This study examines, in a prospectively-constructed birth cohort, the association between continuity in infancy and health care utilization and recommended preventive care in early childhood.
Abstract
BACKGROUND AND OBJECTIVES:
Continuity of care is a key aspect of the patient-centered medical home and improves pediatric outcomes. Health care reform requires high-quality data to demonstrate its continued value. We hypothesized that increased provider continuity in infancy will reduce urgent health care use and increase receipt of preventive services in early childhood.
METHODS:
Continuity, using the Usual Provider of Care measure, was calculated across all primary care encounters during the first year of life in a prospectively-constructed cohort of 17 773 infants receiving primary care from birth through 3 years at 30 clinics. Health care utilization and preventive care outcomes were measured from ages 1 to 3 years. Confounders, including chronic conditions, number of sick visits in the first year, socioeconomic status, and site, were addressed by using multivariable regression models incorporating a propensity score.
RESULTS:
Demographics associated with the lowest continuity quartile included white race (adjusted odds ratio [aOR] 1.43; 95% confidence interval [CI] 1.25–1.64), Medicaid insurance (aOR 1.41; 95% CI 1.23–1.61), and asthma (aOR 1.59; 95% CI 1.30–1.93). Lower continuity was associated with more ambulatory care-sensitive hospitalizations (adjusted incidence rate ratio 2.74; 95% CI 1.49–5.03), ambulatory sick visits (adjusted incidence rate ratio 1.08; 95% CI 1.05–1.11), and lower odds of lead screening (aOR 0.61; 95% CI 0.46–0.79). These associations were stronger for children with chronic conditions. Continuity measured during well visits was not associated with outcomes.
CONCLUSIONS:
Continuity may improve care quality and prevent high-cost health encounters, especially for children with chronic conditions. Novel solutions are needed to improve continuity in the medical home.
What’s Known on This Subject:
Continuity of care is a central aspect of the medical home and is associated with improved outcomes. The Affordable Care Act incentivizes the medical home, yet uncertainty about the future of health care reform emphasizes the need for high-quality data.
What This Study Adds:
Higher continuity in infancy is associated with decreased urgent health care utilization and improved receipt of recommended preventive care from ages 1 to 3 years. Strengthening the medical home may improve pediatric outcomes and result in cost savings.
Continuity of care is a central component of the patient-centered medical home.1,2 The American Academy of Pediatrics states that a medical home should be accessible, continuous, family-centered, coordinated, compassionate, and culturally effective.2 In adults, higher continuity is linked with fewer urgent health services and improved patient satisfaction and health outcomes.3–7 In pediatrics, studies have found an association with higher continuity and decreased emergency department (ED) visits,8,9 ambulatory care-sensitive hospitalizations (ACSHs),10 higher well visit adherence,11 and improved receipt of preventive screening.12 The Patient Protection and Affordable Care Act (PPACA) incentivizes the medical home by expanding funding to providers who qualify.13–16 Given the uncertain future of the PPACA, accurate and up-to-date data demonstrating the value of the medical home is needed.15
The association between continuity and outcomes is potentially confounded by various patient and provider factors, which can obscure the causal pathway. A variety of statistical techniques, such as construction of propensity scores and its incorporation into multivariable regression, can reduce measured bias and thus improve causal inference in observational data.17,18 The propensity score can improve the balance of measured confounders between the continuity groups, improving the ability to draw causal inference in observational data. Our specific aim was to use these techniques to examine the association of provider continuity of care in the first year of life with health care use and receipt of recommended preventive care from ages 1 to 3 years. We hypothesized that improved continuity in infancy would be associated with decreased urgent health encounters and improved preventive care in early childhood.
Methods
Setting and Study Population
The sample population was a prospectively-constructed birth cohort of children born in 2007 to 2008 establishing care by age 4 months at 1 of 30 clinics within The Children’s Hospital of Philadelphia’s (CHOP’s) greater Philadelphia primary care network (n = 22 900) in urban and suburban settings. Inclusion criteria included a minimum of 3 well visits and 5 total primary care visits within the first year of life to improve the opportunity for meaningful continuity (n = 22 104). In addition, participants were required to have a minimum of 1 encounter during ages 1 to 3 years as well as 1 encounter beyond age 3 to exclude complete loss of follow-up over the evaluation period (n = 17 773). Providers documented patient information in the electronic health record by using the EPIC Hyperspace system (EPIC manufacturing, Verona, WI).
