Through a computerized priming task, this study captures evidence of implicit weight bias among children.
Abstract
OBJECTIVES:
Assess implicit weight bias in children 9 to 11 years old.
METHODS:
Implicit weight bias was measured in children ages 9 to 11 (N = 114) by using the Affect Misattribution Procedure. Participants were shown a test image of a child for 350 milliseconds followed by a meaningless fractal (200 milliseconds), and then they were asked to rate the fractal image as “good” or “bad.” We used 9 image pairs matched on age, race, sex, and activity but differing by weight of the child. Implicit bias was the difference between positive ratings for fractals preceded by an image of a healthy-weight child and positive ratings for fractals preceded by an image of an overweight child.
RESULTS:
On average, 64% of abstract fractals shown after pictures of healthy-weight children were rated as “good,” compared with 59% of those shown after pictures of overweight children, reflecting an overall implicit bias rate of 5.4% against overweight children (P < .001). Healthy-weight participants showed greater implicit bias than over- and underweight participants (7.9%, 1.4%, and 0.3% respectively; P = .049).
CONCLUSIONS:
Implicit bias toward overweight individuals is evident in children aged 9 to 11 years with a magnitude of implicit bias (5.4%) similar to that in studies of implicit racial bias among adults.
What’s Known on This Subject:
Weight bias has a significant impact on the quality of life of individuals with obesity. Both explicit and implicit weight bias have been identified in adults.
What This Study Adds:
This study demonstrates feasibility of identifying implicit weight bias in 9- to 11-year-old children. The level of implicit bias against children with obesity is similar to that seen for race.
Children and adolescents with obesity report significant levels of weight-related victimization, or weight stigma. This stigma is reported as coming from peers, family, teachers, health care workers, and the general public.1 Among children and adolescents, weight stigma has a major impact on quality of life.2,3 Experiencing weight stigma has been linked to many negative emotional consequences, including depression, anxiety, body dissatisfaction, and, in some individuals, increased risk for suicidal ideation.2 Furthermore, it has been found to adversely affect peer relationships and social bonding among children, academic performance, physical health outcomes, and participation in physical activity.2 It can also lead to disordered eating behaviors, such as binge eating, purging, and the use of diet pills or laxatives.2,4–6
Despite clear evidence that weight stigma is harmful, measuring bias is more difficult, and people who attempt to measure bias should consider the stigma as experienced by individuals with obesity or the bias that underlies stigmatizing behaviors. Some approaches have relied on the perception of bias and assess the individual’s own experience of perceived weight bias, such as the Stigmatizing Situations Inventory.7,8 Other measures, such as the Fat Phobia Scale 3,9,10 and FAT subscale of the Universal Measure of Bias,11 assess the individual’s attitude and opinions about individuals with obesity. These methods, however, do not capture “implicit weight bias”: an unconscious bias an individual holds toward individuals with overweight or obesity.12
Implicit bias is conceptually distinct from conscious, or explicit, bias; conscious and implicit biases are typically correlated but not identical.13 Explicit weight bias is common among adults worldwide, with individuals willing to endorse beliefs that individual blame and willpower are the cause of obesity.14 Implicit measures, unlike those that are explicit in nature, measure attitudes the individual is not aware they hold, and these may better predict behaviors that are discriminatory in nature or socially undesirable.15–20 Even in the context of widespread explicit weight bias, implicit weight bias remains critical, because both likely influence the stigma experienced by individuals with obesity. Several methods of capturing implicit bias have been used to examine bias associated with age, race, and many other factors. The study of implicit weight bias in adults has shown negative attitudes toward people with obesity, including among individuals who themselves are overweight.15,20
Children have also demonstrated significant levels of explicit weight bias.21 However, existing research is extremely limited in its examination of implicit weight bias among school-aged children. Although findings show that children do, in fact, exhibit implicit weight bias, most previous studies have used drawings rather than actual photographs of children. One such study distributed a version of the Implicit Association Test by using schematic figures developed in a study of children’s body perception and preference,21,22 whereas another showed participants a series of drawings depicting children with obesity, various disabilities, or no disability, and asked them to rank them in order of who they “liked” best.23
Although the Implicit Association Test is a commonly used measure of implicit attitudes, drawbacks include the requirement of relative measurement (eg, African American individuals versus white individuals) rather than distinct attitudes toward each and its reliance on reaction time rather than a simple judgment.24 In contrast, the Affect Misattribution Procedure (AMP) uses a priming approach by presenting an image for a brief time and asking respondents to make an assessment of a neutral image after the prime. Positive responses for each are assessed, and the difference in positive responses represents implicit bias. Previous use of the AMP has demonstrated differences in positive responses for African American faces and white faces of 5 to 9 percentage points.25
The simplicity of the task may make the AMP more appropriate for children. Additionally, the use of a wide variety of matched photographs rather than line drawings may promote assessment based more specifically on weight differences. Our objective was to determine the feasibility of administering a version of the AMP to children aged 9 to 11 years and to quantify any implicit bias toward children with overweight or obesity.
