Abstract
Hip arthroscopy is increasing in popularity for the diagnosis and management of hip preservation. The basics of hip arthroscopy positioning, fluoroscopic assessment, and portal establishment are reviewed in the first 2 parts of this series. This article is the third installment in which we describe a systematic approach to performing a diagnostic hip arthroscopy. A mastery of diagnostic arthroscopy is necessary for surgeons treating hip disorders.
Arthroscopic evaluation of the hip is a valuable tool for identifying and treating intra- and extra-articular pathology.1, 2 Although the surgeon develops a plan prior to arthroscopy, a well-executed diagnostic hip arthroscopy can identify pathology and provide intraoperative information that is not readily apparent with current imaging techniques. A systematic approach to diagnostic hip arthroscopy can identify all intra-articular pathology and enable the surgeon to effectively treat the patient. A consistent approach to the diagnostic arthroscopy may also maximize the efficiency of operative time to best address the identified pathology. In this series of articles, we previously described the positioning for hip arthroscopy3 and establishment of arthroscopic portals.4 The current article and accompanying video is the third in the series in which we outline the steps necessary to perform a diagnostic hip arthroscopy.
Surgical Technique
Patient Positioning and Portal Establishment
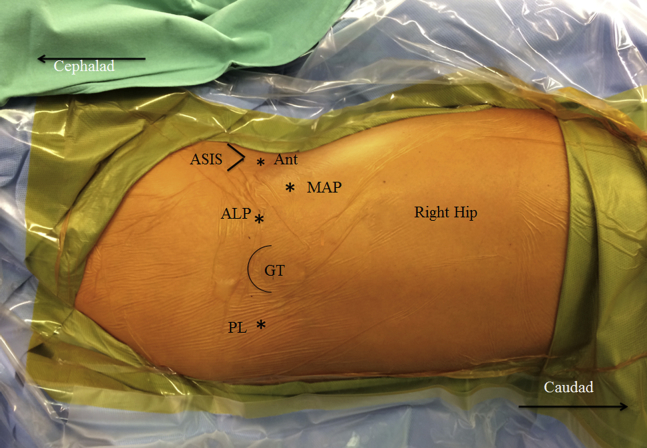
The patient is positioned in the supine position, and portal placement and entry to the hip joint are performed as described in part I and II of this series. In summary, the patient is placed supine on a fracture table with a lateralized perineal post under general anesthesia. The patient is secured on a well-padded table and the arm ipsilateral to the operative extremity is padded and folded over the patient's chest. The perineal post must be well padded to minimize the risk of pudendal nerve compression. At our institution, we use the padded post from K.A.F. positioning kit (Bledsoe Philippon K.A.F. Positioning Kit with perineal post pad; Bledsoe, Grand Prairie, TX). The feet are secured using well-padded boots. The use of traction in hip arthroscopy is not without potential complications and we have recommended the following tips to minimize traction-related complications in Table 1. After sterile preparation and draping, we mark and establish our portals. We use 2 portals for the diagnostic hip arthroscopy: the modified anterior portal and the anterolateral portal (Fig 1). Atraumatic entry may be facilitated by fluoroscopic or ultrasound guidance. We previously described our preferred method of establishment of arthroscopic hip arthroscopy portals with limited use of fluoroscopy.4 A 70° 4-mm arthroscope is used for the duration of the procedure. Intra-articular visualization is optimized with appropriate fluid flow (a medium flow rate of approximately 0.7 L/min), fluid pressure balanced with mean arterial pressure (fluid with pump-assisted flow at 40 mmHg), and dilute epinephrine (1:100,000) in the arthroscopic fluid.
Table 1.
Traction Complications: Pearls and Pitfalls for Hip Arthroscopy in the Supine Position
| Traction and Positioning Pitfalls | Strategy to Avoid Pitfalls |
|---|---|
| Skin injury | Use a well-padded traction boot |
| Properly secure the foot | |
| Limit traction time to <2 hours | |
| Pudendal nerve and genital injury | Locate the perineal post eccentrically |
| Use a >9-cm post pad | |
| Assess prior to, during, and after traction application | |
| Limit traction time to <2 hours | |
| Sciatic nerve injury | Avoid flexing the hip >20° while in traction |
| Limit traction time to <2 hours |
Fig 1.
