For prevention of SIDS, the AAP recommends infant-parent room-sharing until age 1. However, these new data show potential unintended consequences of room-sharing.
Abstract
OBJECTIVES:
The American Academy of Pediatrics recommends infant-parent room-sharing until age 1. We assessed the association between room-sharing and sleep outcomes.
METHODS:
The Intervention Nurses Start Infants Growing on Healthy Trajectories study is an obesity prevention trial comparing a responsive parenting intervention with a safety control among primiparous mother-infant dyads. Mothers completed the Brief Infant Sleep Questionnaire at 4, 9, 12, and 30 months. Reported sleep duration and overnight behaviors, adjusted for intervention group, were compared among early independent sleepers (own room <4 months), later independent sleepers (own room between 4 and 9 months), and room-sharers at 9 months.
RESULTS:
At 4 months, reported overnight sleep duration was similar between groups, but compared with room-sharers, early independent sleepers had better sleep consolidation (longest stretch: 46 more minutes, P = .02). At 9 months, early independent sleepers slept 40 more minutes nightly than room-sharers and 26 more minutes than later independent sleepers (P = .008). The longest stretch for early independent sleepers was 100 and 45 minutes more than room-sharers and later independent sleepers, respectively (P = .01). At 30 months, infants sleeping independently by 9 months slept >45 more minutes nightly than those room-sharing at 9 months (P = .004). Room-sharers had 4 times the odds of transitioning to bed-sharing overnight at both 4 and 9 months (P < .01 for both).
CONCLUSIONS:
Room-sharing at ages 4 and 9 months is associated with less nighttime sleep in both the short and long-term, reduced sleep consolidation, and unsafe sleep practices previously associated with sleep-related death.
What’s Known on This Subject:
The American Academy of Pediatrics recommends infant-parent room-sharing through age 1. Short sleep duration during infancy has been associated with adverse outcomes for infants and families. The effect of room-sharing on sleep outcomes has been inadequately explored.
What This Study Adds:
Room-sharing at ages 4 and 9 months is associated with less nighttime sleep, shorter sleep stretches, and unsafe sleep practices previously associated with sleep-related death.
The importance of getting an adequate night’s sleep has been increasingly recognized by professional societies including the American Academy of Pediatrics1 (AAP) and the American Academy of Sleep Medicine.2 Inadequate sleep has been associated with poorer cognitive, psychomotor, physical, and socioemotional development, which includes emotion regulation, mood, and behavior in infancy and childhood.3–6 Insufficient sleep is generally accepted as an important risk factor for obesity,7,8 with links between sleep and weight beginning in infancy.9–14 Short sleep duration during infancy is also associated with inadequate sleep later in childhood,15 emphasizing the importance of developing healthy sleep-related behaviors during the first months after birth. Also, infant sleep has a bidirectional relationship with parent outcomes as demonstrated by associations between infant sleep and parental sleep, maternal sensitivity, relationship quality, parental emotional health, and parenting practices.16–18
The desire to optimize infant sleep duration and consolidation, however, must be balanced with safe infant sleep, a fact reinforced by the 3500 infants who tragically die of sudden infant death syndrome (SIDS) or other sleep-related deaths annually.19 According to the Eunice Kennedy Shriver National Institute of Child Health and Human Development’s “Safe to Sleep” campaign, most SIDS deaths occur when infants are 1 to 4 months old, 90% occurring before the age of 6 months.20 Despite these figures, the recently published AAP Policy Statement, SIDS and Other Sleep-Related Infant Deaths, recommended that infants sleep in their parents’ room on a separate surface, ideally for the entire first year but at least for the first 6 months.21 The 1-year recommendation has questionable congruence with the epidemiology of SIDS (as risk is far lower after 6 months), and it runs counter to the common clinical advice parents receive. Based on evidence of improved infant sleep,22–24 clinicians may encourage parents to establish independent sleep environments (ie, in a separate room from parents) during the middle of the first year to promote healthy and sustainable sleep patterns before the typical onset of separation anxiety later in the first year.25 Therefore, in this secondary data analysis, we sought to evaluate the associations between room-sharing on a separate sleep surface and sleep-related outcomes from the cohort participating in the Intervention Nurses Start Infants Growing on Healthy Trajectories (INSIGHT) study. We hypothesized that room-sharing would be associated with shorter nighttime sleep duration and problematic sleep-related behaviors during infancy when compared with independent sleeping in a separate room. We also sought to examine risk factors for SIDS among infants who were and were not independent sleepers.
Methods
Participants and Design
As previously described,26–28 mothers and their newborns were recruited after delivery from one maternity ward (Penn State Milton S. Hershey Medical Center, Hershey, PA) for participation in the INSIGHT study from January 2012 to March 2014. The study design and inclusion and exclusion criteria have been previously published.26 Major eligibility criteria specified that the subjects be term singletons weighing ≥2500 g delivered to English-speaking, primiparous mothers ≥20 years old. Dyads were randomly assigned 2 weeks after delivery to a responsive parenting (RP) intervention or a safety control group. 279 mother-infant dyads completed the first home visit and are considered the study cohort for outcomes as specified before study initiation in the protocol. For the current analyses, those parents who reported bed-sharing with their newborn were excluded because the goal was to compare those who were sleeping independently in a separate room from parents with those still room-sharing but not bed-sharing (as recommended by the AAP).