Methods
Population
This study of implicit bias was part of a larger National Institutes of Health–funded study examining how children perceive obesity-related messaging in movies. Children ages 9 to 11 were recruited by using flyers that were shared through the following methods: distributed electronically to parents of children at the 11 local public elementary schools; distributed electronically via university e-mail lists for faculty, staff, and students; and posted in locations frequented by children and their parents, such as the local public library, Young Men’s Christian Association, and pediatrics clinics.
Measures
The AMP has been previously described.26 In this implementation, participants used a computer to view first a gray screen for 500 milliseconds, then an image that is the bias target for 350 milliseconds, followed by an abstract fractal for 200 milliseconds and were then asked to rate the fractal as “good” or “bad.” Recent meta-analyses suggest that the AMP is both valid as a measure of implicit attitudes and is high in reliability, although it has not been specifically validated in children.24,27
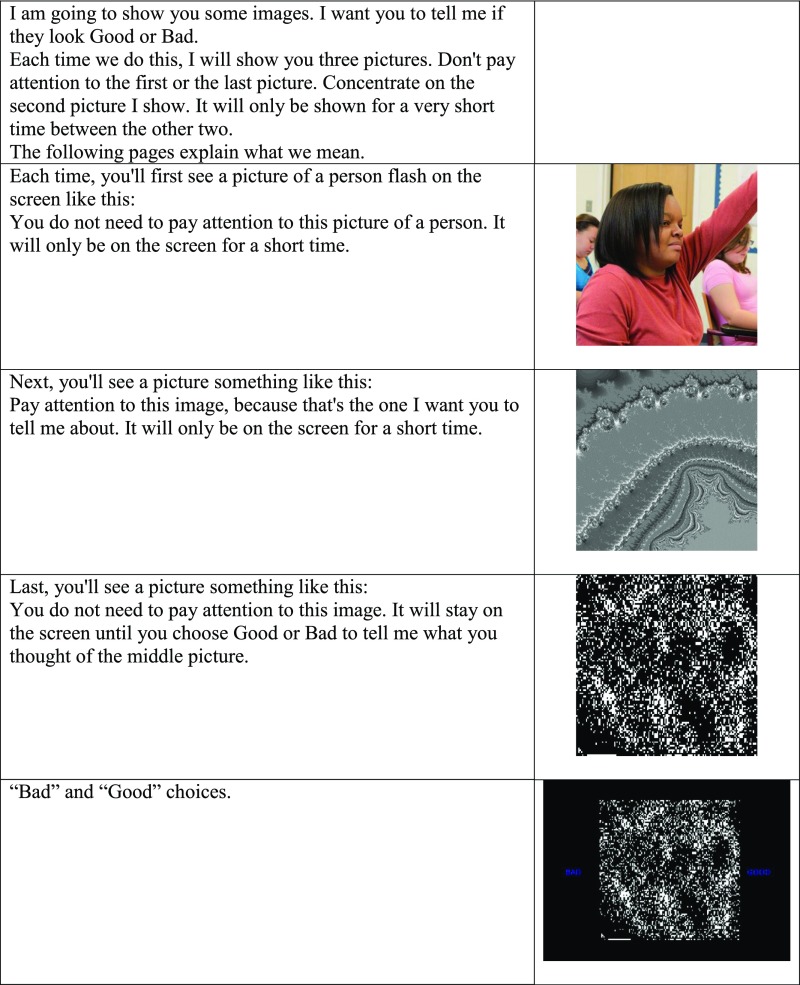
Our primary modification, guided by author K. P. (developer of the AMP), involved identifying photographs of older children and young adolescents to include in the AMP. Using freely available Internet images, we identified photos of children engaged in nonstigmatizing outdoor and educational activities, such as running, canoeing, reading, and classroom activities. We included activities that were both counter to weight-based stereotypes (eg, running) and neutral with regard weight-based stereotypes (eg, reading, standing). For each activity, a pair of images was used that matched on visually apparent characteristics of the individuals: race, ethnicity, age, and sex. Because of the use of activities as the basis for image choice, images were well matched on overall appearance (eg, life vests on children canoeing, shorts on children running). Additionally, we matched facial expressions (eg, smiling) and whether the subject was looking at the camera. We created a total of 9 pairs of images, with one in each pair depicting a child with a visual appearance of thinness, which we will refer to as the “healthy weight” image, and the second depicting a child with a visual appearance of a “larger body,” which we will refer to as the “overweight” image. Figure 1 shares the complete instructions and sample images.
FIGURE 1.
Example image and instructions for the AMP. UConn Rudd Center for Food Policy & Obesity.
