Abstract
BACKGROUND
The purpose of this study was to identify risk factors and outcome implications for 30-day hospital readmission in lung transplant recipients.
METHODS
We conducted a retrospective cohort study of lung transplant cases from a single, high-volume lung transplant program between January 2000 and March 2012. Demographic and health data were reviewed for all patients. Risk factors for 30-day readmission (defined as readmission within 30 days of discharge from index lung transplant hospitalization) were modeled using logistic regression, with selection of parameters by backward elimination.
RESULTS
The sample comprised 795 patients after excluding scheduled readmissions and in-hospital deaths. Overall 30-day readmission rate was 45.4% (n = 361). Readmission rates were similar across different diagnosis categories and procedure types. By univariate analysis, post-operative complications that predisposed to 30-day readmission included pneumonia, any infection, and atrial fibrillation (all p < 0.05). In the final multivariate model, occurrence of any post-transplant complication was the most significant risk factor for 30-day readmission (odds ratio = 1.764; 95% confidence interval, 1.259–2.470). Even for patients with no documented perioperative complication, readmission rates were still > 35%. Kaplan-Meier analysis and multi-variate regression modeling to assess readmission as a predictor of long-term outcomes showed that 30-day readmission was not a significant predictor of worse survival in lung recipients.
CONCLUSIONS
Occurrence of at least 1 post-transplant complication increases risk for 30-day readmission in lung transplant recipients. In this patient population, 30-day readmission does not predispose to adverse long-term survival. Quality indicators other than 30-day readmission may be needed to assess hospitals that perform lung transplantation.
Keywords: readmission, lung transplantation, clinical outcomes, transplantation, health economics
It is estimated that overall hospital 30-day readmission rates are 20% to 25%, with associated costs of nearly $17.4 billion annually.1–3 The US Centers for Medicare and Medicaid Services has identified 30-day readmission as a major indicator of clinical quality and cost-effectiveness, and readmission rates have become a major target for health care improvement under the Patient Protection and Affordable Care Act.2 In October 2012, the first set of 30-day readmission benchmarks were established for 3 conditions with an estimated average penalty of up to $125,000 to be levied on hospitals within the first year.4 Data on 30-day readmission rates suggest that typical readmission rates vary considerably by condition and by medical specialty. In a 2012 study looking at readmission rates after percutaneous coronary intervention, the authors noted 30-day readmission rates of 4.6%.5 Studies have described readmission rates of 18% after treatment for acute myocardial infarction, 23% after complex vascular surgery procedures, and 16.5% after revascularization procedures for coronary artery disease.6–8 These differing readmission rates reflect the varying characteristics and clinical needs of patients with different medical conditions. As benchmark rates for 30-day readmission are extended to hospitalization for other medical conditions, it will be imperative that expectations reflect the realities of clinical care to ensure that clinicians are not inappropriately incentivized or penalized when assessing patients for readmission.
Lung transplant recipients represent a unique patient population, and several important factors affect the clinical course and discharge considerations in these patients. First, the considerable degree of functional disability of many of these patients and the complexity of the surgical procedure required for treatment complicate the postoperative management of lung transplant recipients. Additionally, the intricacies involved with optimizing immunosuppression regimens—along with the accompanying susceptibility to infection—mean that management of these patients often requires prolonged and/or repeated trials to ensure adequate pharmacologic protection. Considering these factors, lung transplant recipients are bound to have readmission rates that differ from observed rates after other surgical procedures. The purpose of this study was to identify the rate, risk factors, and outcome implications for 30-day hospital readmission in lung transplant recipients.