Research nurses conducted home visits at infant ages of 3 to 4 weeks and 4, 6, and 9 months. Research center visits occurred at 1 and 2 years of age. Intervention components have been previously described.27 Among other sleep-related topics discussed at the 3- to 4-week home visit, the RP group received guidance encouraging parents to consider moving their child’s sleep location at the age of 3 months to the room they would prefer the infant to sleep in at 1 year of age, with the advice that such a move would be more difficult if the family waited much beyond that point.25 This point was reinforced at the 4-month home visit. The safety control group received education regarding prevention of SIDS, which included direct observation of the sleep environment by the visiting nurses with individual feedback to improve safety at the first 3 home visits. This study was approved by the Penn State College of Medicine’s Human Subjects Protection Office and registered at www.clinicaltrials.gov.
Measures
Data were collected and managed by using REDCap (Vanderbilt University, Nashville, TN).29 Mothers completed the online surveys with paper surveys mailed to those lacking internet connectivity (n = 20). A detailed list of measures was published.26
Background Characteristics
Demographic information collected at enrollment included parent and child race/ethnicity, maternal education, annual income, and marital status. Data extracted from medical charts included maternal age, prepregnancy weight, gestational weight gain, infant gestational age, and birth anthropometrics.
Sleep
The validated Brief Infant Sleep Questionnaire was used to assess sleep at 4 and 9 months of age with an abbreviated version administered at 12 and 30 months.30 This survey assesses infant sleep location, before-bedtime activities, and sleep patterns. Sleep duration is divided into nighttime (7 pm–7 am) and daytime (7 am–7 pm) and is reported in hours and minutes. Additional questions regarding sleep location, night waking, night feedings, bedtime routine components and duration, infant sleep behaviors and environment, and parenting responses to night wakings were asked at 4 and 9 months. Instructions for the infant sleep survey guided mothers to think about her child’s sleep during the past week when answering the questions and base responses on a “typical night.” Maternal sleep quality was measured at 4 months of infant age by using the PROMIS Sleep Disturbance instrument (PROMIS Network, American Institutes for Research, Chapel Hill, NC).31
Other
Feeding mode was assessed by using a food frequency questionnaire. Infants were categorized as predominantly breastfed if ≥80% of milk feedings were breastmilk.32
Statistical Analysis
Data were analyzed by using SAS version 9.4 (SAS Institute, Cary, NC). Descriptive statistics were generated for sleep duration and behaviors on the basis of the timing of our 2 sleep assessments during infancy at 4 and 9 months of age, which created 3 groups: early independent sleepers (own room <4 months), later independent sleepers (own room between 4 and 9 months), and room-sharers at 9 months. For continuous outcomes, differences by sleep location were assessed by using analysis of variance (ANOVA) at each of the 4 times, adjusting for study group assignment. Categorical outcomes were assessed by using logistic regression, adjusting for study group. Analyses including socioeconomic covariates (eg, income, living in a single-family home) did not result in major differences in results, and thus results from models that included only study group are presented. Statistical significance was defined as P ≤ .05.
Results
Among 279 participants,27,28 259 (93%) remained in the study through 9 months of age. Among this group, 20 were bed-sharing at 4 and/or 9 months and 9 had missing data on sleep. These participants were excluded from further analyses, leaving a sample of 230 mother-infant pairs as the sample for this manuscript. The majority of infants, 142 (62%), were “early independent sleepers,” sleeping independently without room-sharing by 4 months (Table 1). Another 62 (27%) were “later independent sleepers” who began sleeping independently between 4 and 9 months of age, whereas 26 (11%) were room-sharing at 9 months. There were no differences between intervention groups in terms of frequency of bed-sharing or room-sharing at 4 or 9 months. Room-sharing was associated with demographic variables including race/ethnicity, lower income and education, unmarried and/or not cohabiting with partner, fewer bedrooms in the home, and extended family and/or other people living in the home.
TABLE 1.