Participants responded to a total of 72 trials: 8 for each pair of images. Because participants were instructed to judge a meaningless fractal, we would expect “good” and “bad” ratings to be evenly distributed across images. A significant difference between the proportion of positive ratings for fractals shown after a child at a healthy weight and the proportion of positive ratings for fractals shown after a child with overweight was considered to index implicit bias.
Procedures
As part of a larger children’s movie study, we recruited children ages 9 to 11 years to participate in a study that involved answering a set of questionnaires, watching a movie, and participating in a focus group about the movie. Before the study day, each participant completed an online survey on a computer or tablet, which they were directed to complete without a parent’s help. One portion of this survey included the AMP. All methods were approved by the institutional review board.
Statistical Methods
We used t tests to compare positive responses to fractals shown after images featuring healthy-weight children versus children with obesity. We then calculated implicit bias as the difference between the proportion of “good” ratings after the healthy weight pictures and the proportion of “good” ratings after overweight pictures, such that a higher number indicated more positive responses to healthy-weight children (and greater bias against overweight children). We used this bias measurement to assess for differences by self-reported race, age, sex, and weight categories using χ2 tests.
The study was approved by the Institutional Review Board at the University of North Carolina at Chapel Hill. Before completing the survey, parents provided informed consent and children provided assent.
Results
The sample of 114 children, aged 9 to 11 years, was 69% white, 5% African American, and 10% Hispanic. Table 1 shows the demographics of children in the sample.
TABLE 1.
Demographics
| Characteristic | Total % N = 114 |
|---|---|
| Sex | |
| Female | 48.3 |
| Male | 51.8 |
| Age | |
| 9 | 40.4 |
| 10 | 37.7 |
| 11 | 21.9 |
| Race/ethnicity | |
| White | 69.3 |
| African American | 5.3 |
| Hispanic | 9.7 |
| Other | 15.8 |
| Weight status | |
| Underweight | 8.5 |
| Healthy weight | 70.8 |
| Overweight or obese | 20.8 |
On average, 64% of fractals followed by pictures of healthy-weight children were rated as “good,” whereas only 59% of fractals followed by pictures of overweight children were rated as “good.” This equates to an overall implicit bias rate of 5.4% against overweight children (P < .001). Table 2 shows differences in implicit weight bias by participant characteristics. Healthy-weight participants showed greater bias (7.9%) than overweight participants (1.4%) or underweight participants (0.3%), (P = .049).