External view depicting anatomic location of bony prominences and arthroscopic portals of a right hip in supine position. The 2 portals used in this surgical technique are the anterolateral portal (AL) and the modified anterior portal (MAP). In 3-portal techniques, the anterior portal (Ant) and/or the posterolateral portal (PL) have traditionally been used. Also depicted here are the bony landmarks used to identify portal location: the anterior superior iliac spine (ASIS) and the greater trochanter (GT).
© 2017 Allston J. Stubbs, M.D. All rights reserved.
Diagnostic Arthroscopy of the Central Compartment of the Hip
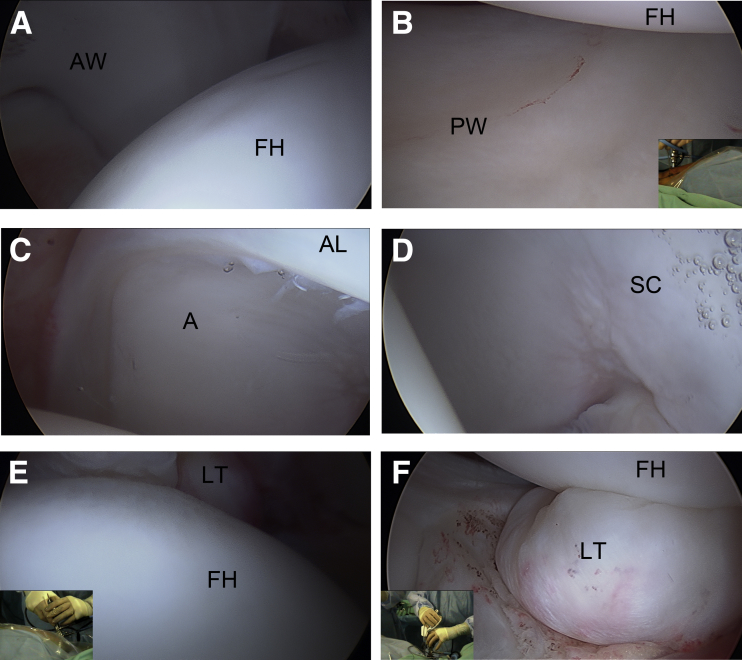
The arthroscope is initially placed in the modified anterior portal with instrumentation in the anterolateral portal. The central compartment is entered first (Table 2). A 5- to 6-mm capsulotomy is performed to facilitate instrument mobility. This step is performed using an arthroscopic Beaver blade (Becton-Dickenson, Franklin Lakes, NJ) under direct visualization. A capsulotomy may also improve the accessibility of an anterolateral portal placed too anterior or posterior. A temperature-controlled flexible radiofrequency ablation probe (E-flex RF Wand; Smith & Nephew, Andover, MA) is used to achieve hemostasis, perform a synovectomy to improve visualization, and as a flexible probe. The arthroscope is placed in the anterolateral portal to visualize the anterior acetabular wall (Fig 2A). Next, the camera is directed to the posterior acetabular wall with the corresponding physeal scar (Fig 2B). The physeal scar is the remnant of the triradiate cartilage and should not be interpreted as a fracture line. After inspecting the posterior acetabular wall, the acetabular stellate crease is identified. The acetabular stellate crease corresponds to the 12-o'clock acetabular position (Fig 2 C and D). Maneuvering in the hip joint requires changing the direction of the light source, camera horizon, and limited physical movement of the arthroscope in the confined femoroacetabular central compartment of the hip joint.
Table 2.
Systematic Approach to Diagnostic Hip Arthroscopy
| Step | Portal | Compartment | Visualized Structure | Potential Pathology |
|---|---|---|---|---|
| 1 | ALP | Central | Anterior acetabular wall | Chondral defects or delamination |
| Chondrolabral tears | ||||
| 2 | ALP | Central | Posterior acetabular wall | Chondral defects or delamination |
| Chondrolabral tears | ||||
| 3 | ALP | Central | Cotyloid space (fat pad and the ligamentum teres) | Ligamentum teres tears with possible tears |
| Incarcerated loose bodies | ||||
| Ligamentum teres impingement within or against acetabular fossa | ||||
| 4 | ALP | Central | Anterior-superior chondrolabral junction | Labral tears or fibrillations |
| Labral instability | ||||
| Chondral defects or delamination | ||||
| 5 | MAP | Peripheral | Medial femoral circumflex artery and retinacular vessels along posterior-superior femoral head-neck junction | |
| 6 | MAP | Peripheral | Anterior femoral head-neck junction | Cam impingement signs (convexity, fibrillation, discoloration) |
| 7 | MAP | Peripheral | Inferior head-neck junction with posterior-inferior capsular recess and zona orbicularis | Loose bodies |
ALP, anterolateral portal; MAP, modified anterior portal.