Differences in Maternal Demographics and Home Characteristics by Mother-Infant Sleeping Arrangements
| Early Independent Sleepers | Later Independent Sleepers | Still Room-Sharing at 9 mo | P | |
|---|---|---|---|---|
| N = 142 | N = 62 | N = 26a | ||
| Maternal demographics | ||||
| Maternal age, y (SD) | 29.1 (3.9) | 29.8 (4.9) | 28.1 (6.4) | .25 |
| Prepregnancy BMI (SD) | 26.0 (5.5) | 24.7 (4.3) | 26.0 (7.1) | .28 |
| Race/ethnicity, N (%) | .001 | |||
| White, non-Hispanic | 135 (95) | 54 (87) | 19 (73) | |
| Other | 7 (5) | 8 (13) | 7 (27) | |
| Annual household income, N (%) | .01 | |||
| <$25 000 | 8 (6) | 5 (8) | 5 (19) | |
| $25 000–$49 999 | 13 (9) | 3 (5) | 4 (15) | |
| $50 000–$74 999 | 41 (29) | 14 (23) | 9 (35) | |
| ≥$75 000 | 77 (54) | 36 (58) | 5 (19) | |
| Don’t know or declined to answer | 3 (2) | 4 (6) | 3 (12) | |
| Education, N (%) | <.001 | |||
| High school graduate or less | 10 (7) | 4 (6) | 4 (15) | |
| Some college | 26 (18) | 18 (29) | 14 (54) | |
| College graduate or higher | 106 (75) | 40 (65) | 8 (31) | |
| Married and/or living with partner, N (%) | 138 (97) | 59 (95) | 21 (81) | .004 |
| Returned to work ≤12 wk postpartum, N (%) | 72 (51) | 29 (48) | 19 (73) | .07 |
| Predominantly breastfeeding, N (%) | ||||
| At 1 mo | 82 (58) | 47 (77) | 14 (56) | .03 |
| At 4 mo | 64 (45) | 36 (58) | 11 (42) | .21 |
| At 6 mo | 52 (37) | 29 (47) | 6 (24) | .12 |
| At 9 mo | 46 (32) | 24 (39) | 7 (27) | .51 |
| Home characteristics | ||||
| Single-family home, N (%) | 102 (72) | 38 (63) | 14 (56) | .20 |
| Number of bedrooms, N (%) | <.001 | |||
| 1 | 0 (0) | 2 (3) | 3 (12) | |
| 2 | 27 (19) | 18 (29) | 8 (31) | |
| 3+ | 115 (81) | 42 (68) | 15 (58) | |
| Extended family and/or others living in home, N (%) | 16 (12) | 8 (14) | 10 (42) | .005 |
Includes 5 infants who were not room-sharing at 4 mo.
Reported Sleep Duration, Consolidation, Night Wakings, and Night Feedings
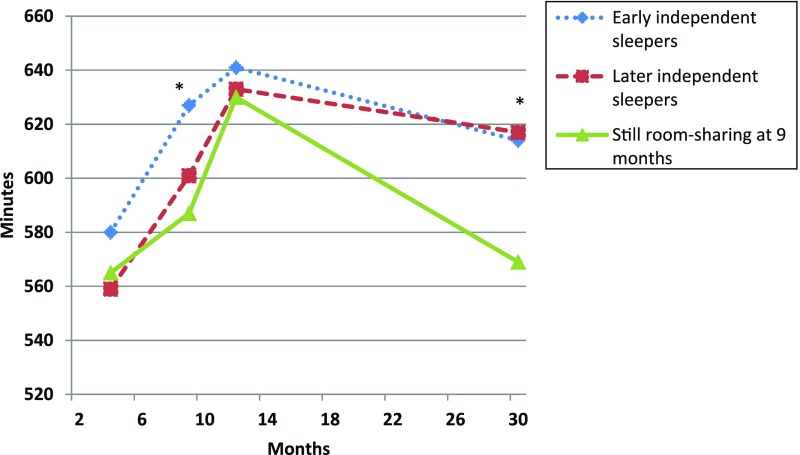
At 4 months, no significant differences in nighttime or total sleep duration were observed between those who were early independent sleepers and those who room-shared at 4 and/or 9 months (Fig 1). However, the early independent sleepers had better sleep consolidation at 4 months of age with a longest (mean ± SD) sleep stretch averaging 469 ± 139 minutes compared with 423 ± 158 minutes for those who were room-sharing (Table 2) (P = .02). While the mean number of night wakings was similar between early independent and nonindependent sleeping infants at 4 months of age, those sleeping independently had fewer night feedings (1.1 vs 1.4; P = .02). Nonindependent sleepers also had twice the odds of being fed back to sleep overnight compared with independent sleepers (adjusted odds ratio [aOR] 1.95, 95% confidence interval [CI] 1.09–3.50).
FIGURE 1.
Room-sharing group and nighttime sleep duration at 4, 9, 12, and 30 months of age. * P < .01.
TABLE 2.