TABLE 2.
Differences in Weight Bias by Participant Characteristics
| Characteristic | Weight Bias | P |
|---|---|---|
| Sex | ||
| Male | 6.6 | .421 |
| Female | 4.1 | — |
| Age | ||
| 9 | 7.4 | .255 |
| 10 | 2.2 | — |
| 11 | 7.2 | — |
| Race/ethnicity | ||
| White | 6.5 | .195 |
| African American | 9.3 | — |
| Hispanic | 1.5 | — |
| Other | 1.5 | — |
| Weight status | ||
| Underweight | 0.3 | .049 |
| Healthy weight | 7.9 | — |
| Overweight | 1.4 | — |
Higher percentages represent greater preference for images of healthy-weight children. —, not applicable.
Discussion
As one of few studies examining implicit weight bias among children, and the first, to our knowledge, to use age-, race-, and sex-matched photographs to do so, our results find significant evidence of implicit weight bias among US children aged 9 to 11. The overall magnitude of implicit weight bias seen in the current study is similar to that seen in other studies for race.25 Additionally, findings of the current study are comparable to those from previous studies using schematic figure drawings of children of varying body weight,21,22 as well as those using drawings of children with obesity or various disabilities,23 as a component of their assessment of bias.
As a pilot study, our findings provide a critical base for future research. Although we were not powered to detect differences in bias by demographic characteristics, our findings emphasize the need to further examine how bias differs by race and weight among this age group. Furthermore, it will be important to examine factors that influence and strengthen implicit weight bias and negative attitudes children hold. Studies in adults, for example, have found that, despite all participants demonstrating high implicit weight bias, participants shown stereotypical or negative portrayals of individuals with obesity had stronger implicit biases compared with those who were shown neutral or nonstigmatizing images.12,19 Consistent with adult literature, healthy weight participants had higher levels of implicit bias than participants with overweight or obesity.28
Importantly, we were also able to demonstrate the feasibility of conducting the AMP with preadolescent children. Although multiple trials are required for the validity of the AMP, children may be particularly susceptible to fatigue from the repetitions, and future researchers should be aware of this potential limitation. Future work should also determine if a fewer number of trials reduces fatigue while yielding valid results.
Our sample was limited in the fact that it was a convenience sample of preadolescents in 1 location who were primarily white and of higher socioeconomic status than the general population. The generalizability of our findings will need to be replicated in other, more representative samples. Strengths of our study include using a well-validated procedure for assessing implicit bias and the large number of children assessed. The use of photographs, rather than line drawings like those used in early studies, also strengthens the external validity of our findings.
Because this is one of the first examples of implicit bias in children about overweight and obesity, this study stimulates as many questions as it answers. Are the findings noticed here for racial differences borne out in larger studies with greater diversity? Does having greater implicit bias relate to eating, activity, socialization, or bullying behaviors? And, finally, does implicit bias change with various exposures and/or interventions?
This study is important in that high levels (similar to what is seen with race) of implicit weight bias are seen in school-aged children. This high level of bias is particularly concerning in an era when one-third of children are overweight or obese and with previous research suggesting that experiencing weight stigma is itself a pathway to unhealthy eating.2,4–6 Implicit weight bias deserves further research in the “real world,” outside of a laboratory-like setting, to evaluate its impact on the explicit attitudes children hold as well as to more closely examine its effects on behaviors. In the future, it will be crucial to develop interventions to lessen the perpetuation of weight bias and weight-based victimization, such that children will be relieved of the harmful consequences caused by experiencing this type of stigma.