Fig 2.
Central compartment viewed from the anterolateral portal of the right hip in the supine position. (A) Visualization of the anterior acetabular wall (AW) with the anterior superior femoral head (FH). (B) Posterior acetabular wall (PW) with the femoral head (FH). (C) 12-o'clock position revealed the acetabulum (A) and anterior labrum (AL). (D) Acetabular stellate crease (SC). (E) View of the fovea, which may identify tears of the ligamentum teres (LT) or incarcerated loose bodies. (F) Ligamentum teres (LT) and the femoral head (FH).
© 2017 Allston J. Stubbs, M.D. All rights reserved.
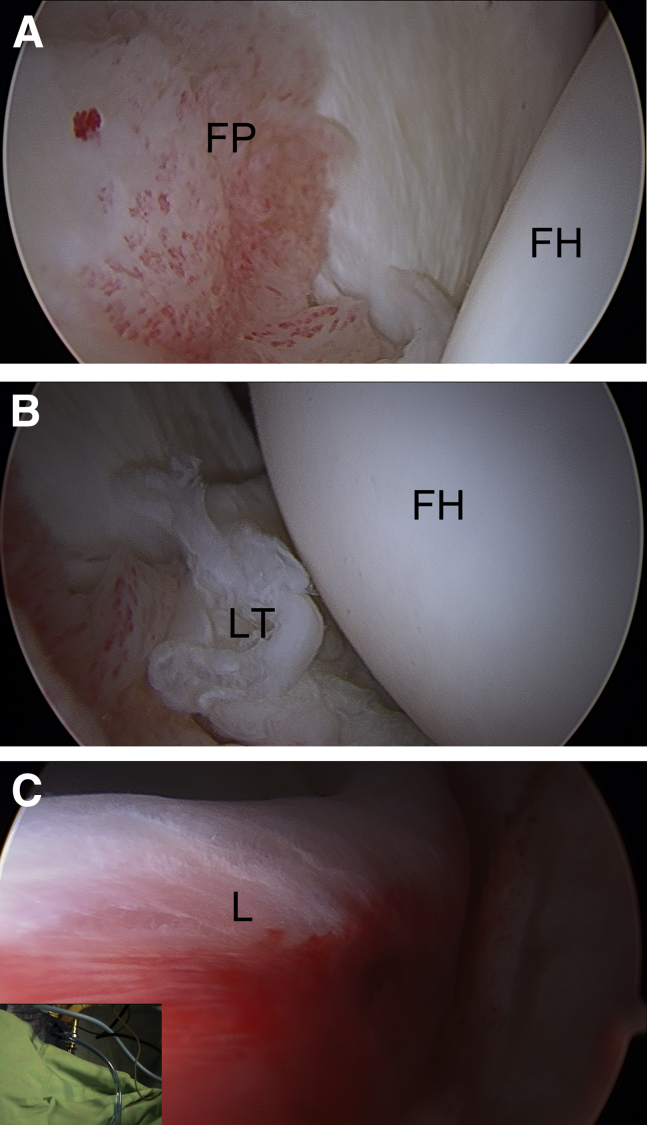
The next view shows the cotyloid space, which is composed of the fat pad and ligamentum teres (Fig 2 E and F). The ligamentum teres is dynamically assessed by internal and external rotation of the foot under mild traction. Dynamic assessment of the ligamentum teres may better identify tears, incarcerated loose bodies, and impingement of the ligamentum teres within or against the acetabular fossa (Fig 3 A and B). A technical pearl for assessment of the ligamentum teres is best performed by movement of the operative extremity by the circulating nurse to place the structure on tension for optimal visualization. Traction is then released. After evaluation of the ligamentum teres, the anterior-superior acetabular chondrolabral junction is inspected and probed to evaluate for fraying and tears (Fig 3C). The accompanying video (Video 1) shows a typical anterosuperior labral tear with associated ecchymosis, fibrillation, and instability. A probe may be used to further evaluate the chondrolabral interface.
Fig 3.