Methods
Study design and patient population
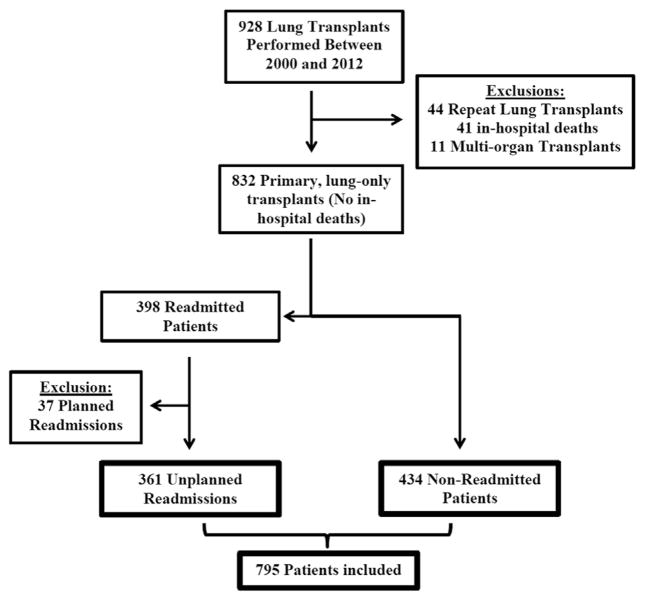
This study was designed as a retrospective cohort analysis of lung transplant cases at a single high-volume center from January 1, 2000, to March 1, 2012. The study protocol was approved by the institutional review board. Records were included in the study based on receipt of lung allografts before March 2012 and on availability of demographic and outcome data in the perioperative period. As demonstrated in Figure 1, exclusion criteria included retransplantation, multi-organ transplantation, and in-hospital death during the initial hospitalization. Patients were excluded from final risk factor analysis if readmission was planned as part of post-operative management (e.g., readmission for fundoplication after lung transplant).
Figure 1.
STROBE (STrengthening the Reporting of OBservational studies in Epidemiology) diagram of the study population—patients who were discharged after primary lung-only transplant without scheduled readmission.
Data sources
Our institution maintains an enterprise data warehouse containing patient-specific and encounter-specific information that is accessible to investigators. Available data include clinical and administrative information generated during patient care.9 Data on comorbidities existing at the time of transplant were obtained, along with information on patient demographics, operative characteristics, and post-operative complications. We also collected survival and other outcome data related to individual patient records. Finally, we collected data on total encounter charges and on International Classification of Diseases, Ninth Revision, codes associated with readmission episodes to characterize the financial costs of readmission as well as the reasons for rehospitalization. These data were validated, supplemented, and cross-referenced with manual chart review and with data obtained from our institutional database for cardiovascular disease. Additional information was obtained from site-specific reports provided through the United Network for Organ Sharing. Survival data were cross-referenced with tumor registries and with the Social Security Death Index, providing for increased reliability of outcome data, particularly in situations where patients may have been lost to follow-up at our center.
Identification of readmission in administrative data
To identify the index readmission episode, each patient record was linked to our institutional data warehouse to search for readmissions that occurred within 30 days of post-transplant discharge. Records were excluded if readmission was planned—for example, as follow up for performance of a fundoplication procedure. Any available information on reason for admission was obtained from the associated readmission encounter record. Additionally, charge data reflecting the total dollars associated with each readmission encounter were obtained from our hospital system financial analysts.
Statistical analysis
All statistical analyses were carried out using SAS version 9.2 (SAS Institute Inc., Cary, NC). Unadjusted analysis of associations between study variables and early readmission was performed using the chi-square test if the variable was categorical and using Student’s t-test if the variable was continuous. Logistic regression models were employed for multi-variate analysis of relationships between study variables and occurrence of readmission. The short-term complication variables associated with early readmission at p < 0.20 were entered into a multivariable model. Parameter selection for final regression models was performed by backward elimination, and a retention criterion of p < 0.05 was used to identify candidate variables for our prediction model. Kaplan-Meier and log-rank hazard ratio analyses were performed to assess the relationship between readmission and survival.
Results
Demographics
Between January 2000 and March 2012, 874 primary lung transplant procedures were performed at our center. After excluding patients because of in-hospital death, repeat transplantation, and multi-organ transplantation, 832 patients were left in the sample. Total 30-day readmission rate including planned and unplanned readmissions was 47.8% (n = 398). Further exclusion to account for scheduled readmission left 795 patients in the final sample for analysis. The overall rate of unplanned readmission at 30 days was 45.4% (n = 361). The demographics and procedure characteristics for the study population are shown in Table 1. Rates of the most common long-term and short-term outcomes are shown in Table 2. Age, underlying diagnosis, lung allocation score, and transplant procedure (single vs double) were not significantly associated with differential risk for unscheduled readmission. Similarly, length of stay during the initial hospitalization did not differ between readmitted and non-readmitted populations. Patient sex showed a trend toward significance with a higher proportion of female patients in the readmission group. However, this relationship did not achieve statistical significance at the 5% level.
Table 1.