Glossary
- AMP
Affect Misattribution Procedure
Footnotes
Dr Skinner helped to conceptualize and design the study, designed the data collection instruments, collected data, conducted the data analysis, drafted the initial manuscript, and revised the manuscript; Dr Payne developed and validated the data collection procedure, designed the data collection instruments, supervised data analysis, and reviewed and revised the manuscript; Dr A. Perrin conceptualized and designed the study, assembled the team, secured funding for the project, designed the data collection instruments, supervised data collection, collected data, and reviewed and revised the manuscript; Drs Panter and Steiner helped to conceptualize and design the study, and reviewed and revised the manuscript; Ms Howard helped to conceptualize and design the study, helped design the data collection instruments, coordinated and supervised data collection, and reviewed and revised the manuscript; Dr Bardone-Cone helped to conceptualize and design the study, designed the data collection instruments, collected data, and reviewed and revised the manuscript; Dr Bulik helped to conceptualize and design the study, designed the data collection instruments, and reviewed and revised the manuscript; and Dr E. Perrin conceptualized and designed the study, assembled the team, secured funding for the project, supervised data collection, designed the data collection instruments, collected data, and reviewed and revised the manuscript.
FINANCIAL DISCLOSURE: Dr Bulik acknowledges funding from the Swedish Research Council (VR Dnr: 538-2013-8864); the other authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: All phases of this study were supported by funding from grant R24CA186212 from the National Institutes of Health/National Cancer Institute. Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: Dr Bulik is a grant recipient from Shire and a consultant for Ironshore; the other authors have indicated they have no potential conflicts of interest to disclose.
References
- 1.Puhl RM, Heuer CA. The stigma of obesity: a review and update. Obesity (Silver Spring). 2009;17(5):941–964 [DOI] [PubMed] [Google Scholar]
- 2.Puhl RM, King KM. Weight discrimination and bullying. Best Pract Res Clin Endocrinol Metab. 2013;27(2):117–127 [DOI] [PubMed] [Google Scholar]
- 3.Puhl RM, Luedicke J, Heuer C. Weight-based victimization toward overweight adolescents: observations and reactions of peers. J Sch Health. 2011;81(11):696–703 [DOI] [PubMed] [Google Scholar]
- 4.Haines J, Neumark-Sztainer D, Eisenberg ME, Hannan PJ. Weight teasing and disordered eating behaviors in adolescents: longitudinal findings from Project EAT (Eating Among Teens). Pediatrics. 2006;117(2). Available at: www.pediatrics.org/cgi/content/full/117/2/e209 [DOI] [PubMed] [Google Scholar]
- 5.Puhl RM, Heuer CA. Obesity stigma: important considerations for public health. Am J Public Health. 2010;100(6):1019–1028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Storch EA, Milsom VA, Debraganza N, Lewin AB, Geffken GR, Silverstein JH. Peer victimization, psychosocial adjustment, and physical activity in overweight and at-risk-for-overweight youth. J Pediatr Psychol. 2007;32(1):80–89 [DOI] [PubMed] [Google Scholar]
- 7.Myers A, Rosen JC. Obesity stigmatization and coping: relation to mental health symptoms, body image, and self-esteem. Int J Obes Relat Metab Disord. 1999;23(3):221–230 [DOI] [PubMed] [Google Scholar]
- 8.Vartanian LR. Development and validation of a brief version of the Stigmatizing Situations Inventory. Obes Sci Pract. 2015;1(2):119–125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bacon JG, Scheltema KE, Robinson BE. Fat phobia scale revisited: the short form. Int J Obes Relat Metab Disord. 2001;25(2):252–257 [DOI] [PubMed] [Google Scholar]
