessler RC. Social fears and social phobia in a community sample of adolescents and young adults: Prevalence, risk factors and co-morbidity. Psychological Medicine. 1999;29(2):309–23. [DOI] [PubMed] [Google Scholar]
- 11.Diagnostic and statistical manual of mental disorders: DSM-5™ (5th ed.). Arlington, VA, US: American Psychiatric Publishing, Inc.; 2013. [Google Scholar]
- 12.Ruscio AM, Brown TA, Chiu WT, Sareen J, Stein MB, Kessler RC. Social fears and social phobia in the USA: Results from the National Comorbidity Survey Replication. Psychological Medicine. 2008;38(1):15–28. doi: 10.1017/S0033291707001699 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Craske MG. Anxious processes In: Craske MG, editor. Origins of phobias and anxiety disorders: Why more women than men? Oxford: Elsevier; 2003. p. 71–98. [Google Scholar]
- 14.Mowrer OH. A stimulus-response analysis of anxiety and its role as a reinforcing agent. Psychological Review. 1939;46(6):553–65. [Google Scholar]
- 15.Mowrer OH . 'Sin': The lesser of two evils. American Psychologist. 1960;15(5):301–4. [Google Scholar]
- 16.Clark DM. A cognitive approach to panic. Behaviour Research and Therapy. 1986;24(4):461–70. [DOI] [PubMed] [Google Scholar]
- 17.Clark DM. A cognitive model of panic attacks In: Rachman S, Maser JD, Rachman S, Maser JD, editors. Panic: Psychological perspectives. Hillsdale, NJ, US: Lawrence Erlbaum Associates, Inc; 1988. p. 71–89. [Google Scholar]
- 18.Rachman SJ. The overprediction of fear: A review. Behaviour Research and Therapy. 1994;32(7):683–90. [DOI] [PubMed] [Google Scholar]
- 19.Rachman S, Lopatka C. Match and mismatch in the prediction of fear: I. Behaviour Research and Therapy. 1986;24(4):387–93. [DOI] [PubMed] [Google Scholar]
- 20.Davey GC. Classical conditioning and the acquisition of human fears and phobias: A review and synthesis of the literature. Advances in Behaviour Research & Therapy. 1992;14(1):29–66. [Google Scholar]
- 21.Field AP, Davey GCL. Conditioning models of childhood anxiety In: Silverman WK, Treffers PDA, Silverman WK, Treffers PDA, editors. Anxiety disorders in children and adolescents: Research, assessment and intervention. Cambridge child and adolescent psychiatry. New York, NY, US: Cambridge University Press; 2001. p. 187–211. [Google Scholar]
- 22.Clark DM, Wells A. A cognitive model of social phobia In: Heimberg RG, Liebowitz MR, Hope DA, Schneier FR, Heimberg RG, Liebowitz MR, et al. , editors. Social phobia: Diagnosis, assessment, and treatment. New York, NY, US: Guilford Press; 1995. p. 69–93. [Google Scholar]
- 23.Heimberg RC, Brozovich FA, Rapee RM. A cognitive-behavioral model of social anxiety disorder In: Hofmann SG, DiBartolo PM, Hofmann SG, DiBartolo PM, editors. Social anxiety: Clinical, developmental, and social perspectives (3rd ed). San Diego, CA, US: Elsevier Academic Press; 2014. p. 705–28. [Google Scholar]
- 24.Rapee RM, Heimberg RG. A cognitive-behavioral model of anxiety in social phobia. Behaviour Research and Therapy. 1997;35(8):741–56. [DOI] [PubMed] [Google Scholar]
- 25.Salkovskis PM. The importance of behaviour in the maintenance of anxiety and panic: A cognitive account. Behavioural Psychotherapy. 1991;19(1):6–19. [Google Scholar]
- 26.Wells A, Clark DM, Salkovskis P, Ludgate J, Hackmann A, Gelder M. Social phobia: The role of in-situation safety behaviors in maintaining anxiety and negative beliefs. Behavior Therapy. 1995;26(1):153–61. [DOI] [PubMed] [Google Scholar]
- 27.Abramowitz JS, Deacon BJ, Whiteside SPH. Exposure therapy for anxiety: Principles and practice. New York, NY, US: Guilford Press; 2011. [Google Scholar]
- 28.Barlow DH. Anxiety and its disorders: The nature and treatment of anxiety and panic., 2nd ed. New York, NY, US: Guilford Press; 2002. [Google Scholar]