Patient Characteristics
| Characteristic | Overall, N (%) or mean (SD) | No readmission, n (%) or mean (SD) | Readmission, n (%) or mean (SD) | p-valuea |
|---|---|---|---|---|
| Demographics and donor factors | ||||
| Patients (%) | 795 (100.0) | 434 (54.6) | 361 (45.4) | |
| Age of recipient, years (SD) | 52.9 (15.0) | 52.8 (15.2) | 53.0 (14.8) | 0.7163 |
| Age of donor, years (SD) | 34.5 (15.4) | 34.9 (15.3) | 34.0 (15.4) | 0.4048 |
| Female sex (%) | 323 (40.6) | 166 (38.2) | 157 (43.4) | 0.1341 |
| White race (%) | 699 (87.9) | 382 (88.0) | 317 (87.8) | 0.9982 |
| Diagnosis (%) | 0.7345 | |||
| Obstructive disease | 255 (32.0) | 135 (31.1) | 120 (33.2) | |
| Restrictive disease | 352 (44.2) | 195 (44.9) | 157 (43.4) | |
| CF/bronchiectasis | 137 (17.2) | 75 (17.2) | 62 (17.1) | |
| Primary pulmonary hypertension | 14 (1.7) | 6 (1.3) | 8 (2.2) | |
| Other | 37 (4.6) | 23 (5.3) | 14 (3.8) | |
| Ischemic time, hours (SD) | 6.5 (1.7) | 6.6 (1.8) | 6.4 (1.7) | 0.2199 |
| No. unknown | 182 | |||
| End match LAS (SD) | 47.6 (16.5) | 47.9 (16.9) | 47.2 (15.9) | 0.6052 |
| No. unknown | 288 | |||
| Pre-existing comorbidities | ||||
| BMI (SD) | 23.5 (4.0) | 23.4 (4.1) | 23.8 (4.0) | 0.2215 |
| No. unknown | 101 | |||
| Diabetes mellitus (%) | 129 (16.2) | 66 (15.2) | 63 (17.4) | 0.3928 |
| COPD (%) | 305 (38.3) | 171 (39.4) | 134 (37.1) | 0.5103 |
| CHF (%) | 59 (7.4) | 28 (6.4) | 31 (8.5) | 0.2527 |
| CAD (%) | 216 (27.1) | 114 (26.2) | 102 (28.2) | 0.5308 |
| Atrial fibrillation (%) | 51 (6.4) | 26 (5.9) | 25 (5.9) | 0.5924 |
| PVD (%) | 19 (2.3) | 11 (2.5) | 8 (2.2) | 0.7699 |
| Operative and post-operative factors | ||||
| Bilateral transplant (%) | 680 (85.5) | 367 (84.5) | 313 (86.7) | 0.3928 |
| Cardiopulmonary bypass (%) | 96 (18.7) | 51 (18.0) | 45 (19.7) | 0.6216 |
| No. unknown | 284 | |||
| Post-operative LOS (SD) | 21.8 (26.3) | 22.3 (28.7) | 21.2 (23.3) | 0.5514 |
| No. unknown | 9 | |||
| ICU days (SD) | 8.00 (1.9) | 8.04 (1.2) | 7.9 (11.4) | 0.9325 |
BMI, body mass index; CAD, coronary artery disease; CF, cystic fibrosis; CHF, congestive heart failure; COPD, chronic obstructive pulmonary disease; ICU, intensive care unit; LAS, lung allocation score; LOS, length of stay; PVD, peripheral vascular disease.
Chi-square or t-test.
Table 2.
Patient Outcomes
| Characteristic | Overall, N (%) | No Readmission, n (%) | Readmission, n (%) | p-valuea |
|---|---|---|---|---|
| Post-operative complications (short-term) | ||||
| Acute rental failure | 103 (12.9) | 59 (13.6) | 44 (12.1) | 0.5483 |
| Any infection | 381 (47.9) | 131 (44.0) | 190 (52.6) | 0.0154b |
| Atrial fibrillation | 263 (33.0) | 130 (29.9) | 133 (36.8) | 0.0399b |
| Pneumonia | 241 (30.3) | 114 (26.2) | 127 (35.1) | 0.0065b |
| Pulmonary embolism | 25 (3.1) | 10 (2.3) | 15 (4.1) | 0.1365 |
| Sepsis | 79 (9.9) | 50 (11.5) | 29 (8.0) | 0.1017 |
| Stroke | 25 (3.1) | 18 (4.1) | 7 (1.9) | 0.0757 |
| Any complication | 597 (75.0) | 308 (70.9) | 289 (80.0) | 0.0032b |
| Long-term complications | ||||
| Mortality | ||||
| 1-year (n = 688) | 70 (10.1) | 39 (10.6) | 31 (9.6) | 0.6936 |
| 3-year (n = 525) | 144 (27.3) | 73 (26.6) | 71 (28.2) | 0.6731 |
| 5-year (n = 433) | 199 (45.9) | 98 (44.3) | 101 (47.6) | 0.4910 |
| Dialysis | 96 (12.0) | 45 (10.3) | 51 (14.1) | 0.1054 |
| CKD3+ (6 months) | 509 (68.6) | 251 (63.5) | 258 (74.3) | 0.0016b |
| No. unknown | 53 | |||
| Non-skin malignancy | 189 (23.7) | 98 (22.5) | 91 (25.2) | 0.3863 |
CKD3+, chronic kidney disease stage 3 or worse.
