Abstract
Background
Mothers In Motion (MIM), a randomized controlled trial, aimed to help young, low-income overweight and obese mothers prevent weight gain by promoting stress management, healthy eating, and physical activity. This paper describes MIM recruitment challenges and reports demographic characteristics affecting enrollment.
Methods
Participants who were African American or Non-Hispanic White were recruited from the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) in Michigan. We faced numerous recruitment challenges and learned that several strategies facilitated recruitment. Logistic regression analyses were performed to examine demographic characteristics that affect enrollment.
Results
Women who had a higher body mass index (BMI, OR 1.06, 95% CI 1.02–1.10); were at late postpartum, (OR 1.24, 95% CI 1.10–1.40), were breastfeeding (OR 5.0, 95% CI 2.34–10.65); or were at early postpartum and breastfeeding (OR 0.42, 95% CI 0.22–0.81) were more likely to enroll than their counterparts. Compared to African American women, Non-Hispanic White women were more likely to enroll (OR 1.77, 95% CI 1.29–2.42). Also, women who were non-smokers (OR 0.54, 95% CI 0.40–0.73) or had a higher education were more likely to enroll (OR 1.21, 95% CI 1.04–1.42) than those who smoked or had a lower education.
Conclusion
Future lifestyle behavioral intervention studies for similar target audiences may consider tailoring their recruitment messages based on relevant participant demographic characteristics identified as potential determinants of enrollment in this study.
Trial registration
Clinical Trials NCT01839708.
Keywords: Obesity, Lifestyle behavior, Low-income women, Enrollment, Recruitment
1. Introduction
Interventions to reduce medical costs associated with overweight and obesity [1], [2] are currently limited by lack of effective strategies to address the exceptional needs of young low-income overweight and obese mothers. To have a broad public health impact on obesity, we conducted Mothers In Motion (MIM), a theory-based culturally sensitive intervention, aimed to help low-income overweight and obese young mothers prevent weight gain by promoting stress management, healthy eating, and physical activity.
Recruitment challenges have been well-documented. McDonald et al. [3] reviewed 122 trials and found that only 31% of studies reached their original recruitment target number; about 24% of studies recruited at least 80% of but less than 100% of target numbers. The authors also found that about 35% of studies had to reduce the intended sample size. Of studies reducing sample size, about 45% of studies reached the revised target number. Moreover, about 58% of the reviewed studies requested extensions from the funding agencies and 41% delayed the start of recruitment. Even though 75% of studies identified their study sites during the grant application stage, about 20% of studies had pre-identified sites that did not participate as planned, due to a variety of reasons, e.g., problems with funding and delays in recruitment. Foy et al. [4] evaluated the recruitment of dyspepsia management studies and found that about 43% (3/7) of such studies closed prematurely due to poor recruitment and 57% (4/7) extended their length of recruitment. Even with extended length of recruitment, only 1 trial met its target number.
Reduced enrollment rates, which is not typically reported by intervention studies may influence sample representation and study validity. In general, the enrollment rate ranges from 60% to 77% and differs by the purpose of the interventions and target populations. Reported study enrollment rates for low-income young mothers are typically around two-thirds (66% for an African American caregiver feeding and preschooler body weight intervention [5] to 68% for a birth control intervention reaching a predominantly White target audience [6]). A smoking relapse prevention program for low-income postpartum women reported enrollment rates of 60% for the intervention group and 92% for the comparison group [7]. Enrollment rates for studies of pregnant women ranged from 69% (pregnancy weight gain intervention for overweight and obese women who were predominantly White) [8] to 90% (behavioral intervention to reduce smoking, depression and violence for low-income African Americans and Latinas) [9]. Enrollment rates for middle aged adults have fallen in a similar range. For example, diabetes self-management studies showed a 59% enrollment rate for African Americans [10] and 71% for overweight and obese adults with diverse racial and ethnic backgrounds [11]. Enrollment was about 76% for a weight management program for overweight and obese adults [12] and 77% for obese adults with hypertension [13]. Factors that influence enrollment rate have not been reported by previous studies and determinants of this important aspect of program planning have been noted as nearly impossible to identify [12]. This paper describes recruitment challenges and examines the relationships among demographic characteristics and enrollment.
2. Methods
2.1. Setting and participants
Our MIM was conducted in partnership with The Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) at the state and local levels in Michigan. WIC is a federally funded community program that provides health screening, specific nutrient-dense food benefits and nutrition consultation and makes health and community agency referrals for women who are pregnant, breastfeeding, or postpartum and for infants and young children up to age 5 years old. To be eligible to enroll in WIC, an individual must have an income at or below 185% of the federal poverty line. A detailed description of setting and study criteria has been published [14]. Briefly, participants were Non-Hispanic White or African American women who were between 18 and 39 years old, between 6 weeks and 5 years postpartum, overweight or obese (BMI 25.0–39.9 kg/m2), and had no self-reported type 1 or type 2 diabetes. All participants were recruited from 5 collaborating WIC agencies (10 WIC offices) in Michigan. Nearly 76% of clients in these WIC agencies had incomes at or below 130% of the federal poverty line.
2.2. Recruitment strategies, challenges, and lessons learned
Our recruitment and enrollment were about 5 months behind the initial timeline due to a delay of intervention development. Still, the project was able to enroll 634 women, which exceeded the target number (N = 525) in 28 months. We purposely oversampled participants because we planned to exclude data from women who became pregnant during the trial and a recent Michigan WIC report showed an overall increase in pregnancy rates (∼5%) for our target population.
2.3. Recruitment strategies
Women coming to our collaborating WIC agencies during the data collection dates (September 2012 to January 2015) were personally invited by peer recruiters (who were themselves WIC mothers) to participate while waiting for their appointments.