Examples of central compartment pathology of a right hip viewed from modified anterior portal in the supine position. (A) Fat pad inflammation within the cotyloid space. (B) Ligamentum teres (LT) tear. (C) Labral ecchymosis from impingement of the chondrolabral junction. (FH, femoral head; FP, fat pad inflammation; L, labral ecchymosis.)
© 2017 Allston J. Stubbs, M.D. All rights reserved.
Diagnostic Arthroscopy of the Peripheral Compartment of the Hip
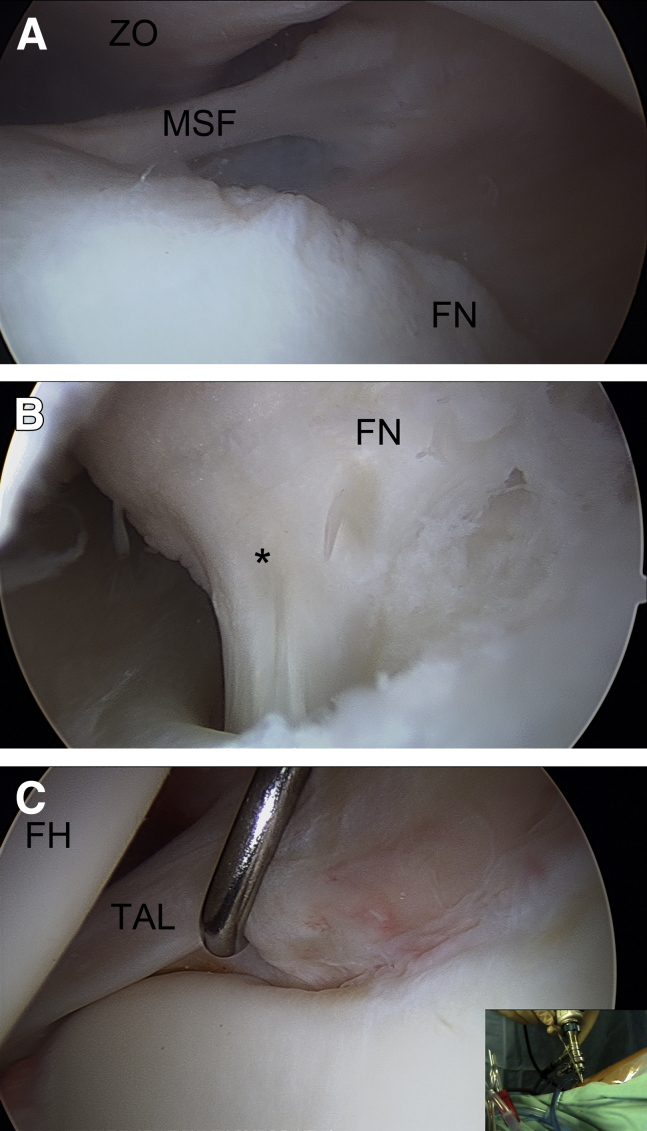
Peripheral compartment entry is facilitated as a direct transition from the central to the peripheral space. The arthroscope is positioned in the modified anterior portal with instrumentation in the anterolateral portal. Strategic retraction of intra-articular soft tissue by placing the camera against the zona orbicularis while viewing through the midanterior portal may optimize the effective visual space of the peripheral compartment (Fig 4A). The medial femoral circumflex artery and retinacular vessels can be visualized along the posterior-superior head-neck junction with gentle hip internal rotation and relative hip extension (Fig 4B). The location of the vessels along the lateral synovial fold helps define the safe zone for the femoroplasty; the safe zone is reported from the 12- to 6-o'clock position.7 The anterior labrum transition to the transverse acetabular ligament may also be visualized (Fig 4C).
Fig 4.
Peripheral compartment of a right hip viewed from the modified anterior portal in the supine position. (A) View of the medial synovial fold, which is an important reference for the medial limit for osteochondroplasty in femoroacetabular impingement. (B) The medial retinacular vessels (*) along the femoral neck (FN). (C) The anterior labral transition to the transverse acetabular ligament (TAL) is revealed by the probe. The picture inlay shows the hand position of the arthroscopy in the modified anterior portal. (FH, femoral head; MSF, medial synovial fold; ZO, zona orbicularis.)
© 2017 Allston J. Stubbs, M.D. All rights reserved.
Relative hip flexion then creates an effective anterior space that permits evaluation of the anterior femoral head-neck junction. In the setting of femoroacetabular impingement, the anterior head-neck junction may exhibit signs of cam impingement comprising the findings of convexity, fibrillation, and discoloration. Occasionally, visualization may be improved with a peripheral synovectomy performed with a 4.5-mm shaver.