Chi-square or t-test. Statistically significant at 5% level.
Statistically significant at the 5% level.
Reason for readmission
Each readmission episode was associated with several International Classification of Diseases, Ninth Revision, diagnosis codes. The “primary” readmission diagnosis was often described using non-specific diagnosis codes, such as 996.84 for “Complication of transplanted lung” (76.3%) and V42.6 for “Lung replaced by transplant” (67.2%). Looking only at the more specific codes, pleural effusion (35.6%), diabetes mellitus (34.7%), atrial fibrillation (23.7%), pneumonia (23.15), and shortness of breath (22.2%) were the most common reasons for readmission. Table 3 provides a complete list of diagnoses that are associated with at least 10% of unplanned readmissions.
Table 3.
Readmission Diagnoses Present in ≥10% of Rehospitalized Patients
| Reason for readmission | ICD-9 code | n | % |
|---|---|---|---|
| Complications of transplanted lung | 996.84 | 360 | 76.3 |
| Lung replaced by transplant | V42.6 | 317 | 67.2 |
| Surgical operation with transplant of whole organ causing abnormal patient reaction, or later complication, without mention of misadventure at time of operation | E878.0 | 274 | 58.1 |
| Esophageal reflux | 530.81 | 184 | 39.0 |
| Unspecified pleural effusion | 511.9 | 168 | 35.6 |
| Diabetes mellitus without mention of complication, type II or unspecified type, not stated as uncontrolled | 250.00 | 164 | 34.7 |
| Long-term (current) use of other medications | V58.69 | 117 | 24.8 |
| Atrial fibrillation | 427.31 | 112 | 23.7 |
| Pneumonia, organism unspecified | 486 | 109 | 23.1 |
| Shortness of breath | 786.05 | 105 | 22.2 |
| Other dyspnea and respiratory abnormality | 786.09 | 105 | 22.2 |
| Unspecified essential hypertension | 401.9 | 102 | 21.6 |
| Encounter for therapeutic drug monitoring | V58.83 | 92 | 19.5 |
| Anemia, unspecified | 285.9 | 84 | 17.8 |
| Cystic fibrosis without mention of meconium ileus | 277.00 | 67 | 14.2 |
| Other and unspecified hyperlipidemia | 272.4 | 64 | 13.6 |
| Other specified disorders of pancreatic internal secretion | 251.8 | 62 | 13.1 |
| Coronary atherosclerosis of native coronary vessel | 414.01 | 61 | 12.9 |
| Acute kidney failure, unspecified | 584.9 | 57 | 12.1 |
| Personal history of tobacco use, presenting hazards to health | V15.82 | 54 | 11.4 |
| Anxiety state, unspecified | 300.00 | 52 | 11.0 |
| Hypoxemia | 799.02 | 52 | 11.0 |
| Acute respiratory failure | 518.81 | 51 | 10.8 |
| Adrenal cortical steroids causing adverse effects in therapeutic use | E932.0 | 51 | 10.8 |
| Long-term (current) use of insulin | V58.67 | 49 | 10.4 |
| Hyperpotassemia | 276.7 | 48 | 10.2% |
ICD-9, International Classification of Diseases, Ninth Revision.
Recipient comorbidities
Of several comorbidities considered as determinants of readmission, none were found to be a significant predictor of unplanned rehospitalization. These comorbidities included diabetes mellitus (n = 129), chronic obstructive pulmonary disease (n = 305), congestive heart failure (n = 59), coronary artery disease (n = 16), atrial fibrillation (n = 51), and peripheral vascular disease (n = 19).