The recruiters were trained to be culturally sensitive, to build rapport quickly and to relate to the potential participants. Training emphasized using a gentle and caring voice, demonstrating understanding, empathy, and excitement about the study while maintaining eye contact, and offering assistance with small tasks [15]. Recruiters explained the study purpose, confidentiality and study requirements and emphasized the MIM's flexible schedule and its easy, no-cost availability. WIC mothers who were not interested in participation filled out the demographic survey. Those who were interested filled out both demographic and screening surveys based on the study criteria.
We learned from our pilot MIM [16] that not fully understanding the study requirements and incentives was one of the key factors leading to a high dropout rate. Therefore, we conducted cognitive interviews to develop an easy-to-read flyer (pictorial) that outlined the study's purpose, expectations, and incentives as presented in the consent form. Also, we implemented sequential screening to minimize a potential high dropout. A detailed description of sequential screening (screening I and II) has been published [14]. Screening I. Briefly, eligible participants read the flyer, then the recruiters interviewed them to assess their understanding of study requirements and their interest in participation. The recruiters would obtain consent from eligible women only if the women could demonstrate understanding of the study requirements. Screening II. Consented women were required to complete a baseline phone interview before returning to their WIC office (in person) to be randomized and enrolled within 2 weeks of signing the consent form. The study procedure was approved and monitored by the Michigan State University and Michigan Department of Community Health Institutional Review Boards.
2.4. Recruitment challenges and lessons learned
Based on lessons learned from our previous pilot of MIM [14], we implemented numerous strategies to enhance recruitment but still experienced 6 major challenges. Below, we described these challenges and strategies recommended to minimize them. We monitored enrollment rate on a monthly basis by recruiters and study sites (WIC agencies).
2.4.1. Gaining access to study sites
When our proposal was submitted, 4 WIC agencies had agreed to collaborate with us. To increase our recruitment pool, we intended to expand the study sites from 4 to 6–7 WIC agencies, but only 1 of the 4 local WIC agencies that we contacted agreed to collaborate. When recruitment started in Year 2, 1 of the original local partner agencies had to be eliminated because of personnel change and disruptions caused by building remodeling. In Year 3, we eliminated another site because of persistent recruitment protocol violations (described later). To maintain our recruitment pool, we worked with the State of Michigan WIC to identify 2 more potential agencies. After 10 months of contract negotiations, we were able to recruit participants at 1 of the new sites. We have worked with WIC for more than a decade and learned that personnel changes greatly affect an agency's readiness for collaboration. Negative perceptions of working with researchers, fear of adding to existing staff burdens, or competing priorities may have further exacerbated the difficulties we experienced in identifying suitable sites for recruitment [17].
2.4.2. Closing a study site
In the middle of recruitment, we discontinued recruitment activities at 1 WIC agency that is located in an urban area because hiring and training a qualified peer recruiter was taking an inordinate amount of time and effort, exacerbated by the travel needed to supervise recruiters at this distant location (described below). Some recruiters chose to leave before their first day of work. Others violated the study protocols (e.g., only screening normal weight or morbidly obese women who were not part of our target audience). Some participants from this site withdrew shortly after enrolling. These problems were compounded by the fact that we were unable to reach nearly 70% of consented participants to complete the baseline phone interview because of wrong numbers or inability to reach by phone. We subsequently learned that participation was hindered by the extremely dangerous neighborhoods in this location. After enrolling only 22 women during 3 months of enrollment efforts at 3 WIC offices in this urban area (60–70 women were expected), we closed the site and discontinued study activities with the remaining participants from this location [17].
2.4.3. Ineffective recruitment flyer
A lack of interest in modifying eating behavior and physical activity for the mothers themselves might have been a key barrier to recruitment at the start of our study. Initially, our recruitment flyers and our recruiters' comments focused on healthy eating and physical activity as desired outcomes. About the second month of recruitment, we learned that the flyer and emphasis were ineffective. Thus, we worked with WIC administrators at collaborating local agencies to emphasize stress management, no-cost, convenience, and happier and healthier family, and deemphasize healthy eating and physical activity. We posted the flyer at more strategic locations in WIC offices, food pantries and low-income housing areas. The flyers posted in the WIC offices yielded some interest and inquiries, subsequently a few screened and enrolled. The flyers posted in other locations yielded a few calls and resulted in no screening [17].
2.4.4. Participant failure to respond to calls from the study office
At the first few months of recruitment, we could not reach many consented participants to schedule the baseline phone interviews because they did not answer the calls with caller IDs from outside their area code. Based on advice from community partners, our recruiters started emphasizing and reminding participants of the area code of the study office number so that we were able to reach most of them to schedule the baseline phone interview [17].
2.4.5. Emphasizing study incentives
In the first 3 months of recruitment, most recruiters emphasized the study incentives, e.g., a large box of diapers. As a result, we had about 43% enrollment rate. The diaper incentives were not helpful overall. Many participants called the study office to request a specific diaper size or express urgent need for diapers; they said that diapers and incentives were the key reasons for participation. After receiving the diapers, some participants dropped immediately. Hence, we stopped providing diapers and de-emphasized incentive gifts [17].
2.4.6. Peer recruiter hiring and supervision challenge
Working with peer recruiters was a major challenge because we needed to supervise their activities from a long distance. Our recruiters worked at collaborative WIC offices, about 60–120 miles radius of Michigan State University. Recruiters were expected to work independently and communicate with their supervisor (Principal Investigator [PI], MC) and the study office over the phone. We posted recruiter position openings at our collaborative WIC offices and it usually took about 2–4 months to receive a few applications. The recruiter turnover rate was high. Once they were hired, some recruiters were unable to follow the recruitment protocol and had excessive tardiness and absences. Others had disruptive behaviors (e.g., arguing with WIC staff or interfering with staff activities). Some left for other employment. Hiring non-WIC mothers as recruiters did not solve these problems, so we put more effort into identifying and training WIC mothers as peer recruiters [17].