- 10.McClure KJ, Puhl RM, Heuer CA. Obesity in the news: do photographic images of obese persons influence antifat attitudes? J Health Commun. 2011;16(4):359–371 [DOI] [PubMed] [Google Scholar]
- 11.Pearl RL, Puhl RM, Brownell KD. Positive media portrayals of obese persons: impact on attitudes and image preferences. Health Psychol. 2012;31(6):821–829 [DOI] [PubMed] [Google Scholar]
- 12.Teachman BA, Gapinski KD, Brownell KD, Rawlins M, Jeyaram S. Demonstrations of implicit anti-fat bias: the impact of providing causal information and evoking empathy. Health Psychol. 2003;22(1):68–78 [DOI] [PubMed] [Google Scholar]
- 13.Nosek BA, Hawkins CB, Frazier RS. Implicit social cognition: from measures to mechanisms. Trends Cogn Sci. 2011;15(4):152–159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Puhl RM, Latner JD, O’Brien K, Luedicke J, Danielsdottir S, Forhan M. A multinational examination of weight bias: predictors of anti-fat attitudes across four countries. Int J Obes. 2015;39(7):1166–1173 [DOI] [PubMed] [Google Scholar]
- 15.Bessenoff GR, Sherman JW. Automatic and controlled components of prejudice toward fat people: evaluation versus stereotype activation. Soc Cogn. 2000;18:329–353 [Google Scholar]
- 16.Dovidio JF, Kawakami K, Johnson C, Johnson B, Howard A. On the nature of prejudice: automatic and controlled processes. J Exp Soc Psychol. 1997;33(5):510–540 [Google Scholar]
- 17.Fazio RH, Jackson JR, Dunton BC, Williams CJ. Variability in automatic activation as an unobtrusive measure of racial attitudes: a bona fide pipeline? J Pers Soc Psychol. 1995;69(6):1013–1027 [DOI] [PubMed] [Google Scholar]
- 18.Greenwald AG, Poehlman TA, Uhlmann EL, Banaji MR. Understanding and using the implicit association test: III. Meta-analysis of predictive validity. J Pers Soc Psychol. 2009;97(1):17–41 [DOI] [PubMed] [Google Scholar]
- 19.Hinman NG, Burmeister JM, Kiefner AE, Borushok J, Carels RA. Stereotypical portrayals of obesity and the expression of implicit weight bias. Body Image. 2015;12:32–35 [DOI] [PubMed] [Google Scholar]
- 20.Wang SS, Brownell KD, Wadden TA. The influence of the stigma of obesity on overweight individuals. Int J Obes Relat Metab Disord. 2004;28(10):1333–1337 [DOI] [PubMed] [Google Scholar]
- 21.Solbes I, Enesco I. Explicit and implicit anti-fat attitudes in children and their relationships with their body images. Obes Facts. 2010;3(1):23–32 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Collins ME. Body figure perceptions and preferences among preadolescent children. Int J Eat Disord. 1991;10:199–208 [Google Scholar]
- 23.Latner JD, Stunkard AJ. Getting worse: the stigmatization of obese children. Obes Res. 2003;11(3):452–456 [DOI] [PubMed] [Google Scholar]
- 24.Payne BK, Lundberg K. The affect misattribution procedure: ten years of evidence on reliability, validity, and mechanisms. Soc Personal Psychol Compass. 2014;8(12):672–686 [Google Scholar]
- 25.Payne BK, Krosnick JA, Pasek J, Lelkes Y, Akhtar O, Tompson T. Implicit and explicit prejudice in the 2008 American presidential election. J Exp Soc Psychol. 2010;46:367–374 [Google Scholar]
- 26.Payne BK, Cheng CM, Govorun O, Stewart BD. An inkblot for attitudes: affect misattribution as implicit measurement. J Pers Soc Psychol. 2005;89(3):277–293 [DOI] [PubMed] [Google Scholar]
- 27.Cameron CD, Brown-Iannuzzi JL, Payne BK. Sequential priming measures of implicit social cognition: a meta-analysis of associations with behavior and explicit attitudes. Pers Soc Psychol Rev. 2012;16(4):330–350 [DOI] [PubMed] [Google Scholar]
- 28.Marini M, Sriram N, Schnabel K, et al. . Overweight people have low levels of implicit weight bias, but overweight nations have high levels of implicit weight bias. PLoS One. 2013;8(12):e83543. [DOI] [PMC free article] [PubMed] [Google Scholar]