Definition of Continuity
Continuity was measured during the first 12 months of life (see Fig 1). Several indices have been developed to measure continuity, 2 of which were used. The Usual Provider of Care (UPC) score is a commonly-used measure that is relatively easy to interpret.19 It is calculated by: # of primary care visits with the most commonly seen provider / total # of primary care visits (including well and sick visits). Another measure, the Bice and Boxerman index, accounts for continuity with a small core of providers rather than a single provider only, but the numerical value can be more difficult to calculate and interpret.20 A recent study demonstrated strong correlation between 4 commonly used measures, including the UPC and Bice and Boxerman index.21 For this reason, and for its ease of calculation and interpretation, we selected the UPC index (divided into quartiles), although we also calculated continuity by using the Bice and Boxerman index. A separate UPC index was calculated across well visits only. The attending physician or nurse practitioner was coded as the encounter provider. Residents see patients in 4 continuity clinics, but these encounters constitute the minority of visits at these sites.
FIGURE 1.
Timing of the measurements of continuity and outcomes.
Confounding Variable Definitions
Gestational age, sex, and race/ethnicity were obtained from the electronic medical record. Zip code-level neighborhood demographics (high school graduation rate, percentage below poverty, median income) were obtained. Insurance was categorized as: (1) self-pay: any visit with no insurance; (2) any use of Medicaid (including the Children’s Health Insurance Plan) with no self-pay encounters; or (3) sole use of private insurance.
Chronic Disease Status
We dichotomized children into categories by the presence or absence of chronic conditions using the comprehensive list of International Classification of Diseases, Ninth Revision (ICD-9) codes used in previous studies (see Supplemental Information).22–28 In accordance with previous studies, a minimum of two 493.XX codes were required to meet asthma criteria.8,10,29
Health Care Utilization and Preventive Care Variable Definitions
All outcomes were measured from ages 12 to 36 months to ensure the outcome occurred after the measurement of continuity. We analyzed the number of primary care as well as number of well visits and sick visits. Well visits were defined as any encounter with an ICD-9 code of V20.0, V20.1, or V70.0. ED visits and hospitalizations were analyzed in our Center City population only, a cohort that received care at 1 of 5 clinics and who reliably used CHOP for these encounters (n = 4200). A detailed description of this methodology has been described previously.11
We further categorized an admission as an ACSH using a modified list of conditions created by the Agency for Healthcare Research and Quality, which excluded adult-specific conditions.30,31 In accordance with a previous study, we included acute respiratory tract infections (ICD-9 codes 464, 466), pneumococcal meningitis (ICD-9 code 320.1), streptococcal meningitis (ICD-9 code 320.2), and Haemophilus influenzae sepsis (ICD-9 code 038.41), because they are pertinent to young children and/or are vaccine preventable.10
Subjects were considered up-to-date on immunizations if they received all recommended vaccines through 18 months, excluding influenza. Influenza vaccination status was assessed in the second eligible winter because this outcome occurred after measurement of continuity. It was defined as (1) receiving 1 dose in their second eligible winter after receiving 2 doses in their first eligible winter, or (2) receiving 2 doses spaced 4 weeks apart during their second eligible winter if they did not receive 2 doses their first winter.32 On the basis of current guidelines, we evaluated the receipt of anemia and lead screening by age 12 months in the Medicaid population only (n = 4480).33
Statistical Analysis
We used multiple methods to improve causal inference between continuity and outcomes: (1) establishing separate intervals for measuring continuity and assessing outcomes, (2) generating a propensity score to balance covariates between continuity quartiles, and (3) incorporating the propensity score and other confounders in multivariable regression models.
To construct the regression models, we identified patient factors (sex, gestational age, presence of chronic condition) and sociodemographics (race, insurance, neighborhood demographics) associated with continuity by using descriptive statistics and univariable analyses, including χ2 tests, t tests, and analysis of variance for parametric continuous data. Nonparametric tests such as the Wilcoxon rank sum test and the Kruskal-Wallace test were used where appropriate. Variables were included in regression models if they were associated with continuity at a P value of <.10. We included interaction terms when there was a priori suggestion of effect modification and the test of homogeneity produced a P value <.05. We analyzed the association between continuity and outcomes in unadjusted and adjusted logistic, linear, and Poisson regression models. Zero-inflated negative binomial regression models were used for outcome variables with excess zeroes and a nonparametric distribution (eg, hospitalizations).