2.5. Recruitment facilitators
2.5.1. Weekly teleconferences
The PI had a weekly teleconference with the recruiters to identify recruitment challenges and brainstorm strategies to solve problems as they arose. The recruiters also shared tips with each other to improve recruitment strategies. Our recruiters enjoyed the opportunities to share and learn from each other and found the weekly teleconference to be helpful with recruitment. They felt empowered and being part of the team. We also learned that it was helpful to build recruiters' confidence by identifying and acknowledging their specific strengths and/or efforts with recruitment.
2.5.2. Acknowledging contributions
Despite the challenges outlined above, many of our peer recruiters who were reliable, followed the study protocol, and were personally committed to helping their peers were valuable to the project. We learned that acknowledging their contributions to the project was critical. For example, when our intervention participants returned to the collaborative WIC offices for the follow up data collection and shared with recruiters the helpfulness of the program, we reminded recruiters about their important contributions to the participants' quality of life. We found that some participants would respond to a call made or text message from the recruiters more readily than calls from the study office and they were more open in explaining reasons for missing a phone interview or not enrolling in the project when talking to their peer recruiters. Our peer recruiters had generally established good relationships with the participants and understood their life situations. Thus, we asked recruiters to document participants' reasons for not completing the baseline interview or not enrolling. Domestic disruptions (divorce or losing a boyfriend), personal tragedy such as a death in the family, or having to take care of an ill family member were typical reasons for failure to enroll after recruitment. These reasons have not been documented in prior studies of this kind.
2.5.3. WIC staff collaboration
Prior to recruitment, the PI met with WIC staff at each collaborating WIC agency during regular staff meeting to explain the study purpose and emphasize the fact that our recruitment would not interrupt their work flow or WIC staff activities. She also showed WIC staff the MIM introduction video lesson and shared successful stories from the intervention participants. After learning the program's strengths and previous successes with WIC clients, WIC staff members proved to be effective partners in facilitating the project's recruitment and enrollment activities.
2.6. Intervention
A detailed description of MIM intervention has been published [14]. Briefly, the study participants were randomly assigned to an intervention or comparison group (2:1 ratio). Both groups received usual WIC care. Intervention participants received a 16-week home-based intervention (weekly [weeks 1–4] or every other week [weeks 5–16] at home to minimize common barriers to participation, e.g., transportation and child care issues. They watched 10 designated video lessons via DVD according to a scheduled sequence. Each lesson was 20 min long and the topics were stress management (4), healthy eating (5) and physical activity (1). Participants also joined peer support group teleconferences by phone. There were 10 30-min teleconference sessions led by peer educators and WIC nutrition educators who were trained in motivational interviewing and group facilitation skills. The comparison participants read printed written educational materials with emphasis on stress management, healthy eating, and physical activity at home.
2.7. Measures
2.7.1. Demographic and screening surveys
Demographic and screening data were collected via pencil-and-paper surveys while women were waiting at the collaborative WIC offices for their appointments. Demographic measures included birthdays of each study participant and her youngest child (used to calculate postpartum status) along with race/ethnicity, breastfeeding, smoking, education, and employment status. We also asked if they had been diagnosed with an eating disorder, depression, or a psychiatric condition such as bipolar disorder.
2.8. Statistical analysis
After excluding data from non-eligible women and the 22 participants from the WIC agency that was discontinued during recruitment, our data analyses focused on non-pregnant women who had at least 1 biological child enrolled at WIC. We calculated participants' ages and postpartum status by using the participant's birthdate and their youngest child's birthdate minus the date of the participant filling the demographic survey. We defined enrollment as complete when women who consented to participate completed a baseline phone interview and returned to their WIC office to be randomized within 2 weeks of signing the consent form. We performed descriptive analysis (mean and percentage), T-test analysis for continuous variables and Chi-squared analysis for categorical variables. To examine the relationships among demographic characteristic and enrollment, we performed multiple logistic regression analysis with k independent variables to identify a subset of demographic variables that may adequately explain our data. While many criteria have been suggested for identifying the “best” subset, we used a hierarchical forward search approach [18] to locate the “best subset” of predictors. With this algorithm, the term with the largest log likelihood was entered into the model. Next, we added the term that increased the log likelihood the most. This selection was continued until all the terms had been entered or until the maximum predefined subset size had been reached.
3. Results
3.1. Demographic characteristics
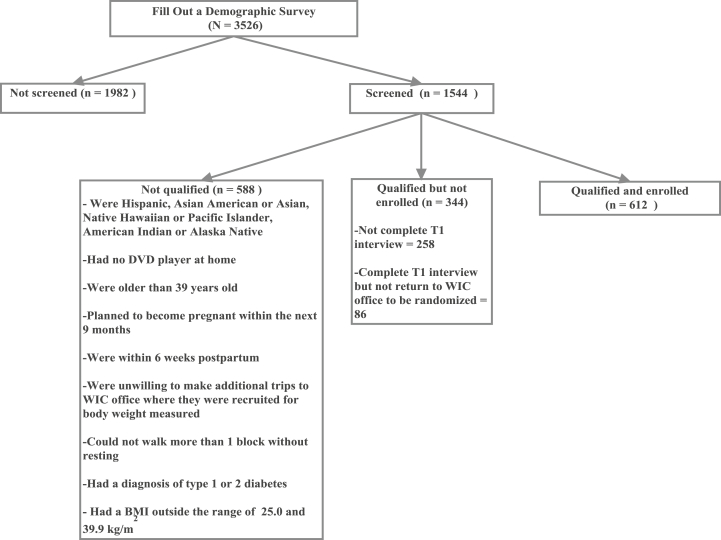
A total of 3526 WIC women filled out demographic surveys. Fig. 1 presents a CONSORT chart of the study participants. The key reasons for disqualification was having a BMI outside the range of 25.0 and 39.9 kg/m2. Table 1 shows demographics of participants who were screened versus those who were initially recruited but not screened. The key reasons for not screening were no time (need to leave WIC office immediately) or lack of interest in participation. There were significant differences between women being screened and not being screened: age of the study participants, race, breastfeeding, and smoking status. Table 2 shows demographic of women being screened: 1) screen but not qualified; 2) screen, qualified, but not enrolled; and 3) screened, qualified, and enrolled. Our enrollment rate was 64.0% (612 qualified and enrolled divided by 956 qualified). There were significant differences among these 3 groups: age of the study participants, race, breastfeeding, smoking, and education.