Complications
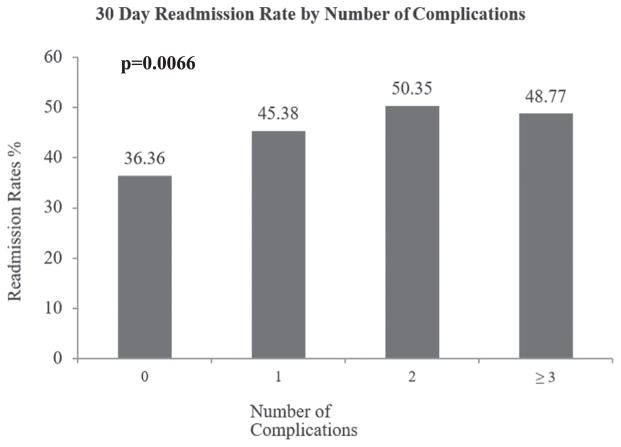
Rates of various complications are shown in Table 2. Table 4 shows results from univariate logistic regression looking at post-operative complications as predictors of readmission. Significantly increased rates of readmission were observed among patients with post-operative pneumonia (p = 0.007), atrial fibrillation (p = 0.040), or infection of any kind (p = 0.016). Sepsis, pulmonary embolism, and stroke in the post-operative period showed trends toward significance but were not contributors at the 5% level. An aggregate variable was created to represent the number of complications experienced by any given patient. Of the sample, 75% (n = 597) had at least 1 complication. Unadjusted logistic regression identified occurrence of at least 1 post-operative complication as a significant predictor of readmission (p = 0.003). Readmission risk was 1.6 times greater for patients with at least 1 complication compared with patients with no complications (95% confidence interval [CI], 1.2–2.3). Figure 2 shows the rate of readmission by number of complications experienced by each patient. Overall, there is a statistically significant increase in the readmission rate with increasing number of complications (Cochran-Armitage trend test: 2-sided p = 0.0066).
Table 4.
Unadjusted Associations Between Complications and Early Readmissiona
| Complication | n | % readmitted | p-value | OR (95% CI) |
|---|---|---|---|---|
| Pneumonia | 241 | 52.7 | 0.0066b | 1.523 (1.124–2.065) |
| Sepsis | 79 | 36.7 | 0.1034 | 0.671 (0.415–1.085) |
| Any infection | 381 | 49.8 | 0.0155b | 1.414 (1.068–1.871) |
| Pulmonary embolism | 25 | 60.0 | 0.1420 | 1.838 (0.816–4.143) |
| Stroke | 25 | 28.0 | 0.0827 | 0.457 (0.189–1.107) |
| Atrial fibrillation | 263 | 50.0 | 0.0401b | 1.364 (1.014–1.835) |
| Any complication | 597 | 48.4 | 0.0033b | 1.642 (1.179–2.286) |
CI, confidence interval; OR, odds ratio.
For p ≤ 0.20.
Significant at 5% level.
Figure 2.
Readmission rate stratified by total number of complications in each patient. Bar graph demonstrates a significant increase in readmission rate with increasing number of complications (Cochran-Armitage trend test: 2-sided p = 0.0066).
Results from multivariate models controlling for demographic factors, comorbidities, and complications are reported in Table 5. All characteristics that generated p < 0.20 on univariate analysis were considered for inclusion in the final model. Post-operative sepsis (odd ratio [OR] = 0.576; 95% CI, 0.353–0.938) and occurrence of any complication (OR = 1.764; 95% CI, 1.259–2.470) both came out of the adjusted model as significant predictors of readmission at 30 days.
Table 5.
Multivariate Logistic Regression Model of Complications Associated With Readmission
| Complication | Adjusted OR (95% CI) | p-value |
|---|---|---|
| Complication ≥ 1 | 1.764 (1.259–2.470) | 0.0010 |
| Sepsis | 0.576 (0.353–0.938) | 0.0268 |
| Pneumoniaa | ||
| Any infectiona | ||
| Pulmonary embolisma | ||
| Strokea | ||
| Atrial fibrillationa |
CI, confidence interval; OR, odds ratio.
Removed from final model (by backward elimination).