Additional visualization in the peripheral compartment is achieved with relative hip flexion and external rotation. This maneuver exposes the inferior head-neck junction and medial synovial fold. Advancement of the camera along the inferior head-neck junction improves visualization of the posterior-inferior capsular recess and the zona orbicularis. Loose bodies are frequently encountered in the posterior-inferior capsular recess. Direct visualization of the anterior-superior head-neck junction is optimized with hip flexion of approximately 45° and neutral rotation. This surgical position optimizes the visualization of a majority of cam lesions in femoroacetabular impingement pathology. At this point, the diagnostic hip evaluation is complete, and the surgeon may address all pathologies.
Discussion
Arthroscopic evaluation of the hip joint is a valuable surgical tool for diagnostic and therapeutic hip procedures. Although the preoperative plan will be based on a preliminary diagnosis, a thorough diagnostic arthroscopy will prevent missing secondary or subtler diagnoses. Proper patient positioning and portal establishment is critical to efficiently and effectively perform a diagnostic hip arthroscopy (Table 3).3, 4 Systematic review of the anatomy will ensure that all pathology is identified. We strategically evaluate and treat the central compartment first and then progress to the peripheral compartment of the hip. This approach allows treatment of the most to least symptomatic pathology. During our basic diagnostic hip arthroscopy, we prefer to use the modified anterior portal and the anterolateral portal to view the internal hip anatomy.
Table 3.
Portal Pearls and Pitfalls for Hip Arthroscopy in the Supine Position
| Advantage | Pearls | Pitfalls | |
|---|---|---|---|
| Anterolateral portal | Portal may be directed between the tensor fascia lata and gluteus medius in active patients | Starting point may be identified by palpating the greater trochanter with the surgeon's long finger (left hand for a right hip) and using the index finger to palpate approximately 1 cm anterior and superior to the greater trochanter | Superior gluteal nerve is 44-64 mm superior to the portal5, 6 |
| Distention of the joint will aid in separating the capsule from the labrum and facilitate entry into the joint | The labrum may be pierced by the cannula if the joint is not distended | ||
| Anterior portal | Site of anterior portal is at the intersection of a sagittal line from the ASIS distally and a transverse line along the superior margin of the greater trochante. | Direct a spinal needle 30° medial and 45° cephalad under direct visualization into the joint6 | Lateral femoral cutaneous nerve branches are frequently within 2-4 mm of the portal |
| Modified anterior portal | A more lateral and distal variation of the anterior portal | May enable more accurate intra-articular triangulation | Lateral femoral cutaneous nerve is still at risk but has typically branched at this distal level |
| An isosceles triangle may be used where the long aspect of the triangle is equidistant from the anterior portal and the anterolateral portal |
ASIS, anterior superior iliac spine.
A mastery of basic hip arthroscopy will provide the surgeon with the diagnostic information to perform more advanced therapeutic procedures. Although it is possible to perform an arthroscopy through a single portal,8 the procedure relies on special instrumentation adapted from the knee, advanced maneuvers, and specific patient characteristics to be effective for therapeutic arthroscopy. We consequently endorse the above strategy for performing the diagnostic arthroscopy. We typically prefer a modified anterior portal for central compartment access, which can also be helpful for placing labral anchors. The modified anterior portal was originally described as an equilateral triangle between the anterior portal, anterolateral portal, and the midanterior portal; however, our preference is to further modify it to an isosceles triangle, with the long aspects of the triangle equidistant from the anterior portal and the anterolateral portal as depicted (Fig 1). The 2-portal technique is not without risks, and both portals place neurovascular structures at risk.5, 6 The anterolateral portal places the superior gluteal nerve and the sciatic nerve at risk, whereas the modified anterior portal places the lateral femoral cutaneous nerve and lateral femoral cutaneous artery at risk. These risks can be minimized by proper anatomic placement of the portal and by establishing the safer anterolateral portal prior to establishing additional portals (Table 3). If these portals are insufficient for performing additional procedures, supplementary accessory portals can be placed to facilitate viewing of pathologic structures or access to particular areas of hip joint anatomy. An effective diagnostic hip arthroscopy should identify not only the preoperatively diagnosed pathology but also subtler pathology that could otherwise be missed. A thorough diagnostic hip arthroscopy will provide the necessary intraoperative information for the surgeon to most effectively treat the patient with hip pain.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: A.V.S. receives support from Smith & Nephew (grant for suture anchor and graft research). S.M. receives support from Wake Forest Innovations Spark Award Research Grant (institutional research funding for development of a tensioning device for use during rotator cuff tendon repair and similar tendon repair surgery); and receives institutional support for patent (with MF Tanaka and CJ Tuohy) “Tissue tensioning devices and related methods, Patent Number 08926626,” to Wake Forest University Health Sciences. A.J.S. is a board member in the International Society of Hip Arthroscopy (no money paid); consultant for Smith & Nephew Endoscopy (no money/financial benefit received for this project); employee of Wake Forest Baptist Health; receives research grant support from Bauerfeind, not related to this project; has patents pending not related to project; is a shareholder in Johnson & Johnson; is a committee member of the Arthroscopy Association of North America and receives travel support; and is on the editorial board of the Journal of Arthroscopy.