Fig. 1.
CONSORT Chart.
Table 1.
| Demographics characteristics | Not screened (n = 1982) |
Screened (n = 1544) |
P value | ||
|---|---|---|---|---|---|
| Mean | SD | Mean | SD | ||
| Age (years)c | 29.54 | 11.63 | 27.76 | 5.08 | <0.001 |
|
Postpartum (years)c |
1.65 |
1.25 |
1.61 |
1.24 |
0.32 |
|
n |
% |
n |
% |
||
| Raced | <0.001 | ||||
| African American | 294 | 15.09% | 388 | 25.21% | |
| White (non Hispanic) | 1531 | 78.59% | 1142 | 74.20% | |
| Asian American or Asian | 17 | 0.87% | 0 | 0% | |
| Native Hawaiian or Pacific Islander | 3 | 0.15% | 0 | 0% | |
| American Indian or Alaska Native | 13 | 0.67% | 2 | 0.13% | |
| Other | 90 | 4.62% | 7 | 0.45% | |
| Breastfeedingd(Yes) | 204 | 10.30% | 206 | 13.34% | 0.005 |
| Smoking statusd | 0.004 | ||||
| Never smoked | 855 | 43.45% | 607 | 39.31% | |
| Smoked, but quit | 549 | 27.90% | 418 | 27.07% | |
| Smoker | 564 | 28.66% | 519 | 33.61% | |
| Educationd | 0.41 | ||||
| 8th grade or less | 16 | 0.81% | 9 | 0.58% | |
| Some high School | 242 | 12.30% | 209 | 13.54% | |
| High school graduate | 609 | 30.96% | 407 | 26.36% | |
| Some college or technical school | 799 | 40.62% | 676 | 43.78% | |
| College graduate or higher | 301 | 15.30% | 243 | 15.44% | |
| Employment statusd | 0.394 | ||||
| Full time | 463 | 23.56% | 337 | 21.85% | |
| Part time | 440 | 22.39% | 356 | 23.09% | |
| Unemployed | 435 | 22.14% | 358 | 23.22% | |
| Homemaker | 423 | 21.53% | 347 | 22.50% | |
| Self-employed | 41 | 2.09% | 35 | 2.27% | |
| Student | 108 | 5.50% | 81 | 5.25% | |
| Other | 55 | 2.80% | 28 | 1.82% | |
There were 0.06% missing data except race (1.7% for not screened).
P value < 0.05 shown on this Table may be due to the large sample sizes between screened and not screened groups.
T-test analysis.
Chi-squared analysis.
Table 2.
Participant characteristics (N = 1544).
| Characteristics |
Screen but not qualified (n = 588) |
Screened, qualified, but not enrolled (n = 344) |
Screened, qualified, and enrolled (n = 612) |
P value | |||
|---|---|---|---|---|---|---|---|
| Demographics | Mean | SD | Mean | SD | Mean | SD | |
| Age (years)a | 27.38 | 5.00 | 27.42 | 5.26 | 28.32 | 5.02 | 0.002 |
|
Postpartum (years)a |
1.57 |
1.23 |
1.51 |
1.18 |
1.70 |
1.27 |
0.053 |
|
n |
% |
n |
% |
n |
% |
||
| Raceb | <0.001 | ||||||
| African American | 149 | 25.47% | 109 | 31.69% | 130 | 21.24% | |
| White (non Hispanic) | 428 | 73.16% | 234 | 68.02% | 482 | 78.76% | |
| Asian American or Asian | 0 | 0% | 0 | 0% | 0 | 0% | |
| Native Hawaiian or Pacific Islander | 0 | 0% | 0 | 0% | 0 | 0% | |
| American Indian or Alaska Native | 1 | 0.17% | 1 | 0.29% | 0 | 0% | |
| Other | 7 | 1.20% | 0 | 0% | 0 | 0% | |
| Breastfeedingb(Yes) | 82 | 13.95% | 24 | 6.98% | 100 | 16.34% | <0.001 |
| Smoking statusb | <0.001 | ||||||
| Never smoked | 212 | 36.05% | 115 | 33.43% | 280 | 45.75% | |
| Smoked, but quit | 172 | 29.25% | 77 | 22.38% | 169 | 27.61% | |
| Smoker | 204 | 34.69% | 152 | 44.19% | 163 | 26.63% | |
| Educationb | <0.001 | ||||||
| 8th grade or less | 5 | 0.85% | 2 | 0.58% | 2 | 0.33% | |
| Some high School | 80 | 13.61% | 61 | 17.73% | 68 | 11.11% | |
| High school graduate | 177 | 30.10% | 98 | 28.49% | 132 | 21.57% | |
| Some college or technical school | 242 | 41.16% | 144 | 41.86% | 290 | 47.39% | |
| College graduate or higher |
84 |
14.29% |
39 |
11.34% |
120 |
19.61% |
|
|
n |
% |
n |
% |
n |
% |
||
| Employment statusb | 0.109 | ||||||
| Full time | 122 | 20.82% | 81 | 23.55% | 134 | 21.90% | |
| Part time | 146 | 24.91% | 83 | 24.13% | 127 | 20.75% | |
| Unemployed | 141 | 24.06% | 92 | 26.74% | 125 | 20.42% | |
| Homemaker | 126 | 21.50% | 59 | 17.15% | 162 | 26.47% | |
| Self-employed | 13 | 2.22% | 6 | 1.74% | 16 | 2.61% | |
| Student | 27 | 4.61% | 18 | 5.23% | 36 | 5.88% | |
| Other | 11 | 1.88% | 5 | 1.45% | 12 | 1.96% | |
| Diagnosed with type 1 or 2 diabetesb | 42 | 7.22% | 0 | 0% | 0 | 0% | NA |
| Diagnosed with eating disorderb | 21 | 3.61% | 9 | 2.62% | 13 | 2.13% | 0.292 |
| Diagnosed with depressionb | 244 | 42.07% | 124 | 36.05 | 253 | 41.34% | 0.165 |
| Diagnosed with psychiatricbcondition | 86 | 14.83% | 49 | 14.24% | 64 | 10.46% | 0.057 |
T-test analysis.