Long-term outcomes
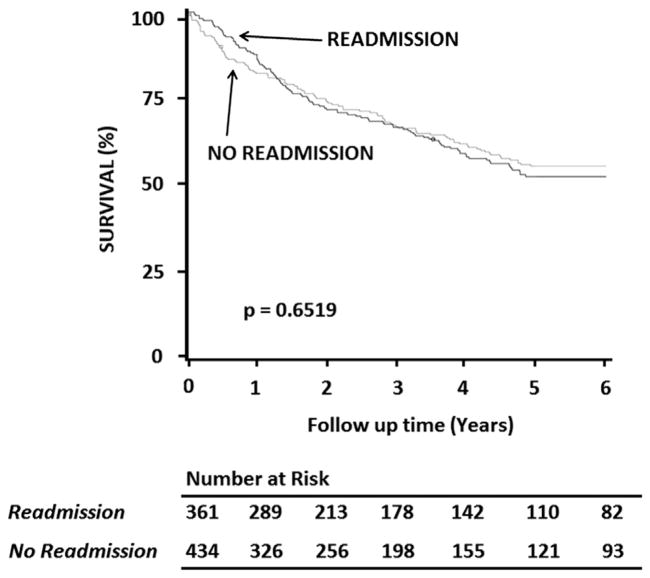
On univariate analysis, readmission status was identified as a predictor of chronic kidney disease at 6 months (OR = 1.7; 95% CI, 1.2–2.3) but not as a predictor of mortality. Kaplan-Meier survival analysis presented in Figure 3 provides further confirmation of the non-discriminatory effect of readmission status as a predictor of patient survival. Multi-variate regression models were created to look at the effect of readmission status on predicting the occurrence of chronic kidney disease. Characteristics identified in previous analyses as predictors of these long-term outcomes—age at transplant, procedure type, sex, congestive heart failure, peripheral vascular disease, ischemic time, and donor age—were included in the model. Final results demonstrate that readmitted patients are 1.734 times more likely to develop clinically significant chronic kidney disease (stage 3 or worse) at 6 months (95% CI, 1.181–2.546). The 30-day readmission cohort had a statistically increased number of readmissions within 1 year after index hospitalization discharge relative to the cohort that did not have a readmission within 30 days (3.6 vs 2.1, p < 0.001).
Figure 3.
Kaplan-Meier analysis of survival to 5 years, stratified by readmission status. There is no difference in survival between patients who were readmitted early and patients who were not.
Charges associated with readmission
We analyzed data on the total charge billed to each patient for services provided during readmission episodes. Analysis was limited to readmission encounters related to transplants performed in 2010 and 2011. The charges for each readmission episode represent the overall cost to patients and to the US health care system for unplanned readmissions. The average readmitted patient was charged approximately $200,000 for services provided during the readmission episode. This cost is in addition to an average index hospitalization cost of $402,000. In comparison, the average index hospitalization cost for patients without readmission was $488,000. Between 2010 and 2011, 230 lung transplant procedures were performed at our center with 99 unscheduled readmissions.
Discussion
This study assessing rates, predictors, and implications of 30-day readmission in lung transplant recipients highlights several important factors affecting rehospitalization in this patient population. We observed a rate of unplanned readmission of 45.4% in lung recipients, considerably higher than rates observed in other patient populations. As described earlier, several factors contribute to this high rate of readmission, including infection, complications with the lung allograft, and problems related to immunosuppression. Additionally, our finding that readmission is more common for patients with post-transplant complications suggests that clinical and surgical difficulties after surgery are major contributors to increased readmission rates in this population. This finding is in accordance with other studies that have identified post-transplant complications as a major predictor of 30-day readmission after surgical procedures.1,7,8,10 In the United States, 30-day readmission is a well-examined end-point specifically by the Centers for Medicare and Medicaid Services. Since the passage of the Patient Protection and Affordable Care Act, the federal law requiring all citizens to possess health insurance, hospitals are now being penalized for high 30-day readmission rates.4 However, our results suggest that 30-day readmission may not be the best end-point for quality improvement in lung transplantation.
Understanding the effect of post-operative complications on 30-day readmission rates presents an important opportunity for improving on high rates of rehospitalization in lung transplant populations. Given the unique considerations for transplant patients, it is unlikely that readmission rates will ever be as low as they are in other clinical specialties, and it is even less likely that readmission will be eliminated completely. However, developing strategies to minimize post-operative complications will help reduce readmission rates. Our study identified specific post-operative complications that are associated with high rates of readmission, including infection, pulmonary embolism, stroke, and atrial fibrillation. Peri-operative interventions to reduce these complications will be important as we work toward minimizing early readmission in health care. Controlled clinical studies of appropriate peri-operative infection, deep vein thrombosis, and atrial fibrillation prophylaxis could lead to dramatic decreases in early readmission after lung transplantation.