We constructed a propensity score to achieve better balance of covariates between quartiles.17 Propensity scores predict who, on the basis of baseline characteristics, is most likely to receive treatment or be exposed, in this case the lowest continuity quartile compared with the highest. The score was generated by selecting variables known to be associated with continuity as well as those that reached statistical significance in our univariable analyses (P < .10), which included gestational age, chronic condition, race, insurance, neighborhood demographics, and clinic site.
Regression model 1 adjusts for patient factors and sociodemographic factors that were associated with continuity, including sex, gestational age, presence of any chronic condition, asthma diagnosis, race, insurance, neighborhood demographics, and the propensity score. Clustering at the site of the clinic was accounted for with clustered SEs. We then created model 2 by adding clinic site as a covariate to further address clustering. Sick visits in the first 12 months of life were added to model 3 because they may indicate illness severity not captured by chronic condition diagnoses, and may also reflect parental health utilization behaviors.34
We conducted several secondary analyses: (1) well visit only continuity versus total primary care continuity, (2) stratification by presence or absence of chronic conditions, and (3) continuity by using the Bice and Boxerman index. Data were analyzed by using Stata version 12 (StataCorp LP, College Station, TX). The CHOP Institutional Review Board approved this study.
Results
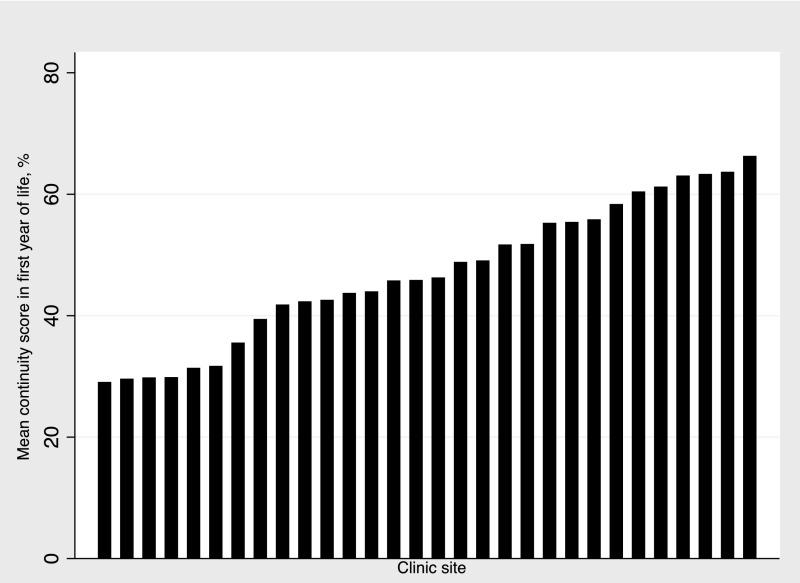
The mean UPC score was 0.28 in the lowest quartile compared with 0.78 in the highest quartile (see Table 1). Mean UPC score varied widely across the 30 clinic sites with a range of 0.29 to 0.66 (see Fig 2). Children with chronic conditions comprised a larger portion of the lowest continuity quartile (30.2% vs 28.2% of highest quartile; P = .03); this was driven by clustering of asthmatic patients in the lowest quartile (8.8% vs 5.9%; P < .001). After adjustment for patient and neighborhood factors, white race (adjusted odds ratio [aOR] 1.43; 95% confidence interval [CI] 1.25–1.64), Medicaid insurance (aOR 1.41; 95% CI 1.23–1.61), male sex (aOR 1.10; 95% CI 1.00–1.21), higher gestational age (aOR 1.03 for each week older; 95% CI 1.00–1.05), and a diagnosis of asthma (aOR 1.59; 95% CI 1.30–1.93) were associated with increased odds of being in the lowest continuity quartile (data not shown). In unadjusted analyses, those in the lowest quartile had more sick visits, ED visits, hospitalizations, and ACSHs (see Table 2). Children in the lowest continuity quartile were also less likely to be up-to-date on routine immunizations (61% vs 65%; P < .001) and to have received anemia (68.0% vs 89.0%; P < .001) and lead screenings (43.2% vs 78.3%; P < .001).
TABLE 1.