Chi-squared analysis.
3.2. Relationship between demographic characteristics and enrollment
Table 3 presents results of multiple logistic regression analysis to examine demographic characteristics that may have influenced enrollment. Women with a higher BMI were more likely to enroll than women with a lower BMI (OR 1.06, 95% CI 1.02–1.10). Late postpartum women were more likely to enroll than early postpartum women (OR 1.24, 95% CI 1.10–1.40). Breastfeeding women were more likely to enroll than non-breastfeeding women (OR 5.0, 95% CI 2.34–10.65). Breastfeeding women who were at their early postpartum (interaction between postpartum and breastfeeding) were more likely to enroll than breastfeeding women who were late postpartum (OR 0.42, 95% CI 0.22–0.81). Compared to African American women, Non-Hispanic White women were more likely to enroll (OR 1.77, 95% CI 1.29–2.42). Non-smokers were more likely to enroll than smokers (OR 0.54, 95% CI 0.40–0.73). Women with a higher education were more likely to enroll than women with a lower education (OR 1.21, 95% CI 1.04–1.42).
Table 3.
Multiple logistic regression for enrolling to the study.
| Variables | Regression coefficient | Standard error | P value | Odds ratio | 95% Confidence interval |
|---|---|---|---|---|---|
| Intercept | −3.17 | 0.64 | <0.01 | 0.04 | 0.01–0.15 |
| BMI (kg/m2) | 0.06 | 0.02 | <0.01 | 1.06 | 1.02–1.10 |
| Postpartum (years) | 0.22 | 0.06 | <0.01 | 1.24 | 1.10–1.40 |
| Breastfeeding | 1.61 | 0.39 | <0.01 | 5.0 | 2.34–10.65 |
| Postpartum status*breastfeeding | −0.86 | 0.33 | <0.01 | 0.42 | 0.22–0.81 |
| Race | 0.57 | 0.16 | <0.01 | 1.77 | 1.29–2.42 |
| Smoking status | −0.62 | 0.15 | <0.01 | 0.54 | 0.40–0.73 |
| Education | 0.19 | 0.08 | 0.02 | 1.21 | 1.04–1.42 |
*Interaction. Breastfeeding: 0 = No, 1 = Yes. Race: 1 = African American, 2 = White. Smoking: 0 = No, 1 = Yes. Education: 1 = 8th. grade or less, 2 = some high school, 3 = high school graduate, 4 = some college or technical school, and 5 = college graduate or higher.
4. Discussion
We have implemented numerous innovative strategies that were not documented in the literature to reach a 64.0% enrollment rate. Our enrollment rate is similar to a study of pregnancy weight gain intervention study with 69% enrollment rate [8]. While the previous study recruited low-income overweight and obese pregnant women (defined as income at or below 500% of the federal poverty line) [8], we recruited non pregnant low-income overweight and obese women (6 weeks–5 years postpartum) with incomes at or below 185% of the federal poverty line. This is the first weight management intervention study examining the demographic characteristics associated with enrollment rate. Thus, further comparison of our study findings to findings of previous studies is limited. Accordingly, our discussion section will focus on potential strategies that may enhance recruitment efforts for programs with similar target audiences and objectives.
We found that heavier women were about 100% more likely to enroll than women who weighed less. Stress is associated with obesity [19], [20] and our recruitment message emphasized stress management and a happier and healthier family. Therefore, it is possible that heavier women were more interested in enrolling because of their heightened interest in stress management.
Our results revealed that late postpartum women were more likely to enroll than early postpartum women. This is a great concern because nearly 65–86% of women who were overweight or obese prior to becoming pregnant gained more weight during pregnancy than that recommended by the 2009 Institute of Medicine pregnancy weight gain guidelines [21], [22], [23], [24]. Excessive gestational weight gain increases risk of adverse maternal (e.g., gestational diabetes) [25], [26], [27], [28] and birth outcomes (e.g., having a large baby) [29], [30], [31]. It also predicts postpartum weight retention [32], [33], [34], [35], [36], leading to long-term obesity [37] associated with numerous chronic conditions (e.g., type 2 diabetes) contributing to $200 billion of annual direct health care costs in the US [1], [2]. At 1 year postpartum, 32% of higher-income but 68% of low-income women experience significant postpartum weight retention (≥10 lbs) [24]. It is possible that some early postpartum women were less inclined to follow through with our intervention because they had not yet failed to lose much of the weight they had gained during pregnancy. Unfortunately, we did not emphasize weight loss during recruitment for 2 reasons. First, young low-income overweight and obese mothers with young children who had participated in our pilot MIM [16] and attended focus group discussions to evaluate the recruitment strategies suggested de-emphasizing weight management, suggesting a more motivating focus on having a healthier and happier family. Second, most of our recruiters were obese WIC mothers and they did not feel comfortable talking about weight loss through healthy eating and physical activity during recruitment when they already struggled with their own weight management issues. An alternative method for future studies may consider having potential participants watch a short recruitment video that features the target audience with a similar body size providing testimonies about benefits of weight loss.