Enhanced patient education, treatment, and health care provider outpatient follow-up aimed at particularly high-risk complications may also lead to decreased readmission rates. In this study, we identified several diagnoses that are most commonly associated with readmission in lung transplant populations. Patients often return for clinical management of conditions such as diabetes mellitus, pleural effusion, atrial fibrillation, and pneumonia. These and other associated diagnoses present additional opportunities for health care providers in the field of lung transplantation to intervene and prevent early readmission in their patients. Appropriate clinical management after discharge will be essential for detecting these conditions early on, before they deteriorate to the point of requiring hospital admission. Coordination with other providers, including endocrinologists, cardiologists, and infectious disease specialists, assisting in the care of lung transplant patients will be an essential part of achieving this goal.
We did not observe a significant association between readmission rates and mortality. This finding is important not because it negates the importance of readmission rates, but because it highlights a potential disconnect between priorities of clinicians and priorities of health systems. In US health care, 30-day readmission rates have been identified as a system-wide marker of quality of care.11 Part of this shift in emphasis is attributable to the fact that early readmission is associated with increasing health care costs. In our patient population, the average readmission episode is associated with patient charges of nearly $200,000 per episode. This adds up to slightly less than $20 million for the 99 unplanned readmissions that occurred over the 2-year time period of our financial data analysis. Although the index hospitalization was on average less expensive for readmitted patients, the high cost associated with the readmission episode wipes away any financial gains that may have been made from a cheaper initial hospital stay. Large dollar amounts could be saved if some of these readmission episodes were prevented.
Even with such striking findings from financial analysis, the lack of correlation between 30-day readmission and outcomes that are traditionally valued in medicine—such as mortality—suggests that providers may be providing “quality” care for patients, but that these kinds of patients may require more frequent inpatient health care. Overall, this is indicative of the need for widespread education to align the priorities of physicians with the priorities of health industry leaders interested in controlling health care costs. Thus, this study may also suggest that a 30-day readmission rate is an inappropriate barometer for quality of care in highly specialized areas of medicine such as lung transplantation. Perhaps 30-day readmission is not a marker of bad quality, but rather good quality in terms of ability to rescue and achieve equivalent outcomes. This study also highlights the need for other quality indicators, such as the failure to rescue which refers to the occurrence of preventable adverse events. In this context, events that could potentially have been prevented by bringing patients back to the hospital in the early post-operative period.
This discussion leads us to consider current efforts to help providers improve the care being delivered to patients. Evidence suggests that recommendations coming from health industry leaders have failed to generate improvements in the quality of care that patients receive.2 The study by Stefan et al2 compared performance on process measures with 30-day readmission rates and found no relationship between level of performance and success at minimizing the rate of unplanned rehospitalization. The existence of such a striking disconnect underlines the need for better clinician leadership in the identification of appropriate tools for improving quality of care. Such leadership as well as additional research is needed in the lung transplant field.
In this study, we found no association between patient comorbidities and 30-day readmission. This finding is inconsistent with other studies, in which authors have observed significant relationships between specific pre-existing conditions and increased rates of 30-day readmission in surgical patients.7,12 Examples of existing comorbidities associated with early readmission include disseminated cancer, pre-operative open wound, and dyspnea. The comorbidities were not included as variables in our models because they are either less relevant to lung transplant populations (in cases of disseminated cancer and pre-operative open wound) or too intimately linked with lung pathology to provide for meaningful analysis (in the case of dyspnea). Although we do not claim to have exhausted all other possibilities for comorbidities associated with readmission, we believe that our study has covered the comorbidities that are most relevant in lung transplant recipients.
This study has some limitations. First, the observational design of our study means that there is a possibility of unmeasured factors that could be confounders of the relationships described. We have attempted to address this limitation by considering as many variables as were available to us for inclusion in our regression models. Second, our study was based on data from a single institution. This imposes sample size hindrances that limit power and increase the risk of type II error. Large, multi-institutional databases address the power problem but are of limited value in this study considering that readmission is the dependent variable of interest. Likewise, most national databases for transplant do not provide enough clinical granularity to allow investigators to accurately identify patients who were readmitted at 30 days. These limitations are important considerations for health care providers who may wish to look at our findings as they apply to their own transplant programs. However, we believe that our work provides many meaningful insights into the nature of readmission in lung transplant recipients and opportunities for improving this outcome measure. Additionally, our analysis involves a period of 12 years during which the general approach to lung transplantation has changed. Lastly, our institution is a high-volume lung transplantation center with a high case complexity, which possibly would affect our readmission rate. Despite this possibility, we believe this would not necessarily affect the risk factors of readmission.