Patient Demographics, a Comparison of the Lowest and Highest Continuity Quartiles
| Lowest Quartile (n = 4781) | Highest Quartile (n = 4366) | P | |
|---|---|---|---|
| UPC score, mean (SD) | 0.28 (0.05) | 0.78 (0.10) | — |
| Infant demographics | |||
| Sex, % male | 51.9 | 49.4 | .02 |
| Gestational age, wk, mean (SD) | 38.8 (2.0) | 38.7 (2.2) | <.001 |
| Gestational age, % | .09 | ||
| <28 wk | 0.4 | 0.6 | |
| 28–31 and 6/7 wk | 1.1 | 1.0 | |
| 32–36 and 6/7 wk | 8.0 | 9.2 | |
| 37 wk and greater | 90.5 | 89.2 | |
| Race, % | <.001 | ||
| White | 67.7 | 55.2 | |
| Black | 28.6 | 40.5 | |
| Other | 3.7 | 4.0 | |
| Insurance status, % | <.001 | ||
| Private | 57.9 | 54.3 | |
| Medicaid | 24.9 | 28.7 | |
| Self-pay | 18.2 | 17.0 | |
| Chronic medical conditions | |||
| Presence of a chronic condition, % | 30.2 | 28.2 | .03 |
| Chronic illness not including asthma | 24.5 | 24.6 | .89 |
| Asthma | 8.8 | 5.9 | <.001 |
—, not applicable.
FIGURE 2.
Mean continuity in first year of life by clinic site.
TABLE 2.
Health Care Utilization and Receipt of Preventive Care From Ages 1–3 y, a Comparison of the Lowest and Highest Continuity Quartiles
| Lowest Quartile | Highest Quartile | P | |
|---|---|---|---|
| Health care utilization, mean (SD) | |||
| Acute care visitsa | |||
| ED visits | 3.2 (4.0) | 2.2 (3.1) | <.001 |
| Hospitalizations | 0.7 (2.2) | 0.5 (1.9) | .01 |
| ACSHs | 0.2 (0.7) | 0.1 (0.6) | <.001 |
| Primary care visits | |||
| All visits | 11.0 (6.1) | 8.7 (4.7) | <.001 |
| Well visits | 3.6 (0.9) | 3.7 (0.9) | .03 |
| Sick visits | 6.9 (5.6) | 4.5 (4.1) | <.001 |
| Receipt of preventative services, % | |||
| Immunization up-to-date | |||
| Routine, through 18 mo | 60.6 | 65.0 | <.001 |
| Influenza, second eligible winter | 40.2 | 39.9 | .74 |
| Anemia screening, by 12 mob | 68.0 | 89.0 | <.001 |
| Lead screening, by 12 mob | 43.2 | 78.3 | <.001 |
Center City practices only.
Medicaid only.
After adjustment for patient characteristics (model 1), clinic site (model 2), and sick visits in the first 12 months (model 3), many of our findings remained significant (see Table 3). Although ED visits were no longer significant in model 3, those in the lowest quartile had nearly a threefold increased risk of an ACSH (adjusted incidence rate ratio [aIRR] 2.74; 95% CI 1.49–5.03). The lowest quartile also had a slight but statistically significant decrease in well visits (aIRR 0.97; 95% CI 0.95–0.99) and increase in sick visits (aIRR 1.08; 95% CI 1.05–1.11). The lowest quartile had 39% lower odds of receiving lead screening (95% CI 0.46–0.79).
TABLE 3.
Adjusted Model of Health Care Utilization and Primary Care Outcomes, a Comparison of the Lowest and Highest Continuity Quartiles
| Lowest Versus Highest (ref) Quartile | |||
|---|---|---|---|
| Model 1a | Model 2b | Model 3c | |
| Health care utilization | |||
| Acute care encounters, aIRR (95% CI)d | |||
| ED visits | 1.15 (1.05–1.25)e | 1.10 (1.00–1.21)e | 1.07 (0.97–1.19) |
| Hospitalizations | 0.99 (0.84–1.17) | 0.98 (0.85–1.14) | 0.97 (0.84–1.13) |
| ACSHs | 2.66 (1.46–4.86)e | 2.89 (1.61–5.19)e | 2.74 (1.49–5.03)e |
| Primary care visits, aIRR (95% CI) | |||
| Total | 1.06 (1.03–1.10)e | 1.06 (1.03–1.09)e | 1.01 (0.99–1.03) |
| Well | 0.98 (0.96–0.99)e | 0.97 (0.95–0.99)e | 0.97 (0.95–0.99)e |
| Sick | 1.15 (1.09–1.21)e | 1.16 (1.12–1.21)e | 1.08 (1.05–1.11)e |
| Receipt of preventative services | |||
| Immunizations up-to-date, aOR (95% CI) | |||
| Routine, through 18 mo | 1.06 (0.89–1.26) | 0.93 (0.77–1.11) | 0.92 (0.77–1.10) |
| Influenza, second eligible winter | 1.07 (0.95–1.20) | 1.05 (0.93–1.17) | 1.02 (0.91–1.14) |
| Anemia screening, by 12 mo, aOR (95% CI)f | 0.73 (0.54–0.99)e | 0.88 (0.68–1.16) | 0.85 (0.64–1.13) |
| Lead screening, by 12 mo, aOR (95% CI)f | 0.61 (0.51–0.72)e | 0.62 (0.47–0.81)e | 0.61 (0.46–0.79)e |
Adjusted for sex, gestational age, presence of any chronic condition, asthma diagnosis, race, insurance type, neighborhood census data, and propensity score.