Sleep Outcome Differences Between Infants Who Are Independently Sleeping by 4 mo Versus Those Who Are Not
| Early Independent Sleepers | Later Independent Sleepers | Still Room-Sharing at 9 mo | Early Independent Sleepers Versus Other Groups | Pa | |
|---|---|---|---|---|---|
| N = 142 | N = 62 | N = 26b | aOR (95% CI) | ||
| 4-mo assessment | |||||
| Bedtime routine, N (%) | |||||
| Consistent bedtime routine | 53 (37) | 12 (20) | 8 (32) | 1.93 (1.05–3.53) | .03 |
| Falls asleep while feeding | 72 (51) | 41 (66) | 10 (40) | 0.76 (0.44–1.31) | .32 |
| Put to bed drowsy but awake | 61 (43) | 19 (27) | 7 (28) | 1.70 (0.96–3.03) | .07 |
| Bedtime 8 pm or earlier | 60 (42) | 18 (22) | 5 (20) | 1.93 (1.06–3.53) | .03 |
| Longest sleep stretch, min (SD) | 469 (139) | 415 (154) | 440 (165) | — | .02 |
| Night wakings, mean ± SD | 1.1 (1.1) | 1.4 (1.0) | 1.3 (0.8) | — | .14 |
| Night feedings, mean ± SD | 1.1 (1.1) | 1.4 (1.0) | 1.4 (1.2) | — | .02 |
| Fed back to sleep, N (%) | 78 (55) | 46 (74) | 16 (64) | 0.51 (0.29–0.92) | .02 |
| Sleep safety, N (%) | |||||
| Nonsupine sleep position | 12 (9) | 3 (5) | 4 (16) | 1.03 (0.39–2.72) | .96 |
| Unapproved object on sleep surface | 48 (34) | 29 (48) | 14 (56) | 0.49 (0.28–0.85) | .02 |
| Brought to parent bed overnight | 7 (5) | 9 (15) | 6 (24) | 0.24 (0.09–0.61) | .003 |
| Maternal sleep poor or very poor, N (%) | 11 (8) | 10 (17) | 3 (12) | 0.47 (0.20–1.11) | .09 |
Reported P values are comparing the first column (independent sleeping by 4 mo) versus the other 2 combined, adjusted for study group by using ANOVA for continuous outcomes and logistic regression for categorical outcomes.
Includes 5 infants who were not room-sharing at 4 mo.
By 9 months of age, significant differences in nighttime sleep duration emerged between groups (Table 3). The early independent sleepers slept on average 627 ± 67 minutes per night compared with 601 ± 73 minutes for later independent sleepers and 587 ± 83 minutes for those who were room-sharing at 9 months of age (P = .008). Those who were early independent sleepers had the best sleep consolidation with the longest sleep stretches, averaging 542 ± 162 minutes versus 497 ± 166 minutes for later independent sleepers and 442 ± 158 minutes for room-sharers (P = .01). Although night wakings, night feedings, and odds of being fed back to sleep overnight did not differ among groups at 9 months of age, total daily sleep duration was longest among early independent sleepers (796 ± 86 vs 760 ± 94 vs 773 ± 96 minutes, P = .04).
TABLE 3.
Sleep Outcomes at 9 mo by Timing of Independent Sleeping
| Early Independent Sleepers | Later Independent Sleepers | Still Room-Sharing at 9 mo | P (Main Effect of Room-Sharing Category)a | Independent Sleepers Versus Room Sharers, aOR (95% CI) | Pb | |
|---|---|---|---|---|---|---|
| N = 142 | N = 62 | N = 26c | ||||
| 9 mo assessment | ||||||
| Bedtime routine, N (%) | ||||||
| Consistent bedtime routine | 67 (47) | 19 (31) | 8 (31) | .06 | 1.65 (0.68–3.99) | .27 |
| Falls asleep while feeding | 51 (36) | 26 (42) | 13 (50) | .41 | 0.59 (0.25–1.36) | .22 |
| Put to bed drowsy, but awake | 115 (81) | 42 (68) | 16 (62) | .05 | 2.16 (0.90–5.19) | .08 |
| Bedtime 8 pm or earlier | 93 (65) | 34 (55) | 10 (38) | .03 | 2.79 (1.18–6.61) | .02 |
| Longest sleep stretch, min (SD) | 542 (162) | 497 (166) | 442 (158) | .01 | — | — |
| Night wakings, mean ± SD | 1.0 (1.0) | 1.0 (0.9) | 1.4 (1.2) | .10 | — | — |
| Night feedings, mean ± SD | 0.5 (0.9) | 0.7 (0.9) | 0.8 (0.9) | .19 | — | — |
| Fed back to sleep, N (%) | 36 (25) | 24 (39) | 11 (42) | .10 | 0.56 (0.24–1.30) | .17 |
| Sleep safety, N (%) | ||||||
| Nonsupine sleep position | 116 (82) | 51 (82) | 21 (84) | .96 | 0.86 (0.28–2.67) | .80 |
| Unapproved object on sleep surface | 97 (69) | 41 (67) | 14 (54) | .33 | 1.89 (0.82–4.37) | .14 |
| Brought to parent bed overnight | 13 (9) | 11 (18) | 9 (35) | .004 | 0.25 (0.01–0.63) | .003 |
P value is for main effect of room-sharing category, controlling for study group by using ANOVA for continuous outcomes and logistic regression for categorical outcomes.
P value is for odds ratio for early independent sleepers and later independent sleepers combined compared with room-sharers as a reference group, controlling for the study group.
Includes 5 infants who were not room-sharing at 4 mo.
At 12 months of age, no differences existed between groups for nighttime or total daily sleep duration. However, the 30-month assessment revealed that both early and later independent sleepers slept on average more than 45 minutes longer at night than those who were room-sharing at 9 months (614 ± 51 vs 617 ± 70 vs 569 ± 79; P = .004). Total daily sleep duration was similar among groups at 30 months of age.