- 29.Craske MG, Mystkowski JL. Exposure Therapy and Extinction: Clinical Studies In: Craske MG, Hermans D, Vansteenwegen D, Craske MG, Hermans D, Vansteenwegen D, editors. Fear and learning: From basic processes to clinical implications. Washington, DC, US: American Psychological Association; 2006. p. 217–33. [Google Scholar]
- 30.Norton PJ, Price EC. A meta-analytic review of adult cognitive-behavioral treatment outcome across the anxiety disorders. Journal of Nervous and Mental Disease. 2007;195(6):521–31. doi: 10.1097/01.nmd.0000253843.70149.9a [DOI] [PubMed] [Google Scholar]
- 31.Mayo-Wilson E, Dias S, Mavranezouli I, Kew K, Clark DM, Ades AE, et al. Psychological and pharmacological interventions for social anxiety disorder in adults: A systematic review and network meta-analysis. The Lancet Psychiatry. 2014;1(5):368–76. doi: 10.1016/S2215-0366(14)70329-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Choy Y, Fyer AJ, Lipsitz JD. Treatment of specific phobia in adults. Clinical Psychology Review. 2007;27(3):266–86. doi: 10.1016/j.cpr.2006.10.002 [DOI] [PubMed] [Google Scholar]
- 33.Zlomke K, Davis TE III. One-session treatment of specific phobias: A detailed description and review of treatment efficacy. Behavior Therapy. 2008;39(3):207–23. doi: 10.1016/j.beth.2007.07.003 [DOI] [PubMed] [Google Scholar]
- 34.Wolitzky-Taylor KB, Horowitz JD, Powers MB, Telch MJ. Psychological approaches in the treatment of specific phobias: A meta-analysis. Clinical Psychology Review. 2008;28(6):1021–37. doi: 10.1016/j.cpr.2008.02.007 [DOI] [PubMed] [Google Scholar]
- 35.Fedoroff IC, Taylor S. Psychological and pharmacological treatments of social phobia: A meta-analysis. Journal of Clinical Psychopharmacology. 2001;21(3):311–24. [DOI] [PubMed] [Google Scholar]
- 36.Feske U, Chambless DL. Cognitive behavioral versus exposure only treatment for social phobia: A meta-analysis. Behavior Therapy. 1995;26(4):695–720. [Google Scholar]
- 37.Gould RA, Buckminster S, Pollack MH, Otto MW, Yap L. Cognitive-behavioral and pharmacological treatment for social phobia: A meta-analysis. Clinical Psychology: Science and Practice. 1997;4(4):291–306. [Google Scholar]
- 38.Ruhmland M, Margraf J. Effektivität psychologischer Therapien von Panik und Agoraphobie: Meta-Analysen auf Störungsebene. = Efficacy of psychological treatments for panic and agoraphobia. Verhaltenstherapie. 2001;11(1):41–53. [Google Scholar]
- 39.Powers MB, Sigmarsson SR, Emmelkamp PMG. A meta-analytic review of psychological treatments for social anxiety disorder. International Journal of Cognitive Therapy. 2008;1(2):94–113. [Google Scholar]
- 40.Taylor S. Meta-analysis of cognitive-behavioral treatment for social phobia. Journal of Behavior Therapy and Experimental Psychiatry. 1996;27(1):1–9. [DOI] [PubMed] [Google Scholar]
- 41.Morgan H, Raffle C. Does reducing safety behaviors improve treatment response in patients with social phobia? Australian and New Zealand Journal of Psychiatry. 1999;33(4):503–10. doi: 10.1080/j.1440-1614.1999.00599.x [DOI] [PubMed] [Google Scholar]
- 42.Kim E-J. The effect of the decreased safety behaviors on anxiety and negative thoughts in social phobics. Journal of Anxiety Disorders. 2005;19(1):69–86. doi: 10.1016/j.janxdis.2003.11.002 [DOI] [PubMed] [Google Scholar]
- 43.De Castella K, Goldin P, Jazaieri H, Heimberg RG, Dweck CS, Gross JJ. Emotion beliefs and cognitive behavioural therapy for social anxiety disorder. Cognitive Behaviour Therapy. 2015;44(2):128–41. doi: 10.1080/16506073.2014.974665 [DOI] [PubMed] [Google Scholar]
- 44.Hudson JL, Keers R, Roberts S, Coleman JRI, Breen G, Arendt K, et al. Clinical predictors of response to cognitive-behavioral therapy in pediatric anxiety disorders: The Genes for Treatment (GxT) study. Journal of the American Academy of Child & Adolescent Psychiatry. 2015;54(6):454–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Clark LA, Watson D. Editorial: Distress and fear disorders: an alternative empirically based taxonomy of the 'mood' and 'anxiety' disorders. The British Journal of Psychiatry. 2006;189(6):481–3. [DOI] [PubMed] [Google Scholar]