Model 1 covariates plus clinic site.
Model 1 covariates plus clinic site and # of sick visits in first year of life.
Center City practice only.
P value < .05
Medicaid only.
Continuity measured across well visits only did not yield any statistically significant differences in outcomes (data not shown). Stratification by presence of a chronic condition showed different effect sizes for ACHSs and lead screening outcomes (data not shown). For those with chronic conditions, the odds of having any ACSH was 2.81 times higher in the lowest versus highest quartile (95% CI 1.21–6.53), whereas it did not meet statistical significance in healthy children (aOR 1.94; 95% CI 0.99–3.78). The odds of receiving lead screening was 50% lower in the chronic condition cohort (aOR 0.50; 95% CI 0.39–0.66), but not in the healthy cohort (aOR 0.70; 95% CI 0.48–1.02). Calculating continuity with the Bice and Boxerman index had a slightly different impact on outcomes (data not shown). As opposed to the UPC, ED visits were slightly increased in the lowest quartile (aIRR 1.13; 95% CI 1.05–1.21). There was a similar impact on ACSHs (aIRR 2.82; 95% CI 1.42–5.60) and lead screening in the lowest quartile (aOR 0.58; 95% CI 0.46–0.72).
Discussion
Higher continuity in infancy is linked to decreased ACSHs and improved receipt of preventive care, particularly for children with chronic conditions. This is the first study to demonstrate both decreased utilization and improved receipt of preventive care in a single cohort. We also found that continuity across all primary care visits was linked to outcomes, whereas continuity across well visits was not.
The link between continuity and ASCHs is important because ACSHs are potentially preventable and related to ambulatory quality, with billed charges exceeding $4 billion in a single year.35 Tom et al10 was the first to demonstrate a link between continuity and pediatric ACSHs. The impact of continuity for children with chronic conditions in their study was similar to our results. Contrary to other studies, we did not find an association with ED visits, except a small increase in the lowest quartile as measured by the Bice and Boxerman index. ED visits were only measured in our Center City population, which may have limited our ability to detect an association between continuity and ED use. One additional possibility is our inclusion of sick visits in the first year.8,9 Increased ambulatory visits have been linked to ED utilization and may reflect illness severity.36 Increased visits may also be caused by variation in parental health behaviors such as differing thresholds to bring children to care.37 Although we did not capture ambulatory-sensitive ED visits in our data set, the authors of a recent article demonstrated that nearly 1 in 7 ED visits may be preventable, and thus associated with continuity.38
In addition to reducing costly health encounters, our data on lead screening demonstrate the positive association of continuity and improved preventive care, which mirrors findings of previous work.12 Providers who are more familiar with their patients may have more time to address routine screening topics. Parents who received higher continuity demonstrate higher knowledge of anticipatory guidance topics, such as dentition and nutrition.39
Several patient- and provider-level factors may influence the link between continuity and outcomes. Parent satisfaction correlates with continuity and may mediate this association.40,41 Continuity influences parental trust and perceptions of care quality and coordination.40–42 One study demonstrated that comprehensive access to ambulatory-based urgent visits, especially with their primary provider, is associated with higher continuity and better care coordination.41
Potential solutions exist at multiple levels. Availability of sick visits with ambulatory providers decreases ED use, suggesting that improving the availability of these slots may reduce costs overall by reducing high-cost encounters.43,44 The creation of accountable care organizations under the PPACA can link the costs of strengthening continuity with savings from fewer high-cost urgent encounters. Furthermore, scheduling protocols with protected sick appointments can improve continuity.44 Also, a continuity index may be a useful quality measure to provide timely and meaningful feedback. The results from our data reveal that continuity with a small group may be as effective as or more effective than continuity with a single provider, which has been demonstrated in adults and ED use.45 This strategy may also be more feasible to implement. Discussing benefits of continuity with families may also improve continuity.