Supplementary Data
Diagnostic hip arthroscopy. The video shows our preferred systematic approach to the diagnostic hip arthroscopy of a right hip using a 2-portal (anterolateral and modified anterior) technique. The central compartment is first assessed with the hip in traction and the arthroscope in the modified anterior portal and instrumentation in the anterolateral portal. The traction is then relaxed and the operative extremity is dynamically assessed. The hip remains out of traction and placed in flexion for diagnostic assessment and treatment of the peripheral compartment. © 2017 Allston J. Stubbs, M.D. All rights reserved.
References
- 1.Montgomery S.R., Ngo S.S., Hobson T. Trends and demographics in hip arthroscopy in the United States. Arthroscopy. 2013;29:661–665. doi: 10.1016/j.arthro.2012.11.005. [DOI] [PubMed] [Google Scholar]
- 2.Bozic K.J., Chan V., Valone F.H., 3rd, Feeley B.T., Vail T.P. Trends in hip arthroscopy utilization in the United States. J Arthroplasty. 2013;28(suppl):140–143. doi: 10.1016/j.arth.2013.02.039. [DOI] [PubMed] [Google Scholar]
- 3.Mannava S., Howse E.A., Stone A.V., Stubbs A.J. Basic hip arthroscopy: Supine patient positioning and dynamic fluoroscopic evaluation. Arthrosc Tech. 2015;4:e391–e396. doi: 10.1016/j.eats.2015.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Howse E.A., Botros D.B., Mannava S., Stone A.V., Stubbs A.J. Basic hip arthroscopy: Anatomic establishment of arthroscopic portals without fluoroscopic guidance. Arthrosc Tech. 2016;5:e247–e250. doi: 10.1016/j.eats.2015.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Robertson W.J., Kelly B.T. The safe zone for hip arthroscopy: A cadaveric assessment of central, peripheral, and lateral compartment portal placement. Arthroscopy. 2008;24:1019–1026. doi: 10.1016/j.arthro.2008.05.008. [DOI] [PubMed] [Google Scholar]
- 6.Byrd J.W., Pappas J.N., Pedley M.J. Hip arthroscopy: An anatomic study of portal placement and relationship to the extra-articular structures. Arthroscopy. 1995;11:418–423. doi: 10.1016/0749-8063(95)90193-0. [DOI] [PubMed] [Google Scholar]
- 7.McCormick F., Kleweno C.P., Kim Y.J., Martin S.D. Vascular safe zones in hip arthroscopy. Am J Sports Med. 2011;39(suppl):64S–71S. doi: 10.1177/0363546511414016. [DOI] [PubMed] [Google Scholar]
- 8.Mannava S., Howse E.A., Kelsey T.J., Barnes R.H., Antunes A., Stubbs A.J. Single-portal arthroscopy of the central compartment of the hip. Arthrosc Tech. 2015;4:e273–e277. doi: 10.1016/j.eats.2015.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Diagnostic hip arthroscopy. The video shows our preferred systematic approach to the diagnostic hip arthroscopy of a right hip using a 2-portal (anterolateral and modified anterior) technique. The central compartment is first assessed with the hip in traction and the arthroscope in the modified anterior portal and instrumentation in the anterolateral portal. The traction is then relaxed and the operative extremity is dynamically assessed. The hip remains out of traction and placed in flexion for diagnostic assessment and treatment of the peripheral compartment. © 2017 Allston J. Stubbs, M.D. All rights reserved.