- 46.Craske MG, Rauch SL, Ursano R, Prenoveau J, Pine DS, Zinbarg RE. What is anxiety disorder? Depression and Anxiety. 2009;26(12):1066–85. doi: 10.1002/da.20633 [DOI] [PubMed] [Google Scholar]
- 47.Becker ES, Türke V, Neumer S, Soeder U, Krause P, Margraf J. Incidence and prevalence rates of mental disorders in a community sample of young women: results of the “Dresden study” In: Heeb-Erler G, Manz R, Kirch W, editors. Public Health Research and Practice: Report of the Public Health Research Association Saxony Regensburg: Roderer; 2000. p. 259–92. [Google Scholar]
- 48.Trumpf J, Vriends N, Meyer AH, Becker ES, Neumer S-P, Margraf J. The Dresden Predictor Study of anxiety and depression: Objectives, design, and methods. Social Psychiatry and Psychiatric Epidemiology. 2010;45(9):853–64. doi: 10.1007/s00127-009-0133-2 [DOI] [PubMed] [Google Scholar]
- 49.Rudaz M, Becker ES, Margraf J, Ledermann T, Meyer AH, Craske MG . Dysfunctional Attitudes and Anxiety Sensitivity in the Manifestation and First Onset of Social Anxiety Disorder versus Specific Phobia and Healthy: A Prospective Longitudinal Study. Psychology. 2016;7(14):1810. [Google Scholar]
- 50.Rudaz M, Craske MG, Becker ES, Ledermann T, Margraf J. Health anxiety and fear of fear in panic disorder and agoraphobia vs. social phobia: A prospective longitudinal study. Depression and Anxiety. 2010;27(4):404–11. doi: 10.1002/da.20645 [DOI] [PubMed] [Google Scholar]
- 51.Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime Prevalence and Age-of-Onset Distributions of DSM-IV Disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62(6):593–602. doi: 10.1001/archpsyc.62.6.593 [DOI] [PubMed] [Google Scholar]
- 52.Bijl RV, Ravelli A, van Zessen G. Prevalence of psychiatric disorder in the general population: Results of the Netherlands Mental Health Survey and Incidence Study (NEMESIS). Social Psychiatry and Psychiatric Epidemiology. 1998;33(12):587–95. [DOI] [PubMed] [Google Scholar]
- 53.DiNardo PA, Brown TA, Barlow DH. Anxiety Disorders Interview Schedule for DSM-IV: Lifetime version (ADIS-IV-I). Albany, New York: Graywind Publications; 1995. [Google Scholar]
- 54.Margraf J, Schneider S, Soeder U, Neumer S, Becker ES. F–DIPS: Diagnostisches Interview bei Psychischen Störungen (Forschungsversion) [Diagnostic Interview for Psychological Disorders (Research version)]. Berlin: Springer; 1996. [Google Scholar]
- 55.Association AP. Diagnostic and statistical manual of mental disorders (DSM-IV). Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- 56.Suppiger A, In-Albon T, Herren C, Bader K, Schneider S, Margraf J. Reliabilität des diagnostischen interviews bei psychischen störungen (DIPS für DSM-IV-TR) unter klinischen routinebedingungen. = Reliability of the structured diagnostic interview for mental disorders (DIPS for DSM-IV-TR) in clinical routine. Verhaltenstherapie. 2008;18(4):237–44. [Google Scholar]
- 57.Schneider S, Margraf J, Spörkel H, Franzen U. Therapiebezogene Diagnostik: Reliabilität des Diagnostischen Interviews bei psychischen Störungen (DIPS). = Therapy-related diagnosis: Reliability of the Diagnostic Interview for Mental Disorders (DIMD). Diagnostica. 1992;38(3):209–27. [Google Scholar]
- 58.In-Albon T, Suppiger A, Schlup B, Wendler S, Margraf J, Schneider S. Validität des Diagnostischen Interviews bei psychischen Störungen (DIPS für DSM-IV-TR). = Validity of the 'Diagnostisches Interview bei psychischen Störungen' (DIPS für DSM-IV-TR). Zeitschrift für Klinische Psychologie und Psychotherapie: Forschung und Praxis. 2008;37(1):33–42. [Google Scholar]
- 59.Margraf J, Schneider S, Spörkel H. Therapiebezogene Diagnostik: Validität des Diagnostischen Interviews für psychische Störungen (DIPS). = Therapy-oriented diagnosis: The validity of the Diagnostic Interview for Mental Disorders (DIMD). Verhaltenstherapie. 1991;1(2):110–9. [Google Scholar]