Bedtime Routines
Significant differences existed for bedtime routines at 4 months of age. Early independent sleepers had increased odds of having a consistent bedtime routine (aOR 1.93, 95% CI 1.05–3.53) and being put to bed by 8 pm (aOR 1.93, 95% CI 1.06–3.53) relative to room-sharers. At 9 months of age, room-sharing was associated with greater odds of having a bedtime after 8 pm; room-sharers also had lower odds than independent sleepers of being put to sleep drowsy but awake (P ≤ .05 for both).
Sleep Safety
At 4 months of age, room-sharing infants had greater odds of having an unapproved object (blankets, pillows, positioners, etc) on their sleep surface than those who were sleeping independently (aOR 2.04, 95% CI 1.17–3.57). Additionally, room-sharing parents with infants at 4 months of age had over 4 times the odds of bringing their infant into their bed overnight than those parenting early independent sleepers (aOR 4.24, 95% CI 1.64–10.95). Similarly, at 9 months of age, room-sharing parents had 4 times the odds than those who were sleeping independently of bringing their infant into their bed after waking overnight (aOR 3.97, 95% CI 1.59–9.90).
Discussion
These secondary analyses from the INSIGHT study demonstrate that infant-parent room-sharing at 4 and 9 months of age is associated with less reported nighttime sleep in both the short- and long-term, worse sleep consolidation, and unsafe sleep practices previously associated with sleep-related death. The findings raise questions about the well-intended AAP recommendation that room-sharing should ideally occur for all infants until their first birthday.21
The recommendation to room-share until the age of 1 year is not evidence-based for the prevention of SIDS, given that 90% of these tragedies occur before the age of 6 months.20 The data presented by the AAP Task Force on Sudden Infant Death Syndrome to support the recommendation21 came from 3 European case-control reports.33–35 In the first by Blair et al,33 infants who died of SIDS at over 4 months of age were more likely than controls to be room-sharing without bed-sharing (46% vs 41%) and less likely to be sleeping independently in their own rooms (43% vs 53%; statistical comparison not performed), yet the age stratification presented in this paper was not acknowledged in a recently published letter by the Task Force.36 The second report involved mostly infants <6 months old and used data from the early- to mid-1990s, when prone sleeping was still common.34 The third study involved only 123 cases of SIDS with a mean age of 13.6 ± 9.5 weeks, indicating that most cases included infants <6 months old.35 This small study included only 15 infants who slept in their own room and died of SIDS. Therefore, it is unlikely that any conclusions can be made about those who were 6 to 12 months old on the basis of this small sample size and the epidemiology of the condition. Importantly, the biggest risk factor for SIDS in this third report was “sharing the same sleep surface as the last sleep location,” something that more commonly occurred among infants who initially shared their mother’s room in our study.
In addition to the lack of data supporting the recommendation to room-share until 1 year of age, the Policy Statement authored by the Task Force did not describe a mechanism by which room-sharing would prevent SIDS or how parents should apply this recommendation to achieve better outcomes than those parents choosing to have their infants sleep independently. Although the Task Force’s recent letter cited more frequent arousals among room-sharers as the potential protective mechanism,36 the 2 studies referenced do not support that conclusion. The first is a case-control study of 18 infants.37 Among 9 room-sharers, 5 were bed-sharers, making conclusions about arousals among those who are room-sharing but not bed-sharing (versus independent sleepers) problematic. The second study, which also included bed-sharers in the room-sharing group, states that parental presence in the room at bedtime (eg, holding, rocking, feeding to sleep) explained much of the variance in night wakings and that night-long room-sharing had a “negligible (<1%) independent contribution to the explained variance.”22
The AAP recommendation to room-share until the age of 1 year conflicts with sleep expert guidance,25 which recognizes developmental changes that occur over the first year. The suggestion that parents wait to move the infant out of their bedroom until the end of the first year, when separation anxiety is normative and increasing, is likely to result in frustrated parents and unhappy infants. It also conflicts with other data that room-sharing is associated with more sleep disruption for mothers.24,38
Our data showing shorter night sleep and shorter sleep bouts for infants who are room-sharing has potentially important consequences. Inadequate sleep affects nearly every health domain, including emotional regulation, mood, and behavior in infancy and childhood.3–6 As demonstrated in our analyses, room-sharing and short sleep duration during infancy are also associated with inadequate sleep later in childhood,15 which emphasizes the importance of developing healthy sleep-related behaviors during the first months of life. Infant sleep also affects parental sleep, which can affect other outcomes, including maternal sensitivity, relationship quality, parental emotional health, and parenting practices.16,17 Fatigue is related to somatic complaints, anxiety, depression, paranoia, and crashes or unintentional injuries involving motor vehicles among healthy adults39,40 and has been associated with postpartum depression,41 abusive head trauma, and child abuse.42 At a time when family-centered guidance is strongly encouraged, parent fatigue should be considered in any guideline related to infant sleep.