This study has limitations. Data were observational and obtained from an electronic health record designed for clinical purposes. Unmeasured confounders or mediators may exist that we could not account for. Furthermore, it is possible that patients seen in clinics with high continuity have different health behaviors and differential use. We used multiple methods, however, to account for clustering. Also, data on ED visits, hospitalizations, and ACSHs were limited to our Center City population, which has a higher proportion of black and Medicaid patients. Thus, some of the outcomes may be limited by insufficient power or may be less generalizable.
The results of our data reveal the value of the medical home, which is particularly important given uncertainty in health care reform. Cost savings and improved patient outcomes may be realized if health systems and insurance companies strengthen the medical home and improve continuity across all ambulatory visits. Provider continuity is key to high-quality pediatric primary care.
Acknowledgments
We would like to acknowledge Ashley E. Martin, MPH, and Jo Ann D’Agostino, DNP, CRNP, from the Center for Outcomes Research at The Children’s Hospital of Philadelphia for their valuable contributions to this protocol and manuscript.
Glossary
- ACSH
ambulatory care-sensitive hospitalization
- aIRR
adjusted incidence rate ratio
- aOR
adjusted odds ratio
- CHOP
The Children’s Hospital of Philadelphia
- CI
confidence interval
- ED
emergency department
- ICD-9
International Classification of Diseases, Ninth Revision
- PPACA
Patient Protection and Affordable Care Act
- UPC
Usual Provider of Care
Footnotes
Dr Enlow conceptualized and designed the study, conducted the initial analyses, and drafted the initial manuscript; Ms Passarella assisted with data collection and analysis and reviewed and revised the manuscript; Dr Lorch coordinated and supervised data collection and data analysis and critically reviewed the manuscript; and all authors approved the final manuscript as submitted.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: All phases of this study were supported by the National Institutes of Health grant R01 HD057168. Dr Enlow also received support from the Ruth L. Kirschstein National Research Service Award T32 HL098054. Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
References
- 1.Long WE, Bauchner H, Sege RD, Cabral HJ, Garg A. The value of the medical home for children without special health care needs. Pediatrics. 2012;129(1):87–98 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Medical Home Initiatives for Children With Special Needs Project Advisory Committee; American Academy of Pediatrics . The medical home. Pediatrics. 2002;110(1 pt 1):184–186 [PubMed] [Google Scholar]
- 3.Cabana MD, Jee SH. Does continuity of care improve patient outcomes? J Fam Pract. 2004;53(12):974–980 [PubMed] [Google Scholar]
- 4.Chu HY, Chen CC, Cheng SH. Continuity of care, potentially inappropriate medication, and health care outcomes among the elderly: evidence from a longitudinal analysis in Taiwan. Med Care. 2012;50(11):1002–1009 [DOI] [PubMed] [Google Scholar]
- 5.Nyweide DJ, Anthony DL, Bynum JP, et al. Continuity of care and the risk of preventable hospitalization in older adults. JAMA Intern Med. 2013;173(20):1879–1885 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Leleu H, Minvielle E. Relationship between longitudinal continuity of primary care and likelihood of death: analysis of national insurance data. PLoS One. 2013;8(8):e71669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chen CC, Tseng CH, Cheng SH. Continuity of care, medication adherence, and health care outcomes among patients with newly diagnosed type 2 diabetes: a longitudinal analysis. Med Care. 2013;51(3):231–237 [DOI] [PubMed] [Google Scholar]
- 8.Christakis DA, Mell L, Koepsell TD, Zimmerman FJ, Connell FA. Association of lower continuity of care with greater risk of emergency department use and hospitalization in children. Pediatrics. 2001;107(3):524–529 [DOI] [PubMed] [Google Scholar]