We found women who breastfed their babies were about 5 times more likely to enroll than women who were not breastfeeding. It is more likely that breastfeeding women were more motivated to eat healthier for the good health of their babies than non-breastfeeding women. We also found that women who breastfed their babies during their early postpartum period were more likely to enroll than breastfeeding women at late postpartum. It is very likely that late postpartum women who still breastfed might think they already knew how to eat healthier and their babies are already eating supplemental foods.
We found that Africa American women were less likely than Non-Hispanic White women to enroll in the study. This may be partially due to the fact that most of our African American women who were recruited lived in the areas with severe economic disadvantage and a high crime rate that made it difficult to follow through with study requirements. This could represent an important public health concern because many of these high-need mothers are in survival mode, with inadequate problem solving skills and minimal access to needed resources. Future studies may consider partnering with local community agencies that provide resources dealing with crisis when recruiting participants from very poor neighborhoods with high crime. We found that non-smokers were more about 0.5 times likely to enroll than smokers. Also, educated women were 1.2 times more likely to enroll than less educated women. Similar to women living in high poverty/crime situations, women with less education and women who have not been able to quit smoking may be interested in this type of study but less able to commit to a study requiring them to follow a calendar of mandatory activities.
In addition to identifying demographic characters associated with enrollment, we also identified potential reasons for not enrolling to the study based on our recruiters' logs. Reasons such as divorce and serious family illness caused serious disruptions in the potential participants' ability to continue with the study. Some of our participants requested a suspension so they could re-enroll at a later time when their personal crisis had abated. Researchers may be able to enhance retention by telling potential participants who are dealing with a sudden life crisis to seek help and come back to be screened at a later time. To help women deal with crisis, researchers may consider providing a list of useful community resources or making a referral to the collaborating community programs.
Personal and family values motivate and guide behavioral change [38]. At the conclusion of Mothers In Motion, we identified personal and family values that were common among young low-income overweight and obese mothers through our peer support group teleconferences. A detailed description of the peer support group teleconference has been published [14]. The common personal and family values that we identified were being happy, being healthy, having more energy to play with one's children, being a good role model for one's children, not feeling overwhelming by stress, and losing weight. Emphasizing family and personal values proved to be very important in our study, since we experienced only about 40% enrollment rate at the start of recruitment when we placed more emphasis on healthy eating and physical activity. When we started to emphasize personal and family values such as having a happier and healthier family and reducing stress and feeling happier, our recruitment efforts were much more successful. Future studies may consider identifying family and personal values of the target audience prior to or at the early stage of recruitment, then connect the target audience personal and family values to the objectives and goals of the planned program. Also, researchers may consider tailoring their program to the personal and family values of specific subgroups of their target audience to enhance recruitment efforts.
Lastly, researchers may consider the benefits and drawbacks of using recruiters who are personally familiar with the program and its benefits. At the beginning of recruitment, we did not allow peer recruiters to watch our intervention videos because we were concerned that they would want to share the contents with others during recruitment, thus introducing a systematic bias. Recruiters were frequently asked by the potential participants if they had watched the videos and whether they found them to be beneficial. Many potential participants expressed skepticism, commenting that recruiters could not know the program's true benefits. Thus, we allowed peer recruiters to watch the MIM videos and read printed materials but at the same time we asked them not to share the program's content with others while the study was underway.
5. Conclusion
Recruiting young low-income overweight and obese mothers with young children to a weight management intervention presents many challenges. We have identified several approaches to address common barriers and facilitate recruitment.
Acknowledgements
The project was supported by NIH-NIDDK Grant Number R18-DK-083934-01. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Diabetes and Digestive and Kidney Disease or the National Institutes of Health. The authors would like to thank WIC administrators (Dr. Velonda Thompson, Ms. Nina Nikitenko, Ms. Jennifer Barr, Ms. Stefani Horning and Monica Smith) and staff at City of Detroit, County Health Department of Berrien, Calhoun, Jackson, and Kent and study participants.
Contributor Information
Mei-Wei Chang, Email: chang.1572@osu.edu.
Susan Nitzke, Email: nitzke@nutrisci.wisc.edu.
Roger Brown, Email: rlbrown3@wisc.edu.
M. Jean Brancheau Egan, Email: EganJ@michigan.gov.
Christopher M. Bendekgey, Email: christopher.bendekgey@kentcountymi.gov.
Diana Buist, Email: dbuist@calhouncountymi.gov.
List of abbreviation
- BMI
Body Mass Index
- MIM
Mothers In Motion
- WIC
The Special Supplemental Nutrition Program for Women, Infants, and Children
Competing interest
The authors declare that they have no competing interests.
Authors' contributions
MC, SN, JE, CB, and DB participated in the design of recruitment and RB conducted data analysis and data interpretation. MC drafted and revised the manuscript and SN and RB involved in revision. JE, CB, and DB provided feedback for revision. All the authors have read and approved the final manuscript.