In conclusion, as we develop a more comprehensive understanding of the factors behind early hospital readmission, we will be better equipped to cater to the needs of patients who are at greatest risk for readmission. In this study, we demonstrate that lung transplant recipients are at high risk for early readmission and that the development of any post-operative complication is the most meaningful predictor of readmission in this population. Thus, efforts to reduce rates of early readmission in this group must begin with programs to minimize complications in the peri-operative period. Additionally, special attention must be paid to at-risk groups (i.e., patients with complications) in terms of patient and family education at discharge and care coordination after discharge. Optimizing these aspects of patient care will help us identify problems before they deteriorate to the point where they require readmission.
Although we did not observe a significant relationship between early readmission and adverse long-term outcomes, we do recognize the considerable financial costs of 30-day readmission to providers and to the economy at large. To facilitate the process of cost control, it is imperative that clinical priorities be aligned with financial goals so that clinicians have natural incentives to reduce costs, while still providing high-quality care to patients. At the same time, we are limited in knowing what the outcomes would be for these complicated patients if they had not been readmitted for appropriate care. Perhaps quality-of-care metrics such as 30-day readmission rates are not feasible or clinically appropriate universally in medicine, and great care extrapolating among differing fields will be necessary.
Footnotes
Disclosure statement
Institutional funding was the primary funding source for this study. B.A.Y. and M.G.H. are supported by the National Institutes of Health–funded Cardiothoracic Surgery Trials Network Grant No. 5U01HL088953-05.
None of the authors has a financial relationship with a commercial entity that has an interest in the subject of the presented manuscript or other conflicts of interest to disclose.
References
- 1.McCormack R, Michels R, Ramos N, Hutzler L, Slover JD, Bosco JA. Thirty-day readmission rates as a measure of quality: causes of readmission after orthopedic surgeries and accuracy of administrative data. J Healthc Manag. 2013;58:64–76. discussion 77. [PubMed] [Google Scholar]
- 2.Stefan MS, Pekow PS, Nsa W, et al. Hospital performance measures and 30-day readmission rates. J Gen Intern Med. 2013;28:377–85. doi: 10.1007/s11606-012-2229-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360:1418–28. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- 4.Burke RE, Coleman EA. Interventions to decrease hospital readmissions: keys for cost-effectiveness. JAMA Intern Med. 2013:695–8. doi: 10.1001/jamainternmed.2013.171. [DOI] [PubMed] [Google Scholar]
- 5.Ricciardi MJ, Selzer F, Marroquin OC, et al. Incidence and predictors of 30-day hospital readmission rate following percutaneous coronary intervention (from the National Heart, Lung, and Blood Institute Dynamic Registry) Am J Cardiol. 2012;110:1389–96. doi: 10.1016/j.amjcard.2012.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dunlay SM, Weston SA, Killian JM, Bell MR, Jaffe AS, Roger VL. Thirty-day rehospitalizations after acute myocardial infarction: a cohort study. Ann Intern Med. 2012;157:11–8. doi: 10.7326/0003-4819-157-1-201207030-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kassin MT, Owen RM, Perez SD, et al. Risk factors for 30-day hospital readmission among general surgery patients. J Am Coll Surg. 2012;215:322–30. doi: 10.1016/j.jamcollsurg.2012.05.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.McPhee JT, Barshes NR, Ho KJ, et al. Predictive factors of 30-day unplanned readmission after lower extremity bypass. J Vasc Surg. 2013;57:955–62. doi: 10.1016/j.jvs.2012.09.077. [DOI] [PubMed] [Google Scholar]
- 9.Horvath MM, Winfield S, Evans S, Slopek S, Shang H, Ferranti J. The DEDUCE Guided Query tool: providing simplified access to clinical data for research and quality improvement. J Biomed Inform. 2011;44:266–76. doi: 10.1016/j.jbi.2010.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vigneswaran WT, Helenowski M, Bhorade SM, Lamounier F, Alex C, Garrity ER., Jr Early readmission is a predictor of overall survival following isolated lung transplantation. Int Surg. 2010:299–304. [PubMed] [Google Scholar]
- 11.Sellers MM, Merkow RP, Halverson A, et al. Validation of new readmission data in the American College of Surgeons National Surgical Quality Improvement Program. J Am Coll Surg. 2013:420–7. doi: 10.1016/j.jamcollsurg.2012.11.013. [DOI] [PubMed] [Google Scholar]
- 12.Schneider EB, Hyder O, Wolfgang CL, et al. Patient readmission and mortality after surgery for hepato-pancreato-biliary malignancies. J Am Coll Surg J Am Coll Surg. 2012;215:607–15. doi: 10.1016/j.jamcollsurg.2012.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]