Perhaps our most troubling finding was that room-sharing was associated with overnight transitions to bed-sharing, which is strongly discouraged by the AAP.21 Bed-sharing overnight was more common in our sample among 4- and 9-month-olds who began the night on a separate surface in their parents’ room. This finding is consistent with those from another recently described cohort.43
There are limitations to our analyses. The data come from a randomized controlled trial with 2 interventions. The control group received information aimed at reducing the risk of SIDS, although no recommendation was made regarding sleep location. The RP intervention included guidance to improve sleep duration and sleep-related behaviors, including recommending independent infant sleep by 4 months of age. However, sleep location did not vary significantly by intervention group (data not shown), and all analyses were adjusted for study group. Next, the findings we report are correlational, and causal effects cannot be inferred. It is possible that parents of infants with poorer sleep prefer that infants sleep more closely to them. The relatively homogeneous INSIGHT sample is another potential limitation, as are the self-reported data, although the Brief Infant Sleep Questionnaire has been validated against objective measures of sleep.30 Some previous studies have shown discrepancies between subjective and objective measures of sleep,24,38 and the lack of an objective measure may have resulted in unreported night wakings in which the infant self-soothed back to sleep. This possibility would particularly influence the sleep consolidation data, especially for independent sleepers. However, this possibility, if true, would only reinforce the concept that room-sharing may result in either unnecessary parental responses to infant night wakings or, alternatively, the infant’s expectation of caretaking behaviors from parents, both of which can be expected to lead to decreased sleep for infant and parent. In addition, parental perceptions of their infant’s sleep are the basis for whether they report sleep problems and request guidance from health care providers.
Our data showing that room-sharing families had lower education, income, and less likelihood of living in a single-family residence emphasize that not all parents have a choice regarding their infant’s sleep location and may not have the option to have the infant sleep independently, a factor we could not fully address although demographics and home characteristics were assessed in data analyses. Cultural norms may also lead to preferences for room-sharing in some patient populations, as described by Mileva-Seitz et al.44 Lastly, we did not assess room-sharing beyond 9 months of age.
Conclusions
While substantial progress has been made over the past several decades to improve the safety of infant sleep, the AAP recommendation that parents room-share with their infants until the age of 1 year is not supported by data, is inconsistent with the epidemiology of SIDS, is incongruent with our understanding of socioemotional development in the second half of the first year, and has the potential for unintended consequences for infants and families. Our findings showing poorer sleep-related outcomes and more unsafe sleep practices among dyads who room-share beyond early infancy suggest that the AAP should reconsider and revise the recommendation pending evidence to support room-sharing through the age of 1 year.
Glossary
- AAP
American Academy of Pediatrics
- ANOVA
analysis of variance
- aOR
adjusted odds ratio
- CI
Confidence Interval
- INSIGHT
Intervention Nurses Start Infants Growing on Healthy Trajectories
- RP
responsive parenting
- SIDS
sudden infant death syndrome
Footnotes
Dr Paul co-led all aspects of the study concept, design, and analysis and drafted the initial manuscript; Dr Hohman led the data management, performed the data analyses, and participated in critical revision of the manuscript; Dr Loken contributed to analyses and participated in critical revision of the manuscript; Dr Savage contributed to the design of the study, intervention curriculum development, and data analysis and participated in critical revision of the manuscript; Dr Anzman-Frasca contributed to the design of the study and intervention curriculum development and participated in critical revision of the manuscript; Ms Carper participated in intervention design and delivery and participated in critical revision of the manuscript; Ms Marini contributed to the data collection and analysis and participated in critical revision of the manuscript; Dr Birch co-led all aspects of the study concept, design, and analysis, and participated in critical revision of the manuscript; and all authors approved the final manuscript as submitted.
This trial has been registered at www.clinicaltrials.gov (identifier NCT01167270).
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: This research was supported by grant R01DK088244 and the Ashley Nicole Shellenberger SIDS Research Fund at the Penn State College of Medicine. Additional support was received from the Children’s Miracle Network at Penn State Children’s Hospital. US Department of Agriculture grant 2011-67001-30117 supported graduate students. REDCap support was received from The Penn State Clinical and Translational Science Institute, Pennsylvania State University’s Clinical and Translational Science Award, and the National Institutes of Health /National Center for Advancing Translational Sciences (NCATS) grant UL1 TR000127. Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
COMPANION PAPER: A companion to this article can be found online at www.pediatrics.org/cgi/doi/10.1542/peds.2017-1323.