References
- 1.Cawley J., Meyerhoefer C. The medical care costs of obesity: an instrumental variables approach. J. Health Econ. 2012;31(1):219–230. doi: 10.1016/j.jhealeco.2011.10.003. [DOI] [PubMed] [Google Scholar]
- 2.Finkelstein E.A., Trogdon J.G., Cohen J.W., Dietz W. Annual medical spending attributable to obesity: payer-and service-specific estimates. Health Aff. 2009;28(5):w822–831. doi: 10.1377/hlthaff.28.5.w822. [DOI] [PubMed] [Google Scholar]
- 3.McDonald A.M., Knight R.C., Campbell M.K., Entwistle V.A., Grant A.M., Cook J.A., Elbourne D.R., Francis D., Garcia J., Roberts I. What influences recruitment to randomised controlled trials? A review of trials funded by two UK funding agencies. Trials. 2006;7:9. doi: 10.1186/1745-6215-7-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Foy R., Parry J., Duggan A., Delaney B., Wilson S., Lewin-Van Den Broek N.T., Lassen A., Vickers L., Myres P. How evidence based are recruitment strategies to randomized controlled trials in primary care? Experience from seven studies. Fam. Pract. 2003;20(1):83–92. doi: 10.1093/fampra/20.1.83. [DOI] [PubMed] [Google Scholar]
- 5.Brannon E.E., Kuhl E.S., Boles R.E., Aylward B.S., Ratcliff M.B., Valenzuela J.M., Johnson S.L., Powers S.W. Strategies for recruitment and retention of families from low-income, ethnic minority backgrounds in a longitudinal study of caregiver feeding and child weight. Child. Health Care J. Assoc. Care Child. Health. 2013;42(3):198–213. doi: 10.1080/02739615.2013.816590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rdesinski R.E., Melnick A.L., Creach E.D., Cozzens J., Carney P.A. The costs of recruitment and retention of women from community-based programs into a randomized controlled contraceptive study. J. Health Care Poor Underserved. 2008;19(2):639–651. doi: 10.1353/hpu.0.0016. [DOI] [PubMed] [Google Scholar]
- 7.French G.M., Groner J.A., Wewers M.E., Ahijevych K. Staying smoke free: an intervention to prevent postpartum relapse. Nicot. Tob. Res. Off. J. Soc. Res. Nicot. Tob. 2007;9(6):663–670. doi: 10.1080/14622200701365277. [DOI] [PubMed] [Google Scholar]
- 8.Coleman-Phox K., Laraia B.A., Adler N., Vieten C., Thomas M., Epel E. Recruitment and retention of pregnant women for a behavioral intervention: lessons from the maternal adiposity, metabolism, and stress (MAMAS) study. Prev. Chronic Dis. 2013:10. doi: 10.5888/pcd10.120096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.El-Khorazaty M.N., Johnson A.A., Kiely M., El-Mohandes A.A., Subramanian S., Laryea H.A., Murray K.B., Thornberry J.S., Joseph J.G. Recruitment and retention of low-income minority women in a behavioral intervention to reduce smoking, depression, and intimate partner violence during pregnancy. BMC Public Health. 2007;7:233. doi: 10.1186/1471-2458-7-233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wisdom K., Neighbors K., Williams V.H., Havstad S.L., Tilley B.C. Recruitment of African Americans with type 2 diabetes to a randomized controlled trial using three sources. Ethn. Health. 2002;7(4):267–278. doi: 10.1080/1355785022000060727. [DOI] [PubMed] [Google Scholar]
- 11.Horowitz C.R., Brenner B.L., Lachapelle S., Amara D.A., Arniella G. Effective recruitment of minority populations through community-led strategies. Am. J. Prev. Med. 2009;37(6 Suppl 1):S195–S200. doi: 10.1016/j.amepre.2009.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Parra-Medina D., D'Antonio A., Smith S.M., Levin S., Kirkner G., Mayer-Davis E. Study P: successful recruitment and retention strategies for a randomized weight management trial for people with diabetes living in rural, medically underserved counties of South Carolina: the POWER study. J. Am. Dietetic Assoc. 2004;104(1):70–75. doi: 10.1016/j.jada.2003.10.014. [DOI] [PubMed] [Google Scholar]
- 13.Warner E.T., Glasgow R.E., Emmons K.M., Bennett G.G., Askew S., Rosner B., Colditz G.A. Recruitment and retention of participants in a pragmatic randomized intervention trial at three community health clinics: results and lessons learned. BMC Public Health. 2013;13:192. doi: 10.1186/1471-2458-13-192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chang M.W., Nitzke S., Brown R., Resnicow K. A community based prevention of weight gain intervention (Mothers in Motion) among young low-income overweight and obese mothers: design and rationale. BMC Public Health. 2014;14:280. doi: 10.1186/1471-2458-14-280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chang M., Brown R., Nitzke S. Participant recruitment and retention in a pilot program to prevent weight gain in low-income overweight and obese mothers. BMC Public Health. 2009;9:424. doi: 10.1186/1471-2458-9-424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chang M., Nitzke S., Brown R. Design and outcomes of a mothers in motion behavioral intervention pilot study. J. Nutr. Educ. Behav. 2010;42(3 Suppl.):S11–S21. doi: 10.1016/j.jneb.2010.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chang M., Nitzke S., Resnicow K., Brown R., Egan J., Eghtedary K., Rosenfeld C. Reversing harmful DOHaD effects. In: Missouri Rosenfeld C., editor. The Epigenome and Developmental Origins of Health and Disease Edn. Elsvier; 2015. pp. 486–505. [Google Scholar]
- 18.Menard S. Sage; Thousand Oaks, CA: 1995. Applied Logistic Regression Analysis. [Google Scholar]