- 9.Brousseau DC, Meurer JR, Isenberg ML, Kuhn EM, Gorelick MH. Association between infant continuity of care and pediatric emergency department utilization. Pediatrics. 2004;113(4):738–741 [DOI] [PubMed] [Google Scholar]
- 10.Tom JO, Tseng CW, Davis J, Solomon C, Zhou C, Mangione-Smith R. Missed well-child care visits, low continuity of care, and risk of ambulatory care-sensitive hospitalizations in young children. Arch Pediatr Adolesc Med. 2010;164(11):1052–1058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.D’Agostino JA, Passarella M, Saynisch P, Martin AE, Macheras M, Lorch SA. Preterm infant attendance at health supervision visits. Pediatrics. 2015;136(4). Available at: www.pediatrics.org/cgi/content/full/136/4/e794 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Flores AI, Bilker WB, Alessandrini EA. Effects of continuity of care in infancy on receipt of lead, anemia, and tuberculosis screening. Pediatrics. 2008;121(3). Available at: www.pediatrics.org/cgi/content/full/121/3/e399 [DOI] [PubMed] [Google Scholar]
- 13.HHS The Affordable Care Act supports patient-centered medical homes in health centers. Available at: www.hhs.gov/news/press/2014pres/08/20140826a.html. Accessed October 5, 2015
- 14.Rosenthal MB. Beyond pay for performance–emerging models of provider-payment reform. N Engl J Med. 2008;359(12):1197–1200 [DOI] [PubMed] [Google Scholar]
- 15.Zamora A. Patient-centered medical homes. Health Aff (Millwood). 2012;31(6):1369. [DOI] [PubMed] [Google Scholar]
- 16.Davis K, Abrams M, Stremikis K. How the Affordable Care Act will strengthen the nation’s primary care foundation. J Gen Intern Med. 2011;26(10):1201–1203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.D’Agostino RB., Jr Propensity score methods for bias reduction in the comparison of a treatment to a non-randomized control group. Stat Med. 1998;17(19):2265–2281 [DOI] [PubMed] [Google Scholar]
- 18.Newgard CD, Hedges JR, Arthur M, Mullins RJ. Advanced statistics: the propensity score–a method for estimating treatment effect in observational research. Acad Emerg Med. 2004;11(9):953–961 [DOI] [PubMed] [Google Scholar]
- 19.Breslau N, Reeb KG. Continuity of care in a university-based practice. J Med Educ. 1975;50(10):965–969 [DOI] [PubMed] [Google Scholar]
- 20.Bice TW, Boxerman SB. A quantitative measure of continuity of care. Med Care. 1977;15(4):347–349 [DOI] [PubMed] [Google Scholar]
- 21.Pollack CE, Hussey PS, Rudin RS, Fox DS, Lai J, Schneider EC. Measuring care continuity: a comparison of claims-based methods. Med Care. 2016;54(5):e30–e34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ireys HT, Anderson GF, Shaffer TJ, Neff JM. Expenditures for care of children with chronic illnesses enrolled in the Washington State Medicaid program, fiscal year 1993. Pediatrics. 1997;100(2 pt 1):197–204 [DOI] [PubMed] [Google Scholar]
- 23.Feudtner C, Christakis DA, Connell FA. Pediatric deaths attributable to complex chronic conditions: a population-based study of Washington State, 1980-1997. Pediatrics. 2000;106(1 pt 2):205–209 [PubMed] [Google Scholar]
- 24.Feudtner C, Hays RM, Haynes G, Geyer JR, Neff JM, Koepsell TD. Deaths attributed to pediatric complex chronic conditions: national trends and implications for supportive care services. Pediatrics. 2001;107(6). Available at: www.pediatrics.org/cgi/content/full/107/6/e99 [DOI] [PubMed] [Google Scholar]
- 25.Neuzil KM, Wright PF, Mitchel EF Jr, Griffin MR. The burden of influenza illness in children with asthma and other chronic medical conditions. J Pediatr. 2000;137(6):856–864 [DOI] [PubMed] [Google Scholar]
- 26.Seferian EG, Lackore KA, Rahman AS, Naessens JM, Williams AR. Comparison of chronic illness among children receiving mechanical ventilation in a cohort of children’s hospitals in 1991 and 2001. J Pediatr. 2006;149(6):788–792 [DOI] [PubMed] [Google Scholar]
- 27.Valentine JM, Neff J, Park AN. Pediatric hospitalization patterns for selected chronic health conditions using hospital abstract reporting system data: methods and findings. Health Serv Outcomes Res Methodol. 2000;1(3–4):335–350 [Google Scholar]