- 60.Suppiger A, In-Albon T, Hendriksen S, Hermann E, Margraf J, Schneider S. Acceptance of structured diagnostic interviews for mental disorders in clinical practice and research settings. Behavior Therapy. 2009;40(3):272–9. doi: 10.1016/j.beth.2008.07.002 [DOI] [PubMed] [Google Scholar]
- 61.Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: Psychometric properties. Journal of Consulting and Clinical Psychology. 1988;56(6):893–7. [DOI] [PubMed] [Google Scholar]
- 62.Margraf J, Ehlers A. BAI: Beck Angst-Inventar. Manual. Deutsche Bearbeitung [BAI: Beck Anxiety Inventory. Manual. German Adaptation]. Frankfurt am Main: Harcourt Test Services GmbH; 2007. [Google Scholar]
- 63.Cohen J. Statistical power analysis for the behavioral sciences (2nd ed.). Hillsdale, NJ: Erlbaum; 1988. [Google Scholar]
- 64.Faul F, Erdfelder E, Lang A-G, Buchner A. GPower 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavior Research Methods. 2007;39(2):175–91. [DOI] [PubMed] [Google Scholar]
- 65.Aiken LS, West SG. Multiple regression: Testing and interpreting interactions. Thousand Oaks, CA, US: Sage Publications, Inc; 1991. [Google Scholar]
- 66.Johnson PO, Neyman J. Tests of certain linear hypotheses and their application to some educational problems. Statistical Research Memoirs. 1936;1:57–93. [Google Scholar]
- 67.Bögels SM, Mansell W. Attention processes in the maintenance and treatment of social phobia: Hypervigilance, avoidance and self-focused attention. Clinical Psychology Review. 2004;24(7):827–56. doi: 10.1016/j.cpr.2004.06.005 [DOI] [PubMed] [Google Scholar]
- 68.Clark DM, McManus F. Information processing in social phobia. Biological Psychiatry. 2002;51(1):92–100. [DOI] [PubMed] [Google Scholar]
- 69.Hirsch CR, Clark DM. Information-processing bias in social phobia. Clinical Psychology Review. 2004;24(7):799–825. doi: 10.1016/j.cpr.2004.07.005 [DOI] [PubMed] [Google Scholar]
- 70.Taylor CT, Cross K, Amir N. Attentional control moderates the relationship between social anxiety symptoms and attentional disengagement from threatening information. Journal of Behavior Therapy and Experimental Psychiatry. 2016;50:68–76. doi: 10.1016/j.jbtep.2015.05.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Vanden Bogaerde A, De Raedt R. The moderational role of anxiety sensitivity in flight phobia. Journal of Anxiety Disorders. 2011;25(3):422–6. doi: 10.1016/j.janxdis.2010.11.005 [DOI] [PubMed] [Google Scholar]
- 72.Beesdo‐Baum K, Knappe S, Fehm L, Höfler M, Lieb R, Hofmann SG, et al. The natural course of social anxiety disorder among adolescents and young adults. Acta Psychiatrica Scandinavica. 2012;126(6):411–25. doi: 10.1111/j.1600-0447.2012.01886.x [DOI] [PubMed] [Google Scholar]
- 73.Hendriks SM, Spijker J, Licht CMM, Beekman ATF, Penninx BWJH. Two‐year course of anxiety disorders: Different across disorders or dimensions? Acta Psychiatrica Scandinavica. 2013;128(3):212–21. doi: 10.1111/acps.12024 [DOI] [PubMed] [Google Scholar]
- 74.Wittchen H-U, Lieb R, Pfister H, Schuster P. The waxing and waning of mental disorders: Evaluating the stability of syndromes of mental disorders in the population. Comprehensive Psychiatry. 2000;41(2, Suppl 1):122–32. [DOI] [PubMed] [Google Scholar]
- 75.Gloster AT, Richard DCS, Himle J, Koch E, Anson H, Lokers L, et al. Accuracy of retrospective memory and covariation estimation in patients with obsessive-compulsive disorder. Behaviour Research and Therapy. 2008;46(5):642–55. doi: 10.1016/j.brat.2008.02.010 [DOI] [PubMed] [Google Scholar]
- 76.Marks M, Hemsley D. Retrospective versus prospective self-rating of anxiety symptoms and cognitions. Journal of Anxiety Disorders. 1999;13(5):463–72. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(XLSX)
(XLSX)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.