- 19.Brantley P.J., Stewart D.W., Myers V.H., Matthews-Ewald M.R., Ard J.D., Coughlin J.W., Jerome G.J., Samuel-Hodge C., Lien L.F., Gullion C.M. Psychosocial predictors of weight regain in the weight loss maintenance trial. J. Behav. Med. 2014;37(6):1155–1168. doi: 10.1007/s10865-014-9565-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Barrington W.E., Ceballos R.M., Bishop S.K., McGregor B.A., Beresford S.A. Perceived stress, behavior, and body mass index among adults participating in a worksite obesity prevention program, Seattle, 2005-2007. Prev. Chronic Dis. 2012;9:E152. doi: 10.5888/pcd9.120001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kraschnewski J.L., Chuang C.H., Downs D.S., Weisman C.S., McCamant E.L., Baptiste-Roberts K., Zhu J., Kjerulff K.H. Association of prenatal physical activity and gestational weight gain: results from the first baby study. Womens Health Issues. 2013;23(4):e233–238. doi: 10.1016/j.whi.2013.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ferrari R.M., Siega-Riz A.M. Provider advice about pregnancy weight gain and adequacy of weight gain. Matern. Child Health J. 2013;17(2):256–264. doi: 10.1007/s10995-012-0969-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gould Rothberg B.E., Magriples U., Kershaw T.S., Rising S.S., Ickovics J.R. Gestational weight gain and subsequent postpartum weight loss among young, low-income, ethnic minority women. Am. J. Obstet. Gynecol. 2011;204(1) doi: 10.1016/j.ajog.2010.08.028. 52 e51–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Endres L.K., Straub H., McKinney C., Plunkett B., Minkovitz C.S., Schetter C.D., Ramey S., Wang C., Hobel C., Raju T. Postpartum weight retention risk factors and relationship to obesity at 1 year. Obstet. Gynecol. 2015;125(1):144–152. doi: 10.1097/AOG.0000000000000565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Doherty D.A., Magann E.F., Francis J., Morrison J.C., Newnham J.P. Pre-pregnancy body mass index and pregnancy outcomes. Int. J. Gynaecol. Obstet. 2006;95(3):242–247. doi: 10.1016/j.ijgo.2006.06.021. [DOI] [PubMed] [Google Scholar]
- 26.Villamor E., Cnattingius S. Interpregnancy weight change and risk of adverse pregnancy outcomes: a population-based study. Lancet. 2006;368(9542):1164–1170. doi: 10.1016/S0140-6736(06)69473-7. [DOI] [PubMed] [Google Scholar]
- 27.Heslehurst N., Simpson H., Ells L.J., Rankin J., Wilkinson J., Lang R., Brown T.J., Summerbell C.D. The impact of maternal BMI status on pregnancy outcomes with immediate short-term obstetric resource implications: a meta-analysis. Obes. Rev. 2008;9(6):635–683. doi: 10.1111/j.1467-789X.2008.00511.x. [DOI] [PubMed] [Google Scholar]
- 28.Koebnick C., Smith N., Huang K., Martinez M.P., Clancy H.A., Kushi L.H. The prevalence of obesity and obesity-related health conditions in a large, multiethnic cohort of young adults in California. Ann. Epidemiol. 2012;22(9):609–616. doi: 10.1016/j.annepidem.2012.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Baeten J.M., Bukusi E.A., Lambe M. Pregnancy complications and outcomes among overweight and obese nulliparous women. Am. J. Public Health. 2001;91(3):436–440. doi: 10.2105/ajph.91.3.436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kabali C., Werler M.M. Pre-pregnant body mass index, weight gain and the risk of delivering large babies among non-diabetic mothers. Int. J. Gynaecol. Obstet. 2007;97(2):100–104. doi: 10.1016/j.ijgo.2007.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Johansson S., Villamor E., Altman M., Bonamy A.K., Granath F., Cnattingius S. Maternal overweight and obesity in early pregnancy and risk of infant mortality: a population based cohort study in Sweden. BMJ. 2014;349:g6572. doi: 10.1136/bmj.g6572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Siega-Riz A.M., Herring A.H., Carrier K., Evenson K.R., Dole N., Deierlein A. Sociodemographic,perinatal, behavioral, and psychosocial predictors of weight retention at 3 and 12 months postpartum. Obesity. 2010;18(10):1996–2003. doi: 10.1038/oby.2009.458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Olson C.M., Strawderman M.S., Hinton P.S., Pearson T.A. Gestational weight gain and postpartum behaviors associated with weight change from early pregnancy to 1 y postpartum. Int. J. Obes. Relat. Metab. Disord. J. Int. Assoc. Study Obes. 2003;27(1):117–127. doi: 10.1038/sj.ijo.0802156. [DOI] [PubMed] [Google Scholar]
- 34.Ostbye T., Krause K.M., Lovelady C.A., Morey M.C., Bastian L.A., Peterson B.L., Swamy G.K., Brouwer R.J., McBride C.M. Active Mothers Postpartum: a randomized controlled weight-loss intervention trial. Am. J. Prev. Med. 2009;37(3):173–180. doi: 10.1016/j.amepre.2009.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ostbye T., Peterson B.L., Krause K.M., Swamy G.K., Lovelady C.A. Predictors of postpartum weight change among overweight and obese women: results from the Active Mothers Postpartum study. J. Women's Health. 2012;21(2):215–222. doi: 10.1089/jwh.2011.2947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Phelan S., Phipps M.G., Abrams B., Darroch F., Grantham K., Schaffner A., Wing R.R. Does behavioral intervention in pregnancy reduce postpartum weight retention? Twelve-month outcomes of the Fit for Delivery randomized trial. Am. J. Clin. Nutr. 2014;99(2):302–311. doi: 10.3945/ajcn.113.070151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Amorim A.R., Rossner S., Neovius M., Lourenco P.M., Linne Y. Does excess pregnancy weight gain constitute a major risk for increasing long-term BMI? Obesity. 2007;15(5):1278–1286. doi: 10.1038/oby.2007.149. [DOI] [PubMed] [Google Scholar]
- 38.Markland D., Ryan R.M., Tobin V.J., Rollnick S. Motivational interviewing and self-determination theory. J. Soc. Clin. Psychol. 2005;24(6):811–831. [Google Scholar]