References
- 1.American Academy of Pediatrics Recommended amount of sleep for pediatric populations. Pediatrics. 2016;138(2):e20161601. [DOI] [PubMed] [Google Scholar]
- 2.Paruthi S, Brooks LJ, D’Ambrosio C, et al. . Recommended amount of sleep for pediatric populations: a consensus statement of the American Academy of Sleep Medicine. J Clin Sleep Med. 2016;12(6):785–786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sivertsen B, Harvey AG, Reichborn-Kjennerud T, Torgersen L, Ystrom E, Hysing M. Later emotional and behavioral problems associated with sleep problems in toddlers: a longitudinal study. JAMA Pediatr. 2015;169(6):575–582 [DOI] [PubMed] [Google Scholar]
- 4.Ross CN, Karraker KH. Effects of fatigue on infant emotional reactivity and regulation. Infant Ment Health J. 1999;20(4):410–428 [Google Scholar]
- 5.Spruyt K, Aitken RJ, So K, Charlton M, Adamson TM, Horne RS. Relationship between sleep/wake patterns, temperament and overall development in term infants over the first year of life. Early Hum Dev. 2008;84(5):289–296 [DOI] [PubMed] [Google Scholar]
- 6.Moore M, Mindell JA. The impact of behavioral interventions for sleep problems on secondary outcomes in young children and their families In: Wolfson A, Montgomery-Downs H, eds. Oxford Handbook of Infant, Child, and Adolescent Sleep and Behavior. New York, NY: Oxford Press; 2013 [Google Scholar]
- 7.Wu Y, Zhai L, Zhang D. Sleep duration and obesity among adults: a meta-analysis of prospective studies. Sleep Med. 2014;15(12):1456–1462 [DOI] [PubMed] [Google Scholar]
- 8.Fatima Y, Doi SA, Mamun AA. Longitudinal impact of sleep on overweight and obesity in children and adolescents: a systematic review and bias-adjusted meta-analysis. Obes Rev. 2015;16(2):137–149 [DOI] [PubMed] [Google Scholar]
- 9.Taveras EM, Rifas-Shiman SL, Oken E, Gunderson EP, Gillman MW. Short sleep duration in infancy and risk of childhood overweight. Arch Pediatr Adolesc Med. 2008;162(4):305–311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tikotzky L, DE Marcas G, Har-Toov J, Dollberg S, Bar-Haim Y, Sadeh A. Sleep and physical growth in infants during the first 6 months. J Sleep Res. 2010;19(1 pt 1):103–110 [DOI] [PubMed] [Google Scholar]
- 11.Bell JF, Zimmerman FJ. Shortened nighttime sleep duration in early life and subsequent childhood obesity. Arch Pediatr Adolesc Med. 2010;164(9):840–845 [DOI] [PubMed] [Google Scholar]
- 12.Taveras EM, Gillman MW, Peña MM, Redline S, Rifas-Shiman SL. Chronic sleep curtailment and adiposity. Pediatrics. 2014;133(6):1013–1022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hart CN, Carskadon MA, Considine RV, et al. . Changes in children’s sleep duration on food intake, weight, and leptin. Pediatrics. 2013;132(6). Available at: www.pediatrics.org/cgi/content/full/132/6/e1473 [DOI] [PubMed] [Google Scholar]
- 14.Woo Baidal JA, Locks LM, Cheng ER, Blake-Lamb TL, Perkins ME, Taveras EM. Risk factors for childhood obesity in the first 1,000 days: a systematic review. Am J Prev Med. 2016;50(6):761–779 [DOI] [PubMed] [Google Scholar]
- 15.Touchette E, Petit D, Paquet J, et al. . Factors associated with fragmented sleep at night across early childhood. Arch Pediatr Adolesc Med. 2005;159(3):242–249 [DOI] [PubMed] [Google Scholar]
- 16.Teti DM, Crosby B, McDaniel BT, Shimizu M, Whitesell CJ. Marital and emotional adjustment in mothers and infant sleep arrangements during the first six months. Monogr Soc Res Child Dev. 2015;80(1):160–176 [DOI] [PubMed] [Google Scholar]
- 17.Hall WA, Hutton E, Brant RF, et al. . A randomized controlled trial of an intervention for infants’ behavioral sleep problems. BMC Pediatr. 2015;15:181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sadeh A, Anders TF. Infant sleep problems: origins, assessment, interventions. Infant Ment Health J. 1993;14(1):17–34 [Google Scholar]
- 19.Braveman P, Egerter S, Pearl M, Marchi K, Miller C. Problems associated with early discharge of newborn infants. Early discharge of newborns and mothers: a critical review of the literature. Pediatrics. 1995;96(4 pt 1):716–726 [PubMed] [Google Scholar]
- 20.Margolis LH. A critical review of studies of newborn discharge timing. Clin Pediatr (Phila). 1995;34(12):626–634 [DOI] [PubMed] [Google Scholar]
- 21.Task Force on Sudden Infant Death Syndrome SIDS and other sleep-related infant deaths: updated 2016 recommendations for a safe infant sleeping environment. Pediatrics. 2016;138(5):e20162938. [DOI] [PubMed] [Google Scholar]
- 22.Mindell JA, Sadeh A, Kohyama J, How TH. Parental behaviors and sleep outcomes in infants and toddlers: a cross-cultural comparison. Sleep Med. 2010;11(4):393–399 [DOI] [PubMed] [Google Scholar]