- 28.Fowler JF, Gallagher PM, Homer CJ. Identifying children with special needs. In: Cynamon ML, Kulka RA, eds. Seventh Conference on Health Survey Research Methods. Hyattsville, MD: Department of Health and Human Services; 2001: 181–188 [Google Scholar]
- 29.Lozano P, Connell FA, Koepsell TD. Use of health services by African-American children with asthma on Medicaid. JAMA. 1995;274(6):469–473 [PubMed] [Google Scholar]
- 30.Billings J, Zeitel L, Lukomnik J, Carey TS, Blank AE, Newman L. Impact of socioeconomic status on hospital use in New York City. Health Aff (Millwood). 1993;12(1):162–173 [DOI] [PubMed] [Google Scholar]
- 31.Agency for Healthcare Research and Quality AHRQ Quality Indicators-Guide to Prevention Quality Indicators: Hospital Admission for Ambulatory Care Sensitive Conditions. Appendix A. Rockville, MD: AHRQ; 2001 [Google Scholar]
- 32.Fiore AE, Shay DK, Haber P, et al. ; Advisory Committee on Immunization Practices (ACIP), Centers for Disease Control and Prevention (CDC) . Prevention and control of influenza. Recommendations of the Advisory Committee on Immunization Practices (ACIP), 2007. MMWR Recomm Rep. 2007;56(RR-6):1–54 [PubMed] [Google Scholar]
- 33.American Academy of Pediatrics Committee on Environmental Health Lead exposure in children: prevention, detection, and management. Pediatrics. 2005;116(4):1036–1046 [DOI] [PubMed] [Google Scholar]
- 34.Christakis DA, Kazak AE, Wright JA, Zimmerman FJ, Bassett AL, Connell FA. What factors are associated with achieving high continuity of care? Fam Med. 2004;36(1):55–60 [PubMed] [Google Scholar]
- 35.Lu S, Kuo DZ. Hospital charges of potentially preventable pediatric hospitalizations. Acad Pediatr. 2012;12(5):436–444 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Flood C, Sheehan K, Crandall M. Predictors of emergency department utilization among children in vulnerable families [published online ahead of print March 8, 2016]. Pediatr Emerg Care. doi: 10.1097/PEC.0000000000000658 [DOI] [PubMed] [Google Scholar]
- 37.Nelson BB, Coller RJ, Saenz AA, et al. How avoidable are hospitalizations for children with medical complexity? Understanding parent perspectives. Acad Pediatr. 2016;16(6):579–586 [DOI] [PubMed] [Google Scholar]
- 38.Jaeger MW, Ambadwar PB, King AJ, Onukwube JI, Robbins JM. Emergency care of children with ambulatory care sensitive conditions in the United States. J Emerg Med. 2015;49(5):729–739 [DOI] [PubMed] [Google Scholar]
- 39.Bradford WD, Kaste LM, Nietert PJ. Continuity of medical care, health insurance, and nonmedical advice in the first 3 years of life. Med Care. 2004;42(1):91–98 [DOI] [PubMed] [Google Scholar]
- 40.Christakis DA, Wright JA, Zimmerman FJ, Bassett AL, Connell FA. Continuity of care is associated with high-quality careby parental report. Pediatrics. 2002;109(4). Available at: www.pediatrics.org/cgi/content/full/109/4/e54 [DOI] [PubMed] [Google Scholar]
- 41.Christakis DA, Wright JA, Zimmerman FJ, Bassett AL, Connell FA. Continuity of care is associated with well-coordinated care. Ambul Pediatr. 2003;3(2):82–86 [DOI] [PubMed] [Google Scholar]
- 42.Horn IB, Mitchell SJ, Wang J, Joseph JG, Wissow LS. African-American parents’ trust in their child’s primary care provider. Acad Pediatr. 2012;12(5):399–404 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sturm JJ, Hirsh DA, Lee EK, Massey R, Weselman B, Simon HK. Practice characteristics that influence nonurgent pediatric emergency department utilization. Acad Pediatr. 2010;10(1):70–74 [DOI] [PubMed] [Google Scholar]
- 44.Fortuna RJ, Garfunkel L, Mendoza MD, et al. Factors associated with resident continuity in ambulatory training practices. J Grad Med Educ. 2016;8(4):532–540 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Werner RM, Canamucio A, Marcus SC, Terwiesch C. Primary care access and emergency room use among older veterans. J Gen Intern Med. 2014;29(suppl 2):S689–S694 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.