- 23.Mindell JA, Meltzer LJ, Carskadon MA, Chervin RD. Developmental aspects of sleep hygiene: findings from the 2004 National Sleep Foundation Sleep in America Poll. Sleep Med. 2009;10(7):771–779 [DOI] [PubMed] [Google Scholar]
- 24.Volkovich E, Ben-Zion H, Karny D, Meiri G, Tikotzky L. Sleep patterns of co-sleeping and solitary sleeping infants and mothers: a longitudinal study. Sleep Med. 2015;16(11):1305–1312 [DOI] [PubMed] [Google Scholar]
- 25.Mindell JA. Sleeping Through the Night: How Infants, Toddlers, and Their Parents Can Get a Good Night’s Sleep. New York, NY: HarperCollins Publishers, Inc; 2005 [Google Scholar]
- 26.Paul IM, Williams JS, Anzman-Frasca S, et al. . The Intervention Nurses Start Infants Growing on Healthy Trajectories (INSIGHT) study. BMC Pediatr. 2014;14:184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Paul IM, Savage JS, Anzman-Frasca S, Marini ME, Mindell JA, Birch LL. INSIGHT responsive parenting intervention and infant sleep. Pediatrics. 2016;138(1):e20160762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Savage JS, Birch LL, Marini M, Anzman-Frasca S, Paul IM. Effect of the INSIGHT responsive parenting intervention on rapid infant weight gain and overweight status at age 1 year: a randomized clinical trial. JAMA Pediatr. 2016;170(8):742–749 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)–a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sadeh A. A brief screening questionnaire for infant sleep problems: validation and findings for an Internet sample. Pediatrics. 2004;113(6). Available at: www.pediatrics.org/cgi/content/full/113/6/e570 [DOI] [PubMed] [Google Scholar]
- 31.Buysse DJ, Yu L, Moul DE, et al. . Development and validation of patient-reported outcome measures for sleep disturbance and sleep-related impairments. Sleep. 2010;33(6):781–792 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Grummer-Strawn LM, Scanlon KS, Fein SB. Infant feeding and feeding transitions during the first year of life. Pediatrics. 2008;122(suppl 2):S36–S42 [DOI] [PubMed] [Google Scholar]
- 33.Blair PS, Fleming PJ, Smith IJ, et al. . Babies sleeping with parents: case-control study of factors influencing the risk of the sudden infant death syndrome. CESDI SUDI research group. BMJ. 1999;319(7223):1457–1461 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Carpenter RG, Irgens LM, Blair PS, et al. . Sudden unexplained infant death in 20 regions in Europe: case control study. Lancet. 2004;363(9404):185–191 [DOI] [PubMed] [Google Scholar]
- 35.Tappin D, Ecob R, Brooke H. Bedsharing, roomsharing, and sudden infant death syndrome in Scotland: a case-control study. J Pediatr. 2005;147(1):32–37 [DOI] [PubMed] [Google Scholar]
- 36.Moon RY, Moon RY, Darnall RA, et al. . Author’s response. Pediatrics. 2017;139(3):e20164132C. [DOI] [PubMed] [Google Scholar]
- 37.Mao A, Burnham MM, Goodlin-Jones BL, Gaylor EE, Anders TF. A comparison of the sleep-wake patterns of cosleeping and solitary-sleeping infants. Child Psychiatry Hum Dev. 2004;35(2):95–105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Teti DM, Shimizu M, Crosby B, Kim BR. Sleep arrangements, parent-infant sleep during the first year, and family functioning. Dev Psychol. 2016;52(8):1169–1181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kahn-Greene ET, Killgore DB, Kamimori GH, Balkin TJ, Killgore WD. The effects of sleep deprivation on symptoms of psychopathology in healthy adults. Sleep Med. 2007;8(3):215–221 [DOI] [PubMed] [Google Scholar]
- 40.Jackson ML, Croft RJ, Kennedy GA, Owens K, Howard ME. Cognitive components of simulated driving performance: sleep loss effects and predictors. Accid Anal Prev. 2013;50:438–444 [DOI] [PubMed] [Google Scholar]
- 41.Ross LE, Murray BJ, Steiner M. Sleep and perinatal mood disorders: a critical review. J Psychiatry Neurosci. 2005;30(4):247–256 [PMC free article] [PubMed] [Google Scholar]
- 42.Adamsbaum C, Grabar S, Mejean N, Rey-Salmon C. Abusive head trauma: judicial admissions highlight violent and repetitive shaking. Pediatrics. 2010;126(3):546–555 [DOI] [PubMed] [Google Scholar]
- 43.Batra EK, Teti DM, Schaefer EW, Neumann BA, Meek EA, Paul IM. Nocturnal video assessment of infant sleep environments. Pediatrics. 2016;138(3):e20161533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Mileva-Seitz VR, Bakermans-Kranenburg MJ, Battaini C, Luijk MP. Parent-child bed-sharing: the good, the bad, and the burden of evidence. Sleep Med Rev. 2017;32:4–27 [DOI] [PubMed] [Google Scholar]